A cluster of cases of pneumonia caused by a novel coronavirus, COVID-19, was first reported in Wuhan in the Hubei province in China in late December 2019. Since then, several thousand cases have been reported in mainland China, with spread to over two dozen countries. Although many comparisons to other coronavirus epidemics have been made, the potential impact of this coronavirus is uncertain. We seek to summarize what is known about COVID-19, compare this epidemic to prior coronavirus outbreaks, and provide a primer on novel coronaviruses for practicing clinicians.
Coronaviruses are widespread among mammals and birds. The widest varieties of genotypes infect bats, but 2 subtypes infect humans: alpha and beta coronaviruses.1 Beta coronaviruses include severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory syndrome coronavirus (MERS-CoV), and the coronavirus variant COVID-19 virus first described in Wuhan. In humans, these coronaviruses have short incubation periods, ranging from days for SARS-CoV and weeks for MERS-CoV, with the COVID-19 appearing to fall in between the two.2 , 3 Although information about the COVID-19 is emerging, SARS-CoV and MERS-CoV provide some context for understanding the public health significance of coronaviruses.
SARS- CoV
SARS-CoV was first noted in the Guangdong province of China in November 2002.4 , 5 The index case was a physician from that province who then traveled to Hong Kong and infected several others. Subsequently, SARS-CoV resulted in over 8000 cases and approximately 750 deaths occurred worldwide over the next several months. The outbreak finally ended in July 2003.4, 5, 6 Severe acute respiratory syndrome coronavirus typically presented with fever and symptoms of lower respiratory tract infection with radiographic evidence of pneumonia or acute respiratory distress syndrome (ARDS).
SARS-CoV disproportionately impacted health care workers (HCWs) in countries with the most reported cases. However, in countries with relatively few cases, transmission was much rarer. This finding suggests that infection control measures are adequate to interrupt transmission to HCWs, but consistency is critical because the greater number of opportunities for lapses in the hardest hit centers likely led to more HCW infections.7
The incubation period of SARS-CoV is between 2 and 10 days.8 Diagnosis is based on polymerase chain reaction testing. Treatments attempted included corticosteroids and ribavirin, which were not found to be beneficial. Supportive care remains the cornerstone of care for SARS-CoV, although in vitro studies suggest that antivirals developed in the wake of the Ebola virus epidemic may inhibit SARS-CoV replication as well.9
MERS-CoV
MERS-CoV was first reported in September 2012.10 The virus was isolated from sputum of a man in Saudi Arabia hospitalized with a respiratory tract infection.10 Since then, more than 2400 cases of MERS-CoV have been reported to the World Health Organization (WHO) in and around the Arabian Peninsula.11 Periodic infections and localized outbreaks have continued. Similar to SARS-CoV, presentation is typically fever with symptoms of lower respiratory tract infection and radiographic evidence of pneumonia or ARDS. Other manifestations might include renal failure, anorexia, nausea, vomiting, diarrhea, abdominal pain, and disseminated intravascular coagulation. Again, HCWs were disproportionately infected, although a large number of those cases were mild or asymptomatic.7
The incubation period of MERS-CoV ranges from 1 to 14 days. Diagnosis is made by identifying the virus in respiratory samples by polymerase chain reaction testing. Treatment is largely supportive,11 focusing on management of complications of sepsis and ARDS in intensive care units. Antivirals such as ribavirin and interferon-based treatments have had questionable benefit, but the role for these treatments remains experimental.12
COVID-19
Epidemiology
Most recently, a novel strain of the coronavirus, COVID-19, was identified in Wuhan, a city in the Hubei province of China.3 Initial cases were associated with a seafood market that also sold live animals.2 The seafood market was shut down and disinfected to contain what was thought to be a zoonotic infection, ie, one that is transmitted from animals to humans. Despite this intervention, the reported number of persons infected increased rapidly, and on January 21, 2020, Chinese health authorities first reported human-to-human transmission including transmission to HCWs. Since then, case counts have been increasing rapidly.13 Cases have now been reported outside mainland China, with the spread of cases internationally to several countries in Asia, Europe, North America, and to Australia. Person to person transmission has been reported to family members, other close contacts, and to HCWs.
Clinical Features
Initial reports suggest an incubation period similar to the incubation period of SARS-CoV and MERS-CoV.2 The clinical features are also rather similar to these viruses: fever, cough, chest tightness, dyspnea, and difficulty breathing.14 , 15 Severe cases with ARDS have been reported, with this being a leading reason for admission to the intensive care unit.2
Gastrointestinal symptoms have been reported in 10% of cases, a higher proportion than seen with other coronaviruses. The novel coronavirus also is associated with fewer upper respiratory tract symptoms and lower respiratory symptoms than other coronaviruses.14 Fever is a prominent symptom, present in 98.6% of cases.16
Between 20% and 25% require intensive care unit admission. Patients admitted to ICU had higher serum white blood cell counts, lower serum albumin, liver function test disorders, and higher D-dimer.14 Significantly, severe cases appear to cluster in the elderly, and thus far, severe disease has not been widely reported in children.16
The Centers for Disease Control and Prevention (CDC) has issued interim guidance for HCWs.17 Novel coronavirus should be suspected if patients meet the criteria described in Table 1 . The WHO uses similar criteria for case identification.
Table 1.
COVID-19 Diagnosis Criteria to Serve as Guidance for Evaluation
| COVID-19 Clinical features | COVID-19 Epidemiological risk |
|---|---|
| Fever AND symptoms of lower respiratory tract illness including, but not limited to, cough, difficulty breathing → | AND any one of the following: |
| (a) In the past 14 days (before symptom onset), a history of travel from Wuhan City, China | |
| OR | |
| (b) In the past 14 days (before symptom onset), close contact with a person who is under investigation for COVID-19 while that person was ill | |
| Fever OR symptoms of lower respiratory tract illness including, but not limited to, cough, difficulty breathing → | AND |
| In the past 14 days (before symptom onset), close contact with an ill patient with laboratory-confirmed COVID-19 |
COVID-19 = 2019 novel coronavirus.
Adapted from the Centers for Disease Control and Prevention.16
Approach to a Suspected Case and Diagnosis
The current approach includes early diagnosis and identification, prevention of spread, and management of complications.18 Optimal supportive care with appropriate isolation and infection control precautions are cornerstones of treatment. Health care professionals who encounter suspected cases should contact local infection control and public health offices regarding potential cases and appropriate next steps based on regional resources and protocols.
Many unknowns remain regarding COVID-19. The exact mode of transmission has not been established. It appears that most transmission occurs by droplet spread, ie, large droplets that are generated when a patient coughs or sneezes. Protection against this type of transmission involves use of face masks with eye protection, gloves, gowns, and hand hygiene. There is concern that airborne transmission may also be playing a role. This possibility is more problematic because airborne infectious particles can remain suspended in the air for long periods, the infection can be transmitted to larger numbers of people including those not in close contact with the index case, and protective measures include wearing a respirator and patient placement in negative air pressure rooms that may not be available at all medical centers. At the present time, the CDC recommends a combination of airborne precautions (patient placement in a negative air pressure room, HCWs to wear respirators), contact precautions (HCWs to wear gloves and gowns for all patient contact), and use of eye protection for patients hospitalized with suspected COVID-19 infection.
An initial report suggested transmission from an asymptomatic individual to several other people who attended business meetings with the index case. This has since been reported to be inaccurate.19 Table 2 presents a comparison of clinical symptoms of the 3 coronavirus strains that have caused worldwide outbreaks. As more cases are identified, the epidemiology and clinical characteristics of this disease will be better elucidated.
Table 2.
Comparison of Clinical Symptoms and Public Health Characteristics of 3 Coronavirus Strains
| Characteristic | SARS-CoV (2002-2003) | MERS-CoV (2012-2013) | COVID-19 (2019-2020) |
|---|---|---|---|
| Clinical presentation | (1) Fever | (1) Pneumonia | (1) Fever, cough, dyspnea |
| (2) Symptoms of lower respiratory tract infection (cough, dyspnea, difficulty breathing) | (2) Renal injury | (2) Radiologic evidence of pneumonia | |
| (3) Radiologic evidence of pneumonia or ARDS | (3) ARDS | (3) ARDS | |
| (4) Diarrhea | |||
| (5) Vomiting | |||
| Incubation period | 2-10 d | 1-14 d | 5-7 d (per initial reports) |
| Geographic location | China | Arabian Peninsula | Australia |
| Hong Kong | United States (2 imported cases) | Belgium | |
| Canada | South Korea (MERS-CoV outbreak in 2015) | Cambodia | |
| Singapore | Canada | ||
| Vietnam | China (including Hong Kong and Macau) | ||
| Finland | |||
| France | |||
| Germany | |||
| India | |||
| Italy | |||
| Japan | |||
| Malaysia | |||
| Nepal | |||
| Nepal | |||
| Singapore | |||
| South Korea | |||
| Spain | |||
| Sri Lanka | |||
| Sweden | |||
| Taiwan | |||
| Thailand | |||
| United Arab Emirates | |||
| United Kingdom | |||
| United States | |||
| Vietnam | |||
| Cases | 8096 | 2468 | 37,592a |
| Case fatality rate | 14%-15%20 | 35%12 | 2.2%a |
ARDS = acute respiratory distress syndrome; MERS-CoV = Middle East respiratory syndrome coronavirus; COVID-19 = 2019 novel coronavirus; SARS-CoV = severe acute respiratory syndrome coronavirus.
As of February 9, 2020.
Laboratory Testing
The release of the viral genome sequence has made it possible for the CDC to create a rapid molecular diagnostic test for COVID-19. The test received expedited approval from the FDA and the test is being made available to state health departments and selected commercial laboratories. At this time the test is only performed at the CDC but it is likely that the test will be made available at several state health departments in the near feature. The currently available diagnostic tests for other coronaviruses (eg, FilmArray Respiratory Panel [BioFire Diagnostics]) do not detect the COVID-19.
Because of the potential for transmission to laboratory workers from patient specimens, the CDC recommends that laboratory workers use a class 2 biological safety cabinet and personal protective equipment when processing specimens with potential to generate fine particulate matter. Decontamination of work surfaces and equipment with Environmental Protection Agency–registered hospital disinfectant is of paramount importance.21 When transporting suspected case specimens, the International Air Transport Association guidelines for dangerous goods must be followed.21
Response and Public Health Impact
Chinese officials closed the fish market initially suspected as the source of the virus on January 1, 2020. On January 20, China confirmed human to human transmission of this virus.22 , 23 On January 23, the Chinese government suspended air, road, and rail travel in the area around Wuhan in an effort to limit the spread outside the city over the Chinese New Year, traditionally a very busy time to travel. In addition, public gatherings for New Year festivities were banned all over the country. Over the next few days, quarantine orders were extended to cover the entire province of Hubei. Despite these stringent measures, case counts continued to rise within China, and several countries including the United States reported imported cases.
On January 30, the WHO declared that the COVID-19 outbreak was a public health emergency of international consequence (PHEIC). On January 31, the United States announced that it would bar entry of foreign nationals who had visited China and quarantine United States citizens arriving from China for 14 days. Simultaneously, several major United States airlines suspended flights to mainland China. Since then several other nations have imposed similar travel bans. However, at the time of this writing over 35,000 cases have been confirmed in 28 countries and there have been more than 800 deaths.24, 25, 26
China was initially lauded for its efforts to control the outbreak, including the construction of a 1000 bed medical facility in less than 10 days. More recently, the death of a Chinese physician Li Wenlinag, who was reprimanded by Chinese authorities for sounding the alarm about a cluster of pneumonia in December, has rekindled misgivings about how China is handling the situation.
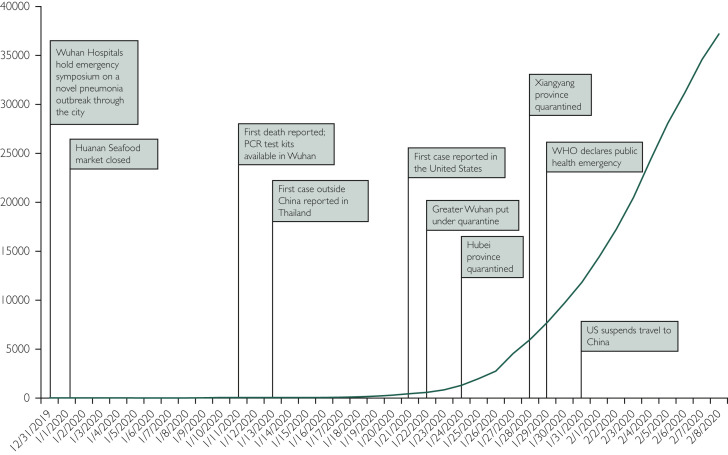
At the time of this report, there have been more than 35,000 confirmed cases of COVID-19, with more than 800 confirmed deaths (Figure).27 , 28 Deaths appear to be occurring predominantly in the elderly, with a median age of 75 years in reported cases, but lately, younger patients have died as well.
Figure.
Timeline of events since the first report of COVID-19.
Conclusion
The COVID-19 has resulted in a large outbreak of febrile respiratory illness originating in mainland China. There are still many unknowns: mode of transmission, risk factors for infection and mortality, and whether there is a nonhuman reservoir that could cause additional outbreaks. China has taken unprecedented measures to contain the infection by quarantining large cities, imposing bans on mass gatherings, and canceling public events associated with the Chinese New Year. Travel bans imposed by several countries have slowed, but not completely eliminated, the spread outside of China. In addition to the suffering and loss of life, the impact on the global supply chain is likely to be very significant as China as a whole, and Wuhan in particular, are major manufacturing hubs.
There are fears that we are on the verge of a global pandemic. We are better prepared today than we have ever been in the past to limit the spread of infections in health care facilities in the United States. The CDC has provided conservative guidance on infection control measures to be used for a patient with the COVID-19 infection, but this is dependent on early recognition. There are no specific features that distinguish this infection from other respiratory viral infections. Following standard precautions, a set of infection control principles that recommend common sense precautions, including providing a mask to persons with a cough in outpatient settings, promoting hand hygiene, and asking sick individuals to maintain social distancing, are key to controlling rapid spread of the COVID-19 and all respiratory infections in general.
Footnotes
Potential Competing Interests: Dr Sampathkumar reports consultancy fees from Merck. The other authors report no competing interests.
Supplemental Online Material
References
- 1.Chan J.F., Lau S.K., To K.K., Cheng V.C., Woo P.C., Yuen K.Y. Middle East respiratory syndrome coronavirus: another zoonotic betacoronavirus causing SARS-like disease. Clin Microbiol Rev. 2015;28(2):465–522. doi: 10.1128/CMR.00102-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Imai N., Dorigatti I., Cori A., Riley S., Ferguson N.M. Imperial College London; London, UK: January 17, 2020. Estimating the potential total number of novel coronavirus (COVID-19) cases in Wuhan City, China. [Google Scholar]
- 3.World Health Organization Novel coronavirus (COVID-19). World Health Organization website. Published 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 4.Christian M.D., Poutanen S.M., Loutfy M.R., Muller M.P., Low D.E. Severe acute respiratory syndrome. Clin Infect Dis. 2004;38(10):1420–1427. doi: 10.1086/420743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peiris J.S., Yuen K.Y., Osterhaus A.D., Stohr K. The severe acute respiratory syndrome. N Engl J Med. 2003;349(25):2431–2441. doi: 10.1056/NEJMra032498. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. World Health Organization website. http://www.who.int/csr/sars/country/table2004_04_21/en/index.html. Accessed January 27, 2020.
- 7.Park B.J., Peck A.J., Kuehnert M.J. Lack of SARS transmission among healthcare workers, United States. Emerg Infect Dis. 2004;10(2):244–248. doi: 10.3201/eid1002.030793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sampathkumar P., Temesgen Z., Smith T.F., Thompson R.L. SARS: epidemiology, clinical presentation, management, and infection control measures. Mayo Clin Proc. 2003;78(7):882–890. doi: 10.4065/78.7.882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agostini M.L., Andres E.L., Sims A.C. Coronavirus susceptibility to the antiviral remdesivir (GS-5734) is mediated by the viral polymerase and the proofreading exoribonuclease. mBio. 2018;9(2):e00221–e00228. doi: 10.1128/mBio.00221-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zaki A.M., van Boheemen S., Bestebroer T.M., Osterhaus A.D., Fouchier R.A. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia [published correstion appears in N Engl J Med. 2013;369(4):394] N Engl J Med. 2012;367(19):1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 11.Sampathkumar P. Middle East respiratory syndrome: what clinicians need to know. Mayo Clin Proc. 2014;89(8):1153–1158. doi: 10.1016/j.mayocp.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arabi Y.M., Balkhy H.H., Hayden F.G. Middle East respiratory syndrome. N Engl J Med. 2017;376(6):584–594. doi: 10.1056/NEJMsr1408795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention Lesson 6: Investigating an outbreak. Centers for Disease Control and Prevention website. https://www.cdc.gov/csels/dsepd/ss1978/lesson6/section2.html
- 14.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China [published online ahead of print January 24, 2020] https://doi.org/10.1016/S0140-6736(20)30183-5 Lancet. [DOI] [PMC free article] [PubMed]
- 15.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019 [published online ahead of print January 24, 2020] https://doi.org/10.1056/NEJMoa2001017 N Engl J Med. [DOI] [PMC free article] [PubMed]
- 16.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. [published online ahead of print February 7, 2020] https://doi.org/10.1001/jama.2020.1585 JAMA. [DOI] [PMC free article] [PubMed]
- 17.Centers for Disease Control and Prevention 2019 Novel coronavirus: interim guidance for healthcare professionals. Centers for Disease Control and Prevention website. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-criteria.html Updated February 12, 2020. Accessed February 12, 2020.
- 18.World Health Organization Infection prevention and control. World Health Organization website. Published 2020. https://www.who.int/csr/disease/coronavirus_infections/prevention_control/en/
- 19.Rothe C., Schunk M., Sothmann P. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany [published online ahead of print January 30, 2020] N Engl J Med. 2020 doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yanan W., Moritsugu K. Human-to-human transmission confirmed in China coronavirus. AP News website. https://apnews.com/14d7dcffa205d9022fa9ea593bb2a8c5 PublishedJanuary 19, 2020. Accessed Januray 19, 2020.
- 21.Roos R. Estimates of SARS death rates revised upward. University of Minnesota Center for Infectious Disease Research and Policy website. http://www.cidrap.umn.edu/news-perspective/2003/05/estimates-sars-death-rates-revised-upward Published May 7, 2003. Accessed Januray 27, 2020.
- 22.Centers for Disease Control and Prevention Interim laboratory biosafety guidelines for handling and processing specimens associated with 2019 novel coronavirus (COVID-19). Centers for Disease Control and Prevention website. https://www.cdc.gov/coronavirus/COVID-19/lab-biosafety-guidelines.html Reviewed February 2, 2020. Accessed January 17, 2020.
- 23.Wuhan Tianhe Airport was put into operation on April 15, 1995. CNHubei website. https://web.archive.org/web/20171107024254/http://www.cnhubei.com/xwzt/2008zt/hbgg30y/bhdss/tianhe/fazhan/200804/t287403.shtml Published April 17, 2008. Accessed Januray 27, 2020.
- 24.Civil Aviation Administration of China Statistics of key performance indicators for China's civil aviation industry in October 2019. Civil Aviation Administration of China website. http://www.caac.gov.cn/en/HYYJ/SJ/201912/t20191223_199948.html Updated December 23, 2019. Accessed January 27, 2020.
- 25.Coronavirus what airport measures are in place to detect sick passengers? The Guardian website. https://www.theguardian.com/world/2020/jan/18/coronavirus-what-airport-measures-are-in-place-to-detect-for-sick-passengers Published January 18, 2020. Accessed January 27, 2020.
- 26.Ahmed I., Roxburgh H. US confirms first case of China virus as death toll reaches six. International Business Times website. https://www.ibtimes.com/china-says-virus-spreading-between-humans-who-set-meet-2906266 Published January 21, 2020. Accessed January 27, 2020.
- 27.Visual and Data Journalism Team Coronavirus: a visual guide to the outbreak. BBC News website. https://www.bbc.com/news/world-51235105 Updated February 7, 2020. Accessed January 27, 2020.
- 28.Talmazan Y., Baculinao E., Chen L., Abbas M. China coronavirus death toll climbs to 106 as government scrambles to contain outbreak. NBC News website. https://www.nbcnews.com/news/world/china-coronavirus-death-toll-climbs-80-government-scrambles-contain-outbreak-n1123561 Published January 27, 2020. Updated January 28, 2020. Accessed January 27, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.