Abstract
Sore throat is a common medical complaint seen by the emergency practitioner, internist, pediatrician, and otolaryngologist. The differential for sore throat is vast. However, with a directed history this can often be narrowed down to 2 to 3 possible diagnoses. By paying particular attention to the associated symptoms and duration of symptoms, common self-limited etiologies like viral pharyngitis and nonstreptococcal tonsillitis can be distinguished from those that require more investigation, such as supraglottitis and tonsillar cancer. A sore throat is most commonly caused by an infectious, inflammatory, or neoplastic etiologic factor.
Keywords: Sore throat, Pharyngitis, Tonsillitis, Laryngitis, URI
Impact
The National Health Care Survey in 2001 to 2002 reported more than 21 million outpatient and emergency room visits with complaints relating to the throat, and acute pharyngitis was diagnosed in nearly 12 million patients.1 Although the underlying cause is often benign and the course is typically mild, the high annual incidence translates into a tremendous impact on public health from decreased productivity and overutilization of antibiotics. On the other hand, practitioners can make a significant public health contribution with small changes to their everyday practices. For instance, the addition of routine rapid streptococcal antigen testing on patients with presumptive pharyngitis reduced antibiotic prescriptions by nearly 50% in a pediatric emergency department.2 Patient education and early identification of highly transmissible diseases, such as the 2009 H1N1 influenza virus, help to control the spread of disease and overall public health burden. Even seemingly basic symptomatic relief can speed the return to work and school and improve overall productivity.
Anatomy
The throat anatomically consists of the pharynx and the larynx. It begins superiorly at the level of the skull base and nasopharynx, extending down to the esophageal inlet and most proximal aspect of the trachea. It is bounded anteriorly by the nasal cavity and oral cavity. The level of the choanae divides the nasal cavity and nasopharynx. A vertical line drawn between the junction of the hard and soft palate and the circumvallate papillae of the tongue divides the oral cavity and oropharynx. Disease processes limited to the oral cavity do not typically elicit a complaint of sore throat, and are not discussed in this article.
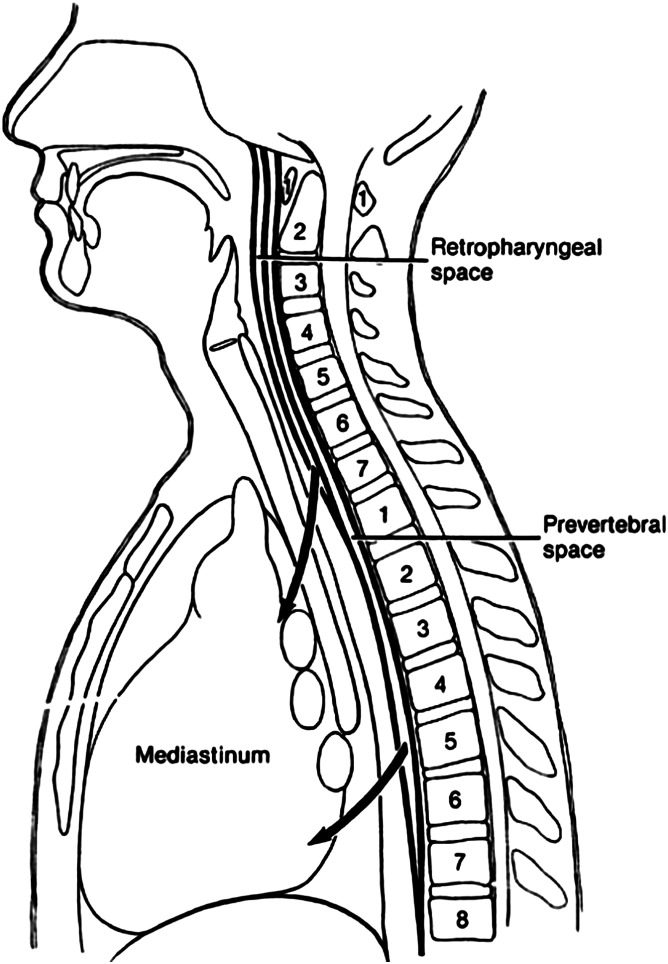
The larynx consists of the supraglottis, the glottis, and the subglottis. The supraglottis is made up of structures above the true vocal folds: epiglottis, arytenoids, aryepiglottic folds, false vocal folds, and ventricles (Fig. 1 ). The glottis extends from the horizontal apex of the ventricle down to 1 cm below the level of the true vocal folds. The subglottis begins 1 cm below the level of the true vocal folds.
Fig. 1.
Fiberoptic view of laryngeal anatomy. A, arytenoid; BOT, base of tongue; E, esophageal inlet; EP, epiglottis; FVC, false vocal cord; IA, interarytenoid mucosa; PC, postcricoid mucosa; PP, posterior pharyngeal wall; PS, pyriform sinus; TVC, true vocal cord.
The pharynx consists of the nasopharynx, the oropharynx, and the hypopharynx. The hypopharyngeal structures include the posterior pharyngeal wall, the pyriform sinuses that lie on either side of the esophageal inlet, and the postcricoid area that is the party wall between the larynx and the pharynx.
Sensory innervation to the throat is provided by the glossopharyngeal and vagus nerves. These nerves also supply sensation to the ear; hence, referred otalgia can be seen when the primary disease process involves the throat. Blood is supplied to this region by the ascending pharyngeal arteries and branches of the superior and inferior thyroid arteries.
Clinical history
Sore throat can be the presenting symptom of a myriad of different diagnoses. In most cases it is attributable to a benign viral process. A thorough clinical history will often help to differentiate these self-limited cases from those needing more investigation and possible referral to a specialist.
Because the complaint sore throat may mean irritation, scratchiness, burning sensation, or frank pain, the patient should be asked to elaborate on the description. In addition, from a patient's perspective, throat may refer to the entire pharynx and larynx, the soft tissues of the neck, or a single localized area. Having the patient indicate the epicenter of the discomfort with one finger can often be revealing. Discomfort that is located laterally and around the level of the hyoid corresponds to vallecular and tonsillar processes. Soreness or globus originating near the thyroid cartilage or cricothyroid membrane may indicate something in the hypopharynx. Globus at the level of the suprasternal notch could imply a foreign body anywhere in the esophagus. In general, well-localized symptoms are more concerning than diffuse complaints.
The duration of symptoms is an important indicator. Any sore throat that has persisted beyond 3 weeks deserves further investigation. Progression of the sore throat such as increasing pain or persistent irritation also warrants closer inspection.
The constellation of associated symptoms such as odynophagia, fever, voice change, and globus can narrow the differential and are now discussed in more detail.
Sore Throat and Odynophagia
Odynophagia or pain with swallowing is often associated with sore throat, particularly in infectious and inflammatory processes. Common clinical examples of sore throat and odynophagia include tonsillitis, peritonsillar abscess, thrush, and epiglottitis. It is sometimes the absence of odynophagia that is more helpful in narrowing down the differential. For instance, throat irritation from laryngeal reflux or postnasal drip will not typically be associated with odynophagia.
Sore Throat and Fever
Fever is sometimes present with infectious causes of sore throat such as tonsillitis, viral pharyngitis, retropharyngeal abscess, and epiglottitis. Exogenous pyrogens such as the lipopolysaccharides in bacterial cell walls or endogenous cytokines can trigger fever. Noninvasive fungal throat infections do not routinely cause fever; however, in an immunocompromised individual, the presence or absence of fever is a less reliable indicator. Fungal infections are notoriously opportunistic in an immunocompromised situation, and must remain in the differential in these cases.
Sore Throat and Globus
Globus pharyngeus is a foreign body sensation in the throat. Patients will complain of “something stuck in my throat.” Globus that can be well localized may stem from a neoplasm, a vocal cord granuloma, tonsilliths, or an actual foreign body. A more vague or diffuse sense of globus can also arise from edema of the postcricoid area (see Fig. 1). The postcricoid area is the party wall between the larynx and esophageal inlet, and can be affected by refluxed stomach contents from below, or infectious or allergic mediators found in nasal discharge from above. All patients with a chronic sore throat should be questioned about their allergic history and reflux symptoms such as prior diagnosis of gastroesophageal reflux or ulcer, epigastric burning, sour brash, chronic throat clearing, intermittent voice change, and globus.
Sore Throat and Voice Change
A peritonsillar abscess may cause a characteristic muffled quality to the voice, often referred to as a “hot potato” voice. This condition occurs because the soft palate is no longer able to move as freely due to tethering of the peritonsillar muscles and edema of the palate, which causes a transient velopharyngeal insufficiency and muffled oral resonance.3 A similar voice change can be seen with significant hypertrophy of the tonsils from tonsillitis, or a disease process causing lymphoid hypertrophy such as mononucleosis or lymphoma.
The symptom of hoarseness indicates a process that has caused edema or irregularity of smooth free edge of the true vocal cords. Neoplasms or infections of the glottis can cause hoarseness directly. Neoplasms of the supraglottis or the hypopharynx can cause sore throat with hoarseness once the disease has extended to involve the true vocal folds, impinge on the recurrent laryngeal nerve, or involve the area between the thyroid cartilage and vocal folds called the paraglottic space. Moreover, progression of disease in these areas may lead to stridor or dyspnea, two signs that should always elicit an immediate airway evaluation by a specialist.
Sore Throat with Airway Compromise
A patient in airway distress may manifest some or all of the following signs: stridor, tachypnea, forward positioning with the neck extended to open up the airway, also known as “tripoding,” drooling, cyanosis, or complete obstruction. These are signs that no practitioner should miss. Infectious, inflammatory, and neoplastic processes can lead to this picture. Common pathological conditions include epiglottitis or supraglottitis, retropharyngeal abscess, parapharyngeal abscess or mass, and obstructing laryngeal and pharyngeal masses.
Sore Throat and Nasal Symptoms
Nasal symptoms such as congestion and rhinorrhea may be present with seasonal allergies or a viral pharyngitis. Nasal congestion or obstruction may also be associated with snoring and chronic mouth breathing during the day or night, which can cause a dry and irritated posterior pharyngeal mucosa and sore throat. It is also imperative to ask the patient presenting with sore throat about seasonal or perennial allergic symptoms such as nasal congestion, rhinorrhea, postnasal drip, palatal pruritus, itchy eyes, or sneezing. Chronic postnasal drip can also cause an irritated throat.
Sore Throat and Cough
Cough is a manifestation of airway irritation. Classification of the cough as wet or dry, productive or nonproductive, night-time only, or worse after meal times can aid in the diagnosis. A staccato “a-hem” or throat-clearing cough with a chronically irritated throat may be due to reflux or postnasal drip. Cough with an acute sore throat is more likely viral in nature. When cough is present with sore throat, it is less likely a streptococcal sore throat.4 Cough can persist after resolution of the sore throat and other viral symptoms, and is thought to be caused by inflammatory irritation of the recurrent laryngeal nerve.
Sore Throat and Lymphadenopathy
Lymphadenopathy can occur with many reactive, infectious, and neoplastic processes. Notable posterior cervical lymphadenopathy is seen with infectious mononucleosis and mono-like illness. Anterior lymphadenopathy is present more often than other bacterial causes in streptococcal pharyngitis. Kawasaki disease is a pediatric autoimmune vasculitis that often presents with high fevers, lymphadenopathy, sore throat, and erythematous mucus membranes.
Timing
A sore throat related to extraesophageal reflux is typically worse after meals, when supine at night, or first thing in the morning. Similarly, postnasal drip related to allergic rhinitis can be worse at night or first thing in the morning. Chronic mouth breathing can lead to a dry and irritated posterior pharyngeal mucosa and a sore throat that is worse in the morning.
In summary, in patients presenting with sore throat the following elements their history should be sought: detailed description of the symptoms, specific location of the soreness, duration of symptoms, associated symptoms, timing of symptoms, presence of reflux, and allergic rhinitis symptoms. This evaluation will narrow the differential to a few possibilities and facilitate timely, appropriate treatment.
Differential, workup, and treatment
Table 1 outlines possible causes of sore throat. Some of the most common causes are discussed here in more detail.
Table 1.
Common causes of sore throat
| Class | Etiology |
|---|---|
| Infectious | Viral pharyngitis Influenza Mononucleosis Nonstreptococcal bacterial pharyngotonsillitis Streptococcal pharyngitis Peritonsillar abscess Tonsilliths Thrush Deep space neck infection (retropharyngeal/parapharyngeal space infection) Epiglottitis/supraglottitis Fungal Laryngitis Herpangina Syphilis Lemierre syndrome Fusospirochetal infection (Vincent angina) |
| Inflammatory | Laryngopharyngeal reflux (LPR) Allergic rhinitis with post nasal drip Chronic mouth breathing Foreign body Muscle tension dysphonia Vocal cord granuloma Mucositis Granulomatous diseases (rheumatoid arthritis, gout) Pemphigus Kawasaki disease |
| Neoplastic | Squamous cell carcinoma Lymphoma Sarcoma Adenocarcinoma |
Viral Pharyngitis
By far the most common cause of sore throat is viral infection. Common viruses include rhinovirus, coronavirus, adenovirus, parainfluenza virus, influenza virus, Coxsackievirus, herpes simplex virus, Epstein-Barr virus, cytomegalovirus (CMV), and human immunodeficiency virus (HIV).4 The associated symptoms and season can give a clue as to which virus may be responsible. For instance, conjunctival involvement occurs with adnenovirus. The presence of ulcers may be due to Coxsackievirus or herpes virus. Profuse lymphadenopathy can be seen with Epstein-Barr virus, CMV, and HIV. Muscle aches would be more typical of influenza.
Viral pharyngitis typically is treated expectantly with fluids, antipyretics, and pain relief without further testing. Two exceptions to this are the influenza and Epstein-Barr viruses. These 2 viruses are now discussed in more detail.
Mononucleosis
Epstein-Barr virus (EBV) is the causative agent in infective mononucleosis. Symptoms may include sore throat, high fever, extreme fatigue lasting 1 or more weeks, swollen tonsils with or without exudate, large anterior and posterior neck nodes, faint body rash, and petechiae along the palate. Lymphoid hypertrophy, in particular involvement of the posterior nodes, is one of the most distinguishing features from other causes of sore throat. Hepatomegaly and splenomegaly can also be present.
Patients who present with these symptoms should have a complete blood count (CBC) and monospot test. Because streptococcal pharyngitis presents very similarly, a rapid streptococcal antigen test is also warranted if there is any question. The CBC will show lymphocytosis with greater than 10% atypical lymphocytes.5 Thrombocytopenia may also be present.
The monospot test is a serum test that detects the presence of heterophil antibodies with high specificity. The monospot does not detect presence of the virus. Heterophil antibodies are produced in the first 4 to 6 weeks after exposure. If testing is negative but the suspicion remains high, the test can be repeated in 1 week or antibody titers to viral components can be checked.6 The combination of IgM and IgG to the viral capsid antigen, IgM to the early antigen, and antibody to a nuclear antigen (Epstein-Bar virus nuclear antigen) are helpful in interpreting the stage of infection. CMV can also cause a mono-like picture. IgM and IgG titers for CMV can also help to distinguish between primary, latent, or reactivated CMV infection.
The purpose of testing is to confirm the diagnosis and obviate the need for extensive workups for diffuse lymphadenopathy or fever of unknown origin. Treatment is supportive, with rest, fluids, and antipyretics. Antibiotics and antivirals have no role in the treatment of mononucleosis. Ampicillin specifically should be avoided in patients suspected of mononucleosis. If given, this will elicit a pruritic rash in most patients. Steroids are occasionally given for patients whose tonsil and adenoid hypertrophy has caused airway obstruction or sleep apnea. A nasal trumpet can also be used for sleep apnea related to adenotonsillar hypertrophy. Patients should be cautioned to avoid contact sports or other vigorous activity because there is a potentially increased risk of splenic rupture. The disease typically resolves in 1 to 4 weeks but may last up to 4 months.
If lymphadenopathy persists beyond this period, referral to an otolaryngologist for fine-needle aspiration, incisional biopsy, or excisional biopsy is warranted.
Influenza
Although influenza presents with sore throat, fever, and cough similar to the “common cold,” it represents a unique global health risk. The virus spreads around the world in seasonal epidemics, and harbors the potential for pandemics such as the deadly 1918 Spanish Flu pandemic and the recent 2009 H1N1 pandemic. In comparison with other infectious agents, influenza virus has abundant natural reservoirs including humans, pigs, poultry, horses, and dogs. Influenza has a tendency to mutate, so vaccines must be revised yearly. It is spread easily via aerosolized droplets and direct contact, and is highly virulent due to frequent mutations. Strain to strain Influenza is also highly variable in its pathogenicity. Some viruses cause relatively minor symptoms whereas others are quick to cause severe disease and mortality.
Symptoms may include high fevers (>102°F/39°C), chills, myalgias, sore throat, coughing, malaise, rigors, and generalized body aches. Symptoms are typically more severe than those with a common cold. Physical examination findings are nonspecific.7
It is not cost-effective to test everyone suspected of having influenza. However, during an outbreak viral testing can help confirm those with the disease. These individuals should be counseled to avoid public spaces until afebrile for 24 hours. If identified in the first 48 hours of onset of symptoms, commencement of antiviral neuraminidase inhibitors may decrease severity of symptoms and shedding time of the virus.8 Moreover, close contacts can also be started on therapy. This approach has been shown to provide postexposure prophylaxis against symptomatic influenza, although it does not necessarily prevent transmission of the virus.9, 10
Annual influenza vaccinations are the mainstay of prevention. Vaccination not only protects the individual but also conveys herd immunity to those not immunized.11 Its effectiveness, however, is contingent on how well the yearly vaccine represents the actual viral strain in the community. The vaccine is composed of components of influenza A and B, but science cannot always predict with 100% accuracy what strains will predominate. In these situations, antiviral therapy plays a more important role.
According to the 2009 Centers for Disease Control and Prevention guidelines, antiviral therapy with neuraminidase inhibitors such as zanamivir (Relenza) and oseltamivir (Tamiflu) are currently recommended within 48 hours of symptoms for all patients at high risk for severe courses or complications of influenza. This group includes the elderly older than 65 years, pregnant women, children younger than 2 years, and patients with certain comorbid medication conditions such as asthma, heart disease, and immunodeficiency. Patients with severe or progressive cases of influenza requiring hospitalization should also be started on antiviral therapy as soon as possible, preferably within 48 hours. Antivirals may be considered for all other patients. Treatment is commenced empirically, without laboratory confirmation of influenza.12 Prophylaxis with neuraminidase inhibitors is recommended for the following patients who have had close contact of a person with suspected or confirmed influenza during the infectious period: persons at high risk for complications of influenza, health care workers and emergency medical personnel, and pregnant women. High-risk vaccinated patients who received vaccine in poor-match years and immunosuppressed patients who have been vaccinated are also good candidates for antiviral prophylaxis.12
Bacterial Pharyngitis and Tonsillitis
Several bacteria can cause pharyngitis and tonsillitis. Commonly involved bacteria include Streptococcus, Corynebacterium diphtheriae, Neisseria gonorrhoeae, Chlamydia pneumoniae, and Mycoplasma pneumoniae. Group A Streptococcus (GAS) is by far the most predominant causative organism. GAS is responsible for 15% to 30% of pediatric cases and 5% to 10% of adult cases.4, 13 Special attention is paid to identification of GAS because of the potential for preventable sequelae such as rheumatic fever, heart valve vegetations, and glomerulonephritis. Streptococcus is the only cause of pharyngitis for which antibiotics are definitely indicated.
Streptococcal infections are particularly prevalent in the winter and early spring. Patients with streptococcal throat infection present with sore throat, odynophagia, fevers, and anterior cervical lymphadenopathy. On examination, erythema of the tonsils and tonsillar pillars is present with exudates.
Several sets of clinical prediction rules have been proposed to aid in the clinical diagnosis of streptococcal pharyngitis. Two popular systems are the Walsh pharyngitis criteria and the Centor criteria. According to Walsh, patients who tested positive for GAS presented with a significantly higher frequency of recent exposure to streptococcal infection, presence of pharyngeal exudate, enlarged or tender cervical nodes, and high fever above 101°F/39°C. Presence of cough was a predictor of a negative streptococcal culture.14 The scoring system of the original Walsh system was complex and has been simplified to give 1 point to the 4 positive predictors and −1 point to cough, the only negative predictor. The Centor system similarly consists of 4 criteria: history of fever, tonsillar exudates, tender anterior cervical adenopathy, and absence of cough. The Centor system has a stronger negative predictive value (81%) than its positive predictive value (48%)15 These clinical prediction rules are helpful for stratifying patients into low, intermediate, and high probability of disease categories, which can guide treatment and the need for further testing.
There are 3 modalities for confirmation of GAS: routine throat culture, rapid streptococcal antigen test, and optical immunoassay. The rapid streptococcal antigen test is the quickest of the 3 and is highly specific (95%–98%), but is notably less sensitive than throat culture (75%–85%). One of the primary arguments in favor of rapid streptococcal testing is that it is relatively quick and minimally invasive. The rapid streptococcal test works by detecting the presence of a carbohydrate antigen unique to GAS; it consists of a throat swab and delivers a result in 10 to 20 minutes. This test allows the practitioner to determine the need for antibiotics while the patient is present, and studies have shown a decrease in overall antibiotic prescriptions in centers where the test was used routinely.2
Throat culture is highly sensitive and specific for diagnosis of streptococcal pharyngitis. Throat culture is sometimes recommended for confirmation after rapid streptococcal antigen testing is negative. Culture confirmation of negative rapid streptococcal testing, however, is the least cost-efficient method for managing possible pharyngitis.16 Furthermore, culture confirmation of negative rapid streptococcal tests does not prevent more streptococcal complications than use of a single diagnostic test.17 Exceptions to this include conditions in which there is a low probability of streptococcal throat infection (eg, summer months), when an antigen test with a poor sensitivity is used, and during an epidemic of acute rheumatic fever.16
Intramuscular penicillin G or oral penicillin V (penicillin V potassium, penicillin VK), the phenoxymethyl analogue of penicillin G, have long been the standard of care for streptococcal pharyngitis. It is interesting that over 5 decades there has not been a reported resistance to penicillin in the treatment of pharyngitis.18 Penicillin V, 500 mg 3 times a day for 10 days, is recommend and the potassium salt, penicillin VK, is more resistant to degradation by gastric acids than penicillin G. Other antibiotics such as amoxicillin, various cephalosporins, azithromycin, and clindamycin have been tried and advocated on the basis of taste or convenience, but currently penicillin V and penicillin G are still the recommended drugs of choice of the major medical academies.19, 20 Erythromycin is the first-line alternative for those with penicillin allergies. Of note, benzathine penicillin G is the only antibiotic proven in controlled studies to prevent rheumatic fever, and is available as a one-time injection of 1.2 million units given intramuscularly.20 Procaine penicillin alone is not an appropriate treatment.
Frequent tonsil infections (7 per year in 1 year) and recurrent streptococcal pharyngitis are indications for tonsillectomy, and a referral to an otolaryngologist should be initiated.
Thrush
A fungal infection involving the oropharynx or esophagus may cause sore throat, dysphagia, burning tongue, and occasionally nausea and vomiting. Usually there is no frank throat pain. The most commonly involved microorganisms are Candida species, but other opportunistic fungi such as Aspergillus species are emerging. On examination, a creamy white or light tan coating covers the affected areas such as the tongue, tonsils, posterior pharynx, or buccal mucosa. This appearance can be differentiated from leukoplakia by scraping with a tongue blade; the thrush will be removable but the leukoplakia is adherent. An erythematous base may be seen under the whitish plaques. Patients may have a history of recent antibiotics, immunosuppression from long-term steroids or other immune-modulating medications, or immunocompromised status from diseases such as diabetes, lymphoma, or HIV.
If typical plaques are seen in the oropharynx, treatment with antifungals can commence without further testing. Typical topical treatment is either nystatin, 500,000 units 3 to 5 times a day for 10 to 14 days, or clotrimazole (Mycelex) troches, 10 mg orally 5 times a day for 10 to 14 days. Troches or lozenges are an effective means of treating thrush that involves the oral cavity and oropharynx, because the drug is held locally. For esophageal involvement, nystatin suspension offers a topical option. If these are ineffective, then systemically absorbed medications such as fluconazole (Diflucan), 100 mg orally given daily for 10 to 14 days or itraconazole (Sporonox), 200 mg orally daily for 10 to 14 days may be more effective. Of these 2, itraconazole has the broadest spectrum of activity and will treat Aspergillus species, whereas fluconazole will not. Ketoconazole (Nizoral) is a similar azole antifungal drug but is used much less often as it is more toxic than the other 2, and the absorption is decreased by antacids and other medications that raise the pH of the stomach. All 3 medications work by inhibiting the cytochrome P450 system of the liver, so the concentration of other medications can be affected and liver function tests in some patients can become elevated.
If typical plaques are not seen in the oral cavity or oropharynx and the patient complains of dysphagia, either a barium swallow, esophagogastroduodenoscopy (EGD), or transnasal esophagoscopy can confirm the diagnosis. On barium swallow, the lining of the esophagus may appear irregular or shaggy. With long-standing candidal esophagitis, there may be nodularities and barium-filling defects along the side walls of the esophagus on barium swallow.
Thrush occurs when there is an imbalance between the oral bacterial flora and fungal microbes that are normally present in a small amounts in the skin and mucus membranes. Probiotic foods such as yogurt, lactobacillus packets, or acidophilus have been recommended for restoration of normal flora. However, thus far only limited studies in mice have shown that probiotics accelerate the eradication of thrush.21 Some human studies have shown that regular probiotics decrease the colonization of fungal species, but whether this translates into decreased opportunistic infections has not been demonstrated.22 Decreasing refined sugar consumption is also frequently recommended for treatment of thrush because sugars are the common carbon energy source for yeast; however, there are no studies to show that a change in carbohydrate consumption leads to a significant decrease in the available energy for yeast or leads to faster elimination of thrush.
A culture is not routinely recommended because the appearance and history are characteristic. For patients who develop candidal esophagitis without an alterative explanation, the possibility of HIV seropositivity and AIDS should be pursued.
Tonsilliths
Tonsilliths are small concretions of sloughed epidermis, bacteria, and deposited salts that congregate in tonsillar crypts. These can often cause an ipsilateral irritation of the throat or a foreign body sensation on that side. A history of refractory halitosis may also be present. A small white pearl or multiple spots of white debris typically are seen on the surface of the tonsil. The tonsilliths will slowly extrude out of the crypt and a soft foul-smelling whitish pebble anywhere from 2 to 5 mm is found. These pebbles have the appearance and consistency of a kernel of cottage cheese. Tonsilliths are benign; however, patients are usually most bothered by the associated halitosis. Treatment of allergic rhinitis, pos-nasal drip, and extraesophageal reflux are reasonable initial measures. Active hydration with noncaffeinated beverages and gargling with nonalcoholic mouth rinses such as Biotene and Closys are also helpful initial recommendations. Curetting by the patient is not recommended because of the potential for bleeding. However, if the tonsilliths and halitosis persist, a patient may opt for a tonsillectomy, which is usually effective for both eradication of the tonsilliths and halitosis.
Peritonsillar Abscess
Peritonsillar abscess is a collection of pus between the lateral aspect of the tonsil and the pharyngeal constrictor muscles. A peritonsillar abscess is sometimes difficult to differentiate from a severe case of tonsillitis. Both present with sore throat, fever, odynophagia, tonsil hypertrophy, and possible tonsillar exudates. Drooling and asymmetric tonsils also may be present in both severe tonsillitis and peritonsillar abscess. Patients with peritonsillar abscess have a characteristic muffled “hot potato” voice, but the hallmark of a peritonsillar abscess, which is not present in simple tonsillitis, is trismus. Trismus indicates that the inflammation and pus has tracked above the tonsil in the pterygoid region. Pain that is worse on one side, asymmetric tonsils, and bulging of the palate are also tell-tale signs. A deviated uvula is not as reliable a sign in the absence of the aforementioned.
Treatment of a peritonsillar abscess includes hydration, incision and drainage, and antibiotics to cover common oral aerobes and anaerobes. A dose of intravenous steroids can help to relieve pain and trismus and allow access to the palate for drainage.
Needle drainage, conventional incision and drainage, and quinsy tonsillectomy have all been shown to have similar effectiveness in treating peritonsillar abscesses acutely.23 Incision and drainage is preferred by the author when pus is found on needle aspiration. This is a procedure that most practitioners can quickly become competent to perform. One should keep in mind that the carotid lies 2 cm posterolateral to the tonsils and no that instrument should be placed deeper than 1 cm beyond the surface of the soft palate.
Common antibiotics used for peritonsillar abscesses include clindamycin, penicillin, penicillin and metronidazole combined, and cephalosporins. A culture typically is not obtained before commencing therapy, as it is not timely enough to dictate therapy and has no proven effect on outcome.24 Antibiotic therapy should be aimed at covering both common aerobic and anaerobic organisms, as these abscesses tend to be polymicrobial. The most common anaerobic organisms found are Prevotella, Porphyromonas, Fusobacterium, and Peptostreptococcus species, whereas aerobic organisms are primarily GAS (Streptococcus pyogenes), Staphylococcus aureus, and Haemophilus influenzae.25
Peritonsillar abscess is a clinical diagnosis that usually requires no imaging. Ultrasound has been used increasingly by emergency room physicians for locating the pus when performing incision and drainage, with good reliability.26 Radiographs will show soft tissue thickening and possibly the presence of air within soft tissue; however, radiographs are not the imaging modality of choice if one is needed. Computed tomography (CT) and ultrasound can be useful adjuncts when the picture is unclear or when the abscess is located inferiorly. An inferior pole abscess occurs only in rare cases but should not be missed, as it can more readily lead to serious complications including parapharyngeal abscess, airway obstruction, aspiration of pus with resultant pneumonia or lung abscess, internal jugular vein thrombophlebitis, carotid artery rupture, mediastinitis, and pericarditis.27
Recurrent peritonsillar abscess (>1/lifetime) is an indication for referral to an otolaryngologist for tonsillectomy. An interval tonsillectomy after the acute infection has subsided is often preferred over immediate (quinsy) tonsillectomy, except in the case of an inferior pole abscess when immediate tonsillectomy is the treatment of choice. Previous experience with quinsy tonsillectomy cautioned that higher rates of bleeding and other complications occur after immediate tonsillectomy, but recent reports have attempted to reverse this previous thinking.28, 29
Parapharyngeal Abscess and Retropharyngeal Abscess
Retropharyngeal abscess and parapharyngeal abscess are 2 of the most common deep space neck infections, with similar presentations, workup, treatment, and concerns. A parapharyngeal abscess (PPA) usually arises from direct extension from pharyngeal and odontogenic infections. A retropharyngeal abscess (RPA) originates most commonly from retropharyngeal lymphadenitis. RPA may also occur after penetrating trauma to the posterior pharyngeal wall. Because the parapharyngeal space communicates with all of the other deep spaces of the neck, spread can also occur from one space to another.
A throat infection may precede presentation of the retropharyngeal abscess by 1 to 3 weeks, during which time these previously inflamed, infected nodes progress to central necrosis and suppuration. Retropharyngeal nodes are prominent up until 4 years of age when they begin to fibrose and regress. A typical presentation involves a young child, roughly 1 to 5 years old, who has had an antecedent upper airway infection and then develops neck stiffness, odynophagia, dysphagia, and high fevers. Any degree of airway obstruction may be present from a muffled voice to drooling, tripod positioning, tachypnea, stertor, stridor, and complete airway obstruction. There may be external neck swelling and the pharyngeal wall may be seen to bulge, though this may be subtle, especially if the examination is limited by trismus. Parapharyngeal abscess may present in the same way but tends to afflict an older demographic than RPA.
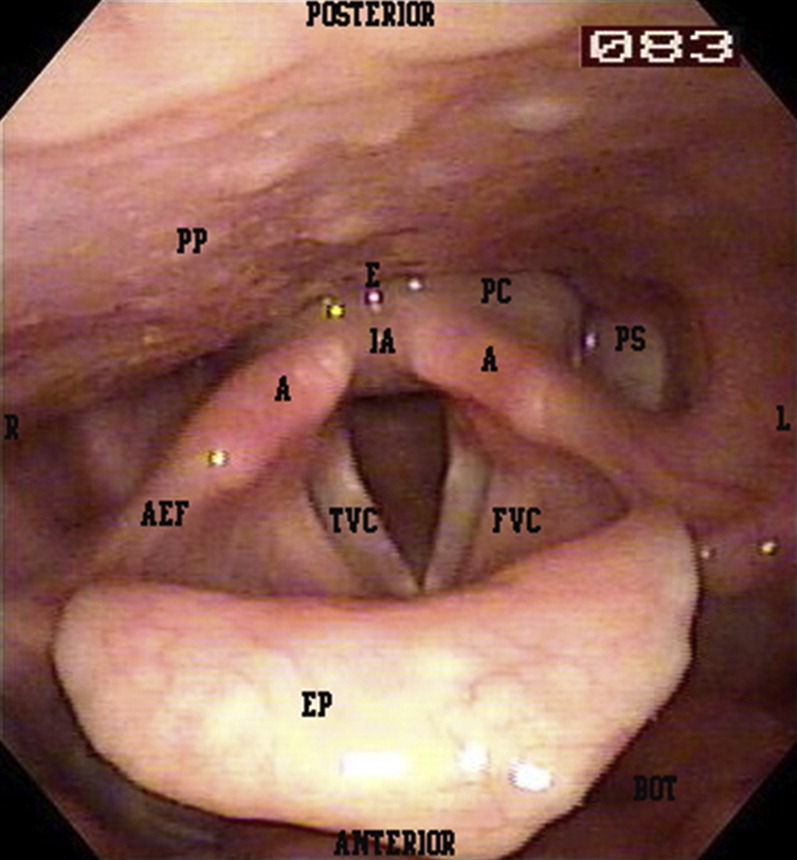
The retropharynx is a potential space that is bounded anteriorly by the buccopharyngeal fascia that surrounds the constrictor muscles, larynx, and trachea. It is bounded posteriorly by the alar fascia, which lies just anterior to the prevertebral fascia. The retropharyngeal space extends down to the level of the superior mediastinum around the level of the bifurcation of the trachea (Fig. 2 ). It is bounded laterally by the parapharyngeal spaces, which include the carotid sheaths. The potential for rapid progression to life-threatening complications exists on all sides.
Fig. 2.
Retropharyngeal and prevertebral spaces and their relationship to the spinal column and mediastinum.
From Flint PW. Cummings otolaryngology: head & neck surgery, 5th edition. St Louis (MO): Mosby Elsevier; 2010. Chapter 12, Fig. 12–20; with permission.
The retropharyngeal space is separate from the so-called danger space. The danger space lies posterior to the retropharyngeal space between the alar fascia and the prevertebral fascia. It extends down to the diaphragm. The retropharyngeal space, danger space, and prevertebral space all lie in the same plane separated by millimeter-thick layers of fascia. Infections of the retropharyngeal space can be distinguished from the latter 2 by a midline raphe which, in theory, restricts abscesses of the retropharyngeal space from crossing the midline.
The parapharyngeal space is lateral to the superior pharyngeal constrictor and medial to the mandible. It is often described as an inverted pyramid with its base at the skull base and its tip at the level of the hyoid. This space connects to every other major fascial neck space and contains nerves, salivary glands, fat and, most importantly, the carotid sheaths, which extend to the mediastinum. If a deep neck infection such as RPA or PPA goes unrecognized, complications may include: airway compromise, rupture of the abscess with aspiration and pneumonia or lung abscess, extension to parapharyngeal spaces, internal jugular vein thrombosis, vertebral osteomyelitis, vertebral body subluxation, spinal abscesses, mediastinitis, pericarditis, and sepsis.
Workup includes first and foremost, airway management. If a patient presents with a suspected deep neck abscess, a plan for airway management needs to be determined from the start. Even those patients who are seemingly stable can be tipped over to a life-threatening emergency by thoughtless airway manipulation. Airway management options include observation with continuous monitoring, fiberoptic or direct intubation, tracheostomy, and cricothyroidotomy. Minimal palpation of the abscess, limiting oropharyngeal instrumentation, and avoidance of sedation are recommended when outside of a controlled and prepared environment such as an operating room. Airway management should ideally be done by the physician(s) who will provide definitive therapy. An otolaryngology consultation should be initiated immediately for laryngoscopic assessment of the entire airway, and anesthetists should be made aware of impending airway needs.
Once the patient is deemed stable, a workup can be initiated. Neck radiographs are a quick method of assessment and do not require the patient to lay supine. Radiography is a good initial study that can quickly help to triage a patient in the proper direction of care. A lateral neck radiograph in the setting of retropharyngeal abscess may show soft tissue thickening or free air in the posterior pharyngeal soft tissues (Fig. 3 ). A good rule of thumb is that if the width of the overlying soft tissues is greater than one-half the width of the corresponding vertebrae, there is significant swelling that should be evaluated further. This method is gross but easily applied. Any radiograph, however, is greatly limited if the patient's neck is not fully extended and the film is not taken during end-inspiration. These suboptimal positions may yield a false-positive result. Lateral neck films were found to have a sensitivity of 83% for determining the presence of a pediatric deep neck infection, whereas CT scanning with contrast had a sensitivity of 100%.30
Fig. 3.
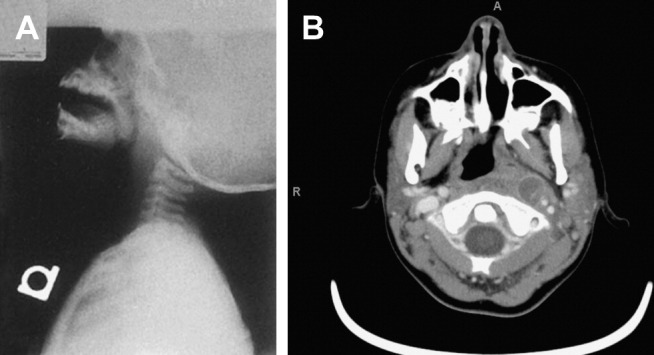
Retropharyngeal abscess. (A) lateral neck radiograph shows widening of the soft tissues anterior to the vertebral bodies. (From Flint PW. Cummings otolaryngology: head & neck surgery, 5th edition. St. Louis (MO): Mosby Elsevier; 2010. Chapter 196, Fig. 196-7A and B; with permission.) (B) CT scan with contrast of neck shows rim-enhancing collection consistent with a left retropharyngeal abscess.
Courtesy of Guy Efune, MD, Dallas, TX.
CT of the neck with contrast remains the study of choice for evaluation of suspected deep space neck infection (see Fig. 3, Fig. 4 ). From a respiratory and hemodynamic standpoint the patient must be stable enough to travel to radiology. Excessive secretions may preclude lying supine for the entire scan. CT findings include a rim-enhanced area of low density, loss of fat stranding, edema of the surrounding tissues, and possible deviation of nearby structures such as the airway. With RPA there is some controversy as to what specific radiographic findings are consistent with pus at the time of incision and drainage.31, 32, 33 Some investigators advocate that irregularity of the abscess wall was a stronger predictor than just rim enhancement for the presence of pus at the time of incision and drainage.33
Fig. 4.
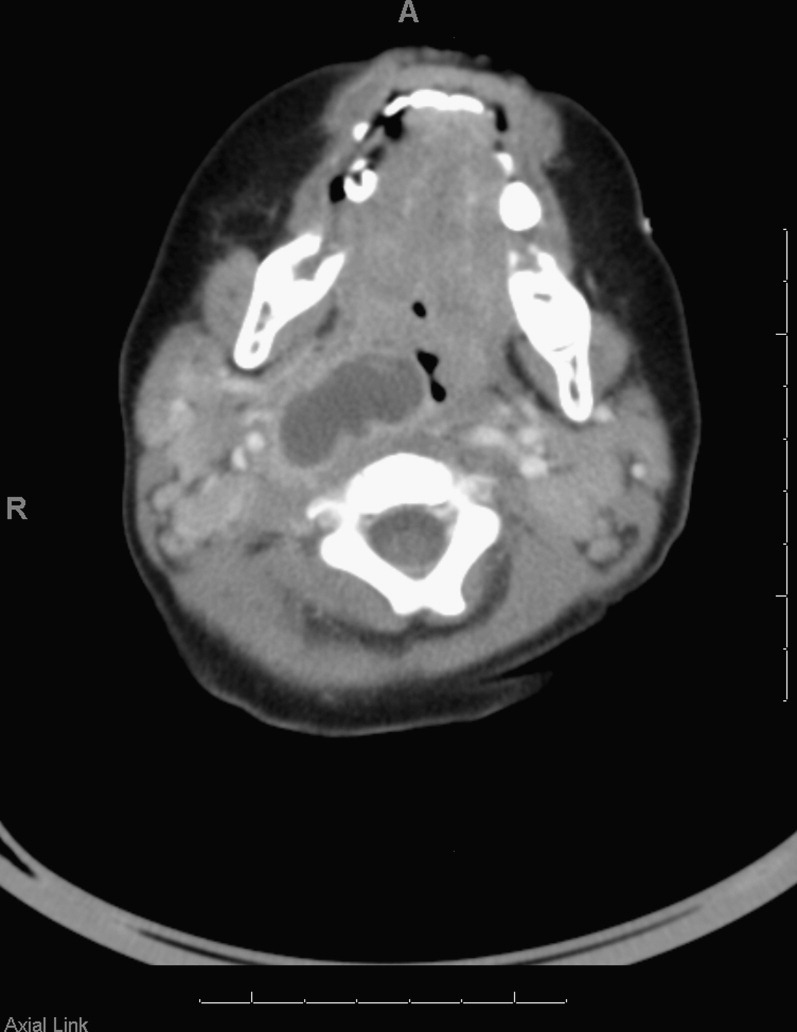
Right parapharyngeal abscess with impingement on the airway.
Courtesy of Tim Booth, MD, Department of Radiology, Children's Medical Center, Dallas, TX.
Although the information from a magnetic resonance (MR) image may be superior to that of CT for evaluation of deep space neck infections, the longer duration lying supine and the remote location are undesirable. MR imaging is also often not tolerated by young children without sedation. The ultrasound does not provide the spatial relationships necessary to assist in localizing the collection intraoperatively.
CBC and blood cultures should be checked and broad-spectrum antibiotics commenced without delay. Antibiotics should be directed at a polymicrobial mix of gram-positive aerobes and anaerobic organisms. GAS, S aureus, and H influenzae are common aerobic organisms that are found. Anaerobes include Eikenella (formerly Bacteroides), Peptostreptococcus, Fusobacterium, and Prevotella.25 Clindamycin is the usual antibiotic of choice, as it has both gram-positive and anaerobic coverage. A β-lactam resistant cephalosporin may be used in combination with clindamycin. β-Lactamase has been found to be present in up to 60% to 70% of organisms.34, 35
Parapharyngeal abscesses are drained immediately. The potential for tracheostomy at the time of surgery should always be considered and discussed in the consent. The approach to treatment of retropharyngeal abscesses is changing. Studies have shown that a trial of intravenous antibiotics for small (<2 cm), limited retropharyngeal abscesses is often effective and may obviate the need for surgery.36, 37 Failure to improve after 48 hours of antibiotics is an indication for incision and drainage. If incision and drainage is performed, a culture should be obtained to help direct therapy. Unusual organisms such as m. tuberculosis should be suspected in patients who are refractory to conventional therapies or who have traveled outside the United States.
Supraglottitis/Epiglottis
Supraglottitis is an inflammation of any of the supraglottic structures including the epiglottis, arytenoids, aryepiglottic folds, and false vocal folds. It is usually of an infectious origin and more is commonly referred to as epiglottitis because of the prominent cherry-red epiglottis seen in affected children.
Epiglottitis was formerly an affliction of toddlers and young children aged 2 to 7 years. However, since the widespread use of the Haemophilus type B vaccine starting in 1985, the incidence of pediatric epiglottitis in countries that mandate vaccination has decreased dramatically.38 Despite this decline, there have been documented cases of Haemophilus type B positive cultures from previously immunized patients with epiglottitis.39 The incidence of adult supraglottitis in the meantime has remained stable, and may be increasing.39, 40
Patients present with history of sore throat, high fevers, and odynophagia so severe that the patient refuses to eat or drink. On examination the patient often appears acutely ill and may have any degree of airway involvement including muffled voice, inspiratory stridor, tachypnea, drooling, tripod positioning, and use of accessory muscles. The patient may have an exquisitely tender anterior neck.
When epiglottitis is suspected, management of the airway is paramount. This disease process can progress rapidly to airway compromise within hours. Otolaryngology and anesthesiology consultations should be initiated immediately. In pediatric patients, any intervention including placement of intravenous access, imaging studies, and invasive examinations such as laryngoscopy should be avoided. Although the typical cherry-red epiglottis can sometimes be seen on oral examination, great caution should be used with any potentially stimulating examination. The child must be kept calm and comfortable. Sedatives and narcotics should be used very sparingly. The patient's airway is ideally assessed in the operating room with readiness for definitive airway management including nasotracheal intubation, oral intubation, or tracheostomy. A CBC, surface cultures, and blood cultures can be obtained at this time. If time will not allow and the patient's airway needs to be secured emergently, a cricothyroidotomy should be performed immediately, followed by endoscopy in the operating room, and revision of the cricothyroidotomy site to a tracheostomy.
The approach to the adult and adolescent patient with supraglottitis differs slightly. Older patients tend to be able to tolerate laryngoscopy and are more often managed with close observation in the intensive care unit with or without intubation.
Laryngoscopy is more sensitive than radiography in making the diagnosis, and provides a quicker definitive diagnosis than CT. If a radiograph is obtained, a widened epiglottis on lateral neck radiograph, referred to as the thumb sign, is a classic finding (Fig. 5 ). If associated abscess is suspected, a CT scan is warranted after the airway has been assessed and secured.
Fig. 5.

Epiglottitis. Widened epiglottis (asterisk) and aryepiglottic folds (arrowheads).
From Flint PW. Cummings otolaryngology: head & neck surgery, 5th edition. St Louis (MO): Mosby Elsevier; 2010. Chapter 102, Fig. 102–30; with permission.
Whereas Haemophilus type B predominated in the past, nowadays S aureus and Streptococcus species are more often seen.39 Clindamycin, cephalosporins, and β-lactamase resistant penicillins are typical first-line antibiotics. Intravenous steroids are also frequently given, although no there are no studies to prove their efficacy in resolving the disease process more quickly. Racemic epinephrine, frequently used in other airway emergencies, provides no improvement in epiglottitis.
Opportunistic fungal infections occasionally can cause a supraglottis that is more insidious in onset. Chronic throat irritation and voice change are common presenting symptoms. Immunosuppression or regular use of an inhaled particulate steroid such as fluticasone/salmetrol diskus (Advair) in immunocompetent patients can predispose to fungal supraglottitis. Candida is the most commonly involved fungus but in endemic areas Coccidioides, Histoplasma, Cryptococcus, and Blastomyces may also be present. Fungal supraglottitis is treated with systemic antifungals and by addressing the underlying etiology.
Laryngopharyngeal Reflux
Gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) are increasingly implicated in diseases of the upper aerodigestive tract. Since the 1990s reflux has been considered a contributor to laryngeal irritation, and more recently studies have sought to understand its role in chronic nonspecific pharyngitis.41 The mucosa of the larynx and pharynx are more sensitive to acid and pepsin than the gastric or esophageal mucosa. The larynx and pharynx lack bicarbonate production and peristalsis, which are protective to the stomach and esophagus. Koufman42 demonstrated that even trace amounts of reflux, 3 times a week, are enough to cause mucosa trauma to the larynx. Recent studies in cell culture have shown that pepsin can damage hypopharyngeal cells in the absence of acid.43
LPR is thought to be a distinct entity from GER. GER is a high-volume problem whereas LPR is a low-volume, high-susceptibility problem. Those with LPR are typically daytime upright refluxers whereas patients with GER are symptomatically worse when supine. Symptoms of LPR can be present in the absence of common gastroesophageal reflux symptoms such as sour brash and heartburn. Only about 25% of patients with LPR develop esophagitis. Some patients may suffer from both problems and have a mixture of associated symptoms.
Patients with nonspecific pharyngitis may complain of a chronically irritated or sore throat, globus sensation, and chronic throat clearing. Intermittent hoarseness may also be present. Symptoms are typically worse after a meal or possibly after lying supine. Sore throat may be the result of direct irritation or chronic coughing.
Studies have shown that patients with complaint of chronic sore throat for which no other attributable cause was found scored higher on both reflux symptoms and reflux findings. Their symptom and finding scores also decreased compared with controls after 2 months of twice-daily proton pump inhibitor (PPI) therapy.41
There are 3 approaches to confirming the diagnosis of LPR: (1) response of symptoms to behavioral and empiric medical treatment, (2) endoscopic observation of mucosal injury, and (3) demonstration of reflux events by impedance and pH-monitoring studies or barium swallow esophagram. The first approach can be trialed by any primary practitioner. The latter 2 require referral to either an otolaryngologist or gastroenterologist for evaluation. On laryngoscopic examination, patients may manifest edema of the posterior glottis including the arytenoids and interarytenoid area. Erythema may also be present along the posterior glottis and posterior pharyngeal wall. There may be hypervascularity or edema of the true vocal folds (Fig. 6 ).
Fig. 6.

Laryngeal changes from chronic reflux. Edema of the interarytenoid mucosa (asterisk). Irregular, edematous, and erythematous true vocal cord mucosa (arrowheads).
Courtesy of Ted Mau, MD, PhD, Dallas, TX.
Behavioral modifications PPIs such as omeprazole, rabeprazole, esomeprazole, lansoprazole, and pantoprazole are the treatments of choice for LPR. Treatment can be initially commenced on the basis of laryngoscopic findings alone. Behavioral modifications include eating smaller and more frequent meals, not lying supine after a meal, avoiding a pre-bedtime or midnight snack, and raising the head of bed 6 to 8 inches by placing on cinderblocks or phone books under the uppermost bedposts. Patients should also be given a list of reflux-provoking foods to avoid such as caffeine, mints, chocolate, tomato sauces, fried or fatty foods, high-cholesterol foods, spicy foods, carbonated beverages, and citrus.
There are 2 theories of drug therapy: a “step-up” method and a “step-down” method. In the step-up method, patients are started first on antacids, advanced to H2 blockers if still symptomatic, then started on daily PPIs, and finally twice-daily therapy if this is not effective. Alternatively, some advocate that starting on twice-daily therapy and then stepping down is more effective and less costly in the long run.44 Patients should be counseled that it is important to take the PPI 30 minutes before meals for optimal effect. Two to 3 months of therapy usually are required to see effects. Persistent symptoms despite compliant therapy warrant referral to a specialist for further evaluation and consideration of surgical intervention such as a fundoplication.
Rhinitis
Rhinitis or rhinosinusitis may be caused by allergic, infectious, or inflammatory diseases. Patients may present with nasal congestion, rhinorrhea, postnasal drip, or nasal irritation. Nasal congestion, nasal obstruction, and postnasal drip can all contribute to a chronically sore throat.
Postnasal drip itself is not a pathological phenomenon. It is the conscious sensation of a naturally occurring process caused by increased volume or increased viscosity of the mucus. Mucus is secreted by the nasal mucosa with the purpose of trapping irritants, pollutants, infectious organisms, and allergens, which are routinely passed backward into the pharynx to be swallowed into the acidic environment of the stomach. This mucus consists of enzymes, proteins, and inorganic salts. Increased production of mucus occurs with allergic disease, viral infections, bacterial or fungal sinusitis, vasomotor rhinitis, hormonal changes, aging, or exposure to cold.
Postnasal drip may cause a chronically irritated throat, globus sensation, excessive phlegm, or chronic cough. Patients with chronic diffuse sore throat should be asked about postnasal drip and other symptoms of chronic rhinitis or sinusitis including thick or thin rhinorrhea, sneezing, congestion, watery eyes, facial pressure, or a seasonal component to their symptoms. The timing of the sore throat in these cases tends to be worse at night or in the early morning.
Postnasal drip is most frequently associated with allergic rhinitis. Examination findings consistent with allergic rhinitis include enlarged or boggy turbinates, clear secretions that may be either thin or tacky, cobblestoned and hypervascular posterior pharyngeal wall, erythema of the tonsils or tonsillar pillars, pale edema of the posterior larynx, and erythema of the conjunctiva.
Nasal congestion is the sensation of limited air flow through the nose, which waxes and wanes with different exposures and positioning. It differs from nasal obstruction, which is more often a static obstruction attributable to a structural problem such as a deviated nasal septum or nasal mass. Nasal congestion can be seen with rhinitis that is allergic, vasomotor, or infectious in nature. It can also occur after chronic use of intranasal decongestants such as oxymetazoline (Afrin) and phenylephrine (Neosynephrine). The severe nasal congestion that occurs after prolonged use of these over-the-counter nasal sprays is called rhinitis medicamentosa, and will only abate after cessation of the medication.
Both nasal congestion and nasal obstruction can lead to chronic mouth breathing. Mouth breathing bypasses the natural humidification of the nose and is especially problematic at night when dependent nasal congestion occurs. This chronic mouth breathing can lead to a dry and irritated posterior pharynx and complaint of a chronic sore throat.
Saline irrigations and steroid nasal sprays are the first-line therapy for nasal congestion and postnasal drip related to allergic rhinitis. If this is not sufficient, consideration of an antihistamine, either intranasally or orally, may be effective. Ipratropium bromide (Atrovent) is particularly effective for vasomotor rhinitis. Cessation of over-the-counter intranasal decongestants is required for relief of rhinitis medicamentosa. Surgery may be necessary for significant nasal obstruction caused by septal deviation or nasal masses.
Foreign Body
A foreign body in the pharynx may cause a sensation of globus, and the patient may complain of a sore throat if the foreign body causes abrasion or erosion; this is usually a well-localized irritation. Pills are a particularly common irritation for the elderly and those with underlying swallowing or motility disorders. Large pill size and sustained-release pills, especially when taken in the supine position with only a small amount of liquid, are risk factors for pill dysphagia. Fish bones and chicken bones are other common causes of persistent foreign body sensation. Even after the foreign body has passed, inflammation and irritation can persist from the damaged mucosa. This is typically self-limited but sucralfate can provide some additional protection to the mucosa as it heals.
Any persistent foreign body sensation should be evaluated with anteroposterior and lateral neck films. Laryngoscopy may also be required if the suspected foreign body is radiolucent. Pharyngeal and laryngeal foreign bodies require endoscopic removal because of their threat to the patient's airway. Organic material that has passed below the cricopharyngeus can be allowed to continue through the gastrointestinal tract. Batteries must be removed immediately regardless of location, because the acid they contain has the potential to leak and cause a caustic burn in the aerodigestive tract.
Neoplasms
Both benign and malignant neoplasms in the larynx or pharynx can cause globus, irritation, or frank pain in the throat. Benign neoplasms more often cause a sensation of globus without pain or discomfort. Pain is a concerning sign and raises the suspicion of malignancy. Depending on the location, associated symptoms may include dysphagia, odynophagia, otalgia, voice change, weight loss, and lymphadenopathy.
The most common malignant neoplasm in the throat is squamous cell carcinoma and of these, tonsil cancers are the most frequent. Adenocarcinoma, sarcoma, and lymphoma can also occur in the throat and present with sore throat. Patients with persistent sore throats, worsening symptoms, or well-localized pain should be referred to an otolaryngologist for a full evaluation.
Footnotes
Disclosure: The author has no conflicts of interest to disclose.
References
- 1.Schappert S.M., Burt C.W. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 2001-02. Vital Health Stat 13. 2006;159:1–66. [PubMed] [Google Scholar]
- 2.Ayanruoh S., Waseem M., Quee F. Impact of rapid streptococcal test on antibiotic use in a pediatric emergency department. Pediatr Emerg Care. 2009;25(11):748–750. doi: 10.1097/PEC.0b013e3181bec88c. [DOI] [PubMed] [Google Scholar]
- 3.Finkelstein Y., Bar-Ziv J., Nachmani A. Peritonsillar abscess as a cause of transient velopharyngeal insufficiency. Cleft Palate Craniofac J. 1993;30(4):421–428. doi: 10.1597/1545-1569_1993_030_0421_paaaco_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 4.Bisno A. Acute pharyngitis. N Engl J Med. 2001;344(3):205–211. doi: 10.1056/NEJM200101183440308. [DOI] [PubMed] [Google Scholar]
- 5.Hoagland R.J. Infectious mononucleosis. Prim Care. 1975;2:295–307. [PubMed] [Google Scholar]
- 6.Ebell M. Epstein Barr virus infectious mononucleosis. Am Fam Physician. 2004;70(7):1279–1287. [PubMed] [Google Scholar]
- 7.Ebell M.H., White L.L., Casault T. A systematic review of the history and physical examination to diagnose influenza. J Am Board Fam Pract. 2004;17:1–5. doi: 10.3122/jabfm.17.1.1. [DOI] [PubMed] [Google Scholar]
- 8.Moscona A. Neuraminidase inhibitors for influenza. N Engl J Med. 2005;353(13):1363–1373. doi: 10.1056/NEJMra050740. [DOI] [PubMed] [Google Scholar]
- 9.Jefferson T., Jones M., Doshi P. Neuraminidase inhibitors for preventing and treating influenza in healthy adults: systematic review and meta-analysis. BMJ. 2009;339:b5106. doi: 10.1136/bmj.b5106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cooper N.J., Sutton A.J., Abrams K.R. Effectiveness of neuraminidase inhibitors in treatment and prevention of influenza A and B: systematic review and meta-analyses of randomised controlled trials. BMJ. 2003;326(7401):1235. doi: 10.1136/bmj.326.7401.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glezen W.P. Herd protection against influenza. J Clin Virol. 2006;37(4):237–243. doi: 10.1016/j.jcv.2006.08.020. [DOI] [PubMed] [Google Scholar]
- 12.http://www.cdc.gov/h1n1flu/recommendations.htm Available at: Accessed January 30, 2010.
- 13.Komaroff A.L., Pas T.M., Aronson M.D. The prediction of streptococcal pharyngitis in adults. J Gen Intern Med. 1986;1:1–7. doi: 10.1007/BF02596317. [DOI] [PubMed] [Google Scholar]
- 14.Walsh B.T., Bookheim W.W., Johnson R.C. Recognition of streptococcal pharyngitis in adults. Arch Intern Med. 1975;135(11):1493–1497. [PubMed] [Google Scholar]
- 15.Marín Cañada J., Cubillo Serna A., Gómez-Escalonilla Cruz N. Is streptococcal pharyngitis diagnosis possible? Aten Primaria. 2007;39(7):361–365. doi: 10.1157/13107724. [in Spanish] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Webb K.H. Does culture confirmation of high-sensitivity rapid streptococcal tests make sense? A medical decision analysis. Pediatrics. 1998;101(2):E2. doi: 10.1542/peds.101.2.e2. [DOI] [PubMed] [Google Scholar]
- 17.Webb K.H., Needham C.A., Kurtz S.R. Use of a high-sensitivity rapid strep test without culture confirmation of negative results: 2 years' experience. J Fam Pract. 2000;49(1):34–38. [PubMed] [Google Scholar]
- 18.Kaplan E.L., Johnson D.R., Del Rosario M.C. Susceptibility of group A beta-hemolytic streptococci to thirteen antibiotics: examination of 301 strains isolated in the United States between 1994 and 1997. Pediatr Infect Dis J. 1999;18:1069–1072. doi: 10.1097/00006454-199912000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Shulman S.T., Gerber M.A. So what's wrong with penicillin for strep throat? Pediatrics. 2004;113(6):1816–1819. doi: 10.1542/peds.113.6.1816. [DOI] [PubMed] [Google Scholar]
- 20.Gerber M.A., Baltimore R.S., Eaton C.B. Prevention of rheumatic fever and diagnosis and treatment of acute Streptococcal pharyngitis: a scientific statement from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translational Biology, and the Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics. Circulation. 2009;119(11):1541–1551. doi: 10.1161/CIRCULATIONAHA.109.191959. [DOI] [PubMed] [Google Scholar]
- 21.Elahi S., Pang G., Ashman R. Enhanced clearance of Candida albicans from the oral cavities of mice following oral administration of Lactobacillus acidophilus. Clin Exp Immunol. 2005;141(1):29–36. doi: 10.1111/j.1365-2249.2005.02811.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hatakka K., Ahola A.J., Yli-Knuuttila H. Probiotics reduce the prevalence of oral candida in the elderly—a randomized controlled trial. J Dent Res. 2007;86(2):125–130. doi: 10.1177/154405910708600204. [DOI] [PubMed] [Google Scholar]
- 23.Johnson R.F., Stewart M.G. The contemporary approach to diagnosis and management of peritonsillar abscess. J Oral Maxillofac Surg. 2004;62(12):1545–1550. doi: 10.1097/01.moo.0000162259.42115.38. [DOI] [PubMed] [Google Scholar]
- 24.Cherukuri S., Benninger M.S. Use of bacteriologic studies in the outpatient management of peritonsillar abscess. Laryngoscope. 2002;112(1):18–20. doi: 10.1097/00005537-200201000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Brook I. Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses. Curr Opin Otolaryngol Head Neck Surg. 2005;13(3):157–160. doi: 10.1097/01.moo.0000162259.42115.38. [DOI] [PubMed] [Google Scholar]
- 26.Lyon M., Blaivas M. Intraoral ultrasound in the diagnosis and treatment of suspected peritonsillar abscess in the emergency department. Acad Emerg Med. 2005;12(1):85–88. doi: 10.1197/j.aem.2004.08.045. [DOI] [PubMed] [Google Scholar]
- 27.Licameli G.R., Grillone G.A. Inferior pole peritonsillar abscess. Otolaryngol Head Neck Surg. 1998;118:95–99. doi: 10.1016/S0194-5998(98)70381-X. [DOI] [PubMed] [Google Scholar]
- 28.Windfuhr J.P., Chen Y.S. Immediate abscess tonsillectomy—a safe procedure? Auris Nasus Larynx. 2001;28(4):323–327. doi: 10.1016/s0385-8146(01)00098-0. [DOI] [PubMed] [Google Scholar]
- 29.Suzuki M., Ueyama T., Mogi G. Immediate tonsillectomy for peritonsillar abscess. Auris Nasus Larynx. 1999;26(3):299–304. doi: 10.1016/s0385-8146(98)00070-4. [DOI] [PubMed] [Google Scholar]
- 30.Nagy M., Backstrom J. Comparison of the sensitivity of lateral neck radiographs and computed tomography scanning in pediatric deep-neck infections. Laryngoscope. 1999;109(5):775–779. doi: 10.1097/00005537-199905000-00017. [DOI] [PubMed] [Google Scholar]
- 31.Shefelbine S.E., Mancuso A.A., Gajewski B.J. Pediatric retropharyngeal lymphadenitis: differentiation from retropharyngeal abscess and treatment implications. Otolaryngol Head Neck Surg. 2007;136(2):182–188. doi: 10.1016/j.otohns.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 32.Malloy K.M., Christenson T., Meyer J.S. Lack of association of CT findings and surgical drainage in pediatric neck abscesses. Int J Pediatr Otorhinolaryngol. 2008;72(2):235–239. doi: 10.1016/j.ijporl.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 33.Kirse D.J., Roberson D.W. Surgical management of retropharyngeal space infections in children. Laryngoscope. 2001;111(8):1413–1422. doi: 10.1097/00005537-200108000-00018. [DOI] [PubMed] [Google Scholar]
- 34.Brook I. Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses. J Oral Maxillofac Surg. 2004;62(12):1545–1550. doi: 10.1016/j.joms.2003.12.043. [DOI] [PubMed] [Google Scholar]
- 35.Brook I. Microbiology of retropharyngeal abscesses in children. Am J Dis Child. 1987;141(2):202–204. doi: 10.1001/archpedi.1987.04460020092034. [DOI] [PubMed] [Google Scholar]
- 36.McClay J.E., Murray A.D., Booth T. Intravenous antibiotic therapy for deep neck abscesses defined by computed tomography. Arch Otolaryngol Head Neck Surg. 2003;129(11):1207–1212. doi: 10.1001/archotol.129.11.1207. [DOI] [PubMed] [Google Scholar]
- 37.Page N.C., Bauer E.M., Lieu J.E. Clinical features and treatment of retropharyngeal abscess in children. Otolaryngol Head Neck Surg. 2008;138(3):300–306. doi: 10.1016/j.otohns.2007.11.033. [DOI] [PubMed] [Google Scholar]
- 38.Frantz T.D., Rasgon B.M. Acute epiglottitis: changing epidemiologic patterns. Otolaryngol Head Neck Surg. 1993;109(3 Pt 1):457–460. doi: 10.1177/019459989310900311. [DOI] [PubMed] [Google Scholar]
- 39.Shah R.K., Roberson D.W., Jones D.T. Epiglottitis in the Haemophilus influenzae type B vaccine era: changing trends. Laryngoscope. 2004;114(3):557–560. doi: 10.1097/00005537-200403000-00031. [DOI] [PubMed] [Google Scholar]
- 40.Berger G., Landau T., Berger S. The rising incidence of adult acute epiglottitis and epiglottic abscess. Am J Otolaryngol. 2003;24(6):374–383. doi: 10.1016/s0196-0709(03)00083-8. [DOI] [PubMed] [Google Scholar]
- 41.Yazici Z.M., Sayin I., Kayhan F.T. Laryngopharyngeal reflux might play a role on chronic nonspecific pharyngitis. Eur Arch Otorhinolaryngol. 2010;267(4):571–574. doi: 10.1007/s00405-009-1044-2. [DOI] [PubMed] [Google Scholar]
- 42.Koufman J.A. The Otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope. 1991;101(Suppl 53):1–78. doi: 10.1002/lary.1991.101.s53.1. [DOI] [PubMed] [Google Scholar]
- 43.Johnston N., Wells C.W., Samuels T.L. Pepsin in nonacidic refluxate can damage hypopharyngeal epithelial cells. Ann Otol Rhinol Laryngol. 2009;118(9):677–685. doi: 10.1177/000348940911800913. [DOI] [PubMed] [Google Scholar]
- 44.Ofman J.J., Dorn G.H., Fennerty M.B. The clinical and economic impact of competing management strategies for gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2002;16(2):261–273. doi: 10.1046/j.1365-2036.2002.01167.x. [DOI] [PubMed] [Google Scholar]