Abstract
Background
Little is known about the long-term consequence of severe acute respiratory syndrome (SARS). We carried out an assessment on SARS patients after their recovery from their acute illness.
Method
Postal survey comprising Health-Related Quality of Life (HRQoL) questionnaires and anxiety and depression measures was sent to them at 3 months' postdischarge.
Results
There was a significant impairment in both the HRQoL and mental functioning. Forty-one percent had scores indicative of a posttraumatic stress disorder (PTSD); about 30% had likely anxiety and depression.
Conclusion
SARS has significant impact on HRQoL and psychological status at 3 months.
Keywords: Quality of life, Psychological, Depression, Anxiety, Stress disorder
Introduction
Severe acute respiratory syndrome (SARS) is a new disease caused by a novel strain of coronavirus. It causes flu-like symptoms in the victim, which may subsequently develop into clinical pneumonia. Its acute effects and features have been characterized and reported [1], [2], [3], [4]. Little is known about its longer-term physical and psychological sequelae. From our experience, fatigue, breathlessness despite lack of lung signs, and poor concentration have been common complaints among recovered victims. The cause, nature, and duration of these complaints remain unclear.
Although the impact of the outbreaks on the economy and the health care system had been described [5], the impact upon individuals appeared to have paled into oblivion. As clinicians, we are concerned about the effect on the quality of life and mental health of the sufferers. Cheng et al. [6] and Maunder et al. [7] reported small case series on SARS victims, but a systematic study has not yet been completed. Hence, in this study, we undertook to ascertain systematically the quality of life and psychological well-being of SARS survivors 3 months' postdischarge from the acute episode.
Methodology
The study assessed recovered SARS patients and explored factors that might influence the psychological outcome. Comparison was also made between the psychological status of SARS and other medical and psychiatric conditions.
Patients
This was a postal study on SARS patients who recovered from a clinical episode of the viral illness 3 months ago. They were earlier treated in a hospital designated for SARS. Then, other services of this 1000-bed general hospital were shut down, and all the probable cases of SARS were channeled there. A small number were invited at random to participate at 6 weeks' postdischarge as a pilot project.
Eligible patients were to complete a self-administered psychological assessment package mailed to them.
Inclusion criteria were as follows:
Patients admitted for treatment of SARS fulfilling the WHO criteria [8] for a probable case of SARS. These included (a) high fever (38°C); (b) cough or breathing difficulty; (c) history of contact or positive history of travel; (d) radiographic evidence of infiltrates consistent with pneumonia or respiratory distress syndrome on chest X-ray. (Incidentally, post hoc finding showed those included for study were all tested positively for SARS serologically.)
Exclusion criteria were as follows:
-
1.
Patients who had left the country, e.g., foreigners who contracted SARS and left after recovery.
-
2.Patients below 18 years old. This was based on a few considerations:
-
a.Children were observed to generally have a milder disease.
-
b.They were at a different physiological developmental phase.
-
c.There was no local HRQol database on this age group for comparison.
-
a.
-
3.
Patients above 65 years old. These were very few in number, and, likewise, there was no local HRQol database for this age group.
Materials
The psychological assessment came in the form of self-administered questionnaires, which included the following:
-
1.
The Impact of Event Scale (IES) [9]. This measures distress experienced by a victim or witness of recent serious life changes/event. It has been commonly used to assess persons with posttraumatic stress disorder (PTSD). It can be broken down into an intrusion scale and an avoidance scale. A cutoff of 26 and above has been suggested for a clinically significant reaction to a psychological trauma, although the IES alone does not diagnose PTSD or reflect a person's ability to function.
-
2.
The Hospital Anxiety and Depression Scales (HADS) [10]. This is a 14-item self-rated scale for measurement of both anxiety and depression (seven questions each). It was designed for use in a medical population as it does not contain questions on physical symptomology, which may contaminate the scores. Higher scores indicate greater anxiety or depression. Scores from 8 to 10 on each scale indicate possible clinical disorder and 11 to 21 probable clinical disorder.
-
3.
The Short-Form 36 Health Survey (SF-36) [11], [12]. This is a measure of Health-Related Quality of Life (HRQoL) used in many different diseases and provides measures of different aspects of functioning and limitations. Higher scores indicate higher level of functioning. In Singapore, it has been used to assess the quality of life of a few disease populations, including systemic lupus erythematosus (SLE), osteo-arthritis, and differentiated thyroid carcinoma. A working example of the calculation of the expected scores in the Singapore population adjusted for age, gender, and ethnicity is illustrated in Table 1 .
Table 1.
Calculation of expected HRQol SF-36 scores in a population adjusted for age, gender, and ethnicity
| Ethnicity |
Male |
Female |
||||||
|---|---|---|---|---|---|---|---|---|
| 21–30 | 31–40 | 41–50 | ≥51 | 21–30 | 31–40 | 41–50 | ≥51 | |
| Chinese | 0 | 2 | 1 | 4 | 4 | 1 | 0 | 5 |
| Malay | 0 | 1 | 2 | 2 | 1 | 2 | 0 | 6 |
| Indian | 2 | 0 | 0 | 1 | 1 | 1 | 0 | 1 |
| Total | 2 | 3 | 3 | 7 | 6 | 4 | 0 | 12 |
| Grand total=2+3+3+7+6+4+12=37 | ||||||||
| 21–30 | 31–40 | 41–50 | ≥51 | Row total | ||||
| Chinese | Male (n) | 0 | 2 | 1 | 4 | |||
| National mean | C1 | C2 | C3 | C4 | 2×C1+C3+4×C4 | |||
| Female (n) | 4 | 1 | 0 | 5 | ||||
| National mean | C5 | C6 | C7 | C8 | 4×C5+C6+5×C8 | |||
| Malay | Male (n) | 0 | 1 | 2 | 2 | |||
| National mean | M1 | M2 | M3 | M4 | M2+2×M3+2×M4 | |||
| Female (n) | 1 | 2 | 0 | 6 | ||||
| National mean | M5 | M6 | M7 | M8 | M5+2×M6+6×M8 | |||
| Indian | Male (n) | 2 | 0 | 0 | 1 | |||
| National mean | I1 | I2 | I3 | I4 | 2×I1+I4 | |||
| Female (n) | 1 | 1 | 0 | 1 | ||||
| National mean | I5 | I6 | I7 | I8 | I5+I6+I8 | |||
C1–C4 are the national means for male Chinese of respective age groups; C5–C8 are the national means for female Chinese of respective age groups; M indicates Malay; I, Indian.
Expected Mean Score for a domain on the HRQol SF-36={(2×C1+C3+4×C4)+(4×C5+C6+5×C8)+(M2+2×M3+2×M4)+(M5+2×M6+6×M8)+(2×I1+I4)+(I5+I6+I8)}/(37).
In addition, demographic data such as age, sex, duration of hospital stay, and occupation were captured from the inpatient records.
Any response set that amounted to a significant psychiatric morbidity was advised to seek professional advice.
Statistical analysis
SPSS version 12 was used for simple descriptive statistics. Chi-square test and t-test were used to compare the profiles of the responders and nonresponders and simple correlation test for association between parameters of interest.
Results
Out of 159 eligible candidates, 11 responded at 6 weeks but not at 12 weeks and were not included in the analysis. Another three responded much later than 12 weeks and were likewise excluded. A total of 63 participated in the psychological study and were analysed. Six of them participated in the pilot assessment at Week 6, and the responses were used for a side analysis.
The responders and the nonresponders were comparable on demographic parameters, duration of hospital stay, pre-illness health status, as well as the proportion of patients admitted to the intensive care unit (Table 2 ). The slight overrepresentation by health care workers accounted for a slightly higher female-to-male ratio as majority of the nurses were female locally. The response rate was about 40%. As only English questionnaires were administered, it is likely that many who did not respond were not English literate.
Table 2.
Demographic and clinical characteristics of responders and nonresponders
| Demographic parameters | Responders (n=63) | Nonresponders (n=82) | P values |
|---|---|---|---|
| Age (means) | 34.83 (S.D. 10.49) | 36.82 (S.D. 13.28) | .33 |
| % Female | 79.4 | 71.1 | .34 |
| % Health care workers | 54.0 | 47.0 | .50 |
| % With significant preexisting illness | 3.2 | 7.5 | .47 |
| Duration of hospitalization | 15.24 days (S.D. 10.88) | 15.99 days (S.D. 16.4) | .75 |
| % Admitted to ICU | 9.5% | 10.8% | 1.00 |
| Ethnic groups | .58 | ||
| Chinese | 57.1% | 67.1% | |
| Malay | 15.9% | 14.6% | |
| Indian | 12.7% | 7.3% | |
| Others | 14.3% | 11.0% |
The Short-Form 36 Health Survey
At 3 months, a fair proportion of the victims reported a decline in different aspects of their functionality, using the national norms [14] (adjusted for age, sex, and ethnicity) for comparison (Table 3 ). There was no significant correlation between any of the scores with the duration of the hospitalisation and age of the patients.
Table 3.
SF-36 at 3 months, comparing with national norms of Singapore population, adjusted for age, sex, and ethnicity
| Domains of SF-36 | PF | RP | RE | SF | MH | VT | BP | GH |
|---|---|---|---|---|---|---|---|---|
| National norms | 79.65 | 81.95 | 80.64 | 80.86 | 72.58 | 64.07 | 79.41 | 69.77 |
| Study population (n=63) | 73.08 | 59.52 | 72.49 | 67.20 | 69.55 | 59.84 | 71.95 | 61.17 |
| Difference in scores | −6.57 | −22.43 | −8.15 | −13.66 | −3.03 | −4.23 | −7.46 | −8.6 |
Psychopathology scores
The mean scores on IES, HADS Depression, and HADS Anxiety are shown in Table 4 . The percentages of possible cases of psychiatric disorders as defined by the cutoffs of the respective scales are also indicated. The rate of a possible PTSD, defined by a total IES score >26 (moderate severity), was 41.7%.
Table 4.
Psychiatric scores and percentage of cases among responders
| Psychological scales | Mean score at 3 months | Cutoffs used | % of cases at 3 months |
|---|---|---|---|
| IES | (Higher score indicates greater severity) | (Scores higher than cutoff) | |
| Total | 21.8 (S.D. 16.3) | ≥9 (mild) | 69.8% |
| ≥26 (moderate) | 41.7% | ||
| ≥30 (severe) | 36.7% | ||
| Intrusiveness | 9.5 (S.D. 7.8) | ||
| Avoidance | 12.4 (S.D. 9.6) | ||
| HADS | |||
| Depression score | 4.9 (S.D. 4.1) | ≥8 (mild) | 27% |
| ≥11 (moderate) | 11.1% | ||
| Anxiety score | 6.2 (S.D. 4.5) | ≥8 (mild) | 33.3% |
| ≥11 (moderate) | 17.5% |
If defined by a cutoff of ≥8 on the HADS, 27% and 33% among the responders attained scores indicative of a depressive or anxiety disorder, respectively.
Six weeks vs. 12 weeks
There were six participants who answered the same questionnaires at Week 6 and at Week 12. The means were compared and shown in Table 5 . Essentially, all the parameters showed improvement with time.
Table 5.
Comparison between scores at 6 and 12 weeks
| Psychological parameters | 6 weeks, mean (S.D.) | 12 weeks, mean (S.D.) | t values (paired t-test) | P value |
|---|---|---|---|---|
| IES—Total | 23.0 (13.3) | 9.5 (13.9) | 2.37 | |
| IES—Intrusive | 9.7 (9.4) | 3.3 (5.4) | 2.78 | .039 |
| IES—Avoidance | 13.3 (7.7) | 6.2 (8.6) | 1.38 | |
| HADS—Depression | 5.0 (3.6) | 3.3 (2.7) | 2.99 | .03 |
| HADS—Anxiety | 5.2 (4.7) | 1.8 (2.5) | 2.02 | .09 |
| SF-36 | ||||
| Physical functioning | 73.3 (21.8) | 85.0 (13.4) | −2.77 | .04 |
| Role—physical | 45.8 (43.1) | 79.2 (40.1) | −1.87 | |
| Role—mental | 61.1 (49.1) | 77.8 (40.4) | −1.00 | |
| Social functioning | 59.3 (34.9) | 79.6 (28.4) | −1.81 | |
| Mental health | 78.7 (19.0) | 88.0 (15.8) | −1.90 | |
| Vitality | 68.3 (16.6) | 82.5 (16.4) | −1.90 | |
| Pain | 75.9 (27.6) | 79.6 (23.7) | −1.00 | |
| Quality of life fatigue | 14.5 (6.9) | 10.2 (4.9) | 2.63 | .46 |
The ICU patients
The SF-36 Quality of Life measures at 3 months appeared to have a slightly different profile for those who were admitted to the ICU (see Table 6 and Fig. 1 ). They suffered more in terms of role restriction due to physical problems. They also had a worse vitality score, which made intuitive sense.
Table 6.
SF-36 at 3 months, of SARS-ICU, comparing with national norms of Singapore population, adjusted for age, sex, and ethnicity
| Domains of SF-36 | PF | RP | RE | SF | MH | VT | BP | GH |
|---|---|---|---|---|---|---|---|---|
| National norms | 80.87 | 83.68 | 80.42 | 82.20 | 72.77 | 63.70 | 79.85 | 69.74 |
| ICU patients (n=6) | 75.83 | 41.67 | 66.67 | 68.52 | 65.33 | 60.83 | 72.22 | 68.00 |
| Difference in scores | −5.04 | −42.01 | −13.75 | −13.68 | −7.44 | −2.87 | −7.63 | −1.74 |
Fig. 1.
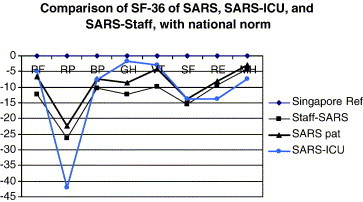
Comparison of the difference in mean scores of SF-36 (using Singapore population norms as reference) between SARS ICU, SARS staff, and all SARS patients. PF: physical functioning; RP: role physical; BP: bodily pain; GH: general health; VT: vitality; SF: social functioning; RE: role emotional; MH: mental health.
The mean psychiatric morbidity scores of the ICU patients were comparable with the rest of the SARS patients: IES total (S.D.)=23.5 (15.73), HADS Depression (S.D.)=4.33 (3.39), HADS Anxiety (S.D.)=5.00 (5.12) (compare figures in Table 4).
The health care workers
The health care workers appeared to be more adversely affected than nonstaff based on both the HRQol SF-36 scores (Fig. 1, see staff-SARS) and the mean scores for IES, and the HADS Depression and Anxiety scores, although these were not significant. This was despite significantly shorter hospitalization duration in the health care worker group.
Correlation between HRQoL SF-36 and other psychiatric scores
When age and duration of stay were controlled for, all the domains of the HRQoL SF-36 were significantly correlated with the total IES score, the HADS Anxiety score, and all but the physical function and role limitation (physical) were also significantly correlated with the HADS Depression score (Table 7 ).
Table 7.
Correlation between various psychiatric scores and domains of SF-36, controlling for age and duration of hospitalization
| SF-36 | IES—total |
Anxiety score |
Depression score |
|||
|---|---|---|---|---|---|---|
| Correlation | Significance | Correlation | Significance | Correlation | Significance | |
| Physical function | −.498 | .000⁎ | −.416 | .002⁎ | −.241 | .085 |
| Role limitation—physical | −.444 | .001⁎ | −.499 | .000⁎ | −.255 | .068 |
| Social functioning | −.524 | .000⁎ | −.437 | .001⁎ | −.312 | .024⁎ |
| Mental health | −.617 | .000⁎ | −.648 | .000⁎ | −.441 | .001⁎ |
| Vitality | −.356 | .010⁎ | −.465 | .001⁎ | −.360 | .009⁎ |
| Bodily pain | −.464 | .001⁎ | −.409 | .003⁎ | −.409 | .003⁎ |
| General health | −.263 | .060 | −.490 | .000⁎ | −.441 | .001⁎ |
| Role limitation—emotional | −.540 | .000⁎ | −.580 | .000⁎ | −.436 | .001⁎ |
Indicates statistical significance (i.e., P<.05).
Discussion
We found firstly a significant proportion of previously healthy people who continued to be suboptimal functionally even after 12 weeks' postdischarge. Secondly, a large proportion of them had significant psychological morbidity.
Health-related quality of life
Table 3 shows the HRQoL SF-36 scores of the SARS patients and the adjusted national norms. All the domains of the quality of life measured were affected. Although the clinical episode was over, the illness was far from being over after 3 months. This is a strong reminder of the difference in disease and illness concepts, the latter being the one that tends to be overlooked by clinicians.
The duration of hospitalisation and admission to ICU are often used as measures of the severity of illness. From our data, admission to ICU and not the duration of hospitalisation impacted on the physical domain of the instruments. It appeared that ICU admission is a more appropriate index of severity of SARS febrile episode. Those with a greater respiratory compromise ended up with worse physical role restriction and lower vitality scores. The main caveat here is that the number of ICU patients is too small to be conclusive.
Compared to other diseases (Fig. 2, Fig. 3 ), the patients had a different profile on the HRQoL SF-36. Evaluated against local SLE patients [13], the SARS patients were more affected in two domains: the physical role limitation and social functioning. The degree of impairment reached that of SLE patients. The decline in social functioning could be partly accounted for by the fact that SARS was a highly contagious disease, and, consciously or otherwise, patients might reduce social activities. The decline in physical role was intriguing, considering that there was no proportional corresponding decline in physical function or vitality, as in the case of the SLE population. This could be due to the failure of the instrument to detect the decline. Alternatively, the role limitation due to emotional factor might have been misperceived as role limitation due to physical concerns.
Fig. 2.
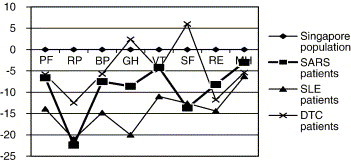
Comparison of the difference in mean scores of SF-36 (using Singapore population norms as reference) among different populations: SARS, SLE, and differentiated thyroid carcinoma (DTC).
Fig. 3.
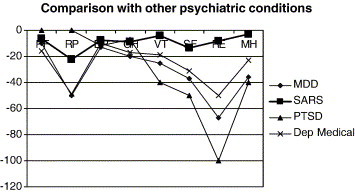
Comparison of the difference in mean scores of SF-36 (using US norms as reference) among different populations: SARS, major depressive disorder, depressed medical patients, and PTSD patients [18], [19], [20].
The health care workers appeared to be more adversely affected judging from the HRQoL SF-36 scores. The reason is not clear. Psychologically, the proximity to “ground zero” might have contributed to the impact of the outbreak on the staff. Besides, health care workers had to deal with grief issues seeing their colleagues die and fall sick. Indeed, Kwek et al. [14] found that some staff reported a sense of failure when previously healthy patients died of SARS. Some had fear of returning to the ward to resume duty. Favaro and Zaetta [15] also reported that the degree of traumatic exposure significantly predicts the presence of PTSD.
Psychological morbidity
Given a national prevalence of minor psychiatric disorders of 17%, the rates of possible PTSD, depression, and anxiety disorders in our population are significantly high: 42%, 27%, and 33%, respectively. This again has implications for the care of these patients.
The small number notwithstanding, it is noteworthy that, although ICU admission impacted on the physical domain of the HRQoL SF-36, it had no significant effect on the psychiatric morbidity. Some patients actually reported they became somewhat confused during their ICU admission and perhaps that had protected them from the traumatising effect of the fearful experience.
The likely PTSD rate (using a cutoff of 25/26) of about 40% appeared high, considering only about 10% was admitted to the ICU. Tedstone and Tarrier [16] studied the rates of PTSD cited in various published studies on different clinical conditions and settings, which ranged from 0% to over 70%, depending on several factors, such as the timing of assessment. Ironson et al. [17], in their study of the impact of Hurricance Andrew, found 44% of their sample scored in the high-impact range of the IES between 1 and 4 months after the disaster. The SARS outbreak had assumed the status of a national disaster. Its novelty, contagion, lethality, and the necessary isolation strategy most likely had contributed to the distress experienced by the victims.
Possible mechanisms
There are a few possible explanations that take into account both the physical and the psychiatric morbidity. Firstly, SARS could have impacted upon the physiology, leading to neuropsychiatric changes.
Secondly, the psychiatric morbidity could be due to the psychological effect of the outbreak. Many patients reported being shocked and intensely fearful of the disease when it first broke out in Singapore. This is borne out by the strong correlation between the psychiatric scores and the HRQoL SF-36 scores (Table 7). Further, the HRQoL SF-36 profile of the SARS patients also shares the typical physical role limitation like that of depressed patients, with a disproportionate impairment in the physical function (Fig. 3) [18], [19]. In the report by Malik et al. [20] on the quality of life of PTSD sufferers (Fig. 3), however, there was neither physical impairment nor physical role limitation. Hence, this does not fully account for the small although significant impairment in physical function, if it were indeed purely psychological.
Whatever the mechanism might be, the comparison between the 6th and 12th week scores shows that the psychological morbidity improved with the passage of time. However, only time will tell if these will eventually resolve completely.
Clinical implications
-
(1)
Psychological care appears important during an outbreak such as SARS.
-
(2)
Recovery in quality of life trails behind the recovery from an acute episode of disease.
-
(3)
Careful follow-up after discharge from an acute episode should be part of the management plan.
Limitations of this study
-
(1)
There was no information collected on past history of psychiatric morbidity. However, going by the low national rates of minor and major psychiatric morbidities, as well as previously well-functioning status, it was unlikely that this impacted on the study outcome.
-
(2)
The response rate was less than half of the total number of victims. As explained earlier, only English questionnaires were sent and hence that could have effectively excluded the Chinese-speaking victims. As it was a postal survey, it was not possible to list English nonliteracy as an exclusion criterion. So the results could only rightly be representative of English-literate victims.
-
(3).
This is a cross-sectional study. While it was interesting to test out the association between parameters, no further conclusion could be drawn about the relationship between them. It would probably shed more light with a further assessment and exploration.
Future directions
Based on this report, a few areas of future research are of relevance.
Firstly, correlation studies on physical parameters (e.g., antibodies titer, hormonal profile, etc.) and psychological status may give a clue on the likely explanation for the psychiatric morbidity in this population. Secondly, studying the immunological status of post-SARS survivors and their psychological status may uncover links between the two functions of the body. Third but not least, study into ways of coping may yield dividend in knowledge of what is helpful and what is not in an outbreak situation.
Footnotes
This study was supported by a grant from the A*STAR Biomedical Research Council.
References
- 1.Poutanen SM, Low DE. Identification of severe acute respiratory syndrome in Canada. N Engl J Med. March 31, 2003 doi: 10.1056/NEJMoa030634. http://www.nejm.org at. [DOI] [PubMed] [Google Scholar]
- 2.Yueng MC, Yu WC. Outbreak of severe acute respiratory syndrome in Hong Kong special administrative region: case report. BMJ. 2003;326:850–852. doi: 10.1136/bmj.326.7394.850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drosten C, Gunther S. Identification of a novel corona virus in patients with severe acute respiratory syndrome. N Engl J Med. April 10, 2003 doi: 10.1056/NEJMoa030747. http://www.nejm.org at. [DOI] [PubMed] [Google Scholar]
- 4.Ksiazek TG, Erdman D. A novel Corona virus associated with severe acute respiratory syndrome. N Engl J Med. 2003 doi: 10.1056/NEJMoa030781. http://www.nejm.org April 10, 2003 at. [DOI] [PubMed] [Google Scholar]
- 5.Nickell LA, Crighton EJ, Tracy CS, Al-Enazy H, Bolaji Y, Hanjrah S. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ. 2004;170(5):793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng SKW, Tsang JSK, Ku KH, Wong CW, Ng YK. Psychiatric complications in patients with severe acute respiratory syndrome (SARS) during the acute treatment phase: a series of 10 cases. Br J Psychiatry. 2004;184:359–360. doi: 10.1192/bjp.184.4.359. [DOI] [PubMed] [Google Scholar]
- 7.Maunder R, Hunter J, Vincent L, Bennett J, Peladeau N, Leszcz M. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168(10):1245–1251. Ovid Full Text Bibliographic Link. [PMC free article] [PubMed] [Google Scholar]
- 8.WHO case definitions for surveillance of severe acute respiratory syndrome (SARS). http://www.who.int/csr/sars/casedefinition/en/.
- 9.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 11.Ware JE, Sherbourne CD. The MOS 36-item short form health survey: I. Conceptual framework and item selection. Med Care. 1991;30:473–483. [PubMed] [Google Scholar]
- 12.McHorney C, Ware JEJ, Raczek A. The MOS 36-item short form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Thumboo J, Chan SP, Machin D. Measuring health-related quality of life in Singapore: normal values for the English and Chinese SF-36 health survey. Ann Acad Med Singapore. 2002;31:366–374. [PubMed] [Google Scholar]
- 14.Kwek SK, Low BL, Ong TC. The psychological impact of SARS on health care providers. Critical Care and Shock. 2004;7:99–106. [Google Scholar]
- 15.Favaro A, Zaetta C. Surviving the Vajont disaster: psychiatric consequences 36 years later. J Nerv Ment Dis. 2004;192(3):227–231. doi: 10.1097/01.nmd.0000117590.81374.7c. [DOI] [PubMed] [Google Scholar]
- 16.Tedstone JE, Tarrier N. Posttraumatic stress disorder following medical illness and treatment. Clin Psychol Rev. 2003;23:409–448. doi: 10.1016/s0272-7358(03)00031-x. [DOI] [PubMed] [Google Scholar]
- 17.Ironson G, Wynings C. Posttraumatic stress symptoms, intrusive thoughts, loss, and immune function after Hurricane Andrew. Psychosom Med. 1997;59(2):128–141. doi: 10.1097/00006842-199703000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Ware JE, Snow KK, Kosinski M, Gandek B. New England Medical Center Health Institute; Boston: 1993. SF-36 health survey manual and interpretation guide. [Google Scholar]
- 19.Jackson-Triche ME, Sullivan JG, Wells KB, Rogers W, Camp P, Mazel R. Depression and health-related quality of life in ethnic minorities seeking care in general medical settings. J Affect Disord. 2000;58:89–97. doi: 10.1016/s0165-0327(99)00069-5. [DOI] [PubMed] [Google Scholar]
- 20.Malik ML, Connor KM, Sutherland SM, Smith RD, Davison RM, Davidson RT. Quality of life and post traumatic stress disorder: a pilot study assessing changes in SF-36 scores before and after treatment in a placebo-controlled trial of fluoxetine. J Trauma Stress. 1999;12(2):387–393. doi: 10.1023/A:1024745030140. [DOI] [PubMed] [Google Scholar]


