Abstract
Background
The 23-valent pneumococcal polysaccharide vaccine is recommended for elders, especially those with chronic conditions.
Objective
The aim of this study was to determine if an additional multi-component health education intervention increases the uptake rate of the pneumococcal vaccination among older patients with chronic diseases.
Methods
A cluster randomized controlled trial was conducted from 3 December 2007 to 7 March 2008. The clusters were the individual weeks within five Hong Kong outpatient clinics over a 10-week period. A sample of 2517 patients aged 65 or above with chronic diseases was recruited. Intervention group received a 3-min brief telephone education intervention before and a 3-min face-to-face intervention during scheduled medical appointments at the respective clinics. All subjects received standard care including health education leaflets and/or a video show at the clinics. Pneumococcal vaccination rate and awareness of the vaccination at 3-month follow up were measured.
Results
The vaccination rate was higher in the intervention group compared to the control group (57% vs 48%; relative risk = 1.20, 95% CI = 1.06–1.37), but the two groups did not differ significantly in their awareness of the vaccination at 3-month follow up (65% vs 59%, relative risk = 0.86, 95% CI = 0.69–1.07).
Discussion
A nurse-delivered brief health education intervention was effective in increasing uptake of pneumococcal vaccination among older patients with chronic diseases.
Keywords: Interventions, Older patients, Pneumococcal vaccination, Randomized controlled trial
What is already known about this topic?
-
•
Pneumococcal vaccination has been recommended for elders by the Hong Kong SAR Government since October 2007.
-
•
Pneumococcal vaccination is relatively new to people, especially in Hong Kong.
-
•
No study on testing the use of health educational programmes to promote pneumococcal vaccination uptake in the Asian countries.
What this paper adds
-
•
Evaluation of a nurse-delivered health education intervention which aimed to improve pneumococcal vaccination rate among older patients with chronic diseases.
-
•
The vaccination rate was higher in older patients who received a 3-min brief telephone education intervention and/or a 3-min face-to-face intervention than those only received standard care including health education leaflets and/or a video show at the clinics.
-
•
The two groups did not differ significantly in their awareness of the vaccination at 3-month follow up.
1. Introduction
Streptococcus pneumoniae causes invasive pneumococcal diseases (IPD) including septicaemia, meningitis and bacteraemic pneumonia in all age groups, especially in children, elders, and persons with chronic illnesses (Centers for Disease Control and Prevention, 1997). The incidence rate of IPD in older people is triple of those aged 15–64 years, and they have the highest risk of death from IPD (Robinson et al., 2001). Globally, IPD had caused 1.6 million deaths annually in 2005 (World Health Organization, 2012). In developed countries, the annual incidence rates of IPD range from 10 to 100 per 100,000 with higher incidence rates in those aged ≥65 years (20–80 per 100,000), whilst in Hong Kong the average annual incidence rate of IPD was 7.7 per 100,000 from 2000 to 2004 (Center for Health Protection, 2012).
The 23-valent pneumococcal polysaccharide vaccine (PPV) is recommended for elders, especially those with chronic conditions. PPV is efficacious in reducing the risk of systematic infection in institutionalized elders (Hutchison et al., 1999), and preventing mortality due to pneumonia (Fisman et al., 2006, Jackson et al., 2003, Loeb, 2003) from observational studies, but its efficacy from randomized controlled trials in older patients with chronic diseases, is still unclear and subject of debate (Moberley et al., 2008). As pneumococcal infections become increasingly difficult to treat due to drug resistance, vaccination is an important and efficient way for preventing IPD due to S. pneumonia (Spindler et al., 2008).
Despite recommendations made by governments in many western countries including Finland, Sweden, UK, US and some regions in Spain to deliver PPV to the elders and patients with chronic diseases, the vaccination rates vary substantially across countries. The uptake rates ranged from 3% in Finland to 60% in the US (Ruutu et al., 2004, United States Department of Health and Human Services, 2010). Several strategies involving health care professionals in improving the uptake rate of PPV have been proved effective in randomized trials. A computerized system reminding health professionals about the eligibility of patients for PPV increased the uptake rate from 0.8% to 35.8%, while an education program for patients through videotape-brochure was more effective than video-only and the control group (Dexter et al., 2001, Thomas et al., 2003). A program with educational outreaching visits about the importance of vaccination to practicing physicians and a nurse-delivered education intervention to patients on discharge increased the vaccination rates (Siriwardena et al., 2002, Thomas et al., 2005). However, to the best of our knowledge, no study on testing the use of a nurse-delivered brief telephone and face-to-face health education intervention to promote PPV uptake in Asian countries has been reported.
PPV has been recommended for elders by the Hong Kong SAR Government since October 2007 (Hutchison et al., 1999). Prior to 2007, vaccination for pneumococcal infection was not common and the estimated use of PPV was less than 10% for those aged over 65 years (Ho et al., 2004). The uptake rate of influenza vaccination was also very low even after the outbreak of Severe Acute Respiratory Syndrome and substantial promotion from the Government, as reflected by a 2004 study in Hong Kong which estimated that about 70% of patients visiting a public clinic did not have influenza vaccination within the past 5 years of the clinic visit (Mok et al., 2006). Consequently, additional efforts, other than mass media promotion, are needed to improve the uptake rate of vaccination. As PPV is relatively new to people in Hong Kong, it is important to implement and evaluate appropriate health education interventions to promote PPV and improve the vaccination rate, especially in vulnerable older patients with chronic diseases. Nurses are the largest group of health care professionals who have the greatest frequency and duration of contact with patients, and thus have a strong potential to influence patients’ behaviors. This large cluster randomized controlled trial, therefore, was conducted to test the effectiveness of a nurse-delivered multiple component health education intervention on the uptake rate of PPV and awareness of PPV at 3-month follow up among older patients with chronic diseases in Hong Kong.
2. Methods
2.1. Design, sample, and settings
A single-blinded cluster randomized controlled trial with stratification by clinic was conducted from 3 December 2007 to 7 March 2008 for 10 weeks (excluding the weeks of Christmas and Chinese New Year) in the five Hong Kong Hospital Authority West Cluster outpatient clinics. Each week of the 10 week study period was randomized to either intervention or control using random numbers generated by http://www.random.org. For each location, five weeks were allocated to intervention and five to the control. Thus, there were 25 clusters (i.e. study weeks) in the intervention and 25 clusters in the control, making a total of 50 clusters.
Two of the participating clinics are specialist outpatient clinics (SOPCs) providing acute patient care and specialist services in cardiothoracic and pulmonary diseases, respectively. The remaining three clinics are general outpatient clinics (GOPCs) which provide comprehensive primary medical care, serving an estimated population of 0.53 million in the Central, Western and Southern Districts of Hong Kong Island, Hong Kong. Subjects were eligible for inclusion if they were aged 65 years or above, had chronic diseases (hypertension, cardiac diseases, diabetes, respiratory diseases, kidney diseases, liver diseases, and cancers), had no prior PPV and had scheduled medical appointments at the 5 study sites during the study period. Older patients who were cognitively impaired, not able to communicate effectively, had any febrile respiratory illnesses or other active infections were excluded. This study was approved by University of Hong Kong and the Hong Kong West Cluster of Hospital Authority Institutional Review Board on November 17, 2007.
2.2. Procedures
Lists of all patients with medical appointments from 9:00 am to 5:00 pm of the five study sites each of the 10 study weeks were obtained from the respective clinics. One week before the medical appointments, two groups of trained research nurses (RNs) of the project called the eligible subjects in the intervention and control groups separately to confirm whether their self-reported medical diagnosis matched the inclusion criteria, and if yes, they were invited to participate in the study while those could not be reached before their scheduled appointments were considered as missing the opportunity for enrollment into the study. After obtaining oral consent, the project RNs responsible for the intervention group administered the baseline questionnaire and delivered the telephone health education intervention. The project RNs responsible for the control group administered the baseline questionnaire only. The baseline questionnaire collected information on subjects’ awareness of PPV, perceived stress, self-efficacy to manage disease in general, history of diseases and vaccinations, lifestyles and demographics.
During the selected 10-week medical appointment sessions of the 5 participating clinics, all patients, regardless of whether they had consented to participate in the study, received either the face-to-face health education intervention or standard care including promotional leaflets, poster displays, and health education video show, according to the cluster randomization. The 3-min face-to-face health education was delivered by the project RNs or a group of two medical/nursing students (during their clinical practicum) supervised by one of the project RNs in case there were students attending clinical practicum at the study clinics. However, only those who had consented and completed the baseline questionnaires before the medical appointments were included in the current study. PPV, if accepted, was administered by the nurses of the participating clinics to the patients according to the respective clinical procedures.
All subjects were contacted via telephone at 1-week and 3-month follow-up after their medical consultations. Trained research assistants who were blinded to subject group assignments conducted the telephone interviews using a structured follow-up questionnaire. The follow-up questionnaire collected information on subjects’ self-reported PPV status, awareness and beliefs of PPV, barriers of not up taking PPV, perceived stress and self-efficacy to manage disease in general. A subject was considered as lost-to-follow-up after non-response to eight telephone calls made at different times of the day/night.
2.3. Intervention
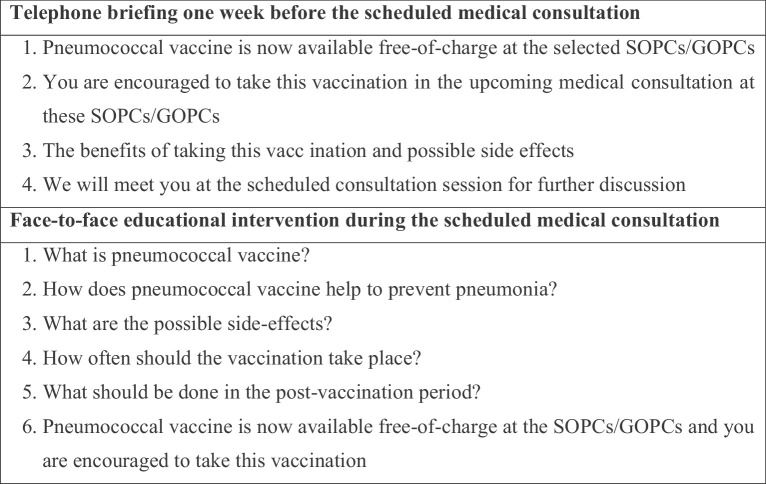
The health education intervention comprised of parts, a 3-min brief health education telephone intervention before and a 3-min face-to-face health education intervention during subjects’ medical appointments. The telephone briefing and face-to-face interventions, designed using the framework of pragmatism (Baert, 2004), included learning the facts of the health problem (pneumonia) and intervention (vaccination), and then the older patients were guided to interpret the given information from their own perspectives (to consider the pros and cons of receiving or rejecting the vaccination) so as to make decisions on whether to take the vaccination. The 3-min brief health education telephone intervention focused on the advantages and side effects of PPV, and highlighted the vaccine was free-of-charge at the selected clinics at the selected time. The face-to-face health education covered knowledge of PPV, including its nature and benefits, possible side-effects and care and support after receiving PPV. The control group received a reminder on their upcoming medical appointment after completing the baseline questionnaire. All study sites provided standard care including promotional leaflets, poster displays, and health education video show throughout the study period. Fig. 1 records the details of the health education intervention used in the current study.
Fig. 1.
Topics covered in the multi-component health education intervention for the intervention group.
All the RNs and medical and nursing students who were responsible to deliver the intervention had attended a one-day workshop delivered by the research team leaders on knowledge of PPV including its benefits and side effects, details of both parts of the health education interventions, study procedures and questionnaires, as well as communication skills with older patients.
2.4. Outcome measures
The primary outcome was the Hospital Authority Clinical Management System (CMS)-recorded uptake rate of PPV by 30 May 2008. The secondary outcome was awareness of PPV at 3-month follow-up. In addition, reasons for not taking the PPV were examined at 1-week follow-up.
2.5. Statistical analysis
The estimated 10% uptake rate of PPV reported previously in Hong Kong was not used for sample size calculation due to the changing situation in PPV provision in the community where PPV used to be only available in private clinics on a fee-for-service basis, and the HKSAR Government now provides free PPV in selected public hospitals. Thus, the required sample size calculated in the current study was on the basis of an increase in the vaccination rate from 54% to 61% (Thomas et al., 2005), a ratio of control to intervention participants of 1:1, 80% power, and a significance level of 5%. We did not have prior information regarding the intra-class correlation coefficient (ICC) on PPV in outpatient clinics in Hong Kong. Previous studies reported ICC was typically around 0.05 for primary care trials and usually less than 0.01 for community-based randomized trials (Campbell et al., 2007). As the current study included chronic patients receiving secondary care treatment in the clinics, we took the ICC = 0.01 in calculating the sample size. This gave a target sample size of a total 2250 subjects, with 1125 subjects in each group. We enrolled 45 subjects in each study week (one cluster) since there were 50 study weeks (10 weeks in 5 clinics) available in the trial.
Proportions and means were used to summarize subject characteristics. Generalized estimating equations (GEE) at the individual level to allow adjustment for clustering by study week using an exchangeable correlation structure were performed to compare the primary outcome and the secondary outcomes between the intervention and control groups. In GEE, models were fitted with adjustment for study week, clinic, three baseline variables of patient's educational level (primary level or below vs above primary level), whether had any type of vaccination in the past 12 months, and whether was aware of PPV. A sensitivity analysis using GEE was conducted by treating patients in the control group who also received the 3-min face-to-face health education at the clinic in the intervention group. Relative risks (RRs) and their 95% confidence intervals (CIs) were reported whenever applicable. Fisher exact tests were used to compare the reasons for not receiving PPV at 1-week follow up. All analyses (except the sensitivity analysis) were performed using SPSSv16.0 in 2009 and by intention-to-treat principle which is a strategy that compares study groups in terms of the treatment to which they were randomly allocated, rather than the treatment they actually received. In other words, analyses were performed according to the assigned treatment group, regardless of participant compliance, withdrawal or protocol deviation. Also, for the secondary outcome of awareness of PPV at 3-month, the patients who were lost to follow-up were treated as not aware of PPV.
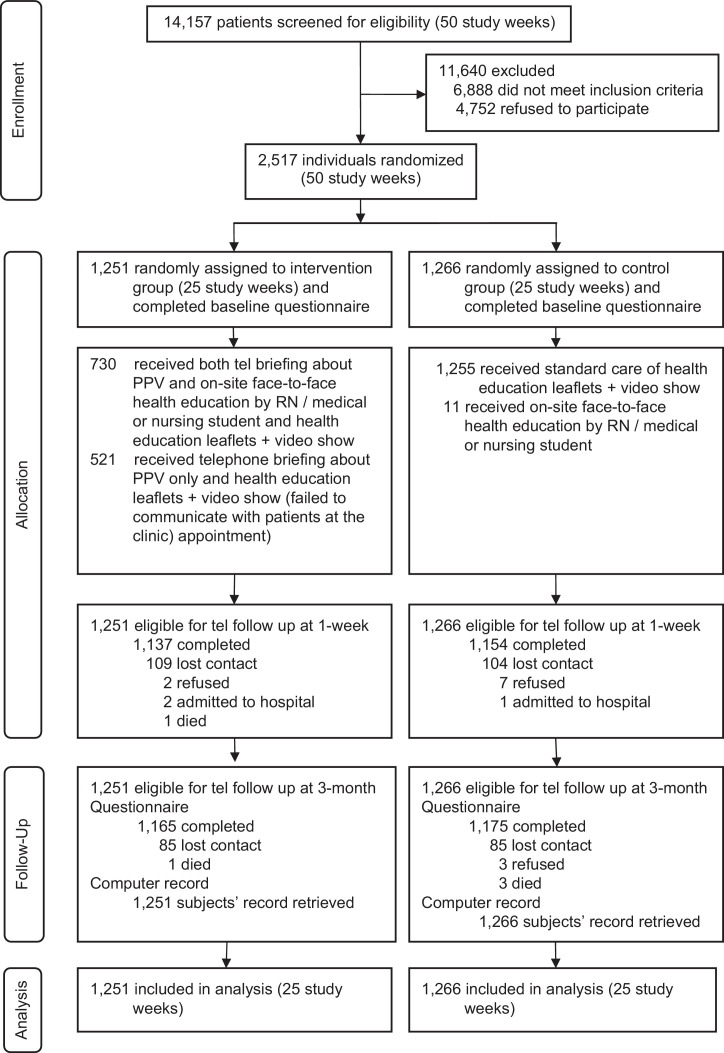
3. Results
A total of 14,157 patients were screened for study eligibility in the 5 participating clinics. Of the 7269 eligible subjects, a total of 2517 (35%) agreed to participate with 1251 in the intervention group and 1266 in the control group. In the intervention group, 730 (58%) of the subjects had received both the brief telephone intervention and the on-site face-to-face intervention (full compliance), while 521 (42%) received the brief telephone intervention about PPV only (partial compliance). However, an on-site nurse reported that 11 subjects in the control group also had also received the intervention but they remained in the control group by the intention-to-treat principle. A total of 1137 subjects (91%) in the intervention group and 1154 (91%) in the control group were successfully followed up at 1-week (follow up rate of 91%); and 1165 (93%) in the intervention group and 1175 (93%) in the control group at 3-month follow up (follow up rate of 93%) (Fig. 2 ). The 3-month follow up was completed in June 2008. The baseline variables between the intervention and control groups were similar (Table 1 ).
Fig. 2.
Flow chart of study participants through the trial.
Table 1.
Baseline characteristics of subjects in the intervention and control groups, n (%) unless otherwise stated.
| Characteristics | Intervention group (n = 1251) | Control group (n = 1266) |
|---|---|---|
| Mean (SD) age in years | 74.4 (5.4) | 74.7 (5.8) |
| Male | 519 (41) | 556 (44) |
| Married | 984 (79) | 928 (73) |
| Primary Education or below | 955 (76) | 928 (73) |
| More than 1 chronic disease | 412 (33) | 375 (30) |
| Current smoker | 77 (6) | 59 (5) |
| Current drinker | 90 (7) | 71 (6) |
| Exercise in the past 30 days | 982 (79) | 1027 (81) |
| Perceived good health in the past month | 991 (79) | 1013 (80) |
| Prior vaccination other than PPV | 610 (49) | 550 (43) |
| Awareness of PPV | 266 (21) | 314 (25) |
| Mean (SD) perceived stress (range: 0–4, higher score indicates higher stress)a | 1.26 (0.77) | 1.19 (0.78) |
| Mean (SD) self-efficacy in controlling disease (range: 0–4, higher score indicates better control)b | 2.50 (0.76) | 2.57 (0.81) |
PPV, pneumococcal polysaccharide vaccine.
11 subjects in the intervention group and 13 subjects in the control group did not complete the scale and were excluded from the analysis.
9 subjects in the intervention group and 8 subjects in the control group did not complete the scale and were excluded from the analysis.
By May 30, 2008, a total of 1325 (53%) subjects received the PPV injection during the study period as recorded in the CMS, with 716 (57%) subjects in the intervention group and 609 (48%) in the control group. The ICC of the CMS-recorded PPV uptake in the study by randomizing the study time in the participating clinics was 0.051. When adjusted for clustering effects using GEE, the adjusted relative risk (ARR) for CMS-recorded PPV uptake associated with the intervention was 1.20 (95% CI = 1.06–1.37). The intervention effect remained significant (ARR = 1.3, 95% CI = 1.09–1.45) after treating the 11 patients in the control group who received the face-to-face health education as intervention subjects in the sensitivity analysis.
The two groups, however, were similar in awareness of PPV at 3-month follow up (n = 803, 64% vs n = 734, 58%) and its corresponding ICC was 0.082. From the GEE results, the adjusted relative risk for the awareness of PPV at 3-month follow up was 0.86 (95% CI = 0.69–1.07), indicating no intervention effect. The intervention effect on the awareness of PPV remained insignificant (ARR = 1.06, 95% CI = 0.94–1.20) in the sensitivity analysis. At 3-month follow up, 800 (64%) subjects of the intervention group and 772 (61%) of the control group reported that the nurses had advised them to receive PPV, while only 162 (13%) subjects of the intervention group and 215 (17%) of the control group reported they received advice from the doctors.
Of the 2291 subjects completed 1-week follow up survey, 448 (20%) subjects in intervention group and 532 (23%) in control group did not receive the vaccination. Exploratory analysis of these subjects revealed fewer subjects in the intervention group reported no need for the vaccination, had received all necessary vaccinations, and lack of knowledge about the availability and accessibility of the vaccination, while more subjects in the intervention group reported they did not want to receive PPV, as compared to the control group (Table 2 ) and these differences were statistically significant. It is worth noting that 24 (5.4%) subjects of the intervention group and 17 (3.2%) of the control group reported that they were suggested not to receive PPV by their physicians.
Table 2.
PPVa uptake and reasons for not receiving PPV at 1-week.
| Intervention (n = 1251) | Control (n = 1266) | ARRb (95% CI) | |
|---|---|---|---|
| Computer-recorded PPV uptake n (%) | 716 (57.2) | 609 (48.1) | 1.2 (1.06, 1.37) |
| Awareness of PPV at 3-month, n (%) | 803 (64.2) | 734 (58.0) | 0.86 (0.69, 1.07) |
| Reason(s) for not receiving PPV at 1-week | Intervention (n = 448) | Control (n = 532) | p-Value |
|---|---|---|---|
| No need to receive PPV | 130 (29.0) | 188 (35.3) | 0.040 |
| Had received all necessary vaccinations | 27 (6.0) | 62 (11.7) | 0.002 |
| Too expensive | 1 (0.2) | 2 (0.4) | 1.000 |
| Don’t know where to receive vaccination | 37 (8.3) | 75 (14.1) | 0.005 |
| Sick/not feeling well | 28 (6.3) | 35 (6.6) | 0.896 |
| Would have surgery soon | 8 (1.8) | 8 (1.5) | 0.803 |
| No time | 5 (1.1) | 1 (0.2) | 0.099 |
| No one mentioned abut PPV at medical appointment | 25 (5.6) | 30 (5.6) | 1.000 |
| Have PPV later | 11 (2.5) | 7 (1.3) | 0.234 |
| Doctor did not recommend | 24 (5.4) | 17 (3.2) | 0.109 |
| Don’t want to receive PPV | 15 (3.3) | 2 (0.4) | <0.001 |
| Forgot to follow-up | 12 (2.7) | 12 (2.3) | 0.684 |
| Afraid of side effects of PPV/injection | 113 (25.2) | 68 (12.8) | <0.001 |
| Others | 12 (2.7) | 25 (4.7) | 0.129 |
PPV, pneumococcal polysaccharide vaccine.
Relative risk (RR) for Clinical Management System-recorded PPV uptake associated with the intervention adjusted for the effects of clustering, clinic, patient's educational level, whether have vaccination in the past 12 months and whether was aware of PPV at baseline.
4. Discussion
A multiple-component brief health education intervention including a 3-min telephone briefing and a 3-min face-to-face education intervention was effective in motivating 716 (57%) of the older patients to receive PPV vs 609 (48%) in the control group, a 9% increase. Although not directly comparable, the uptake rate in the intervention group was similar to a previous study using a nurse-delivered intervention with face-to-face patient contact. Winston et al. (2007) reported a much lower uptake rate using a similar ‘telephone outreach’ intervention (<20%) among a community older adult group (Winston et al., 2007); and other studies reported a comparably higher uptake rate (52%) with a more intensive approach such as promotional intervention, educational brochures, and a reply card (Krieger et al., 2000). These results indicated that there are multiple strategies to improve vaccination uptake, and it seems that uptake rates may increase with intensity of the intervention.
Furthermore, both intervention and control groups showed a marked increase in the overall awareness of PPV (n = 1537, 61%) at 3-month follow up comparing at baseline (n = 579, 23%), although there was no between group difference. The overall standard promotion of PPV at the clinics, and the telephone calls prior to the scheduled appointments for completing the baseline questionnaires might have exerted some effects on raising the awareness of PPV in both groups. Providing health information such as promotional leaflet, poster, and educational video can raise the awareness of patients about the health problems, but adding a multiple component health education intervention, with direct communication with the older patients offering an opportunity for support can further motivate older patients to receive PPV. Subjects in this study were older patients with chronic diseases and low education levels, and hence these patients might need a more direct approach in communicating health messages such as face-to-face counseling, so that opportunities were given to ask questions, if any.
About one-third of the patients who did not receive the vaccination reported that there was no need to receive the vaccine, suggesting more intensive intervention is needed to understand the reasons behind such thoughts and to motivate this group to consider the vaccination. Although previous studies showed that advice from physicians on PPV was one of the crucial factors in promoting the uptake of the vaccination (United States Department of Health and Human Services, 2010), family doctors at the clinics in Hong Kong have a very heavy workload that they can only spend a few minutes with every patient (Hedley, 1990). Hence nurses can fill this important gap, and as indicated in this study, about two-third of the patients reported they had received advices from nurses about receiving PPV.
It is worth noting that 25% (n = 113) of the intervention group who did not receive PPV reported it was because of the expected side effects of PPV as compared to 13% (n = 68) in the control group. This result suggested that the older patients might have negative perception on the health information provided by the nurses and developed some anxiety toward the vaccination leading to an adverse effect on the PPV uptake rates in the intervention group. Further programmes thus should allow more time to discuss the side effects and adopt an appropriate balance of highlighting the benefits and possible side effects of PPV injection.
Finally, the study has provided estimate of ICC on older patients with chronic diseases with regular visits to clinics for secondary care prevention which is very important in large vaccination studies as such an estimate of ICC can enable accurate sample size estimation in further studies in a similar context. Nevertheless, there were a few limitations in this study. First, the subjects were limited to older patients with chronic diseases and hence the results may not be entirely comparable to other studies which targeted all elders aged over 65 years. Furthermore, although all the five selected clinics were from the same region in Hong Kong, they had variations in their services provided and population served. For example, the three GOPCs provided primary medical care services and their patients had less acute chronic illnesses such as hypertension, while the two SOPCs provided follow up consultations, and their patients might have more acute illnesses and usually require more frequent follow ups. Further studies with a wider coverage of all elders from different regions in Hong Kong would be desirable. Second, only 58.4% (n = 730) of the patients in the intervention group had received both telephone briefing and on-site face-to-face intervention in the real clinical situation, hence the intervention effect could have been weakened. This situation was due to the busy day-to-day clinic routine, thus preventing the nurses from approaching all the randomized patients. In addition, some patients in both groups did not turn up at their scheduled appointments and hence did not receive the onsite intervention, leading to a 41.6% (n = 521) of the intervention group only received telephone briefing. Although the sensitive analysis showed the intervention effect remained significant by treating the 11 patients in the control group who had received the face-to-face health education at the clinics, future studies would require integrating health education into clinic procedures to improve efficiency. Third, we had underestimated the ICC in sample size calculation that the ICC in this study was similar to clinical studies, not in between clinical and community studies (Campbell et al., 2007) as expected. The underestimation of ICC inevitably lowered the statistical power of the study. A retrospective calculation of the power of the study using an estimated ICC of 0.051 indicating the study only has a power of 0.44 to detect a difference on 7% in the PPV uptake rates between the two groups at a 5% significance level. Fourth, the physical space of some clinics was very small and crowded with patients with no designated space for delivering health education, hence limiting the quality of delivering the intervention. Fifth, we had included medical and nursing students to deliver the second component of the intervention which might have induced variability in the quality of the intervention, although prior training was provided. Because they had less experience in health promotion, the intervention effect might have been weakened. Finally, only one-third of the eligible patients consented to the study which might also limited the generalizability of the current findings. The situation, however, was expected as PPV was very new to people in Hong Kong and a certain degree of reluctance to try a new type of vaccination is expected. Furthermore, the study included multiple components and follow-up telephone calls and older patients might not want to be engaged into these activities. As a result, those participated in the study could be more cooperative and willing to take risks (from the patient's perspective) and hence willingness to receive PPV might be greater in both groups.
5. Conclusions
A nurse-delivered brief multi-component health education intervention was effective in promoting and increasing uptake of PPV among older patients with chronic diseases. The traditional mode of uni-directional health education using pamphlets and videos can increase the awareness of health actions, but may not be able to change behaviors. Physicians’ advice has shown to be effective in increasing the uptake of PPV, but as nurses have more frequent contact with patients, they can fill this important gap and provide more direct communication with patients in motivating them to take appropriate health actions such as receiving PPV.
Acknowledgements
We would like to express gratitude to the five Hong Kong Hospital Authority West Cluster outpatient clinics under Hospital Authority for their assistance during the study period.
Conflict of interest: None declared.
Funding: This study was supported by a donation from the Li Ka Shing Foundation, the University of Hong Kong and the Hospital Authority.
Ethical approval: Approved by University of Hong Kong and the Hong Kong West Cluster of Hospital Authority Institutional Review Board on November 17, 2007; Hong Kong University Clinical Trial Register HKCTR-550.
References
- Baert P. Pragmatism as a philosophy of the social sciences. Eur. J. Soc. Theor. 2004;7(3):355–369. [Google Scholar]
- Campbell M.J., Donner A., Klar N. Developments in cluster randomized trials and statistics in medicine. Stat. Med. 2007;26(1):2–19. doi: 10.1002/sim.2731. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Prevention of pneumococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Morb. Mortal. Wkly. Rep. 1997;46:1–24. [Google Scholar]
- Center for Health Protection . 2012. Scientific Committee on Vaccine Preventable Diseases Recommendations on the Use of Pneumococcal Vaccines. Available at http://www.chp.gov.hk/files/pdf/Recommendations_on_the_Use_of_Pneumococcal_Vaccines.pdf (accessed 04.10.12) [Google Scholar]
- Dexter P.R., Perkins S., Overhage J.M., Maharry K., Kohler R.B., McDonald C.J. A computerized reminder system to increase the use of preventive care for hospitalized patients. N. Engl. J. Med. 2001;345(13):965–970. doi: 10.1056/NEJMsa010181. [DOI] [PubMed] [Google Scholar]
- Fisman D.N., Abrutyn E., Spaude K.A., Kim A., Kirchner C., Daley J. Prior pneumococcal vaccination is associated with reduced death, complications, and length of stay among hospitalized adults with community-acquired pneumonia. Clin. Infect. Dis. 2006;42(8):1093–1101. doi: 10.1086/501354. [DOI] [PubMed] [Google Scholar]
- Hedley A.J. Problems in the delivery of primary health care in the public and private sections. Hong Kong Pract. 1990;12:1098–1105. [Google Scholar]
- Ho P.L., Que T.L., Chiu S.S., Yung R.W., Ng T.K., Tsang D.N., Lau Y.L. Fluoroquinolone and other antimicrobial resistance in invasive pneumococci, Hong Kong, 1995–2001. Emerg. Infect. Dis. 2004;10(7):1250–1257. doi: 10.3201/eid1007.030612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchison B.G., Oxman A.D., Shannon H.S., Lloyd S., Altmayer C.A., Thomas K. Clinical effectiveness of pneumococcal vaccine. Meta-analysis. Can. Fam. Physician. 1999;45:2381–2393. [PMC free article] [PubMed] [Google Scholar]
- Jackson L.A., Neuzil K.M., Yu O., Benson P., Barlow W.E., Adams A.L., Thompson W.W. Effectiveness of pneumococcal polysaccharide vaccine in older adults. N. Engl. J. Med. 2003;348(18):1747–1755. doi: 10.1056/NEJMoa022678. [DOI] [PubMed] [Google Scholar]
- Krieger J.W., Castorina J.S., Walls M.L., Weaver M.R., Ciske S. Increasing influenza and pneumococcal immunization rates: a randomized controlled study of a senior center-based intervention. Am. J. Prev. Med. 2000;18(2):123–131. doi: 10.1016/s0749-3797(99)00134-8. [DOI] [PubMed] [Google Scholar]
- Loeb M. Pneumonia in older persons. Clin. Infect. Dis. 2003;37(10):1335–1339. doi: 10.1086/379076. [DOI] [PubMed] [Google Scholar]
- Moberley S.A., Holden J., Tatham D.P., Andrews R.M. Vaccines for preventing pneumococcal infection in adults. Cochrane Database Syst. Rev. 2008;(1):CD000422. doi: 10.1002/14651858.CD000422.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mok E., Yeung S.H., Chan M.F. Prevalence of influenza vaccination and correlates of intention to be vaccinated among Hong Kong Chinese. Public Health Nurs. 2006;23(6):506–515. doi: 10.1111/j.1525-1446.2006.00590.x. [DOI] [PubMed] [Google Scholar]
- Robinson K.A., Baughman W., Rothrock G. Epidemiology of invasive Streptococcus pneumoniae infections in the united states, 1995–1998: opportunities for prevention in the conjugate vaccine era. JAMA. 2001;285(13):1729–1735. doi: 10.1001/jama.285.13.1729. [DOI] [PubMed] [Google Scholar]
- Ruutu P., Kuusi M., Nuorti P.J., Koskinen S. National Public Health Institute; Helsinki: 2004. Communicable Diseases. [Google Scholar]
- Siriwardena A.N., Rashid A., Johnson M.R., Dewey M.E. Cluster randomised controlled trial of an educational outreach visit to improve influenza and pneumococcal immunisation rates in primary care. Br. J. Gen. Pract. 2002;52(482):735–740. [PMC free article] [PubMed] [Google Scholar]
- Spindler C., Hedlund J., Jasir A., Normark B.H., Örtqvist Å. Effects of a large-scale introduction of the pneumococcal polysaccharide vaccine among elderly persons in Stockholm, Sweden. Vaccine. 2008;26(43):5541–5546. doi: 10.1016/j.vaccine.2008.06.073. [DOI] [PubMed] [Google Scholar]
- Thomas C., Loewen A., Coffin C., Campbell N. Improving rates of pneumococcal vaccination on discharge from a tertiary center medical teaching unit: a prospective intervention. BMC Public Health. 2005;5(1):110. doi: 10.1186/1471-2458-5-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas D.M., Ray S.M., Morton F.J., Drew J.S., Offutt G., Whitney C.G., Jacobson T.A. Patient education strategies to improve pneumococcal vaccination rates: randomized trial. J. Investig. Med. 2003;51(3):141–148. doi: 10.1136/jim-51-03-16. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics . 2010. National Health Interview Survey 2009. [Google Scholar]
- Winston C.A., Mims A.D., Leatherwood K.A. Increasing pneumococcal vaccination in managed care through telephone outreach. Am. J. Manag. Care. 2007;13(10):581–588. [PubMed] [Google Scholar]
- World Health Organization . 2012. Pneumococcal Conjugate Vaccines. Available at http://www.who.int/biologicals/areas/vaccines/pneumo/en/ (accessed 04.10.12) [Google Scholar]