Abstract
In December 2003, the largest outbreak of highly pathogenic avian influenza H5N1 occurred among poultry in 8 Asian countries. A limited number of human H5N1 infections have been reported from Vietnam and Thailand, with a mortality rate approaching 70%. Deaths have occurred in otherwise healthy young individuals, which is reminiscent of the 1918 Spanish influenza pandemic. The main presenting features were fever, pneumonitis, lymphopenia, and diarrhea. Notably, sore throat, conjunctivitis, and coryza were absent. The H5N1 strains are resistant to amantadine and rimantadine but are susceptible to neuraminidase inhibitors, which can be used for treatment and prophylaxis. The widespread epidemic of avian influenza in domestic birds increases the likelihood for mutational events and genetic reassortment. The threat of a future pandemic from avian influenza is real. Adequate surveillance, development of vaccines, outbreak preparedness, and pandemic influenza planning are important. This article summarizes the current knowledge on avian influenza, including the virology, epidemiology, diagnosis, and management of this emerging disease.
Since mid-December 2003, 8 Asian countries—Cambodia, China, Indonesia, Japan, Laos, South Korea, Thailand, and Vietnam—have reported outbreaks of highly pathogenic avian influenza caused by the H5N1 strain among poultry. This is the largest outbreak of avian influenza in poultry ever described. Most of these countries experienced outbreaks of avian influenza for the first time. During the past 3 months, more than 100 million domestic poultry have died, or they have been culled to contain the epidemic and prevent the potential transmission to humans. Despite the widespread infection of avian influenza viruses among poultry in Asia, reported infection in humans has been rare to date. As of March 8, 2004, only Vietnam and Thailand have reported influenza H5N1 infection in humans. Thirty-two human cases were laboratory confirmed, resulting in 22 deaths, a mortality rate approaching 70%.1 However, most of the affected countries have limited capacity for surveillance of human disease. In addition, poultry production contributes substantially to the economies of the affected countries, resulting in considerable political pressure to minimize the extent and seriousness of the epidemic. Therefore, the reported human cases of avian influenza may be underestimated.
Historically, this avian epidemic zoonosis is unprecedented in its scale, geographical distribution, economic losses, challenge for control, and potential public health consequences.2 The potential development of a human influenza pandemic similar to that of 1918 due to Spanish influenza is a major concern. Two of the 3 key criteria that characterized the pandemic of 1918-1919 have already been fulfilled in the current epidemic: (1) the ability of the virus to infect humans resulting in high mortality and (2) a global immunologically naive human population.3 The third criterion, efficient human-to-human transmission, has thus far not been observed.4 The adaptation that would result in human-to-human transmission might involve changes in the receptor properties or improved viral replication efficiency. This adaptation might be achieved by mutation of an avian virus genome or by mixing segments of an avian virus with segments from a virus already adapted to humans (genetic reassortment), leading to the emergence of a new influenza subtype with pandemic potential.5 Both events may occur easily. First, influenza viruses mutate frequently, potentially allowing them to change the host receptor specificity from avian to human.6 Second, the segmented viral genome allows the exchange of genes between viruses if they infect the same host cell, which serves as the “mixing vessel.”7
In the current H5N1 outbreak in Asia, no genetic reassortment among avian and human influenza viruses has been found; all genes are of avian origin.4, 8 However, the widespread epidemic of avian influenza in domestic birds increases the likelihood for mutational events and genetic reassortment. In view of the high mortality observed in the limited number of infections in humans, the prospect of a severe pandemic is of considerable importance.9 We review current knowledge about avian influenza, including the virology, epidemiology, diagnosis, and management of this emerging disease.
VIROLOGY
Antigenic Diversity
Influenza viruses type A, B, and C belong to the family of Orthomyxoviridae. These enveloped viruses contain a segmented single-stranded RNA genome. A key difference among influenza virus types is their host range.10 Type A viruses have been isolated from a wide range of species, including humans, pigs, horses, seals, ferrets, mink, whales, and birds. Types B and C viruses infect humans predominantly but have also been isolated from seals and pigs, respectively.7 Influenza A viruses can be divided into subtypes based on surface glycoproteins, hemagglutinin and neuraminidase. To date, 15 different hemagglutinin (H1-H15) and 9 neuraminidase (N1-N9) proteins have been identified.10 Hemagglutinin facilitates entry of the virus into host cells through its attachment to sialic acid on epithelial cell receptors, promotes membrane fusion, and elicits protective neutralizing antibody response. Hemagglutinin is the crucial component of influenza vaccines. Neuraminidase has enzyme activity, which cleaves sialic acid on virion proteins, facilitating the release of progeny virions from infected cells. It is an important target for antiviral agents.11 Although all influenza A virus subtypes have been found in birds, only 3 different hemagglutinin (H1, H2, or H3) and 2 different neuraminidase (N1 or N2) proteins have circulated widely in humans.
A Constantly Changing Virus
The antigenic characteristics of influenza virus change gradually by accumulation of point mutations (antigenic drift) or profoundly by genetic reassortment (antigenic shift) in the genes encoding primarily hemagglutinin and neuraminidase. During antigenic drift, mutations occur because of the lack of the proofreading activity of viral RNA polymerases. As a consequence, new antigenic variants emerge constantly, allowing the virus to evade immune recognition and giving rise to annual epidemics. The antigenic drift of influenza viruses requires the replacement of influenza strains used in the vaccine every several years.12 During antigenic shift, new strains appear to which most humans have no immunity and that have the potential to cause severe global outbreaks of human influenza. These pandemic strains derive from nonhuman viruses by interspecies transmission of the whole virus or by genetic reassortment between avian and human viruses that have infected a single cell. Pigs have receptors for both avian and human influenza viruses and have been considered an intermediate host for the reassortment of influenza viruses. Reemergence of a previously circulating virus to which most of the population is immunologically naive is another mechanism by which pandemic strains can occur.13
The nomenclature of influenza viruses includes the type of virus (A, B, or C), host of origin (excluding humans), geographical site of origin, strain number, and year of isolation, followed in parentheses by the antigenic description of the hemagglutinin and neuraminidase glycoproteins, eg, A/chicken/Hong Kong/258/97 (H5N1).
Interspecies Transmission
Avian influenza viruses do not replicate efficiently in humans, which suggested initially that direct avian-to-human transmission would not occur. The hemagglutinins of avian strains bind preferentially to host receptors terminating in an α(2,3)-linked sialic acid, whereas human strains bind preferentially to receptors terminating in an α(2,6)-linkage. The predominance of these receptors in different tissues partly reflects the tropism of influenza in different species.5 Receptor specificity and inability of efficient replication in vivo were believed to provide a barrier against human infection by avian influenza virus. High doses of avian influenza virus strains were required for replication in volunteers. The first human infections by avian H5N1 virus in Hong Kong in 1997 showed that receptor specificity was not a definitive host restriction factor.14 In this epidemic, an intermediate host was not necessary for transmission of avian strains to humans.
AVIAN INFLUENZA IN ANIMALS
Influenza in Wild Animals
All birds are thought to be susceptible to infection with avian influenza viruses. Wild waterfowl and migrating bird populations provide an extensive natural reservoir for influenza A viruses (Figure 1 ).15 The virus multiplies in the intestines of these birds, particularly in wild ducks, and they can carry the virus without developing signs of infection, indicating an optimal level of viral adaptation in these hosts. Therefore, influenza is not an eradicable disease, and prevention and control of outbreaks are the only realistic goals.16 Unlike mammalian influenza virus strains, avian viruses have shown little antigenic variability during the past decades. The high level of genetic conservation suggests that avian viruses have reached an evolutionary stage in which antigenic changes provide no selective advantage.
Figure 1.
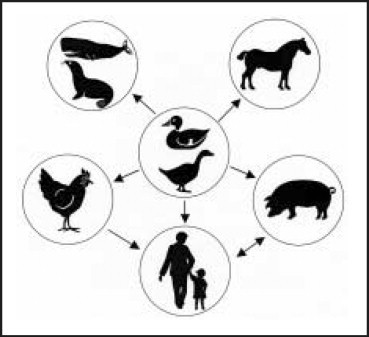
Wild aquatic birds are the main reservoir for influenza A viruses, from which viruses can be transmitted to other hosts such as horses, pigs, poultry, whales, seals, and humans. As indicated by arrows, humans can also be infected by pigs and poultry.
Infected birds excrete large amounts of virus in respiratory secretions, saliva, and feces. In the Northern Hemisphere, the prevalence of avian influenza peaks between late summer and early winter when the birds leave their breeding grounds and migrate; up to 30% of these birds may excrete virus.15 Water sources that are contaminated by wild bird droppings and used by domestic poultry are a common and efficient means of viral spread. Migratory birds are capable of flying long distances, and those migrating longitudinally appear to play a key role in viral transmission.7
Influenza in Domestic Animals
The fowl plague was first described in 1878 as a disease affecting chickens in Italy. The causative agent was isolated from a chicken in 1902, which was the first identified influenza virus (the human influenza virus was not identified until 1933). Domestic poultry flocks are highly vulnerable to avian influenza, particularly birds that are raised outdoors. Once introduced into domestic flocks, the virus can spread among farms via contaminated inanimate objects, contributing to the rapid evolution of epidemics. Avian influenza in birds is characterized by a wide spectrum of symptoms, ranging from a mild illness to a highly contagious, severe, and rapidly fatal disease with a mortality rate approaching 100%. The latter syndrome was formerly known as fowl plague; it is now termed highly pathogenic avian influenza and is characterized by coughing, sneezing, excessive lacrimation, cyanosis of the unfeathered skin, edema of the head, ruffled feathers, diarrhea, nervous system disorders, or sudden death without clinical signs.15 In the past, most outbreaks of highly pathogenic avian influenza in poultry have been due to subtypes H5 or H7.
Epidemics of avian influenza among poultry have produced serious economic consequences.7 In addition to a highly pathogenic avian influenza, viruses of low pathogenicity resulting in mild respiratory symptoms and reduced egg production can cause substantial economic losses. In 1995, 178 turkey farms in Minnesota were affected by influenza virus H9N2, resulting in an economic loss of approximately $6 million.15 Moreover, avian influenza viruses of low pathogenicity can mutate into highly pathogenic viruses after circulating for several months. During the 1999-2001 epidemic in Italy, the H7N1 virus mutated within 9 months to a highly pathogenic form, and more than 13 million birds died or were culled.1
Since 1997, outbreaks of highly pathogenic avian influenza have increased in frequency and severity, and the number of novel strains suggests that the next influenza pandemic is imminent.9 In 2004, outbreaks of highly pathogenic avian influenza occurred among chickens at farms in Delaware, Pennsylvania, Texas, and Maryland. The diseased and exposed birds were killed, and a quarantine zone was implemented around the affected farms. On February 20, 2004, H5N1 infection was confirmed in 2 dead domestic cats and in a tiger in a zoo in Thailand. To date, these animals have not been considered susceptible to influenza viruses. This raises concern about the need for surveillance in animals other than birds.1
Breeding Ground for Avian Influenza
Since the late 1970s, live poultry markets have been considered the source of human influenza viruses. These permanent live animal markets (wet markets) are embedded strongly in the food culture of Asian countries. Close human contact with live animals provides an ideal environment for the zoonotic transfer and evolution of infectious disease agents.17 The most important control measure for containing the outbreak in Hong Kong in 1997 was rapid destruction of the entire poultry population, proper disposal of carcasses, and rigorous disinfection of farms. To reduce the risk of reemergence of avian influenza, all aquatic birds were removed from retail markets, including ducks, geese, and quails (source of the H5N1 strain). Monthly “clean days” were introduced when all markets are emptied and cleaned simultaneously. New regulations mandate quarantine of poultry in designated farms in mainland China for 5 days and testing for H5 infection before importation to Hong Kong.18 Other control measures include continuous surveillance of influenza virus strains in humans and in birds, careful protection of cullers through appropriate personal protective equipment, restrictions on the movement of live poultry, and use of the human influenza vaccine to reduce the risk of coinfection in poultry workers and cullers.4
HUMAN INFLUENZA
Severe Influenza Pandemics Throughout History
A global outbreak of influenza usually occurs when a new influenza virus emerges, spreads, and causes disease worldwide.13 Descriptions of widespread and serious epidemics of respiratory disease suggestive of influenza have been recorded for centuries. Hippocrates in ancient Greece described the first case of influenza-like illness. In the 20th century, 4 human influenza pandemics emerged with intervals of 9 to 39 years .14 The Spanish influenza of 1918-1919 (H1N1) was the most devastating pandemic in recorded human history, resulting in 25 to 50 million deaths worldwide; nearly half of those who died were healthy young adults. This figure is at least double the number of soldiers killed on the battlefields of Europe during World War I. Other less catastrophic pandemics occurred in 1957 (Asian influenza), 1968 (Hong Kong influenza), and 1977 (Russian influenza). The Asian (H2N2) and Hong Kong (H3N2) pandemic strains were generated by reassortment between human and avian viral genes. The Russian influenza virus (H1N1) circulated in the 1950s and reemerged in 1977. The illness occurred almost exclusively among persons younger than 20 years. The relatively low mortality rate associated with this pandemic can be attributed to the immunity of older individuals who had antibodies from their previous exposure to nearly identical viruses.7
Transmission of Avian Influenza Viruses to Humans
To date, human infection with avian influenza viruses has been confirmed on several occasions (Table 1 ). In 1997, the first documented direct transmission of an avian influenza virus to humans occurred in Hong Kong, when an H5N1 strain caused a severe respiratory disease in 18 previously healthy young adults, 6 of whom died.3 The outbreak in Hong Kong was controlled by the destruction of the entire poultry population; within 3 days, more than 1.5 million chickens were killed. In 1999, avian influenza H9N2 viruses were isolated for the first time in humans; 2 children were hospitalized with uncomplicated upper respiratory tract infection in Hong Kong, and both recovered completely.19 In May 2001 and in February and April 2002, the poultry stocks in Hong Kong were again destroyed when the highly pathogenic H5N1 virus reemerged in flocks. However, no more human cases of H5N1 influenza were identified until February 2003, when 2 cases were confirmed in 2 Hong Kong residents after travel to China, 1 of whom died.19 In February 2003, a large outbreak of H7N7 avian influenza occurred in poultry farms in the Netherlands.20 The virus caused mild illness in several farm workers, but a veterinarian who had visited an affected farm died of pneumonia. The virus isolated from the fatal case displayed 14 amino acid substitutions, which possibly contributed to the increased disease severity. All farm workers received mandatory influenza vaccination and prophylaxis with oseltamivir.21 The H7N7 poultry outbreak subsequently spread to Germany and Belgium but was eventually controlled by destruction of more than 30 million domestic poultry. In February 2004, another outbreak of H7N7 avian influenza occurred on a poultry farm in British Columbia, Canada, and resulted in at least 5 humans with infection, mainly conjunctivitis.1 Recently, the crystal structure of the hemagglutinin from the 1918 virus was determined, explaining why this virus was able to spread efficiently in the human population despite retainment of the avian receptor-binding site.6
Table 1.
Human Influenza Pandemics in the 20th Century
| No. of deaths |
||||||
|---|---|---|---|---|---|---|
| Year | Colloquial name | Subtype | Country of origin | Origin of viral genes | Worldwide | United States |
| 1918-1919 | Spanish flu* | H1N1 | China? Europe? North America? | Unclear, contains mammalian and avian genes | 25-50 million | >500,000 |
| 1957 | Asian flu | H2N2† | China | Reassortment with avian virus | >1 million | About 70,000 |
| 1968 | Hong Kong flu | H3N2† | China | Reassortment with avian virus | >1 million | About 34,000 |
| 1977 | Russian flu‡ | H1N1† | China, Russia | Reappearance of 1950s H1N1 virus (from frozen source?) | Low mortality | Low mortality |
Many people died within the first few days after infection, nearly half of whom were healthy young adults.
Virus is still circulating.
Illness occurred almost exclusively among persons younger than 20 years. This pandemic did not increase mortality.
Human-to-Human Transmission
Epidemiological studies suggest that most human H5N1 infections resulted from contact with infected birds or surfaces contaminated with their excretions. However, evidence of limited human-to-human transmission of avian influenza viruses has occurred (Table 2 ). A case-control study of 15 patients hospitalized for influenza virus H5N1 disease in 1997 was conducted in Hong Kong.22 Exposure to live poultry in the week before the onset of illness was significantly associated with H5N1 disease, whereas traveling, eating, or preparing poultry products and recent exposure to persons with respiratory illness showed no significant association. In a cohort study including 3 hospitals in Hong Kong at which patients infected with H5N1 strains had been admitted, a significantly higher seropositivity rate for H5N1 was found among exposed health care workers (3.7%) than among nonexposed ones (0.7%), providing epidemiological evidence of transmission from infected patients to health care workers.23 In the Netherlands in 2003, 3 family members of farm workers were infected during the H7N7 outbreak, demonstrating the ability of human-to-human transmission.20
Table 2.
Confirmed Human Infections With Avian Influenza Viruses
| Year | Country | Subtype | Characteristics |
|---|---|---|---|
| 1997 | Hong Kong* | H5N1 | 18 people were infected, 6 of whom died |
| 1999 | Hong Kong | H9N2 | Virus was isolated from 2 children with mild influenza-like symptoms; both recovered |
| 2003 | Hong Kong | H5N1 | Infection occurred among 2 family members after returning from China, 1 of whom died; source of infection remains uncertain |
| 2003 | The Netherlands* | H7N7 | Infection occurred in 83 humans (mostly conjunctivitis), 1 of whom died |
| 2003 | Hong Kong | H9N2 | Child was hospitalized with influenza symptoms and recovered |
| 2003 | Several Asian countries*† | H5N1 | This is the largest outbreak of avian influenza in poultry ever reported |
| 2004 | British Columbia, Canada | H7N7 | Infection (mostly conjunctivitis) occurred in 5 humans |
Limited person-to-person transmission occurred.
As of March 8, 2004, outbreaks in poultry have been confirmed in 8 countries: Cambodia, China, Indonesia, Japan, Laos, South Korea, Thailand, and Vietnam. In most of these countries, this is the first outbreak of avian influenza.
CURRENT OUTBREAK OF H5N1 INFLUENZA IN ASIA
Chronology of Events
The present epidemic of highly pathogenic avian influenza virus in Asia is historically unprecedented and extremely challenging.4 Between December 5 and 11 in 2003, sudden death occurred in 19,000 chickens at a farm near Seoul, South Korea; this was later confirmed as being caused by the highly pathogenic avian influenza virus H5N1. On January 8, 2004, authorities in Vietnam also reported several outbreaks of avian influenza H5N1 at farms in the southern provinces. Human cases of H5N1 avian influenza presenting as severe respiratory illness occurred, with a mortality rate of more than 70%. On January 11, 2004, the World Health Organization alerted the Global Outbreak Alert and Response Network to support health authorities in the epidemiological investigation and containment of human cases. These H5N1 viruses are substantially different from the H5N1 viruses in outbreaks in Hong Kong in 1997 and 2003, indicating that the virus has mutated. On January 23, 2004, authorities in Thailand reported an outbreak of highly pathogenic avian influenza among poultry, with laboratory-confirmed cases of H5N1 infection in humans.24 Japan, the European Union, the United States, and other major export markets banned import of poultry products from the affected Asian countries.
Clinical Features
Preliminary clinical data from 10 confirmed human cases of H5N1 avian influenza from the current epidemic in Vietnam were summarized recently.25 The mean age of the patients was 13.7 years (range, 5-24 years); none had any clinically important preexisting medical conditions. Of the 10 patients, 9 had a history of direct contact with poultry (chicken or ducks), with a median time before onset of illness of 3 days (range, 2-4 days). The main clinical features were fever, shortness of breath, cough, and diarrhea. Notably, sore throat, coryza, and conjunctivitis were absent. All patients presented with pronounced lymphopenia (mean lymphocyte count, 0.7 × 109/L) and important chest radiographic abnormalities including diffuse, multifocal, or patchy infiltrates or segmental or lobular consolidation. Eight of the 10 patients (80%) died after a mean of 10 days of illness. The clinical features, together with liver dysfunction, renal failure, coagulopathy, and pancytopenia seen in the 1997 Hong Kong H5N1 outbreak, are similar to those seen in patients with severe acute respiratory syndrome.
Similarly, human infection with avian influenza H5N1 reported in 1997 in Hong Kong presented as an influenzalike illness with pneumonia.26 Reactive hemophagocytic syndrome was the most characteristic pathologic finding and probably contributed to the lymphopenia, liver dysfunction, and abnormal clotting profiles that were observed among these patients.27 Gastrointestinal manifestations, renal failure unrelated to rhabdomyolysis, and pancytopenia were unusually prominent. Factors associated with severe disease included older age, delay in hospitalization, lower respiratory tract involvement, and leukopenia or lymphopenia at admission. The preliminary findings suggest that cytokine dysfunction contributes to the severity of H5N1 disease.19 There is no evidence of H5N1 virus replication outside the respiratory tract. Viral replication seems to trigger a burst of cytokine production that may ultimately result in multiorgan failure.
LABORATORY DIAGNOSIS
All patients who present to a health care setting with fever and respiratory symptoms should be questioned regarding their recent travel and exposure history.8 In patients at risk for avian influenza H5N1, laboratory testing is indicated (Table 3 ). The optimal specimen for influenza virus detection is a nasopharyngeal aspirate obtained within 3 days of the onset of symptoms; however, nasopharyngeal swabs and other specimens can be used. The H5N1 influenza virus can be detected by rapid antigen tests, virus culture, and reverse transcriptase-polymerase chain reaction (RT-PCR). At least 6 rapid antigen detection assays are commercially available and provide results in 15 to 30 minutes but are not as sensitive or specific as virus culture or RT-PCR.10 Virus isolation in cell cultures enables further antigenic and genetic characterization, drug susceptibility testing, and vaccine preparation. However, cultures take 2 to 10 days and must be performed under Biosafety Level 3+ laboratory conditions. Conventional and real-time PCR assays detect diverse influenza type A viruses, including the avian H5N1 strains.28, 29 Polymerase chain reaction primers are directed to the conserved matrix gene of the virus, and therefore this assay would be expected to detect recombinant avian strains of the virus. Of emphasis, avian influenza virus may be recombinant strains of the virus and may not contain the essential genes for replication in laboratory cultures.14 Rapid antigen detection and RT-PCR can be performed with standard Biosafety Level 2 laboratory conditions in a class II biological safety cabinet. Serologic diagnosis of influenza is based on the detection of a 4-fold or greater increase in specific antibody titer in paired serum samples; the first should be collected as soon as possible after onset of illness and the second, 10 to 14 days later. This limits the usefulness of serology in the diagnosis and treatment of acute illness.
Table 3.
Indications for Laboratory Testing for Avian Influenza H5N18
|
ANTIVIRAL TREATMENT
The current H5N1 strains are resistant to amantadine and rimantadine but are susceptible to neuraminidase inhibitors (oseltamivir and zanamivir). These drugs are effective for prophylaxis and treatment of influenza A virus infection, including the avian influenza H5N1. However, no efficacy trials have been performed due to the small number of human cases. Because a potential vaccine may be in short supply, antiviral drugs may play an important role in reducing the severity and spread of infection during the first stages of a pandemic.32 For prophylaxis, oseltamivir should be administered to individuals exposed to H5N1 avian influenza within 48 hours. Therefore, a global influenza strategy in the 21st century calls for stockpiling antiviral drugs and drafting plans for rapid distribution.9
PREVENTION
General Precautions
In geographic areas affected by avian influenza, individuals should avoid contact with poultry, and they should perform thorough and frequent hand hygiene using soap and water or alcohol-based hand rubs. The virus is killed by heat (56°C for 3 hours, 60°C for 30 minutes, or 70°C for 1 minute) and common disinfectants such as alcohol, bleach, formalin, or iodine compounds. Generally, 5% bleach solution is appropriate for dealing with biohazardous spillage. Influenza virus can survive in feces for several months. It can survive in water for up to 4 days at 22°C, for more than 30 days at 0°C, and indefinitely in frozen material.1 Therefore, poultry, including the eggs, should be cooked thoroughly. Recently, the Centers for Disease Control and Prevention issued guidelines for airline flight crews and persons meeting passengers arriving from areas with avian influenza.30 Protection of persons involved in outbreak eradication activities includes strict adherence to hand hygiene practices and the use of appropriate personal protective equipment (gloves, disposable clothing, shoe covers, safety goggles, and particulate respirators).30 During handling of human specimens, formation of aerosols and droplets should be minimized.
Patient Isolation
Isolation precautions identical to those recommended for severe acute respiratory syndrome should be implemented for all hospitalized patients diagnosed as having or being evaluated for avian influenza H5N1 (Table 4 ).31 These precautions should be continued for 14 days after onset of symptoms, until an alternative diagnosis is established, or until diagnostic test results indicate that the patient is not infected with influenza A virus. Patients managed as outpatients or hospitalized patients discharged before 14 days should be isolated in the home setting.30
Table 4.
|
NIOSH = National Institute of Occupational Safety and Health.
Vaccine Development
The current inactivated trivalent human influenza vaccine provides no protection against the H5 and H7 avian influenza strains. However, an important control measure is providing the seasonal human influenza vaccine to people at risk for avian influenza to reduce the risk of coinfection with avian and human influenza viruses simultaneously and to decrease the possibility of reassortment. The resultant hybrid virus could be highly transmissible among humans.
A prototype virus and candidate vaccines have been developed for protection against the H5N1 virus strain that infected 2 people and resulted in 1 death in Hong Kong in 2003.2 However, the avian subtypes are rapidly lethal to chicken embryos, and therefore the traditional chicken embryo method is not applicable. Alternative means of producing H5 and H7 vaccines were exploited, including the plasmid-based reverse genetic technology.9 A vaccine strain can be created by merging selected hemagglutinin and neuraminidase genes from the target virus with a laboratory virus. The resulting virus is recognized by the human immune system and causes a protective immune response but no disease. However, such vaccines have yet to be studied in clinical trials, and safety testing must be completed.
CONCLUSION
The occurrence of avian influenza H5N1 in humans is another reminder of our vulnerability to an emerging pandemic. Several measures can help to minimize the global public health risk. An immediate priority is to halt further spread of epidemics in poultry populations that would reduce the opportunities for human exposure to the virus. Clinicians should be cognizant of human influenza H5N1 infection among patients with the appropriate epidemiological exposure, so that patients can be identified quickly and managed appropriately and health care workers can be protected. The reemergence of H5N1 influenza in humans emphasizes the need to develop a vaccine against this virus.
| World Health Organization | www.who.int/en/ |
| Centers for Disease Control and Prevention | www.cdc.gov/ |
| World Organization for Animal Health | www.oie.int/eng/en_index.htm |
| Animal and Plant Health Inspection Service, US Department of Agriculture | www.aphis.usda.gov/ |
| Food and Agriculture Organization of the United Nations | www.fao.org/ |
Footnotes
A question-and-answer section appears at the end of this article.
Questions About Avian Influenza
-
1.Which one of the following statements about avian influenza viruses is false?
-
a.Viruses are divided into subtypes on the basis of surface glycoproteins hemagglutinin and neuraminidase
-
b.Receptor specificity is an absolute barrier against human infection by avian influenza viruses
-
c.The H5N1 avian influenza subtype mutates rapidly and has the propensity to acquire genes from viruses infecting other species
-
d.Migratory aquatic birds are the natural reservoir of avian influenza viruses
-
e.Transmission by feces provides an efficient way for wild birds to spread viruses
-
a.
-
2.Which one of the following subtypes of influenza viruses is responsible for the current avian influenza outbreak in Asia?
-
a.H5N2
-
b.H9N2
-
c.H5N1
-
d.H7N7
-
e.H3N2
-
a.
-
3.Which one of the following human influenza out-breaks was the most devastating in recorded human history?
-
a.Spanish influenza of 1918-1919 (H1N1)
-
b.Asian influenza in 1957 (H2N2)
-
c.Hong Kong influenza in 1968 (H3N2)
-
d.Russian influenza in 1977 (H1N1)
-
e.Hong Kong avian influenza in 1997 (H5N1)
-
a.
-
4.Which one of the following statements about the current H5N1 avian influenza outbreak in Asia is true?
-
a.Most human cases of avian influenza presented with conjunctivitis and/or mild upper respiratory tract symptoms
-
b.No evidence exists for direct human-to-human transmission of avian influenza virus
-
c.The avian influenza virus is killed by freezing at −20°C
-
d.The optimal specimen for influenza virus detection is a nasopharyngeal aspirate obtained within 3 days of the onset of symptoms
-
e.The first documented human infection by avian influenza viruses occurred in mainland China in 2003
-
a.
-
5.Which one of the following isolation precautions is not recommended for hospitalized patients being evaluated for avian influenza?
-
a.Strict hand hygiene before and after all patient contact
-
b.Use of gloves and gown for all patient contact
-
c.Use of eye protection when within 3 feet (1 m) of the patient
-
d.Use of shoe covers when entering the isolation room
-
e.Placement of the patient in an airborne isolation room
-
a.
Correct answers:
-
1.
b,
-
2.
c,
-
3.
a,
-
4.
d,
-
5.
d
REFERENCES
- 1.World Health Organization Avian influenza. Available at: www.who.int/csr/disease/avian_influenza/en/ Accessibility verified March 8, 2004.
- 2.World Health Organization Development of a vaccine effective against avian influenza H5N1 infection in humans. Wkly Epidemiol Rec. 2004;79:25–26. [PubMed] [Google Scholar]
- 3.Claas EC, Osterhaus AD, van Beek R. Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus [published correction appears in Lancet. 1998;351:1292] Lancet. 1998;351:472–477. doi: 10.1016/S0140-6736(97)11212-0. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization Avian influenza A(H5N1) Wkly Epidemiol Rec. 2004;79:65–70. [PubMed] [Google Scholar]
- 5.Zambon MC. The pathogenesis of influenza in humans. Rev Med Virol. 2001;11:227–241. doi: 10.1002/rmv.319. [DOI] [PubMed] [Google Scholar]
- 6.Gamblin SJ, Haire LF, Russell RJ. The structure and receptor-binding properties of the 1918 influenza hemagglutinin. Science. February 5, 2004 doi: 10.1126/science.1093155. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Horimoto T, Kawaoka Y. Pandemic threat posed by avian influenza A viruses. Clin Microbiol Rev. 2001;14:129–149. doi: 10.1128/CMR.14.1.129-149.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention Outbreaks of avian influenza A (H5N1) in Asia and interim recommendations for evaluation and reporting of suspected cases—United States, 2004. MMWR Morb Mortal Wkly Rep. 2004;53:97–100. [PubMed] [Google Scholar]
- 9.Webby RJ, Webster RG. Are we ready for pandemic influenza? Science. 2003;302:1519–1522. doi: 10.1126/science.1090350. [DOI] [PubMed] [Google Scholar]
- 10.Nicholson KG, Wood JM, Zambon M. Influenza. Lancet. 2003;362:1733–1745. doi: 10.1016/S0140-6736(03)14854-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gubareva LV, Kaiser L, Hayden FG. Influenza virus neuraminidase inhibitors. Lancet. 2000;355:827–835. doi: 10.1016/S0140-6736(99)11433-8. [DOI] [PubMed] [Google Scholar]
- 12.Hilleman MR. Realities and enigmas of human viral influenza: pathogenesis, epidemiology and control. Vaccine. 2002;20:3068–3087. doi: 10.1016/s0264-410x(02)00254-2. [DOI] [PubMed] [Google Scholar]
- 13.Laver G, Garman E. Pandemic influenza: its origin and control. Microbes Infect. 2002;4:1309–1316. doi: 10.1016/s1286-4579(02)00013-8. [DOI] [PubMed] [Google Scholar]
- 14.Baigent SJ, McCauley JW. Influenza type A in humans, mammals and birds: determinants of virus virulence, host-range and interspecies transmission. Bioessays. 2003;25:657–671. doi: 10.1002/bies.10303. [DOI] [PubMed] [Google Scholar]
- 15.Fouchier RA, Osterhaus AD, Brown IH. Animal influenza virus surveillance. Vaccine. 2003;21:1754–1757. doi: 10.1016/s0264-410x(03)00067-7. [DOI] [PubMed] [Google Scholar]
- 16.Webster RG. Influenza: an emerging disease. Emerg Infect Dis. 1998;4:436–441. doi: 10.3201/eid0403.980325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Webster RG. Wet markets—a continuing source of severe acute respiratory syndrome and influenza? Lancet. 2004;363:234–236. doi: 10.1016/S0140-6736(03)15329-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan PK. Outbreak of avian influenza A(H5N1) virus infection in Hong Kong in 1997. Clin Infect Dis. 2002;34(suppl 2):S58–S64. doi: 10.1086/338820. [DOI] [PubMed] [Google Scholar]
- 19.Peiris M, Yuen KY, Leung CW. Human infection with influenza H9N2. Lancet. 1999;354:916–917. doi: 10.1016/s0140-6736(99)03311-5. [DOI] [PubMed] [Google Scholar]
- 20.Fouchier RA, Schneeberger PM, Rozendaal FW. Avian influenza A virus (H7N7) associated with human conjunctivitis and a fatal case of acute respiratory distress syndrome. Proc Natl Acad Sci U S A. 2004;101:1356–1361. doi: 10.1073/pnas.0308352100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koopmans M, Wilbrink B, Conyn M. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet. 2004;363:587–593. doi: 10.1016/S0140-6736(04)15589-X. [DOI] [PubMed] [Google Scholar]
- 22.Mounts AW, Kwong H, Izurieta HS. Case-control study of risk factors for avian influenza A (H5N1) disease, Hong Kong, 1997. J Infect Dis. 1999;180:505–508. doi: 10.1086/314903. [DOI] [PubMed] [Google Scholar]
- 23.Bridges CB, Lim W, Hu-Primmer J. Risk of influenza A (H5N1) infection among poultry workers, Hong Kong, 1997-1998. J Infect Dis. 2002;185:1005–1010. doi: 10.1086/340044. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention Cases of influenza A (H5N1)—Thailand, 2004. MMWR Morb Mortal Wkly Rep. 2004;53:100–103. [PubMed] [Google Scholar]
- 25.Hien TT, Liem NT, Dung NT, World Health Organization International Avian Influenza Investigative Team Avian influenza A (H5N1) in 10 patients in Vietnam. N Engl J Med. 2004;350:1179–1188. doi: 10.1056/NEJMoa040419. [DOI] [PubMed] [Google Scholar]
- 26.Yuen KY, Chan PK, Peiris M. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet. 1998;351:467–471. doi: 10.1016/s0140-6736(98)01182-9. [DOI] [PubMed] [Google Scholar]
- 27.To KF, Chan PK, Chan KF. Pathology of fatal human infection associated with avian influenza A H5N1 virus. J Med Virol. 2001;63:242–246. doi: 10.1002/1096-9071(200103)63:3<242::aid-jmv1007>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 28.Fouchier RA, Bestebroer TM, Herfst S, Van Der Kemp L, Rimmelzwaan GF, Osterhaus AD. Detection of influenza A viruses from different species by PCR amplification of conserved sequences in the matrix gene. J Clin Microbiol. 2000;38:4096–4101. doi: 10.1128/jcm.38.11.4096-4101.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boivin G, Cote S, Dery P, De Serres G, Bergeron MG. Multiplex real-time PCR assay for detection of influenza and human respiratory syncytial viruses. J Clin Microbiol. 2004;42:45–51. doi: 10.1128/JCM.42.1.45-51.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention Avian influenza. Available at: www.cdc.gov/flu/avian/index.htm Accessibility verified March 8, 2004.
- 31.Sampathkumar P, Temesgen Z, Smith TF, Thompson RL. SARS: epidemiology, clinical presentation, management, and infection control measures. Mayo Clin Proc. 2003;78:882–890. doi: 10.4065/78.7.882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bridges CB, Fukuda K, Uyeki TM, Cox NJ, Singleton JA. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2002;51(RR03):1–31. [PubMed] [Google Scholar]


