Abstract
Background
The outbreak of severe acute respiratory syndrome (SARS) in Hong Kong posed many challenges for health promotion activities among a group of older adults with low socio-economic status (SES). With concerns that this vulnerable group could be at higher risk of contracting the disease or spreading it to others, the implementation of health promotion activities appropriate to this group was considered to be essential during the epidemic.
Objectives
To assess the effectiveness of delivering a telephone health education programme dealing with anxiety levels, and knowledge and practice of measures to prevent transmission of SARS among a group of older adults with low SES.
Design
Pretest/posttest design.
Settings
Subjects were recruited from registered members of a government subsidized social service center in Hong Kong and living in low-cost housing estates.
Participants
The eligibility criteria were: (1) aged 55 or above; (2) able to speak Cantonese; (3) no hearing impairment, and (4) reachable by telephone. Of the 295 eligible subjects, 122 older adults completed the whole study.
Methods
The interviewers approached all eligible subjects by telephone during the period of 15–25 May 2003. After obtaining the participants’ verbal consent, the interviewer collected baseline data by use of a questionnaire and implemented a health education programme. A follow-up telephone call was made a week later using the same questionnaire.
Results
The level of anxiety was lowered (t=3.28, p<0.001), and knowledge regarding the transmission routes of droplets (p<0.001) and urine and feaces (p<0.01) were improved after the intervention. Although statistical significant difference was found in the practice of identified preventive measures before and after intervention, influence on behavioral changes needed further exploration.
Conclusion
The telephone health education seemed to be effective in relieving anxiety and improving knowledge of the main transmission routes of SARS in this group, but not the practice of preventing SARS. Telephone contact appears to be a practical way of providing health education to vulnerable groups when face-to-face measure is not feasible and may be useful in raising health awareness during future outbreaks of emerging infections.
Keywords: Older adults, Health education, Severe Acute Respiratory Syndrome (SARS), Telephone intervention
What is already known about the topic?
-
•
Empirical evidence on the effectiveness of telephone health education among older adults with minimal or no formal education is lacking.
-
•
Low health literacy among the older adults may hinder understanding of mass health education against SARS, which might be essential for effecting behavioral change.
-
•
Telephone counseling could be an effective means in improving health knowledge by providing individual counseling on health behaviors and social support among older adults who lives alone.
What this paper adds
-
•This is the first systematic study to assess the effectiveness of delivering telephone health education to older adults during the outbreak of SARS in Hong Kong.
-
•The findings of the study added some knowledge on feasibility and effectiveness of providing telephone intervention for older adults during an infectious disease epidemic, thus enlightened its applicability in possible pandemics such as avian and other influenzas
-
•Telephone health education is a safe measure to provide health education when face-to-face measures are not feasible during outbreaks of infection.
-
•
1. Introduction
The aging population is growing in Hong Kong, as it is elsewhere. In Hong Kong, an adult aged 55 or above is considered as an older adult because of the lowering age of retirement (Neugarten, 1996), with approximately 21.2% (n=1,475,000) of the total population aged 55 years or above (Hong Kong Census and Statistic Department (HKCSD), 31 December 2005). Unlike other demographic groups in Hong Kong, literacy rates are low in this group with more than 31.2% not having undertaken any formal education. Among those who have undertaken some formal education, 39.5% completed primary schooling only (HKCSD, 26 October 2001). In other words, only a small proportion of older adults in Hong Kong are educated above primary level. This situation presents many challenges for health promotion and disease prevention activities, as many of the usual methods of disseminating health information are not appropriate for this population. Such challenges were particularly noticeable during the outbreak of severe acute respiratory syndrome (SARS) (February–June 2003) in Hong Kong. Over the course of the outbreak, 1755 cases were reported with 300 deaths. Adults 55 years of age or older were 26.2% of the SARS cases (HKSARSEC, 2003); however, the age-specific mortality rate for this age demographic was about 54.5% (Leung et al., 2004). The Hong Kong Government launched a campaign to keep the city healthy and clean. Measures to prevent the transmission of SARS related to personal hygiene and environmental sanitation were publicized daily in the media as a way to minimize infection. However, the presence of functional impairments resulting from chronic illness or knowledge deficits due to low literacy levels among the older adults may affect their understanding and perceived relevance to habitual hygiene practice. Their compliance to recommended infection control measures may be low. Thus, more concern about older adults especially those living alone was expressed by health care providers and in the media (Kong, 2003). The non-compliance to health measures among this susceptible group could pose higher risks for contracting SARS and transmitting the virus to others once becoming a carrier. In view of this challenge, an alternative means to provide health education and support for them was considered essential to ensure the effectiveness of communicating the necessary health messages to this vulnerable group, especially during the outbreak of SARS.
According to the World Health Organization (WHO, n.d.), E-health refers to the use of electronic means into the practice of protecting and promoting health. It can help provide health information and services to the public who have difficulty in accessing healthcare institutions due to physical illness, insufficient resources, environmental constraints or other reasons. E-health relies on a variety of technologies ranging from simple systems (e.g., telephone, facsimile machines) to complex systems (e.g., satellite links, and integrated services digital network). Among various types of technologies, the telephone can offer an inexpensive, convenient and simple method of delivery for health information, education and psychosocial support for older adults at home (Blixen et al., 2004; Hiltunen et al., 2005). Ninety-three percent of the population have a telephone at home (Hong Kong Office of Telecommunications Authority, 2006, January 10) and it is also considered to be a safe measure of communication during the SARS epidemic.
Several studies have indicated that telephone contacts can have a positive effect on various health promotion or disease prevention programmes (Hull et al., 2002; Zhu et al., 2002). Hull et al. (2002) examined the effect of telephone appointments for influenza immunization at a nurse-run clinic for 1820 older adults in the United Kingdom. They found that the uptake of immunization among the older adults was boosted by 6% using telephone appointment. Zhu et al. (2002) investigated the effectiveness of a telephone quit smoking service for about 3300 participants in the USA. Using a randomized controlled trial design, they found that the rates of smoking abstinence for the intervention group were significantly higher than for the control group (p<0.001). Similar results regarding telephone counseling for smoking cessation (Stead et al., 2005), attitude towards current treatment (Theiler et al., 2002), knowledge on disease (Branch et al., 1994) and prescribed regular medications (Ayanian et al., 2002) were also reported.
Although not all literature supports the positive effects of telephone education on health promotion activities (Gallagher et al., 2003; Stoddard et al., 2002), for the purposes of this study, it was considered to be a cost-effective means of communication, and safe for both older adults and interviewers under the spirit of minimal contact during the SARS epidemic. A group of faculty and nursing students of a university in Hong Kong therefore implemented a telephone health promotion programme for a group of older adults. The aims of the study were:
-
(1)
To assess the baseline data of older adults regarding their level of anxiety, knowledge of the main transmission routes of SARS, and measures taken to prevent the transmission of SARS.
-
(2)
To provide older adults with knowledge related to the transmission modes of SARS and preventive measures as well as support through a health education programme.
-
(3)
To examine the effectiveness of the programme in terms of the participants’ anxiety, knowledge about the main transmission routes of SARS and measures for preventing SARS.
2. Method
2.1. Sample and design
The study used a pretest/posttest design. Potential subjects were recruited from registered members of a government subsidized social service center in the Southern District of Hong Kong which provides various services to older adults such as home visits, social activities and meals-on-wheels service. The eligibility criteria were subjects who: (1) aged 55 or above; (2) were able to speak Cantonese; (3) had no hearing impairment, and (4) were reachable by telephone.
Initially, 295 registered members of the social service center were contacted by telephone to determine their eligibility; a total of 182 older adults were successfully contacted at baseline for health assessment and health education (i.e., response rate=61.7%). However, only 122 completed the post intervention questionnaire (i.e., follow-up rate=67%). The attrition in the follow-up was mainly due to refusal and non-response telephone calls (Fig. 1 ).
Fig. 1.
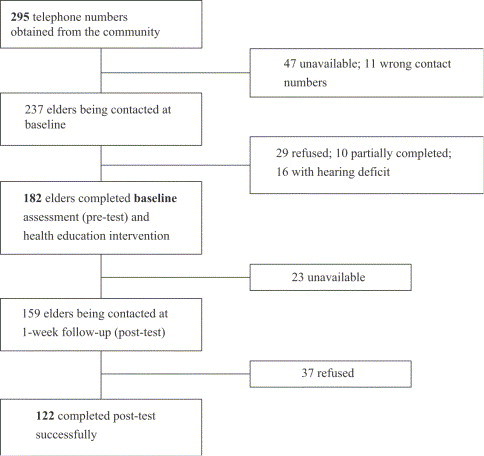
Recruitment of older adults in the community.
2.2. Measurement
A survey instrument developed by Leung et al. (2003) was modified and adapted for the use in this study. The original survey instrument comprised 60 questions and is divided into seven parts: (1) self-perceived general health status and level of anxiety; (2) use of health services; (3) possibility of contacting diagnosed SARS cases; (4) belief of contracting SARS; (5) knowledge of transmission of SARS; (6) measures taken to prevent transmission of SARS; and (7) socio-demographics. Other details of the instrument have been described in So et al. (2004) and Leung et al. (2003). In this paper, the level of anxiety, knowledge level regarding SARS transmission modes, and practice of preventive measures will be presented.
2.3. Training program for the interviewers
Twenty-six nursing students from the University of Hong Kong received a training programme conducted by faculty with expertise in gerontology, health education, and counseling. The training program aims to improve the students’ knowledge and skills and it include: (1) the purpose of the research including the research questions; (2) how to conduct a telephone survey (e.g., communication techniques, how to obtain informed consent, consistent use of the study procedure, and data recording); (3) how to communicate with the elders and to handle questions; (4) assessment of their learning and ability through observation during role play and practice; and (5) elucidate and reinforce compliance with study protocols.
2.4. Procedure
The Institutional Review Board approved this study. All the potential subjects were approached via telephone during the period between 15 and 25 May 2003 to determine their eligibility. After gaining their verbal consent, interviewers collected the baseline data regarding the level of anxiety, knowledge and preventive measures taken to prevent transmission of SARS. Based on the results of the baseline data, the interviewer provided health education to the participants and clarified their misconceptions. A follow-up phone call was made 1 week after the collection of the baseline data and interviewers used the same questionnaire for evaluation.
2.5. Data analysis
The level of anxiety, knowledge and practice of preventive measures regarding SARS were the main outcome variables. Descriptive statistics were used to assess all variables. Paired-sample t-test was used to assess the level of anxiety before and after the intervention. The McNemar test was used to examine the change of the level of knowledge about the transmission routes of SARS prior to and after the intervention. Sign test was used to investigate the change of practice of preventive measures before and after the intervention. An alpha of 0.05 or less was considered significant.
3. Results
3.1. Demographics
Information about the demographics of the participants is presented in Table 1 . The majority of the participants were female (63.0%). More than half of the participants (58.3%) did not live with the family. The majority did not have any formal education (50.0%) or received low educational level (30.2%). About 83.0% were retired and did not have a monthly income.
Table 1.
Demographic characteristics (n=122)
| Characteristics | n (%) |
|---|---|
| Age (years old) | |
| 55–64 | 12 (10.3) |
| 65–74 | 49 (42.2) |
| 75 or above | 55 (47.4) |
| Gender | |
| Female | 75 (63.0) |
| Male | 44 (37.0) |
| Educational attainment | |
| No formal education | 58 (50.0) |
| Primary | 35 (30.2) |
| Secondary or above | 23 (19.8) |
| Marital status | |
| Single/divorced/widower | 77 (63.1) |
| Married | 38 (31.1) |
| Has children | 57 (49.6) |
| Living with family members | 48 (41.7) |
| Occupation | |
| Retired | 96 (82.8) |
| Unemployed/seeking job | 8 (6.9) |
| Housewife | 11 (9.5) |
| Employed | 1 (0.9) |
| Monthly personal income (HK$) | |
| No income | 88 (83.0) |
| <$1,000 | 18 (17.0) |
Note: Missing values: age=6, gender=3, education attainment=6, marital status=6, has children=7, and living with family members=7.US$1=HKS 7.8; UK£1=HK$ 13.0.
3.2. Level of anxiety
The levels of anxiety before and after the intervention are presented in Table 2 . Only 33.6% perceived a medium level of anxiety or above. While their anxiety level was generally low before the intervention, it was significantly lower following the intervention (t=3.28, df=102, p<0.005).
Table 2.
State-Trait Anxiety Inventory (STAI) scores grouped by three levels of anxiety (N=122)
| Before intervention |
After intervention |
Paired sample t | df | p | |
|---|---|---|---|---|---|
| M (SD) | M (SD) | ||||
| STAI scores | 35.56 (8.80) | 33.13 (7.09) | 3.28 | 118 | <0.001⁎⁎⁎ |
|
n (%) |
n (%) |
||||
| Low level of anxiety | 81 (66.4) | 90 (75.6) | NS | ||
| Medium level of anxiety | 36 (29.5) | 29 (24.4) | NS | ||
| High level of anxiety | 5 (4.1) | / | NA |
Note. Low level of anxiety=20–39; Medium level of anxiety=40–59; High level of anxiety=60–80 (Spielberger, 1983).
McNemar test was informed and no significant changes were found in all levels of anxiety.
p<0.001; NS=not significant; NA=not applicable.
3.3. Knowledge of the transmission of SARS
Changes of the participants’ knowledge of the three main transmission routes (droplets, direct physical contact, and urine/feces) before and after the intervention are presented in Table 3 . A significant difference was found in their knowledge of droplet (p<0.001) and urine/feaces (p<0.005) transmission. Although no statistically significant change was found in the transmission route of direct physical contact (p>0.05), more participants answered correctly following the intervention.
Table 3.
Knowledge of main transmission routes of SARS before and after intervention (N=122)
| Before intervention | After intervention (n) |
p-Value | |
|---|---|---|---|
| Correct | Incorrect | ||
| Droplets | |||
| Correct | 62 | 4 | < 0.001*** |
| Incorrect | 28 | 19 | |
| Contact with urine and feces | |||
| Correct | 49 | 7 | < 0.01** |
| Incorrect | 22 | 35 | |
| Direct physical contact | |||
| Correct | 46 | 13 | NS |
| Incorrect | 23 | 28 | |
| Airborne | |||
| Correct | 16 | 10 | NS |
| Incorrect | 17 | 68 | |
| Animals | |||
| Correct | 12 | 10 | NS |
| Incorrect | 9 | 80 | |
Note:***p<0.001; **p<0.01; NS=not significant.
3.4. Preventive measures to prevent transmission of SARS
Results of taking preventive measures before and after the intervention are presented in Table 4 . Significant differences were found in the practice of covering mouth when sneezing/coughing (p<0.001), washing hands after sneezing/coughing (p<0.001), washing hands with liquid soup (p<0.001), wearing mask in public (p<0.001), and avoiding the use of serving towels (p<0.05). Older adults showed less frequent practice in some measures while more practice in others after the intervention.
Table 4.
Preventive measures taken to prevent transmission of SARS (N=122)
| Preventive measures | Before/ after intervention | N | Mean | Median | SD | p-Value |
|---|---|---|---|---|---|---|
| Cover mouth when sneezing/coughing | Before | 118 | 1.30 | 1 | 0.46 | <0.001⁎⁎⁎ |
| After | 114 | 1.90 | 2 | 1.05 | ||
| Wash hands after sneezing/coughing | Before | 118 | 1.26 | 1 | 0.44 | <0.001⁎⁎⁎ |
| After | 115 | 1.65 | 1 | 0.89 | ||
| Wash hands with liquid soap | Before | 118 | 1.14 | 1 | 0.35 | <0.001⁎⁎⁎ |
| After | 118 | 1.53 | 1 | 0.82 | ||
| Wash hands after contact with possible contaminated materials | Before | 116 | 1.76 | 1 | 1.08 | NS |
| After | 118 | 1.69 | 1 | 0.97 | ||
| Wear a face mask in public | Before | 118 | 1.31 | 1 | 0.46 | <0.001⁎⁎⁎ |
| After | 118 | 2.15 | 2 | 1.12 | ||
| Use serving spoons/chopsticks at meals | Before | 108 | 3.09 | 4 | 1.21 | NS |
| After | 102 | 3.24 | 4 | 1.15 | ||
| Lower toilet lid before flushing | Before | 115 | 2.75 | 4 | 1.39 | NS |
| After | 117 | 2.55 | 3 | 1.38 | ||
| Avoid using serving towels | Before | 110 | 2.45 | 2 | 1.39 | <0.05* |
| After | 109 | 2.10 | 2 | 1.26 |
Note: Frequency of taking preventive measures were evaluated by a 4-point scale ranging from 1 (very often) to 4 (not at all).
p<0.001; *p<0.05; NS=not significant.
4. Discussion
4.1. Level of anxiety
Overall, the participants experienced low levels of anxiety at the time of baseline data collection. This may be due to geographic location among the participants who lived in an area with the least severe outbreak of SARS. Although their level of anxiety was low at both measurement periods, the mean total scores of anxiety were significantly lower after the intervention. More participants reported a low level of anxiety following the telephone intervention. These findings support those of Car and Sheikh (2003), who reported that the provision of care through telephone is an effective means to provide psychosocial support to clients at home.
4.2. Knowledge of the transmission of SARS
Significant changes of the knowledge of the two main transmission routes of SARS (i.e., droplet and urine/feaces) were noted after the intervention. Although no statistical significant changes were found in the knowledge of direct physical contact transmissions before and after intervention (p>0.05), more participants’ misconceptions were corrected after intervention. While the telephone could be an effective means of delivering health education to this vulnerable group, older adults usually take a longer time to acquire new knowledge and information (Eliopoulos, 2001), and continuing health education or further follow up calls may be necessary to monitor their knowledge regarding transmission of SARS.
4.3. Preventive measures to prevent transmission of SARS
Our results showed that older adults had less frequent practice on some preventive measures at follow up. However, the mean difference between the preventive measures before and after the intervention was less than one, and therefore, the results could not reflect the actual behavioral outcomes. In fact, several factors may have affected the less frequent practice of the precautionary measures in the older adults. At the time of follow up, the situation of the SARS epidemic had much improved, and the practice of preventive measures such as wearing masks may not be considered necessary by the older adults. However, personal hygiene practices such as washing hands after sneezing/coughing and contact with possible contaminated materials, had shown a slight increase in frequency of practice and it may imply that these practices could have been internalized as a routine practice and sustained after the intervention. Other preventive measures as advised by the Department of Health, such as using serving spoons/chopsticks at mealtime and avoid using serving towels may not be relevant in this group because they lived alone. Changing health behavior is a complex issue and individual as well as social contextual factors need to be taken into consideration. A single telephone call may not be sufficient to influence practice, but nevertheless it served as a means of support for the elderly during such epidemic. Additional research is needed to clarify the lack of compliance to these measures, and how to influence the change of such behavior.
5. Implications
Although WHO removed Hong Kong from the SARS list in 23 June 2003, the possibility of another outbreak of SARS or other infectious diseases still exists. Recently, the Hong Kong Government emphasizes the importance of preparedness for an influenza pandemic (Hong Kong Health, Welfare and Food Bureau, n.d.) and healthcare professionals play a vital role to deliver health promotion and education to the public. It is, therefore, important that healthcare professionals understand how to deliver key health-related information to the public effectively, particularly to vulnerable groups such as older adults with low socio-economic status (SES). In contrast to the general population, older adults in Hong Kong are comparatively socially isolated and have low literacy rates. Alternative methods of disseminating essential information to older adults are important to enable them to acquire updated information and take appropriate preventive measures to maintain health. E-health is an effective method for health education and promotion and many older adults are more likely to have access to information technologies such as telephone and television. Results of the study supported that telephone health education was effective in relieving anxiety and improving knowledge of the main transmission routes of SARS in older adults, but not fostering practice of preventing SARS. Therefore, the strategy that this study used could be helpful for the future development of health education and promotion for older adults. A combined measure, such as television health education and telephone follow up calls may be desirable to improve health behaviour practices, especially when dealing with possibly pandemics such as avian and other influenzas.
6. Limitations
First, the older adults in this study were recruited from a district that was later reported to have the lowest infection and mortality rate of SARS among the 18 districts in Hong Kong. Therefore, generalization of the results to all older adults in Hong Kong is questionable. Furthermore, the study results indicated a low level of anxiety in the older adults, which could have resulted from living in a relatively “safe” district.
Second, the small sample size and a relatively short time period between the intervention and the follow-up may have resulted in the insignificant differences in the practice of preventive measures after the intervention.
Third, the infection rate of SARS was gradually decreasing during the study period. The Hong Kong daily infection rate of SARS (Leung et al., 2003) was about 3 cases per day during baseline data collection (May 15–25, 2003), and it further declined to about 1 case per day during the 1-week follow-up. This could have affected the perceived importance of practicing the preventive measures since the overall risk seemed to have reduced as the epidemic was waning. Further follow-up could be useful in identifying sustainable changes of relevant behaviors and practices.
Fourth, although providing telephone intervention was the safest means to communicate with the older adults during the SARS epidemic, there were several drawbacks. For example, there is only limited amount of information that one can provide in a single telephone call. Thus, the interviewers have to balance the time spent on each call and to ensure the provision of adequate information for each respondent. It is not advisable to overload the older adults with too much information, as they may not be able to capture and remember all the contents in one single telephone call.
Finally, the older adults might be exposed to other health education and preventive measures on SARS via television and other media during the outbreak. Therefore, it is difficult to attribute the positive changes solely to the interventions.
7. Conclusion
This is the first systematic study to assess the effectiveness of telephone health education in improving older adults’ knowledge and practice of preventive measures during the SARS epidemic. Our initial findings are encouraging in demonstrating the effectiveness of a telephone health education programme in relieving anxiety and improving knowledge of the main transmission routes of SARS in older adults. However, an effective intervention to change the embedded health behaviors remains to be established and tested. The use of technologies such as telephone appears to be an effective means to educate and provide social support to the vulnerable older adults during outbreaks of SARS and other possibly pandemic crises. Future research should explore the effectiveness of health promotion programmes using multiple information technologies that are accessible to, and appropriate for, older adults in changing their health behavior practice.
Acknowledgements
We thank the Aberdeen Kai Fong Welfare Association Social Service Centre for their cooperation, the Bachelor of Nursing students for conducting the telephone interviews, and Professor Judith Parker for reviewing the manuscript. Lastly, we are grateful to the SARS Research Fund, the University of Hong Kong, for providing funding for this study.
References
- Ayanian J.Z., Landrum M.B., McNeil B.J. Use of cholesterol-lowering therapy by elderly adults after myocardial infarction. Archives of Internal Medicine. 2002;162(9):1013–1019. doi: 10.1001/archinte.162.9.1013. [DOI] [PubMed] [Google Scholar]
- Branch L.G., Walker L.A., Wetle T.T., DuBeau C.E., Resnick N.M. Urinary incontinence knowledge among community-dwelling people 65 years of age and older. Journal of the American Geriatrics Society. 1994;42(12):1257–1262. doi: 10.1111/j.1532-5415.1994.tb06507.x. [DOI] [PubMed] [Google Scholar]
- Blixen C.E., Bramstedt K.A., Hammel J.P., Tilley B.C. A pilot study of health education via a nurse-run telephone self-management programme for elderly people with osteoarthritis. Journal of Telemedicine and Telecare. 2004;10(1):44. doi: 10.1258/135763304322764194. [DOI] [PubMed] [Google Scholar]
- Car J., Sheikh A. Telephone consultations. British Medical Journal. 2003;326:966–969. doi: 10.1136/bmj.326.7396.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliopoulos C. Fifth ed. Lippincott; Philadelphia: 2001. Gerontological Nursing. [Google Scholar]
- Gallagher R., McKinley S., Dracup K. Effects of a telephone counseling intervention on psychosocial adjustment in women following a cardiac event. Heart & Lung. 2003;32(2):79–87. doi: 10.1067/mhl.2003.19. [DOI] [PubMed] [Google Scholar]
- Hiltunen E.F., Winder P.A., Rait M.A., Buselli E.F., Carroll D.L., Rankin S.H. Implementation of efficacy enhancement nursing interventions with cardiac elders. Rehabilitation Nursing. 2005;30(6):221. doi: 10.1002/j.2048-7940.2005.tb00116.x. [DOI] [PubMed] [Google Scholar]
- Hong Kong Census and Statistic Department (HKCSD), 31 December 2005. Hong Kong Statistics. Retrieved 20 January 2006, from http://www.censtatd.gov.hk/hong_kong_statistics/statistical_tables/index.jsp
- Hong Kong Census and Statistic Department, 26 October 2001. 2001 population census: Hong Kong resident population aged 15 and over by quinqennial age group and educational attainment (highest level attended),2001. Retrieved 25 November 2003, from http://www.info.gov.hk/censtatd/eng/hkstat/fas/01c/cd0192001_index.html.
- Hong Kong Health, Welfare and Food Bureau (n.d). Hong Kong's preparedness for influenza pandemic—prevention and protection. Retrieved 20 January 2006 from http://www.chp.gov.hk/files/pdf/Policy_brief_en_20051102.pdf
- Hong Kong Office of Telecommunications Authority, 10 January 2006. Key Telecommunications Statistics. Retrieved 10 February 2006 from http://www.ofta.gov.hk/common/fn/printOpt.asp?zh=&docsrc=http%3A//www.ofta.gov.hk/en/datastat/key_stat.html
- Hong Kong SARS Expert Committee (HKSARSEC), 2 October 2003. SARS in Hong Kong: from experience to action. Retrieved 3 October, 2003 from http://www.sars-expertcom.gov.hk/english/reports/reports/reports.fullrpt.html
- Hull S., Hagdrup N., Hart B., Griffiths C., Hennessy E. Boosting uptake of influenza immunization: a randomized controlled trial of telephone appointing in general practice. British Journal of General Practice. 2002;52(482):712–716. [PMC free article] [PubMed] [Google Scholar]
- Kong T.K. The Hong Kong Geriatrics Society; Hong Kong: 2003. Message from the president. The Hong Kong geriatrics society newsletter. May 2003, pp. 1–2. [Google Scholar]
- Leung G.M., Hedley A.J., Ho L.M., Chau P., Wong I.O., Thach T.Q. The epidemiology of severe acute respiratory syndrome in the 2003 Hong Kong epidemic: an analysis of all 1755 patients. Annals of Internal Medicine. 2004;141(9):662–673. doi: 10.7326/0003-4819-141-9-200411020-00006. [DOI] [PubMed] [Google Scholar]
- Leung G.M., Lam T.H., Ho L.M., Ho S.Y., Chan B.H.Y., Wong I.O.L. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. Journal of Epidemiology and Community Health. 2003;57:857–863. doi: 10.1136/jech.57.11.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neugarten D.A. London; The University of Chicago Press: 1996. The Meanings of Age: selected Papers of Bernice L. Neugarten. [Google Scholar]
- So W.K.W., Chan S.S.C., Lee A.C.K., Tiwari A.F.Y. The knowledge level and precautionary measures taken by older adults during the SARS outbreak in Hong Kong. International Journal of Nursing Studies. 2004;41:901–909. doi: 10.1016/j.ijnurstu.2004.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger C.D. Consulting Psychologists Press; Palo Alto, CA: 1983. Manual for the State-Trait Anxiety Inventory (Form Y): Self-evaluation questionnaire. [Google Scholar]
- Stead, L.F., Lancaster, T., Perera, R., 2005. Telephone counseling for smoking cessation. The Cochrane Library, vol. 4. Retrieved 17 January 2006 from http://gateway.ut.ovid.com/gw1/ovidweb.cgi
- Stoddard A.M., Fox S.A., Costanza M.E., Lane D.S., Andersen M.R., Urban N., Lipkus I., Rimer B.K. Effectiveness of telephone counseling for mammography: Results from five randomized trials. Preventive Medicine. 2002;34(1):90–99. doi: 10.1006/pmed.2001.0960. [DOI] [PubMed] [Google Scholar]
- Theiler R., Bischoff H.A., Good M., Uebelhart D. Rofecoxib improves quality of life in patients with hip or knee osteoarthritis. Swiss Medical Weekly. 2002;132(39–40):566–573. doi: 10.4414/smw.2002.10075. [DOI] [PubMed] [Google Scholar]
- World Health Organization (n.d.). E-Health. Retrieved 14 January 2006, from http://www.who.int/trade/glossary/story021/en/print.html
- Zhu S.H., Anderson C.M., Tedeschi G.J., Rosbrook B., Johnson C.E., Byrd M., Gutierrez-Terrell E. Evidence of real-world effectiveness of a telephone quitline for smokers. New England Journal of Medicine. 2002;347(14):1077–1093. doi: 10.1056/NEJMsa020660. [DOI] [PubMed] [Google Scholar]


