Abstract
A replication-incompetent adenoviral vector encoding the heavy chain C-fragment (HC50) of botulinum neurotoxin type C (BoNT/C) was evaluated as a mucosal vaccine against botulism in a mouse model. Single intranasal inoculation of the adenoviral vector elicited a high level of HC50-specific IgG, IgG1 and IgG2a in sera and IgA in mucosal secretions as early as 2 weeks after vaccination. The antigen-specific serum antibodies were maintained at a high level at least until the 27th week. Immune sera showed high potency in neutralizing BoNT/C as indicated by in vitro toxin neutralization assay. The mice receiving single dose of 2 × 107 p.f.u. (plaque-forming unit) of adenoviral vector were completely protected against challenge with up to 104 × MLD50 of BoNT/C. The protective immunity showed vaccine dose dependence from 105 to 2 × 107 p.f.u. of adenoviral vector. In addition, animals receiving single intranasal dose of 2 × 107 p.f.u. adenoviral vector could be protected against 100 × MLD50 27 weeks after vaccination. Animals with preexisting immunity to adenovirus could also be vaccinated intranasally and protected against lethal challenge with BoNT/C. These results suggest that the adenoviral vector is a highly effective gene-based mucosal vaccine against botulism.
Keywords: botulinum neurotoxin, mucosal vaccine, protective immunity, replication-incompetent adenovirus
Introduction
Extremely potent botulinum neurotoxins (BoNTs) produced from the strictly anaerobic Gram-positive bacterium Clostridium botulinum (C. botulinum) are likely candidates to be used by terrorists.1, 2 There are seven serotypes (A–G) of C. botulinum, each producing immunologically distinguishable neurotoxin variants, type A through G.3 Human botulism mainly involves types A, B, E and F.4 The BoNTs are the most deadly natural toxic substances known.5, 6 The heavy chain of the BoNT is composed of N-terminal translocation domain and C-terminal receptor-binding domain.4, 7 The 50-kDa C-terminal end of the heavy chain (HC50) is responsible for specific toxin binding at neuromuscular junction.7 Numerous previous studies have proved that the HC50 subunits of BoNTs are non-toxic and antigenic, and are capable of eliciting immunity response against botulism.8, 9, 10, 11, 12, 13
There is no licensed vaccine for protection of botulism, although a pentavalent botulinum toxoid (PBT) investigational new drug (IND) vaccine against type A through E is available.10, 14 The vaccine is a mixture of chemically inactivated BoNTs that were produced from C. botulinum; concerns have been raised regarding safety in the process of producing the toxins, creating limitations in producing a timely supply.7, 15, 16 To eliminate the risk and difficulty associated with producing a toxin-based vaccine, and alternative vaccine against botulism is being sought. To date, the most progress has occurred with a recombinant HC50 subunit vaccine.7, 10, 11, 16, 17, 18, 19, 20
Replication-incompetent adenoviruses expressing vaccine antigens can be effectively delivered by either the parenteral or mucosal route. The transgene expression with adenovirus vectors is usually robust and can be further enhanced by driving gene expression with strong heterologous promoters. The vector genome does not insert into the host chromosome, ensuring safe delivery. In addition, adenoviruses can be grown to very high titers in qualified cell lines.21, 22, 23, 24 These advantages make adenoviruses attractive vaccine vectors and they are being used widely in the development of vaccines against HIV, SARS (severe acute respiratory syndrome), avian influenza, tuberculosis and anthrax.25, 26, 27, 28, 29, 30 In a previous study, we constructed a replication-incompetent adenoviral vector containing a synthesized condon-optimized gene encoding the HC50 of BoNT type C (Ad/opt-BoNT/C-HC50) and evaluated its vaccine potential by intramuscular (i.m.) injection.31 In this study, we use the same adenovirus-based vaccine delivered by the intranasal (i.n.) mucosal route and show that long-lasting protective immunity occurs after a single dose.
Results
Serum antibody responses against BoNT/C-Hc50
The immune response in sera after a single i.n. vaccination with varying doses of adenoviral vector Ad/opt-BoNT/C-HC50 is shown in Figure 1. The pre-immune sera (week 0) and sera from mice vaccinated with negative control vector (Ad/Null, adenovirus vector without transgene, data not shown) were negative. IgG, IgG1 and IgG2a responses to BoNT/C-HC50 were detectable at week 2 for all three doses evaluated. Even at the lowest dose of Ad/opt-BoNT/C-HC50 (1 × 105 p.f.u., plaque-forming unit), serum IgG levels were significantly higher than those of control mice receiving Ad/null (P<0.01). The time course of the response in serum for IgG, IgG1 and IgG2a to BoNT/C-HC50 in the vaccinated mice is also shown in Figure 1. Overall, the dose ranging study showed that the serum IgG concentration in mice receiving 2 × 107 p.f.u. Ad/opt-BoNT/C-HC50 was the highest.
Figure 1.
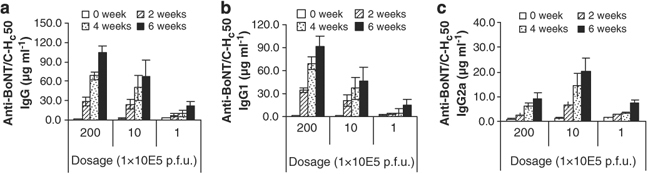
Serum antibody responses against BoNT/C-HC50 in vaccinated mice. Mice were vaccinated intranasally with different doses of Ad/opt-BoNT/C-HC50 (1 × 105–2 × 107 p.f.u./mouse) in week 0. Serum samples were obtained in weeks 0, 2, 4 and 6 to measure anti-BoNT/C-HC50 IgG (a), IgG1 (b) and IgG2a (c) antibody concentrations by quantitative ELISA. The data are expressed as mean±s.e. (n=8).
The mice receiving 1 × 105, 1 × 106 or 2 × 107 p.f.u./mouse of Ad/opt-BoNT/C-HC50 achieved serum anti-BoNT/C-HC50 IgG concentrations of 6.83±2.61, 24.14±7.32 and 28.86±6.81 μg ml−1, respectively, at week 2; 9.61±4.87, 50.16±19.11 and 68.49±5.58 μg ml−1 at week 4; and 22.59±6.67, 67.20±24.83 and 104.98±9.63 μg ml−1 at week 6. Serum IgG antibodies against BoNT/C-HC50 continued to increase with time from 2 to 6 weeks after vaccination (Figure 1).
The IgG1 responses to BoNT/C-HC50 in the mice 6 weeks after vaccination with Ad/opt-BoNT/C-HC50 accounted for about three-fourths of the total IgG. IgG1 concentrations against BoNT/C-HC50 in sera of vaccinated mice were significantly increased by week 2 compared with those in week 0. IgG2a antibody also was produced after vaccination, although of lower magnitude than IgG1 (Figure 1).
Persistence of antibodies after mucosal vaccination
In a separate experiment, we assessed antibody persistence after the single i.n. dose of 2 × 107 p.f.u./mouse of Ad/opt-BoNT/C-HC50 adenoviral vector vaccine (Figure 2). Measurements were made at 11, 19 and 27 weeks post vaccination for IgG, IgG1 and IgG2a. We found antibody levels persisted at levels similar to those at post week 6 after vaccination and they did not significantly decline between weeks 11 and 27; they showed the same IgG1>IgG2a predominance as observed at post week 6.
Figure 2.
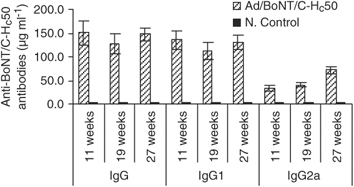
Sustaining of antigen-specific antibody responses after intranasal vaccination with the adenovirus-vectored vaccine in mice. Mice were intranasally inoculated with a single dose of 2 × 107 p.f.u. of Ad/opt-BONT/C-HC50 (vaccination group) or with Ad/Null (control group) in week 0. Serum samples were obtained in weeks 11, 19 and 27 before challenging with active BoNT/C. The anti-BoNT/C-HC50 IgG antibody concentrations in sera were determined by quantitative ELISA. The data are expressed as mean±s.e. (n=7 or 8 in the vaccination group and n=4 in the control group).
Antibody responses against BoNT/C-HC50 in mucosal secretions
To evaluate the mucosal immune response, we analyzed specific IgG and IgA antibody concentrations in saliva, nasal wash and vaginal wash samples after i.n. vaccination with Ad/opt-BoNT/C-HC50 adenoviral vector vaccine. A single i.n. vaccination with 2 × 107 p.f.u./mouse of Ad/opt-BoNT/C-HC50 resulted in significant IgG and IgA antibody responses (Figure 3). At 2 weeks after vaccination, high local antibody responses were measurable, whereas no specific antibodies were detectable in the samples from control mice. All the examined antibody levels in the saliva, nasal wash and vaginal wash samples from vaccinated mice at week 4 were significantly higher than those at week 2. The BoNT/C-HC50-specific IgG, IgG1 and IgG2a antibody concentrations in mucosal samples were lower than those in sera (P<0.01), and the ratio of IgG2a/IgG1 was reversed compared with that in serum (P<0.01). Mucosal anti-BoNT/C-HC50 IgA in saliva reached 160.4±50 ng ml−1 at week 2 and 393±132 ng ml−1 at week 4, whereas sera anti-BoNT/C-HC50 IgA (data not shown) was not detectable.
Figure 3.
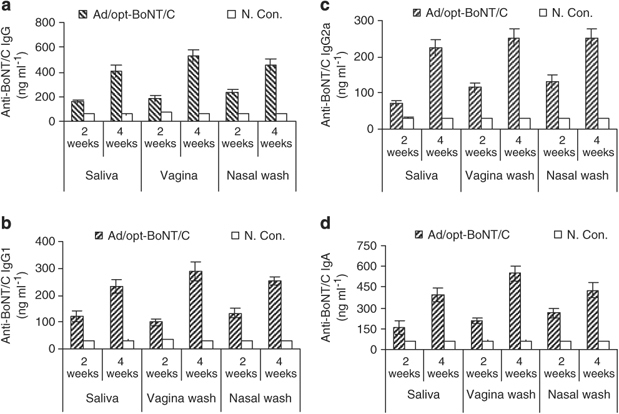
Mucosal antibody responses against BoNT/C-HC50 in vaccinated mice. Mice were intranasally inoculated with a single dose of 2 × 107 p.f.u. of Ad/opt-BONT/C-HC50 (vaccination) or with Ad/Null (control) in week 0. Saliva, nasal and vaginal wash samples were collected in weeks 2 and 4. Anti-BoNT/C-HC50 IgG (a), IgG1 (b), IgG2a (c) and IgA (d) concentrations were measured by quantitative ELISA. The data are expressed as mean±s.e. (n=8 in the vaccination group and n=4 in the control group).
Neutralizing capacity of anti-sera to BoNT
The neutralization capacity of anti-sera from mice vaccinated with Ad/opt-BoNT/C-HC50 adenoviral vector vaccine was determined using a mouse bioassay. Owing to the limited amount of serum available, the sera from eight vaccinated mice were pooled. The results are shown in Figure 4. The neutralization titer from the mice receiving single doses of 2 × 107 p.f.u./mouse of Ad/opt-BoNT/C-HC50 was 6.4 IU ml−1 6 weeks after vaccination. The antiserum from these mice, diluted by ⩽64-fold, completely neutralized 100 × 50% mouse lethal dose (MLD50) of BoNT/C resulting in a 100% survival. Serum from control mice did not neutralize the neurotoxin.
Figure 4.
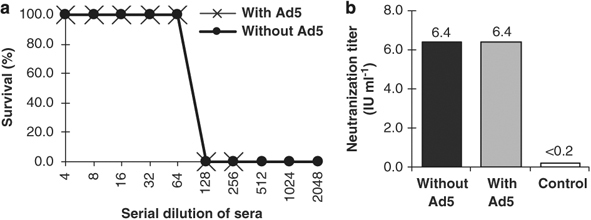
Serum anti-BoNT/C neutralizing antibody titer assay. Each mouse was inoculated intranasally with or without 2 × 107 p.f.u. of Ad5 in week 0, then subsequently vaccinated intranasally with 2 × 107 p.f.u. of Ad/opt-BONT/C-HC50 or inoculated with 2 × 107 p.f.u. of control Ad/Null in week 4.A volume of 50 μl of serum from each mouse in the same group were pooled 6 weeks after vaccination. Sera were 1:4 diluted initially with Dulbecco's PBS and then in twofold series to determine anti-BoNT/C neutralization titers. (a) Survival rates of mice after challenge with neutralized BoNT/C and (b) serum anti-BoNT/C neutralization titers (IU ml−1). 1 IU=10 000 × MLD50. With or without Ad5, pre-inoculation with or without adenovirus type 5 (n=4).
Protection against active BoNT/C in vaccinated mice
After a single dose of i.n. vaccination of adenoviral vector, mice were challenged intraperitoneally (i.p.) with 100 × MLD50 of active BoNT/C. The results are summarized in Figure 5. At 7 weeks after a single vaccination, none of the mice receiving control vector Ad/Null survived the toxin challenge, whereas all mice (8/8, or 100%) receiving 2 × 107 p.f.u. of Ad/opt-BoNT/C-HC50 and 92% of mice (11/12) receiving 1 × 106 p.f.u./mouse of Ad/opt-BoNT/C-HC50 survived 100 × MLD50 challenge with no botulism symptoms (Figure 5a). Overall 50% (4/8) of the mice at the lowest vaccine dose studied (1 × 105 p.f.u. of Ad/opt-BoNT/C-HC50) died and one of the four surviving mice showed botulism symptoms. In contrast, 83% (10/12) of the mice that received one dose (50 μl/mouse) of botulinum toxoid adsorbed pentavalent vaccine (ABCDE) survived 100 × MLD50 challenge (Figure 5a). In addition, as shown in Figures 5b–d, 11, 19 and 27 weeks after immunization, mice given 2 × 107 p.f.u. of Ad/opt-BoNT/C-HC50 were also completely protected from 100 × MLD50 of BoNT/C toxin.
Figure 5.
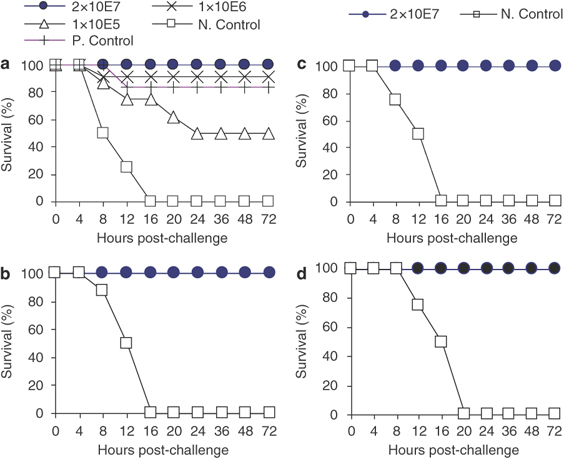
Protection against active BoNT/C challenge in vaccinated mice. Mice were intranasally inoculated with Ad/Null (N. Control group) or 1 × 105–2 × 107 of Ad/opt-BoNT/C-HC50 or injected i.m. with 50 μl of the botulinum toxoid adsorbed pentavalent (ABCDE) vaccine (P. Control group) in week 0. Animals were then challenged with 100 × MLD50 of BoNT/C in weeks 7 (a), 11 (b), 19 (c) and 27 (d). Adenovirus dosages for vaccination groups I, II, III and N. Con group are 1 × 105, 1 × 106, 2 × 107 and 2 × 107 p.f.u./mouse, respectively (n=4 for N. Control groups; n=8 for vaccination groups and n=12 for P. Control group).
To further show the vaccine potency for protection, higher doses of active BoNT/C up 105 × MLD50 were also used in toxin challenge. Figure 6 shows that animals i.n. vaccinated with 2 × 107 p.f.u. of Ad/opt-BoNT/C-HC50 could be completely protected against challenge with 104 × MLD50 of BoNT/C 4 weeks after vaccination. However, the protection rate decreased to 14% (1/7 mice) when the BoNT/C toxin challenge dose increased to 105 × MLD50. This shows the protective immunity is also toxin challenge dose dependent.
Figure 6.
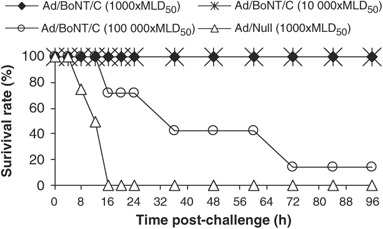
Botulinum neurotoxin dose-dependent protection in mice vaccinated with adenovirus-vectored vaccine. Mice were intranasally vaccinated with 2 × 107 p.f.u. of Ad/opt-BoNT/C-HC50 in week 0 and then challenged in week 4 with 103–105 × MLD50 of BoNT/C. Ad/Null, negative control and animals were inoculated intranasally with 2 × 107 p.f.u. of Ad/Null and challenged with 103 × MLD50 of BoNT/C. (n for Ad/Null, vaccinated groups 103 × MLD50, 104 × MLD50 and 105 × MLD50 are 4, 8, 8 and 7, respectively).
Effects of preexisting anti-Ad5 immunity on vaccination
To determine the impact of preexisting anti-human Ad5 neutralization antibody on the efficacy of vaccination with Ad/opt-BoNT/C-HC50, mice were pre-inoculated i.n. with 2 × 107 p.f.u. of wild-type Ad5 4 weeks before receiving Ad/opt-BoNT/C-HC50 vaccine. Significant serum anti-Ad5 neutralizing antibody titers were produced (Figure 7a). The animals with preexisting immunity to Ad5 were then given a single i.n. dose of 2 × 107 p.f.u. of Ad/opt-BoNT/C-HC50 and then 7 weeks after vaccination the animals were i.p. challenged with BoNT/C. All the vaccinated animals were fully protected against 100 × MLD50 BoNT/C challenge (Figure 7b). In contrast, none of the control mice survived the toxin challenge (Figure 7b). In addition, in an in vitro toxin neutralization assay, we found that a single dose of our vaccine elicited the same titers of anti-toxin antibody responses (titer, 6.4 IU ml−1) regardless of host preexisting immunity to the adenoviral vector (Figure 4). These data suggest that Ad/opt-BoNT/C-HC50 vector could provide protection against BoNT/C neurotoxin under preexisting immunity to adenovirus in the host.
Figure 7.
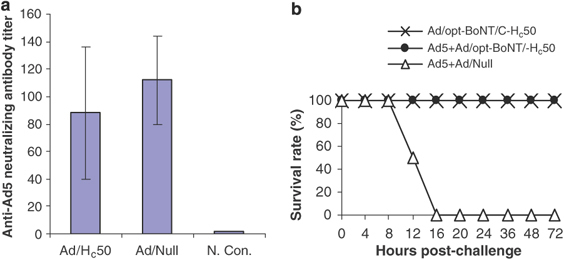
Effects of preexisting immunity on vaccination efficacy. (a) Anti-adenovirus neutralizing antibodies in mice inoculated with adenovirus pre-vaccination. Mice were intranasally inoculated with 2 × 107 p.f.u. of wild-type human adenovirus serotype 5 in week 0. Serum samples were obtained in week 4. Sera from two mice in the same group were pooled and the anti-Ad5 neutralizing antibody titers of the serum pools were subsequently measured. Mean=X±s.e. Ad/Hc50: the group was subsequently vaccinated with Ad/opt-BoNT/C-HC50 (panel b); Ad/Null: the group was subsequently inoculated with Ad/Null (panel b); and N. Con: data were obtained from mouse pre-inoculation of adenovirus (n=4). (b) Effects of preexisting immunity to adenovirus on the efficacy of the adenovirus-vectored mucosal vaccine. Each mouse was inoculated intranasally with or without 2 × 107 p.f.u. of Ad5 in week 0 as shown in panel a, then subsequently inoculated intranasally with 2 × 107 p.f.u. of Ad/opt-BoNT/C-HC50 in the vaccination group or with Ad/Null in the control group in week 4, and challenged with 100 × MLD50 BoNT/C in week 11 (n=8 in experiment groups and n=4 in control group).
Discussion
The neurotoxins produced by C. botulinum are among the most potent poisons known and there is a need to prepare for their use in a bioterrorism attack.1, 2 Naturally, human botulism mainly involves BoNT types A, B, E and F,4 and serotypes C and D mostly affect domestic animals. Given the ease of preparation and potential toxicity of all these neurotoxins, it is equally important to develop vaccines against all these toxins for biodefense. In this study, we evaluated the vaccination strategy against the BoNT/C and expect ultimately to apply the same platform to develop vaccines against all serotypes of BoNTs. Here, we have described a novel adenoviral vector delivery of a botulism vaccine against type C neurotoxin that when delivered as a single i.n. dose proved to be a highly effective vaccine. Owing to the single i.n. route of vaccination, this vaccine could be self-administered to protect the population in the event of terrorist attack with C. botulism or neurotoxins. In addition to the ease of administration and rapid onset of protection described here, the vaccine could be produced inexpensively, in high quantity and in a short time frame. We chose HC50 fragment of BoNT type C because the HC50 subunits of BoNTs are non-toxic and antigenic, and are capable of eliciting immunity responses against botulism.8, 10, 11, 12 Also in a previous study we showed that i.m. vaccination with Ad/opt-BoNT/C-HC50 elicited strong systemic immunity that lasted at least 27 weeks and mice receiving the vaccine were fully protected against BoNT/C challenge.31
BoNTs can be lethal by ingestion of minute amounts in food and/or by inhalation. The latter delivery mode is the strongest bioterrorism-related threat.32, 33 The mucosal immune system is the first line of defense against botulism. However, the current injection-type botulism toxoid vaccine only provides protective immunity in the systemic compartment. Clearly, the development of a safe and effective mucosal vaccine should be a high priority against bioterrorism-related botulism.34 Previous research by Kobayashi et al.35 showed that nasal vaccination with BoNT/A toxoid plus a mutant of cholera toxin (E112K) effectively prevents mucosal BoNT intoxication in mice. Maddaloni et al.36 recently showed that mucosal vaccination with adenovirus type 2 fiber fused with HC50 of BoNT/A elicited robust mucosal antibody response, and addition of cholera toxin (CT) as an adjuvunt in the vaccine further enhanced protective immunity in mice against challenge with active BoNT/A. These studies proved the feasibility for developing a nasal vaccine against botulism. Adenoviruses invade their host naturally through the mucosa surface, notably in the respiratory or gastrointestinal tract.37 Adenoviral vector vaccines can be effectively delivered by i.n. mucosal route and can induce strong adaptive immune responses in mammalian hosts.21, 22 The replication-incompetent adenoviral vector Ad/opt-BoNT/C-HC50 studied here given as a protective, single i.n. vaccination elicited not only high serum antibody response to BoNTC/HC50 but also high specific antibody response in mucosal secretions.
Protection against botulism neurotoxin is expected to be antibody-mediated and antibody levels have been correlated with protection.17, 19 The mice receiving Ad/opt-BoNT/C-HC50 developed high and persistent serum neutralization titers and high mucosal antibody levels. A functional antibody response that neutralized active BoNT was shown in our experiments and, in protection against BoNT/C in the vaccinated animals, was shown to persist for at least 27 weeks. In future studies, we plan to determine whether toxin-specific mucosal antibodies are protective. We will measure toxin neutralizing antibody titers in mucosal secretions after mucosal immunization and perform toxin challenge through nasal and the mucosal route in addition to i.p. route.
Other studies have established that preexisting anti-adenovirus antibody may drastically reduce the intake of adenovirus-vectored vaccines,21, 38, 39, 40 but immunity to the vector has been overcome in some situations.23, 41, 42 Our challenge experiments indicate that preexisting anti-adenovirus immunity did not reduce the 100% protection in vaccinated mice, similar to our previous results after i.m. vaccination.31 To make our observation more convincing, similar experiments with higher doses of toxin for challenge and with lower doses of our vaccine in mice with preexisting immunity to adenovirus would be helpful.
In summary, in this study we have shown for the first time that a single i.n. vaccination of an adenovirus-based vector encoding a humanized HC 50-kDa of BoNT/C can elicit systemic and mucosa immunity responses and provide full protection in vaccinated mice against BoNT type C. The protective immunity can last at least 27 weeks and is not compromised by preexisting antibody to adenovirus. Together with our previous results with i.m. vaccination, the adenoviruses vector platform deserves further study as a multivalent vaccine against all serotypes of BoNTs.
Materials and methods
Construction of adenoviral vector encoding codon-optimized HC50 of BoNT/C
A replication-incompetent human adenovirus serotype 5 vector Ad/opt-BoNT/C-HC50 expressing HC50 of BoNT/C, and a control vector Ad/Null (adenovirus vector with no transgene) were constructed using the AdEasy System (Stratagene, La Jolla, CA, USA) as described previously.31, 43, 44 The vector Ad/opt-BoNT/C-HC50 contained a synthesized human codon-optimized gene encoding the HC50 of BoNT type C145 and a native gene encoding the signal peptide of human tissue plasminogen activator (PLAT) (amino acids 1–25, GenBank accession no. BC002795). The recombinant adenoviruses were produced in AD293 cells (Stratagene), purified by CsCl gradients centrifugation and stored in 1.0 M sucrose in a −80 °C freezer, their titers (p.f.u.) were determined by plaque assay.
Animals, treatments, sample collection and challenge
BALB/c mice (female, 5–6 weeks old), purchased from Jackson Laboratory (Bar Harbor, ME, USA), were housed in the animal facility of University of Rochester Medical Center, four animals per cage. All experimental tests were carried out in accordance with the US Public Health Service Guide for the Care and Use of Laboratory Animals (NRC Publication, 1996 ed.) and other related federal statutes and regulations in Animal Welfare Act.
Vaccination dose-dependent test
To evaluate an optimal dose, 40 mice were allotted into 4 experimental groups and two control groups, 8 mice per group. The animals were vaccinated by i.n. inhalation with Ad/opt-BoNT/C-HC50 adenoviral vector at doses of 1 × 104, 1 × 105, 1 × 106 and 2 × 107 p.f.u./mouse, respectively, in the experimental groups, and Ad/Null at a dose of 2 × 107 p.f.u./mouse in the negative control group. In the positive control group, mice were injected i.m. with the botulinum toxoid adsorbed pentavalent vaccine (ABCDE) (50 μl/mouse), an IND vaccine that was produced by the Michigan Department of Public Health. Serum samples were obtained at weeks 0, 2, 4 and 6 and stored at −20 °C until further assayed. The vaccinated mice were i.p. challenged with BoNT 1 week after the last bleeding as described in the following section.
Saliva, nasal wash and vagina wash specimens
For these experiments, 16 mice were divided into 2 test groups and 2 control groups, 8 mice per group. The animals were vaccinated with 2 × 107 p.f.u./mouse of Ad/opt-BoNT/C-HC50 in the test groups and same amount of Ad/Null in the control groups at week 0; saliva, nasal wash and vaginal wash samples were collected at week 2 in one test group and one control group, and at week 4 in one test group and one control group at each time point. The mice were anesthetized by i.p. injection with 2 mg of ketamine HCl (Bedford Laboratories, Bedford, OH, USA) plus 0.2 mg of xylazine (Butler Company, Columbus, OH, USA). Vaginal washes were collected by flushing the vagina with 100 μl phosphate-buffered saline (PBS) by repeated aspiration using a pipette with an animal feeding needle (with a ball head) until turbid.46 The saliva samples were collected using a 200-μl pipette fitted with a plastic tip, after i.p. injection of carbachol (Sigma Chemical Co., St Louis, MO, USA; 10 μg in 0.1 ml), to stimulate salivation as described previously.47, 48 The mice were then incised ventrally along the median line from the xiphoid process to the chin, the heads were removed and the lower jaws were excised. A hypodermic needle was inserted into the posterior opening of the nasopharynx and 200 μl of PBS was injected repeatedly to collect the nasal wash samples.49
Challenge with BoNT
The vaccinated and control mice were i.p. challenged with 102–105 × MLD50 of C. botulinum neurotoxin BoNT/C (Metabiolgics Inc., Madison, WI, USA) per mouse as specified in each experiment. The challenged animals were monitored every 4 h for the first 2 days and twice a day thereafter for total 7 days. The number of deaths for each group was recorded as the end point.31, 50
Long-term protective immunity trial
In these experiments, 48 mice were allotted into 3 test groups and 3 control groups, 8 mice per group. The animals were i.n. vaccinated at week 0 with Ad/opt-BoNT/C-HC50 vector at doses of 2 × 107 p.f.u./mouse in test groups, and Ad/Null at the same dosage in the control groups. One test group and one control group mice were challenged with BoNT/C at weeks 11, 19 and 27, respectively. The serum samples were obtained at week 0 and 1 week before challenge.
Vaccination efficacy test under preexisting immunity to adenovirus
A total of 12 mice were allotted into one experimental group (8 mice) and one control group (4 mice). All animals were i.n. inoculated with wide-type human adenovirus serotype 5 (WT Ad5; ATCC, Manassas, VA, USA) at a dose of 2 × 107 p.f.u./mouse, and then vaccinated by nasal inhalation at week 4 with Ad/opt-BoNT/C-HC50 vector at a dose of 2 × 107 p.f.u./mouse in the experimental group and Ad/Null at the same dose in the control group. The serum samples were obtained at weeks 0 and 4, before inoculation with WT Ad5 and i.n. vaccination with Ad/opt-BoNT/C-HC50, respectively. The vaccinated animals were subsequently challenged with 100 × MLD50 of BoNT/C at week 11.
Quantitative ELISA
ELISA Quantitation Kits (Bethel Lab. Inc., Montgomery, TX, USA) were used to measure IgG, IgG1, IgG2a and IgA concentrations in serum, saliva, nasal wash and vaginal wash samples against BoNT/C-HC50 as described previously.31 Briefly, 96-well plates were coated at 4 °C overnight with recombination protein BoNT/C-HC50 (0.5 μg/well) in 100 μl of coating buffer (0.05 M carbonate–bicarbonate buffer, pH 9.6). After rinsing with wash buffer (0.05% Tween 20 in PBS) for five times, the nonspecific binding sites were blocked with 200 μl of blocking buffer (1% bovine serum albumin (BSA) in PBS, pH 7.4) for 1 h at room temperature followed by washing five times. Later 100 μl of 1:100 dilutions of sera in PBS (pH 7.4) with 0.05% Tween 20 and 1% BSA was added to each well and then incubated at 37 °C for 2 h. After five washes, the plates were incubated for 1 h at room temperature with 100 μl/well of 1:10 000 dilution of goat anti-mouse IgG, IgG1 or IgG2a conjugated with alkaline phosphates. The color reaction was developed by incubation with the p-nitrophenylphosphate phosphatase substrate system (KPL, Gaithersburg, MD, USA) for 30 min at room temperature, and then the absorbance values (OD405) were obtained using a Dynatech MR4000 microplate reader. A standard curve for antibody quantitation (the company source) was generated in parallel to allow antibody concentration calculations.48
Measurement of neurotoxin neutralizing antibody titer
Neutralization titer of mice sera to BoNT/C was determined as described previously.31 Briefly, the sera from eight mice 6 weeks after vaccination with Ad/opt-BoNT/C-HC50 (2 × 107 p.f.u./mouse) were pooled, and then diluted in twofold series in PBS. Active BoNT/C was added into each dilution, followed by incubation at room temperature for 1 h. A mouse was injected i.p with the mixture of anti-serum and the BoNT/C corresponding 100 × MLD50 of BoNT/C before neutralization, four mice for each dilution. The animals were monitored for 4 days, and the number of deaths at each sample dilution was recorded. The animal survived from 100 × MLD50 of BoNT/C when the toxin was neutralized. Neutralizing antibody titers was defined as the maximum number of IU of antitoxin per ml of serum, resulting in 100% survival after challenge. One IU of type C antitoxin neutralizes 10 000 × MLD50.11, 51
Anti-adenovirus neutralizing antibody titer assay
Anti-adenovirus neutralizing antibody titers were evaluated using a modification of a previously described method.31, 52, 53, 54 Briefly, AD293 cells (Stratagene) were seeded in 96-well plates at a density of 104 cells/well in 200 μl of Eagle's minimum essential medium (EMEM) containing 10% fetal bovine serum (FBS) and incubated at 37 °C, 5% CO2 overnight before infection. Mouse sera were serially twofold diluted in EMEM containing 2% FBS after heat-inactivated at 55 °C for 45 min. A volume of 50 μl (104 p.f.u.) human WT Ad5 was prepared in EMEM containing 2% FBS and then combined with 50 μl of each diluted serum sample before an 1-h incubation at 37 °C. The virus–serum mixture was subsequently added to AD293 cells and incubated for 2 h at 37 °C. After the incubation, the virus–serum medium was replaced with 200 μl of EMEM containing 10% FBS. The cells were incubated at 37 °C until the negative wells (without antiserum) exhibited 90% cytopathic effect. The anti-Ad5 neutralizing antibody titer was defined as the reciprocal of maximum antiserum dilution that allowed >90% of cells to remain viable relative to the control.
Statistical analysis
Serum and mucosal antibody concentrations among different groups at different time points were compared using the LSD test, ANOVA/MANOVA (analysis of variance/multivariate analysis of variance) with Statistica 7.1 software (StatSoft, Tulsa, OK, USA). In comparing groups, those with P-values <0.05 and <0.01 were considered to be significant and very significant, respectively.
Acknowledgements
This work was supported by the US Public Service research Grant AI055946 (MZ) from the National Institute of Allergy and Infectious Diseases. ME and LLS were supported by National Institutes of Health Contract NO1-AI30028, Grants NS022153 and GM57345. We are grateful to Eric D Hesek for constructing and purifying the adenoviral vectors.
Accession codes
Accessions
GenBank/EMBL/DDBJ
Footnotes
Disclosure
Opinions, interpretations, conclusions and recommendations are those of the authors and are not necessarily endorsed by the US Army.
References
- 1.Villar RG, Elliott SP, Davenport KM. Botulism: the many faces of botulinum toxin and its potential for bioterrorism. Infect Dis Clin North Am. 2006;20:313–327. doi: 10.1016/j.idc.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 2.Atlas RM. Bioterriorism: from threat to reality. Annu Rev Microbiol. 2002;56:167–185. doi: 10.1146/annurev.micro.56.012302.160616. [DOI] [PubMed] [Google Scholar]
- 3.Montgomery VA, Makuch RS, Brown JE, Hack DC. The immunogenicity in humans of a botulinum type F vaccine. Vaccine. 1999;18:728–735. doi: 10.1016/S0264-410X(99)00264-9. [DOI] [PubMed] [Google Scholar]
- 4.Takeda M, Kasai H, Torii Y, Mukamoto M, Kohda T, Tsukamoto K. Protective effect of botulinum C/D mosaic toxoid against avian botulism. J Vet Med Sci. 2006;68:325–330. doi: 10.1292/jvms.68.325. [DOI] [PubMed] [Google Scholar]
- 5.Bennett AM, Perkins SD, Holley JL. DNA vaccination protects against botulinum neurotoxin type F. Vaccine. 2003;21:3110–3117. doi: 10.1016/S0264-410X(03)00260-3. [DOI] [PubMed] [Google Scholar]
- 6.Segelke B, Knapp M, Kadkhodayan S, Balhorn R, Rupp B. Crystal structure of Clostridium botulinum neurotoxin protease in a product-bound state: Evidence for noncanonical zinc protease activity. Proc Natl Acad Sci USA. 2004;101:6888–6893. doi: 10.1073/pnas.0400584101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woodward LA, Arimitsu H, Hirst R, Oguma K. Expression of HC subunits from Clostridium botulinum types C and D and their evaluation as candidate vaccine antigens in mice. Infect Immun. 2003;71:2941–2944. doi: 10.1128/IAI.71.5.2941-2944.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Byrne MP, Smith LA. Development of vaccines for prevention of botulism. Biochimie. 2000;82:955–966. doi: 10.1016/S0300-9084(00)01173-1. [DOI] [PubMed] [Google Scholar]
- 9.Oshima M, Hayakari M, Middlebrook JL, Atassi MZ. Immune recognition of botulinum neurotoxin type A: regions recognized by T cells and antibodies against the protective H(C) fragment (residues 855–1296) of the toxin. Mol Immunol. 1997;34:1031–1040. doi: 10.1016/S0161-5890(97)00107-7. [DOI] [PubMed] [Google Scholar]
- 10.Webb RP, Smith TJ, Wright PM, Montgomery VA, Meagher MM, Smith LA. Protection with recombinant Clostridium botulinum C1 and D binding domain subunit (Hc) vaccines against C and D neurotoxins. Vaccine. 2007;25:4273–4282. doi: 10.1016/j.vaccine.2007.02.081. [DOI] [PubMed] [Google Scholar]
- 11.Byrne MP, Smith TJ, Montgomery VA, Smith LA. Purification, potency, and efficacy of the botulinum neurotoxin type A binding domain from Pichia pastoris as a recombinant vaccine candidate. Infect Immun. 1998;66:4817–4822. doi: 10.1128/iai.66.10.4817-4822.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atassi MZ, Oshima M. Structure, activity, and immune (T and B cell) recognition of botulinum neurotoxins. Crit Rev Immunol. 1999;19:219–260. [PubMed] [Google Scholar]
- 13.Ravichandran E, Al-Saleem FH, Ancharski DM, Elias MD, Singh AK, Shamim M. Trivalent vaccine against botulinum toxin serotypes A, B, and E that can be administered by the mucosal route. Infect Immun. 2007;75:3043–3054. doi: 10.1128/IAI.01893-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith LA, Rusnak JM. Botulinum neurotoxin vaccines: past, present, and future. Crit Rev Immunol. 2007;27:303–318. doi: 10.1615/CritRevImmunol.v27.i4.20. [DOI] [PubMed] [Google Scholar]
- 15.Baldwin MR, Tepp WH, Pier CL, Bradshaw M, Ho M, Wilson BA. Characterization of the antibody response to the receptor binding domain of botulinum neurotoxin serotypes A and E. Infect Immun. 2005;73:6998–7005. doi: 10.1128/IAI.73.10.6998-7005.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith LA, Jensen MJ, Montgomery VA, Brown DR, Ahmed SA, Smith TJ. Roads from vaccines to therapies. Mov Disord. 2004;19:S48–S52. doi: 10.1002/mds.20009. [DOI] [PubMed] [Google Scholar]
- 17.Byrne MP, Titball RW, Holley J, Smith LA. Fermentation, purification, and efficacy of a recombinant vaccine candidate against botulinum neurotoxin type F from Pichia pastoris. Protein Expr Purif. 2000;18:327–337. doi: 10.1006/prep.2000.1200. [DOI] [PubMed] [Google Scholar]
- 18.Boles J, West M, Montgomery V, Tammariello R, Pitt ML, Gibbs P. Recombinant C fragment of botulinum neurotoxin B serotype (rBoNTB (HC)) immune response and protection in the rhesus monkey. Toxicon. 2006;47:877–884. doi: 10.1016/j.toxicon.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 19.Holley JL, Elmore M, Mauchline M, Minton N, Titball RW. Cloning, expression and evaluation of a recombinant sub-unit vaccine against Clostridium botulinum type F toxin. Vaccine. 2000;19:288–297. doi: 10.1016/S0264-410X(00)00155-9. [DOI] [PubMed] [Google Scholar]
- 20.Lee JS, Pushko P, Parker MD, Dertzbaugh MT, Smith LA, Smith JF. Candidate vaccine against botulinum neurotoxin serotype A derived from a Venezuelan equine encephalitis virus vector system. Infect Immun. 2001;69:5709–5715. doi: 10.1128/IAI.69.9.5709-5715.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bangari DS, Mittal SK. Development of nonhuman adenoviruses as vaccine vectors. Vaccine. 2006;24:849–862. doi: 10.1016/j.vaccine.2005.08.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tatsis N, Ertl HC. Adenoviruses as vaccine vectors. Mol Ther. 2004;10:616–629. doi: 10.1016/j.ymthe.2004.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Babiuk LA, Tikoo SK. Adenoviruses as vectors for delivering vaccines to mucosal surfaces. J Biotechnol. 2000;83:105–113. doi: 10.1016/S0168-1656(00)00314-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu Q, Arevalo MT, Pichichero ME, Zeng M. A new complementing cell line for replication-incompetent E1-deleted adenovirus propagation. Cytotechnology. 2006;51:133–140. doi: 10.1007/s10616-006-9023-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoelscher MA, Garg S, Bangari DS, Belser JA, Lu X, Stephenson I. Development of adenoviral-vector-based pandemic influenza vaccine against antigenically distinct human H5N1 strains in mice. Lancet. 2006;367:475–481. doi: 10.1016/S0140-6736(06)68076-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kobinger GP, Figueredo JM, Rowe T, Zhi Y, Gao G, Sanmiguel JC. Adenovirus-based vaccine prevents pneumonia in ferrets challenged with the SARS coronavirus and stimulates robust immune responses in macaques. Vaccine. 2007;25:5220–5231. doi: 10.1016/j.vaccine.2007.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shu Y, Winfrey S, Yang ZY, Xu L, Rao SS, Srivastava I. Efficient protein boosting after plasmid DNA or recombinant adenovirus immunization with HIV-1 vaccine constructs. Vaccine. 2007;25:1398–1408. doi: 10.1016/j.vaccine.2006.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hu RL, Liu Y, Zhang SF, Zhang F, Fooks AR. Experimental immunization of cats with a recombinant rabies-canine adenovirus vaccine elicits a long-lasting neutralizing antibody response against rabies. Vaccine. 2007;25:5301–5307. doi: 10.1016/j.vaccine.2007.05.024. [DOI] [PubMed] [Google Scholar]
- 29.Santosuosso M, McCormick S, Zhang X, Zganiacz A, Xing Z. Intranasal boosting with an adenovirus-vectored vaccine markedly enhances protection by parenteral Mycobacterium bovis BCG immunization against pulmonary tuberculosis. Infect Immun. 2006;74:4634–4643. doi: 10.1128/IAI.00517-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zeng M, Xu Q, Hesek ED, Pichichero ME. N-fragment of edema factor as a candidate antigen for immunization against anthrax. Vaccine. 2006;24:662–670. doi: 10.1016/j.vaccine.2005.08.056. [DOI] [PubMed] [Google Scholar]
- 31.Zeng M, Xu Q, Elias M, Pichichero ME, Simpson LL, Smith LA. Protective immunity against botulism provided by a single dose vaccination with an adenovirus-vectored vaccine. Vaccine. 2007;25:7540–7548. doi: 10.1016/j.vaccine.2007.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arnon SS, Schechter R, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS. Bioterrorism: Guidelines for Medical and Public Health Management. AMA Press: Chicago, IL; 2002. Botulinum toxin as a biological weapon; pp. 141–165. [Google Scholar]
- 33.Caya JG, Agni R, Miller JE. Clostridium botulinum and the clinical laboratorian: a detailed review of botulism, including biological warfare ramifications of botulinum toxin. Arch Pathol Lab Med. 2004;128:653–662. doi: 10.5858/2004-128-653-CBATCL. [DOI] [PubMed] [Google Scholar]
- 34.Fujihashi K, Staats HF, Kozaki S, Pascual DW. Mucosal vaccine development for botulinum intoxication. Expert Rev Vaccines. 2007;6:35–45. doi: 10.1586/14760584.6.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kobayashi R, Kohda T, Kataoka K, Ihara H, Kozaki S, Pascual DW. A novel neurotoxoid vaccine prevents mucosal botulism. J Immunol. 2005;174:2190–2195. doi: 10.4049/jimmunol.174.4.2190. [DOI] [PubMed] [Google Scholar]
- 36.Maddaloni M, Staats HF, Mierzejewska D, Hoyt T, Robinson A, Callis G. Mucosal vaccine targeting improves onset of mucosal and systemic immunity to botulinum neurotoxin A. J Immunol. 2006;177:5524–5532. doi: 10.4049/jimmunol.177.8.5524. [DOI] [PubMed] [Google Scholar]
- 37.Lemiale F, Kong WP, Akyurek LM, Ling X, Huang Y, Chakrabarti BK. Enhanced mucosal immunoglobulin A response of intranasal adenoviral vector human immunodeficiency virus vaccine and localization in the central nervous system. J Virol. 2003;77:10078–10087. doi: 10.1128/JVI.77.18.10078-10087.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Casimiro DR, Chen L, Fu TM, Evans RK, Caulfield MJ, Davies ME. Comparative immunogenicity in rhesus monkeys of DNA plasmid, recombinant vaccinia virus, and replication-defective adenovirus vectors expressing a human immunodeficiency virus type 1 gag gene. J Virol. 2003;77:6305–6313. doi: 10.1128/JVI.77.11.6305-6313.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang Y, Li Q, Ertl HC, Wilson JM. Cellular and humoral immune responses to viral antigens create barriers to lung-directed gene therapy with recombinant adenoviruses. J Virol. 1995;69:2004–2015. doi: 10.1128/jvi.69.4.2004-2015.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barouch DH, McKay PF, Sumida SM, Santra S, Jackson SS, Gorgone DA. Plasmid chemokines and colony-stimulating factors enhance the immunogenicity of DNA priming-viral vector boosting human immunodeficiency virus type 1 vaccines. J Virol. 2003;77:8729–8735. doi: 10.1128/JVI.77.16.8729-8735.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Papp Z, Babiuk LA, Baca-Estrada ME. The effect of pre-existing adenovirus-specific immunity on immune responses induced by recombinant adenovirus expressing glycoprotein D of bovine herpesvirus type 1. Vaccine. 1999;17:933–943. doi: 10.1016/S0264-410X(98)00279-5. [DOI] [PubMed] [Google Scholar]
- 42.Fischer L, Tronel JP, Pardo-David C, Tanner P, Colombet G, Minke J. Vaccination of puppies born to immune dams with a canine adenovirus-based vaccine protects against a canine distemper virus challenge. Vaccine. 2002;20:3485–3497. doi: 10.1016/S0264-410X(02)00344-4. [DOI] [PubMed] [Google Scholar]
- 43.He TC, Zhou S, da Costa LT, Yu J, Kinzler KW, Vogelstein B. A simplified system for generating recombinant adenoviruses. Proc Natl Acad Sci USA. 1998;95:2509–2514. doi: 10.1073/pnas.95.5.2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zeng M, Smith SK, Siegel F, Shi Z, Van Kampen KR, Elmets CA. AdEasy system made easier by selecting the viral backbone plasmid preceding homologous recombination. Biotechniques. 2001;31:260–262. doi: 10.2144/01312bm04. [DOI] [PubMed] [Google Scholar]
- 45.Kimura K, Fujii N, Tsuzuki K, Murakami T, Indoh T, Yokosawa N. The complete nucleotide sequence of the gene coding for botulinum type C1 toxin in the C-ST phage genome. Biochem Biophys Res Commun. 1990;171:1304–1311. doi: 10.1016/0006-291X(90)90828-B. [DOI] [PubMed] [Google Scholar]
- 46.Singh SR, Hulett K, Pillai SR, Dennis VA, Oh MK, Scissum-Gunn K. Mucosal immunization with recombinant MOMP genetically linked with modified cholera toxin confers protection against Chlamydia trachomatis infection. Vaccine. 2006;24:1213–1224. doi: 10.1016/j.vaccine.2005.08.097. [DOI] [PubMed] [Google Scholar]
- 47.Russell MW, Wu HY. Distribution, persistence, and recall of serum and salivary antibody responses to peroral immunization with protein antigen I/II of Streptococcus mutans coupled to the cholera toxin B subunit. Infect Immun. 1991;59:4061–4070. doi: 10.1128/iai.59.11.4061-4070.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zeng M, Xu Q, Pichichero ME. Protection against anthrax by needle-free mucosal immunization with human anthrax vaccine. Vaccine. 2007;25:3558–3594. doi: 10.1016/j.vaccine.2007.01.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Watanabe I, Hagiwara Y, Kadowaki SE, Yoshikawa T, Komase K, Aizawa C. Characterization of protective immune responses induced by nasal influenza vaccine containing mutant cholera toxin as a safe adjuvant (CT112K) Vaccine. 2002;20:3443–3455. doi: 10.1016/S0264-410X(02)00351-1. [DOI] [PubMed] [Google Scholar]
- 50.Arimitsu H, Lee JC, Sakaguchi Y, Hayakawa Y, Hayashi M, Nakaura M. Vaccination with recombinant whole heavy chain fragments of Clostridium botulinum Type C and D neurotoxins. Clin Diagn Lab Immunol. 2004;11:496–502. doi: 10.1128/CDLI.11.3.496-502.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nowakowski A, Wang C, Powers DB, Amersdorfer P, Smith TJ, Montgomery VA. Potent neutralization of botulinum neurotoxin by recombinant oligoclonal antibody. Proc Natl Acad Sci USA. 2002;99:11346–11350. doi: 10.1073/pnas.172229899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shi Z, Zeng M, Yang G, Siegel F, Cain LJ, van Kampen KR. Protection against tetanus by needle-free inoculation of adenovirus-vectored nasal and epicutaneous vaccines. J Virol. 2001;75:11474–11482. doi: 10.1128/JVI.75.23.11474-11482.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Harvey BG, Hackett NR, El-Sawy T, Rosengart TK, Hirschowitz EA, Lieberman MD. Variability of human systemic humoral immune responses to adenovirus gene transfer vectors administered to different organs. J Virol. 1999;73:6729–6742. doi: 10.1128/jvi.73.8.6729-6742.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zabner J, Ramsey BW, Meeker DP, Aitken ML, Balfour RP, Gibson RL. Repeat administration of an adenovirus vector encoding cystic fibrosis transmembrane conductance regulator to the nasal epithelium of patients with cystic fibrosis. J Clin Invest. 1996;97:1504–1511. doi: 10.1172/JCI118573. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


