Abstract
Sepsis, acute lung injury, and ARDS contribute substantially to the expanding burden of critical illness within our ICUs. Each of these processes is characterized by a myriad of injurious events, including apoptosis, microvascular dysfunction, abnormal coagulation, and dysregulated host immunity. Only recently have platelets—long considered merely effectors of thrombosis—been implicated in inflammatory conditions and the pathobiology of these disease processes. A growing body of evidence suggests a prominent role for maladaptive platelet activation and aggregation during sepsis and ARDS and has begun to underscore the pluripotential influence of platelets on outcomes in critical illness. Not only do platelets enhance vascular injury through thrombotic mechanisms but also appear to help orchestrate pathologic immune responses and are pivotal players in facilitating leukocyte recruitment to vulnerable tissue. These events contribute to the organ damage and poor patient outcomes that still plague the care of these high-risk individuals. An understanding of the role of platelets in critical illness also highlights the potential for both the development of risk stratification schema and the use of novel, targeted therapies that might alter the natural history of sepsis, acute lung injury, and ARDS. Future studies of adenosine, platelet polyphosphates, and the platelet transcriptome/proteome also should add considerably to our ability to unravel the mysteries of the versatile platelet.
Abbreviations
- ADP
adenosine diphosphate
- ALI
acute lung injury
- CRP
C-reactive protein
- GP IIb/IIIa
glycoprotein IIb/IIIa
- PCI
percutaneous coronary intervention
- vWF
von Willebrand factor
Sepsis, acute lung injury (ALI), and ARDS all contribute substantially to the expanding burden of critical illness within the United States. Epidemiologic estimates suggest an incidence of 200,000 patients annually for ALI/ARDS,1, 2 with a comparably large and growing incidence of sepsis.3 The morbidity and mortality of these disease processes likewise are staggering. In-hospital death rates range from 26% to 38% in studies of ARDS,1, 2 whereas sepsis kills nearly one-half of those severely affected.4 For patients who ultimately survive their initial hospitalization, quality of life often is dramatically reduced, and the economic impact is considerable. Sepsis, for instance, contributes nearly $17 billion toward the burgeoning costs of US critical care delivery.5
From a pathophysiologic perspective, sepsis, ALI, and ARDS are all characterized by abnormally enhanced coagulation, dysregulated and often injurious host immunity, microvascular dysfunction, and tissue necrosis. Increasing evidence suggests that hematologic derangements are associated with and may be important contributors to disease severity, largely influenced by alterations in platelet and leukocyte function.6 Although platelet-mediated thrombosis has been implicated in their pathobiology, a host of other platelet-associated effects can influence their natural history. Understanding the pluripotential impact of platelets in immunopathology and their specific role in the development and progression of critical illness is vitally important to those clinicians and investigators who hope to improve the care of these high-risk patients.
Overview of Platelet Structure and Function
Platelets are anucleate cells of myeloid origin that continuously flow in a quiescent state throughout the human vasculature.7 Derived from megakaryocytes, the circulating platelet readies itself to perform a myriad of hemostatic, inflammatory, and reparative tasks once activated.8 Under conditions of heightened demand, platelet production can increase by as much as 20-fold. When summoned by tissue injury and inflammation, this amplified platelet offensive can then exert its influence on a variety of other cells directly or through the release of highly potent intracellular constituents.
Platelet recruitment and adhesion are orchestrated by a number of specialized chemokines, adhesion molecules, and receptors. In particular, platelets express cell surface receptors called integrins. Integrins make up a large family of receptors that are constitutively expressed on the surface of many cells and whose job it is to facilitate both cell-to-cell and cell-to-extracellular matrix interactions.9 Perhaps the most well known and most abundant platelet integrin is the glycoprotein IIb/IIIa (GP IIb/IIIa) receptor. Following cellular activation, GP IIb/IIIa binds fibrinogen, fibrin, and other ligands, mediating adhesive events and stimulating platelet aggregation. Other integrins play key roles in adhesion, aggregation, thrombus formation, and vascular repair.
In addition to the integrins, there are a number of G-protein-coupled receptors present on the platelet surface that promote platelet activation, changes in platelet rheology, and enhanced aggregation. Protease-activated receptor 1, for example, plays a pivotal role in the activation of platelets.9 Thromboxane A2 induces aggregation and vascular smooth muscle contraction. Stimulation of adenosine diphosphate (ADP) receptors on the platelet surface results in alterations in platelet shape and supports further platelet aggregation.
The metabolically primed armamentarium of the platelet extends beyond these cell surface receptors, however. Platelets also express and release a variety of adhesion molecules, mitogenic factors, and vasoactive compounds, all of which play key roles in modulating endothelial function, aggregation, and cellular interactions. These compounds include cytoplasmic substances such as serotonin, epinephrine, norepinephrine, nitric oxide, vascular endothelial growth factor, and transforming growth factor β8; the selectins, which interact with cell surface glycoconjugates to mediate adhesion and cellular communication10; and mitochondrial lysosomes, which store and release potent glycosidases, proteases, and cationic proteins.11 Platelets also contain α granules, which release important contributors to coagulation,9 and dense granules, which release nonprotein molecules, including ADP, calcium, and serotonin, that modulate inflammatory and thrombotic processes (Table 1 ).11
Table 1.
Platelet Receptors, Surface Molecules, and Intracellular Constituents Contributing to the Inflammatory Response During Critical Illness
| Platelet Components | Stimuli | Effects |
|---|---|---|
| Receptors and surface molecules | ||
| Integrins | ||
| GP IIb/IIIa | Fibrinogen, fibrin | Platelet aggregation |
| G-protein-coupled receptors | ||
| Protease-activated receptors | Thrombin | Platelet activation |
| Thromboxane receptors | Thromboxane A2 | Activation, aggregation |
| ADP receptors | ADP | Activation, aggregation, altered rheology |
| P-selectin | Inflammation and tissue injury | Adhesion, cellular communication |
| Intracellular constituents | ||
| Cytoplasmic substances | ||
| Serotonin | Inflammation and tissue injury | Platelet activation |
| Epinephrine | Inflammation and tissue injury | Platelet activation |
| α Granules | Inflammation and tissue injury | Secretion facilitates coagulation |
| Dense granules | Inflammation and tissue injury | Release ADP, calcium, serotonin |
ADP = adenosine diphosphate; GP IIb/IIIa = glycoprotein IIb/IIIa.
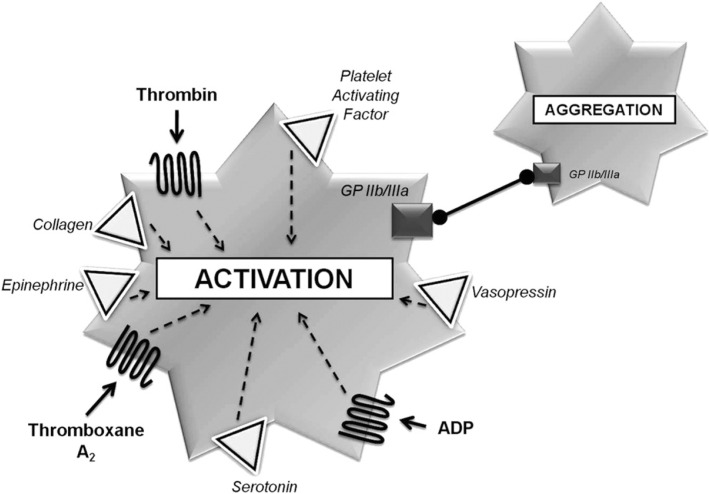
It is well known that platelets are the primary effector cells of hemostasis, and their roles in both thrombosis and vascular repair have been well established. There are four main phases governing platelet function: (1) activation, (2) adhesion, (3) aggregation, and (4) secretion. Under the influence of substances, including thrombin, collagen, epinephrine, vasopressin, platelet-activating factor, and arachidonic acid metabolites, released from sites of tissue injury, platelets are activated and undergo robust rheologic transformation (Fig 1 ). When components of the subendothelial matrix then become exposed to circulating blood, platelet glycoproteins and von Willebrand factor (vWF) mediate an intense adhesive process. Platelet aggregation firmly ensues, largely supported by the GP IIb/IIIa receptor, and these events are then ultimately reinforced by a potent milieu of vasoactive compounds secreted from the galvanized platelet offensive.8
Figure 1.
Key participants in human platelet activation and aggregation. ADP = adenosine diphosphate; GP IIb/IIIa = glycoprotein IIb/IIIa.
Platelets in Host Immunity
Platelets have long been considered by many to be vital participants in immune processes and, hence, potentially key instigators in a number of common inflammatory diseases. Once activated, platelets release numerous secretory products and have been shown to express a multitude of receptors involved in the inflammatory response (Table 1). In atherosclerosis, for instance, activated platelets can release adhesive ligands such as P-selectin. P-selectin is capable of creating a phospholipid-rich platform that then facilitates the recruitment of mononuclear cells and lymphocytes to the atherosclerotic plaque.7 Platelet activation has been associated with enhanced cytokine expression in other inflammatory conditions, including acute coronary syndromes, coronary stent restenosis, and solid organ transplant rejection.12, 13
Platelets also interact directly with other inflammatory cells, helping to engineer both physiologic and pathologic immune events. Leukocytes, for instance, are known to play an important role in host defense when recruited to sites of inflammation.14 Although critical in helping to defend the host from invading microorganisms, untoward sequelae of leukocyte recruitment can include tissue injury, hypoxia, and organ dysfunction.15 Platelets have been shown to facilitate the leukocyte response, largely under the influence of P-selectin, which promotes leukocyte-platelet binding.15, 16
Although platelets interact with most leukocyte subpopulations, it is their intimate relationship with neutrophils that seems to drive their primary role in host immunity. Endothelial-bound platelets can induce “secondary capture” of neutrophils by first facilitating platelet-neutrophil interactions and then by directing subsequent neutrophil-endothelial cell contact. Neutrophils also are capable of rolling along a template of adherent platelets—an event regulated by numerous adhesive receptors and promoted by shear forces and alterations in cellular structure.17 This rolling phenomenon is thought to be mediated largely by P-selectin, which directs leukocyte adherence and then supports leukocyte transmigration directly to the site of injury.18
Thrombocytopenia in Critical Illness
From a more clinical perspective, alterations in platelet number and function are frequently recognized in association with critical illness. In particular, the development of thrombocytopenia is commonplace, with an incidence ranging from 20% to nearly 50% across a spectrum of intensive care settings.19, 20 When present, thrombocytopenia is independently associated with increased morbidity and mortality.19, 20
What has been less well established is a causal relationship between thrombocytopenia and critical care outcomes. Whether thrombocytopenia represents platelet activation and consumption as a primary pathologic event or merely serves as a marker for disease severity is unknown. This uncertainty is a consequence of the myriad of conditions known to influence circulating platelet numbers in heterogeneous ICU patients, rendering it difficult for investigators to account for all potential confounders in clinical research. Critically ill individuals may have diminished platelet production due to medication effects, bone marrow suppression, nutritional deficiencies, and infection. They also may have enhanced platelet elimination due to splenic sequestration, consumption related to disseminated intravascular coagulopathy, and thrombocytopenia as a result of hemodilution. Immunologically mediated thrombocytopenia and spurious thrombocytopenia also can introduce complexity into a patient's evaluation and ICU course.
Thrombocytopenia is a poor prognostic marker and a rather powerful predictor of mortality in patients with sepsis and septic shock,21 and the magnitude of platelet reduction seems to correlate with the severity of illness.20, 22 In ALI and ARDS, the development of clinical thrombocytopenia and its influence on outcomes are poorly understood. In small patient series representing noncontemporary treatment eras, thrombocytopenia was believed to occur in as many as 50% of patients with ARDS.18, 23 The degree of thrombocytopenia has been shown to parallel the course of progressive hypoxemic respiratory failure24 but has been inconsistently associated with mortality.24, 25 More recently, thrombocytopenia has been described as a prominent feature among patients with severe acute respiratory syndrome, a rapidly progressive coronavirus-associated respiratory illness resulting in a global outbreak of ALI and shock.26
Platelets in Sepsis
Activation and Aggregability
There are conflicting data about platelet function and response to stimuli in critically ill patients with sepsis. Some would suggest that the septic milieu, in part influenced by lipopolysaccharide and endotoxemia, promotes enhanced platelet aggregation, leading to microvascular obstruction and tissue injury.27 Others have argued that aggregation and platelet responsiveness actually decrease in patients with sepsis,28 whereas still others have suggested that activation may in fact be enhanced during sepsis but that significant platelet degranulation only occurs in those who are most severely decompensated.29
Gawaz and colleagues29 found that plasma from patients with sepsis increased both the adhesion and the aggregability of normal platelets to cultured endothelium. Mavrommatis et al22 later showed that platelet activation was significantly increased in patients with sepsis compared with healthy control subjects. Others have demonstrated that sepsis results in increased P-selectin expression.30 On the other hand, platelet function by aggregometry and flow cytometry was shown to be decreased in studies by Yaguchi et al,31 and Boldt et al32 demonstrated that aggregation decreased over time in a cohort of trauma patients who later developed sepsis.
Recently, both human and murine platelets have been shown to express toll-like receptors 4 that facilitate platelet migration and deposition into tissue during sepsis.33 It is possible that these pattern recognition receptors may represent a unique mechanism by which organ dysfunction develops in severe infection; further research, however, will be necessary to clarify this association.
Acquired deficiencies in the plasma protease ADAMTS13 also may support the enhanced platelet activation that has been described in both sepsis and the systemic inflammatory response syndrome. Nguyen and colleagues34 reported functional decreases in ADAMTS13—the principle physiologic modulator of vWF in human plasma—among patients with sepsis. Others have demonstrated a stepwise decline in ADAMTS13 activity, which paralleled the extent of inflammatory response in small samples of critically ill ICU patients.35
The burden of evidence seems to support the notion that platelet activation and aggregation increase during sepsis. The result of this accelerated platelet response, and the mechanism of resulting tissue injury, is less well defined. Although small studies have shown that platelets can cause microvascular obstruction and tissue hypoperfusion, impairment in cardiac contractility,36 and endothelial dysfunction as a consequence of platelet-induced apoptosis,37 it is likely that a number of other poorly defined pathologic events contribute to the untoward influence of platelets on septic outcomes.
Platelet-Leukocyte Interactions
One such mechanism of injury during sepsis may center around the aforementioned role that platelets play in leukocyte recruitment. Although this likely represents an adaptive response to facilitate host defense, there is mounting evidence to suggest that maladaptive platelet-leukocyte interactions can result in tissue injury.38 In a study of polymicrobial sepsis, Asaduzzaman et al39 found that significant lung injury resulted from enhanced pulmonary infiltration of platelet-bound neutrophils. Other investigators have demonstrated that inhibition of platelet-associated neutrophil recruitment can mitigate all forms of end-organ damage, helping to establish a causal relationship between platelet-neutrophil interactions and the pathologic injury seen in severe sepsis.40, 41
It has been proposed that platelets recruit neutrophils to sites of tissue injury and inflammation, resulting in subsequent damage through a variety of mechanisms. Platelet-neutrophil aggregates may become trapped within narrow sites of organ microvasculature, leading to regional ischemia. Kirschenbaum and colleagues,42 for instance, showed that formation of these aggregates had a pronounced effect on altering blood rheology in patients with sepsis, a process that the investigators believed contributed significantly to impairments in perfusion. Platelets also may adhere directly to inflamed endothelial cells and promote secondary capture of toxic circulating leukocytes. This mechanism has been supported by several small studies in which targeted inhibition of platelet-specific ligands on neutrophils reliably attenuated sepsis-associated endothelial injury.29, 43 Circulating platelet-neutrophil complexes and platelet-stimulated neutrophil extracellular trap formation also can be seen in the patient with sepsis. These neutrophil extracellular traps are believed to represent a subset of activated neutrophils with enhanced ability to adhere, phagocytose, and produce injurious superoxide.43 Finally, other data suggest that lymphotoxicity and lymphoid cell apoptosis may result from sepsis-induced alterations in platelet mRNA profiles.44
Platelets in ALI and ARDS
Dysregulated hemostasis and enhanced inflammation are hallmark pathophysiologic events associated with both ALI and ARDS. Postmortem series of patients with ARDS have shown that platelet deposition within the damaged pulmonary microvasculature is commonplace.45 Ultrastructural examinations of lungs from patients with ARDS have consistently shown platelet accumulation and platelet-fibrin deposition occurring within pulmonary arteries, arterioles, and capillaries as well as within both the pulmonary interstitial and the alveolar compartments of affected individuals.46
Platelet-Specific Mechanisms of Injury
As in sepsis, platelet-neutrophil interactions seem to play a dominant role in tissue injury seen during ARDS. In a murine model of acid-induced lung injury, Zarbock and colleagues41 demonstrated that increased neutrophil adhesion and activation resulted from thromboxane A2 produced by platelet-neutrophil aggregates. Efforts to deplete platelets or disrupt these aggregates resulted in reduced neutrophil migration and permeability, improved gas exchange, and better survival.
Enhanced platelet activation and secretion also have been supported by several other clinical and preclinical studies of ALI. In a ventilator stress-induced model of ARDS, Yiming et al47 demonstrated increased expression of vWF, glycoprotein Ib, and P-selectin on the endothelial surfaces of rat and mice lungs. In a bronchoscopic study of patients with lung injury, Idell and colleagues48 found that levels of platelet-specific α-granule proteins were elevated in BAL fluid from injured tissue and directly correlated with the degree of pulmonary injury. In a study of critically ill patients, investigators not only found that in vivo platelet activation was more robust among those with acute respiratory failure but also showed that marked platelet dysfunction, characterized by impaired aggregation and prolonged bleeding time, was a typical feature in these individuals.49
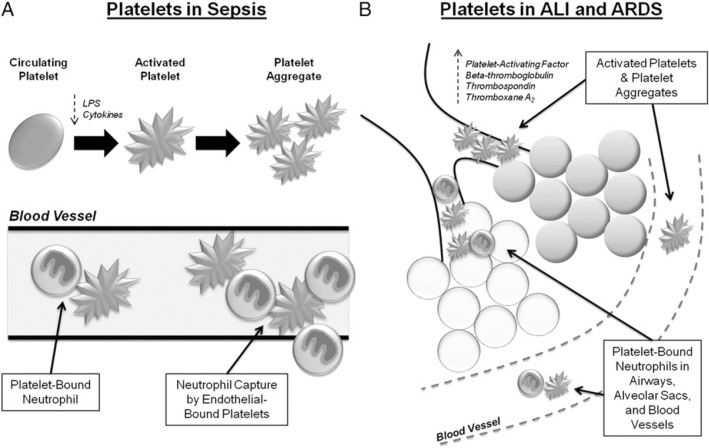
A careful review of several currently used evidence-based therapies for ALI and ARDS provides additional insight into the potential pathologic role of platelet-mediated events. A host of clinical studies have helped to define contemporary treatment strategies for this critical illness, and several of these therapies share, in part, an ability to modify mechanisms of platelet activation and aggregation. Perhaps the most well-validated strategy to reduce mortality is the use of low-tidal-volume ventilation,2 and, in fact, the use of injurious high-tidal-volume ventilation has been shown to upregulate both vWF and P-selectin expression.47 Using lung-protective positive pressure ventilation, however, is associated with decreased ADP- and collagen-mediated platelet aggregation.50 Nitric oxide, another therapy often used in ARDS/ALI despite limited data to support its routine use, has been shown to decrease platelet aggregation by reducing fibrinogen binding to the GP IIb/IIIa receptor.51 As well, the controversial use of corticosteroids in ARDS52 has been associated with decreased platelet activation and activity in some experimental models.53, 54 Although not suggesting that these therapies improved lung injury through their platelet-modifying effects alone, these data do support a biologic plausibility that should be considered when studying the impact of dysregulated platelet activity on patient outcomes (Fig 2 ).
Figure 2.
A, Influence of platelet and platelet-neutrophil interactions on the pathophysiology of sepsis and, B, ALI. In sepsis, platelets may be stimulated by tissue injury, hypoxia, cytokines, LPS, and endotoxemia, leading to microvascular obstruction, cellular necrosis/apoptosis, and an enhanced leukocyte response. In ALI, platelets and platelet-neutrophil complexes can similarly be found within the pulmonary vasculature, airways, interstitial, and alveolar compartments. ALI = acute lung injury; LPS = lipopolysaccharide.
Studies of Antiplatelet Strategies in Critical Illness
Although there is growing evidence to suggest a pathologic role for platelets in a number of inflammatory conditions, including sepsis and ALI, there are far fewer data to support targeted antiplatelet strategies as therapeutic options for managing afflicted patients. Such a strategy, however, is not without historical merit. For years now, the cardiovascular community has been espousing the benefits of antiplatelet agents for reducing inflammation in both acute and chronic atherosclerotic diseases. With this as a platform for novel investigation, there is now burgeoning interest in platelets as therapeutic targets for patients with critical illness.
Antiplatelet Agents and Inflammation
Aspirin
Within a subset of patients enrolled in the Physicians' Health Study, a randomized trial of aspirin vs β-carotene for the primary prevention of cardiovascular disease, the use of aspirin was associated with a significant reduction in the risk of myocardial infarction predominantly among patients with the highest C-reactive protein (CRP) values.55 This finding was among the first pieces of clinical evidence to suggest a possible antiinflammatory role for commonly used antiplatelet therapies. Aspirin also has been shown to have inhibitory effects on the activity of nuclear factor κβ, a transcription factor that is required for the expression of genes encoding a variety of inflammatory molecules.56 In a mouse model of atherosclerosis, the normally enhanced nuclear factor κβ activity was substantially reduced in animals who were treated with aspirin.57
Among healthy volunteers, however, there is little compelling evidence to support an antiinflammatory effect of aspirin,58 and studies among patients with both acute and chronic inflammatory conditions have yielded mixed results. In patients with chronic, stable angina, for instance, aspirin significantly lowered CRP and inflammatory cytokine levels.59 Conversely, in other patients with chronic ischemic heart disease, recent myocardial infarction, and acute coronary syndromes, aspirin failed to reliably reduce CRP.60, 61 In peripheral arterial disease as well, markers of platelet-mediated inflammation were not significantly decreased with aspirin therapy.62 There is also conflicting evidence regarding the potential of aspirin to mitigate pathologic inflammatory interactions between platelets and leukocytes.62, 63
Clopidogrel
Clopidogrel (Plavix), an irreversible antagonist of the G-protein-coupled platelet ADP receptor (P2Y12), has been shown to have a greater influence on cardiovascular risk reduction among patients at heightened inflammatory states. In a post hoc analysis of the Clopidogrel for the Reduction of Events during Observation trial, a study of prolonged clopidogrel therapy following percutaneous coronary intervention (PCI), there was a significant (44%) relative risk reduction in the combined end point of death, myocardial infarction, or stroke at 12 months for those patients in the highest tertile of high-sensitivity CRP levels.64 Likewise, shorter-term cardiovascular events were reduced following PCI in those patients pretreated with clopidogrel who had elevated baseline CRP values.65
Unlike aspirin therapy, however, clopidogrel administration has been shown to reduce the secretion of adhesive ligands and to block the formation of platelet-leukocyte conjugates, with resulting decreases in leukocyte activity. In patients treated with PCI, clopidogrel reduced ADP- and thrombin receptor-activating peptide-induced expression of the platelet P-selectin.66 Evangelista and colleagues67 showed that clopidogrel use had a potent inhibitory effect on platelet-dependent production of reactive oxygen species in neutrophils, as well as monocyte expression of tissue factor. Klinkhardt et al68 found that more-prolonged clopidogrel pretreatment could significantly reduce the volume of both platelet-monocyte and platelet-neutrophil aggregates following ADP stimulation, effects that correlated directly with substantial reductions in P-selectin expression. Similarly, clopidogrel therapy has been shown to reduce platelet-neutrophil and platelet-monocyte conjugates in patients across a spectrum of vascular diseases.62, 69
Other Antiplatelet Agents
Conflicting data have come from studies of the GP IIb/IIIa receptor antagonists in inflammatory conditions. Modest levels of receptor blockade actually have been associated with increases in platelet-mediated proinflammatory effects, along with enhanced expression of P-selectin,70 and increased release of soluble CD40 ligand.71 Furthermore, although the synthetic small-molecule GP IIb/IIIa inhibitor eptifibatide (Integrilin) significantly reduced levels of CRP at 24 h compared with placebo in the Enhanced Suppression of the Platelet IIb/IIIa Receptor with Integrilin Therapy trial, levels subsequently increased beyond baseline 30 h following infusion.72 On the other hand, abciximab (ReoPro), a chimeric Fab fragment of a monoclonal antibody with high affinity for the GP IIb/IIIa receptor, was found to suppress the usual rise in levels of circulating inflammatory markers following percutaneous transluminal coronary angioplasty.73 Finally, among small populations of patients treated with tirofiban (Aggrastat), data have been largely inconclusive.74, 75
Antiplatelet Agents in Critical Illness
In general, there has been limited study of antiplatelet therapeutic strategies in critical care populations. Lösche and colleagues76 found that antiplatelet drugs were associated with a slight reduction in mortality among patients with nonsurgical critical illness and a slightly increased mortality rate among those requiring surgery. When adjusted for differences in baseline characteristics and disease severity, however, antiplatelet therapy use was associated with substantially reduced mortality in both groups.
In a single-center study of hospitalized patients with community-acquired pneumonia, 20% of whom had received antiplatelet agents for the secondary prevention of cardiovascular disease, Winning et al77 found antiplatelet drug use to be associated with a reduction in length of stay and the need for ICU care. Later, in a retrospective study conducted in a mixed medical-surgical ICU, these same investigators found that preexistent treatment with antiplatelet agents reduced the odds ratio for mortality by nearly fivefold.78 Even in patients with signs of active bleeding, including life-threatening intracranial hemorrhage and transfusion-dependent anemia, there still was a strong association between antiplatelet drugs and improved outcomes. This association was most robust among those patients with the greatest disease severity.78 Although limited by the retrospective nature of these analyses and modest design challenges, these data still speak to the potential role of platelets as therapeutic targets among heterogeneous critical care populations.
Antiplatelet Agents in Infection and Sepsis
The impact of antiplatelet agents on circulating platelets and markers of inflammation during systemic infection has yet to be clarified, despite increasing study in both animal and human models. In early studies of antiplatelet drugs in endotoxemic pigs, pretreatment was found to have minimal effects on the pathogenesis of Escherichia coli-induced shock. Despite platelet targeting, clinical sepsis ensued in these animals, with concomitant decreases in levels of platelets along with activation of both the coagulation and fibrinolytic systems.79 Clopidogrel also had no demonstrable effect on hemostatic or inflammatory responses of pigs infused with E coli endotoxin.80 However, when specifically using clopidogrel in other animal models of sepsis, several investigators have reported that not only is platelet activation reduced but also clinical thrombocytopenia is attenuated, clot formation is decreased, cytokine upregulation is mitigated, and neutrophil recruitment may be minimized.68, 81
Antiplatelet Agents in ALI and ARDS
Even fewer data exist regarding antiplatelet strategies in critically ill patients with lung injury. Targeted platelet depletion or disruption of platelet-neutrophil interactions in murine models of ARDS resulted in reduced neutrophil migration and permeability, improved alveolar gas exchange, and increased survival.41 Aspirin use in an experimental transfusion-related ALI model did not prevent neutrophil sequestration; however, the neutrophils that infiltrated the pulmonary parenchyma were rendered incapable of causing lung toxicity.82 Further study clearly is needed to build on these preliminary data in order to clarify the intriguing potential of therapeutic platelet targeting in lung injury populations.
Conclusions and Future Directions
The role of platelets in the pathophysiology of critical illness continues to be elucidated, particularly with respect to lung injury where our understanding is woefully incomplete. No longer are these anucleate cells considered merely executors of the thrombotic process but, instead, are clearly key contributors to the host immune response. Although initially adaptive, unregulated platelet activation during sepsis, ALI, and ARDS leads to organ hypoperfusion, pathologic tissue injury, and poor patient outcomes. Whether modulation of this platelet response will improve the high morbidity and mortality associated with these diseases remains to be seen. Small, nonrandomized clinical studies of antiplatelet strategies have yielded mixed results but should prompt additional investigation.
Following on the heels of these early discoveries, future study may further capitalize on the relationship between platelets and platelet receptors in human critical illness. Building on circumstantial evidence from trials of contemporary antiplatelet therapies, some investigators have begun to focus greater attention on the role of adenosine and its myriad of receptors on the pathobiology of inflammation. During conditions of high metabolic stress, as seen in acute tissue injury and sepsis for instance, extracellular adenosine concentrations often are markedly increased.83 Adenosine is believed to play an important role in preventing neutrophil infiltration into vulnerable tissue,84 and a growing body of data suggests a possible role for adenosine in modulating adaptive immune response to critical illness.
Likewise, increased attention has and should be directed toward the influence of platelet polyphosphates as both proinflammatory and procoagulant mediators during acute illness. Recent investigation has shown that polyphosphates help to trigger fibrin formation and facilitate capillary leakage, which is commonplace among ICU patients. The polyphosphates also seem to play a role in preserving cellular integrity and modulating neutrophil response during inflammation.85
With advances in high-throughput experimental technologies, researchers are now beginning to characterize the full complement of transcripts and functionally relevant proteins that contribute to the versatility and complexity of platelets in human disease.86 A more-integrated understanding of platelet biology undoubtedly will allow for improved clarification of the adaptive and maladaptive influences of platelets in critical illness. The potential for identifying molecular signatures of pathologic platelet activity also could provide an ambitious platform for studying patient variation in disease response, establishing novel risk stratification tools, and developing future therapeutic targets.
As critical care investigators and practitioners, we only recently have begun to understand the true versatility of the human platelet. A more concerted, multidisciplinary effort to unravel the mysteries of the platelet during critical illness clearly will be important if we hope to minimize the devastating impact of sepsis, ALI, and ARDS on an ever-expanding patient population.
Acknowledgments
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Dr Katz has received research support from the Medicines Company. Dr Becker has received research support from AstraZeneca, Bayer Pharmaceuticals, Regado Biosciences Inc, and Schering-Plough Research Institute and has been an advisory board member for Merck, Eli Lilly, and Daiichi. Dr Kolappa has reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Other contributions: We thank Brian Jensen, MD, for his critical review and editorial assistance with this manuscript.
Footnotes
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (http://www.chestpubs.org/site/misc/reprints.xhtml).
References
- 1.Frutos-Vivar F, Nin N, Esteban A. Epidemiology of acute lung injury and acute respiratory distress syndrome. Curr Opin Crit Care. 2004;10(1):1–6. doi: 10.1097/00075198-200402000-00001. [DOI] [PubMed] [Google Scholar]
- 2.The Acute Respiratory Distress Syndrome Network Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 3.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 4.Wheeler AP, Bernard GR. Treating patients with severe sepsis. N Engl J Med. 1999;340(3):207–214. doi: 10.1056/NEJM199901213400307. [DOI] [PubMed] [Google Scholar]
- 5.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Kirschenbaum LA, Aziz M, Astiz ME, Saha DC, Rackow EC. Influence of rheologic changes and platelet-neutrophil interactions on cell filtration in sepsis. Am J Respir Crit Care Med. 2000;161(5):1602–1607. doi: 10.1164/ajrccm.161.5.9902105. [DOI] [PubMed] [Google Scholar]
- 7.Levi M. Platelets in sepsis. Hematology. 2005;10(suppl 1):129–131. doi: 10.1080/10245330512331390177. [DOI] [PubMed] [Google Scholar]
- 8.Bozza FA, Shah AM, Weyrich AS, Zimmerman GA. Amicus or adversary: platelets in lung biology, acute injury, and inflammation. Am J Respir Cell Mol Biol. 2009;40(2):123–134. doi: 10.1165/rcmb.2008-0241TR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zarbock A, Polanowska-Grabowska RK, Ley K. Platelet-neutrophil-interactions: linking hemostasis and inflammation. Blood Rev. 2007;21(2):99–111. doi: 10.1016/j.blre.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Ley K. The role of selectins in inflammation and disease. Trends Mol Med. 2003;9(6):263–268. doi: 10.1016/s1471-4914(03)00071-6. [DOI] [PubMed] [Google Scholar]
- 11.Rendu F, Brohard-Bohn B. The platelet release reaction: granules' constituents, secretion and functions. Platelets. 2001;12(5):261–273. doi: 10.1080/09537100120068170. [DOI] [PubMed] [Google Scholar]
- 12.Neumann FJ, Zohlnhöfer D, Fakhoury L, Ott I, Gawaz M, Schömig A. Effect of glycoprotein IIb/IIIa receptor blockade on platelet-leukocyte interaction and surface expression of the leukocyte integrin Mac-1 in acute myocardial infarction. J Am Coll Cardiol. 1999;34(5):1420–1426. doi: 10.1016/s0735-1097(99)00350-2. [DOI] [PubMed] [Google Scholar]
- 13.Smyth SS, McEver RP, Weyrich AS, 2009 Platelet Colloquium Participants Platelet functions beyond hemostasis. J Thromb Haemost. 2009;7(11):1759–1766. doi: 10.1111/j.1538-7836.2009.03586.x. [DOI] [PubMed] [Google Scholar]
- 14.Liu Y, Shaw SK, Ma S, Yang L, Luscinskas FW, Parkos CA. Regulation of leukocyte transmigration: cell surface interactions and signaling events. J Immunol. 2004;172(1):7–13. doi: 10.4049/jimmunol.172.1.7. [DOI] [PubMed] [Google Scholar]
- 15.Singbartl K, Forlow SB, Ley K. Platelet, but not endothelial, P-selectin is critical for neutrophil-mediated acute postischemic renal failure. FASEB J. 2001;15(13):2337–2344. doi: 10.1096/fj.01-0199com. [DOI] [PubMed] [Google Scholar]
- 16.Yang J, Furie BC, Furie B. The biology of P-selectin glycoprotein ligand-1: its role as a selectin counterreceptor in leukocyte-endothelial and leukocyte-platelet interaction. Thromb Haemost. 1999;81(1):1–7. [PubMed] [Google Scholar]
- 17.Hammer DA, Apte SM. Simulation of cell rolling and adhesion on surfaces in shear flow: general results and analysis of selectin-mediated neutrophil adhesion. Biophys J. 1992;63(1):35–57. doi: 10.1016/S0006-3495(92)81577-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ley K, Laudanna C, Cybulsky MI, Nourshargh S. Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nat Rev Immunol. 2007;7(9):678–689. doi: 10.1038/nri2156. [DOI] [PubMed] [Google Scholar]
- 19.Baughman RP, Lower EE, Flessa HC, Tollerud DJ. Thrombocytopenia in the intensive care unit. Chest. 1993;104(4):1243–1247. doi: 10.1378/chest.104.4.1243. [DOI] [PubMed] [Google Scholar]
- 20.Vanderschueren S, De Weerdt A, Malbrain M. Thrombocytopenia and prognosis in intensive care. Crit Care Med. 2000;28(6):1871–1876. doi: 10.1097/00003246-200006000-00031. [DOI] [PubMed] [Google Scholar]
- 21.Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23(10):1638–1652. doi: 10.1097/00003246-199510000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Mavrommatis AC, Theodoridis T, Orfanidou A, Roussos C, Christopoulou-Kokkinou V, Zakynthinos S. Coagulation system and platelets are fully activated in uncomplicated sepsis. Crit Care Med. 2000;28(2):451–457. doi: 10.1097/00003246-200002000-00027. [DOI] [PubMed] [Google Scholar]
- 23.Fein AM, Lippmann M, Holtzman H, Eliraz A, Goldberg SK. The risk factors, incidence, and prognosis of ARDS following septicemia. Chest. 1983;83(1):40–42. doi: 10.1378/chest.83.1.40. [DOI] [PubMed] [Google Scholar]
- 24.Fowler AA, Hamman RF, Zerbe GO, Benson KN, Hyers TM. Adult respiratory distress syndrome. Prognosis after onset. Am Rev Respir Dis. 1985;132(3):472–478. doi: 10.1164/arrd.1985.132.3.472. [DOI] [PubMed] [Google Scholar]
- 25.Bone RC, Balk R, Slotman G. Adult respiratory distress syndrome. Sequence and importance of development of multiple organ failure. The Prostaglandin E1 Study Group. Chest. 1992;101(2):320–326. doi: 10.1378/chest.101.2.320. [DOI] [PubMed] [Google Scholar]
- 26.Peiris JS, Yuen KY, Osterhaus AD, Stöhr K. The severe acute respiratory syndrome. N Engl J Med. 2003;349(25):2431–2441. doi: 10.1056/NEJMra032498. [DOI] [PubMed] [Google Scholar]
- 27.Whitworth NH, Barradas MA, Mikhailidis DP, Dandona P. An investigation into the effects of bacterial lipopolysaccharide on human platelets. Eur J Haematol. 1989;43(2):112–119. doi: 10.1111/j.1600-0609.1989.tb00266.x. [DOI] [PubMed] [Google Scholar]
- 28.Saba HI, Saba SR, Morelli G, Hartmann RC. Endotoxin-mediated inhibition of human platelet aggregation. Thromb Res. 1984;34(1):19–33. doi: 10.1016/0049-3848(84)90103-8. [DOI] [PubMed] [Google Scholar]
- 29.Gawaz M, Dickfeld T, Bogner C, Fateh-Moghadam S, Neumann FJ. Platelet function in septic multiple organ dysfunction syndrome. Intensive Care Med. 1997;23(4):379–385. doi: 10.1007/s001340050344. [DOI] [PubMed] [Google Scholar]
- 30.Ogura H, Kawasaki T, Tanaka H. Activated platelets enhance microparticle formation and platelet-leukocyte interaction in severe trauma and sepsis. J Trauma. 2001;50(5):801–809. doi: 10.1097/00005373-200105000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Yaguchi A, Pradier O, Lobo F. Platelet aggregation is impaired at the level of cyclo-oxygenase and thromboxane synthetase in severe sepsis. Intensive Care Med. 2001;27(suppl 2):S166. [Google Scholar]
- 32.Boldt J, Menges T, Wollbrück M, Sonneborn S, Hempelmann G. Platelet function in critically ill patients. Chest. 1994;106(3):899–903. doi: 10.1378/chest.106.3.899. [DOI] [PubMed] [Google Scholar]
- 33.Andonegui G, Kerfoot SM, McNagny K, Ebbert KV, Patel KD, Kubes P. Platelets express functional Toll-like receptor-4. Blood. 2005;106(7):2417–2423. doi: 10.1182/blood-2005-03-0916. [DOI] [PubMed] [Google Scholar]
- 34.Nguyen TC, Liu A, Liu L. Acquired ADAMTS-13 deficiency in pediatric patients with severe sepsis. Haematologica. 2007;92(1):121–124. doi: 10.3324/haematol.10262. [DOI] [PubMed] [Google Scholar]
- 35.Bockmeyer CL, Claus RA, Budde U. Inflammation-associated ADAMTS13 deficiency promotes formation of ultra-large von Willebrand factor. Haematologica. 2008;93(1):137–140. doi: 10.3324/haematol.11677. [DOI] [PubMed] [Google Scholar]
- 36.Azevedo LCP, Janiszewski M, Pontieri V. Platelet-derived exosomes from septic shock patients induce myocardial dysfunction. Crit Care. 2007;11(6):R120. doi: 10.1186/cc6176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kuckleburg CJ, Tiwari R, Czuprynski CJ. Endothelial cell apoptosis induced by bacteria-activated platelets requires caspase-8 and −9 and generation of reactive oxygen species. Thromb Haemost. 2008;99(2):363–372. doi: 10.1160/TH07-07-0474. [DOI] [PubMed] [Google Scholar]
- 38.Brown KA, Brain SD, Pearson JD, Edgeworth JD, Lewis SM, Treacher DF. Neutrophils in development of multiple organ failure in sepsis. Lancet. 2006;368(9530):157–169. doi: 10.1016/S0140-6736(06)69005-3. [DOI] [PubMed] [Google Scholar]
- 39.Asaduzzaman M, Lavasani S, Rahman M. Platelets support pulmonary recruitment of neutrophils in abdominal sepsis. Crit Care Med. 2009;37(4):1389–1396. doi: 10.1097/CCM.0b013e31819ceb71. [DOI] [PubMed] [Google Scholar]
- 40.Laschke MW, Dold S, Menger MD, Jeppsson B, Thorlacius H. Platelet-dependent accumulation of leukocytes in sinusoids mediates hepatocellular damage in bile duct ligation-induced cholestasis. Br J Pharmacol. 2008;153(1):148–156. doi: 10.1038/sj.bjp.0707578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zarbock A, Singbartl K, Ley K. Complete reversal of acid-induced acute lung injury by blocking of platelet-neutrophil aggregation. J Clin Invest. 2006;116(12):3211–3219. doi: 10.1172/JCI29499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kirschenbaum LA, McKevitt D, Rullan M, Reisbeck B, Fujii T, Astiz ME. Importance of platelets and fibrinogen in neutrophil-endothelial cell interactions in septic shock. Crit Care Med. 2004;32(9):1904–1909. doi: 10.1097/01.ccm.0000139918.80602.57. [DOI] [PubMed] [Google Scholar]
- 43.Peters MJ, Dixon G, Kotowicz KT, Hatch DJ, Heyderman RS, Klein NJ. Circulating platelet-neutrophil complexes represent a subpopulation of activated neutrophils primed for adhesion, phagocytosis and intracellular killing. Br J Haematol. 1999;106(2):391–399. doi: 10.1046/j.1365-2141.1999.01553.x. [DOI] [PubMed] [Google Scholar]
- 44.Freishtat RJ, Natale J, Benton AS. Sepsis alters the megakaryocyte-platelet transcriptional axis resulting in granzyme B-mediated lymphotoxicity. Am J Respir Crit Care Med. 2009;179(6):467–473. doi: 10.1164/rccm.200807-1085OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bone RC, Francis PB, Pierce AK. Intravascular coagulation associated with the adult respiratory distress syndrome. Am J Med. 1976;61(5):585–589. doi: 10.1016/0002-9343(76)90135-2. [DOI] [PubMed] [Google Scholar]
- 46.Bachofen M, Weibel ER. Structural alterations of lung parenchyma in the adult respiratory distress syndrome. Clin Chest Med. 1982;3(1):35–56. [PubMed] [Google Scholar]
- 47.Yiming MT, Lederer DJ, Sun L, Huertas A, Issekutz AC, Bhattacharya S. Platelets enhance endothelial adhesiveness in high tidal volume ventilation. Am J Respir Cell Mol Biol. 2008;39(5):569–575. doi: 10.1165/rcmb.2007-0332OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Idell S, Maunder R, Fein AM. Platelet-specific alpha-granule proteins and thrombospondin in bronchoalveolar lavage in the adult respiratory distress syndrome. Chest. 1989;96(5):1125–1132. doi: 10.1378/chest.96.5.1125. [DOI] [PubMed] [Google Scholar]
- 49.Carvalho AC, Quinn DA, DeMarinis SM, Beitz JG, Zapol WM. Platelet function in acute respiratory failure. Am J Hematol. 1987;25(4):377–388. doi: 10.1002/ajh.2830250404. [DOI] [PubMed] [Google Scholar]
- 50.von Känel R, Dimsdale JE. Hemostatic alterations in patients with obstructive sleep apnea and the implications for cardiovascular disease. Chest. 2003;124(5):1956–1967. doi: 10.1378/chest.124.5.1956. [DOI] [PubMed] [Google Scholar]
- 51.Samama CM, Diaby M, Fellahi JL. Inhibition of platelet aggregation by inhaled nitric oxide in patients with acute respiratory distress syndrome. Anesthesiology. 1995;83(1):56–65. doi: 10.1097/00000542-199507000-00007. [DOI] [PubMed] [Google Scholar]
- 52.Peter JV, John P, Graham PL, Moran JL, George IA, Bersten A. Corticosteroids in the prevention and treatment of acute respiratory distress syndrome (ARDS) in adults: meta-analysis. BMJ. 2008;336(7651):1006–1009. doi: 10.1136/bmj.39537.939039.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brigham KL, Bowers RE, McKeen CR. Methylprednisolone prevention of increased lung vascular permeability following endotoxemia in sheep. J Clin Invest. 1981;67(4):1103–1110. doi: 10.1172/JCI110123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Han SJ, Choi JH, Ko HM. Glucocorticoids prevent NF-kappaB activation by inhibiting the early release of platelet-activating factor in response to lipopolysaccharide. Eur J Immunol. 1999;29(4):1334–1341. doi: 10.1002/(SICI)1521-4141(199904)29:04<1334::AID-IMMU1334>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 55.Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336(14):973–979. doi: 10.1056/NEJM199704033361401. [DOI] [PubMed] [Google Scholar]
- 56.Weyrich AS, McIntyre TM, McEver RP, Prescott SM, Zimmerman GA. Monocyte tethering by P-selectin regulates monocyte chemotactic protein-1 and tumor necrosis factor-alpha secretion. Signal integration and NF-kappa B translocation. J Clin Invest. 1995;95(5):2297–2303. doi: 10.1172/JCI117921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cyrus T, Sung S, Zhao L, Funk CD, Tang S, Praticò D. Effect of low-dose aspirin on vascular inflammation, plaque stability, and atherogenesis in low-density lipoprotein receptor-deficient mice. Circulation. 2002;106(10):1282–1287. doi: 10.1161/01.cir.0000027816.54430.96. [DOI] [PubMed] [Google Scholar]
- 58.Azar RR, Klayme S, Germanos M. Effects of aspirin (325 mg/day) on serum high-sensitivity C-reactive protein, cytokines, and adhesion molecules in healthy volunteers. Am J Cardiol. 2003;92(2):236–239. doi: 10.1016/s0002-9149(03)00549-6. [DOI] [PubMed] [Google Scholar]
- 59.Ikonomidis I, Andreotti F, Economou E, Stefanadis C, Toutouzas P, Nihoyannopoulos P. Increased proinflammatory cytokines in patients with chronic stable angina and their reduction by aspirin. Circulation. 1999;100(8):793–798. doi: 10.1161/01.cir.100.8.793. [DOI] [PubMed] [Google Scholar]
- 60.Takeda T, Hoshida S, Nishino M, Tanouchi J, Otsu K, Hori M. Relationship between effects of statins, aspirin and angiotensin II modulators on high-sensitive C-reactive protein levels. Atherosclerosis. 2003;169(1):155–158. doi: 10.1016/s0021-9150(03)00158-8. [DOI] [PubMed] [Google Scholar]
- 61.Monakier D, Mates M, Klutstein MW. Rofecoxib, a COX-2 inhibitor, lowers C-reactive protein and interleukin-6 levels in patients with acute coronary syndromes. Chest. 2004;125(5):1610–1615. doi: 10.1378/chest.125.5.1610. [DOI] [PubMed] [Google Scholar]
- 62.Klinkhardt U, Bauersachs R, Adams J, Graff J, Lindhoff-Last E, Harder S. Clopidogrel but not aspirin reduces P-selectin expression and formation of platelet-leukocyte aggregates in patients with atherosclerotic vascular disease. Clin Pharmacol Ther. 2003;73(3):232–241. doi: 10.1067/mcp.2003.13. [DOI] [PubMed] [Google Scholar]
- 63.Li N, Hu H, Hjemdahl P. Aspirin treatment does not attenuate platelet or leukocyte activation as monitored by whole blood flow cytometry. Thromb Res. 2003;111(3):165–170. doi: 10.1016/j.thromres.2003.08.026. [DOI] [PubMed] [Google Scholar]
- 64.Steinhubl SR, Berger PB, Van Lente F. Levels of hs-CRP prior to PCI predict long-term risk and the benefit of clopidogrel therapy: a CREDO substudy. Circulation. 2004;110(suppl 1):III-382. [Google Scholar]
- 65.Chew DP, Bhatt DL, Robbins MA. Effect of clopidogrel added to aspirin before percutaneous coronary intervention on the risk associated with C-reactive protein. Am J Cardiol. 2001;88(6):672–674. doi: 10.1016/s0002-9149(01)01813-6. [DOI] [PubMed] [Google Scholar]
- 66.Quinn MJ, Bhatt DL, Zidar F. Effect of clopidogrel pretreatment on inflammatory marker expression in patients undergoing percutaneous coronary intervention. Am J Cardiol. 2004;93(6):679–684. doi: 10.1016/j.amjcard.2003.11.048. [DOI] [PubMed] [Google Scholar]
- 67.Evangelista V, Manarini S, Dell'Elba G. Clopidogrel inhibits platelet-leukocyte adhesion and platelet-dependent leukocyte activation. Thromb Haemost. 2005;94(3):568–577. [PubMed] [Google Scholar]
- 68.Klinkhardt U, Graff J, Harder S. Clopidogrel, but not abciximab, reduces platelet leukocyte conjugates and P-selectin expression in a human ex vivo in vitro model. Clin Pharmacol Ther. 2002;71(3):176–185. doi: 10.1067/mcp.2002.122018. [DOI] [PubMed] [Google Scholar]
- 69.Xiao Z, Théroux P. Clopidogrel inhibits platelet-leukocyte interactions and thrombin receptor agonist peptide-induced platelet activation in patients with an acute coronary syndrome. J Am Coll Cardiol. 2004;43(11):1982–1988. doi: 10.1016/j.jacc.2003.10.071. [DOI] [PubMed] [Google Scholar]
- 70.Cox D, Smith R, Quinn MJ, Theroux P, Crean P, Fitzgerald DJ. Evidence of platelet activation during treatment with a GPIIb/IIIa antagonist in patients presenting with acute coronary syndromes. J Am Coll Cardiol. 2000;36(5):1514–1519. doi: 10.1016/s0735-1097(00)00919-0. [DOI] [PubMed] [Google Scholar]
- 71.Nannizzi-Alaimo L, Alves VL, Phillips DR. Inhibitory effects of glycoprotein IIb/IIIa antagonists and aspirin on the release of soluble CD40 ligand during platelet stimulation. Circulation. 2003;107(8):1123–1128. doi: 10.1161/01.cir.0000053559.46158.ad. [DOI] [PubMed] [Google Scholar]
- 72.Merino A, Segura I, Vidal B. Eptifibatide blocks C-reactive protein increase after coronary angioplasty. J Am Coll Cardiol. 2003;41(suppl 1):233A. [Google Scholar]
- 73.Lincoff AM, Kereiakes DJ, Mascelli MA. Abciximab suppresses the rise in levels of circulating inflammatory markers after percutaneous coronary revascularization. Circulation. 2001;104(2):163–167. doi: 10.1161/01.cir.104.2.163. [DOI] [PubMed] [Google Scholar]
- 74.Ercan E, Tengiz I, Duman C, Onbasili OA, Baris N. Effect of tirofiban on C-reactive protein in non-ST-elevation myocardial infarction. Am Heart J. 2004;147(1):54–57. doi: 10.1016/s0002-8703(03)00447-2. [DOI] [PubMed] [Google Scholar]
- 75.Akbulut M, Ozbay Y, Gundogdu O. Effects of tirofiban on acute systemic inflammatory response in elective percutaneous coronary interventions. Curr Med Res Opin. 2004;20(11):1759–1767. doi: 10.1185/030079904X4400. [DOI] [PubMed] [Google Scholar]
- 76.Lösche W, Neumann J, Winning J, Claus RA, Reinhart K, Bauer M. Antiplatelet drugs reduce mortality in surgical and non-surgical patients. Infection. 2007;35(suppl 2):14. [Google Scholar]
- 77.Winning J, Reichel J, Eisenhut Y. Anti-platelet drugs and outcome in severe infection: clinical impact and underlying mechanisms. Platelets. 2009;20(1):50–57. doi: 10.1080/09537100802503368. [DOI] [PubMed] [Google Scholar]
- 78.Winning J, Neumann J, Kohl M. Antiplatelet drugs and outcome in mixed admissions to an intensive care unit. Crit Care Med. 2010;38(1):32–37. doi: 10.1097/CCM.0b013e3181b4275c. [DOI] [PubMed] [Google Scholar]
- 79.Svartholm E, Bergqvist D, Haglund U, Ljungberg J, Hedner U. Coagulation and fibrinolytic reactions in experimental porcine septic shock: pretreatment with different antiplatelet factors. Circ Shock. 1987;22(4):291–301. [PubMed] [Google Scholar]
- 80.Lipcsey M, Larsson A, Olovsson M, Sjölin J, Eriksson MB. Early endotoxin-mediated haemostatic and inflammatory responses in the clopidogrel-treated pig. Platelets. 2005;16(7):408–414. doi: 10.1080/09537100500163168. [DOI] [PubMed] [Google Scholar]
- 81.Seidel M, Winning J, Claus RA, Bauer M, Lösche W. Beneficial effect of clopidogrel in a mouse model of polymicrobial sepsis. J Thromb Haemost. 2009;7(6):1030–1032. doi: 10.1111/j.1538-7836.2009.03352.x. [DOI] [PubMed] [Google Scholar]
- 82.Looney MR, Nguyen JX, Hu Y, Van Ziffle JA, Lowell CA, Matthay MA. Platelet depletion and aspirin treatment protect mice in a two-event model of transfusion-related acute lung injury. J Clin Invest. 2009;119(11):3450–3461. doi: 10.1172/JCI38432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Martin C, Leone M, Viviand X, Ayem ML, Guieu R. High adenosine plasma concentration as a prognostic index for outcome in patients with septic shock. Crit Care Med. 2000;28(9):3198–3202. doi: 10.1097/00003246-200009000-00014. [DOI] [PubMed] [Google Scholar]
- 84.Kumar V, Sharma A. Adenosine: an endogenous modulator of innate immune system with therapeutic potential. Eur J Pharmacol. 2009;616(1-3):7–15. doi: 10.1016/j.ejphar.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 85.Müller F, Mutch NJ, Schenk WA. Platelet polyphosphates are proinflammatory and procoagulant mediators in vivo. Cell. 2009;139(6):1143–1156. doi: 10.1016/j.cell.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Macaulay IC, Carr P, Gusnanto A, Ouwehand WH, Fitzgerald D, Watkins NA. Platelet genomics and proteomics in human health and disease. J Clin Invest. 2005;115(12):3370–3377. doi: 10.1172/JCI26885. [DOI] [PMC free article] [PubMed] [Google Scholar]