Abstract
Context
Increased frontal-plane knee motion during functional tasks, or medial knee displacement, is a predictor of noncontact anterior cruciate ligament injury and patellofemoral pain. Intervention studies that resulted in a reduced risk of knee injury included some form of feedback to address aberrant lower extremity movement patterns. Research on integrating feedback into single-legged tasks and the ability to train 1 task and test another is limited.
Objective
To determine if adding real-time visual biofeedback to common lower extremity exercises would improve single-legged landing mechanics in females with medial knee displacement.
Design
Cohort study.
Setting
University laboratory.
Patients or Other Participants
Twenty-four recreationally active females with medial knee displacement were randomized to a visual-biofeedback group (n = 12; age = 19.75 ± 0.87 years, height = 165.32 ± 8.69 cm, mass = 62.41 ± 8.91 kg) or a control group (n = 12; age = 19.75 ± 0.97 years, height = 166.98 ± 6.89 cm, mass = 59.98 ± 6.24 kg).
Intervention(s)
Individuals in the feedback group viewed a real-time digital model of their body segments generated by Microsoft Kinect. The skeletal model changed color according to the knee-abduction angle of the test limb during the exercise tasks.
Main Outcome Measure(s)
Participants completed 3 trials of the single-legged drop vertical jump (SL-DVJ) while triplanar kinematics at the trunk, hip, knee, and ankle were collected via 3-dimensional motion capture. The feedback and control groups completed lower extremity exercises with or without real-time visual biofeedback, respectively. After the intervention, participants completed 3 additional trials of the SL-DVJ.
Results
At baseline, the feedback group had 3.83° more ankle eversion than the control group after initial contact. After the intervention, the feedback group exhibited 13.03° more knee flexion during the flight phase of the SL-DVJ and 6.16° less knee abduction after initial contact than the control group. The feedback group also demonstrated a 3.02° decrease in peak knee-abduction excursion compared with the baseline values (P = .008).
Conclusions
Real-time visual biofeedback immediately improved faulty lower extremity kinematics related to knee-injury risk. Individuals with medial knee displacement adjusted their movement patterns after a single training session and reduced their medial knee motion during a dynamic task.
Keywords: real-time feedback, corrective exercise, dynamic knee valgus
Key Points
Individuals with visually observed medial knee displacement improved their single-legged landing patterns after 1 training session with real-time visual biofeedback.
Improvements to lower extremity kinematics were observed in a task that was different from the training exercises.
After the intervention, 75% of individuals who received real-time biofeedback did not display medial knee displacement during the single-legged squat test.
Aberrant neuromuscular control has been identified as a contributor to lower extremity injury risk. Altered peak lower extremity kinematic variables captured during functional tasks have commonly been recognized in individuals who go on to sustain noncontact knee injuries.1,2 In particular, increased frontal-plane knee motion during functional tasks, known as medial knee displacement (MKD), has been established as a predictor of noncontact anterior cruciate ligament (ACL) injury2 and patellofemoral pain.3
Compared with males, females sustain up to 6 times more noncontact ACL injuries4 and are twice as likely to develop patellofemoral pain.5 They have also demonstrated a greater maximal knee-abduction angle and more total knee-abduction motion during dynamic activities, which is consistent with the MKD movement pattern.1 Medial knee displacement can be identified visually in the frontal plane without equipment and is present when the knee translates medially past the first ray of the foot during a single-legged squat (SLS).6 Hewett et al7 theorized that landing with the knee in an abducted position decreases joint stability, making the knee more susceptible to injury. Furthermore, researchers1 have suggested that this biomechanical alteration is one reason why females sustain more noncontact ACL injuries than males.
Injury-prevention programs have been developed and implemented to correct these faulty lower extremity biomechanics, particularly in female athletes. Success in decreasing the injury risk can be attributed to emphasizing correct landing techniques7 and increasing lower extremity strength8 and proprioception.2 Identifying individuals who display MKD on visual screenings9 may provide insight into who may be at heightened risk and would benefit the most from intervention. Including multiple neuromuscular training components8 (eg, plyometrics, strength training, balance and core stability training, and feedback) may also optimize the effectiveness of these programs. In a meta-analysis of neuromuscular programs for injury prevention, Hewett et al10 concluded that incorporating feedback and analysis of technique during functional tasks decreased the ACL injury risk, whereas those investigators who did not include feedback found no risk reduction.
Cognitive function has been cited as an integral component to the transfer of learned movement from a constrained to a more dynamic environment.11 Using feedback in training or rehabilitation sessions promotes problem solving and intrinsic learning and effectively enhances the learning of new movement patterns. Visual feedback has been implemented in real time12 or posttask13 to target neuromuscular alterations. Real-time visual biofeedback (RTF) enables individuals to observe their movements and make immediate biomechanical alterations.14 Therefore, it may improve on traditional postresponse methods in which feedback is provided after the task is completed.14
Several limitations existed in terms of how RTF was used in previous investigations. For example, positive alterations to lower extremity kinematics were demonstrated when RTF was implemented during both tuck-jump15 and jump-landing tasks.16 However, clinicians have frequently prescribed corrective exercises that are slow, of low intensity, and repetitive.11 Little evidence supports the use of visual biofeedback to alter the mechanics of tasks in which the participants were not trained.12 Many authors who used RTF to improve the mechanics associated with knee-injury risk have also evaluated outcomes using bilateral tasks,12,17 although numerous athletic movements occur on one leg (eg, landing, cutting). Researchers12,15,18 evaluated this intervention in healthy individuals, but its use in a population demonstrating kinematic risk factors for lower extremity injury has not been established. Finally, lower extremity RTF is often provided using a mirror19 or video camera,15 but investigators20 have suggested that gaming systems may optimize motor learning. Therefore, the purpose of our study was to determine if adding RTF, generated by Microsoft Kinect (Microsoft Corp, Redmond, WA), to traditional lower extremity exercises would improve single-legged landing mechanics in females with MKD.
METHODS
Study Design
We conducted a cohort study to evaluate the influence of a single session of exercise with RTF on lower extremity kinematics in individuals with clinically observed MKD. The independent variables were group (visual biofeedback, control) and time (preintervention, postintervention), and the dependent variables were 3-dimensional trunk, hip, knee, and ankle kinematics during a single-legged drop–vertical-jump (SL-DVJ) task.
Participants
A total of 24 self-reported recreationally active females (age range, 15–40 years) with visually observed MKD6 were recruited from the local university community. Recreationally active was defined as participating in activity for 30 minutes per day at least 3 days per week. We used the SLS test6 to determine if the MKD movement pattern was present. Participants stood on 1 limb with their opposite knee flexed to approximately 90° and hands folded across their chests. They were instructed to squat down as low as comfortably possible for 2 seconds and then return to the starting position for 2 seconds. We used a metronome (Pulse Metronome app for iPhone version 2.13; Pulse Technologies, Inc, Quakertown, PA) to ensure consistency in the task duration and provided a 30-second rest period after each complete SLS trial. Both limbs were screened using the SLS test for MKD through visual observation by 1 investigator (A.N.M.), who demonstrated excellent intersession agreement (κ = 0.83).21 Participants were considered to have MKD if the midpoint of the patella crossed medial to the first ray in at least 3 of 5 SLS trials.6 Participants wore self-selected athletic shoes throughout the session, including the screening. If a participant presented with MKD on both sides, the test limb was randomly selected.
Exclusion criteria consisted of any known neurologic condition resulting in decreased balance or proprioception, infection near the trunk or lower limbs, current or previous use of an orthotic device, or known pregnancy. Participants with a history of lower extremity injury were not excluded as long as they were able to complete the tasks during the testing session. Individuals who met the inclusion but none of the exclusion criteria were enrolled in the study. No between-groups differences were observed in participant demographics (Table 1). All participants provided written informed consent, and the study was approved by the University of Virginia's Institutional Review Board for Human Subjects Research.
Table 1.
Participant Demographics
| Characteristic |
Group, Mean ± SD |
P Value |
|
| Visual Biofeedback (n = 12) |
Control (n = 12) |
||
| Age, y | 19.75 ± 0.87 | 19.75 ± 0.97 | .86 |
| Height, cm | 165.32 ± 8.69 | 166.98 ± 6.89 | .18 |
| Mass, kg | 62.41 ± 8.91 | 59.98 ± 6.24 | .47 |
Instruments
Three-dimensional joint kinematics of the trunk, hip, knee, and ankle were measured using a 12-camera motion-analysis system (Vicon Motion Systems, Oxford, United Kingdom) and MotionMonitor software (version 9; Innovative Sports Training Inc, Chicago, IL) at a sampling rate of 250 Hz. Thirty-two 14-mm retroreflective markers were configured in 8 clusters of 4 and secured on semirigid thermoplastic plates. Clusters were affixed bilaterally over the dorsum of the foot, the lateral shank, the lateral thigh, the sacrum, and the thoracic spine with elastic tape.22 Height and mass were collected, and joint centers were digitized using the stylus. A nonconductive force plate embedded in the treadmill (Bertec Corp, Columbus, OH) with a sampling rate of 1000 Hz was used to determine initial contact during the SL-DVJ.
Visual feedback was provided for the feedback group through a Microsoft Kinect camera system (model v2) and a television monitor. All Kinect data were collected at 30 Hz and processed in real time with VirtualCoach software (Kinetech Labs Inc, Charlottesville, VA), which is a custom Visual Studio program (Community 2015; Microsoft Corp), to provide feedback on the knee-abduction angle during the exercise trials. The Kinect sensor was positioned 140 cm from the center of the testing area at a height of 70 cm facing the participant. If the participant exited the Kinect's field of view during a trial, the researcher adjusted the sensor as necessary and deleted the previous trial.
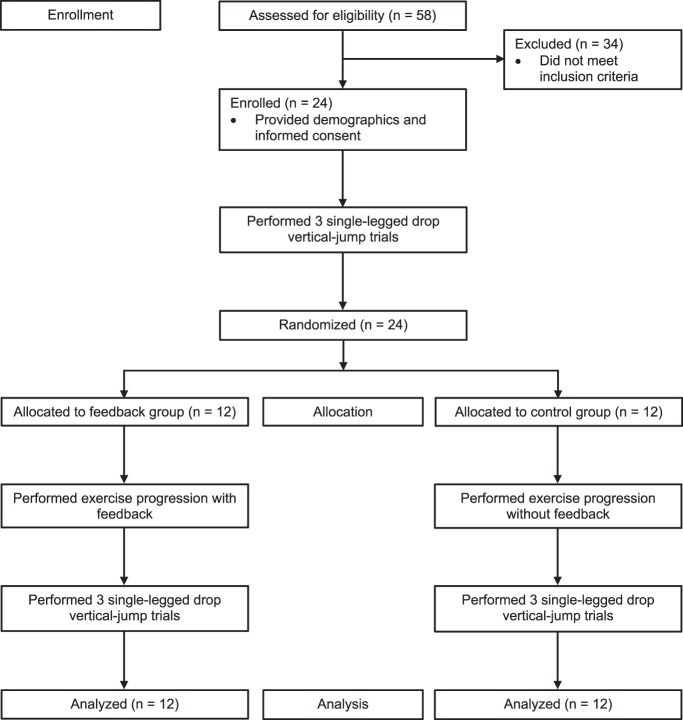
Procedures
The procedures are outlined in Figure 1. After enrollment, participants were set up for motion analysis, and a 5-second bipedal quiet-standing trial was recorded for kinematic normalization. Next, they performed the SL-DVJ task9 using the test limb from a 10-cm box that was positioned at the leading edge of the force plate. They were instructed to drop forward toward the force plate and transition to a maximal vertical jump on ground contact. A target was provided directly above the force plate to minimize forward or lateral trajectory.23 Participants were allotted as many practice trials as necessary to ensure proper form, and data from 3 SL-DVJ trials were collected and used for analysis.
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) flow diagram.
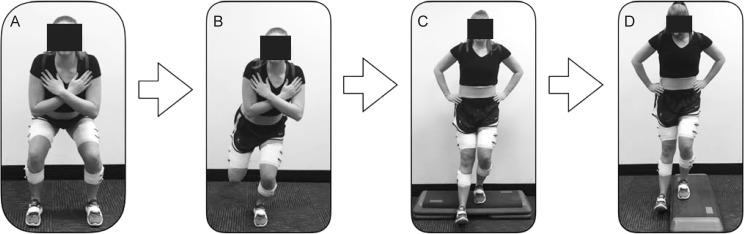
Participants in both groups (feedback, control) completed 4 exercise tasks immediately after baseline testing of the SL-DVJ (Figure 2). Exercises were the double-legged squat, SLS, single-legged step down, and lateral step down and were selected because of their use in the clinical setting and their slow, low-intensity, repetitive nature. Ten repetitions of each exercise were completed, and the single-legged exercises were conducted only on the limb of interest. Participants in the feedback group viewed a real-time digital model of their body segments during the exercise tasks. The skeletal model, generated by Kinect in conjunction with the VirtualCoach software, changed color as the knee-abduction angle2 in the test limb changed (≥8° = red, 5° to <8° = yellow, <5° = green) and was projected onto a monitor for visualization. Participants in the feedback group were instructed to control their medial knee motion so that they performed the exercises while keeping the knee-abduction angle in the green category. No other feedback or coaching was provided. Participants in the control group received no feedback during the exercises.
Figure 2.
Exercise progression. A, Double-legged squat. B, Single-legged squat. C, Single-legged step down. D, Lateral step down.
All participants completed a postintervention assessment immediately after the intervention. The testing procedures were identical to those conducted for kinematics during the SL-DVJ baseline assessment. After the postintervention assessment, participants were screened for MKD with the SLS test.
Data Processing
The researcher who performed the data processing and analysis (A.N.M.) was blinded to group allocation. Kinematic analyses were conducted for the preintervention and postintervention SL-DVJs over a 300-millisecond time epoch beginning 100 milliseconds before initial contact through 200 milliseconds after initial contact.24 Initial contact was defined as the time at which the vertical ground reaction force exceeded 20 N.25 The 300-millisecond time epochs were reduced to 100 frames so that each frame represented 1% of the task, and the mean of the 3 trials was used for analysis.24 Data were filtered with a fourth-order, low-pass Butterworth filter with a cutoff frequency of 14.5 Hz26 and normalized to the kinematics at quiet standing. Joint rotations for the trunk, hip, knee, and ankle were calculated based on a right-hand rule using the Euler rotation method (Y, X′, Z″).25,27
Statistical Analysis
Continuous Analysis
We used Excel (version 16.15; Microsoft Corp) to construct the time series curve analyses for normalized lower extremity kinematics across 100% of the SL-DVJ. Group means and associated 90% confidence intervals (CIs) were plotted for the entire task.28,29 Areas where the CIs did not overlap between the groups for at least 3 consecutive percentage points were considered different.28,29 Mean differences and associated standard deviations were calculated for the identified increments.28,29
Discrete Analysis
Three-dimensional kinematic peaks were extracted and compared with the kinematics during quiet standing to calculate total kinematic excursions during the 300-millisecond time epoch. A 2 × 2 mixed-model analysis of variance was conducted. The between-subjects factor was group (feedback, control) and the within-subject factor with repeated measures was time (preintervention, postintervention). The α level was set a priori at .05 for all analyses, and we did not control for multiple comparisons, as recommended by Hopkins et al.30 Cohen d effect sizes and associated 95% CIs were also calculated to estimate the magnitude of the difference between groups. Effect sizes were interpreted as large (≥0.80), moderate (0.50–0.79), small (0.20–0.49), or trivial (<0.20).31 Data were analyzed using SPSS (version 24.0; IBM Corp, Armonk, NY).
RESULTS
Continuous Analysis
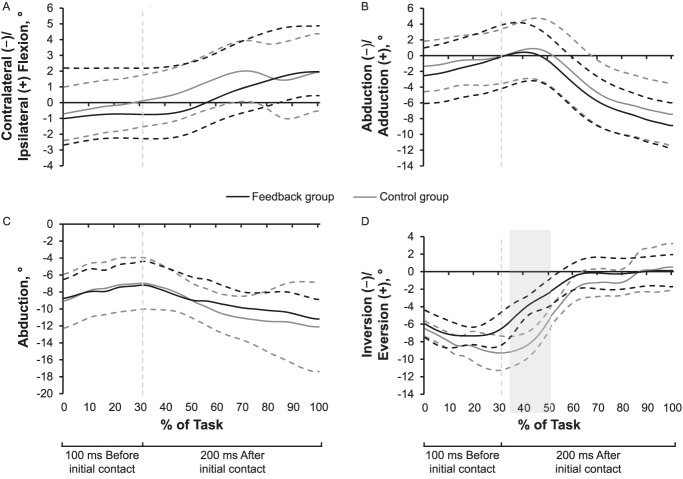
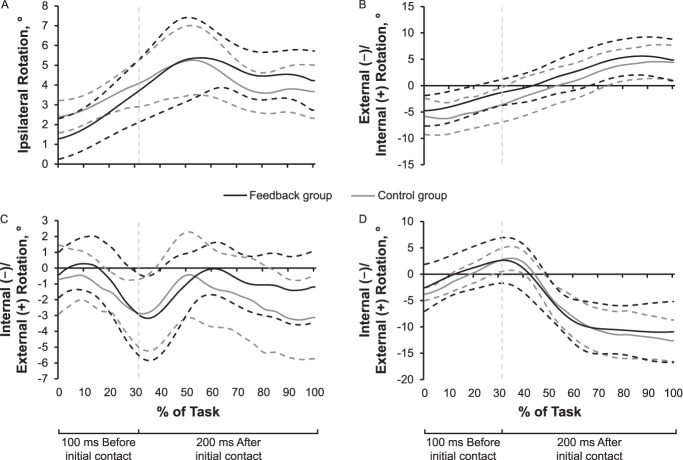
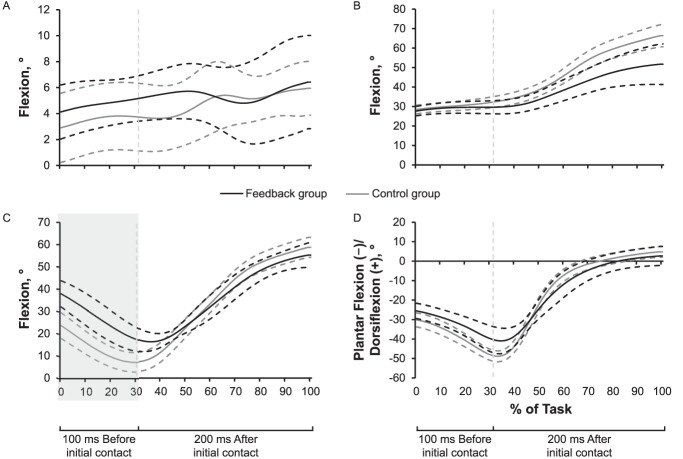
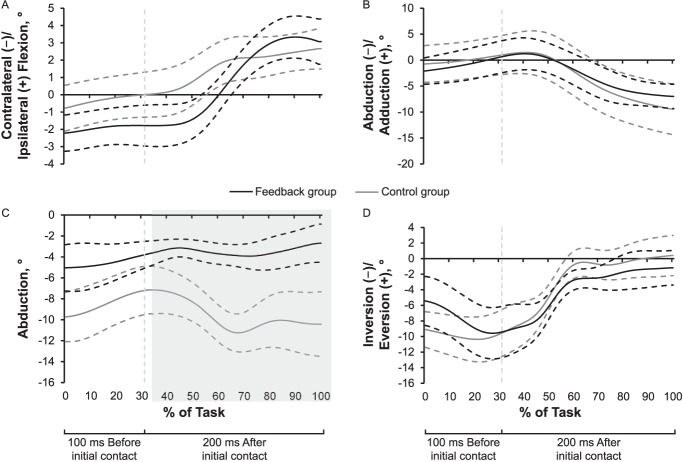
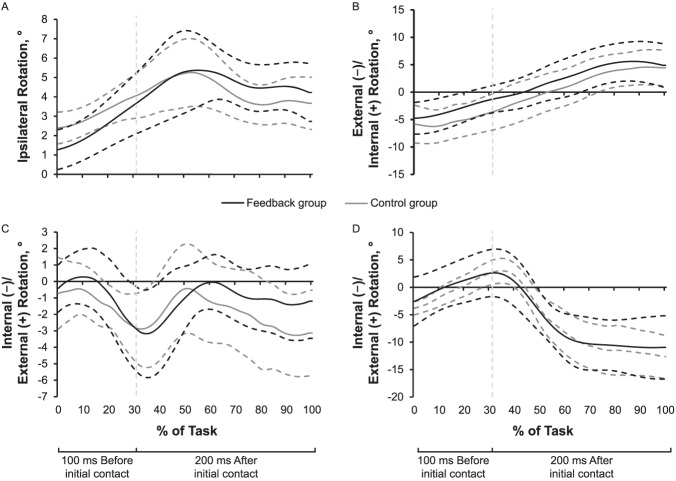
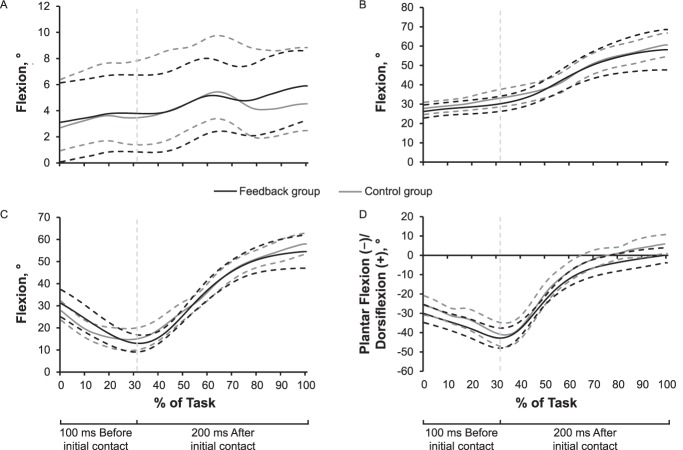
A between-groups difference existed at baseline, such that the feedback group had about 3.83° more ankle eversion than the control group for 17% of the task after initial contact (Figure 3). No other between-groups differences were observed preintervention (Figures 3 through 5). At postintervention, the feedback group exhibited 13.03° more knee flexion than the control group during the first 100 milliseconds before initial contact (0%–31% of the task; Figure 6) and 6.16° less knee abduction than the control group for the 200 milliseconds after initial contact (34%–100%; Figure 7). No other between-groups differences were observed postintervention (Figures 6 through 8).
Figure 3.
Baseline frontal-plane kinematics of the A, trunk, B, hip, C, knee, and D, ankle during the single-legged drop vertical jump. The group means ± 90% confidence intervals throughout the task are indicated by the solid and dotted lines, respectively. The vertical dotted line indicates initial contact. The gray box indicates a difference between groups at the ankle for 17% of the task after initial contact.
Figure 5.
Baseline transverse-plane kinematics of the A, trunk, B, hip, C, knee, and D, ankle during the single-legged drop vertical jump. The group means ± 90% confidence intervals throughout the entire task are indicated by the solid and dotted lines, respectively. The vertical dotted line indicates initial contact.
Figure 6.
Postintervention sagittal-plane kinematics of the A, trunk, B, hip, C, knee, and D, ankle during the single-legged drop vertical jump. The group means ± 90% confidence intervals throughout the entire task are indicated by the solid and dotted lines, respectively. The vertical dotted line indicates initial contact. The gray box indicates a difference between groups at the knee before initial contact.
Figure 7.
Postintervention frontal-plane kinematics of the A, trunk, B, hip, C, knee, and D, ankle during the single-legged drop vertical jump. The group means ± 90% confidence intervals throughout the entire task are indicated by the solid and dotted lines, respectively. The vertical dotted line indicates initial contact. The gray box indicates a difference between groups at the knee after initial contact.
Figure 8.
Postintervention transverse-plane kinematics of the A, trunk, B, hip, C, knee, and D, ankle during the single-legged drop vertical jump. The means ± 90% confidence intervals throughout the entire task are indicated by the solid and dotted lines, respectively. The vertical dotted line indicates initial contact.
Figure 4.
Baseline sagittal-plane kinematics of the A, trunk, B, hip, C, knee, and D, ankle during the single-legged drop vertical jump. The group means ± 90% confidence intervals throughout the entire task are indicated by the solid and dotted lines, respectively. The vertical dotted line indicates initial contact.
Discrete Analysis
Whereas several alterations to peak kinematic excursions appeared to exist, most CIs crossed zero (Tables 2 and 3). The only meaningful change was decreased knee abduction in the feedback group from preintervention (7.95° ± 3.80°) to postintervention (4.93° ± 1.64°), as we observed a large effect with a CI that did not cross zero (Cohen d = −1.03; 95% CI = −1.88, −0.18; Table 3).
Table 2.
Preintervention-Postintervention Single-Legged Drop–Vertical-Jump Hip and Trunk Peak Kinematic Excursions and Cohen d Effect Sizes With 95% Confidence Intervals (CIs)
| Variable |
Group |
P Value |
|||||||
| Visual Biofeedback |
Control |
||||||||
| Mean ± SD, ° |
Effect Sizea (95% CI) |
Mean ± SD, ° |
Effect Sizea (95% CI) |
||||||
| Preintervention |
Postintervention |
Preintervention |
Postintervention |
Time Main Effect |
Group Main Effect |
Group × Time Interaction |
|||
| Hip | |||||||||
| Flexion | 34.74 ± 15.16 | 30.10 ± 12.41 | −0.33 (−1.14, 0.47) | 33.92 ± 11.14 | 38.15 ± 12.21 | 0.36 (−0.44, 1.17) | .85 | .49 | .001b |
| Adduction | 9.34 ± 4.17 | 10.30 ± 1.89 | 0.30 (−0.51, 1.10) | 9.90 ± 3.78 | 11.90 ± 5.21 | 0.44 (−0.37, 1.25) | .03b | .47 | .42 |
| Internal rotation | 12.40 ± 4.70 | 10.58 ± 4.52 | −0.22 (−1.02, 0.58) | 11.61 ± 4.26 | 11.93 ± 5.81 | 0.06 (−0.74, 0.86) | .39 | .88 | .23 |
| Trunk | |||||||||
| Flexion | 7.56 ± 4.42 | 8.54 ± 3.71 | 0.14 (−0.66, 0.95) | 7.98 ± 2.99 | 8.03 ± 2.63 | 0.02 (−0.78, 0.82) | .37 | .97 | .42 |
| Ipsilateral flexion | 3.86 ± 2.20 | 4.51 ± 2.45 | 0.18 (−0.62, 0.99) | 4.94 ± 3.85 | 4.14 ± 1.82 | −0.27 (−1.07, 0.54) | .89 | .71 | .20 |
| Ipsilateral rotation | 6.15 ± 1.73 | 5.38 ± 1.65 | −0.19 (−0.99, 0.61) | 4.98 ± 2.75 | 7.12 ± 4.09 | 0.20 (−1.43, 0.42) | .11 | .79 | .002b |
A positive effect size indicates an increase in kinematic excursion postintervention.
Between-groups difference (P < .05).
Table 3.
Preintervention-Postintervention Single-Legged Drop–Vertical-Jump Ankle and Knee Peak Kinematic Excursions and Cohen d Effect Sizes With 95% Confidence Intervals (CIs)
| Variable |
Group |
P Value |
|||||||
| Visual Biofeedback |
Control |
||||||||
| Mean ± SD, ° |
Effect Sizea (95% CI) |
Mean ± SD, ° |
Effect Sizea 95% CI) |
||||||
| Preintervention, |
Postintervention |
Preintervention |
Postintervention |
Time Main Effect |
Group Main Effect |
Group × Time Interaction |
|||
| Ankle | |||||||||
| Dorsiflexion | 46.80 ± 6.60 | 45.94 ± 13.07 | −0.08 (−0.88, 0.72) | 49.45 ± 5.47 | 49.78 ± 10.16 | 0.04 (−0.76, 0.84) | .92 | .25 | .83 |
| Eversion | 9.08 ± 2.30 | 10.85 ± 2.09 | 0.81 (−0.03, 1.64) | 10.18 ± 4.83 | 11.28 ± 5.42 | 0.21 (−0.59, 1.02) | .24 | .49 | .78 |
| Internal rotation | 15.32 ± 7.59 | 17.73 ± 6.21 | 0.34 (−0.46, 1.15) | 15.69 ± 6.36 | 17.37 ± 8.03 | 0.23 (−0.57, 1.03) | .04b | >.99 | .70 |
| Knee | |||||||||
| Flexion | 43.26 ± 9.81 | 42.89 ± 7.54 | −0.04 (−0.84, 0.76) | 47.32 ± 10.28 | 52.45 ± 7.08 | 0.58 (−0.24, 1.40) | .10 | .05 | .06 |
| Abduction | 7.95 ± 3.80 | 4.93 ± 1.64 | −1.03 (−1.88, −0.18) | 6.98 ± 2.99 | 8.04 ± 3.85 | 0.31 (−0.50, 1.11) | .18 | .34 | .008b |
| Internal rotation | 8.09 ± 3.23 | 6.99 ± 3.65 | −0.32 (−1.12, 0.49) | 7.72 ± 2.41 | 8.45 ± 2.81 | 0.28 (−0.53, 1.08) | .83 | .52 | .33 |
A positive effect size indicates an increase in kinematic excursion postintervention.
Between-groups difference (P < .05).
Postintervention MKD Screening
At postintervention, 25% (n = 3) of the feedback group exhibited MKD on the SLS compared with 66.7% (n = 8) of the control group.
DISCUSSION
The purpose of our study was to determine if common lower extremity exercises augmented with visual feedback about knee-abduction angle improved landing kinematics during the SL-DVJ. We found improved knee frontal- and sagittal-plane kinematics in individuals who received visual feedback. Most importantly, the changes were observed during a task that was different from the feedback training program, and 75% (n = 9) of individuals in the feedback group did not display MKD during the SLS test postintervention.
At postintervention, the feedback group performed the SL-DVJ with 6.16° less knee abduction than the control group during the last 200 milliseconds (after initial contact) of the task (Figure 7). The feedback group also exhibited improved peak knee-abduction excursion postintervention, with a large meaningful effect (Table 2). These findings are similar to those of other researchers who have used RTF to correct lower extremity kinematics. Nyman and Armstrong16 noted improved knee-separation distance (a surrogate for MKD) during landing in young female gymnasts. Their athletes were trained with feedback on knee position during the drop vertical jump and tested during the same task. Ericksen et al18 studied individuals participating in a 4-week feedback program focused on the drop vertical jump. Although they did not observe lasting changes postintervention, they did not screen for faulty kinematic movement before the intervention. Therefore, differences may have been masked in participants who did not have faulty movement patterns at baseline.
In addition to kinematic feedback, RTF based on joint kinetics has also been used; however, the results have been inconsistent.12,17 After 2 sessions of RTF on knee-abduction moment, Beaulieu and Palmieri-Smith17 did not find any changes in landing mechanics during the drop vertical jump. In a pilot study, Ford et al12 compared kinematic- and kinetic-focused RTF provided during double-legged squats and reported that the kinetic feedback improved both knee-abduction moment and maximal knee-abduction angle during the drop vertical jump. They observed improvements using the concept of skill transfer, whereby the participants trained for tasks that were different from those on which they were tested. However, the sample size was small (n = 4), and the researchers evaluated only peak biomechanical variables instead of variables throughout the entire task. Our results were similar, albeit with a different form of RTF.
After the RTF intervention in our study, the feedback group exhibited more knee flexion before initial contact than the control group. When participants were both trained and tested using dynamic and plyometric tasks, Nyman and Armstrong16 demonstrated similar findings after initial contact. We did not detect sagittal-plane differences between groups after initial contact. However, our findings could be attributed to preparation for the landing and may correspond with the decreased knee abduction exhibited by the feedback group. These individuals may have been adjusting their movement strategy to place themselves in a better position for the landing. Chappell et al32 showed that females tended to exhibit less knee and hip flexion in the flight phase before landing than males and hypothesized that these results could relate to a difference in ACL loading during landing. The sagittal-plane findings that we observed at the knee before initial contact could lead to decreased forces at the knee on landing.
Researchers33,34 have consistently reported that feedback using an external focus of attention (ie, the movement effect) rather than an internal focus of attention (ie, one's own movements) is a more effective strategy when introducing motor-learning skills related to sport. For example, an athlete would respond better to instructions to “reach toward the cone with your knee” than “keep your knee over your foot.”20 The underlying mechanism of externally focused feedback is automatic or unconscious neurologic processes,35 which provide individuals with more resources to dedicate to other elements during activity (eg, field conditions, other athletes).20 In contrast, internally focused feedback promotes more conscious control, which constrains the motor system and interferes with this automaticity (ie, the constrained-action hypothesis).35 Furthermore, although posttask feedback has been successful in altering lower extremity movement patterns,13 RTF has been hypothesized to enhance these effects by supplying a constant external reminder during performance of the task, thereby reducing the individual's inclination to concentrate on his or her own movements (ie, internal focus).36–38
Our feedback technique did not require a motion-capture laboratory. The Kinect is a cost-effective device that has excellent measurement properties when compared with the criterion standard 3-dimensional motion capture.39 The efficacy of this method has shown great potential for implementation in a variety of clinical and sport-specific environments, improving participant engagement and compliance.20 In addition, enhancing corrective exercises in this manner reduces the need for constant clinician oversight and offers the user specific and individualized feedback.
We acknowledge that our study had limitations. Although we are the first to evaluate the concept of skill transfer in combination with visual feedback aimed at improving lower extremity kinematics in individuals with MKD, we analyzed only the immediate effects of the intervention. We do not know how long these alterations are retained or how many sessions are needed to make permanent changes to dynamic movement strategies. We also do not know if combining multiple forms of feedback would improve these findings.
CONCLUSIONS
Real-time feedback using Microsoft Kinect facilitated immediate improvements in aberrant kinematics. Individuals with visually observed MKD were able to adjust their single-legged landing patterns after 1 training session. Researchers should evaluate the long-term acquisition and retention of movement-pattern alterations and seek to incorporate this intervention into neuromuscular-training and injury-prevention programs.
REFERENCES
- 1.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35(10):1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 2.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 3.Myer GD, Ford KR, Barber Foss KD, et al. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech (Bristol, Avon) 2010;25(7):700–707. doi: 10.1016/j.clinbiomech.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34(2):86–92. [PMC free article] [PubMed] [Google Scholar]
- 5.Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(5):725–730. doi: 10.1111/j.1600-0838.2009.00996.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mauntel TC, Frank BS, Begalle RL, Blackburn JT, Padua DA. Kinematic differences between those with and without medial knee displacement during a single-leg squat. J Appl Biomech. 2014;30(6):707–712. doi: 10.1123/jab.2014-0003. [DOI] [PubMed] [Google Scholar]
- 7.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24(6):765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 8.Yoo JH, Lim BO, Ha M, et al. A meta-analysis of the effect of neuromuscular training on the prevention of the anterior cruciate ligament injury in female athletes. Knee Surg Sports Traumatol Arthrosc. 2010;18(6):824–830. doi: 10.1007/s00167-009-0901-2. [DOI] [PubMed] [Google Scholar]
- 9.Dingenen B, Malfait B, Nijs S, et al. Can two-dimensional video analysis during single-leg drop vertical jumps help identify non-contact knee injury risk? A one-year prospective study. Clin Biomech (Bristol, Avon) 2015;30(8):781–787. doi: 10.1016/j.clinbiomech.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 10.Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34(3):490–498. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- 11.Bennett R. Injury Prevention and Rehabilitation in Sport. Marlborough, United Kingdom: Crowood Press Ltd; 2015. [Google Scholar]
- 12.Ford KR, DiCesare CA, Myer GD, Hewett TE. Real-time biofeedback to target risk of anterior cruciate ligament injury: a technical report for injury prevention and rehabilitation. J Sport Rehabil. 2015;24(2) doi: 10.1123/jsr.2013-0138. [DOI] [PubMed] [Google Scholar]
- 13.Onate JA, Guskiewicz KM, Marshall SW, Giuliani C, Yu B, Garrett WE. Instruction of jump-landing technique using videotape feedback: altering lower extremity motion patterns. Am J Sports Med. 2005;33(6):831–842. doi: 10.1177/0363546504271499. [DOI] [PubMed] [Google Scholar]
- 14.Winstein CJ. Knowledge of results and motor learning: implications for physical therapy. Phys Ther. 1991;71(2):140–149. doi: 10.1093/ptj/71.2.140. [DOI] [PubMed] [Google Scholar]
- 15.Stroube BW, Myer GD, Brent JL, Ford KR, Heidt RS, Jr, Hewett TE. Effects of task-specific augmented feedback on deficit modification during performance of the tuck-jump exercise. J Sport Rehabil. 2013;22(1):7–18. doi: 10.1123/jsr.22.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nyman E, Jr, Armstrong CW. Real-time feedback during drop landing training improves subsequent frontal and sagittal plane knee kinematics. Clin Biomech (Bristol, Avon) 2015;30(9):988–994. doi: 10.1016/j.clinbiomech.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 17.Beaulieu ML, Palmieri-Smith RM. Real-time feedback on knee abduction moment does not improve frontal-plane knee mechanics during jump landings. Scand J Med Sci Sports. 2014;24(4):692–699. doi: 10.1111/sms.12051. [DOI] [PubMed] [Google Scholar]
- 18.Ericksen HM, Thomas AC, Gribble PA, Armstrong C, Rice M, Pietrosimone B. Jump-landing biomechanics following a 4-week real-time feedback intervention and retention. Clin Biomech (Bristol, Avon) 2016;32:85–91. doi: 10.1016/j.clinbiomech.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 19.Willy RW, Davis IS. Varied response to mirror gait retraining of gluteus medius control, hip kinematics, pain, and function in 2 female runners with patellofemoral pain. J Orthop Sports Phys Ther. 2013;43(12):864–874. doi: 10.2519/jospt.2013.4516. [DOI] [PubMed] [Google Scholar]
- 20.Benjaminse A, Gokeler A, Dowling AV, et al. Optimization of the anterior cruciate ligament injury prevention paradigm: novel feedback techniques to enhance motor learning and reduce injury risk. J Orthop Sports Phys Ther. 2015;45(3):170–182. doi: 10.2519/jospt.2015.4986. [DOI] [PubMed] [Google Scholar]
- 21.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 22.Chang M, Slater LV, Corbett RO, Hart JM, Hertel J. Muscle activation patterns of the lumbo-pelvic-hip complex during walking gait before and after exercise. Gait Posture. 2017;52:15–21. doi: 10.1016/j.gaitpost.2016.11.016. [DOI] [PubMed] [Google Scholar]
- 23.Ford KR, Myer GD, Smith RL, Byrnes RN, Dopirak SE, Hewett TE. Use of an overhead goal alters vertical jump performance and biomechanics. J Strength Cond Res. 2005;19(2):394–399. doi: 10.1519/15834.1. [DOI] [PubMed] [Google Scholar]
- 24.Herb CC, Grossman K, Feger MA, Donovan L, Hertel J. Lower extremity biomechanics during a drop-vertical jump in participants with or without chronic ankle instability. J Athl Train. 2018;53(4):364–371. doi: 10.4085/1062-6050-481-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hansberger BL, Acocello S, Slater LV, Hart JM, Ambegaonkar JP. Peak lower extremity landing kinematics in dancers and nondancers. J Athl Train. 2018;53(4):379–385. doi: 10.4085/1062-6050-465-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trigsted SM, Post EG, Bell DR. Landing mechanics during single hop for distance in females following anterior cruciate ligament reconstruction compared to healthy controls. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1395–1402. doi: 10.1007/s00167-015-3658-9. [DOI] [PubMed] [Google Scholar]
- 27.Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37(11):2108–2116. doi: 10.1177/0363546509337934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Slater LV, Hart JM. The influence of knee alignment on lower extremity kinetics during squats. J Electromyogr Kinesiol. 2016;31:96–103. doi: 10.1016/j.jelekin.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 29.Kuenze C, Hertel J, Weltman A, Diduch DR, Saliba S, Hart JM. Jogging biomechanics after exercise in individuals with ACL-reconstructed knees. Med Sci Sports Exerc. 2014;46(6):1067–1076. doi: 10.1249/MSS.0000000000000217. [DOI] [PubMed] [Google Scholar]
- 30.Hopkins WG, Marshall SW, Batterham AM, Hanin J. Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exerc. 2009;41(1):3–13. doi: 10.1249/MSS.0b013e31818cb278. [DOI] [PubMed] [Google Scholar]
- 31.Cohen J. Statistical Power Analysis for the Behavioral Sciences 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. pp. 24–27. [Google Scholar]
- 32.Chappell JD, Creighton RA, Giuliani C, Yu B, Garrett WE. Kinematics and electromyography of landing preparation in vertical stop-jump: risks for noncontact anterior cruciate ligament injury. Am J Sports Med. 2007;35(2):235–241. doi: 10.1177/0363546506294077. [DOI] [PubMed] [Google Scholar]
- 33.Wulf G. Attentional focus and motor learning: a review of 15 years. Int Rev Sport Exerc Psychol. 2013;6(1):77–104. [Google Scholar]
- 34.Wulf G, McConnel N, Gärtner M, Schwarz A. Enhancing the learning of sports skills through external-focus feedback. J Mot Behav. 2002;34(2):171–182. doi: 10.1080/00222890209601939. [DOI] [PubMed] [Google Scholar]
- 35.Wulf G, McNevin N, Shea CH. The automaticity of complex motor skill learning as a function of attentional focus. Q J Exp Psychol A. 2001;54(4):1143–1154. doi: 10.1080/713756012. [DOI] [PubMed] [Google Scholar]
- 36.Shea CH, Wulf G. Enhancing motor learning through external-focus instructions and feedback. Hum Mov Sci. 1999;18(4):553–571. [Google Scholar]
- 37.Todorov E, Shadmehr R, Bizzi E. Augmented feedback presented in a virtual environment accelerates learning of a difficult motor task. J Mot Behav. 1997;29(2):147–158. doi: 10.1080/00222899709600829. [DOI] [PubMed] [Google Scholar]
- 38.Wulf G, Shea CH. Understanding the role of augmented feedback: the good, the bad and the ugly. In: Williams AM, Hodges NJ, editors. Skill Acquisition in Sport: Research, Theory and Practice. New York, NY: Routledge; 2004. pp. 121–144. [Google Scholar]
- 39.Eltoukhy M, Oh J, Kuenze C, Signorile J. Improved Kinect-based spatiotemporal and kinematic treadmill gait assessment. Gait Posture. 2017;51:77–83. doi: 10.1016/j.gaitpost.2016.10.001. [DOI] [PubMed] [Google Scholar]