Abstract
Objective
Researchers have produced a hypothesis of transient heat intolerance (HI) after exertional heat stroke (EHS). Based on this hypothesis, heat-tolerance testing (HTT) has been postponed until weeks 6 to 8 after EHS and other types of exertional heat illness (EHI). We compared the HTT results of participants after either EHS or other EHI who were tested earlier (≤6-week group) versus those who were tested later (>6-week group) to verify the hypothesis.
Design
Cohort study.
Setting
Data obtained from records of military athletes who experienced EHS or EHI.
Patients or Other Participants
All participants who underwent HTT after EHI or EHS experienced between 2014 and 2018 and for whom complete data regarding the severity of the event (rectal temperature, neurologic symptoms, and laboratory results) and HTT results were available were included. Participants with suspected EHS and those with other EHIs were evaluated separately.
Main Outcome Measure(s)
The percentages of participants with HI and mean probability of heat tolerance were compared between those tested within 6 weeks of the event and those tested later.
Results
A total of 186 participants were included in this study (EHS: 12 in the <6-week group, 9 in the >6-week group; EHI: 94 in the <6-week group, 71 in the >6-week group). In the EHS group, the percentages with HI (33% versus 44%, P = .67) and mean probability of heat tolerance (0.82 versus 0.82, P = .98) did not differ. In the EHI group, participants who were tested after 6 weeks had a greater chance of being diagnosed with HI (38% versus 21.3%, P < .02)
Conclusions
The HTT results were similar between participants with EHS who were tested early (<6 weeks) and those tested late (>6 weeks). Further investigation of heat-tolerance changes in larger cohorts of patients after EHS is required to verify the theory of transient HI.
Keywords: heat intolerance, probability of heat tolerance, return to duty, exertional heat stroke
Key Points
Current guidelines suggest heat-tolerance testing (HTT) at least 6 weeks after heat stroke or any other type of exertional heat illness.
Heat-intolerance rates did not differ between participants who underwent HTT >6 weeks versus 2 to 6 weeks after heat stroke.
Among those who experienced any other exertional heat illness, early testing was associated with higher rates of heat tolerance.
Heat-tolerance testing (HTT) is used by the Israeli Defense Forces (IDF) as a screening tool to assist in the decision on a soldier's return to duty (RTD) after an episode of exertional heat stroke (EHS) or exertional heat illness (EHI).1,2 A positive test suggests heat intolerance (HI): that is, a reduced ability to sustain exercise-induced heat stress3 due to deficient dissipation of metabolic heat. The IDF has used this test for the last 4 decades because it is simple, safe, and reliable (98.2% of participants who had had a negative HTT did not experience a repeat EHI).4 The raw data obtained during the test were analyzed for many years by an experienced physiologist or physician. This requirement was a major disadvantage, which has recently been addressed by applying computational methods for the objective interpretation of results.5
The original HTT protocol, which was based on early observations, was an exercise heat-stress exposure scheduled 6 to 8 weeks after the clinical recovery from the EHI. This relatively long period of recovery was suggested because of the concern that earlier testing might be associated with positive results (HI) in participants who had sustained an EHS.6
The physiological rationale for postponing the HTT was the view of HI as a transient state of deficient thermoregulatory ability, caused by thermal damage during the EHI.7 The precise mechanism of this damage is unknown. According to one theory, the physiological response to heat stress is coordinated by the preoptic area of the hypothalamus. Surprisingly, autopsies of EHS victims who displayed thermal dysregulatory responses revealed no hypothalamic damage, despite the evidence of adjacent brain tissue damage. According to relatively recent evidence, thermoregulation occurs peripherally, without central control.8 However, agreement exists that HI may be observed in cases of multiorgan thermal damage, exacerbated by delayed cooling.6,7
Complementary evidence suggests that HI is an inherent trait. Modifiable factors (eg, heat acclimatization status, aerobic fitness status, hydration status, and anthropometric characteristics) have considerable influence on an individual's ability to effectively regulate body temperature during exercise.7
We believed that a 6- to 8-week waiting time for HTT had a negative effect on these modifiable factors. The relatively long period of limited physical exercise prevented soldiers from training and probably led to reductions in aerobic fitness and acclimatization. Moreover, abstinence from physical exercise for an extended period resulted in almost certain dropout from training. Thus, we questioned the long recovery period before undertaking the HTT. Recent clinical guidelines from the US Army9 recommend that soldiers who sustain EHS be assessed repeatedly approximately 2 weeks after the event. A soldier who does not have any residual symptoms (“evidence of cognitive or behavioral dysfunction, renal impairment, hepatic dysfunction, rhabdomyolysis, or other related pathology”) may return to his or her routine. The National Athletic Trainers' Association guidelines suggest return to activity 1 month after an episode of EHS, again provided that the athlete has no residual dysfunction.10 Following these guidelines, we have started testing for heat tolerance 2 weeks after clinical recovery from any EHI. We report on our initial experience with early HTT testing after an episode of EHS or other EHI.
METHODS
This retrospective cohort study was approved by the IDF Medical Corps Institutional Review Board. The study group included all IDF male soldiers who sustained an episode of EHI between 2014 and 2018 and who were referred to our institution for HTT and RTD recommendations. The HTT was performed according to the protocol described previously.5 Records of all participants were reviewed for information regarding the EHI event date, testing date and result, participant baseline characteristics (age, height, and weight), and EHI event characteristics (type of activity during which the event occurred, cooling delay [immediate cooling versus cooling delayed beyond 30 minutes after the development of the signs of EHI], rectal temperature measurement, neurologic symptoms on presentation, and laboratory abnormalities). The participants were subsequently classified as having EHS based on a rectal temperature of 40°C or higher within 10 minutes of presentation. In all patients, cooling followed the standard IDF protocol: at least 120 L of water is poured on the patient and continued until rectal temperature falls below 37.5°C.
Neurologic symptoms were grouped as mild (headache and dizziness), moderate (fainting, confusion), or severe (loss of consciousness, agitation, and convulsions). Laboratory abnormalities were similarly presented: mild (nonelevated creatinine [<1.1 U/L], creatine kinase [CK] <500 U/L, and nonelevated aspartate aminotransferase [AST] and alanine aminotransferase [ALT]), moderate (creatinine = 1.1–1.5 U/L, CK = 500–1000 U/L, and AST and ALT = 40–80 U/L), or severe (creatinine >1.5 U/L, CK >1000 U/L, AST and ALT >80 U/L).
Types of activities were field training, martial arts (Krav Maga), marches, operational activity, participation in selection process, and performance testing. Heat tolerance was traditionally described as pass (heat tolerance [HT]) or fail (HI).2 In addition, the probability of heat tolerance (PHT; range = 0–1) was presented; a PHT value higher than 0.9 was regarded as HT. This measure was developed by 2 of the authors (H.S. and R.Y.5) using logistic regression to predict the specialist's designation of the HTT results as HI or HT based on rectal temperature and pulse changes throughout the testing. The online application used to calculate PHT from the raw HTT data can be found at https://phtheller.shinyapps.io/HTTest/.
Continuous variables are presented as means and standard deviations, and nominal variables are presented as percentages. Baseline characteristics of participants and the events were compared using an independent-samples t test for continuous variables and χ2 test for nominal variables. The α and β coefficients were set at .05 and .2, respectively. The P values are presented for convenient reporting of testing significance. After the bivariate analysis, a multivariate linear regression model, including the time from the EHI event to testing and the event characteristics, was developed to predict heat tolerance. Statistical analysis was performed on R open-source software (version 3.3.0; R Foundation, Vienna, Austria).
RESULTS
A total of 186 participants were included in the study; 21 (11%) had a rectal temperature of >40°C and were classified as having sustained an EHS event, whereas 165 (89%) were classified as having sustained a heat-injury event. Among the EHS participants, 12 (57%) underwent HTT within 6 weeks of the event, and 9 (43%) were tested later. In the EHI group, 94 (57%) were tested early (≤6 weeks) and 71 (43%) were tested late (>6 weeks).
Participants tested earlier did not differ from those tested later with respect to physical characteristics or the background or severity of EHS and EHI occurrence. The only difference was the distribution of military activities during which the event occurred. More than half of EHS events occurred during performance testing, whereas more than half of EHI events occurred during marches (Table 1).
Table 1.
Baseline Characteristics of Study Participants and Their Exertional Heat–Related Events
| Variable |
Exertional Heat Stroke (n = 21) |
Exertional Heat Illness (n = 165) |
||||
| HTT ≤6 wk (n = 12) |
HTT >6 wk (n = 9) |
P Value |
HTT ≤6 wk (n = 94) |
HTT >6 wk (n = 71) |
P Value |
|
| Time to HTT, mean ± SD, d | 32 ± 9.6 | 64.2 ± 17.1 | <.01 | 27.5 ± 8.9 | 79.1 ± 58 | <.01 |
| Age, mean ± SD, y | 19.3 ± 1.1 | 21.3 ± 3.9 | .17 | 19.9 ± 1.2 | 19.8 ± 1.5 | .57 |
| Height, mean ± SD, cm | 173.6 ± 7.1 | 172 ± 8.9 | .67 | 174.8 ± 6.7 | 174.7 ± 6.3 | .98 |
| Weight, mean ± SD, kg | 71.9 ± 11.5 | 71.6 ± 12.8 | .95 | 71.7 ± 11.7 | 72.7 ± 13.3 | .63 |
| Body mass index, mean ± SD, kg/m2 | 23.8 ± 3 | 24.7 ± 3.5 | .54 | 23.4 ± 3.3 | 23.8 ± 4 | .56 |
| Rectal temperature, mean ± SD (95% confidence interval), °C | 40.8 ± 0.7 (40.4, 41.2) | 40.8 ± 0.9 (40.2, 41.4) | .99 | 38.7 ± 0.7 (38.6, 38.8) | 38.8 ± 0.6 (38.7, 38.9) | .31 |
| Neurologic symptoms, No. (%) | ||||||
| Mild | 4 (33) | 2 (22) | .73 | 34 (36) | 27 (38) | .98 |
| Moderate | 6 (50) | 4 (45) | 43 (46) | 31 (44) | ||
| Severe | 2 (17) | 3 (33) | 17 (18) | 13 (18) | ||
| Laboratory abnormalities, No. (%)a | ||||||
| Mild | 5 (50) | 5 (56) | .70 | 71 (82) | 54 (81) | .46 |
| Moderate | 1 (10) | 2 (22) | 11 (13) | 6 (9) | ||
| Severe | 4 (40) | 2 (22) | 5 (5) | 7 (10) | ||
| Type of activity, No. (%) | ||||||
| Field training | 1 (8) | 0 | .88 | 11 (12) | 4 (6) | .03 |
| Krav Maga | 0 | 0 | 3 (3) | 2 (3) | ||
| March | 4 (33) | 2 (22) | 53 (56) | 39 (55) | ||
| Operational activity | 0 | 0 | 0 | 1 (1) | ||
| Selections | 0 | 1 (11) | 7 (7) | 16 (23) | ||
| Performance testing | 7 (59) | 6 (67) | 20 (22) | 9 (12) | ||
| Treatment, % delayedb | 25 | 33 | 1 | 49 (53) | 38 (54) | 1 |
Abbreviation: HTT, heat-tolerance testing.
Missing enzymes data for 2 participants in the exertional heat-stroke group.
Delayed initiation of the cooling protocol by >30 minutes since the first sign of the exertional heat illness.
In the EHS group, the rates of HI and mean PHT were similar between participants who sustained an EHS and were tested early versus those who were tested late (Table 2). In the EHI group, the diagnosis of HI was more frequent among participants who were tested late compared with those tested early (38% versus 21.3%, P = .02). Participants with EHI who were tested late reached a higher final heart rate and rectal temperature than participants with EHI who were tested early (Table 2). Interestingly, both EHS and EHI participants who were tested late had higher resting heart rates (heart rate at minute 0) than participants who were tested early (Table 2).
Table 2.
Comparison of Heat-Tolerance Testing (HTT) Results Between Participants With Exertional Heat Stroke (EHS) or Exertional Heat Illness (EHI) Participants Tested Early (≤6 Weeks) or Late (>6 Weeks)
| Variable |
EHS (n = 21) |
EHI (n = 165) |
||||
| HTT ≤6 wk (n = 12) |
HTT >6 wk (n = 9) |
P Value |
HTT ≤6 wk (n = 94) |
HTT >6 wk (n = 71) |
P Value |
|
| Dichotomic classification, No. (%) heat intolerant | 4 (33) | 4 (44) | .67 | 20 (21.3) | 27 (38) | .02 |
| Probability of heat tolerance, mean ± SD (95% confidence interval) | 0.82 ± 0.3 (0.66, 0.98) | 0.82 ± 0.2 (0.68, 0.96) | .98 | 0.88 ± 0.3 (0.83, 0.93) | 0.78 ± 0.4 (0.7, 0.86) | .07 |
| Rectal temperature during HTT, mean ± SD, °C | ||||||
| Minute 0 | 36.9 ± 0.4 | 37.1 ± 0.2 | .32 | 36.9 ± 0.3 | 37 ± 0.3 | .10 |
| Minute 60 | 37.9 ± 0.4 | 37.9 ± 0.2 | .97 | 37.6 ± 0.3 | 37.7 ± 0.4 | .29 |
| Minute 120 | 38 ± 0.4 | 38 ± 0.2 | .96 | 37.7 ± 0.3 | 37.8 ± 0.4 | .03 |
| Heart rate during HTT, mean ± SD, beats/min | ||||||
| Minute 0 | 80.4 ± 10.5 | 86.7 ± 18 | .37 | 74.6 ± 16.9 | 79.1 ± 17 | .10 |
| Minute 60 | 115.1 ± 12.8 | 118.6 ± 18.3 | .63 | 109.7 ± 15.3 | 114.5 ± 17.9 | .09 |
| Minute 120 | 120.4 ± 13.6 | 127.4 ± 17.5 | .33 | 116.9 ± 17.5 | 124.7 ± 21.2 | .02 |
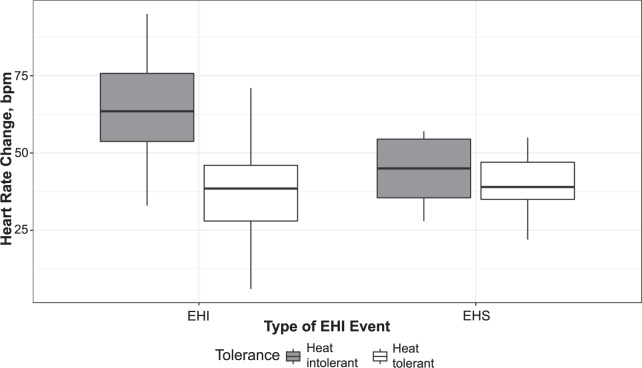
The differences in temperature and heart-rate rise of participants who were diagnosed as having HT and those diagnosed as having HI are demonstrated in Figures 1 and 2. Participants with EHI who had HI displayed higher heart rates during the test compared with HI participants with EHS.
Figure 1.
Core temperature change (°C) during the heat-tolerance testing: the difference between heat-tolerant and heat-intolerant participants among those after heat stroke (right) and those after another exertional heat illness (left). The box designates the 95% confidence interval, and the central horizontal bar designates the mean. Abbreviations: EHI, exertional heat illness; EHS, exertional heat stroke.
Figure 2.
Heart-rate change (beats/min [bpm]) during the heat-tolerance testing: the difference between heat-tolerant and heat-intolerant participants among those after heat stroke (right) and those after another exertional heat illness (left). The box designates the 95% confidence interval, and the central horizontal bar designates the mean. Abbreviations: EHI, exertional heat illness; EHS, exertional heat stroke.
A logistic regression model included the following predictors of HI: diagnosis of EHS or EHI, rectal temperature at the time of the event, timing of cooling initiation (immediate versus delayed), time to HTT, body mass index, and severity of neurologic symptoms (Table 3). The only significant predictors of HI were delayed cooling (odds ratio [OR] = 1.32, P < .001) and moderate (OR = 1.25, P = .01) or severe (OR = 1.27, P = .047) neurologic symptoms.
Table 3.
Predictors of Heat Intolerance
| Variable |
Odds Ratio (95% Confidence Interval) |
P Value |
| Time to heat-tolerance testing, wk | 1.01 (0.99, 1.03) | .17 |
| Rectal temperature | 1.10 (0.98, 1.23) | .12 |
| Delayed cooling (>30 min)a | 1.32 (1.13, 1.55) | <.01 |
| Diagnosis of exertional heat strokeb | 0.89 (0.65, 1.22) | .47 |
| Body mass index | 1.01 (0.98, 1.03) | .58 |
| Moderate neurologic symptomsc | 1.25 (1.06, 1.50) | .01 |
| Severe neurologic symptomsc | 1.27 (1.01, 1.59) | .047 |
Reference variable: immediate cooling (<30 min).
Reference variable: diagnosis of exertional heat illness.
Reference variable: mild neurologic symptoms.
DISCUSSION
The goal of our study was to compare the results of HTTs performed early after recovery from EHS or EHI (≤6 weeks) with those obtained more than 6 weeks after recovery. The main finding was that the diagnosis of HI was similar in both groups of participants with EHS (33% versus 44%, P = .67). However, because of the low statistical power of the comparison, we refrained from drawing generalizable conclusions from the results. Still, we did regard it as an assurance of the safety of early testing in our patients and decided to continue conducting HTTs after a minimum of 2 weeks postevent. One of our concerns was the possibility of a higher rate of multiple false-positive results due to insufficient recovery from the EHS. Yet this concern was not reflected in the findings.
In the subgroup of other EHI patients, a delayed HTT was associated with a lower PHT and higher chance of being diagnosed as having HI. Additionally, participants with EHI who were tested later had higher resting heart rates compared with participants tested earlier (Table 2). Finally, their median heart-rate rise during the test was substantially higher than that of the EHS participants. Because HT is closely related to physical fitness,11,12 based on the above findings, we suspected that all EHI participants had lower fitness levels than the EHS participants, and those who were tested late had lower fitness levels than the EHI participants tested earlier. Cardiovascular insufficiency is a major contributor to heat exhaustion and exertional heat injury, whereas heat accumulation underlies the development of heat stroke. This probably explains the difference in study findings between participants with EHS and another EHI and highlights the detrimental effect of a lengthy wait for test results and the possibility of RTD after an episode of another EHI.
Using multivariate analysis, we found that the type of event (EHS versus EHI), rectal temperature at the time of the event, and participant's body mass index did not have any effect on the odds of a diagnosis of HI. Two significant predictors of an HI diagnosis were identified: delayed initiation of cooling (>30 minutes) and severity of neurologic symptoms on presentation (loss of consciousness, agitation, or confusion as opposed to mild headache or dizziness). The former has been linked to survival and recovery from heat stroke.13,14 The latter has not been documented as such. We suggest that both factors reliably reflect the extent of thermal injury sustained by the participant, as opposed to a single measurement of rectal temperature, no matter how high it is. When cooling is delayed, a participant is exposed to high core temperature for a longer time. Similarly, the degree of neurologic dysfunction may be a reliable indicator of ongoing thermal damage. Based on earlier observations, an event of EHS was theorized to be followed by a state of temporary HI. This was rationalized according to a theory that normal hypothalamic thermoregulatory function might have been compromised during the event and would have to equilibrate during the process of recovery, which takes time. Although the exact mechanism or pattern of injury has not been identified, previous researchers corroborated this assumption by documenting neurologic deficits after EHS, from which (in most cases) the soldiers recovered within a few weeks. Thus, a recovery period of 6 to 8 weeks after the clinical recovery from the event was believed to be long enough to show the baseline thermoregulatory responses that can differentiate between individuals with HT and HI.6,15 Six to 8 weeks is a relatively long lag period, during which soldiers are prevented from physical training and consequently lose some of their physical capacity. However, this relatively long recovery period remained unchanged until recently for 2 main reasons. First, the protocol served for many years as a safety tool in RTD decisions,16 preventing a premature RTD. Second, although most clinical guidelines recommended return to gradual activity only 7 to 21 days after clinical recovery,9,10,14 no evidence has shown that clinical recovery is an accurate indicator of the function of the thermoregulatory mechanism. From a practical perspective, a delicate balance between the patient's medical safety and reliable HTT results should be maintained. Testing too early might give false-positive or false-negative results. Whereas the former is of less significance, because those who fail the test will be retested a few months later, the latter might endanger the patient if full activity is started too early. Given this uncertainty, we still considered it safe enough to perform an HTT as early as 10 to 14 days after the EHS or other EHI.
The findings of this study were not consistent with the theory that the EHS or other EHI may have a residual effect on the thermoregulatory capacity of generally healthy participants with no residual neurologic deficits. Participants who survived an EHS with residual neurologic deficits were not represented in the study group and, therefore, the theory of temporary HI in these patient subgroups may not be dismissed.
The limitations of our study were the retrospective cohort design and relatively small sample, especially the EHS subgroup. A larger number of patients who had an episode of EHS with serial HTT testing starting early post-EHI and complemented with serial physical fitness assessments is required to further investigate the phenomenon of transient HI. This would contribute to our understanding of HT patterns after an EHS event and the interplay between HT and physical fitness.
REFERENCES
- 1.O'Connor FG, Williams AD, Blivin S, Heled Y, Deuster P, Flinn SD. Guidelines for return to duty (play) after heat illness: a military perspective. J Sport Rehabil. 2007;16(3):227–237. doi: 10.1123/jsr.16.3.227. [DOI] [PubMed] [Google Scholar]
- 2.Moran DS, Erlich T, Epstein Y. The heat tolerance test: an efficient screening tool for evaluating susceptibility to heat. J Sport Rehabil. 2007;16(3):215–221. doi: 10.1123/jsr.16.3.215. [DOI] [PubMed] [Google Scholar]
- 3.Strydom NB. Heat intolerance: its detection and elimination in the mining industry. S Afr J Sci. 1980;76(4):154–156. [Google Scholar]
- 4.Schermann H, Heled Y, Fleischmann C, et al. The validity of the heat tolerance test in prediction of recurrent exertional heat illness events. J Sci Med Sport. 2018;21(6):549–552. doi: 10.1016/j.jsams.2017.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Schermann H, Craig E, Yanovich E, Ketko I, Kalmanovich G, Yanovich R. Probability of heat intolerance: standardized interpretation of heat-tolerance testing results versus specialist judgment. J Athl Train. 2018;53(4):423–430. doi: 10.4085/1062-6050-519-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keren G, Epstein Y, Magazanik A. Temporary heat intolerance in a heatstroke patient. Aviat Space Environ Med. 1981;52(2):116–117. [PubMed] [Google Scholar]
- 7.Hosokawa Y, Stearns RL, Casa DJ. Is heat intolerance state or trait? Sports Med. 2019;49(3):365–370. doi: 10.1007/s40279-019-01067-z. [DOI] [PubMed] [Google Scholar]
- 8.Leon LR, Bouchama A. Heat stroke. Compr Physiol. 2015;5(2):611–647. doi: 10.1002/cphy.c140017. [DOI] [PubMed] [Google Scholar]
- 9.US Department of the Army. Standards of medical fitness. Army Regulation 40-501. 2019 Published. https://armypubs.army.mil/epubs/DR_pubs/DR_a/pdf/web/ARN8673_AR40_501_FINAL_WEB.pdf Accessed October 3, 2019.
- 10.Casa DJ, DeMartini JK, Bergeron MF, et al. National Athletic Trainers' Association position statement: exertional heat illnesses. J Athl Train. 2015;50(9):986–1000. doi: 10.4085/1062-6050-50.9.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lisman P, Kazman JB, O'Connor FG, Heled Y, Deuster PA. Heat tolerance testing: association between heat intolerance and anthropometric and fitness measurements. Mil Med. 2014;179(11):1339–1346. doi: 10.7205/MILMED-D-14-00169. [DOI] [PubMed] [Google Scholar]
- 12.Schiffmann N, Schermann H, Mazgaoker S, et al. The cardiovascular reserve index: a noninvasive clinical insight into heat intolerance. Clin J Sport Med. 2018] doi: 10.1097/JSM.0000000000000712. [published online ahead of print December 21. [DOI] [PubMed]
- 13.Armstrong LE, De Luca JP, Hubbard RW. Time course of recovery and heat acclimation ability of prior exertional heatstroke patients. Med Sci Sports Exerc. 1990;22(1):36–48. [PubMed] [Google Scholar]
- 14.O'Connor FG, Casa DJ, Bergeron MF, et al. American College of Sports Medicine roundtable on exertional heat stroke—return to duty/return to play: conference proceedings. Curr Sports Med Rep. 2010;9(5):314–321. doi: 10.1249/JSR.0b013e3181f1d183. [DOI] [PubMed] [Google Scholar]
- 15.Epstein Y. Heat intolerance: predisposing factor or residual injury? Med Sci Sports Exerc. 1990;22(1):29–35. [PubMed] [Google Scholar]
- 16.Schermann H, Heled Y, Fleischmann C, et al. The validity of the heat tolerance test in prediction of recurrent exertional heat illness events. J Sci Med Sport. 2018;21(6):549–552. doi: 10.1016/j.jsams.2017.10.001. [DOI] [PubMed] [Google Scholar]