Abstract
Objective
Adult attachment insecurity is associated with many health outcomes and may be associated with sleep disturbance. The purpose of this study was to test the hypothesis that sleep disturbance mediates the relationship between attachment insecurity and three measures of health (perceived general health, physical symptoms and sick days) in a group that is at high risk of sleep disturbance: hospital based health-care workers.
Methods
One hundred thirty-one nondepressed female hospital workers completed self-report measures of adult attachment, sleep disturbance, depressive symptoms (excluding sleep-related items) and health outcomes. The hypothesis of mediation was tested with sequential regression analyses.
Results
Both attachment anxiety and attachment avoidance were significantly associated with impairment in global sleep quality (ρ=.20 and .19, respectively, P<.05) and physical symptoms (ρ=.21 and .19, P<.05). Attachment anxiety was also associated with depressive symptoms (ρ=.33, P<.001) and sick days (ρ=.21, P<.05). For both physical symptoms and sick days, mediation analyses were consistent with global sleep quality acting as a partial mediator of the relationship between attachment anxiety and physical health. Non-sleep-related depressive symptoms were a stronger mediator.
Conclusions
This study corroborates evidence that attachment insecurity is associated with sleep disturbance and extends this association to the occurrence of physical symptoms and time off work due to sickness among workers in a high-stress occupation.
Keywords: Sleep quality, Attachment insecurity, Physical symptoms, Well-being, Absenteeism
Introduction
Attachment insecurity in close adult relationships is associated with the experience and reporting of physical symptoms, nonadherence to self-management behaviors, impaired social support and amplified stress response [1], [2], [3], [4] and thus has broad consequences for health. Although there are several mechanisms by which insecurity may affect health [3], [5], one path that has been underemphasized is the relationship between attachment insecurity and disturbed sleep.
The attachment system is activated in conditions that increase vulnerability to danger, including darkness and aloneness, and attachment bonds diminish the vulnerability that occurs while one sleeps [6]. If a secure attachment bond facilitates safe sleep, it is plausible that an insecure bond heightens feelings that one is unsafe and increases vigilance, which interferes with sound sleep. Furthermore, the parental interactions that promote secure attachment, including soothing responses to distress, may facilitate the regulatory organization that promotes restorative sleep.
There are several lines of evidence supporting this hypothesis. Mothers of securely attached infants have more consistent, sensitive and responsive nighttime interactions with their infants [7] and have infants with fewer sleep problems [8]. Toddlers with sleep disorders are likely to have insecure patterns of attachment [9]. Among low birth-weight babies, maternal–infant interactions have a direct impact on infant sleep patterns [10]. Furthermore, mothers with high separation anxiety (which challenges their ability to facilitate secure attachment) have infants with more nocturnal waking and lower sleep efficiency [11]. The link between attachment insecurity and sleep disturbance persists in late adolescence [12], in married adults [13] and in senior citizens in the community [14].
Disturbed sleep regulation may link stress responses to subsequent symptoms. In paramedics facing the acute stress of a critical incident, attachment insecurity was associated with a higher incidence of sleep disturbance after the event and a slower recovery of sleep over subsequent nights. The duration of sleep recovery was related to subsequent physical and psychiatric symptoms (J. Halpern, personal communication). In a large Scandinavian sample, sleep disturbance mediated the relationship between impaired attachment-related social support and myocardial infarction [15].
Sleep studies also support the hypothesis. The intrusion of faster alpha EEG waves into slow-wave delta sleep is an anomaly found in fibromyalgia [16], [17] and has been hypothesized to indicate a vigilant state during sleep with resulting daytime symptoms of nonrestorative sleep [18]. In persons referred to a sleep clinic, the proportion of the sleep record in which alpha waves were detected was positively associated with attachment anxiety [19]. Reduced Stage 3–4 sleep has also been reported in women with anxious attachment [20].
The purpose of this investigation was to determine if there was a correlation between adult attachment insecurity and sleep disturbance in a nonclinical sample of adult women and if sleep disturbance mediated a relationship between attachment insecurity and health outcomes. In this analysis, it is necessary to control for depressive symptoms because attachment insecurity, sleep disturbance and physical health are each related to depression. Previous research has shown that attachment anxiety is a risk factor for depressive symptoms [21] and that sleep disturbance is recognized as a symptom of depression, and it is known that depressive symptoms contribute to perceived ill health, physical symptoms and sick time [22]. We posed these questions in a secondary analysis of a database from a study of chronic stress in health-care workers [23].
Methods
Details of the methods have been described previously [23]. Briefly, the study took place in 13 hospital sites in Toronto and Hamilton, Ontario, Canada, between October 2004 and September 2005, 13–26 months after the resolution of the 2003 outbreak of severe acute respiratory syndrome (SARS). Eligible health-care workers included nurses in medical and surgical inpatient units and all staff of intensive care units, emergency departments and SARS isolation units in these hospitals. The study was approved by the Research Ethics Board of each hospital. Participants were surveyed in two waves. The first wave consisted of a survey that included the demographic indices, the Pittsburgh Sleep Quality Index and measures of symptoms and sick days. Of the 769 health-care workers (668 women and 101 men) who completed this survey, 180 (163 women and 17 men) also participated in a second wave (Survey B + diagnostic interview), which included a measure of adult attachment. Subjects who participated or did not participate in Survey B were compared on a wide range of psychological and demographic indices and found to be similar [23]. In addition, participants in the second wave did not differ from those who participated only in the first wave with respect to sleep indices. Since the relationships that are tested in this study may vary with sex and the number of men who completed Survey B is small, we report here only on the women who completed all of the measures analyzed in this report (n=141), excluding 10 further subjects who met Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for current major depression as assessed with the Structured Clinical Interview for DSM-IV [24], [25].
Instruments
Sleep quality
The Pittsburgh Sleep Quality Index is a 19-item self-report measure of global sleep quality that includes seven components of sleep quality. The global sleep quality score range is from 0 to 21. Internal reliability, test–retest reliability and validity are acceptable. In a study of the Pittsburgh Sleep Quality index in cohorts of patients of differing clinical status, the mean global sleep quality score in healthy patients was 2.7; in patients with excessive somnolence, it was 6.5; in patients with difficulties initiating or maintaining sleep, it was 10.4; and in patients with depression, it was 11.1 [26]. A cutoff of 5 distinguishes between healthy subjects and those with depression or sleep disorders [26].
Adult attachment style
The Experience in Close Relationships–Revised (ECR-R) is a 36-item questionnaire probing attitudes toward close relationships with intimate partners. Each item is scored on a seven-point scale ranging from strongly disagree to strongly agree. The ECR-R has been derived through the application of item–response theory to choose 36 items from a pool of 323 attachment items drawn from the commonly used attachment instruments [27], [28]. The ECR-R generates two dimensions of insecurity, attachment anxiety and attachment avoidance, which are theoretically independent; however, in the current study, these two dimensions were strongly correlated (R=.73, P<.001).
Physical symptoms
The frequency of seven physical symptoms (heart pounding or racing without exercise, shortness of breath without exercise, indigestion or upset stomach, trouble swallowing, feeling sweaty or clammy, dizziness, feeling hot or flushed) over the last 4 weeks was measured on a five-point scale from none of the time (0) to all of the time (4).
General perceived health
Three items from the 12-item Short Form [29] measure of quality of life, “I am somewhat ill” (reversed), “I am as healthy as anybody I know” and “My health is excellent,” were rated on a five-point scale from definitely true to definitely false. The scales were averaged to produce a perceived health score between 1 (good) and 5 (poor).
Sick days
Sick days were reported as the number of shifts or work days that participants reported that they had missed “because of stress, illness or fatigue” in the previous 4 months. In order to reduce the impact of extreme values on the analysis (although the interquartile range of sick days was 0 to 3, the maximum reported was 85), a rank-order transformation was used.
Depressive symptoms
Depressive symptoms were measured using the mean of the five items of the K-10 screening scale for psychological distress, which are depressive symptoms, excluding the item “felt tired for no good reason” (felt depressed, nothing could cheer you up, hopeless, everything was an effort, worthless). The K-10 has strong psychometric properties in the clinical range of depressive symptoms [30].
Analysis
Attachment anxiety and attachment avoidance were analyzed separately because they were strongly correlated with each other. Bivariate relationships were tested between each combination of global sleep quality, attachment anxiety, depressive symptoms and health indices (physical symptom score, perceived general health and recent sick days) using Spearman's rank-order correlations. Post hoc tests of the relationship between attachment insecurity and the proportion subjects above a screening cutoff of global sleep quality (score>5) [26] were conducted to illustrate clinical significance. The hypothesis of mediation was tested using a series of regression analyses [31]. The analysis was then repeated substituting attachment avoidance for attachment anxiety.
Results
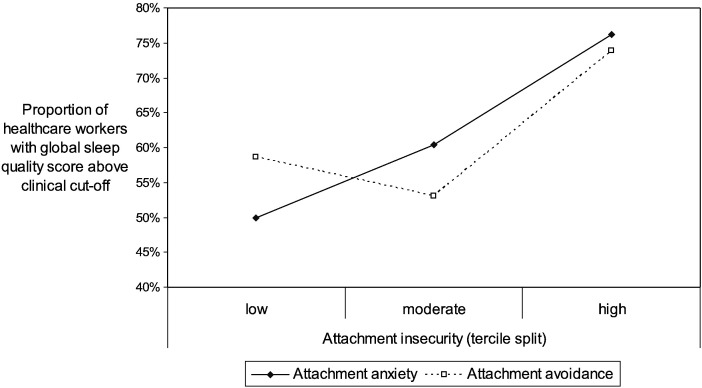
The characteristics of this sample of 131 nondepressed female hospital workers are described in Table 1 . Both attachment anxiety and attachment avoidance were significantly associated with impairment in global sleep quality (Table 2 ). Attachment anxiety was associated with depressive symptoms, physical symptoms and sick days. Attachment avoidance was associated with physical symptoms. Fig. 1 illustrates the clinical significance of the relationship between attachment insecurity and impaired global sleep quality in terms of the proportion of subjects having global sleep quality above the cutoff, which distinguishes between normal adults and those with depression or sleep disorders.
Table 1.
Characteristics of the study sample
| n | % | Range | Median | Interquartile range | |
|---|---|---|---|---|---|
| Job | |||||
| Nurse | 108 | 82.4 | |||
| Other clinical staff | 14 | 10.7 | |||
| Nonclinical staff | 9 | 6.9 | |||
| Marital status | |||||
| Married/common law | 108 | 82.4 | |||
| Single | 12 | 9.2 | |||
| Separated/widowed | 11 | 8.4 | |||
| Age (years) | 25–63 | 45 | 38–52 | ||
| Health-care experience (years) | 2–40 | 20 | 10–30 | ||
| Global sleep quality score (range of scale is 0–21) | 1–17 | 6 | 5–9 | ||
| Perceived general health (range of scale is 1–5) | 1–4.3 | 1.7 | 1.3–2.3 | ||
| Physical symptoms (range of scale is 1–5) | 1–2.7 | 1.3 | 1.0–1.7 | ||
| Sick days in past 4 months | 0–85 | 1 | 0–3 | ||
| Attachment anxiety (range of scale is 1–7) | 1–6.3 | 2.0 | 1.3–3.5 | ||
| Attachment avoidance (range of scale is 1–7) | 1–6.2 | 2.1 | 1.4–2.9 |
Table 2.
Bivariate relationships between attachment insecurity and sleep, depressive symptoms and measures of health
| Attachment anxiety |
Attachment avoidance |
|||
|---|---|---|---|---|
| ρa | Significance | ρa | Significance | |
| Global sleep quality score | .20 | .03 | .19 | .03 |
| Depressive symptoms | .33 | <.001 | .16 | .06 |
| Physical symptoms | .21 | .02 | .19 | .03 |
| Perceived general health | .17 | .06 | .09 | .29 |
| Sick days in past 4 months | .21 | .02 | .11 | .21 |
ρ is Spearman's rank-order correlation.
Fig. 1.
Prevalence of global sleep quality score above clinical cutoff by degree of attachment insecurity.
Impairment in global sleep quality was significantly associated with physical symptoms (Spearman's ρ=.42, P<.001), perceived general health (ρ=.33, P<.001) and sick days (ρ=.33, P<.001). Depressive symptoms were also significantly associated with physical symptoms (Spearman's ρ=.67, P<.001), perceived general health (ρ=.43, P<.001) and sick days (ρ=.44, P<.001).
Table 3 presents the results of a series of regression analyses designed to test global sleep quality as a mediator of the relationship between attachment anxiety and the two physical health outcomes with which it had a significant bivariate relationship. With respect to physical symptoms, adding global sleep quality to the equation makes a significant contribution and reduces the contribution of attachment anxiety from β=.24 to β=.18, although attachment anxiety remains a significant parameter in the regression equation. Similarly, with respect to sick days, global sleep quality reduces the contribution of attachment anxiety from β=.24 to β=.19, although attachment anxiety remains significant. For each of the physical health outcome variables, adding depressive symptoms to the regression equation reduces the contribution of attachment anxiety to nonsignificance (Table 3, Step 2b). In the final regression equation (Table 3, Step 3), only depressive symptoms made a significant contribution to explaining physical symptoms or sick days. A regression analysis of the relationship between attachment avoidance and physical symptoms is not presented because attachment avoidance was essentially noncontributory (R2=.02).
Table 3.
Tests of impaired sleep quality and depressive symptoms as mediators of the relationship between attachment anxiety and three general health and symptom outcomes
| Independent variables | Dependent variable |
|||
|---|---|---|---|---|
| Physical symptoms |
Sick days |
|||
| β | R2 | β | R2 | |
| 1. | ||||
| Attachment anxiety | .24⁎⁎ | .24⁎⁎ | ||
| Model | .06 | .06 | ||
| 2a. | ||||
| Attachment anxiety | .18⁎ | .19⁎ | ||
| Global sleep quality | .33⁎⁎⁎ | .26⁎⁎ | ||
| Model | .17 | .12 | ||
| 2b. | ||||
| Attachment anxiety | −.02 | .07 | ||
| Depressive symptoms | .68⁎⁎⁎ | .44⁎⁎⁎ | ||
| Model | .46 | .22 | ||
| 3. | ||||
| Attachment anxiety | −.02 | .07 | ||
| Global sleep quality | .10 | .13 | ||
| Depressive symptoms | .64⁎⁎⁎ | .39⁎⁎⁎ | ||
| Model | .47 | .24 | ||
P<.05.
P<.01.
P<.001.
Discussion
This study corroborates previous evidence that both dimensions of attachment insecurity, attachment anxiety and attachment avoidance, are associated with impaired global sleep quality. The results of this study are also consistent with previous reports that attachment anxiety is associated with reports of physical symptoms [3], [32]. The finding that attachment avoidance is not related to perceived general health or sick days is consistent with previous research showing the associations between attachment avoidance and aspects of physical health to be weaker and less consistent than is found for attachment anxiety. There are several aspects of the three-way relationship among attachment, sleep and health that require further discussion.
First, the distribution of adult attachment patterns in this study was unusual since attachment anxiety and attachment avoidance were strongly correlated. Since the independence of these dimensions when measured by the ECR-R has been confirmed in several studies [33], their relationship in this study is likely a characteristic of the study sample. A higher than expected intercorrelation suggests that hospital workers who are higher in one dimension of attachment insecurity tend to also be higher the other dimension. Shaver and Mikulincer [34] understand the co-occurrence of attachment anxiety and attachment avoidance (also called “fearful attachment”) as the result of a failure of avoidant defenses in the face of overwhelming stress. In other words, the co-occurrence of these dimensions of attachment insecurity is found in individuals who are predisposed to an avoidant response to attachment stressors (rather than an anxious–preoccupied response), who then experience circumstances in which the avoidant response fails to protect them from underlying attachment-related anxiety. This formulation might help to explain the strong relationship between the dimensions of insecurity in this study, particularly if health-care workers differ from other cohorts in being more prone to avoidant and less prone to anxious–preoccupied responses to attachment stressors. In that case, health-care workers who express attachment insecurity would tend to vary along a single dimension from secure to fearful (combined attachment anxiety and attachment avoidance) because it would be relatively unusual for them to express attachment anxiety alone. Although this speculation conforms to the common sense assumption that anxious attachment styles are not adaptive for those who work in hospitals and thus are underrepresented in a group of veteran (median years of experience=20) hospital workers, there is no evidence from other research that the attachment patterns of health-care workers differ from those found in the general population. Further studies of the adult attachment characteristics of health-care workers may clarify this finding. Since sex differences in adult attachment styles are modest [35], the correlation of attachment anxiety and attachment avoidance is not explained by this study being restricted to women.
The results of this study confirm the expectations that disturbed sleep is common among hospital-based workers [36], [37] and that disturbed sleep is associated with indices of perceived physical health [38], [39]. The finding that attachment insecurity is associated with impaired global sleep quality is consistent with the growing literature linking attachment and sleep. The clinical importance of this link is emphasized by the proportion of health-care workers meeting the screening cutoff for possible sleep disorder. This proportion is high in the entire cohort (61.7%), but the prevalence nonetheless rises from 50% in the lowest tercile of attachment anxiety to 74% in the highest (Fig. 1). Data are not available in this study to determine the impact of shift work on outcomes.
The tests of mediation are consistent with the hypothesis that global sleep quality acts as a partial mediator of the relationship between attachment anxiety and two indices of physical health: physical symptoms and sick days. The pattern of these analyses was similar for these two measures of physical health. In each case the contribution of attachment anxiety to explaining variance in reported physical health is reduced by adding global sleep quality to the model and is rendered nonsignificant by entering depressive symptoms into the model. Depressive symptoms account for substantially more of the variance in indices of physical symptoms than is accounted for by attachment anxiety alone or by global sleep quality. Thus, depressive symptoms mediate the link between attachment anxiety and physical symptoms more strongly than global sleep quality does and make a further contribution to physical symptoms that is independent of attachment insecurity and global sleep quality. In order to interpret this pattern, it is useful to refer to the results of previous research. First, attachment insecurity is a risk factor for both depressive symptoms and the syndrome of major depression [21], [40]. Second, both attachment anxiety and depressive symptoms are known to be consistently related to physical symptoms [3], [22]. Thus, the strong mediating relationship of depressive symptoms is expected. What this study asks, beyond the latter relationship, is what role impaired sleep might have. It appears that impaired sleep is related to both attachment insecurity and to physical symptoms but is not as strong a mediator as depressive symptoms.
The conclusions of this study are limited by its design. With respect to temporal order, a mediating process must follow its cause (independent variable) and precede its effect (dependent variable) [41]. The cross-sectional study design does not allow us to test the assumption that attachment style is a stable variable that precedes sleep disturbance. Previous research indicates that adult attachment patterns are usually sufficiently stable over time to be considered trait phenomena [33], which therefore are likely to temporally precede the state phenomena of impaired sleep quality, depressive symptoms and physical symptoms. However, sleep disturbance among health-care workers is also a chronic phenomenon. Furthermore, the relationship between disturbed sleep and impaired health is complex and bidirectional. Prospective research is required to confirm the temporal sequence of the relationships found in this study. Evidence from previous research suggests that impaired sleep and depressive symptoms may have a bidirectional relationship and that chronic sleep impairment and depressive symptoms increase in concert with each other in health-care workers [42]. The current study cannot tease apart the interrelationship of sleep and depressive symptoms. Furthermore, it is not known prior to replication studies if the findings of this study can be generalized to other groups of people, given that there are several characteristics of the current cohort that are special (i.e., women in health-care professions, many of whom are shift workers).
Shared variance between self-report measures may also confound a mediation analysis, which speaks of the importance of objective measures of attachment, sleep and physical health in future studies. The correlation between subjectively impaired quality of sleep as measured with the Pittsburgh Sleep Quality Index and objective measures of sleep physiology has been inconsistent [43], [44], and so replication using polysomnographic sleep measures would be valuable. On the other hand, two previous studies support a link between attachment insecurity and sleep physiology [19], [20], and so the correlation between attachment anxiety and global sleep quality in the current study is unlikely to be entirely due to a subjective reporting bias.
Attachment insecurity is a developmental risk factor for a variety of physical health outcomes [3], [5]. Multiple pathways have been suggested by which attachment processes can affect health including affect, stress, social support and health-risk behavior [5]. Sleep disturbance may be an additional pathway by which attachment insecurity affects health. Further research on the fundamental association among interpersonal security, sound sleep and health is warranted.
Acknowledgments
This study was funded with a grant from the Canadian Institutes of Health Research (SAR 67807).
References
- 1.Ciechanowski P, Katon W, Hirsch I. Attachment style and adherence in the diabetic patient. Psychosom Med. 1999;61:110. [Google Scholar]
- 2.Mikulincer M, Florian V, Weller A. Attachment styles, coping strategies and posttraumatic psychological distress: the impact of the Gulf War in Israel. J Pers Soc Psychol. 1993;64:817–826. doi: 10.1037//0022-3514.64.5.817. [DOI] [PubMed] [Google Scholar]
- 3.Ciechanowski P, Walker EA, Katon WJ, Russo JE. Attachment theory: a model for health care utilization and somatization. Psychosom Med. 2002;64:660–667. doi: 10.1097/01.psy.0000021948.90613.76. [DOI] [PubMed] [Google Scholar]
- 4.Maunder RG, Lancee WJ, Nolan RP, Hunter JJ, Tannenbaum DW. The relationship of attachment insecurity to subjective stress and autonomic function during standardized acute stress in healthy adults. J Psychosom Res. 2006;60:283–290. doi: 10.1016/j.jpsychores.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 5.Maunder RG, Hunter JJ. Attachment and psychosomatic medicine: developmental contributions to stress and disease. Psychosom Med. 2001;63:556–567. doi: 10.1097/00006842-200107000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Bowlby J. Basic Books; New York: 1973. Attachment and loss: vol 2: separation: anxiety and anger. [Google Scholar]
- 7.Higley E, Dozier M. Nighttime maternal responsiveness and infant attachment at one year. Attach Hum Dev. 2009;11:347–363. doi: 10.1080/14616730903016979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morrell J, Steele H. The role of attachment security, temperament, maternal perception, and care-giving behavior in persistent infant sleeping problems. Infant Ment Health J. 2003;24:447–468. [Google Scholar]
- 9.Benoit D, Zeanah CH, Boucher C, Minde KK. Sleep disorders in early childhood: association with insecure maternal attachment. J Am Acad Child Adolesc Psychiatry. 1992;31:86–93. doi: 10.1097/00004583-199201000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Schwichtenberg AJM, Poehlmann J. A transactional model of sleep–wake regulation in infants born preterm or low birthweight. J Pediatr Psychol. 2009;34:837–849. doi: 10.1093/jpepsy/jsn132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scher A. Maternal separation anxiety as a regulator of infants' sleep. J Child Psychol Psychiatry. 2008;49:618–625. doi: 10.1111/j.1469-7610.2007.01872.x. [DOI] [PubMed] [Google Scholar]
- 12.Scharfe E, Eldredge D. Associations between attachment representations and health behaviors in late adolescence. J Health Psychol. 2001;6:295–307. doi: 10.1177/135910530100600303. [DOI] [PubMed] [Google Scholar]
- 13.Carmichael CL, Reis HT. Attachment, sleep quality, and depressed affect. Health Psychol. 2005;24:526–531. doi: 10.1037/0278-6133.24.5.526. [DOI] [PubMed] [Google Scholar]
- 14.Verdecias RN, Jean-Louis G, Zizi F, Casimir GJ, Browne RC. Attachment styles and sleep measures in a community-based sample of older adults. Sleep Med. 2009;10:664–667. doi: 10.1016/j.sleep.2008.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nordin M, Knutsson A, Sundbom E. Is disturbed sleep a mediator in the association between social support and myocardial infarction? J Health Psychol. 2008;13:55–64. doi: 10.1177/1359105307084312. [DOI] [PubMed] [Google Scholar]
- 16.Branco J, Atalaia A, Paiva T. Sleep cycles and alpha–delta sleep in fibromyalgia syndrome. J Rheumatol. 1994:1113–1117. [PubMed] [Google Scholar]
- 17.Drewes AM, Neilsen KD, Taagholt SJ. Sleep intensity in fibromyalgia: focus on the microstructure of the sleep process. Br J Rheumatol. 1995;34:629–635. doi: 10.1093/rheumatology/34.7.629. [DOI] [PubMed] [Google Scholar]
- 18.Anch A, Lue F, McLean A, Moldofsky H. Sleep physiology and psychological aspects of fibrositis syndrome. Canadian J Psychol. 1991;45:179–184. doi: 10.1037/h0084280. [DOI] [PubMed] [Google Scholar]
- 19.Sloan EP, Maunder RG, Hunter JJ, Moldofsky H. Insecure attachment is associated with the alpha-EEG anomaly during sleep. Biopsychosoc Med. 2007;1:20. doi: 10.1186/1751-0759-1-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Troxel WM, Cyranowski JM, Hall M, Frank E, Buysse DJ. Attachment anxiety, relationship context, and sleep in women with recurrent major depression. Psychosom Med. 2007;69:692–699. doi: 10.1097/PSY.0b013e3180cc2ec7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bifulco A, Moran PM, Ball C, Lillie A. Adult attachment style. II: its relationship to psychosocial depressive-vulnerability. Soc Psychiatry Psychiatr Epidemiol. 2002;37:60–67. doi: 10.1007/s127-002-8216-x. [DOI] [PubMed] [Google Scholar]
- 22.Katon W. The impact of major depression on chronic medical illness. Gen Hosp Psychiatry. 1996;18:215–219. doi: 10.1016/0163-8343(96)00065-5. [DOI] [PubMed] [Google Scholar]
- 23.Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12:1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.First MB, Spitzer RL, Gibbon M, Williams JBW. Biometrics Research Department, Columbia University; New York: 1997. User's guide for the structured clinical interview for DSM-IV axis I disorders. [Google Scholar]
- 25.Williams JB, Gibbon M, First MB, Spitzer RL, Davies M, Borus J. The structured clinical interview for DSM-III-R (SCID). II. Multisite test–retest reliability. Arch Gen Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- 26.Buysee DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 27.Brennan KA, Clark CL, Shaver PR. Self-report measurement of adult attachment: an integrative overview. In: Simpson JA, Rholes WS, editors. Attachment theory and close relationships. Guilford Press; New York: 1998. pp. 46–76. [Google Scholar]
- 28.Fraley RC, Waller NG, Brennan KA. An item response theory analysis of self-report measures of adult attachment. J Pers Soc Psychol. 2002;78:350–365. doi: 10.1037//0022-3514.78.2.350. [DOI] [PubMed] [Google Scholar]
- 29.Ware JE, Kosinki M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 31.Baron RM, Kenny DA. The moderator–mediator distinction in social psychological research: conceptual, strategic and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 32.Ciechanowski PS, Katon WJ, Russo JE, Dwight-Johnson MM. Association of attachment style to lifetime medically unexplained symptoms in patients with hepatitis C. Psychosomatics. 2002;43:206–212. doi: 10.1176/appi.psy.43.3.206. [DOI] [PubMed] [Google Scholar]
- 33.Mikulincer M, Shaver PR. Guilford Press; New York: 2007. Attachment in adulthood: structure, dynamics, and change. [Google Scholar]
- 34.Shaver PR, Mikulincer M. Attachment-related psychodynamics. Attach Hum Dev. 2002;4:133–161. doi: 10.1080/14616730210154171. [DOI] [PubMed] [Google Scholar]
- 35.Mickelson KD, Kessler RC, Shaver PR. Adult attachment in a nationally representative sample. J Pers Soc Psychol. 1997;73:1092–1106. doi: 10.1037//0022-3514.73.5.1092. [DOI] [PubMed] [Google Scholar]
- 36.Weinger MB, Ancoli-Israel S. Sleep deprivation and clinical performance. JAMA. 2002;287:955–957. doi: 10.1001/jama.287.8.955. [DOI] [PubMed] [Google Scholar]
- 37.Scott LD, Hwang WT, Rogers AE, Nysse T, Dean GE, Dinges DF. The relationship between nurse work schedules, sleep duration, and drowsy driving. Sleep. 2007;30:1801–1807. doi: 10.1093/sleep/30.12.1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gold DR, Rogacz S, Bock N, Tosteson TD, Baum TM, Speizer FE. Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. Am J Public Health. 1992;82:1011–1014. doi: 10.2105/ajph.82.7.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kutner NG, Schechtman KB, Ory MG, Baker DI. Older adults' perceptions of their health and functioning in relation to sleep disturbance, falling, and urinary incontinence. FICSIT Group. J Am Geriatr Soc. 1994;42:757–762. doi: 10.1111/j.1532-5415.1994.tb06537.x. [DOI] [PubMed] [Google Scholar]
- 40.Bifulco A, Moran PM, Ball C, Bernazzani O. Adult attachment style. I: its relationship to clinical depression. Soc Psychiatry Psychiatr Epidemiol. 2002;37:50–59. doi: 10.1007/s127-002-8215-0. [DOI] [PubMed] [Google Scholar]
- 41.Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- 42.Rosen IM, Gimotty PA, Shea JA, Bellini LM. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006;81:82–85. doi: 10.1097/00001888-200601000-00020. [DOI] [PubMed] [Google Scholar]
- 43.Buysse DJ, Reynolds CF, Monk TH, Hoch CC, Yeager AL, Kupfer DJ. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI) Sleep. 1991;14:331–338. [PubMed] [Google Scholar]
- 44.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53:737–740. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]