Abstract
The presence of patients with diverse pathologies in hospitals results in an environment that can be rich in various microorganisms including respiratory and enteric viruses, leading to outbreaks in hospitals or spillover infections to the community. All hospital patients are at risk of nosocomial viral infections, but vulnerable groups such as older adults, children and immuno-compromised/-suppressed patients are at particular risk of severe outcomes including prolonged hospitalization or death. These pathogens could transmit through direct or indirect physical contact, droplets or aerosols, with increasing evidence suggesting the importance of aerosol transmission in nosocomial infections of respiratory and enteric viruses. Factors affecting the propensity to transmit and the severity of disease transmitted via the aerosol route include the biological characteristics affecting infectivity of the viruses and susceptibility of the host, the physical properties of aerosol particles, and the environmental stresses that alter these properties such as temperature and humidity. Non-specific systematic and individual-based interventions designed to mitigate the aerosol route are available although empirical evidence of their effectiveness in controlling transmission of respiratory and enteric viruses in healthcare settings are sparse. The relative importance of aerosol transmission in healthcare setting is still an on-going debate, with particular challenge being the recovery of infectious viral bioaerosols from real-life settings and the difficulty in delineating transmission events that may also be a result of other modes of transmission. For the prevention and control of nosocomial infections via the aerosol route, more research is needed on identifying settings, medical procedures or equipment that may be associated with an increased risk of aerosol transmission, including defining which procedures are aerosol-generating; and on the effectiveness of systematic interventions on aerosol transmission of respiratory and enteric viruses in healthcare settings.
Keywords: Nosocomial infections, Viral aerosols, Aerosols, Prevention and control
Highlights
-
•
Respiratory viruses have been recovered in the air in hospitals despite existing systematic and personal level interventions.
-
•
Studies on the relative contribution of different routes of transmission for respiratory and enteric viruses are lacking.
-
•
Physical filtration efficiencies may not directly translate to effectiveness in mitigating virus transmission.
-
•
More effectiveness studies with biological measures (e.g. viral load and infection events) as outcomes are needed.
1. Introduction
Infections that spread predominantly in healthcare settings pose potential threats to public health, and cause considerable morbidity each year. Occasionally emerging infectious diseases cause community infections and major social disruption after initial spread in hospitals, for example the severe acute respiratory syndrome (SARS) outbreaks in 2003, the outbreak of Ebola virus disease (EVD) in West Africa in 2014-15, and the recent Middle East respiratory syndrome (MERS) outbreaks in the Middle East and South Korea (Ansumana et al., 2017, Ho et al., 2003, Ki, 2015). Nosocomial infections may lead to outbreaks among patients and healthcare workers, and may even spillover to the local community when visitors are infected, leading to prolonged hospitalization and increased mortality in hospital patients and increased medical costs in the community. In healthcare settings, respiratory and enteric bacteria and viruses can be transmitted through direct or indirect physical contact (fomites), or through the air as respiratory droplets or droplet nuclei (also referred to as aerosols). There are wide range of systematic and individual-based interventions attempted to mitigate aerosol transmission in healthcare settings.
The purpose of this article is to review the burden of nosocomial infections of respiratory and enteric viruses, studies and methodologies employed to investigate the role of aerosol transmission in nosocomial infections, and prevention and control measures that could mitigate viral aerosols in healthcare settings. We also discuss the challenges and research gaps in studying the importance of aerosol transmission of respiratory and enteric viruses in healthcare settings.
2. Nosocomial infections of respiratory and enteric pathogens in hospitals
2.1. Definition of nosocomial infections
Health care-associated infection (HCAI), also known as nosocomial infection, is defined as ‘an infection occurring in a patient during the process of care in a hospital or other health-care facility which was not present or incubating at the time of admission. This includes infections acquired in the hospital, but appearing after discharge, and also occupational infections among staff of the facility (Benenson, 1995). It is traditionally believed that most HCAIs become apparent at least 48 h after admission to the healthcare facilities (Horan et al., 2008, World Health Organization, 2011), but this definition may not apply to viral infections that have longer mean incubation periods for example measles (12.5 days), adenoviruses (5.6 days), respiratory syncytial virus (RSV, 4.4 days), SARS (4.0 days) and other human coronaviruses (3.2 days), and parainfluenza virus (2.6 days) (Lessler et al., 2009). Theoretically patients (hospitalized or outpatient), healthcare workers (HCWs) and visitors such as the family members of hospitalized patients can all acquire nosocomial infection, but it is more difficult to ascertain nosocomial infections in outpatients and visitors as they could also acquire the infection from the community (Aitken & Jeffries, 2001). Therefore, studies of nosocomial infections mostly focus on infections developed in hospitalized patients or HCWs.
The most frequent HCAIs include urinary tract infections (UTI), surgical site infections (SSI), bloodstream infections (BSI) and hospital-acquired pneumonia (Allegranzi et al., 2011, World Health Organization, 2011) that are device-associated and acquired independently during medical procedures, although transmission of pathogens between patients in the hospital is also considered to contribute considerably to the burden of nosocomial infections (Valenti, Menegus, Hall, Pincus, & Douglas, 1980) with occasional outbreaks of different respiratory and enteric viruses in hospitals (Bobo & Dubberke, 2010). Note that for the group of patients who may acquire pneumonia by attending a hemodialysis clinic or long-term care facilities, which was previously denoted as healthcare-associated pneumonia, it has now been denoted as community-acquired pneumonia by the latest patient management guidelines from the Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) (American Thoracic Society, 2005, Kalil et al., 2016).
2.2. Burden and significance of nosocomial respiratory and enteric viral infections
In a detailed report by the World Health Organization on the worldwide burden of endemic HCAIs, the worldwide HCAI prevalence was 15.5% and HCAIs were more than twice as common in low- and middle-income countries (LMICs) compared to high-income countries (Ling et al., 2015, World Health Organization, 2011). In both high-income and LMIC settings, there is a considerable burden in hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP), and patients admitted to emergency and intensive care unit (ICU) and those with impaired functional status are associated with more nosocomial infections (World Health Organization, 2011). In LMICs, infants less than one year of age or patients with multiple comorbidities are also at higher risk of nosocomial infections (World Health Organization, 2011). In China, it has been reported that 16.2% of ICU patients developed ICU-acquired pneumonia with a mortality rate of 37% (Zhang et al., 2014).
Viruses are considered as the most common cause of infectious diseases acquired within indoor environments (Brankston, Gitterman, Hirji, Lemieux, & Gardam, 2007), and many nosocomial infections are due to respiratory and enteric infections of viruses (Belliot et al., 2014, Bruijning-Verhagen et al., 2012, Kambhampati et al., 2015, Rhinehart et al., 2012). Recent examples of particular concern are emerging infectious diseases such as SARS outbreaks in 2003, the outbreak of EVD in West Africa in 2014-15, and the on-going MERS outbreaks in the Middle East since 2012, where many HCWs were infected and acted as the amplifiers for the spread to the community (Ansumana et al., 2017, Ho et al., 2003, Ki, 2015, Shears and O'Dempsey, 2015). For human avian influenza viruses, although no strong evidence of human-to-human transmission has been reported for the highly pathogenic avian influenza (HPAI) A(H5N1) virus, there have been reports suggesting nosocomial transmission of avian influenza A(H7N9) virus, potentially through aerosols or droplets (Chen et al., 2016, Fang et al., 2015). Infections among HCWs also significantly impeded outbreak controls (Chan, 2014). On the other hand, endemic respiratory and enteric viruses also cause hospital outbreaks regularly. Human seasonal influenza viruses are a common cause of respiratory tract infections both in the community and in hospitals. Salgado, Farr, Hall, and Hayden (2002) reviewed 12 influenza outbreaks in hospitals, and reported the patient infection rates ranged from 3% to 50% in wards affected by the outbreaks compared to 0.7–20% throughout the hospital. Outbreaks of influenza B virus have also been reported in hospitalized older adults (Seale et al., 2009, Van Voris et al., 1982). Other respiratory viruses including adenovirus, rhino/enterovirus, metapneumovirus and RSV could also cause nosocomial infections in pediatric and adult patients (Chow and Mermel, 2017, La Rosa et al., 2013, Sakata et al., 1998, Silva Cde et al., 2012, Yang et al., 2014). We previously reported an outbreak of human metapneumovirus in a hospital ward with bedridden patients with severe motor-and-intellectual disabilities (Yang et al., 2014). For enteric infections, based on the data captured by a German surveillance system, 49% of the norovirus-related and 14% of rotavirus-related hospitalizations were acquired nosocomially, with 65% and 41% in older adults, and 16% and 16% in infants less than one year of age for nosocomial norovirus and rotavirus infections respectively (Lindsay et al., 2015, Spackova et al., 2010). Nosocomial outbreaks of rotaviruses and noroviruses also happened frequently (Bruijning-Verhagen et al., 2012, Kambhampati et al., 2015, Rhinehart et al., 2012). In addition to those mentioned above, other respiratory and enteric viruses such as measles virus and varicella-zoster virus can also cause epidemics in hospitals through airborne transmission, which often leads to serious consequences (Aitken and Jeffries, 2001, Herfst et al., 2016).
Apart from a higher risk of infection, vulnerable groups such as older adults, children, cancer patients, patients undergoing major surgery, and immunocompromised or immunosuppressed patients are susceptible to more severe disease after acquiring nosocomial infection, as the infection may cause deterioration of the patients’ primary disease including prolonged hospital stay, complications and even death. For example, the mortality due to influenza was 33–60% in transplant or ICU patients compared to 16% in patients in acute-care facilities and geriatric hospitals, and pneumonia and death were common complications of influenza in children, transplant and cancer patients undergoing immunosuppressive treatment (Salgado et al., 2002). Álvarez-Lerma et al. (2017) reported ICU patients with hospital-acquired influenza A (H1N1)pdm09 virus infection was associated with higher risk of death than those acquired the infection from the community. A prospective observational cohort study of ventilated children with RSV infection showed that there was an increase in mortality of children patients that acquired RSV infection in pediatric ICUs (26%) or hospital wards (29%), compared to 4% in ventilated children with community-acquired RSV infection (Thorburn, Eisenhut, & Riordan, 2012).
3. Aerosol transmission of respiratory and enteric infections in healthcare settings
3.1. Modes of transmission in healthcare settings
Pathogenic microorganisms can be transmitted through direct or indirect physical contact, or through the air in respiratory droplets and aerosols (Siegel, Rhinehart, Jackson, & Chiarello, 2007), leading to cross-infections or outbreaks in hospitals. Different transmission routes could also interplay with each other. For example, on one hand, inanimate objects contaminated with pathogens from patients’ secretions such as saliva, nasal fluid and feces (fomites) can serve as vehicles for the spread of pathogens directly, contributing to indirect contact transmission (Mubareka et al., 2009); on the other hand, disturbance to fomites (e.g. by toilet flushing) leads to resuspension and generation of contaminated aerosols (La Rosa et al., 2013), contributing to aerosol transmission. In general, viruses infected with aerosol exposure seem to have greater replication efficiency in vivo, such as influenza viruses (Zhang et al., 2017).
Aerosol transmission refers to the dissemination of either droplet nuclei or small particles (aerosols) in the respirable size range containing pathogenic microorganisms that remain infective over time and distance (Siegel et al., 2007). In contrast, droplet transmission occurs when larger particles containing pathogenic microorganisms travel through the air in short distances (unusually suggested as within 1 m / 3 feet) (World Health Organization, 2014) to the mouth, nasal mucosa, ocular conjunctiva or other parts of the susceptible population. To classify between droplet and aerosol transmission, respiratory droplets are typically defined as particles with an aerodynamic diameter > 5 µm, and aerosols as those ≤ 5 µm, since the latter is believed to be deposited in the alveolar region of human lung by settlement (Duguid, 1946, Siegel et al., 2007). Larger inhaled particles (mainly droplets) will deposit in the head airway or trachea-bronchial regions of the respiratory tract, whereas smaller particles (mainly aerosols or droplet nuclei) will primarily deposit in the alveoli (Hinds, 1999, Jones and Brosseau, 2015). However, the proportion of particles that are inhaled and deposit in different regions of the respiratory tract (and therefore classified as via the droplet or aerosol route accordingly) are determined by particle aerodynamic diameter as well as lung morphology and breathing characteristics (Nazaroff, 2016). Separately, some define aerosols as those which can remain suspended in the air for prolonged periods of time with potentially a higher risk of transmission through the air. Particles with aerodynamic diameter around 20 µm take 4 min to fall for a vertical distance of 3 m and those around 5 µm take an hour to fall for the same height (Knight, 1980, Tellier, 2009). Furthermore, respiratory droplets < 20 µm at expulsion could transform into droplet nuclei by evaporation and shrinks to a little less than half of the initial diameter (Nicas et al., 2005, Tellier, 2009, Xie et al., 2007). Especially particles with aerodynamic diameter < 5 µm that can remain suspended in the air for prolonged periods (La Rosa et al., 2013). Bioaerosols are usually defined as aerosols or particulate matter of microbial, plant or animal origin that is often used synonymously with organic dust (Douwes et al., 2003, Tellier, 2009), which generally include bacteria, fungi, viruses and their derivatives such as endotoxin, glucans and mycotoxin (Guan and Yao, 2010) with particle size varying based on the composition of the aerosols, and could range from submicron for those composed of viral particles to as large as 1 mm for those composed of pollen grains (Haig, Mackay, Walker, & Williams, 2016).
In healthcare settings, infection prevention and control measures are often designed to act on particular modes of transmission, and pathogen-specific measures are recommended based on the understood mode(s) of transmission for the particular pathogen ( Table 1) (World Health Organization, 2014). Apart from the transmission results directly from other patients, the presence of patients with diversity in pathologies in hospital environments causes the floors, walls, surfaces of medical equipment and the air to be frequently contaminated with a range of pathogenic microorganisms including respiratory and enteric viruses, namely, MERS-CoV, rhinovirus, Toque teno virus, human adenovirus, rotaviruses, noroviruses et al. (Akhter et al., 1995, Ansari et al., 1991, Gallimore et al., 2008, Kim et al., 2016, Morter et al., 2011, Verani et al., 2014). In one instance, viruses could be recovered from 82% of the surfaces and 85% of air samples collected in a hospital (Verani et al., 2014).
Table 1.
Outline of the four different types of infection prevention and control (IPC) precautions in healthcare settings as recommended by the World Health Organization (2014).
| IPC precautions | Rationale | Measures | Examples |
|---|---|---|---|
| Standard | To minimize spread of infection associated with health care, via avoiding direct contact with patients’ blood, body fluids, secretions and non-intact skin | Hand hygiene, PPE, respiratory hygiene, environmental control, waste management and prevention of needle-stick/sharps injuries | Routine for all patients |
| Contact | Transmitted through contact particularly by hand contamination and self-inoculation into conjunctival or nasal mucosa | PPE (disposable gloves and gowns), specific patient placement and limited patient movement | Parainfluenza |
| Respiratory syncytial virus (RSV) | |||
| Droplet | Transmitted through large droplets which typically remain suspended in the air for a limited period of time and settle within 3 feet of the source | Use of face mask if working within 3 feet of the patients, specific patient placement (cohorting) and limited patient movement | Adenovirus |
| Avian influenza A(H5N1) | |||
| Human influenza | |||
| SARS-CoV | |||
| Airbornea | Transmitted through inhalation of droplet nuclei that remain infectious over a long distance (e.g. over 3 feet) | Requires special air handling including the use of respirators (e.g. N95), specific patient placement (in ventilated isolation rooms) and limited patient movement | SARS-CoV |
| Human influenza during aerosol-generating procedures (AGPs) |
This WHO infection control guideline defines airborne pathogens as those ‘transmitted through inhalation of droplet nuclei that remain infectious over a long distance (e.g. > 1 m), and require special air handling’, and therefore for the purpose of this article can be interpreted as ‘aerosol’.
In the paragraphs below, we will focus on the aerosol and droplet transmission of respiratory and enteric viruses in healthcare settings. Much of the discussion is illustrated using studies on influenza virus since it is one of the respiratory viruses most studied, however we expect the general principles also apply to other respiratory and enteric viruses.
3.2. Aerosol and droplet transmission of respiratory and enteric viruses
The presence of microorganisms in the air can affect the health of humans and animals. These pathogenic microorganisms are often adsorbed on the solid or liquid particles suspended in the air to form aerosols or droplets, whereas very small amounts of pathogenic microorganisms in the air are usually sufficient to cause infection compared to other modes of transmission (Alford, Kasel, Gerone, & Knight, 1966). For many respiratory viruses, the relative importance of different modes in transmission are controversial if not unknown, and can even vary within the same type of virus depending on the various viral, host and environmental factors (Branch-Elliman et al., 2015, Carlson et al., 2010, Gautret et al., 2014). However, in general, respiratory viruses considered to be transmitted mainly through droplets include SARS coronavirus (SARS-CoV), influenza virus, adenovirus, rhinovirus, RSV and parainfluenza virus, and viruses considered to be transmitted mainly through aerosols include measles (rubeola virus) and chickenpox (varicella-zoster virus) (Hall, 2000, Hall, 1982, Tang et al., 2006, Xie et al., 2007), in addition to other modes such as direct or indirect contact (fomite) transmission (Boone and Gerba, 2007, Pica and Bouvier, 2012). One study showed that a large community outbreak in SARS in Hong Kong could be explained by aerosol transmission (Yu et al., 2004), while another study showed that environmental surfaces in the hospitals could be contaminated with SARS-CoV and therefore contact transmission was considered possible (Dowell et al., 2004). It has been suggested that respiratory transmission of Ebola viruses could occur, although this is controversial (Osterholm et al., 2015, Vetter et al., 2016). Several experimental studies indicate that EBOV can be transmitted through aerosols in various animal species (Jaax et al., 1995, Weingartl et al., 2012). In addition to respiratory viruses, some enteroviruses can also be spread by airborne transmission through aerosol particles. For example, the main symptom of noroviruses infections is vomiting, a fine mist of virus particles passes into the air because of projectile vomiting. Droplets being inhaled by anyone in the immediate vicinity can be deposited in the upper respiratory tract, and subsequently be swallowed along with respiratory mucus (Bonifait et al., 2015). The evidences supporting the relative importance of different modes of transmission for respiratory and enteric viruses are summarized in Table 2. Additional discussion on modes of transmissions of these viruses can be found in the review by La Rosa et al. (2013).
Table 2.
Relative importance of aerosol, droplet and indirect contact transmission for common respiratory and enteric viruses transmitted in healthcare settings. Direct contact is not included in this table since most of the research is focused on the possibilities of transmission through these other mechanisms requiring an intermediate medium. Perceived relative importance of the different routes of transmission is indicated for each virus (+++, most important; +, least important). Other modes of transmission include bloodborne, fecal-oral, waterborne and foodborne. Summarized from the review done by La Rosa et al. (2013) and additional references.
3.3. Factors affecting airborne transmission in nosocomial settings
Aerosol transmission of viruses can be affected by many factors, such as the mass, diameter and the shape of the aerosol particles (Hinds, 2012). In addition to these physical parameters of aerosol particles, the properties of the viruses, environmental factors and susceptibility of the host can also affect the probability of infection being established from aerosol transmission ( Table 3). On the other hand, one could also hypothesize which factors may be involved and their effects on aerosol transmission by looking at their roles on different stages of aerosol transmission, namely 1) release of viral particles from infected individuals, 2) the transport of virus-laden particles in the air, and 3) entry and deposition of virus-laden particles in susceptible host.
Table 3.
Factors affecting risk of infection and severity of disease in airborne transmission of respiratory and enteric viruses in healthcare settings. In the table, we use influenza as a model to describe factors that could affect the transmissibility and severity of disease of aerosol transmission.
| Factors | Roles in transmission | References |
|---|---|---|
| Virus | ||
| Molecular structure | Balance of different viral surface proteins affect transmission efficiency via different routes. Survival of enveloped viruses is longer at lower relative humidity (20%−30%), while survival of non-enveloped viruses is longer at higher relative humidity (70%−90%). | Yen et al. (2011); Tang (2009) |
| Dose | Minimal infectious doses required to initiate infection are different across different viruses. | Franz et al. (1997) |
| Host | ||
| Behavior | As source, difference in frequency of coughing or sneezing could affect the total viral load released. On the other hand, it is hypothesized that bioaerosols generated during sneezing mostly originated from the nasopharynx region, while those from coughing originated from the lower respiratory tract. | Hatagishi et al. (2014) |
| Sit of virus release | As source, viral titers in throat or nose may not correlate with that in exhaled breath and cough. The viral loads in the laryngopharynx region and lower airway were significantly different in patients with HPAI H7N9. Under the condition where the virus was negative in laryngopharynx region, 103 to 105 copies/ml of viruses were still detected in lower airway. | Yang et al. (2015); Hatagishi et al. (2014); Milton, Fabian, Cowling, Grantham, and McDevitt (2013) |
| Site of infection | As recipient, the expression of viral receptors at different sites determines the location of pathology (and therefore affecting severity) upon infection and susceptibility to different viruses. | Nicholls, Bourne, Chen, Guan, and Peiris (2007) |
| Immunity | As recipient, prior infections or vaccinations can induce production of antibodies which confers protection to subsequent infection or reduce symptom severity even if infected. | Thomas, Keating, Hulse-Post, and Doherty (2006); Hobson, Curry, Beare, and Ward-Gardner (1972) |
| Environment | ||
| Temperature | As temperature rises, survival of viruses decreases. Temperatures higher than 30 °C can block airborne transmission of influenza virus. At high temperatures, DNA viruses are more stable than RNA viruses. Low temperatures can suppress host immunity in the respiratory tract, which can easily lead to viral infection. | Lowen, Steel, Mubareka, and Palese (2008); Lowen, Mubareka, Steel, and Palese (2007); Harper (1961) |
| Humidity | Survival of enveloped viruses is longer at lower relative humidity (20%−30%), while survival of non-enveloped viruses is longer at higher relative humidity (70%−90%). | Yang and Marr (2012); McDevitt, Rudnick, First, and Spengler (2010); Tang (2009); Lowen et al. (2007) |
| Ultraviolet radiation | Viral bioaerosols could be disinfected with ultraviolet radiation (affected by relative humidity). | McDevitt, Rudnick, and Radonovich (2012); Walker and Ko (2007); Jordan (1961) |
| Organic/ inorganic contents | Contents in blood, feces and sputum e.g. salt content produced by the host, or the materials of the surfaces of which the viral particles are attached to, can reduce/ increase the stress from the environment to viral particles. | Yang and Marr (2012); Tang (2009) |
For the viruses, its ability to infect the new host relies on whether: 1) viruses can survive in the environment; but survival of airborne virus of different types has a different decay time in the ambient air. For example, H1N1 and H5N1 influenza virus show close trend with regards to inactivation, approximately 60% of the virus was inactivated over the first 30 min at air conditions, however, about 50% of H3N2 viral particles were still alive even after 90 min (Pyankov Oleg, Pyankova Olga, & Agranovski Igor, 2012); 2) viruses can invade the target cell; and 3) there is sufficient virus infective dose. The minimal viral load resulting in infection (i.e. minimal infectious dose) varies between different viruses, for example, the viral load of smallpox virus is 10–100 organisms and the amount of hemorrhagic fever virus is only 1–10 organisms (Franz et al., 1997). For the host, as the recipient of the infection, depending on the site of infection and the branches of the immune system that are impaired (e.g. due to aging or immunosuppression), it will have different impacts on the susceptibility to different viruses (Bender et al., 1991, Hobson et al., 1972, Nicholls et al., 2007, Thomas et al., 2006). As the source of infection, the host also affects the risk of infection (in the recipient) via the aerosol route depending on his behavior and the site where the viral particles are released (Hatagishi et al., 2014, Milton et al., 2013, Yang et al., 2015). Environmental factors could also affect virus survival, including temperature, humidity, movement of the air, ultraviolet radiation and organic or inorganic contents where the viral particles are attached (Tang et al., 2006). Temperature can affect microscopically by altering the structure of viral proteins (including proteins that are involved in viral entry and replication) and genome, and could also affect macroscopically by setting up large exchange air flows in space due to temperature difference (Tang, 2009). The influence of humidity on virus survival is mainly related to whether the virus has lipid envelopes or not (Yang & Marr, 2012). But it is important to note that humidity and temperature can interact to affect the survival of viruses in aerosols, viruses decay rapidly in dry and hot environments, and only 4.7% survival over 60 min procedure (Pyankov Oleg, Bodnev Sergey, Pyankova Olga, & Agranovski Igor, 2017). Schaffer, Soergel, and Straube (1976) found that an asymmetrical U-shaped curve for influenza survival with different relative humidity at 21 °C. Airflow can impact the rate of particle gravitational settling (Jones & Brosseau, 2015). Studies have shown that infectivity of viral aerosols could be reduced by ultraviolet radiation (Jordan, 1961, McDevitt et al., 2012, Walker and Ko, 2007). Higher salt content in the viral aerosols could reduce viability of the viral particles (Yang & Marr, 2012), while organic materials (e.g. blood, feces, mucus and saliva) could buffer against extreme environmental stress on viral particles in aerosols (Tang, 2009).
3.4. Methods for sampling and analysis of viral bioaerosols in healthcare settings
The size of the bioaerosol that contains viruses determines the time for which the pathogen is suspended in the air and where it deposits in the respiratory tract (La Rosa et al., 2013, Nazaroff, 2016). Many studies have been conducted with the aim of detecting levels of viral aerosols in the air, so as to inform whether infection control strategies targeting aerosol transmission (Table 1) is needed. At present, the methods used for detection of viruses in bioaerosols include impaction, impingement, cyclone sampling, electrostatic precipitation and filtration (Ghosh et al., 2015, Haig et al., 2016, Hinds, 2012).
The principle of impaction is to collect microorganism and particles in the air, the impaction sampler draws in air and forces to change its direction which causes particles with high inertia to get impacted over collecting surfaces (Ghosh et al., 2015, Henningson and Ahlberg, 1994). The impingement methods are similar to that of impaction, except that the microorganisms are collected into a liquid medium (Ghosh et al., 2015). Some bioaerosol samplers are available by means of impact or impact methods, which can collect a variety of viruses, such as measles virus, influenza A virus, influenza B virus, adenovirus (Bischoff et al., 2016, Lednicky and Loeb, 2013, Nguyen et al., 2016), Cyclone samplers capture microorganisms in a liquid (aerosol to hydrosol) using swirling air and centrifugal force (Ghosh et al., 2015). Grayson, Griffiths, Perez, and Piedimonte (2017) applied stationary 2-stage bioaerosol cyclone samplers to capture RSV-laden particles in a pediatric acute care setting, and their findings indicate that airborne RSV-laden particles can be detected in pediatric outpatient clinics during the epidemic peak. The electrostatic precipitation of airborne particles are mainly precipitated from an airstream by the application of an external force such as electrical force on charged particle (Knutson & Whitby, 1975). Research by Ladhani et al. (2017) showed successful sampling and detection of airborne influenza virus using an electrostatic precipitation (ESP)-based bioaerosol sampler. In filtration methods, airborne microorganisms are collected by passing air through porous membrane filters made of glass fiber, polyvinylchloride (PVC), polycarbonate or cellulose acetate (incubated by transferring onto the surfaces of growth agar media) or gelatin (Ghosh et al., 2015). Membrane filtration and sampling technology of virus can permit monitoring of very low viral content in air (Aintablian et al., 1998, Myatt et al., 2003). Employing these biosamplers, recently there have been increasing studies that demonstrated viruses (including influenza, measles and RSV) can be recovered from the air in healthcare settings (Bischoff et al., 2016, Bischoff et al., 2013, Blachere et al., 2009, Leung et al., 2016, Lindsley et al., 2010).
4. Prevention and control of aerosol transmission in healthcare settings
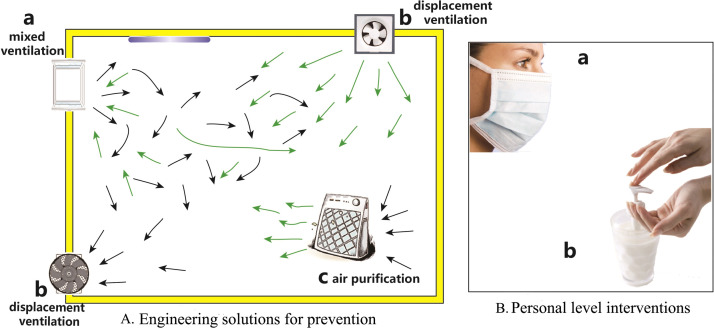
Hospital environments are complex and the exposure of health care workers, patients, and visitors to airborne virus infections remains a substantial problem (McDevitt et al., 2012, Rudnick et al., 2009). Susceptible patients, health care workers and visitors can acquire infections from the hospital environment, through droplet or aerosol transmission from viruses carried by the movement of air, or indirect contact transmission that involves physical contact with contaminated surfaces. The potential risk of nosocomial infections is very high, but there is still lack of effective standard control measures to prevent the outbreak of nosocomial infection, for example, many studies identified the marked lack of evidence for neonatal HAI outbreak management globally (Birt et al., 2016). Understanding the route of transmission is critical for implementing the best control strategies (McDevitt et al., 2012). A range of interventions can be applied for the prevention and control of viral aerosols in hospitals ( Fig. 1) as described in the following subsections.
Fig. 1.
Systematic and personal level interventions for the prevention and control of viral aerosols in healthcare settings.
4.1. Engineering solutions for prevention
The purpose of air filtration and purification in hospitals is to reduce the concentrations of airborne pathogens so that it is lower than their infectious dose. This could be an effective intervention to block aerosol transmission where the following methods can be applied:
First, mixing the contaminated air with uncontaminated air to dilute the contaminated air. This can reduce the peak concentrations of droplet nuclei in the contaminated indoor air (Jensen, Lambert, Iademarco, & Ridzon, 2005). However, the average concentration of droplet nuclei in contaminated indoor air will increase over time unless air filtration systems are adopted.
Second, usage of displacement ventilation. This can increase the air change rate (ac/h) of indoor air so that the contaminated air can be replaced (Jensen et al., 2005). However, the use of displacement ventilation in hospital wards can increase the risk of aerosol transmission because a patient lying in bed may exhale air plumes that can spread over long distances due to differences in air temperature and density (Qian et al., 2006). Existing guidelines recommend that the airflow should be from the room ceiling to the healthcare workers’ region, then to the patients’ region, and lastly expelled through the exhaust vents that are located at a lower level (Jensen et al., 2005). In practice, mixing ventilation and displacement ventilation are commonly used to remove contaminant particles.
Third, installation of air filtration and purification systems. Methods such as air filtration system, ionization and high voltage field, ultraviolet radiation, photocatalytic oxidation, dielectric barrier discharge and others have been adopted to purify or decontaminate indoor air (Alonso et al., 2016, Dee et al., 2006, Kozlova et al., 2010, McDevitt et al., 2012, Zhao et al., 2014; Hyun et al., 2017). At present, national standards and related technical specifications of air purification are lacking. Medical air purifiers used should meet the following requirements: 1) Safety, should not create secondary air pollution; 2) Convenience, low noise operation, and portable; 3) Effectiveness, can effectively kill different types of pathogens. Air purification technology as a means to reduce or eliminate airborne particles or pathogenic microorganism levels has been reported previously in various fields. Traditionally, ultraviolet radiation is widely used to sanitize air (First, Rudnick, Banahan, Vincent, & Brickner, 2007), Several previous studies have indicated that UV air disinfection protects humans from infectious diseases caused by airborne microorganism (such as influenza virus, pox viruses, rhinovirus and coronavirus), and those experiments also show that virus aerosols are less susceptible to UV at higher RH than at lower RH (McDevitt et al., 2012, McDevitt et al., 2007, McDevitt et al., 2008, Scarpino et al., 1998, Walker and Ko, 2007), but some exceptions exist (Walker & Ko, 2007). In addition, the combination of UV-irradiation and other measures for air purification cannot handle large volumes air due to their limited capacity in buildings (Schulz, Bao, Clauss, & Hartung, 2013).
Air filtration system is another common purification technique, which allows the air to pass through a series of filters of decreasing pore size through positive pressure ventilation. Dee et al. (2006) showed that high-efficiency particulate air filtrations which are capable of blocking the passage of particles 0.3 µm or more in diameter can significantly reduce PRRSV transmission. In addition, some filters treating with special material (e.g., dialdehyde starch) can disinfect airborne viruses simultaneously (Woo et al., 2012). Similarly, low-cost filtering systems can also filter PRRSV viruses effectively. An electrostatic particle ionization technology that generates a high negative ion output which results in the electrification of airborne particles. The ionized airborne particles are attracted toward opposite charges and may be cleared from the air by adhesion to the walls or other charged surfaces (Alonso et al., 2016). This ionization technique has been extensively applied to the disinfection of pathogenic microorganisms (including viruses) in poultry and livestock houses (Alonso et al., 2016, Mitchell and King, 1994). The ionization technique can also be combined with other purification technologies such as photocatalytic oxidation, which may provide significant pathogen removal efficiency and biocidal capabilities (Grinshpun et al., 2007; Yu et al., 2008). Multiphase photocatalytic technology is based on the penetration of ultraviolet radiation into photocatalyst (such as titanium dioxide, TiO2). The purpose is to produce an air purification technology by generating highly active hydroxyl radicals to viruses and other pathogenic microorganisms (Kozlova et al., 2010, Paschoalino and Jardim, 2008). Grinshpun's research indicates that approximately 90% of initially viable MS2 viruses were inactivated resulting from 10 to 60 min exposure to the photocatalytic oxidation (Grinshpun et al., 2007). Cold oxygen plasma technology can effectively control the viral titers of airborne respiratory viruses (Terrier et al., 2009), and it can be used as effective measure for case management during influenza epidemics. We previously showed that cold plasma showed good pathogenic effect on influenza A (H1N1) virus aerosol, which was similar to that of common UV lamp (Wang et al., 2012).
In summary, the above-mentioned air purification technologies have shown high efficiency in denaturing airborne viruses in laboratory tests, farm sterilization, etc. Unfortunately, there are few reports on these technologies except for UV irradiation in clinical applications. More field experiments are needed to confirm which of these interventions are most suitable to meet the actual needs of medical institutions.
4.2. Personal level interventions
It was traditionally believed that wearing face masks and respirators can prevent diseases transmitted through droplets and respiratory aerosols (MacIntyre & Chughtai, 2015). A variety of protective devices are used in health care facilities and community settings including cloth masks,medical masks (medical, surgical) and respirators (such as N95, N99, N100, P2, P3, FFP2, and FFP3); But there is no consensus around the choice between facemasks and respirators to prevent respiratory diseases (MacIntyre & Chughtai, 2015). The first study of the value of face masks (cloth masks) by healthcare workers began in 1918 (Weaver, 1918). Subsequent studies found that face masks were also used to protect medical personnel from scarlet fever, measles and influenza (MacIntyre and Chughtai, 2015, Whitelaw, 1919). During the outbreak of SARS, use of masks in the general population in Hong Kong was high enough to observe an effect on all respiratory infections (Leung et al., 2003, Lo et al., 2005), and face mask use did prevent SARS infections in health care workers (Seto et al., 2003). Medical masks have been widely used for 50 years, and respirators were later specifically designed for respiratory protection (MacIntyre & Chughtai, 2015). Bischoff, Reid, Russell, and Peters (2011) found that N95 respirators provided improved protection compared to medical masks (surgical masks). In addition, that study also described the equal importance of wearing goggles to enhance eye protection. For other diseases that are mainly transmitted through aerosols, such as measles, chickenpox, and other viruses, the surgical mask is not adequate in providing protection against viruses transmitted through aerosols, and filter was needed within the face mask. Nevertheless, there are different opinions regarding the efficacy of face mask for personal isolation and protection. Although Smith et al. (2016) have showed the efficacy of N95 respirators and surgical masks in protecting healthcare workers against acute respiratory infection in a meta-analysis, the study also reported that there was no significant difference between N95 respirators and surgical masks in preventing the transmission of acute respiratory infection for the protection of healthcare workers. Large-scale randomized controlled trials are likely needed to evaluate the efficacy of N95 respirators in the prevention of acute respiratory infection. In addition, reuse of facemasks and respirators is widespread globally, but for its safety, the researchers have inconsistent views and lack clinical evidence (MacIntyre and Chughtai, 2015; Chughtai et al., 2015; Loeb et al., 2009). We previously reviewed the use of face masks during the 2009 influenza A(H1N1) pandemic (Cowling, Zhou, Ip, Leung, Aiello, 2010), and found that there is some evidence to support the wearing of masks or respirators during illness to protect others from being infected, and more studies in controlled settings and studies of natural infections in healthcare and community settings are needed to better define the effectiveness of faces masks and respirators in preventing influenza virus transmission.
5. Conclusions and future prospects
Pathogenic airborne respiratory and enteric viruses are important causes of nosocomial infection. These infections are a significant problem for hospitalized patients, which can lead to major burden on health and healthcare costs, particularly in the elderly, children and those with underlying diseases. In this article, we review, from the standpoints of epidemiologists and virologists, the burden and signifiances of nosocomial infections of respiratory and enteric viruses, the possible role of aerosol transmission in these nosocomial infections, and prevention and control measures of aerosol trasmission of respiratory and enteric virus infections in healthcare settings. There is increasing evidence in the scientific literature that aerosol transmission is an important route of a number of respiratory and enteric viruses. Aerosol transmission of viruses can be affected by intrinsic factors, which include aerosol particles physical properties, virus characteristics and host factors; or extrinsic factors, including environmental temperature and humidity. In view of the possibilities of a large number of respiratory viruses and other pathogenic microorganisms that may exist as aerosol virus particles, including those that are generated from the resuspension from the surface of contaminated objects in the hospital, much prevention and control measures have been adopted to mitigate nosocomial infections via the aerosol route which aim to improve aerosol management and surface sterilization, including engineering solutions, hand hygiene and wearing face masks. However, cross infection of viral infectious diseases, some possibly via aerosols, still exists and occurs in the hospital. A number of challenges remain for new prevention and control measures, as well as applied research: 1) The importance of respiratory pathogens in interpersonal transmission, including the range and form of transmission; 2) the potential of aerosols generated by medical instruments or equipment, as well as during medical procedures; 3) the actual contributions of physical contact, droplets and aerosols in transmission of respiratory pathogens; 4) the efficacy of different types of face masks, efficiency of air purification system in reducing the transmission of respiratory viral influenza, as well as the combined forms and effects with hand hygiene and personal protective measures. At the same time, relevant clinical medical research can also be carried out, such as controlled studies of the impact on these measures on biologically relevant measures (e.g. viral loads) and patient outcomes.
Acknowledgments
This study was financially supported by National Natural Science Foundation of China (Grant no. 81490534), Science research project of the Guangdong Province (Grant no. 2016A050503047), Municipal Science and Technology Bureau Foundation of Guangzhou (Grant no. 2014Y2-00031). We acknowledge the contributions of Qiuling Du and Wenbo Huang from Guangzhou Medical University for technical assistance with the figures.
Contributor Information
Benjamin J. Cowling, Email: bcowling@hku.hk.
Zi-Feng Yang, Email: jeffyah@163.com.
References
- AintablianZhao N., Walpita P., Sawyer M.H. Detection of Bordetella pertussis and respiratory synctial virus in air samples from hospital rooms. Infection Control & Hospital Epidemiology. 1998;19(12):918–923. doi: 10.1086/647764. [PubMed: 9872529] [DOI] [PubMed] [Google Scholar]
- Aitken C., Jeffries D.J. Nosocomial spread of viral disease. Clinical Microbiology Reviews. 2001;14(3):528–546. doi: 10.1128/CMR.14.3.528-546.2001. [PubMed: 11432812] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akhter J., al-Hajjar S., Myint S., Qadri S.M. Viral contamination of environmental surfaces on a general paediatric ward and playroom in a major referral centre in Riyadh. European Journal of Epidemiology. 1995;11(5):587–590. doi: 10.1007/BF01719313. [PubMed: 8549735] [DOI] [PubMed] [Google Scholar]
- Alford R.H., Kasel J.A., Gerone P.J., Knight V. Human influenza resulting from aerosol inhalation. Proceedings of the Society for Experimental Biology and Medicine. 1966;122(3):800–804. doi: 10.3181/00379727-122-31255. [PubMed:5918954] [DOI] [PubMed] [Google Scholar]
- Allegranzi B., BagheriNejad S., Combescure C., Graafmans W., Attar H., Donaldson L., Pittet D. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377(9761):228–241. doi: 10.1016/S0140-6736(10)61458-4. [PubMed:21146207] [DOI] [PubMed] [Google Scholar]
- Alonso C., Raynor P.C., Davies P.R., Morrison R.B., Torremorell M. Evaluation of an electrostatic particle ionization technology for decreasing airborne pathogens in pigs. Aerobiologia. 2016;32(3):405–419. doi: 10.1007/s10453-015-9413-3. [PubMed:27616810] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Álvarez-Lerma F., Marín-Corral J., Vilà C., Masclans J.R., Loeches I.M., Barbadillo S.…Rodríguez A. H1N1 GETGAG/SEMICYUC study group. Characteristics of patients with hospital-acquired influenza A (H1N1)pdm09 virus admitted to the intensive care unit. Journal of Hospital Infection. 2017;95(2):200–206. doi: 10.1016/j.jhin.2016.12.017. [PubMed:28153560] [DOI] [PubMed] [Google Scholar]
- American Thoracic Society Infectious diseases society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. American Journal of Respiratory and Critical Care Medicine. 2005;171(4):388–416. doi: 10.1164/rccm.200405-644ST. [PubMed:15699079] [DOI] [PubMed] [Google Scholar]
- Ansari S.A., Springthorpe V.S., Sattar S.A., Rivard S., Rahman M. Potential role of hands in the spread of respiratory viral infections: studies with human parainfluenza virus 3 and rhinovirus 14. Journal of Clinical Microbiology. 1991;29(10):2115–2119. doi: 10.1128/jcm.29.10.2115-2119.1991. [PubMed:1658033] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansumana R., Keitell S., Roberts G.M., Ntoumi F., Petersen E., Ippolito G., Zumla A. Impact of infectious disease epidemics on tuberculosis diagnostic, management, and prevention services: experiences and lessons from the 2014-2015 Ebola virus disease outbreak in West Africa. International Journal of Infectious Diseases. 2017;56:101–104. doi: 10.1016/j.ijid.2016.10.010. [PubMed:27818362] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker J., Jones M.V. The potential spread of infection caused by aerosol contamination of surfaces after flushing a domestic toilet. Journal of Applied Microbiology. 2005;99(2):339–347. doi: 10.1111/j.1365-2672.2005.02610.x. [PubMed:16033465] [DOI] [PubMed] [Google Scholar]
- Belliot G., Lopman B.A., Ambert-Balay K., Pothier P. The burden of norovirus gastroenteritis: an important foodborne and healthcare-related infection. Clinical Microbiology and Infection. 2014;20(8):724–730. doi: 10.1111/1469-0691.12722. [PubMed:24943671] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender B.S., Johnson M.P., Small P.A. Influenza in senescent mice: impaired cytotoxic T-lymphocyte activity is correlated with prolonged infection. Immunology. 1991;72(4):514–519. [PubMed:2037313] [PMC free article] [PubMed] [Google Scholar]
- Benenson A.S. 16th ed. American Public Health Association; Washington: 1995. Control of communicable diseases manual. [Google Scholar]
- Birt J., Le Doare K., Kortsalioudaki C., Lawn J., Heath P.T., Sharland M. Lack of evidence for the efficacy of enhanced surveillance compared to other specific interventions to control neonatal healthcare-associated infection outbreaks. Transactions of the Royal Society of Tropical Medicine and Hygien. 2016;110(2):98–106. doi: 10.1093/trstmh/trv116. [PubMed:26822602] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischoff W.E., Reid T., Russell G.B., Peters T.R. Transocular entry of seasonal influenza-attenuated virus aerosols and the efficacy of n95 respirators, surgical masks, and eye protection in humans. Journal of Infectious Diseases. 2011;204(2):193–199. doi: 10.1093/infdis/jir238. [PubMed:21673029] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischoff W.E., Swett K., Leng I., Peters T.R. Exposure to influenza virus aerosols during routine patient care. Journal of Infectious Diseases. 2013;207(7):1037–1046. doi: 10.1093/infdis/jis773. [PubMed: 23372182] [DOI] [PubMed] [Google Scholar]
- Bischoff W.E., McNall R.J., Blevins M.W., Turner J., Lopareva E.N., Rota P.A. Detection of measles virus RNA in air and surface specimens in a hospital setting. Journal of Infectious Diseases. 2016;213(4):600–603. doi: 10.1093/infdis/jiv465. [PubMed:26386428] [DOI] [PubMed] [Google Scholar]
- Blachere F.M., Lindsley W.G., Pearce T.A., Anderson S.E., Fisher M., Khakoo R. Measurement of airborne in¬fluenza virus in a hospital emergency department. Clinical Infectious Diseases. 2009;48(4):438–440. doi: 10.1086/596478. [PubMed:19133798] [DOI] [PubMed] [Google Scholar]
- Bloch A.B., Orenstein W.A., Ewing W.M., Spain W.H., Mallison G.F., Herrmann K.L., Hinman A.R. Measles outbreak in a pediatric practice: airborne transmission in an office setting. Pediatrics. 1985;75(4):676–683. [PubMed:3982900] [PubMed] [Google Scholar]
- Bobo L.D., Dubberke E.R. Recognition and prevention of hospital-associated enteric infections in the intensive care unit. Critical Care Medicine. 2010;38(8 Suppl):S324–S334. doi: 10.1097/CCM.0b013e3181e69f05. [PubMed:20647790] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonifait L., Charlebois R., Vimont A., Turgeon N., Veillette M., Longtin Y.…Duchaine C. Detection and quantification of airborne norovirus during outbreaks in healthcare facilities. Clinical Infectious Diseases. 2015;61(3):299–304. doi: 10.1093/cid/civ321. [PubMed:25900175] [DOI] [PubMed] [Google Scholar]
- Boone S.A., Gerba C.P. Significance of fomites in the spread of respiratory and enteric viral disease. Applied and Environmental Microbiology. 2007;73(6):1687–1696. doi: 10.1128/AEM.02051-06. [ PubMed:17220247] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branch-Elliman W., Savor Price C., McGeer A., Perl T.M. Protecting the frontline: designing an infection prevention platform for preventing emerging respiratory viral illnesses in healthcare personnel. Infection Control & Hospital Epidemiology. 2015;36(3):336–345. doi: 10.1017/ice.2014.52. [PubMed: 25695176] [DOI] [PubMed] [Google Scholar]
- Brankston G., Gitterman L., Hirji Z., Lemieux C., Gardam M. Transmission of influenza A in human beings. Lancet Infectious Diseases. 2007;7(4):257–265. doi: 10.1016/S1473-3099(07)70029-4. [PubMed:17376383] [DOI] [PubMed] [Google Scholar]
- Bruijning-Verhagen P., Quach C., Bonten M. Nosocomial rotavirus infections: a meta-analysis. Pediatrics. 2012;129(4):e1011–e1019. doi: 10.1542/peds.2011-2779. [PubMed:22392170] [DOI] [PubMed] [Google Scholar]
- Carlson A.L., Budd A.P., Perl T.M. Control of influenza in healthcare settings: early lessons from the 2009 pandemic. Current Opinion in Infectious Diseases. 2010;23(4):293–299. doi: 10.1097/QCO.0b013e32833bb804. [PubMed: 20592530] [DOI] [PubMed] [Google Scholar]
- Chan M. Ebola virus disease in West Africa--no early end to the outbreak. New England Journal of Medicine. 2014;371(13):1183–1185. doi: 10.1056/NEJMp1409859. [PubMed: 25140856] [DOI] [PubMed] [Google Scholar]
- Chang L.Y., Tsao K.C., Hsia S.H., Shih S.R., Huang C.G., Chan W.K.…Lin T.Y. Transmission and clinical features of enterovirus 71 infections in household contacts in Taiwan. JAMA. 2004;291(2):222–227. doi: 10.1001/jama.291.2.222. [PubMed:14722149] [DOI] [PubMed] [Google Scholar]
- Chen H., Liu S., Liu J., Chai C., Mao H., Yu Z.…Chen E. Nosocomial co-transmission of avian influenza A(H7N9) and A(H1N1)pdm09 viruses between 2 patients with hematologic disorders. Emerging Infectious Diseases. 2016;22(4):598–607. doi: 10.3201/eid2204.151561. [PubMed:26982379] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow E.J., Mermel L.A. Hospital-acquired respiratory viral infections: incidence, morbidity, and mortality in pediatric and adult patients. Open Forum Infectious Diseases. 2017;4(1):ofx006. doi: 10.1093/ofid/ofx006. [PubMed: 28480279] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chughtai A.A., Seale H., Chi Dung T., Maher L., Nga P.T., MacIntyre C.R. Current practices and barriers to the use of facemasks and respirators among hospital-based health care workers in Vietnam. American Journal of Infection Control. 2015;43(1):72–77. doi: 10.1016/j.ajic.2014.10.009. [PubMed: 25564127] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couch R.B., Douglas R.G., Jr., Lindgren K.M., Gerone P.J., Knight V. Airborne transmission of respiratory infection with coxsackievirusA type 21. American Journal of Epidemiology. 1970;91(1):78–86. doi: 10.1093/oxfordjournals.aje.a121115. [PubMed:415578] [DOI] [PubMed] [Google Scholar]
- Cowling B.J., Zhou Y., Ip D.K., Leung G.M., Aiello A.E. Face masks to prevent transmission of influenza virus: a systematic review. Epidemiol Infection. 2010;138(4):449–456. doi: 10.1017/S0950268809991658. [PubMed: 20092668] [DOI] [PubMed] [Google Scholar]
- Dee S.A., Batista L., Deen J., Pijoan C. Evaluation of systems for reducing the transmission of porcine reproductive and respiratory syndrome virus by aerosol. Canadian Journal of Veterinary Research. 2006;70(1):28–33. [PubMed:16548329] [PMC free article] [PubMed] [Google Scholar]
- Douwes J., Thorne P., Pearce N., Heederik D. Bioaerosol health effects and exposure assessment: progress and prospects. Annals of Occupational Hygiene. 2003;47(3):187–200. doi: 10.1093/annhyg/meg032. [PubMed: 12639832] [DOI] [PubMed] [Google Scholar]
- Dowell S.F., Simmerman J.M., Erdman D.D., Wu J.S., Chaovavanich A., Javadi M.…Ho M.S. Severe acute respiratory syndrome coronavirus on hospital surfaces. Clinical Infectious Diseases. 2004;39(5):652–657. doi: 10.1086/422652. [PubMed: 15356778] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duguid J.P. The size and the duration of air-carriage of respiratory droplets and droplet-nuclei. Journal of Hygiene. 1946;44(6):471–479. doi: 10.1017/s0022172400019288. [PubMed: 20475760] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang C.F., Ma M.J., Zhan B.D., Lai S.M., Hu Y., Yang X.X.…Cao W.C. Nosocomial transmission of avian influenza A (H7N9) virus in China: epidemiological investigation. BMJ. 2015;351:h5765. doi: 10.1136/bmj.h5765. [PubMed:26586515] [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M., Rudnick S.N., Banahan K.F., Vincent R.L., Brickner P.W. Fundamental factors affecting upper-room ultraviolet germicidal irradiation -part I. Experimental. Journal of Occupational and Environmental Hygiene. 2007;4(5):321–331. doi: 10.1080/15459620701271693. [PubMed:17365506] [DOI] [PubMed] [Google Scholar]
- Franz D.R., Jahrling P.B., Friedlander A.M., McClain D.J., Hoover D.L., Bryne W.R. Clinical recognition and management of patients exposed to biological warfare agents. JAMA. 1997;278(5):399–411. doi: 10.1001/jama.278.5.399. [PMID:9244332] [DOI] [PubMed] [Google Scholar]
- Gallimore C.I., Taylor C., Gennery A.R., Cant A.J., Galloway A., Xerry J., Adigwe J., Gray J.J. Contamination of the hospital environment with gastroenteric viruses: comparison of two pediatric wards over a winter season. Journal of Clinical Microbiology. 2008;46(9):3112–3115. doi: 10.1128/JCM.00400-08. [PubMed: 18614656] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner J.S. Guideline for isolation precautions in hospitals. The hospital infection control practices advisory committee. Infection Control & Hospital Epidemiology. 1996;17(1):53–80. doi: 10.1086/647190. [PubMed: 8789689] [DOI] [PubMed] [Google Scholar]
- Gautret P., Gray G.C., Charrel R.N., Odezulu N.G., Al-Tawfiq J.A., Zumla A., Memish Z.A. Emerging viral respiratory tract infections--environmental risk factors and transmission. Lancet Infectious Diseases. 2014;14(11):1113–1122. doi: 10.1016/S1473-3099(14)70831-X. [PubMed: 25189350] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh B., Lal H., Srivastava A. Review of bioaerosols in indoor environment with special reference to sampling, analysis and control mechanisms. Environment International. 2015;85:254–272. doi: 10.1016/j.envint.2015.09.018. [PubMed: 26436919] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grayson S.A., Griffiths P.S., Perez M.K., Piedimonte G. Detection of airborne respiratory syncytial virus in a pediatric acute care clinic. Pediatric Pulmonology. 2017;52(5):684–688. doi: 10.1002/ppul.23630. [PubMed:27740722] [DOI] [PubMed] [Google Scholar]
- Grinshpun S.A., Adhikari A., Honda T., Kim K.Y., Toivola M., Rao K.S., Reponen T. Control of aerosol contaminants in indoor air: combining the particle concentration reduction with microbial inactivation. Environmental Science & Technology. 2007;1(2):606–612. doi: 10.1021/es061373o. [PubMed:17310729] [DOI] [PubMed] [Google Scholar]
- Guan Tianjia, Yao Maosheng. Use of carbon nanotube filter in removing bioaerosols. Journal of Aerosol Science. 2010;41(6):611–620. [Google Scholar]
- Gustafson T.L., Lavely G.B., Brawner E.R., Jr, Hutcheson R.H., Jr, Wright P.F., Schaffner W. An outbreak of airborne nosocomial varicella. Pediatrics. 1982;70(4):550–556. [PubMed:6289235] [PubMed] [Google Scholar]
- Haig C.W., Mackay W.G., Walker J.T., Williams C. Bioaerosol sampling: sampling mechanisms, bioefficiency and field studies. Journal of Hospital Infection. 2016;93(3):242–255. doi: 10.1016/j.jhin.2016.03.017. [PubMed: 27112048] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall C.B. Respiratory syncytial virus: its transmission in the hospital environment. "The Yale Journal of Biology and Medicine. 1982;55(3-4):219–223. [PubMed:6758370] [PMC free article] [PubMed] [Google Scholar]
- Hall C.B. Nosocomial respiratory syncytial virus infections: the "Cold War" has not ended. Clinical Infectious Diseases. 2000;31(2):590–596. doi: 10.1086/313960. [PubMed: 10987726] [DOI] [PubMed] [Google Scholar]
- Harper G.J. Airborne micro-organisms: survival tests with four viruses. Journal of Hygien. 1961;59:479–486. doi: 10.1017/s0022172400039176. [PubMed:13904777] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatagishi E., Okamoto M., Ohmiya S., Yano H., Hori T., Saito W.…Nishimura H. Establishment and clinical applications of a portable system for capturing influenza viruses released through coughing. PLoS One. 2014;9(8):e103560. doi: 10.1371/journal.pone.0103560. [PubMed:25083787] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henningson E.W., Ahlberg M.S. Evaluation of microbiological aerosol samplers-a review. Journal of Aerosol Science. 1994;25(8):1459–1492. [Google Scholar]
- Herfst S., Bohringer M., Karo B., Lawrence P., Lewis N.S., Mina M.J.…Menge C. Drivers of airborne human-to-human pathogen transmission. Current Opinion in Virology. 2016;22:22–29. doi: 10.1016/j.coviro.2016.11.006. [PubMed:27918958] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds W.C. 2nd ed. JohnWiley& Sons; New York, NY: 1999. Aerosol technology. [Google Scholar]
- Hinds W.C. 2nd ed. John Wiley & Sons; New York: 2012. Aerosol technology: properties, behavior, and measurement of airborne particles. [Google Scholar]
- Ho P.L., Tang X.P., Seto W.H. Vol. 8. 2003. SARS: hospital infection control and admission strategies; pp. Suppl:S41–Suppl:S45. (Respirology). [PubMed:15018133] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobson D., Curry R.L., Beare A.S., Ward-Gardner A. The role of serum haemagglutination-inhibiting antibody in protection against challenge infection with influenza A2 and B viruses. Journal of Hygiene. 1972;70(4):767–777. doi: 10.1017/s0022172400022610. [PubMed: 4509641] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horan T.C., Andrus M., Dudeck M.A. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. American Journal of Infection Control. 2008;36(5):309–332. doi: 10.1016/j.ajic.2008.03.002. [PubMed:18538699] [DOI] [PubMed] [Google Scholar]
- Hviid A., Rubin S., Mühlemann K. Mumps. Lancet. 2008;371(9616):932–944. doi: 10.1016/S0140-6736(08)60419-5. [PubMed: 18342688] [DOI] [PubMed] [Google Scholar]
- Hyun Junho, Lee Sang-Gu, Hwang Jungho. Application of corona discharge-generated air ions for filtration of aerosolized virus and inactivation of filtered virus. Journal of Aerosol Science. 2017;107:31–40. doi: 10.1016/j.jaerosci.2017.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaax N., Jahrling P., Geisbert T., Geisbert J., Steele K., McKee K.…Peters C. Transmission of Ebola virus (Zaire strain) to uninfected control monkeys in a biocontainment laboratory. Lancet. 1995;346(8991-8992):1669–1671. doi: 10.1016/s0140-6736(95)92841-3. [PubMed:8551825] [DOI] [PubMed] [Google Scholar]
- Jennings L.C., Dick E.C., Mink K.A., Wartgow C.D., Inhorn S.L. Near disappearance of rhinovirus along a fomite transmission chain. Journal of Infectious Diseases. 1988;158(4):888–892. doi: 10.1093/infdis/158.4.888. [PubMed:2844923] [DOI] [PubMed] [Google Scholar]
- Jensen P.A., Lambert L.A., Iademarco M.F., Ridzon R. CDC. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Recommendations and Reports. 2005;54(RR-17):1–141. [PubMed:16382216] [PubMed] [Google Scholar]
- Jones R.M., Brosseau L.M. Aerosol transmission of infectious disease. Journal of Occupational and Environmental Medicine. 2015;57(5):501–508. doi: 10.1097/JOM.0000000000000448. [PubMed:25816216] [DOI] [PubMed] [Google Scholar]
- Jordan W.S., Jr. The mechanism of spread of Asian influenza. American Review of Respiratory Disease. 1961;83(2):29–40. doi: 10.1164/arrd.1961.83.2P2.29. [PubMed:13790691] [DOI] [PubMed] [Google Scholar]
- Josephson A., Gombert M.E. Airborne transmission of nosocomial varicella from localized zoster. Journal of Infectious Diseases. 1988;158(1):238–241. doi: 10.1093/infdis/158.1.238. [PubMed:3392417] [DOI] [PubMed] [Google Scholar]
- Kalil A.C., Metersky M.L., Klompas M., Muscedere J., Sweeney D.A., Palmer L.B.…Knight S.L., Brozek J.L. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the infectious diseases society of america and the american thoracic society. Clinical Infectious Diseases. 2016;63(5):e61–e111. doi: 10.1093/cid/ciw353. [PubMed:27418577] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kambhampati A., Koopmans M., Lopman B.A. Burden of norovirus in healthcare facilities and strategies for outbreak control. Journal of Hospital Infection. 2015;89(4):296–301. doi: 10.1016/j.jhin.2015.01.011. [PubMed:25726433] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiology and Health. 2015;37:e2015033. doi: 10.4178/epih/e2015033. [PubMed:26212508] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.H., Chang S.Y., Sung M., Park J.H., Bin Kim H., Lee H.…Min J.Y. Extensive viable middle east respiratory syndrome (MERS) coronavirus contamination in air and surrounding environment in MERS isolation wards. Clinical Infectious Diseases. 2016;63(3):363–369. doi: 10.1093/cid/ciw239. [PubMed:27090992] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight V. Viruses as agents of airborne contagion. Annals of the New York Academy of Sciences. 1980;353:147–156. doi: 10.1111/j.1749-6632.1980.tb18917.x. [PubMed: 6261640] [DOI] [PubMed] [Google Scholar]
- Knutson E.O., Whitby K.T. Aerosol classification by electric mobility: apparatus, theory, and applications. Journal of Aerosol Science. 1975;6:443–451. [Google Scholar]
- Kozlova E.A., Safatov A.S., Kiselev S.A., Marchenko V.Y., Sergeev A.A., Skarnovich M.O.…Vorontsov A.V. Inactivation and mineralization of aerosol deposited model pathogenic microorganisms over TiO2 and Pt/TiO2. Environmental Science and Technology. 2010;44(13):5121–5126. doi: 10.1021/es100156p. [PubMed: 20521809] [DOI] [PubMed] [Google Scholar]
- La Rosa G., Fratini M., Della Libera S., Iaconelli M., Muscillo M. Viral infections acquired indoors through airborne, droplet or contact transmission. Annal Ist Super Sanita. 2013;49(2):124–132. doi: 10.4415/ANN_13_02_03. [PubMed:23771256] [DOI] [PubMed] [Google Scholar]
- Ladhani L., Pardon G., Meeuws H., van Wesenbeeck L., Schmidt K., Stuyver L., van der Wijngaart W. Sampling and detection of airborne influenza virus towards point-of-care applications. PLoS One. 2017;12(3):e0174314. doi: 10.1371/journal.pone.0174314. [PubMed:28350811] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laksono B.M., de Vries R.D., McQuaid S., Duprex W.P., de Swart R.L. Measles virus host invasion and pathogenesis. Viruses. 2016;8(8) doi: 10.3390/v8080210. pii: E210. [PubMed:27483301] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leclair J.M., Zaia J.A., Levin M.J., Congdon R.G., Goldmann D.A. Airborne transmission of chickenpox in a hospital. New England Journal of Medicine. 1980;302(8):450–453. doi: 10.1056/NEJM198002213020807. [PubMed:7351951] [DOI] [PubMed] [Google Scholar]
- Lednicky J.A., Loeb J.C. Detection and isolation of airborne influenza A H3N2 virus using a sioutas personal cascade impactor sampler. Influenza Research and Treatment. 2013;2013:656825. doi: 10.1155/2013/656825. [PubMED:24224087] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lessler J., Reich N.G., Brookmeyer R., Perl T.M., Nelson K.E., Cummings D.A. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infectious Diseases. 2009;9(5):291–300. doi: 10.1016/S1473-3099(09)70069-6. [PubMED: 19393959] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung G.M., Lam T.H., Ho L.M., Ho S.Y., Chan B.H., Wong I.O., Hedley A.J. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. Journal of Epidemiology and Community Health. 2003;57(11):857–863. doi: 10.1136/jech.57.11.857. [PubMed:14600110] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung N.H., Zhou J., Chu D.K., Yu H., Lindsley W.G., Beezhold D.H.…Cowling B.J. Quantification of influenza virus RNA in aerosols in patient rooms. PLoS One. 2016;11(2):e0148669. doi: 10.1371/journal.pone.0148669. [PubMed: 26849130] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay L., Wolter J., De Coster I., Van Damme P., Verstraeten T. A decade of norovirus disease risk among older adults in upper-middle and high income countries: a systematic review. BMC Infectious Diseases. 2015;15:425. doi: 10.1186/s12879-015-1168-5. [PubMed:26467099] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsley W.G., Blachere F.M., Davis K.A., Pearce T.A., Fisher M.A., Khakoo R.…Beezhold D.H. Distribution of airborne influenza virus and respiratory syncytial virus in an urgent care medical clinic. Clinical Infectious Diseases. 2010;50(5):693–698. doi: 10.1086/650457. [PubMed:20100093] [DOI] [PubMed] [Google Scholar]
- Ling M.L., Apisarnthanarak A., Madriaga G. The burden of healthcare-associated infections in southeast asia: A systematic literature review and meta-analysis. Clinical Infectious Diseases. 2015;60(11):1690–1699. doi: 10.1093/cid/civ095. [PubMed:25676799] [DOI] [PubMed] [Google Scholar]
- Lo J.Y., Tsang T.H., Leung Y.H., Yeung E.Y., Wu T., Lim W.W. Respiratory infections during SARS outbreak, Hong Kong, 2003. Emerging Infectious Diseases. 2005;11(11):1738–1741. doi: 10.3201/eid1111.050729. [PubMed:16318726] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb M., Dafoe N., Mahony J., John M., Sarabia A., Glavin V.…Walter S.D. Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA. 2009;302(17):1865–1871. doi: 10.1001/jama.2009.1466. [PubMed:19797474] [DOI] [PubMed] [Google Scholar]
- Lowen A.C., Mubareka S., Steel J., Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathogens. 2007;3(10):1470–1476. doi: 10.1371/journal.ppat.0030151. [PubMed:17953482] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen A.C., Steel J., Mubareka S., Palese P. High temperature (30 °C) blocks aerosol but not contact transmission of influenza virus. Journal of Virology. 2008;82(11):5650–5652. doi: 10.1128/JVI.00325-08. [PubMed:18367530] [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntyre C.R., Chughtai A.A. Facemasks for the prevention of infection in healthcare and community settings. BMJ. 2015;350:h694. doi: 10.1136/bmj.h694. [PubMed: 25858901] [DOI] [PubMed] [Google Scholar]
- McDevitt J., Rudnick S., First M., Spengler J. Role of absolute humidity in the inactivation of influenza viruses on stainless steel surfaces at elevated temperatures. Applied and Environmental Microbiology. 2010;76(12):3943–3947. doi: 10.1128/AEM.02674-09. [PubMed: 20435770] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt J.J., Rudnick S.N., Radonovich L.J. Aerosol susceptibility of influenza virus to UV-C light. Applied and Environmental Microbiology. 2012;78(6):1666–1669. doi: 10.1128/AEM.06960-11. [PubMed:22226954] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt J.J., Milton D.K., Rudnick S.N., First M.W. Inactivation of poxviruses by upper-room UVC light in a simulated hospital room environment. PLoS One. 2008;3(9):e3186. doi: 10.1371/journal.pone.0003186. [PubMed: 18781204] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt J.J., Lai K.M., Rudnick S.N., Houseman E.A., First M.W. Milton DK.Characterization of UVC light sensitivity of vaccinia virus. Applied and Environmental Microbiology. 2007;73(18):5760–5766. doi: 10.1128/AEM.00110-07. [PubMed:17644645] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milton D.K., Fabian M.P., Cowling B.J., Grantham M.L., McDevitt J.J. Influenza virus aerosols in human exhaled breath: Particle size, culturability, and effect of surgical masks. PLoS Pathogens. 2013;9(3):e1003205. doi: 10.1371/journal.ppat.1003205. [PubMed: 23505369] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell B.W., King D.J. Effect of negative air ionization on airborne transmission of Newcastle disease virus. Avian Diseases. 1994;38(4):725–732. [PubMed:7702504] [PubMed] [Google Scholar]
- Morter S., Bennet G., Fish J., Richards J., Allen D.J., Nawaz S.…Gray J. Norovirus in the hospital setting: virus introduction and spread within the hospital environment. Journal of Hospital Infection. 2011;77(2):106–112. doi: 10.1016/j.jhin.2010.09.035. [PubMed:21167622] [DOI] [PubMed] [Google Scholar]
- Mubareka S., Lowen A.C., Steel J., Coates A.L., García-Sastre A., Palese P. Transmission of influenza virus via aerosols and fomites in the guinea pig model. Journal of Infectious Diseases. 2009;199(6):858–865. doi: 10.1086/597073. [PubMed:19434931] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myatt T.A., Johnston S.L., Rudnick S., Milton D.K. Airborne rhinovirus detection and effect of ultraviolet irradiation on detection by a semi-nested RT-PCR assay. BMC Public Health. 2003;3:5. doi: 10.1186/1471-2458-3-5. [PubMed:12525263] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myatt T.A., Johnston S.L., Zuo Z., Wand M., Kebadze T., Rudnick S., Milton D.K. Detection of airborne rhinovirus and its relation to outdoor air supply in office environments. American Journal of Respiratory and Critical Care Medicine. 2004;169(11):1187–1190. doi: 10.1164/rccm.200306-760OC. [PubMed:14754759] [DOI] [PubMed] [Google Scholar]
- Nazaroff W.W. Norovirus, gastroenteritis, and indoor en¬vironmental quality. Indoor Air. 2011;21(5):353–356. doi: 10.1111/j.1600-0668.2011.00735.x. [PubMed:21906175] [DOI] [PubMed] [Google Scholar]
- Nazaroff W.W. Indoor bioaerosol dynamics. Indoor Air. 2016;26(1):61–78. doi: 10.1111/ina.12174. [PubMed:25483392] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen T.T., Poh M.K., Low J., Kalimuddin S., Thoon K.C., Ng W.C.…Gray G.C. Bioaerosol sampling in clinical settings: A promising, noninvasive approach for detecting respiratory viruses. Open Forum Infectious Diseases. 2016;4(1):ofw259. doi: 10.1093/ofid/ofw259. [PubMed:28480252] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicas M., Nazaroff W.W., Hubbard A. Toward understanding the risk of secondary airborne infection: emission of respirable pathogens. Journal of Occupational and Environmental Hygiene. 2005;2(3):143–154. doi: 10.1080/15459620590918466. [PubMed: 15764538] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholls J.M., Bourne A.J., Chen H., Guan Y., Peiris J.S. Sialic acid receptor detection in the human respiratory tract: evidence for widespread distribution of potential binding sites for human and avian influenza viruses. Respiratory Research. 2007;8:73. doi: 10.1186/1465-9921-8-73. [PubMed: 17961210] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterholm M.T., Moore K.A., Kelley N.S., Brosseau L.M., Wong G., Murphy F.A.…Sanders D.A., Kobinger G.P. Transmission of Ebola viruses: what we know and what we do not know. MBio. 2015;6(2):e00137. doi: 10.1128/mBio.00137-15. [PubMed: 25698835] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paschoalino M.P., Jardim W.F. Indoor air disinfection using a polyester supported TiO2 photo-reactor. Indoor Air. 2008;18(6):473–479. doi: 10.1111/j.1600-0668.2008.00548.x. [PubMed:18823342] [DOI] [PubMed] [Google Scholar]
- Pica N., Bouvier N.M. Environmental factors affecting the transmission of respiratory viruses. Current Opinion in Virology. 2012;2(1):90–95. doi: 10.1016/j.coviro.2011.12.003. [PubMed: 22440971] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyankov Oleg V., Pyankova Olga G., Agranovski Igor E. Inactivation of airborne influenza virus in the ambient air. Journal of Aerosol Science. 2012;53:21–28. doi: 10.1016/j.jaerosci.2017.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyankov Oleg V., Bodnev Sergey A., Pyankova Olga G., Agranovski Igor E. Survival of aerosolized coronavirus in the ambient air. Journal of Aerosol Science. 2017 doi: 10.1016/j.jaerosci.2017.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian H., Li Y., Nielsen P.V., Hyldgaard C.E., Wong T.W., Chwang A.T. Dispersion of exhaled droplet nuclei in a two-bed hospital ward with three different ventilation systems. Indoor Air. 2006;16(2):111–128. doi: 10.1111/j.1600-0668.2005.00407.x. [PubMed:16507039] [DOI] [PubMed] [Google Scholar]
- Rhinehart E., Walker S., Murphy D., O'Reilly K., Leeman P. Frequency of outbreak investigations in US hospitals: results of a national survey of infection preventionists. American Journal of Infection Control. 2012;40(1):2–8. doi: 10.1016/j.ajic.2011.10.003. [PubMed:22300590] [DOI] [PubMed] [Google Scholar]
- Rudnick S.N., McDevitt J.J., First M.W., Spengler J.D. Inactivating influenza viruses on surfaces using hydrogen peroxide or triethylene glycol at low vapor concentrations. American Journal of Infection Control. 2009;37(10):813–819. doi: 10.1016/j.ajic.2009.06.007. [PubMed:19822378] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakata H., Taketazu G., Nagaya K., Shirai M., Sugai R., Ikegami K., Maruyama S. Outbreak of severe infection due to adenovirus type 7 in a paediatric ward in Japan. Journal of Hospital Infection. 1998;39(3):207–211. doi: 10.1016/s0195-6701(98)90259-6. [PubMed:9699140] [DOI] [PubMed] [Google Scholar]
- Salgado C.D., Farr B.M., Hall K.K., Hayden F.G. Influenza in the acute hospital setting. Lancet Infectious Diseases. 2002;2(3):145–155. doi: 10.1016/s1473-3099(02)00221-9. [PubMed:11944184] [DOI] [PubMed] [Google Scholar]
- Scarpino P.V., Jensen N.J., Jensen P.A., Ward R. The use of ultraviolet germicidal irradiation (UVGI) in disinfection of airborne bacteria and rhinoviruses. Journal of Aerosol Science. 1998;29(Suppl.1):S777–S778. [Google Scholar]
- Schaffer F.L., Soergel M.E., Straube D.C. Survival of airborne influenza virus: effects of propagating host, relative humidity, and composition of spray fluids. Archives of Virology. 1976;51(4):263–273. doi: 10.1007/BF01317930. [PubMed:987765] [DOI] [PubMed] [Google Scholar]
- Schulz J., Bao E., Clauss M., Hartung J. The potential of a new air cleaner to reduce airborne microorganisms in pig house air: preliminary results. Berliner und Münchener tierärztliche Wochenschrift. 2013;126(3-4):143–148. [PubMed:23540197] [PubMed] [Google Scholar]
- Seale H., Weston K.M., Dwyer D.E., Zhu M., Allchin L., Booy R., MacIntyre C.R. The use of oseltamivir during an influenza B outbreak in a chronic care hospital. Influenza Other Respir Viruses. 2009;3(1):15–20. doi: 10.1111/j.1750-2659.2008.00063.x. [PubMed: 19453437] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seto W.H., Tsang D., Yung R.W., Ching T.Y., Ng T.K., Ho M.…Peiris J.S. Advisors of expert SARS group of hospital authority. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS) Lancet. 2003;361(9368):1519–1520. doi: 10.1016/S0140-6736(03)13168-6. [PubMed:12737864] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shears P., O'Dempsey T.J. Ebola virus disease in Africa: epidemiology and nosocomial transmission. Journal of Hospital Infection. 2015;90(1):1–9. doi: 10.1016/j.jhin.2015.01.002. [PubMed: 25655197] [DOI] [PubMed] [Google Scholar]
- Siegel J.D., Rhinehart E., Jackson M., Chiarello L. Health care infection control practices advisory committee. 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. American Journal of Infection Control. 2007;35(10 Suppl 2):S65–S164. doi: 10.1016/j.ajic.2007.10.007. [PubMed:18068815] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva Cde A., Dias L., Baltieri S.R., Rodrigues T.T., Takagi N.B., Richtmann R. Respiratory syncytial virus outbreak in neonatal intensive care unit: Impact of infection control measures plus palivizumab use. Antimicrob Resist Infect Control. 2012;1(1):16. doi: 10.1186/2047-2994-1-16. [PubMed: 22958306] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J.D., MacDougall C.C., Johnstone J., Copes R.A., Schwartz B., Garber G.E. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. CMAJ. 2016;188(8):567–574. doi: 10.1503/cmaj.150835. [PubMed:26952529] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spackova M., Altmann D., Eckmanns T., Koch J., Krause G. High level of gastrointestinal nosocomial infections in the german surveillance system, 2002-2008. Infection Control & Hospital Epidemiology. 2010;31(12):1273–1278. doi: 10.1086/657133. [PubMed:21047180] [DOI] [PubMed] [Google Scholar]
- Tang J.W. The effect of environmental parameters on the survival of airborne infectious agents. Journal of the Royal Society Interface. 2009;6(Suppl 6):S737–S746. doi: 10.1098/rsif.2009.0227.focus. [PubMed:19773291] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang J.W., Li Y., Eames I., Chan P.K., Ridgway G.L. Factors involved in the aerosol transmission of infection and control of ventilation in healthcare premises. Journal of Hospital Infection. 2006;64(2):100–114. doi: 10.1016/j.jhin.2006.05.022. [PubMed: 16916564] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellier R. Review of aerosol transmission of influenza A virus. Emerging Infectious Diseases. 2006;12(11):1657–1662. doi: 10.3201/eid1211.060426. [PubMed:17283614] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellier R. Aerosol transmission of influenza A virus: a review of new studies. Journal of the Royal Society Interface. 2009;6(Suppl 6):S783–S790. doi: 10.1098/rsif.2009.0302.focus. [PubMed:19773292] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terrier O., Essere B., Yver M., Barthélémy M., Bouscambert-Duchamp M., Kurtz P.…Moules V. Cold oxygen plasma technology efficiency against different airborne respiratory viruses. Journal of Clinical Virology. 2009;45(2):119–124. doi: 10.1016/j.jcv.2009.03.017. [PubMed:19406687] [DOI] [PubMed] [Google Scholar]
- Thomas P.G., Keating R., Hulse-Post D.J., Doherty P.C. Cell-mediated protection in influenza infection. Emerging Infectious Diseases. 2006;12(1):48–54. doi: 10.3201/eid1201.051237. [PubMed: 16494717] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorburn K., Eisenhut M., Riordan A. Mortality and morbidity of nosocomial respiratory syncytial virus (RSV) infection in ventilated children--a ten year perspective. Minerva Anestesiologica. 2012;78(7):782. [PubMed:22415435] [PubMed] [Google Scholar]
- Valenti W.M., Menegus M.A., Hall C.B., Pincus P.H., Douglas R.G., Jr. Nosocomial viral infections: I. Epidemiology and significance. Infection Control. 1980;1(1):33–37. doi: 10.1017/s0195941700052371. [PubMed: 6274823] [DOI] [PubMed] [Google Scholar]
- Van Voris L.P., Belshe R.B., Shaffer J.L. Nosocomial influenza B virus infection in the elderly. Annals of Internal Medicine. 1982;96(2):153–158. doi: 10.7326/0003-4819-96-2-153. [PubMed:7059061] [DOI] [PubMed] [Google Scholar]
- Verani M., Bigazzi R., Carducci A. Viral contamination of aerosol and surfaces through toilet use in health care and other settings. American Journal of Infection Control. 2014;42(7):758–762. doi: 10.1016/j.ajic.2014.03.026. [PubMed:24818773] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vetter P., Fischer W.A., 2nd, Schibler M., Jacobs M., Bausch D.G., Kaiser L. Ebola virus shedding and transmission: Review of current evidence. Journal of Infectious Diseases. 2016;214(Suppl 3):S177–S184. doi: 10.1093/infdis/jiw254. [PubMed: 27443613] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker C.M., Ko G. Effect of ultraviolet germicidal irradiation on viral aerosols. Environmental Science and Technology. 2007;41(15):5460–5465. doi: 10.1021/es070056u. [PubMed:17822117] [DOI] [PubMed] [Google Scholar]
- Wang Yutao, Yang Zifeng, Zhao Suishan, Li Runfeng, Guan Wenda, Qin Sheng, Zeng Guangqiao. Experimental study on effectiveness of cold oxygen plasma to influenza a virus. Chinese Journal of Nosocomiology. 2012;22(4):771–773. [Google Scholar]
- Weaver G.H. The value of the face mask and other measures in prevention of diphtheria, meningitis, pneumonia, etc. JAMA. 1918;70:76–78. [Google Scholar]
- Weingartl H.M., Embury-Hyatt C., Nfon C., Leung A., Smith G., Kobinger G. Transmission of Ebola virus from pigs to non-human primates. Scientific Reports. 2012;2:811. doi: 10.1038/srep00811. [PubMed:23155478] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitelaw T.H. The practical aspects of quarantine for influenza. Canadian Medical Association Journal. 1919;9(12):1070–1074. [PubMed:20311354] [PMC free article] [PubMed] [Google Scholar]
- Woo Myung-Heui, Grippin Adam, Wu Chang-Yu, Baney R.H. Use of dialdehyde starch treated filters for protection against airborne viruses. Journal of Aerosol Science. 2012;46:77–82. doi: 10.1016/j.jaerosci.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO). Report on the burden of endemic health care-associated infection worldwide. Geneva: World Health Organization; 2011. Report No.: 9789241501507.
- World Health Organization (WHO). Infection prevention and control of epidemic-and pandemic prone acute respiratory infections in health care - WHO guidelines. Geneva: World Health Organization; 2014.Available at: 〈http://www.who.int/csr/bioriskreduction/infection_control/publication/en/〉. [PubMed]
- Xie X., Li Y., Chwang A.T., Ho P.L., Seto W.H. How far droplets can move in indoor environments--revisiting the Wells evaporation-falling curve. Indoor Air. 2007;17(3):211–225. doi: 10.1111/j.1600-0668.2007.00469.x. [PubMed:17542834] [DOI] [PubMed] [Google Scholar]
- Yang W., Marr L.C. Mechanisms by which ambient humidity may affect viruses in aerosols. Applied and Environmental Microbiology. 2012;78(19):6781–6788. doi: 10.1128/AEM.01658-12. [PubMed: 22820337] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z., Suzuki A., Watanabe O., Okamoto M., Ohmi A., Huang W., Nishimura H. Outbreak of human metapneumovirus infection in a severe motor-and-intellectual disabilities ward in Japan. Japanese Journal of Infectious Diseases. 2014;67(4):318–321. doi: 10.7883/yoken.67.318. [PubMed: 25056083] [DOI] [PubMed] [Google Scholar]
- Yang Z.F., Mok C.K., Liu X.Q., Li X.B., He J.F., Guan W.D.…Zhong N.S. Clinical, virological and immunological features from patients infected with re-emergent avian-origin human H7N9 influenza disease of varying severity in Guangdong province. PLoS One. 2015;10(2):e0117846. doi: 10.1371/journal.pone.0117846. [PubMed:25723593] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen H.L., Liang C.H., Wu C.Y., Forrest H.L., Ferguson A., Choy K.T.…Peiris M. Hemagglutinin-neuraminidase balance confers respiratory-droplet transmissibility of the pandemic H1N1 influenza virus in ferrets. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(34):14264–14269. doi: 10.1073/pnas.1111000108. [PubMed: 21825167] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu I.T., Li Y., Wong T.W., Tam W., Chan A.T., Lee J.H.…Ho T. Evidence of airborne transmission of the severe acute respiratory syndrome virus. The New England Journal of Medicine. 2004;350(17):1731–1739. doi: 10.1056/NEJMoa032867. [PubMed: 15102999] [DOI] [PubMed] [Google Scholar]
- Yu Kuo-Pin, Lee Grace Whei-May, Lin Szu-Ying, Huang Chien Ping. Removal of bioaerosols by the combination of a photocatalytic filter and negative air ions. Journal of Aerosol Science. 2008;39(5):377–392. doi: 10.1016/j.jaerosci.2007.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Yao Z., Zhan S., Yang Z., Wei D., Zhang J.…Kyaw M.H. Disease burden of intensive care unit-acquired pneumonia in China: a systematic review and meta-analysis. International Journal of Infectious Diseases. 2014;29:84–90. doi: 10.1016/j.ijid.2014.05.030. [PubMed:25449241] [DOI] [PubMed] [Google Scholar]
- Zhang Yi, Guo Zhendong, Wang Zhongyi, Fu Yingying, Zhao Zongzheng, Liu Linna, Qian Jun. Comparison of traditional intranasal and aerosol inhalation inoculation of guinea pigs with visualizing influenza virus. Journal of Aerosol Science. 2017;110:43–52. [Google Scholar]
- Zhao Y., Aarnink A.J., Xin H. Inactivation of airborne Enterococcus faecalis and infectious bursal disease virus using a pilot-scale ultraviolet photocatalytic oxidation scrubber. Journal of the Air & Waste Management Association. 2014;64(1):38–46. doi: 10.1080/10962247.2013.831800. [PubMed:24620401] [DOI] [PubMed] [Google Scholar]