Abstract
Hepatitis B virus (HBV) infection causes major public health problems worldwide. The clinical limitation of current antiviral drugs for HBV, such as lamivudine, is the emergence of drug-resistant viral strains during prolonged antiviral therapy. Cepharanthine hydrochloride (CH), a natural alkaloid-derived compound, has been reported to possess potent activity against various viruses. The present study was performed to evaluate the in vitro activity of CH against clinical wild-type and lamivudine-resistant HBV isolates in transiently transfected cells. HBV DNA was extracted from serum samples collected both before lamivudine therapy and at the time of viral breakthrough and was amplified by polymerase chain reaction (PCR). The amplicons were cloned into a novel expression vector, pHY106, which can initiate the intracellular HBV replication cycle after cell transfection. Following transfection of the cloned amplicon into HepG2 cells, a drug susceptibility assay was performed. The level of viral antigen, HBeAg, was determined by enzyme-linked immunosorbent assay (ELISA). Quantitative real-time PCR (Q-PCR) was used for determining the amount of intracellular HBV DNA. Heat stress cognate 70 (Hsc70), a host protein required for HBV replication, was also analyzed by reverse transcription PCR (RT-PCR) to explore the possible antiviral mechanism of CH. The results showed that CH inhibited replication and HBeAg production by either wild-type or lamivudine-resistant HBV clinical isolates in a dose-dependent manner. The Hsc70 mRNA was also downregulated significantly. In conclusion, CH is active against both wild-type and lamivudine-resistant HBV clinical isolates, and its activity may be associated with its inhibition of host Hsc70.
Keywords: Cepharanthine hydrochloride, Hepatitis B virus, Lamivudine resistance, Antiviral, Heat stress cognate 70
1. Introduction
Hepatitis B virus (HBV) infection causes the major public health problems worldwide. Over the past two decades, the prognosis of chronic hepatitis B has been significantly improved due to the emergence of two formulations of interferon and five orally administered nucleos(t)ide analogs (Yuen and Lai, 2011). However, the prolonged use of nucleos(t)ide analogs frequently result in the emergence of drug-resistant HBV mutants, which are responsible for therapeutic failure and progression of liver disease (Hongthanakorn et al., 2011). It is reported that up to 76% of the patients developed viral resistance after 5 years of lamivudine therapy (Yuen et al., 2009). The signature mutations rtM204V/I, which have been mapped in the conserved tyrosine–methionine–aspartate–aspartate (YMDD) motif within the C domain of the reverse transcriptase (RT), are frequently associated with lamivudine resistance (Allen et al., 1998). Furthermore, they are often associated with the compensatory mutations rtL180M or rtV173L in the B domain of the RT, which partially restore the replicative capacity of the YMDD mutation strains (Delaney et al., 2003, Enomoto et al., 2007). One in vitro study demonstrated that drug susceptibility decreased over 10,000-fold once lamivudine-resistant HBV mutants were selected (Lada et al., 2004). Moreover, the rapid progression or acute exacerbation of hepatitis usually occurs after the emergence of lamivudine resistance (Suzuki et al., 2006). Thus, the discovery and development of novel anti-HBV drugs with innovative targets are urgently needed for the treatment of chronic hepatitis B, especially for rescue therapy of drug-resistant patients.
Natural herbs offer good candidates with special antiviral characteristics and are widely used for chronic hepatitis B treatment (Cui et al., 2010). Cepharanthine hydrochloride (CH) is a compound manufactured by salification from cepharanthine, which is a natural biscoclaurine alkaloid extracted from Stephania cepharantha Hayata. CH has attracted increasing scientific attention in recent years due to the extent of its biological activities, including antitumor, antiviral and anti-inflammatory actions, and its ability to promote leukocyte, induce apoptosis and reverse multidrug resistance induced by long-term chemotherapy (Rogosnitzky and Danks, 2011). With regard to the antiviral activity of CH, thus far there have been several reports on human immunodeficiency virus (HIV) (Baba et al., 2001), severe acute respiratory syndrome coronavirus (SARS-CoV) (Zhang et al., 2005) and herpes simplex virus (HSV) (Liu et al., 2004). However, the in vitro anti-HBV activity of CH has never been explored until our recent unpublished observations demonstrated that CH was an efficient inhibitor of wild-type HBV in the stable HBV-producing cell line HepG2.2.15.
In the present study, we investigated the antiviral activity of CH against wild-type and lamivudine-resistant HBV clinical isolates in transiently transfected HepG2 cells. The preliminary mechanism of action, based on the theory that host heat stress cognate 70 (Hsc70) is required for HBV replication (Wang et al., 2010, Wang et al., 2011), was further explored.
2. Materials and methods
2.1. Patient
A 26-year-old chronically HBV-infected Chinese man initially received oral lamivudine monotherapy at 100 mg per day. The patient's serum HBV DNA decreased from 1.4 × 108 copies/ml to 1.3 × 104 copies/ml after receiving lamivudine monotherapy for 6 months, and became undetectable after additional 6 months of lamivudine therapy. Unfortunately, the patient's serum HBV DNA rebounded to 4.8 × 106 copies/ml after a total of 16 months of lamivudine monotherapy, and continued to rise to the initial level 3 months later. At this time point, a genotypic analysis by direct sequencing of the entire polymerase RT region of the circulating HBV was performed and revealed the presence of rtV173L/L180M/M204V triple mutations, but not additional lamivudine resistance-conferring mutations. The resistant HBV strain was genotype B. The patient was seropositive for HBsAg and HBeAg. Serum samples were collected before lamivudine therapy and after viral breakthrough, respectively, for drug susceptibility analysis. Access to the materials was approved by the ethics committee of Zhengzhou University, Henan, China, and informed consent was obtained from the patient.
2.2. Compounds
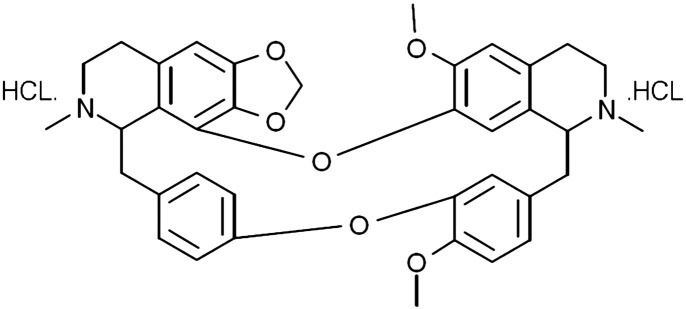
CH (Fig. 1 ) with purity of over 95% as determined by high performance liquid chromatography (HPLC) was maintained in our laboratory. Lamivudine was provided by GlaxoSmithKline Co., Ltd. (Suzhou, China). Adefovir, used as a positive control for the inhibition of the lamivudine-resistant HBV strain, was obtained from GlaxoSmithKline Co., Ltd. (Tianjin, China). Stock solutions (100 mM) of CH, lamivudine and adefovir were dissolved in phosphate buffered saline (PBS) and diluted with culture medium to the desired working concentrations when used.
Fig. 1.
Chemical structure of cepharanthine hydrochloride. Molecular formula: C37H38N2O6·HCL; molecular weight: 679 g/mol.
2.3. Cell line and plasmid
The human hepatoma cell line HepG2 was obtained from the China Center for Typical Culture Collection (CCTCC) (Wuhan, China). The cells were cultured at 37 °C in a humidified 5% CO2 atmosphere in Dulbecco's modified Eagle's medium (DMEM) (Hyclone, USA) supplemented with 10% fetal bovine serum (GIBCO, USA), 100 units/ml penicillin G and 100 μg/ml streptomycin. pHY106, a novel plasmid expression vector, was constructed and kindly provided by William Delaney and Huiling Yang from Gilead Sciences. The plasmid contains 180 bp of HBV sequence that is very well conserved among various HBV genotypes and two SapI sites that allow insertion of the SapI-treated PCR-amplified HBV genome (Yang et al., 2004).
2.4. Cytotoxicity assay
The cytotoxicity of the tested compounds to HepG2 cells was determined by the XTT assay as described by Guo et al. (2010), except that the duration of drug administration was 6 days. Each compound was assayed in four replicates with at least five concentrations. The cytotoxic concentrations of the compounds reducing cell viability by 50% (CC50) were determined.
2.5. Isolation and sequence analysis of clinical HBV strains
HBV DNA was extracted from 200 μl of serum samples using a commercial viral DNA extraction kit (OMEGA, USA). The full-length HBV genome was amplified by polymerase chain reaction (PCR) using the primers and thermocycling conditions described by Günther et al. (1995). The PCR product was digested with SapI (MBI, USA) and then ligated into the SapI-digested and shrimp alkaline phosphatase-treated pHY106 plasmid, producing a recombinant clone termed pHY106-HBV. The recombinant clone served as a template for sequencing the conserved HBV polymerase RT region. The result indicated that the cloned HBV genome that was directly isolated from the serum of the lamivudine-resistant patient harbored the rtV173L/L180M/M204V triple mutations. As expected, the cloned HBV genome from the serum collected before lamivudine therapy contained no mutation and was used as a wild-type control.
2.6. Transfection and drug treatment
The selected recombinant clones containing wild-type or mutated HBV genome were transiently transfected into HepG2 cells as follows. Briefly, six-well culture plates (Corning, USA) were seeded at 6 × 105 HepG2 cells/well 16 h earlier and transfected with 4 μg DNA using 10 μl Lipofectamine 2000 (Invitrogen, USA) according to the manufacturer's protocol. After determining the effects of the compounds on HepG2 cell viability, drug treatment was initiated the next day and lasted for 6 days, with replacement of fresh drug-free or drug-containing media every 2 days. The concentrations of CH, lamivudine and adefovir used for the drug susceptibility assays were 0, 0.01, 0.1, 1, 10 and 100 μM. After 6 days of drug treatment, the cell culture supernatant and cells were collected and stored at − 20 °C for the subsequent experiments.
2.7. Detection of HBV antigens in the cell culture supernatant
After 6 days of drug treatment, HBsAg and HBeAg in the cell culture supernatant were detected using a commercially available ELISA kit (Kehua Bio-engineering Corporation, Shanghai, China) according to the manufacturer's protocol. Inhibition rates (%) were calculated using the following formula: [(A450 of the control wells without drug − A450 of the experimental wells) / (A450 of the control wells without drug − A450 of blank control wells without cells)] × 100%. The 50% inhibitory concentrations (IC50s) were calculated by regression analyses.
2.8. Quantification of intracellular HBV DNA
The quantity of intracellular HBV DNA was determined by quantitative real-time PCR based on the TaqMan technology. In brief, the cells were rinsed twice with cold PBS and lysed with 500 μl of lysis buffer containing 50 mM Tris–HCl (pH 7.4), 150 mm/l NaCL and 0.5% (vol/vol) Nonidet P-40. After centrifugation at 13,000 rpm for 3 min, supernatants were transferred to fresh microcentrifuge tubes, and MgCl2 was added to give a final Mg2 + concentration of 10 mM. Contaminating input plasmid was then digested for 1 h at 37 °C with 20 U of DNase I before the reaction was terminated with 10 mM EDTA. HBV DNA was purified using a commercially available viral DNA extraction kit (OMEGA, USA). Quantitative real-time PCR was performed in a LightCycler (Roche, Germany) with the HBV Fluorescent Quantitative PCR Detection Kit (PG Biotech, Shenzhen, China) according to the manufacturer's instructions. After an initial denaturation at 95 °C for 90 s, 40 cycles of denaturation at 94 °C for 5 s and annealing/extension at 56 °C for 45 s were conducted. The inhibitory rates and IC50s were calculated as described above.
2.9. RT-PCR analysis of host Hsc70 mRNA
To elucidate the antiviral mechanism of CH, the amount of host Hsc70 mRNA was determined by RT-PCR. In brief, after exposure to different concentrations of CH for 6 days, the total RNA was extracted from the collected cell samples with the TRIzol reagent (Invitrogen, USA) and digested with RNase-free DNase I (Promega, USA) for 30 min, followed by RT-PCR analysis. The sequences of the Hsc70 primers were Hsc70-F: 5′-TGCTGCTGCTA TTGCTTACG-3′, and Hsc70-R: 5′-TCAATAGTGAGGATTGACACATCA-3′. As an internal reference, a GAPDH gene segment was amplified with primers GAPDH-F: 5′-GAGTCAACGGATTTGGTCGT-3′ and GAPDH-R: 5′-GACAAGCTTCCCGTTC TCAG-3′. The RT-PCR program was 42 °C for 60 min, 25 °C for 5 min, followed by 30 cycles of 94 °C for 30 s, 54 °C for 30 s, and 72 °C for 30 s. The PCR bands were analyzed by the Quantity One software (Bio-Rad, USA). The amount of gene-specific PCR products was expressed as the ratio of the intensity of each band to that of the corresponding GAPDH internal reference.
2.10. Statistical analysis
Statistical analysis was performed using the SPSS 19.0 software (SPSS Inc., Chicago, IL, USA). The data are expressed as the means ± SD. Student's t-test and one-way ANOVA were used to determine the statistical significance of differences between groups. A value of P < 0.05 was considered statistically significant.
3. Results
3.1. Effects of compounds on cell viability
Cell viability of HepG2 cells was evaluated by the XTT assay after exposure to varying concentrations of compounds for 6 days. Results showed that no significant cytotoxicity was observed with lamivudine at the highest drug concentrations of 1000 μM. whereas the CC50 values for adefovir and CH were 215.06 ± 18.75 μM and 203.47 ± 27.39 μM, respectively.
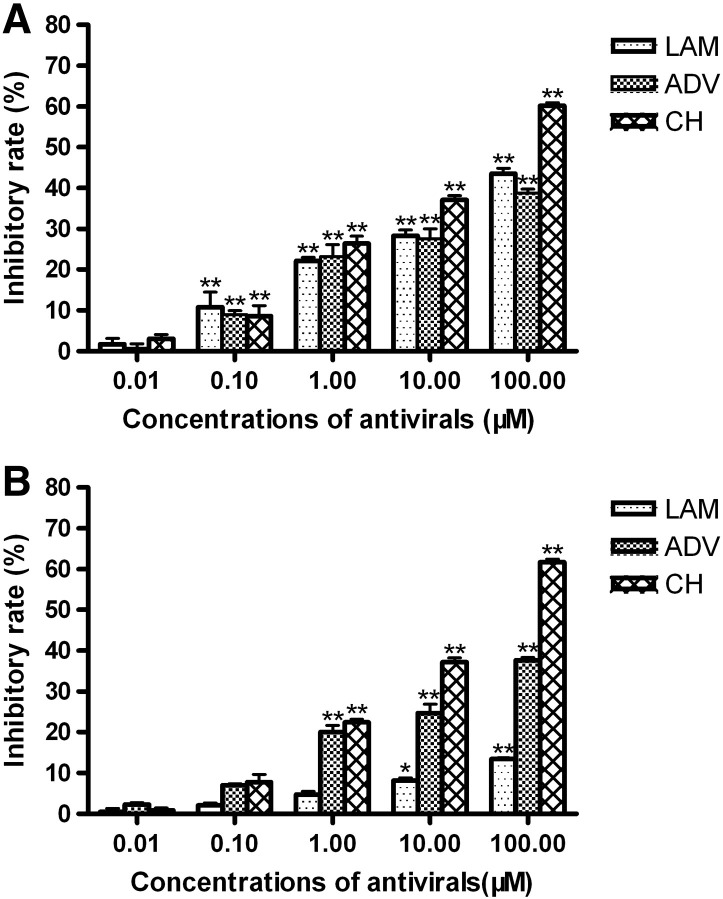
3.2. Effect of CH on antigen production from wild-type and lamivudine-resistant HBV
To assess the inhibitory efficacy of antivirals on HBV antigen production, HBsAg and HBeAg in culture medium were detected by ELISA after 6 days of continuous exposure to increasing concentrations of the antivirals. However, the level of HBsAg from HepG2 cells transfected with the rtV173L/L180M/M204V triple mutant was so low (data not shown), even in the drug-free group, that it was excluded from the antigen criterion. The antigen inhibitory efficiency of antivirals was assessed only based on HBeAg. As shown in Fig. 2A, CH, lamivudine and adefovir dose-dependently inhibited HBeAg production from wild-type HBV transfected cells. The IC50 for the inhibition of HBeAg production by CH was 31.89 ± 5.77 μM. However, neither lamivudine nor adefovir achieved 50% inhibition of HBeAg production, even at the concentration of 100 μM.
Fig. 2.
Effects of antivirals on HBeAg production from wild-type and lamivudine-resistant HBV. HepG2 cells were transiently transfected with the wild-type (A) or lamivudine-resistant (B) HBV genome. Twenty-four hours after transfection, the cells were treated with the indicated concentrations of lamivudine (LAM), adefovir (ADV) or cepharanthine hydrochloride (CH). After 6 days of treatment, HBeAg was detected in the cell culture supernatant using a specific ELISA kit. The experiments were performed in triplicate, and the data are presented as the means ± S.D. of three independent experiments. **P < 0.01, *P < 0.05 compared with the no drug control group.
The inhibitory efficiency of CH, lamivudine, and adefovir on HBeAg production from the lamivudine-resistant HBV mutant was also determined. As expected, lamivudine was not as active on the lamivudine-resistant HBV mutant as it was on wild-type HBV. However, CH caused a similar inhibition of HBeAg production from the lamivudine-resistant HBV (Fig. 2B), indicating that CH was equally effective as an inhibitor against HBeAg expression by lamivudine-resistant HBV as it was on the wild-type virus. After 6 days of treatment with adefovir, the same dose-dependent inhibition of HBeAg production was also observed. It is noteworthy that adefovir showed a relatively weaker inhibition on HBeAg production compared with CH.
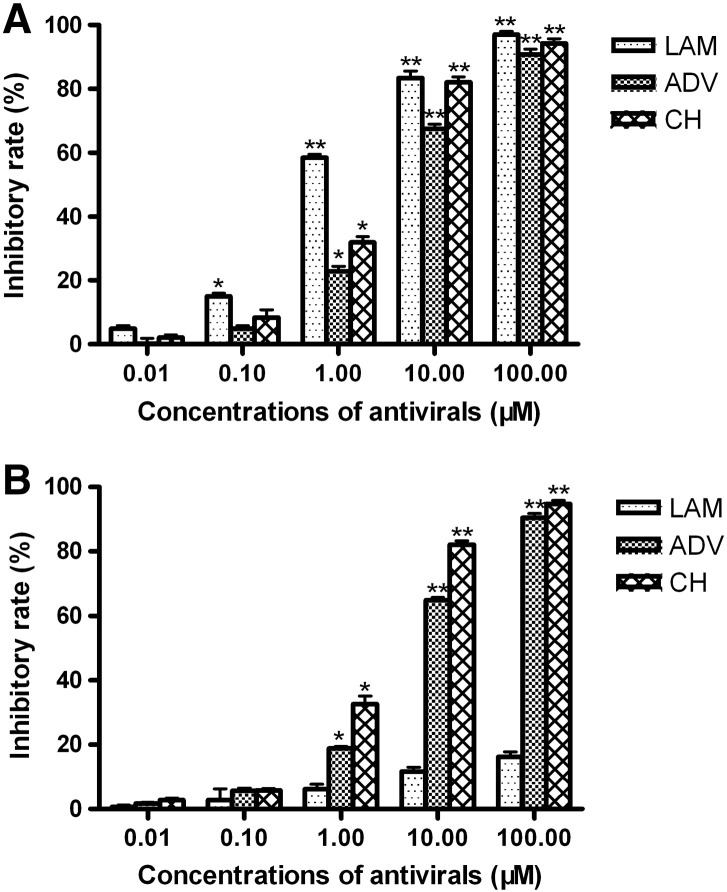
3.3. Effect of CH on viral replication of wild-type and lamivudine-resistant HBV
To evaluate the inhibitory potency of antivirals on HBV replication, intracellular HBV DNA was extracted and submitted to real-time PCR analysis at the end of treatment. As demonstrated in Fig. 3A, consistent with the inhibitory effect on HBeAg production, CH, lamivudine and adefovir inhibited the replication of wild-type HBV in a dose-dependent manner. The most potent inhibition was observed with lamivudine (IC50 = 0.82 ± 0.05 μM), followed by CH (IC50 = 2.14 ± 0.78 μM) and adefovir (IC50 = 4.23 ± 0.32 μM).
Fig. 3.
Inhibitory effects of antivirals on the viral replication of wild-type and lamivudine-resistant HBV. HepG2 cells were transiently transfected with wild-type (A) or lamivudine-resistant (B) HBV genome. Twenty-four hours after transfection, the cultures were treated with the indicated concentrations of lamivudine (LAM), adefovir (ADV) or cepharanthine hydrochloride (CH). After 6 days of treatment, viral DNA was extracted from the cultured cells and quantified by real-time quantitative PCR using a commercially available kit. The experiments were performed in triplicate, and the data are presented as the means ± S.D. of three independent experiments. **P < 0.01, *P < 0.05 compared with the no drug control group.
With respect to lamivudine-resistant HBV mutants, lamivudine was not active on the rtV173L/L180M/M204V triple mutant, with a resistance factor of > 120 (IC50 > 100 μM) compared with the wild-type HBV strain. However, exposure to CH or adefovir produced dose-dependent inhibition of the replication of the mutant HBV (Fig. 3B), with IC50 of 2.1 ± 0.39 μM and 4.88 ± 0.55 μM, respectively.
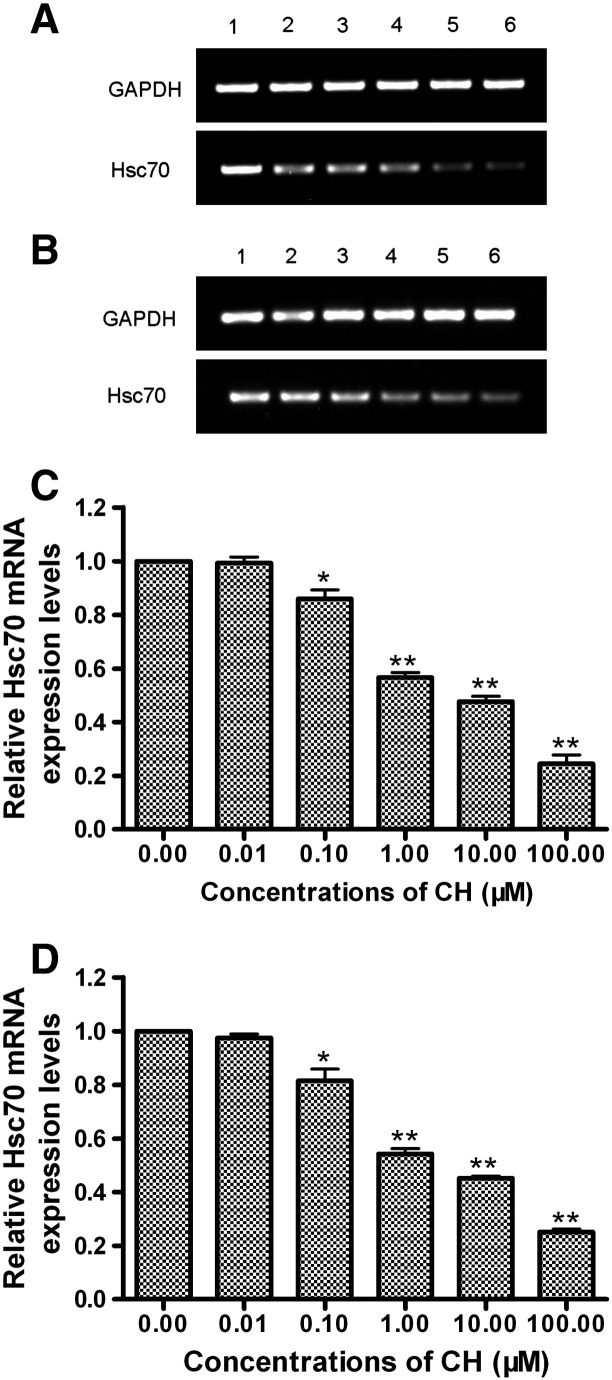
3.4. Effect of CH on host Hsc70 mRNA
After exposure to increasing concentrations of CH for 6 days, the amount of intracellular Hsc70 mRNA was also determined by RT-PCR. As shown in Fig. 4 , in comparison to the drug-free group, the level of Hsc70 mRNA in CH-treated cells transfected with either the wild-type or mutated HBV genome decreased in a dose-dependent manner, which paralleled the reduction of intracellular HBV DNA. It is worth noting that, after exposure to the same concentration of CH, there is no significant difference in the level of Hsc70 mRNA between wild-type HBV-transfected cells and lamivudine-resistant HBV-transfected cells (P > 0.05).
Fig. 4.
Effect of CH on host Hsc70 mRNA. HepG2 cells were transiently transfected with the wild-type or lamivudine-resistant HBV genome and then treated with cepharanthine hydrochloride (CH) at concentrations of 0 (1), 0.01 (2), 0.1 (3), 1 (4), 10 (5) or 100 (6) μM for 6 days. At the end of treatment, the total RNA was extracted, and heat stress cognate 70 (Hsc70) mRNA was determined by RT-PCR (A and B). The levels of Hsc70 mRNA were quantified and normalized relative to the internal reference GAPDH mRNA (C and D). The experiments were performed in triplicate, and a representative set of data is presented. **P < 0.01, *P < 0.05 compared with the no drug control group.
4. Discussion
The emergence of HBV strains resistant to antiviral treatments is a major clinical concern. With the expanding use and prolonged administration of lamivudine, rtV173L/L180M/M204V triple mutant, in which rtV173L and rtL180M act as compensatory mutations partially restoring the replicative capacity of rtM204V mutation strains, were selected more and more frequently and became the next most common mutation profile associated with lamivudine resistance (Westland et al., 2005). One alternative that would delay or overcome the occurrence of drug-resistant mutants is to switch to or add novel drugs that do not share the same resistance profiles. Many natural herbs and related active compounds have been reported to have promising, distinctive and potent anti-HBV activities. In this study, based on the in vitro cell transfection system, we assessed the antiviral activity of CH, a natural alkaloid-derived compound, against wild-type and lamivudine-resistant HBV clinical isolates. The preliminary mechanism of action of CH was also explored.
Due to the lack of a proofreading function of HBV polymerase, combined with the high level viral replication in infected liver cells of chronic hepatitis B patients, it is estimated that 1010 base-pairing errors occur daily (Doo and Liang, 2001). Consequently, HBV in chronically infected patients harbor many virus quasispecies which contain a diversity of genetic context. Presently, the in vitro drug susceptibility assessments of HBV mutants commonly depend on the methods that artificially reproduce one or a few resistant mutations, usually by site-directed mutagenesis of a laboratory strain, on a wild-type virus backbone (Brunelle et al., 2006, Jacquard et al., 2006). However, viruses created by the site-directed mutagenesis of a laboratory strain would not contain the natural genetic context of a mutation identified in clinical strains, and discrepancies between the susceptibilities to antivirals of laboratory- and patient-derived HBV mutants will emerge (Brunelle et al., 2007). Therefore, phenotypic analysis of HBV clinical mutants isolated directly from the sera of patients would offer more relevant and accurate information than that obtained from testing viruses with mutations introduced into laboratory strains.
In this report, a previously reported expression vector for cloning the entire HBV genome was used to facilitate the replication and gene expression of full-length clinical HBV isolates. The novel plasmid pHY106 contains 180 bp of HBV sequences, which are highly conserved among various HBV genotypes, and contains two SapI sites, allowing insertion of the SapI treated PCR-amplified HBV genome, leading to a 1.1-unit length of HBV genome which is necessary and sufficient to enable the synthesis of full-length HBV pregenomic RNA (pgRNA) required to trigger the intracellular HBV cycle (Seeger and Mason, 2000). In the present study, the full-length HBV genome, amplified with high-fidelity PCR polymerase from the serum of a chronic hepatitis B patient who had developed resistance to lamivudine, was cloned to pHY106 and used for drugs susceptibility testing. The sequences of our individual clone matched that of its respective patient serum HBV, indicating that the constructed individual clone represented the dominant serum HBV quasispecies population. Thus, the drug susceptibility results obtained in this report would precisely reflect those of the serum HBV itself.
In the HBV genome, the polymerase gene overlaps the surface antigen gene. As a result, mutations in the RT domain might affect the production of the HBsAg protein by introducing a stop codon into the S open reading frame (ORF) (Pollicino et al., 2009, Wakil et al., 2002). In the present study, after transient transfection with the rtV173L/L180M/M204V triple mutant, HepG2 cells secreted HBsAg at an extremely low level, even in the no drug control group. Thus, HBsAg was excluded from the antigen criterion for evaluating the susceptibility of the triple mutant to antivirals. The antigen inhibitory efficiency of antivirals was assessed based only on HBeAg production.
We recently assessed the in vitro potency of CH for the inhibition of wild-type HBV in a stably expressing HBV cell line HepG2.2.15. In the present study, we confirmed the findings of previous studies, which showed that CH is a potent inhibitor of wild-type HBV in vitro. In HepG2 cells transiently transfected with the wild-type HBV genome, CH inhibited HBV replication and HBeAg expression more efficiently than adefovir, while lamivudine displayed the most potent antiviral activity. Moreover, we provided new information that showed that CH inhibited the replication and HBeAg production of clinical lamivudine-resistant HBV isolates almost as efficiently as it did that of wild-type HBV. The in vitro cross-resistance profile of CH for the lamivudine-resistant variant studied here proved to be more favorable than that of lamivudine and comparable to that of adefovir.
Of course, the in vitro therapeutic potency of a drug does not depend only on its antiviral capacity. Its cytotoxic effect also has to be taken into account, since the selectivity index (IC50/CC50) of a drug may prevent the use of optimal dose to reach a more potent antiviral effect. Interestingly, the cytotoxicity assay indicated that CH and adefovir had similar cytotoxicity to HepG2 cells. Thus, in combination with the antiviral capacity profile of compounds tested, it can be concluded that CH has more favorable therapeutic potency than adefovir.
Although more and more natural herbs and related active compounds have been used for chronic hepatitis B treatment, the mechanisms of action of most of the compounds remain unclear. Recently, researchers have found that Hsc70 is a host protein associated with HBV replication and could be therapeutic target of some natural anti-HBV compounds (Wang et al., 2010, Wang et al., 2011). To gain new insights into the mechanism of inhibition of HBV by CH, we assessed the effect of in vitro CH treatment on host Hsc70 mRNA by RT-PCR. The results showed that CH inhibited host Hsc70 mRNA expression in parallel with the inhibitory effect on intracellular HBV replication, illustrating that CH may suppress HBV via downregulation of host Hsc70 expression. We also investigated the potential influence of the knockdown of the Hsc70 mRNA on the host cells. Interestingly, the reduction of Hsc70 mRNA by CH did not cause apparent negative effects on the growth of human HepG2 cells (unpublished observations). Nevertheless, the downregulation of the protein and the exact mechanism of the downregulation of Hsc70 by CH deserve further studies. Furthermore, the effects of CH on other ATP-binding protein of the heat stress protein like Hsp90 or chaperone proteins like p23 Hsp40 or Hop involved in HBV replication also merit investigations.
In conclusion, our findings indicate that CH is a potent inhibitor of clinical wild-type and lamivudine-resistant HBV isolates and deserves further investigation. This compound may be a new alternative candidate for the treatment of chronic hepatitis B patients who have developed resistance to lamivudine. Furthermore, CH might also be valuable for combination therapies with approved nucleos(t)ide analogs to prevent or delay the emergence of drug-resistant mutants in chronically HBV-infected patients.
Acknowledgments
This work was supported by Natural Science Foundation of Henan Province of China (No. 092300410107). We thank William Delaney and Huiling Yang from Gilead Sciences for providing pHY106 plasmid. We appreciate Prof. Lexun Xue from Laboratory for Cell Biology, Zhengzhou University for critical reading of the manuscript.
References
- Allen M.I., Deslauriers M., Andrews C.W., Tipples G.A., Walters K.A., Tyrrell D.L., Brown N., Condreay L.D. Identification and characterization of mutations in hepatitis B virus resistant to lamivudine. Lamivudine Clinical Investigation Group. Hepatology. 1998;27:1670–1677. doi: 10.1002/hep.510270628. [DOI] [PubMed] [Google Scholar]
- Baba M., Okamoto M., Kashiwaba N., Ono M. Anti-HIV-1 activity and structure–activity relationship of cepharanoline derivatives in chronically infected cells. Antivir. Chem. Chemother. 2001;12:307–312. doi: 10.1177/095632020101200506. [DOI] [PubMed] [Google Scholar]
- Brunelle M.N., Jacquard A.C., Pichoud C., Durantel D., Carrouée-Durantel S., Villeneuve J.P., Trépo C., Zoulim F. Susceptibility to antivirals of a human HBV strain with mutations conferring resistance to both lamivudine and adefovir. Hepatology. 2006;41:1391–1398. doi: 10.1002/hep.20723. [DOI] [PubMed] [Google Scholar]
- Brunelle M.N., Lucifora J., Neyts J., Villet S., Holy A., Trepo C., Zoulim F. In vitro activity of 2,4-diamino-6-[2-(phosphonomethoxy)ethoxy]-pyrimidine against multidrug-resistant hepatitis B virus mutants. Antimicrob. Agents Chemother. 2007;51:2240–2243. doi: 10.1128/AAC.01440-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui X., Wang Y., Kokudo N., Fang D., Tang W. Traditional Chinese medicine and related active compounds against hepatitis B virus infection. Biosci. Trends. 2010;4:39–47. [PubMed] [Google Scholar]
- Delaney W.E., 4th, Yang H., Westland C.E., Das K., Arnold E., Gibbs C.S., Miller M.D., Xiong S. The hepatitis B virus polymerase mutation rtV173L is selected during lamivudine therapy and enhances viral replication in vitro. J. Virol. 2003;77:11833–11841. doi: 10.1128/JVI.77.21.11833-11841.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doo E., Liang T.J. Molecular anatomy and pathophysiologic implications of drug resistance in hepatitis B virus infection. Gastroenterology. 2001;120:1000–1008. doi: 10.1053/gast.2001.22454. [DOI] [PubMed] [Google Scholar]
- Enomoto M., Tamori A., Kohmoto M.T., Morikawa H., Habu D., Sakaguchi H., Takeda T., Seki S., Kawada N., Shiomi S., Nishiguchi S. Mutational patterns of hepatitis B virus genome and clinical outcomes after emergence of drug-resistant variants during lamivudine therapy: analyses of the polymerase gene and full-length sequences. J. Med. Virol. 2007;79:1664–1670. doi: 10.1002/jmv.20984. [DOI] [PubMed] [Google Scholar]
- Günther S., Li B.C., Miska S., Krüger D.H., Meisel H., Will H. A novel method for efficient amplification of whole hepatitis B virus genomes permits rapid functional analysis and reveals deletion mutants in immunosuppressed patients. J. Virol. 1995;69:5437–5444. doi: 10.1128/jvi.69.9.5437-5444.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y.J., Zhao L., Li X.F., Mei Y.W., Zhang S.L., Tao J.Y., Zhou Y., Dong J.H. Effect of Corilagin on anti-inflammation in HSV-1 encephalitis and HSV-1 infected microglias. Eur. J. Pharmacol. 2010;635:79–86. doi: 10.1016/j.ejphar.2010.02.049. [DOI] [PubMed] [Google Scholar]
- Hongthanakorn C., Chotiyaputta W., Oberhelman K., Fontana R.J., Marrero J.A., Licari T., Lok A.S. Virological breakthrough and resistance in patients with chronic hepatitis B receiving nucleos(t)ide analogues in clinical practice. Hepatology. 2011;53:1854–1863. doi: 10.1002/hep.24318. [DOI] [PubMed] [Google Scholar]
- Jacquard A.C., Brunelle M.N., Pichoud C., Durantel D., Carrouée-Durantel S., Trepo C., Zoulim F. In vitro characterization of the anti-hepatitis B virus activity and cross-resistance profile of 2′,3′-dideoxy-3′-fluoroguanosine. Antimicrob. Agents Chemother. 2006;50:955–961. doi: 10.1128/AAC.50.3.955-961.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lada O., Benhamou Y., Cahour A., Katlama C., Poynard T., Thibault V. In vitro susceptibility of lamivudine-resistant hepatitis B virus to adefovir and tenofovir. Antivir. Ther. 2004;9:353–363. [PubMed] [Google Scholar]
- Liu X.J., Wang Y.F., Zhang M.Y., Li G.S., Cen Y.Z. Study on the inhibitory effect of cepharanthine on herpes simplex type-1 virus (HSV-1) in vitro. J. Chin. Med. Mater. 2004;27:107–110. [PubMed] [Google Scholar]
- Pollicino T., Isgrò G., Di Stefano R., Ferraro D., Maimone S., Brancatelli S., Squadrito G., Di Marco V., Craxì A., Raimondo G. Variability of reverse transcriptase and overlapping S gene in hepatitis B virus isolates from untreated and lamivudine-resistant chronic hepatitis B patients. Antivir. Ther. 2009;14:649–654. [PubMed] [Google Scholar]
- Rogosnitzky M., Danks R. Therapeutic potential of the biscoclaurine alkaloid, cepharanthine, for a range of clinical conditions. Pharmacol. Rep. 2011;63:337–347. doi: 10.1016/s1734-1140(11)70500-x. [DOI] [PubMed] [Google Scholar]
- Seeger C., Mason W.S. Hepatitis B virus biology. Microbiol. Mol. Biol. Rev. 2000;64:51–68. doi: 10.1128/mmbr.64.1.51-68.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki F., Akuta N., Suzuki Y., Sezaki H., Arase Y., Hosaka T., Someya T., Kobayashi M., Saitoh S., Ikeda K., Kobayashi M., Matsuda M., Satoh J., Watahiki S., Kumada H. Clinical and virological features of non-breakthrough and severe exacerbation due to lamivudine-resistant hepatitis B virus mutants. J. Med. Virol. 2006;78:341–352. doi: 10.1002/jmv.20546. [DOI] [PubMed] [Google Scholar]
- Wakil S.M., Kazim S.N., Khan L.A., Raisuddin S., Parvez M.K., Guptan R.C., Thakur V., Hasnain S.E., Sarin S.K. Prevalence and profile of mutations associated with lamivudine therapy in Indian patients with chronic hepatitis B in the surface and polymerase genes of hepatitis B virus. J. Med. Virol. 2002;68:311–318. doi: 10.1002/jmv.10205. [DOI] [PubMed] [Google Scholar]
- Wang Y.P., Liu F., He H.W., Han Y.X., Peng Z.G., Li B.W., You X.F., Song D.Q., Li Z.R., Yu L.Y., Cen S., Hong B., Sun C.H., Zhao L.X., Kreiswirth B., Perlin D., Shao R.G., Jiang J.D. Heat stress cognate 70 host protein as a potential drug target against drug resistance in hepatitis B virus. Antimicrob. Agents Chemother. 2010;54:2070–2077. doi: 10.1128/AAC.01764-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y.P., Zhao W., Xue R., Zhou Z.X., Liu F., Han Y.X., Ren G., Peng Z.G., Cen S., Chen H.S., Li Y.H., Jiang J.D. Oxymatrine inhibits hepatitis B infection with an advantage of overcoming drug-resistance. Antiviral Res. 2011;89:227–231. doi: 10.1016/j.antiviral.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Westland C.E., Yang H., Delaney W.E., 4th, Wulfsohn M., Lama N., Gibbs C.S., Miller M.D., Fry J., Brosgart C.L., Schiff E.R., Xiong S. Activity of adefovir dipivoxil against all patterns of lamivudine-resistant hepatitis B viruses in patients. J. Viral Hepat. 2005;12:67–73. doi: 10.1111/j.1365-2893.2005.00578.x. [DOI] [PubMed] [Google Scholar]
- Yang H., Westland C., Xiong S., Delaney W.E., 4th In vitro antiviral susceptibility of full-length clinical hepatitis B virus isolates cloned with a novel expression vector. Antiviral Res. 2004;61:27–36. doi: 10.1016/j.antiviral.2003.07.003. [DOI] [PubMed] [Google Scholar]
- Yuen M.F., Lai C.L. Treatment of chronic hepatitis B: evolution over two decades. J. Gastroenterol. Hepatol. 2011;26:138–143. doi: 10.1111/j.1440-1746.2010.06545.x. [DOI] [PubMed] [Google Scholar]
- Yuen M.F., Fung J., Wong D.K., Lai C.L. Prevention and management of drug resistance for antihepatitis B treatment. Lancet Infect. Dis. 2009;9:256–264. doi: 10.1016/S1473-3099(09)70056-8. [DOI] [PubMed] [Google Scholar]
- Zhang C.H., Wang Y.F., Liu X.J., Lu J.H., Qian C.W., Wan Z.Y., Yan X.G., Zheng H.Y., Zhang M.Y., Xiong S., Li J.X., Qi S.Y. Antiviral activity of cepharanthine against severe acute respiratory syndrome coronavirus in vitro. Chin. Med. J. (Engl). 2005;118:493–496. [PubMed] [Google Scholar]