Abstract
Pulmonary complications are common and often lethal in hematopoietic SCT recipients. The objective of this prospective interventional study was to evaluate the etiology, diagnostic procedures, risk factors and outcome of pulmonary complications in a cohort of hematopoietic SCT recipients followed up for 1 year. For patients suffering from a pulmonary complication, a diagnostic algorithm that included non-invasive and bronchoscopic procedures was performed. We identified 73 pulmonary complications in 169 patients: 50 (68%) were pneumonias; 21 (29%) were non-infectious complications and 2 (3%) were undiagnosed. Viruses (particularly Rhinovirus) and bacteria (particularly P. aeruginosa) (28 and 26%, respectively) were the most common causes of pneumonia. A specific diagnosis was obtained in 83% of the cases. A non-invasive test gave a specific diagnosis in 59% of the episodes. The diagnostic yield of bronchoscopy was 67 and 78% in pulmonary infections. Early bronchoscopy (⩽5 days) had higher diagnostic yield than late bronchoscopy (78 vs 23%; P=0.02) for pulmonary infections. Overall mortality was 22 and 32% of all fatalities were due to pulmonary complications. Pulmonary complications are common and constitute an independent risk factor for mortality, stressing the importance of an appropriate clinical management.
Supplementary information
The online version of this article (doi:10.1038/bmt.2014.151) contains supplementary material, which is available to authorized users.
Subject terms: Haematopoietic stem cells
Introduction
Pulmonary complications (PCs) are among the most common and lethal complications suffered by hematopoietic SCT (HSCT) patients.1, 2, 3, 4 The increasing number of indications and the selection of more debilitated patients as potential candidates for HSCT seem to be changing the epidemiology of PC.5,6 Studies have shown that in immunocompromised patients an early identification of the etiology of PC improves survival.7,8 Fiberoptic bronchoscopy (FOB) has an important role in the diagnosis of PC;9, 10, 11, 12 however, detractors of this technique consider that the information provided may be also obtained by different non-invasive explorations.13, 14, 15 The majority of the studies evaluating the etiology, diagnosis and prognosis of PC in patients with hematologic diseases are retrospective,4,6,16 and include both non-transplantation and transplantation recipients.2,7 We hypothesized that the prospective follow-up of a cohort of HSCT recipients may improve the clinical management of PC. First, the knowledge of the epidemiology of the PC with the different prevalence of infectious and non-infectious etiologies can be accurately determined. Second, predetermined criteria for performing a FOB should clarify the role of this technique by better defining the diagnostic yield, clinical implications and potential complications. Finally, the identification of prognostic factors is much more precise when data are recorded prospectively in a homogeneous group of immunocompromised patients.
The aim of this study was to evaluate the incidence, diagnostic and clinical implications of non-invasive and FOB explorations, risk factors and outcome of PC. To this aim, a cohort of consecutive patients requiring HSCT was followed-up for 1 year and the PC were closely analyzed.
Materials and methods
Patients
This is a prospective interventional study to evaluate the PC in a cohort of consecutive HSCT recipients; that was followed-up for 1 year (Figure 1 and see Supplementary Information).
Figure 1.
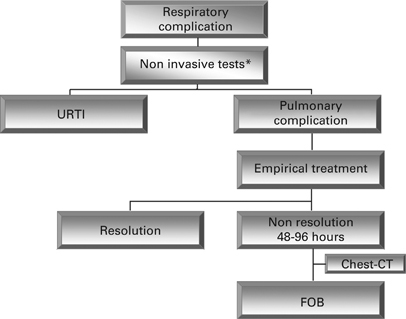
Diagnostic management of respiratory complications. CT=computed tomography; FOB=fiberoptic bronchoscopy; URTI=upper respiratory tract infection. *Non invasive tests: blood samples for culture and antigen determination, sputum culture, nasopharyngeal swabs, urinary antigen tests and chest X-ray.
Data collection
Different variables were recorded after the inclusion in the study and whenever a new respiratory complication was identified (see Supplementary Information).
Diagnostic procedures
On the basis of the results of the diagnostic tests (Figure 1) and the clinical judgment of the physician in charge, empirical treatment was initiated and a decision of whether or not the patient required hospital admission and further diagnostic explorations was made.
Computed tomography was requested after 24–48 h of detection of positive aspergillus galactomannan antigen, after 4–5 days of persistent fever despite empirical treatment or prior to a FOB whenever this exploration was indicated.
FOB was indicated after no response to 48–96 h of empirical treatment (Figure 1). We defined early FOB when the procedure was performed ⩽5 days since the identification of the PC and late FOB when it was performed after this time period.2 Patients were not eligible for FOB if arterial PaO2 was <60 mm Hg with oxygen administration.
Bronchoscopic procedures included bronchial aspiration (diffuse aspiration of airway secretions) and bronchoalveolar lavage (BAL) that involves the instillation and subsequent aspiration of 100 mL of sterile saline solution in two aliquots (50 mL each) in the involved lobe or in the middle lobe or lingula in patients with diffuse pulmonary infiltrates. Other diagnostic techniques such as transbronchial biopsies were exceptionally carried out in selected patients.
Sample processing
Specific primers for influenza viruses types A, B and C, respiratory syncytial virus type A and B, parainfluenza viruses 1, 2, 3 and 4 and adenovirus in one real-timePCR assay were performed in BAL and nasopharyngeal swab as described previously, and for generic detection of rhinoviruses and enteroviruses in another real-time-PCR assay.17,18 More details are described in the Supplementary Information.
CMV detection in serum was done using a monoclonal antibody against the pp65-CMV protein (MonoFluo Kit CMV, Bio-Rad, Redmond, WA, USA) and culture or PCR in BAL.
Detection of aspergillus galactomannan antigen in serum and BAL was performed using an enzyme immunoassay method (Platelia Aspergillus, Sanofi Diagnostics Pasteur, France).
Diagnostic definitions
The etiology of PC was established based on the results of the diagnostic procedures performed, the response to the specific treatment and the histopathological evaluation of biopsy samples when available. PCs were further divided into infectious, non-infectious or undetermined.
Pneumonia was defined as presence of fever (⩾38 °C), cough, dyspnea, and/or purulent expectoration and a new or progressive pulmonary infiltrate not explained by any other non-infectious cause.19
The diagnosis of viral pneumonia was confirmed with multiplex reverse transcription nested real-time-PCR assays performed in BAL. Mixed pneumonia was based on the identification of >1 pathogen.
The classification of proven, probable and possible aspergillosis was established based on definitions of the consensus of the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group.20
Pulmonary edema was diagnosed using both clinical and echocardiographic criteria. Cryptogenetic organizing pneumonia and drug-induced pulmonary toxicity were diagnosed histopathologically from samples obtained by transbronchial or open-lung biopsies. Engraftment syndrome was defined using the Spitzer criteria.21 Capillary leak syndrome was defined as unexplained weight gain of >3% within 24 h, generalized edema, and non-responsiveness to furosemide.22
No response to empirical treatment: chest X-ray or computed tomography-scan revealing new or progressive lung infiltrates and/or persistent fever.
Change in therapy: any addition or deletion to the treatment attributable to positive or negative results from the bronchoscopy.15
Among patients who presented multiple complications, each episode was recorded and considered independently. Early/late PC was considered when appearing before or after 6 months of transplantation.
Transplantation procedure
The conditioning regimen, immunosuppressive and support therapies were administered following international accepted protocols. Non-myeloablative regimens were used in patients older than 50 years, with relevant comorbidity or with previous transplantation. All allo-HSCT recipients received double-drug immunosuppression for GVHD prophylaxis. Donors and recipients were tested for CMV serology pre-transplantation.
As anti-infective prophylaxis, levofloxacin was prescribed until engraftment and fluconazol until +75. Also, a preemptive strategy for CMV infections was followed according to guidelines.23 HEPA-filtered rooms were always used during admission.
Statistical analysis
We used n (%) for categorical variables and mean (s.d.) for continuous variables or median (interquartile range) for those with non-normal distributions. We compared categorical variables with χ2 or Fisher’s exact tests. The unpaired Student’s t-test was used to compare quantitative continuous variables between groups; those with non-normal distribution were analyzed using the Mann–Whitney U-test.
Univariate and multivariate logistic regression analyses were performed to investigate clinical factors associated with an increased risk of mortality. Variables that showed a significant result univariately (P<0.1) were included in the multivariate logistic regression backward stepwise model. Variables highly correlated were excluded from multivariate analyses. The Hosmer–Lemeshow goodness-of-fit test was performed to assess the overall fit of the model.24 Survival curves were obtained using the Kalplan–Meier method and compared using the log-rank test.
The level of significance was set at 0.05 (two tailed). All statistical analyses were done with SPSS version 18.0 (SPSS Inc., Chicago, IL, USA).
Results
Etiology of PC
Between July 2009 and November 2011, 209 HSCT were performed in 203 patients and 175 (84%) of them were included in the study (Table 1).
Table 1.
Patients characteristics
| Characteristics | No (%) |
|---|---|
| Median age (years)±s.d. | 49±14 |
| Sex | |
| Male | 91 (54) |
| Female | 78 (46) |
| Hematologic disease | |
| Multiple myeloma | 40 (23) |
| Non-Hodgkin lymphoma | 37 (21) |
| AML | 33 (19) |
| Hodgkin disease | 14 (8) |
| Amyloidosis | 10 (6) |
| ALL | 9 (5) |
| Myelodysplastic syndrome | 8 (4) |
| CML | 6 (3) |
| Miscellaneous hematologic malignancies | 12 (7) |
| Non-hematologic disease | |
| Crohn | 6 (3) |
| Type of HSCT | |
| Autologous | 96 (55) |
| Allogeneic | 79 (45) |
| Related | 35 (44) |
| Unrelated | 44 (56) |
| Ablative conditioning | 15 (19) |
| Reduced intensity conditioning | 64 (81) |
| Source of stem cells | |
| Peripheral blood | 162 (92) |
| BM | 8 (5) |
| Cord blood | 3 (2) |
| Peripheral blood and BM | 2 (1) |
| Recipient CMV serostatus | |
| Positive | 128 (73) |
| Negative | 47 (27) |
Abbreviation: HSCT=hematopoietic SCT.
A total of 73 episodes of PC were identified in 51 patients (30% of the studied population) (35 patients presented 1 complication; 11 patients, 2 complications; 4 patients, 3 complications; and 1 patient, 4 complications). A specific diagnosis was obtained in 61 of the 73 episodes evaluated (83%).
A total of 50 episodes of pneumonia (Table 2) were identified (68% of PC), most frequently viral (28% of lung infections), followed by bacterial (26%) and fungal (16%). Mixed infections (both bacterial and viral) were diagnosed in five episodes (10%). Rhinovirus and respiratory syncytial virus were the most frequent viruses isolated, and P. aeruginosa was the most frequently involved bacteria causing pneumonia. In particular, P. aeruginosa was involved in 27% of the diagnosed pulmonary infections (considering both isolated and mixed infections). Thirty-six percent of the isolated P. aeruginosa strains were multiresistant.
Table 2.
Chronology of pulmonary infections
| Pathogens | Cases | <3 months | 3–6 months | 6–12 months | >12 months |
|---|---|---|---|---|---|
| Bacterial | |||||
| Gram negative | |||||
| P. aeruginosa | 7 | 2 | 4 | 1 | |
| S. maltophila | 1 | 1 | |||
| Gram positive | |||||
| S. pneumoniae | 2 | 1 | 1 | ||
| E. faecium | 1 | 1 | |||
| Nocardia | 1 | 1 | |||
| Mixed bacterial infections | |||||
| P. aeruginosa+E. faecalis | 1 | 1 | |||
| Viral | |||||
| RSV | 3 | 2 | 1 | ||
| Rhinovirus | 3 | 2 | 1 | ||
| ADV | 2 | 2 | |||
| Parainfluenzae virus type 3 | 2 | 1 | 1 | ||
| CMV | 2 | 1 | 1 | ||
| Enterovirus | 1 | 1 | |||
| Influenza A virus | 1 | 1 | |||
| Fungal | |||||
| Probable fungal infection | 4 | 4 | |||
| Possible fungal infection | 4 | 3 | 1 | ||
| Mixed infections | |||||
| P. aeruginosa+Rhinovirus | 1 | 1 | |||
| P. aeruginosa+Rhinovirus+Coronavirus | 1 | 1 | |||
| P. aeruginosa+S. malthopila+RSV+ADV | 1 | 1 | |||
| S. pneumoniae+Rhinovirus | 1 | 1 | |||
| S. pneumoniae+Influenza A virus | 1 | 1 | |||
| No pathogen isolated | 10 | 5 | 2 | 1 | 2 |
| Total | 50 | 28 (56%) | 12 (24%) | 7 (14%) | 3 (6%) |
Abbreviations: ADV=adenovirus; RSV=respiratory syncytial virus.
Most of the infections occurred during the first 6 months after HSCT (80%). Seventeen out of the 50 (34%) patients suffering a pulmonary infection were neutropenic at diagnosis (15% of bacterial infections, 28% of viral infections and 60% mixed infections).
Non-infectious PC (Table 3) were identified in 21 out of the 73 episodes (29%). Pulmonary edema (4/21, 19%) and underlying disease progression (4/21, 19%) were the most common etiologies. Transbronchial biopsies were performed in three patients with persistent pulmonary infiltrates after empirical treatment and a suspected non-infectious PC. There were no remarkable side effects after transbronchial biopsies. Also, one open-lung biopsy was required to diagnose a case of pharmacologic pulmonary toxicity. Eighty-one percent of the non-infectious pulmonary episodes were early complications.
Table 3.
Chronology of non-infectious pulmonary complications
| Etiological diagnosis | Cases | 3 months | 3–6 months | 6–12 months | >12 months |
|---|---|---|---|---|---|
| Acute pulmonary edema | 4 | 4 | |||
| Underlying disease progression | 4 | 3 | 1 | ||
| Capillary leak syndrome | 3 | 3 | |||
| Multiorgan failure | 3 | 3 | |||
| Engraftment syndrome | 2 | 2 | |||
| Pulmonary hypertension | 1 | 1 | |||
| Bronchiolitis obliterans | 1 | 1 | |||
| Cryptogenic organizing pneumonia | 1 | 1 | |||
| Pulmonary drug toxicity | 1 | 1 | |||
| Interstitial lung disease | 1 | 1 | |||
| Total | 21 | 16 (76%) | 1 (5%) | 4 (19%) | 0 (0%) |
Of the PC diagnosed over the first month, 31% of the infectious and 27% of the non-infectious appeared in the first 7 days after transplantation.
Diagnostic yield of non-invasive diagnostic techniques
Sixteen (76%) non-infectious pulmonary episodes were diagnosed with non-invasive techniques. On the other hand, non-invasive tests gave a specific diagnostic in 27 episodes of pneumonia (54% of infectious PC). Specifically, blood cultures were positive in 9 (18%). Although, all the 14 viral pneumonias identified in our cohort were diagnosed by BAL, interestingly 11 of them also had concordant positive nasopharyngeal swab (diagnostic yield of nasopharyngeal swab of 75%).
Four cases of S. pneumoniae were diagnosed by a urinary antigen test. One of these cases was also confirmed by blood culture, bronchial aspiration and BAL and other one had also a positive blood culture.
Computed tomography was performed in 39 episodes (78%). In 12 cases (31%), the computed tomography was performed at the time the symptoms appear. The most common radiological finding in patients with bacterial pneumonia was consolidation (38%) and in viral pneumonia, ground-glass opacities (43%).
Diagnostic yield of bronchoscopic techniques
FOB was performed in 40 out of the 73 episodes (55%): 67% early and 33% late FOB. Reasons to perform a delayed FOB were: initial contraindication due to severe respiratory in five patients; progression of the pulmonary infiltrates in four patients and to assess pulmonary infiltrates finally diagnosed of non-infectious PC in four patients.
The overall diagnostic yield of FOB was 67% (27/40). This percentage increased up to 78% (26/33) in patients with an infectious PC. Specific diagnosis obtained by FOB was: viral pneumonia in 13 patients, bacterial pneumonia in 6 patients, fungal pneumonia in 3 patients and mixed pneumonia in 4 patients. The diagnostic yield of the different endoscopic techniques, and the influence of the results obtained in treatment decisions are shown in Table 4. The diagnostic yield of FOB for pulmonary infections was significantly higher when performed early (early FOB, 78% vs late FOB, 23%; P=0.02). No differences between early and late FOB were evidenced as regards changes in empirical treatment (44 vs 38%; P=NS). There were no remarkable side effects after FOB. Figure 2 illustrates the diagnostic yield of non-invasive tests and FOB on pulmonary infections.
Table 4.
FOB in 33 patients with pulmonary infections
| Patients (%) | |
|---|---|
| Neutropenia | 14 (42) |
| Diffuse lung infiltrates | 18 (54) |
| Early FOB | 25 (76) |
| FOB-BAL | 33 (100) |
| Diagnostic yield of BAL | 24/33 (73) |
| FOB-BAS | 28 (85) |
| Diagnostic yield of BAS | 8/28 (28) |
| Change empiric therapy | 15 (45) |
| Non-covered microorganisms | 9 |
| Isolation of a resistant pathogen | 5 |
| Removal of medication | 1 |
| Non-invasive mechanical ventilation | 2 (6) |
| Intubated before FOB | 9 (27) |
| Therapy before FOB | |
| Antibiotics | 33 (100) |
| Antifungal agents | 13 (39) |
| Antiviral agents | 8 (24) |
Abbreviations: BAL=bronchoalveolar lavage; BAS=bronchoaspirate; CT=computed tomography; FOB=fiberoptic bronchoscopy.
Figure 2.
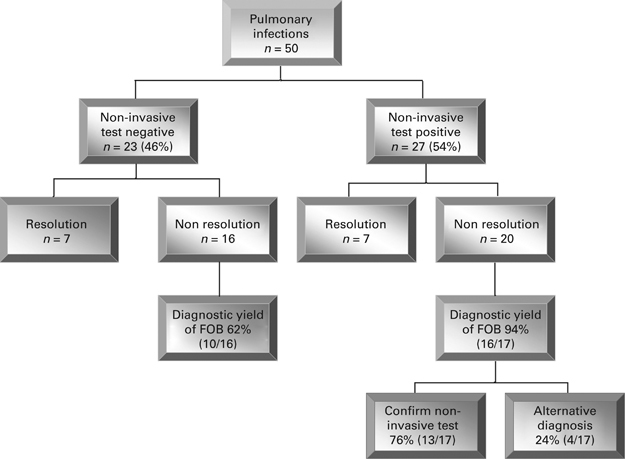
Management of pulmonary infection complications: patient flow chart. FOB=fiberoptic bronchoscopy.
Risk factors for development of PC
Allo-HSCT (58 vs 24%; P<0.001) and duration of neutropenia (15±5 vs 12±3 days; P<0.001) were significant risk factors for development of PC following HSCT. On the other hand, ablative conditioning (47 vs 44%), unrelated donor (48 vs 40%), recipient CMV serostatus positive (29 vs 30%), leukemia (37 vs 26%) and active smoking (32 vs 29%) were not significant risk factors.
The relationship between type of transplantation and risk of PC was particularly evident when only infectious PC were considered. Thus, pulmonary infections occurred in 27/79 (34%) of allo-HSCT patients and 9/96 (9%) of auto-HSCT recipients (P<0.001). Duration of neutropenia (16±5 vs 12±4 days; P<0.001) was also a risk factor associated with pulmonary infections.
Outcome
Overall mortality after 1 year follow-up was 22% (38 of 169 patients). Causes of death are listed in Table 5. Thirty-two percent of all cause mortality was due to PC (12 of 38 cases). Most of the lethal PC were due to infections (9 of 12 cases, 75%). Remarkably, P. aeruginosa was the most commonly involved microorganism causing death (55% of lethal pulmonary infections). Six out of 13 (46%) cases of bacterial pneumonia died compared with 1 out of 14 cases of viral pneumonia (7%) (P=0.026).
Table 5.
Mortality causes in the cohort studied
| Mortality after HSCT | No (%) |
|---|---|
| Total | 38 (22) |
| Causes | |
| Non-pulmonary etiologies | 26 (68) |
| Underlying disease progression | 9 (24) |
| GVHD | 8 (21) |
| Non-pulmonary infections | 3 (8) |
| Lymphoproliferative disorder | 3 (8) |
| Acute myocardical infarction | 1 (2) |
| Hemolytic anemia | 1 (2) |
| Trombotic microangiopathy | 1 (2) |
| Pulmonary etiologiesa | 12 (32) |
| Infectious | 9 (24) |
| P. aeruginosa | 3 |
| S. maltophila | 1 |
| E. faecium | 1 |
| P. aeruginosa+E. faecalis | 1 |
| P. aeruginosa+S. maltophila+RSV+ADV | 1 |
| CMV | 1 |
| Aspergillus | 1 |
| Non-infectious | 3 (8) |
| Non-specific intersticial pneumonia | 1 |
| Pulmonary drug toxicity | 2 |
Abbreviations: ADV=Adenovirus; HSCT=hematopoietic SCT; RSV=respiratory syncytial virus.
aPost-mortem examination was performed in 4 out of the 12 patients who died as a result of the pulmonary complication. In three cases, necropsy confirmed the clinical diagnosis of pneumonia; in one case, demonstrated an undiagnosed S. maltophila pneumonia and one last case demonstrated signs of diffuse pulmonary damage with negative cultures.
Allo-HSCT, presence of PC, grade II–IV acute GVHD and duration of neutropenia were risk factors associated with overall mortality in the univariate analysis (Table 6). In the multivariate analysis, allo-transplantation and presence of PC were independent risk factors for mortality (Table 6). The model to predict mortality was well calibrated with a P-value in the Hosmer-Lemeshow test of 0.075.
Table 6.
Mortality: results of univariate and multivariate analysis
| Deaths | Survivors | Univariate | Multivariate | Multivariate | |
|---|---|---|---|---|---|
| 38 cases | 131 cases | P-value | OR (95% CI) | P-value | |
| Mean age (years)±s.d. | 48±16 | 49±13 | |||
| Sex (%) | |||||
| Male | 22 (58) | 69 (53) | |||
| Female | 16 (42) | 62 (47) | |||
| Underlying disease (%) | |||||
| Lymphoma | 11 (29) | 37 (28) | |||
| AML | 9 (24) | 24 (18) | |||
| CLL | 5 (13) | 1 (1) | |||
| ALL | 4 (10) | 5 (4) | |||
| Multiple myeloma | 3 (8) | 34 (26) | |||
| Amyloidosis | 3 (8) | 7 (5) | |||
| Myelodysplastic syndrome | 0 (0) | 8 (6) | |||
| Other hematologic disorders | 3 (8) | 9 (7) | |||
| Other non-hematologic disorders | 0 (0) | 6 (5) | |||
| Transplantation type (%) | <0.001 | 4.02 (1.55–10.40) | 0.004 | ||
| Autologous | 8 (21) | 82 (63) | |||
| Allogeneic | 30 (79) | 49 (37) | |||
| Conditioning in allo-HSCT | |||||
| Ablative conditioning | 5 (8) | 10 (8) | |||
| Reduce intensive conditioning | 25 (66) | 39 (30) | |||
| Source of stem cells (%) | |||||
| Peripheral blood | 32 (84) | 124 (94) | |||
| BM | 4 (10) | 4 (3) | |||
| Peripheral blood and BM | 1 (3) | 1 (1) | |||
| Cord blood | 1 (3) | 2 (2) | |||
| FEV1 (%) | |||||
| <70% | 4 (11) | 6 (5) | |||
| ⩾70% | 34 (89) | 125 (95) | |||
| DLCO (%) | |||||
| <60 | 7 (18) | 13 (10) | |||
| ⩾60 | 31 (82) | 118 (90) | |||
| Pulmonary complication (%) | <0.001 | 10.94 (4.49–26.68) | <0.001 | ||
| Yes | 28 (74) | 21 (16) | |||
| No | 10 (26) | 110 (84) | |||
| GVHD>grade 2 (%) | 0.018 | ||||
| Yes | 13 (34) | 20 (15) | |||
| No | 25 (66) | 111 (85) | |||
| Duration of neutropenia (days)±s.d. | 15±5 | 13±4 | 0.011 | ||
Abbreviations: DLCO=diffusing capacity for carbon monoxide; FEV1=forced expiratory volume in 1 s; HSCT=hematopoietic SCT.
Discussion
Epidemiology of PC
The present study demonstrates that PCs are common after HSCT, involving almost 30% of the recipients, and are particularly prevalent over the first 6 months after transplantation. These PC are mostly infectious (68%) with an associated mortality of 18% (9/50). The relative frequencies of different PCs vary at different post-transplantation periods.16,25 In this sense, a potential strength of the present study is that by following up all the patients included in the cohort for 1 year, an accurate determination of the prevalence of the different PC can be made. Remarkably, viruses were the most common cause of pulmonary infections, representing 47% (19/40) of pneumonias. Of note, 26% of the episodes of viral pneumonia were mixed (both bacteria and viruses) confirming that co-infection is a common occurrence in these patients.26 The associated mortality of viral pneumonias was lower than the mortality caused by bacteria, corroborating the results from different series.27,28 However, the important role that viruses have in the genesis of PC reinforces the importance of prevention strategies.29
As in other prospective studies, bacteria were involved in 45% of the identified pulmonary infections in our cohort.19 Remarkably, P. aeruginosa infections represented 61% of total bacterial infections. This finding confirms the current predominance of Gram-negative rods over Gram-positive cocci observed by other authors.30 Interestingly, fluoroquinolone resistance was frequent (36% of P. aeruginosa isolates) probably owing to the widespread use of fluoroquinolone prophylaxis. This is particularly important as the associated mortality of P. aeruginosa in our series was 45%. Therefore the implementation of prophylactic protocols should be periodically re-evaluated in HSCT recipients depending on the different resistance patterns of each institution.2,30
Probable aspergillosis was diagnosed in only four patients, accounting for 10% of the diagnosed pulmonary infections. The low incidence of aspergillosis is most likely the result of the intense surveillance and prophylactic programs designed to avoid these infections.31
Diagnostic evaluation of PC
The present study confirms that the majority of the PC can be etiologically identified (83%).2 A significant proportion of these episodes (59%) were diagnosed with the implementation of different non-invasive tests thus avoiding the requirement of more invasive procedures. Remarkably, nasopharyngeal swab was a very useful diagnostic tool providing the diagnosis of viral pneumonia in 75% of cases, and in all of them the results were confirmed with BAL.29 Azoulay et al.17 confirmed the utility of non-invasive tests in critically ill hematology and oncology patients with acute respiratory failure. More controversial is the role of FOB in the management of PC.9,15,32,33 In our cohort, with pre-established criteria to perform FOB, the overall diagnostic yield was 67% and increased up to 78% in pulmonary infections. Overall, 28% of the episodes of pulmonary infection could only be diagnosed by this technique. In almost half of the cases, the information obtained caused a change in the empiric treatment. Interestingly, in cases with negative non-invasive tests, the diagnostic yield of FOB was 62% (Figure 2) demonstrating its utility in this particular scenario. Even in those patients with positive non-invasive tests, but with an unsolved or unfavorable clinical course, FOB identified unsuspected microorganisms in 24% of the cases (Figure 2). Early FOB proportioned a significant increase of isolated pathogens compared with late FOB and mortality in the former group was somewhat lower, although the difference was not statistically significant. Our group had already shown that one of the most critical factors influencing the yield of FOB is the time elapsed between the initiation of symptoms and FOB performance.7,34 Establishing an early diagnosis leads to changes in empirical treatment and probably, improvement in prognosis. Shannon et al.33 highlighted the importance of early diagnosis demonstrating that the diagnostic yield of FOB wanes with the elapsed time following clinical presentation. As in other series, we did not observe remarkable side effects after FOB.2,9,33 In this sense, the conclusive demonstration by Azoulay et al.,17 in a prospective randomized study showing that FOB does not increase the proportion of patients requiring mechanical ventilation, reinforce the safety of this procedure and should help reluctant physicians caring for these patients to implement this procedure in early stages.
Outcome
Although prospective information regarding the outcome of HSCT recipients is scarce, the overall mortality of 22% in our series fits with that obtained recently by Aguilar-Guisado et al.19 in allo-HSCT recipients. As reported in other series, relapse of disease and chronic GVHD were the most important causes of mortality.19,35 Interestingly, suffering a PC, particularly one of infectious origin, was responsible for one-third of the overall mortality and was also an independent risk factor for mortality, stressing the importance of the proper clinical management of these complications.
A limitation of the present study is that all patients were treated at a single centre and the sample size was relatively small, particularly for the evaluation of prognostic factors. However, the study includes every HSCT performed consecutively in the centre during a 1-year follow-up and data related to complications and clinical management have been obtained prospectively.
In summary, PC in HSCT recipients are common. In our series, viral infection is the most frequent etiology; however mortality due to bacterial pneumonia, in particular P. aeruginosa is much higher. PC are responsible for one-third of all the fatalities. Although in this prospective study we have shown the utility of non-invasive tests and the potential role of FOB when the evolution is unfavorable, this must be confirmed in further controlled trials.
Supplementary information
Acknowledgements
CML and CA have contributed in the study design, in the acquisition, analysis and interpretation of data and writing of the manuscript. AT and MR have participated in the study design and in the revision of the article. MAM, JPdlB, MS and JM have contributed in the interpretation of data. RD has contributed in the acquisition of data. AG conducted the statistical analysis. The project was supported by FIS-ISCIII (Fondo de Investigación Sanitaria, Instituto de Salud Carlos III) (PI10/00507), SEPAR 2010 and FUCAP 2010. CML was supported by a clinical research grant from SEPAR 2012 and Hospital Clínic Barcelona (Beca Josep Font 2009-2012).
Competing interests
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on Bone Marrow Transplantation website
References
- 1.Gratwohl A, Baldomero H, Aljurf M, Pasquini MC, Bouzas LF, Yoshimi A. Hematopoietic stem cell transplantation: a global perspective. JAMA. 2010;303:1617–1624. doi: 10.1001/jama.2010.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rañó A, Agustí C, Jimenez P, Angrill J, Benito N, Danés C. Pulmonary infiltrates in non-HIV immunocompromised patients: a diagnostic approach using non-invasive and bronchoscopic procedures. Thorax. 2001;56:379–387. doi: 10.1136/thorax.56.5.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lim DH, Lee J, Lee HG, Park BB, Peck KR, Oh WS. Pulmonary complications after hematopoietic stem cell transplantation. J Korean Med Sci. 2006;21:406–411. doi: 10.3346/jkms.2006.21.3.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho VT, Weller E, Lee SJ, Alyea EP, Antin JH, Soiffer RJ. Prognostic factors for early severe pulmonary complications after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2001;7:223–229. doi: 10.1053/bbmt.2001.v7.pm11349809. [DOI] [PubMed] [Google Scholar]
- 5.Mayaud C, Cadranel J. A persistent challenge: the diagnosis of respiratory disease in the non-AIDS immunocompromised host. Thorax. 2000;55:511–517. doi: 10.1136/thorax.55.6.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forslöw U, Mattson J, Ringden O, Klominek J, Remberger M. Decreasing mortality rate in early pneumonia following hematopoietic stem cell transplantation. Scand J Infect Dis. 2006;38:970–976. doi: 10.1080/00365540600786481. [DOI] [PubMed] [Google Scholar]
- 7.Rañó A, Agustí C, Benito N, Rovira M, Angrill J, Pumarola T. Prognostic factors of non-HIV immunocompromised patients with pulmonary infiltrates. Chest. 2002;122:253–261. doi: 10.1378/chest.122.1.253. [DOI] [PubMed] [Google Scholar]
- 8.Dunagan DP, Baker AM, Hurd DD, Haponik EF. Bronchoscopic evaluation of pulmonary infiltrates following bone marrow transplantation. Chest. 1997;111:135–141. doi: 10.1378/chest.111.1.135. [DOI] [PubMed] [Google Scholar]
- 9.Prasoon J, Sandur S, Meli Y, Arroliga AC, Stoller JK, Mehta AC. Role of flexible bronchoscopy in immunocompromised patients with lung infiltrates. Chest. 2004;125:712–722. doi: 10.1378/chest.125.2.712. [DOI] [PubMed] [Google Scholar]
- 10.Agustí C, Raño A, Rovira M, Filella X, Benito N, Moreno A. Inflammatory response associated with pulmonary complications in non-HIV immunocompromised patients. Thorax. 2004;59:1081–1088. doi: 10.1136/thx.2004.030551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shorr AF, Susla GM, O’Grady NP. Pulmonary infiltrates in the non-HIV-infected immunocompromised patient: etiologies, diagnostic strategies, and outcomes. Chest. 2004;125:260–271. doi: 10.1378/chest.125.1.260. [DOI] [PubMed] [Google Scholar]
- 12.Patel NR, Lee PS, Kim JH, Weinhouse GL, Koziel H. The influence of diagnostic bronchoscopy on clinical outcomes comparing adult autologous and allogeneic bone marrow transplant patients. Chest. 2005;127:1388–1396. doi: 10.1378/chest.127.4.1388. [DOI] [PubMed] [Google Scholar]
- 13.Azoulay E, Schlemmer B. Diagnostic strategy in cancer patients with acute respiratory failure. Intensive Care Med. 2006;32:808–822. doi: 10.1007/s00134-006-0129-2. [DOI] [PubMed] [Google Scholar]
- 14.Azoulay E, Mokart D, Rabbat A, Pene F, Kouatchet A, Bruneel F. Diagnostic bronchoscopy in hematology and oncology patients with acute respiratory failure: prospective multicenter data. Crit Care Med. 2008;36:100–107. doi: 10.1097/01.CCM.0000295590.33145.C4. [DOI] [PubMed] [Google Scholar]
- 15.Hofmeister CC, Czerlanis C, Forsythe C, Stiff PJ. Retrospective utility of bronchoscopy after hematopoietic stem cell transplant. Bone Marrow Transplant. 2006;38:693–698. doi: 10.1038/sj.bmt.1705505. [DOI] [PubMed] [Google Scholar]
- 16.Yoo JH, Lee DG, Choi SM, Choi JH, Park YH, Kim YJ. Infectious complications and outcomes after allogeneic hematopoietic stem cell transplantation in Korea. Bone Marrow Transplant. 2004;34:497–504. doi: 10.1038/sj.bmt.1704636. [DOI] [PubMed] [Google Scholar]
- 17.Azoulay E, Mokart D, Lambert J, Lemiale V, Rabbat A, Kouatchet A. Diagnostic strategy for hematology and oncology patients with acute respiratory failure: randomized controlled trial. Am J Respir Crit Care Med. 2010;182:1038–1046. doi: 10.1164/rccm.201001-0018OC. [DOI] [PubMed] [Google Scholar]
- 18.Coiras MT, Aguilar JC, García ML, Casas I, Pérez-Breña I. Simultaneous detection of fourteen respiratory viruses in clinical specimens by two multiplex reverse transcription nested-PCR assays. J Med Virol. 2004;72:484–495. doi: 10.1002/jmv.20008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aguilar-Guisado M, Jiménez-Jambrina M, Espigado I, Rovira M, Martino R, Oriol A. Pneumonia in allogeneic stem cell transplantation recipients: a multicenter prospective study. Clin Transplant. 2011;25:E629–E638. doi: 10.1111/j.1399-0012.2011.01495.x. [DOI] [PubMed] [Google Scholar]
- 20.De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46:1813–1821. doi: 10.1086/588660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spitzer TR. Engraftment syndrome following hematopoietic stem cell transplantation. Bone Marrow Transplant. 2001;27:893–898. doi: 10.1038/sj.bmt.1703015. [DOI] [PubMed] [Google Scholar]
- 22.Nürnberger W, Willers R, Burdach S, Göbel U. Risk factors for capillary leakage syndrome after bone marrow transplantation. Ann Hematol. 1997;74:221–224. doi: 10.1007/s002770050288. [DOI] [PubMed] [Google Scholar]
- 23.Ljungman P, de la Camara R, Cordonnier C, Einsele H, Engelhard D, Reusser P. Management of CMV, HHV-6, HHV-7 and Kaposi-sarcoma herpesvirus (HHV-8) infections in patients with hematological malignancies and after SCT. Bone Marrow Transplant. 2008;42:227–240. doi: 10.1038/bmt.2008.162. [DOI] [PubMed] [Google Scholar]
- 24.Hosmer D, Lemeshow S. Applied Logistic Regression. Wiley: New York, NY, USA; 1989. [Google Scholar]
- 25.Einsele H, Bertz H, Beyer J, Kiehl MG, Runde V, Kolb HJ. Infectious complications after allogeneic stem cell transplantation: epidemiology and interventional therapy strategies-guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO) Ann Hematol. 2003;82(Suppl 2):S175–S185. doi: 10.1007/s00277-003-0772-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Milano F, Campbell AP, Guthrie KA, Kuypers J, Englund JA, Corey L. Human rhinovirus and coronavirus detection among allogeneic hematopoietic stem cell transplantation recipients. Blood. 2010;115:2088–2094. doi: 10.1182/blood-2009-09-244152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ljungman P, Ward KN, Crooks BN, Parker A, Martino R, Shaw PJ. Respiratory virus infections after stem cell transplantation: a prospective study from the Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Bone Marrow Transplant. 2001;28:479–484. doi: 10.1038/sj.bmt.1703139. [DOI] [PubMed] [Google Scholar]
- 28.Martino R, Porras RP, Rabella N, Williams JV, Rámila E, Margall N. Prospective study of the incidence, clinical features, and outcome of symptomatic upper and lower respiratory tract infections by respiratory viruses in adult recipients of hematopoietic stem cell transplants for hematologic malignancies. Biol Blood Marrow Transplant. 2005;11:781–796. doi: 10.1016/j.bbmt.2005.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luyt CE, Kaiser L. Virus detection in patients with severe pneumonia: still more questions than answers? Am J Respir Crit Care Med. 2012;186:301–302. doi: 10.1164/rccm.201206-1119ED. [DOI] [PubMed] [Google Scholar]
- 30.Mikulska M, Del Bono V, Raiola AM, Bruno B, Gualandi F, Occhini D. Blood stream infections in allogeneic hematopoietic stem cell transplant recipients: reemergence of Gram-negative rods and increasing antibiotic resistance. Biol Blood Marrow Transplant. 2009;15:47–53. doi: 10.1016/j.bbmt.2008.10.024. [DOI] [PubMed] [Google Scholar]
- 31.Morgan J, Wannemuehler KA, Marr KA, Hadley S, Kontoyiannis DP, Walsh TJ. Incidence of invasive aspergillosis following hematopoietic stem cell and solid organ transplantation: interim results of a prospective multicenter surveillance program. Med Mycol. 2005;43(Suppl 1):S49–S58. doi: 10.1080/13693780400020113. [DOI] [PubMed] [Google Scholar]
- 32.Huaringa AJ, Leyva FJ, Signes-Costa J, Morice RC, Raad I, Darwish AA. Bronchoalveolar lavage in the diagnosis of pulmonary complications of bone marrow transplant patients. Bone Marrow Transplant. 2000;25:975–979. doi: 10.1038/sj.bmt.1702335. [DOI] [PubMed] [Google Scholar]
- 33.Shannon VR, Andersson BS, Lei X, Champlin RE, Kontoyiannis DP. Utility of early versus late fiberoptic bronchoscopy in the evaluation of new pulmonary infiltrates following hematopoietic stem cell transplantation. Bone Marrow Transplant. 2010;45:647–655. doi: 10.1038/bmt.2009.203. [DOI] [PubMed] [Google Scholar]
- 34.Shorr AF, Kollef MH. The quick and the dead: the importance of rapid evaluation of infiltrates in the immunocompromised patients. Chest. 2002;122:9–12. doi: 10.1378/chest.122.1.9. [DOI] [PubMed] [Google Scholar]
- 35.Bjorklund A, Aschan J, Labopin M, Remberger M, Ringden O, Winiarski J. Risk factors for fatal infectious complications developing late after allogeneic stem cell transplantation. Bone Marrow Transplant. 2007;40:1055–1062. doi: 10.1038/sj.bmt.1705856. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


