Abstract
Introduction
The dynamics of intimate partner violence (IPV)—one of the world’s leading public health problems—in urban Africa remain poorly understood. Yet, urban areas are key to the future of women’s health in Africa.
Study objectives
We explored survivor-, partner-, and household-level correlates of prevalence rates for types of IPV in urban SSA women.
Method
The study uses DHS data from 42,143 urban women aged 15–49 in 27 SSA countries. Associations at the bivariate level were examined using the Pearson Chi-square test. The modified Poisson regression test estimated the relative prevalence of IPV subtypes in the study population at the multivariate level.
Results
Approximately 36% of women in urban SSA experienced at least one form of IPV; 12.8% experienced two types; and 4.6% experienced all three types. SSA urban women who had only primary-level education, had 3 or more living children, were informally employed, were in polygynous unions, or who approved of wife-beating similarly displayed higher adjusted prevalence rates for all three forms of IPV compared respectively to their counterparts without formal education, without a living child, were unemployed, in monogamous unions, or who do not approve of wife-beating. On the other hand, the region’s urban women who began cohabiting between ages 25 and 35 years or who lived in higher wealth households showed consistently lower adjusted prevalence rates for all three forms of IPV relative to their counterparts who began cohabiting before 18 years or who lived in lower wealth households. Compared to their counterparts without formal education, without a living child, or whose partners did not have formal education, women with secondary and higher education, with 1–2 living children, or whose partners had only primary level schooling displayed higher adjusted prevalence rates for both IPEV and IPPV, but not for IPSV. However, relative to their counterparts whose partners were aged 25 years or below, living with a partner aged 40 years and above was associated with statistically significant reduced prevalence rates for IPPV and IPSV, but not for IPEV. Only for IPPV did women with partners educated at secondary and above levels display statistically significant higher adjusted prevalence rates relative to their counterparts with uneducated partners. Also, solely for IPPV did women who began cohabiting between ages 18 and 24 years or whose partners were employed (whether formally or informally) show decreased adjusted prevalence rates relative to their counterparts who started cohabiting before 18 years or whose partners were unemployed. In addition, only for IPSV did women aged 40 years and above or living in middle wealth households show statistically significant reduced adjusted prevalence rates relative to their counterparts aged less than 25 years or living in lower wealth households.
Discussion and conclusion
By 2030, the majority of SSA women will be urban dwellers. Complexities surround IPV in urban SSA, highlighting the unique dynamics of the problem in this setting. While affirming the link between IPV and marital power inequities and dynamics, findings suggest that the specific correlates of prevalence rates for different IPV sub-types in urban SSA women can, at once, be both similar and unique. The contextual drivers of the differences and similarities in the correlates of the prevalence rates of IPV sub-types among the region’s urban women need further interrogation.
Introduction
Intimate partner violence (IPV) is any behavior, within an intimate relationship, that causes physical, psychological, or sexual harm[1]. It is a leading public health problem and one of the commonest forms of violations experienced by women globally [2]. The implications of IPV are far-reaching, extending beyond women’s physical, emotional, sexual and reproductive health, to encompass their overall well-being, the welfare of their households and communities, and even the economic and social fabric of societies [3]. Among women who suffer intimate partner violence, injuries, visits to health personnel, disabilities and deaths are common [3–5]. Violence corrodes women’s confidence and mental health, hampering their productivity and contribution to development. Abused women often experience emotional distress and tend to consider, attempt, or carry out suicide frequently. They suffer post-traumatic stress syndrome, depression, anxiety, and low self-esteem and other adverse behavioral outcomes such as alcohol and drug abuse, sexual risk-taking, and a higher risk of subsequent victimization [6]. IPV distresses families and communities. It drains household resources, strains family ties, and depresses family members [7,8]. To avoid further violence, abuse and stigma, women survivors of IPV may amend their behaviors to what is acceptable to their aggressors and victimizers, often becoming their own jailers [9].
Although most African countries have assented to many international declarations and developed several national laws that aim to eliminate violence against women, IPV remains widespread in the continent [10,11]. Nearly 40% of ever-partnered women in Africa have experienced physical and/or sexual intimate partner violence at some point in their lives [11]. Urban settings are increasingly critical for efforts to understand and address IPV in Africa. Most of the region is undergoing rapid urban growth under challenging socio-economic conditions. A significant proportion of the future population growth in SSA will occur in urban areas, and by 2050, 50% of the region’s population is expected to be city dwellers [12]. The majority (60%) of residents in SSA’s largest cities—and a swelling proportion of Africans overall—now live in compromised, congested informal settlements, also called slums [13]. The prevalence of IPV against women in SSA is often higher in impoverished urban settlements than in the general urban population[14–16]. Men and boys who live in poor urban communities have also been described as central to the growing epidemic of deadly IPV against women in SSA [17].
With growing realization that the future of global women’s health is urban [18], understanding the dynamics of and tackling IPV in African cities have become both urgent and critical. But while increasing urbanization in the global south may exacerbate women’s exposure to violence and poor health[19–21], the intersections of IPV and urbanization have been ignored or remain poorly studied. Research has associated a variety of socio-economic factors operating at multiple levels (individual, partner, household, and community) with IPV among urban women [15,21–27]. However, these associations are not clear for different IPV subtypes, for different categories of women, and for different countries in the region. Existing IPV studies among urban women in Africa are mainly comparisons of urban and rural areas of Africa [28,29]; focus on the relationship between IPV and health and other outcomes among urban women [7,30], and address poor urban women’s specific risk factors for IPV [31,32]. Few studies explicitly focus the subtypes of IPV among urban women [9]. Even when they do, the bulk of these studies ignore the broader dynamics of IPV within and between countries in SSA and/or use data that is not representative of urban women in the countries and sub-region [9,32,33].
As Africa’s urban population continues to swell, efforts to tackle IPV require robust characterizations of the women at risk for different forms of IPV; grounded analyses of the intersections of factors that expose women to risk; and focused explorations of country- and regional-level dynamics of women’s experiences of IPV forms. The current study is the first major multicounty study of IPV among urban SSA women. It uses comparable, nationally representative data from 27 SSA countries to ask: 1) What are the magnitude and patterns of IPV and its subtypes within and between selected countries in SSA? 2) What factors are associated with the prevalence and experience of IPV subtypes among urban SSA women; and 3) how does the prevalence of IPV subtypes vary within and between countries in SSA? Utilizing a multilevel approach, the study:(a) provides a profile of urban women who experience IPV and its subtypes within and across selected countries in SSA; and (b), tests the central hypothesis that the prevalence of IPV subtypes among urban women differs within and across SSA countries based on survivor-, partner-, and household-level characteristics. The study responds to a growing need for comparative insights on the dynamics of IPV in contexts and spaces that are critical for the future of women’s health, and for evidence to strengthen national, regional and global responses to IPV.
Method
Participants and procedures
The study uses pooled data from 42,143 urban women aged 15–49 years in 27 SSA countries who participated in the most recent Demographic and Health Surveys, Version 6 (DHS-6) or Version 7 (DHS-7) in their countries and completed the Domestic Violence Module of the DHS. The DHS is a nationally representative, population-based, cross-sectional survey sponsored by several governmental agencies, including the United States Agency for International Development (USAID) and administered by ICF International. The DHS collects, describes, and publishes evidence on key demographic and health indicators including HIV, nutrition, violence, livelihoods, sexual and reproductive health, and other indicators (The DHS Program, 2017). It relies on a probability sample of households generated from census frames or, in cases where no census frame exists, from a complete list of villages or communities.
Eligibility for the Domestic Violence Module includes being female, 15–49 years of age, able to complete the survey privately, currently or previously married, and/or living with a male partner. All DHS tools are translated and adapted for each country and then piloted in clusters not selected for inclusion in the survey to assess questionnaire quality (ICF International, 2012). Approximately 2,940 (1.5%) of women that were eligible and agreed to participate in the study countries did not complete the interview due to privacy concerns. The 27 countries and timing of the Demographic and Health Surveys used in the current study are shown in Table 1. Patterns of missingness were examined and found to be minimal (0.01% to 2.8%). The response rate among women completing the Domestic Violence Module stood at 98.2%.
Table 1. Countries, sample sizes, and timing of the DHSs used in the study.
| Countries | Year | Total | Countries | Year | Total |
|---|---|---|---|---|---|
| Angola | 2015–16 | 3,609 | Mali | 2012–13 | 591 |
| Benin | 2017–18 | 1,503 | Mozambique | 2011 | 1387 |
| Burkina Faso | 2010 | 1,927 | Namibia | 2013 | 491 |
| Burundi | 2016–17 | 565 | Nigeria | 2013 | 7,279 |
| Cameroun | 2011 | 1,576 | Rwanda | 2014–15 | 253 |
| Chad | 2014–15 | 215 | Senegal | 2017 | 841 |
| Comoros | 2012 | 652 | Sierra Leone | 2013 | 1,073 |
| Democratic Republic of Congo (DRC) | 2013–14 | 1,439 | South Africa | 2016 | 1,101 |
| Cote d’Ivoire | 2011–12 | 1,704 | Tanzania | 2015–16 | 1,836 |
| Ethiopia | 2016 | 632 | Togo | 2013–14 | 1,743 |
| Gabon | 2012 | 2,555 | Uganda | 2016 | 1,261 |
| Gambia | 2013 | 1,472 | Zambia | 2013–14 | 2,871 |
| Kenya | 2014 | 1,296 | Zimbabwe | 2015 | 1,577 |
| Malawi | 2015–16 | 694 |
Measures and variables
The outcome variables for this study are experiences of any form of IPV, namely physical violence, sexual violence and emotional violence. The DHS asks several different questions to establish if a woman has suffered a form of IPV–physical, sexual and / or emotional violence. Women who are currently or were formerly married or in union, responded to a set of thirteen questions (described in the outcome variables section of Table 2). Responses to the questions were grouped into either physical, sexual or emotional. Each outcome variable was coded ‘0’ when the respondent did not experience it, and ‘1’, when it was reported as having occurred.
Table 2. DHS definition of variables and recodes.
| Variable names | DHS Measurement | Analytical codes |
|---|---|---|
| Individual Variables | Variable measurement | |
| Age | 15–19; 20–24; 25–29; 30–34; 35–39; 40–44; 45–49. | under 25 years; 25–39 years; 40 years + |
| Education | no education; primary; secondary; higher | none; primary; secondary + |
| Occupation | not working; professional/technical/managerial; clerical; sales; agricultural employee; household and domestic; services; skilled manual; unskilled manual; others | none; informal employment; formal employment |
| Age at first cohabitation | single years from age 8 to 49 years | under 18 years; 18–24 years; 25–34 years; 35 years + |
| No. of living children | single digits from 0 to 14 | 0 children; 1–2 children; 3–4 children; 5+ children |
| Approval of wife beating | beating justified if wife goes out without telling husband; beating justified if wife neglects the children; beating justified if wife argues with husband; beating justified if wife refuses to have sex with husband; beating justified if wife burns the food (a positive answer to any of the 5 questions is indicated as a justification for wife -beating). |
not supportive of wife-beating; support wife-beating |
| Spouse/Partner variables | ||
| Age | single years of age from 15 years to 93 years | under 25 years; 25–39 years; 40 years + |
| Education | no education, primary; secondary; higher | ‘none; primary; secondary+ |
| Occupation | not working; professional/technical/managerial; clerical; sales; agricultural employee; household and domestic; services; skilled manual; unskilled manual; others | none; informal employment; formal employment |
| Household variables | ||
| Household wealth | poorest; poorer; middle; richer; richest | low; middle; higher |
| Number of wives | family type: no other wives; other wives from 1 to 9 | one; more than one |
| Outcome variables | ||
| Physical violence | spouse ever pushed, shook or threw something at respondent; spouse ever slapped respondent; spouse ever twisted respondent’s arm or pulled her hair; spouse ever punched respondent with fist or something harmful; spouse ever kicked; dragged or beat up respondent; spouse ever tried to strangle or burn respondent; spouse ever threatened respondent with knife/gun or another weapon; spouse ever attacked respondent with knife/gun or another weapon | yes = experience of at least one of the listed acts of violence No = experience of none of the listed acts of violence |
| Sexual Violence | spouse ever physically forced respondent to have sex when not wanted; spouse ever forced other sexual acts when not wanted by respondent; spouse ever used threats to force sexual acts when not wanted by respondent? | yes = experience of at least one of the listed acts of violence no = experience of none of the listed acts of violence |
| Emotional Violence | spouse ever said or did something to humiliate respondent in front of others; spouse ever threatened to hurt or harm respondent including close relatives; spouse ever insulted or made respondent feel bad | yes = experience of at least one of the listed acts of violence no = experience of none of the listed acts of violence |
Explanatory variables in the study were selected individual-, household- and partner-level socio-economic and demographic factors, including responding women’s age, level of education, employment status, age at first cohabitation, number of children alive and beliefs regarding wife-beating. Other adjusted variables were the age, level of education, and occupation of the responding women’s spouses or partners, the household wealth and union types of the women. Previous studies [8,16,27,34–44] have linked the selected explanatory variables to IPV in a variety of contexts. Operational definitions of all outcome and explanatory variables are presented in Table 2. The ICF International’s institutional review board reviewed and approved the Demographic and Health Surveys (DHS) used in the current study. The surveys were further approved by the national ethics regulatory boards of the different countries in which the studies were implemented. We sought and received formal permission from MEASURE DHS to use the dataset. All DHS datasets are publicly available at https://dhsprogram.com/data/available-datasets.cfm.
Data analysis
Statistical analyses were run at univariate, bivariate and multivariate levels. Estimates of the prevalence of outcomes and explanatory variables are presented at the univariate level and stratified at the individual, household, partner, and country levels. Associations between and levels of significance of explanatory, adjusted and outcome variables were examined at the bivariate level using Pearson Chi-square tests. A multilevel generalized linear model with Poisson distribution measured associations between individual-, household- and partner-level variables and IPV within and between countries. Following the lead of previous studies on IPV [45–47], we relied on the modified Poisson regression approach to estimate the incidence ratio (IRR) and 95% confidence interval (CI) of experiencing IPV. We adjusted for selected variables at the multivariate analysis level using three models. Model I was restricted to associations between selected individual characteristics and outcome variables at both within- and between-country levels. Model II included partner- characteristics and model I. Model III included Model I, Model II as well as household-level variables to assess effect measure modification. The model was fitted using the Hosmer Lemeshow Test. All analyses incorporated sampling weights to account for complex survey design and the unequal probability of selection for each participant in the survey. Standard errors for cluster sampling of the primary sampling units were also adjusted for using svyset commands in Stata. Before results were interpreted, multicollinearity between explanatory variables was assessed through the variance inflation factors (VIF) at a reference value of 5. All study estimates were weighted appropriately using the weights assigned to the domestic module in the DHS dataset. Significance levels were estimated at p<0.05, p<0.01 and p<0.001. Analysis was conducted using STATA 15.1 (StataCorp, 2015).
Results
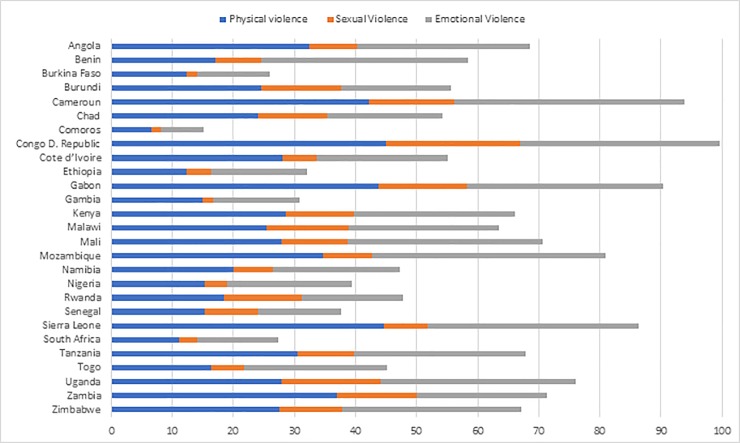
Fig 1 shows prevalence estimates of IPV among currently in-union urban women in the study countries. The proportion of urban women who reported at least one form of IPV ranged from 10.8% in Comoros to 56.3% in DRC. Reports of intimate partner physical violence (IPPV) and intimate partner sexual violence (IPSV) were lowest in Comoros (6.5% and 1.7% respectively) and commonest in DRC (45% and 21.9% respectively). The proportion of women reporting intimate partner emotional violence (IPEV) ranged from 7% in Comoros to 38.3% in Mozambique. While the proportion of women who reported all IPV forms was lowest in Comoros (0.4%), it was highest in DRC (11.1%). Overall, 35.7% of women in urban SSA experienced at least one form of IPV; 12.8% experienced two subtypes; and 4.6% of the women experienced all subtypes. (see also S1 Table).
Fig 1. Prevalence of IPV sub-types among urban women in SSA.
IPPV prevalence rate was lowest among women in the higher wealth category in South Africa (3.4%), and in women aged 40 and above (3.6%) in Comoros. It was highest among women in the lower wealth status in Gabon (55%) and Burundi (51.6%), ranged from 6.9% to 47.9% in women aged 25 to 39 in Comoros and Sierra Leone respectively, and from 3.6% to 44.2% in women aged above 39 years in Comoros and DRC respectively. IPSV was most commonly reported (49.8%) among women in the lowest wealth status in Cote d’ Ivoire and lowest (0.3%) among women aged 40 and above in Comoros; women in the highest wealth category in Gambia (0.4%), and women in formal employment in Ethiopia (0.3%). Prevalence of IPEV was lowest among women in the highest wealth category (3.9%) in Comoros and highest among women in the lowest wealth status in Togo (54.2%) and Cote d’Ivoire (49.8), and among women in informal employment in Cameroun (45.5%) (see S2–S4 Tables).
Bivariate tests of association indicated that while all the explanatory variables of interest were significantly associated with IPPV in Uganda, none was significantly associated with it in Chad and Senegal. In Malawi, Mali, and Sierra Leone, only women’s educational level, women’s occupation, and the number of living children were respectively associated with IPPV. None of the explanatory variables at the bivariate level showed significant association with IPSV in Burkina Faso, Chad, Mali, and Senegal. In Comoros and Sierra Leone respectively, only women’s educational level and women’s approval of wife-beating were significantly associated with IPSV. No association was evident at the bivariate level between the explanatory variables and IPEV in Chad, Mozambique, and Namibia. In Angola, Sierra Leone, and South Africa, only spousal educational level, spousal occupation, and women’s attitude towards wife-beating respectively, were significantly associated with IPEV prevalence. The only variable that was not significantly associated with IPEV prevalence in Burundi was the woman’s age (see S5–S7 Tables).
Intimate partner physical violence (IPPV)
Regression results for IPPV and selected variables, including IRRs and their associated CIs are provided in Table 3. Women’s educational level was positively associated with an increased prevalence rate for IPPV. Compared to women without formal education, women with primary education had a 27% higher adjusted prevalence rate for IPPV. Women with secondary and higher education also had 1.25 times greater adjusted prevalence rate than that of uneducated women (p <0 .001). Informal employment was associated with significantly heightened rates for IPPV. In Model III, women in informal employment had a prevalence rate for IPPV 1.17 times that of unemployed women (p<0.001). Higher ages (18–34) at first cohabitation were associated with decreased prevalence for IPPV. In the adjusted model, women who began cohabitating between ages 18 and 24 experienced a 5% decreased IPPV prevalence rate relative to women who began cohabiting earlier than their 18th birthday. Also, women who began to cohabit between ages 25 and 34 had a 27% lower adjusted IPPV prevalence rate than those who started cohabiting earlier than 18 years.
Table 3. Modified Poisson regression of IPPV on selected characteristics of urban women in sub-Saharan African countries.
| Variables | Model I | Model II | Model III | |||
|---|---|---|---|---|---|---|
| IRR | 95% C. I. | IRR | 95% C. I. | IRR | 95% C. I. | |
| Age—Under 25 years ref | ||||||
| 25–39 years | 0.98 | 0.92–1.05 | 1.03 | 0.97–1.10 | 1.04 | 0.97–1.11 |
| 40 years + | 0.88 | 0.80–0.96** | 0.97 | 0.87–1.07 | 0.98 | 0.88–1.08 |
| Level of Education–None ref | ||||||
| Primary | 1.31 | 1.21–1.41 *** | 1.26 | 1.16–1.36 *** | 1.27 | 1.18–1.38*** |
| Secondary + | 1.22 | 1.12–1.32 *** | 1.21 | 1.11–1.31 *** | 1.25 | 1.15–1.36 *** |
| Employment Status–None ref | ||||||
| Informal | 1.18 | 1.12–1.24 *** | 1.18 | 1.11–1.24 *** | 1.17 | 1.11–1.23 *** |
| Formal | 0.95 | 0.85–1.046 | 0.99 | 0.89–1.11 | 1.01 | 0.90–1.13 |
| Age of Cohabitation—Under 18 years ref | ||||||
| 18–24 years | 0.94 | 0.90–0.98 ** | 0.94 | 0.90–0.99 * | 0.95 | 0.91–1.00* |
| 25–34 years | 0.71 | 0.65–0.78 *** | 0.72 | 0.66–0.79 *** | 0.73 | 0.67–0.80 *** |
| 35 years + | 0.74 | 0.49–01.13 | 0.76 | 0 49–1.17 * | 0.76 | 0.49–1.18 |
| No. of Children Alive– 0 ref | ||||||
| 1–2 children | 1.27 | 1.16–1.40 *** | 1.28 | 1.16–1.41 *** | 1.28 | 1.16–1.41*** |
| 3–4 children | 1.43 | 1.29–1.59 *** | 1.45 | 1.30–1.61 *** | 1.44 | 1.30–1.61*** |
| 5 children + | 1.41 | 1 25–1.58 *** | 1.44 | 1.27–1.62*** | 1.42 | 1.26–1.60 *** |
| Supports Wife beating–No ref | ||||||
| Yes | 1.32 | 1.26–1.39 *** | 1.31 | 1.25–1.38*** | 1.30 | 1.23–1.36*** |
| Partner’s Age—Under 25 years ref | ||||||
| 25–39 years | 0.93 | 0.83–1.04 | 0.93 | 0.84–1.04 | ||
| 40 years + | 0.84 | 0.75–0.95 ** | 0.84 | 0.74–0.94** | ||
| Partner’s Level of Education–None ref | ||||||
| Primary | 1.21 | 1.11–1.30 *** | 1.22 | 1.13–1.32** * | ||
| Secondary + | 1.07 | 0.99–1.16 | 1.09 | 1.01–1.19 * | ||
| Partner’s Employment Status–None ref | ||||||
| Informal | 0.90 | 0.83–0.98* | 0.90 | 0.83–0.98* | ||
| Formal | 0.81 | 0.73–0.89*** | 0.81 | 0.73–0.90*** | ||
| Household Wealth–Lower ref | ||||||
| Middle | 0.95 | 0.88–1.01 | ||||
| Higher | 0.88 | 0.80–0.95** | ||||
| No. of wives–one ref | ||||||
| more than one | 1.14 | 1.08–1.21*** | ||||
| Country | ||||||
| Angola | 0.84 | 0.71–0.99 * | 0.81 | 0.69–0.96** | 0.79 | 0.67–0.93** |
| Benin | 0.48 | 0.39–0.59 *** | 0.47 | 0.39–0.58*** | 0.47 | 0.38–0.57*** |
| Burkina Faso | 0.34 | 0.28–0.42*** | 0.35 | 0.28–0.42*** | 0.36 | 0.29–0.44*** |
| Burundi | 0.64 | 0.53–0.77 *** | 0.61 | 0.50–0.74*** | 0.64 | 0.53–0.77*** |
| Cameroun | 1.06 | 0.93–1.22 | 1.05 | 0.92–1.20 | 1.04 | 0.90–1.19 |
| Chad | 0.60 | 0.45–0.81 *** | 0.62 | 0.46–0.83** | 0.64 | 0.47–0.86** |
| Comoros | 0.20 | 0.15–0.28 *** | 0.20 | 0.15–0.27*** | 0.20 | 0.14–0.27*** |
| DRC ref | --- | --- | --- | --- | --- | --- |
| Cote D’ivoire | 0.77 | 0.65–0.92 ** | 0.79 | 0.67–0.94** | 0.80 | 0.68–0.95** |
| Ethiopia | 0.34 | 0.24–0.46*** | 0.33 | 0.24–0.45*** | 0.34 | 0.25–0.47*** |
| Gabon | 1.16 | 1.01–1.34* | 1.16 | 1.01–1.33* | 1.11 | 0.96–1.28 |
| Gambia | 0.42 | 0.31–0.57*** | 0.44 | 0.32–0.60*** | 0.43 | 0.32–0.59*** |
| Kenya | 0.75 | 0.63–0.89*** | 0.72 | 0.61–0.85*** | 0.72 | 0.61–0.85*** |
| Malawi | 0.71 | 0.53–0.95* | 0.69 | 0.51–0.92* | 0.70 | 0.52–0.94* |
| Mali | 0.71 | 0.58–0.87*** | 0.66 | 0.53–0.82*** | 0.69 | 0.56–0-.86*** |
| Mozambique | 0.95 | 0.81–1.11 | 0.90 | 0.77–1.05 | 0.89 | 0.77–1.05 |
| Namibia | 0.62 | 0.48–0.79*** | 0.60 | 0.47–0.77*** | 0.57 | 0.44–0.73*** |
| Nigeria | 0.42 | 0.35–0.49*** | 0.42 | 0.36–0.49*** | 0.41 | 0.35–0.49*** |
| Rwanda | 0.49 | 0.35–0.68*** | 0.46 | 0.33–0.64*** | 0.48 | 0.34–0.66*** |
| Senegal | 0.43 | 0.33–0.56*** | 0.44 | 0.34–0.57*** | 0.44 | 0.34–0.57*** |
| Sierra Leone | 1.15 | 0.98–1.35 | 1.18 | 1.00–1.39* | 1.21 | 1.03–1.42* |
| South Africa | 0.38 | 0.28–0.50*** | 0.37 | 0.28–0.48*** | 0.35 | 0.27–0.47*** |
| Tanzania | 0.73 | 0.62–0.85*** | 0.68 | 0.58–0.80*** | 0.70 | 0.59–0.82*** |
| Togo | 0.44 | 0.37–0.53*** | 0.43 | 0.36–0.52*** | 0.43 | 0.36–0.52*** |
| Uganda | 0.69 | 0.58–0.82*** | 0.67 | 0.57–0.79*** | 0.66 | 0.56–0.78*** |
| Zambia | 0.93 | 0.81–1.08 | 0.90 | 0.78–1.04 | 0.91 | 0.79–1.05 |
| Zimbabwe | 0.75 | 0.64–0.87*** | 0.73 | 0.63–0.86*** | 0.73 | 0.62–0.86*** |
*p<0.05
**p<0.01
***p<0.001
Having higher numbers of living children was associated with higher IPPV prevalence rates. In the adjusted model, women with 1–2, 3–4, and 5 + living children had 28%, 44%, and 42% respectively higher prevalence rate of IPPV than women without a living child. Women who approve of wife-beating also had 1.30 times higher adjusted IPPV prevalence rate than those who do not and women whose partners were aged 40 years and above had a 16% lower adjusted prevalence rate for IPPV compared to women whose partners were aged less than 25 years. Interestingly, having a partner with only primary education and having a partner with secondary and higher level of education were both independently associated with an increased IPPV rate in Model III. In the adjusted model, the prevalence rate for IPPV among the former women was 1.22 times (p< 0.001), and among the latter group of women, 1.09 times (p<0.05) greater than women whose partners had no formal education. In the same model, partners’ employment status was also significantly associated with rates for IPPV among women: respondents whose partners were in informal employment and those whose partners were in formal employment respectively had 10% and 19% decreased IPPV prevalence rates compared to women with unemployed partners. While higher household wealth was associated with a decreased adjusted prevalence rate (IRR: 0.88; p:< 0.001) for IPPV, women in polygynous households reported IPPV 14% times more than women in monogamous unions.
In Model I, women in Cameroun, Sierra Leone and Gabon had higher IPPV prevalence rates compared to women in DRC. However, this was only significant in Gabon. In Model II, the reduced IPPV prevalence rates among urban women in the region relative to the DRC counterparts remained generally stable, becoming statistically significant in Sierra Leone and Gabon, but slightly attenuating in significance in Chad. In Model III, the IPPV prevalence rate patterns among urban women in the region relative to their counterparts in DRC were also largely retained, though women in Gabon lost some of their comparative advantages relative to their DRC counterparts.
Intimate partner sexual violence (IPSV)
Table 4 shows the prevalence rates for IPSV and associated IRRs and CIs. Women aged 40 years and above had a 22% lower adjusted prevalence rate for IPSV compared to their counterparts aged less than 25 years. On the other hand, women with only primary-level education and women in informal employment showed higher adjusted IPSV prevalence rates relative to their uneducated and unemployed counterparts respectively. IPSV prevalence rate was also higher among women with 3 and more living children than in their counterparts with no living child. Compared to those without a living child, women with 3–4 and 5 + living children had 35% and 30% higher prevalence rate respectively for IPSV. Women who approve of wife-beating also had a 63% higher adjusted prevalence rate for IPSV than those who do not. And relative to their counterparts who started cohabiting earlier than their 18th birthday, women who began cohabiting between their 25th and 34th birthdays had a 32% diminished adjusted IPSV prevalence rate.
Table 4. Modified Poisson regression of IPSV on selected characteristics of urban women in sub-Saharan African countries.
| Variables | Model I | Model II | Model III | |||
|---|---|---|---|---|---|---|
| IRR | 95% C. I. | IRR | 95% C. I. | IRR | 95% C. I. | |
| Age—Under 25 years ref | ||||||
| 25–39 years | 0.89 | 0.78–1.01 | 0.94 | 0.82–1.08 | 0.96 | 0.84–1.10 |
| 40 years + | 0.66 | 0.55–0.80*** | 0.76 | 0.61–0.94** | 0.78 | 0.63–0.96* |
| Level of Education–None ref | ||||||
| Primary | 1.31 | 1.13–1.53*** | 1.28 | 1.09–1.52** | 1.33 | 1.12–1.57*** |
| Secondary + | 1.11 | 0.95–1.30 | 1.11 | 0.92–1.33 | 1.20 | 0.99–1.45 |
| Employment Status–None ref | ||||||
| Informal | 1.31 | 1.18–1.44*** | 1.31 | 1.19–1.45*** | 1.30 | 1.17–1.43*** |
| Formal | 0.99 | 0.80–1.23 | 1.02 | 0.82–1.26 | 1.04 | 0.84–1.29 |
| Age of Cohabitation—Under 18 years ref | ||||||
| 18–24 years | 0.93 | 0.84–1.03 | 0.94 | 0.85–1.03 | 0.95 | 0.86–1.05 |
| 25–34 years | 0.66 | 0.55–0.80*** | 0.67 | 0.56–0.81 | 0.68 | 0.57–0.83*** |
| 35 years + | 1.45 | 0.86–2.46 | 1.49 | 0.87–2.54 | 1.50 | 0.87–2.57 |
| No. of Children Alive– 0 ref | ||||||
| 1–2 children | 1.15 | 0.97–1.36 | 1.16 | 0.98–1.38 | 1.16 | 0.98–1.38 |
| 3–4 children | 1.33 | 1.10–1.60** | 1.36 | 1.13–1.64*** | 1.35 | 1.11–1.63** |
| 5 children + | 1.27 | 1.03–1.58* | 1.33 | 1.07–1.66** | 1.30 | 1.05–1.62* |
| Supports Wife beating–No ref | ||||||
| Yes | 1.67 | 1.52–1.85*** | 1.66 | 1.50–1.84*** | 1.63 | 1.47–1.80*** |
| Partner’s Age—Under 25 years ref | ||||||
| 25–39 years | 0.89 | 0.74–1.07 | 0.90 | 0.99–1.35 | ||
| 40 years + | 0.76 | 0.61–0.95* | 0.76 | 0.61–0.95* | ||
| Partner’s Level of Education–None ref | ||||||
| Primary | 1.13 | 0.96–1.32 | 1.15 | 0.99–1.35 | ||
| Secondary + | 1.01 | 0.85–1.19 | 1.06 | 0.90–1.25 | ||
| Partner’s Employment Status–None ref | ||||||
| Informal | 0.91 | 0.77–1.08 | 0.91 | 0.72–0.94 | ||
| Formal | 0.89 | 0.72–1.10 | 0.91 | 0.73–0.84 | ||
| Household Wealth–Lower ref | ||||||
| Middle | 0.82 | 0.72–0.94** | ||||
| Higher | 0.71 | 0.61–0.84*** | ||||
| No. of wives–one ref | ||||||
| more than one | 1.21 | 1.08–1.35*** | ||||
| Country | ||||||
| Angola | 0.46 | 0.35–0.60*** | 0.44 | 0.33–0.58*** | 0.42 | 0.32–0.55*** |
| Benin | 0.46 | 0.34–0.63*** | 0.45 | 0.33–0.61*** | 0.44 | 0.32–0.59*** |
| Burkina Faso | 0.10 | 0.06–0.17*** | 0.10 | 0.06–0.17*** | 0.11 | 0.06–0.18*** |
| Burundi | 0.74 | 0.55–0.99* | 0.70 | 0.52–0.94** | 0.77 | 0.57–1.04 |
| Cameroun | 0.75 | 0.59–0.95* | 0.74 | 0.58–0.94* | 0.74 | 0.58–0.94* |
| Chad | 0.57 | 0.35–0.95* | 0.58 | 0.35–0.97* | 0.63 | 0.37–1.04 |
| Comoros | 0.12 | 0.06–0.23*** | 0.12 | 0.06–0.23*** | 0.11 | 0.06–0.21*** |
| DRC ref | --- | --- | --- | --- | --- | --- |
| Cote d’Ivoire | 0.31 | 0.21–0.46*** | 0.31 | 0.21–0.46*** | 0.33 | 0.22–0.49*** |
| Ethiopia | 0.24 | 0.13–0.44*** | 0.23 | 0.12–0.42*** | 0.25 | 0.14–0.47*** |
| Gabon | 0.83 | 0.63–1.08 | 0.82 | 0.63–1.07 | 0.74 | 0.57–0.97* |
| Gambia | 0.10 | 0.06–0.17*** | 0.10 | 0.06–0.18*** | 0.10 | 0.06–0.17*** |
| Kenya | 0.64 | 0.47–0.86** | 0.61 | 0.45–0.83** | 0.61 | 0.45–0.82*** |
| Malawi | 0.91 | 0.65–1.26 | 0.87 | 0.63–1.21 | 0.91 | 0.66–1.25 |
| Mali | 0.56 | 0.39–0.80*** | 0.53 | 0.35–0.63*** | 0.58 | 0.39–0.87** |
| Mozambique | 0.50 | 0.38–0.67*** | 0.47 | 0.35–0.63*** | 0.47 | 0.35–0.63*** |
| Namibia | 0.46 | 0.30–0.71*** | 0.44 | 0.29–0.68*** | 0.40 | 0.26–0.62*** |
| Nigeria | 0.22 | 0.17–0.30*** | 0.22 | 0.17–0.30*** | 0.22 | 0.16–0.30*** |
| Rwanda | 0.76 | 0.43–1.35 | 0.71 | 0.39–1.28 | 0.76 | 0.42–1.37 |
| Senegal | 0.54 | 0.37–0.79** | 0.54 | 0.37–0.81** | 0.55 | 0.37–0.81** |
| Sierra Leone | 0.38 | 0.25–0.59*** | 0.39 | 0.25–0.60*** | 0.41 | 0.28–0.63*** |
| South Africa | 0.27 | 0.14–0.51*** | 0.26 | 0.14–0.49*** | 0.24 | 0.13–0.45*** |
| Tanzania | 0.46 | 0.35–0.59*** | 0.43 | 0.33–0.56*** | 0.45 | 0.35–0.59*** |
| Togo | 0.33 | 0.25–0.46*** | 0.33 | 0.24–0.45*** | 0.34 | 0.25–0.46*** |
| Uganda | 0.87 | 0.68–1.12 | 0.84 | 0.65–1.08 | 0.82 | 0.64–1.05 |
| Zambia | 0.73 | 0.58–0.92** | 0.71 | 0.56–0.90** | 0.72 | 0.57–0.92** |
| Zimbabwe | 0.68 | 0.53–0.87** | 0.67 | 0.52–0.86** | 0.67 | 0.52–0.86** |
*p<0.05
**p<0.01
***p<0.001
The prevalence of IPSV was lower in women whose partners were aged 40 years and above than in women whose partners were aged less than 25 years. The former group women had a 24% lower adjusted prevalence of IPSV compared to the latter. Women in middle and in higher wealth households also had decreased IPSV prevalence rates (IRR: 0.82, p<0.01; and IRR: 0.77, p<0.001) respectively) compared to their counterparts in lower wealth households. However, being in a polygynous union increased IPSV prevalence rate in women by 21% compared to living in monogamous households.
In Model I, urban women in the region generally showed significantly reduced prevalence rates of IPSV compared to their counterparts in DRC, except in Gabon, Malawi, Rwanda, and Uganda. In Model II, while IPSV prevalence rates remained significantly stable across the countries, Burundian women displayed a sturdier reduced IPSV prevalence rate compared to their DRC counterparts. In Model III, with the exceptions of Burkina Faso, Burundi and Chad, the region’s urban women generally retained their statistically significant reduced IPSV prevalence rates compared to their counterparts in DRC.
Intimate partner emotional violence (IPEV)
Table 5 shows regression results for IPEV prevalence rates and selected variables. Controlling for all variables, women with only primary-level education or with secondary and above levels of education respectively had 25% or 28% higher IPEV prevalence rates than their uneducated counterparts. The higher prevalence rate for IPEV among women in informal employment, compared to their unemployed counterparts, found in Models I (IRR: 1.17, p <0.001) and II (IRR: 1.16, p <0.001) remained significant in Model III (IRR: 1.15, p <0.001). Across the models, women who began cohabiting between their 25th and 34th birthdays retained consistently decreased prevalence rates for IPEV relative to those who began cohabiting earlier than their 18th birthday. In Models I, II and III, the former group of women had 19%, 18% and 18% decreased prevalence rate for IPEV compared to the latter group. Numbers of living child were associated with increased IPEV prevalence rates: women with 1–2, 3–4, and 5 + living children had 27%, 46%, and 43% respectively higher adjusted prevalence rate of IPPV than women without a living child. Also, the higher prevalence rates for IPEV among women who approve of wife-beating, compared to their counterparts who do not, found in Models I (IRR: 1.29, p <0.001) and II (IRR: 1.28, p <0.001) remained statistically significant, diminishing only slightly in the full model (IRR: 1.26, p <0.001). On the other hand, the higher IPEV prevalence rate among women whose partners had only primary-level education relative to women with uneducated partners rose from 19% in Model II to 21% in Model III. Further, while women in higher wealth households showed decreased adjusted IPEV prevalence rates (IRR: 0.86, p<0.001) relative to their counterparts from lower wealth households, being in polygynous unions amplified women’s IPEV prevalence rate by 14% compared to their monogamous counterparts.
Table 5. Modified Poisson regression of IPEV on selected characteristics of urban women in sub-Saharan African countries.
| Variables | Model I | Model II | Model III | |||
|---|---|---|---|---|---|---|
| IRR | 95% C. I. | IRR | 95% C. I. | IRR | 95% C. I. | |
| Age-Under 25 years ref | ||||||
| 25–39 years | 1.03 | 0.96–1.10 | 1.04 | 0.97–1.12 | 1.05 | 0.98–1.12 |
| 40 years+ | 0.97 | 0.88–1.06 | 0.98 | 0.89–1.09 | 0.99 | 0.90–1.10 |
| Level of education–None ref | ||||||
| Primary education | 1.27 | 1.18–1.38*** | 1.23 | 1.14–1.34*** | 1.25 | 1.16–1.36*** |
| Secondary + | 1.23 | 1.13–1.33*** | 1.23 | 1.13–1.34*** | 1.28 | 1.17–1.40*** |
| Employment status- None ref | ||||||
| Informal | 1.17 | 1.10–1.24*** | 1.16 | 1.10–1.23*** | 1.15 | 1.09–1.22*** |
| Formal | 1.03 | 0.92–1.14 | 1.05 | 0.94–1.18 | 1.07 | 0.95–1.19 |
| Age of Cohabitation—Under 18 years ref | ||||||
| 18–24 years | 0.99 | 0.94–1.04 | 0.99 | 0.95–1.04 | 1.00 | 0.95–1.05 |
| 25–34 years | 0.81 | 0.74–0.89*** | 0.82 | 0.75–0.89*** | 0.82 | 0.76–0.90*** |
| 35 years + | 0.79 | 0.53–1.17 | 0.80 | 0.53–1.19 | 0.80 | 0.53–1.20 |
| No. of Children Alive– 0 ref | ||||||
| 1–2 children | 1.27 | 1.15–1.40*** | 1.27 | 1.15–1.40*** | 1.27 | 1.15–1.40*** |
| 3–4 children | 1.47 | 1.32–1.64*** | 1.47 | 1.31–1.64*** | 1.46 | 1.31–1.63*** |
| 5 children + | 1.46 | 1.30–1.65*** | 1.45 | 1.28–1.64*** | 1.43 | 1.27–1.62*** |
| Supports Wife beating–No ref | ||||||
| Yes | 1.29 | 1.22–1.36*** | 1.28 | 1.21–1.35*** | 1.26 | 1.20–1.33*** |
| Partner’s Age—Under 25 years ref | ||||||
| 25–39 years | 0.96 | 0.85–1.08 | 0.96 | 0.85–1.08 | ||
| 40 years + | 0.95 | 0.84–1.09 | 0.95 | 0.83–1.08 | ||
| Partner’s Level of Education–None ref | ||||||
| Primary | 1.19 | 1.09–1.29*** | 1.21 | 1.11–1.31*** | ||
| Secondary + | 1.04 | 0.96–1.14 | 1.08 | 0.99–1.18 | ||
| Partner’s Employment Status–None ref | ||||||
| Informal | 0.96 | 0.87–1.06 | 0.96 | 0.87–1.06 | ||
| Formal | 0.89 | 0.80–1.00 | 0.90 | 0.81–1.01 | ||
| Household Wealth–Lower ref | ||||||
| Middle | 0.94 | 0.86–1.02 | ||||
| Higher | 0.86 | 0.79–0.94*** | ||||
| No. of wives–one ref | ||||||
| more than one | 1.14 | 1.07–1.22*** | ||||
| Country | ||||||
| Angola | 0.98 | 0.81–1.19 | 0.97 | 0.80–1.18 | 0.94 | 0.77–1.25 |
| Benin | 1.28 | 1.09–1.49*** | 1.26 | 1.08–1.48*** | 1.33 | 1.06–1.46** |
| Burkina Faso | 0.44 | 0.35–0.57*** | 0.44 | 0.35–0.57*** | 0.46 | 0.36–0.59*** |
| Burundi | 0.63 | 0.51–0.77*** | 0.60 | 0.49–0.74*** | 0.63 | 0.51–0.78*** |
| Cameroun | 1.29 | 1.13–1.49*** | 1.27 | 1.10–1.46*** | 1.25 | 1.08–1.44** |
| Chad | 0.66 | 0.47–0.94* | 0.67 | 0.47–0.95* | 0.69 | 0.49–0.98* |
| Comoros | 0.29 | 0.22–0.38*** | 0.28 | 0.22–0.37*** | 0.28 | 0.21–0.36*** |
| DRC ref | --- | --- | --- | --- | --- | --- |
| Cote d’Ivoire | 0.80 | 0.65–0.98* | 0.80 | 0.65–0.99* | 0.81 | 0.66–1.00* |
| Ethiopia | 0.59 | 0.44–0.76*** | 0.56 | 0.43–0.74*** | 0.59 | 0.45–0.78*** |
| Gabon | 1.13 | 0.96–1.34 | 1.13 | 0.95–1.33 | 1.07 | 0.90–1.27 |
| Gambia | 0.54 | 0.40–0.71*** | 0.54 | 0.41–0.72*** | 0.54 | 0.40–0.71*** |
| Kenya | 0.92 | 0.78–1.10 | 0.89 | 0.75–1.06 | 0.89 | 0.75–1.06 |
| Malawi | 0.93 | 0.71–1.19 | 0.90 | 0.70–1.17 | 0.92 | 0.71–1.20 |
| Mali | 1.14 | 0.90–1.43 | 1.10 | 0.85–1.41 | 1.15 | 0.90–1.48 |
| Mozambique | 1.45 | 1.24–1.69*** | 1.38 | 1.18–1.62*** | 1.38 | 1.18–1.61*** |
| Namibia | 0.82 | 0.65–1.04 | 0.80 | 0.64–1.02 | 0.76 | 0.60–0.97* |
| Nigeria | 0.74 | 0.62–0.87*** | 0.73 | 0.61–0.87*** | 0.72 | 0.60–0.86*** |
| Rwanda | 0.58 | 0.43–0.79*** | 0.55 | 0.40–0.74*** | 0.57 | 0.42–0.78*** |
| Senegal | 0.52 | 0.39–0.69*** | 0.52 | 0.39–0.69*** | 0.51 | 0.38-.69*** |
| Sierra Leone | 1.21 | 1.01–1.46* | 1.23 | 1.02–1.48* | 1.26 | 1.05–1.52** |
| South Africa | 0.58 | 0.45–0.74*** | 0.56 | 0.44–0.73*** | 0.54 | 0.42–0.70*** |
| Tanzania | 0.92 | 0.77–1.10 | 0.86 | 0.72–1.03 | 0.89 | 0.74–1.06 |
| Togo | 0.85 | 0.70–1.03 | 0.83 | 0.69–1.01 | 0.84 | 0.69–1.01 |
| Uganda | 1.08 | 0.91–1.249 | 1.05 | 0.88–1.25 | 1.03 | 0.87–1.23 |
| Zambia | 0.73 | 0.62–0.86*** | 0.71 | 0.61–0.84*** | 0.72 | 0.61–0.85*** |
| Zimbabwe | 1.06 | 0.90–1.23 | 1.04 | 0.89–1.22 | 1.04 | 0.89–1.22 |
*p<0.05
**p<0.01
***p<0.001
In Model I, only in Benin, Cameroun, Gabon, Mozambique, and Sierra Leone did urban women display statistically significant higher IPEV prevalence rates compared to their DRC counterparts. In the same model, urban women in 12 of the countries (Burkina Faso, Burundi, Chad, Comoros, Cote d’Ivoire, Ethiopia, Gambia, Nigeria, Rwanda, Senegal, South Africa and Zambia) had significantly decreased IPEV prevalence rates compared to their counterparts in DRC. These patterns were largely retained in Models II and III. However, it was only in Model III that Namibian women joined the bulk of the region’s women to experience a statistically significant reduced IPEV prevalence rate (IRR:0.76, p<0.05) relative to their DRC counterparts.
Discussion
This paper is arguably the first truly regional exploration of prevalence rates for IPV subtypes among urban women across SSA. By focusing on IPV subtypes and their particular correlates in urban women across 27 countries in SSA, the study constitutes a major shift from research that treats IPV as an invariable phenomenon or focuses only on a few of its forms in few African contexts [5,32,33,48]. Some notable patterns and findings emerge from the study. Descriptive findings showed critical patterns in the extent, magnitude and correlates of IPV forms in different countries and among diverse groups of women in SSA. In general, urban IPV rates among urban women in the countries we studied closely mirror prevalence rates of IPV globally, nationally and regionally. Globally, over a third (35%) of women have experienced physical and/or sexual violence by a partner or non-partner. A WHO study showed that the global lifetime prevalence of IPV among ever-partnered women for Africa was nearly 40% [11]. In Nigeria, estimates put the prevalence of IPV at 31% to 61% for psychological/emotional violence, 20% to 31% for sexual violence, and 7% to 31% for physical violence [49]. While IPPV has been the focus of many studies, the current research shows that IPEV and IPSV are also common in urban areas in SSA. The low report for IPSV should, however, be interpreted with caution. IPSV remains a taboo topic in many African contexts. As a result, few survivors feel comfortable to report it in surveys [50].
With regards to IPV in urban SSA, Comorian women were safest while women in DRC were the least unsafe. The proportion of urban women in SSA who report IPV is significantly high in conflict and post-conflict states such as DRC, Uganda, and Sierra Leone. Conflict and post-conflict situations increase women’s risk for violence within and outside unions [47,51–55]. Social protection mechanisms deteriorate at multiple levels during conflicts, intensifying the conditions and circumstances that expose women to risks for violence [40,56].
Our findings indicate the unique dynamics of IPV in urban SSA. To illustrate, only five correlates—having only primary-level education, having 3 or more living children, being informally employed, being in polygynous unions, or supporting wife-beating—were commonly associated with higher adjusted prevalence rates for all three forms of IPV. Conversely, two variables–starting to cohabit between ages 25 and 35 years or living in higher wealth households showed consistently lower adjusted prevalence rates for all three forms of IPV. Relative to their counterparts without formal education, without a living child, or whose partners did not have formal education, women with secondary and higher education, with 1–2 living children, or whose partners had only primary level schooling exhibited higher adjusted prevalence rates for both IPEV and IPPV, but not for IPSV. Also, in comparison with their counterparts whose partners were aged 25 years or below, living with a partner aged 40 years and above was statistically associated with reduced prevalence rates for IPPV and IPSV, but not for IPEV. Only for IPPV did women with partners educated at secondary and above levels display statistically significant higher adjusted prevalence rates relative to their counterparts with uneducated partners. Only for IPPV too did women who began cohabiting between ages 18 and 24 years or whose partners were employed (whether formally or informally) show decreased adjusted prevalence rates relative to their counterparts who started cohabiting before 18 years or whose partners were unemployed. However, it was only for IPSV that women aged 40 years and above or living in middle wealth households showed statistically significant reduced adjusted prevalence rates relative to their counterparts aged less than 25 years or living in lower wealth households.
Many of these findings challenge existing studies, raising the need for multifaceted interventions that respond to the unique complexities of IPV and its subtypes in the region’s urban contexts. For instance, research suggests that men with higher educational attainment have more equitable attitudes and practices towards women and may be less violent to their marital partners [57]. Our study suggested otherwise, at least for IPPV. These inconsistencies also imply that there may be other variables operating at the partner- and household-level characteristics that need further exploration. There is, for example, ample evidence that substance and alcohol abuse by male partners can exacerbate violence in the household [58–62].
Among the critical findings in this study is the link between IPV, gender dynamics, and marital power inequities. IPV is often used to maintain and assert power by men [39,63,64]. Situations that diminish men’s sense of control over their female partners can exacerbate their use of violence to affirm control and power [65,66]. Threats to men’s feelings of power in intimate relationships can emerge from diverse sources, including the stresses and disruptions associated with conflicts and post-conflict situations [40,55]. There is evidence that some men may find economically independent and educated female partners threatening. IPV can be part of such threatened men’s strategies to enforce control over female partners [67]. Further, while education can facilitate woman’s recognition and reporting of IPV generally, it can also increase women’s risk for IPV. Educated women may threaten men’s sense of themselves as household heads, decision-makers and breadwinners, especially if such men subscribe to traditional masculine norms regarding the role and authority of men in the household [68]. Also, while previous research shows that economically dependent women are particularly at risk of IPV [69,70], there is also evidence that such women may resort to relationship practices that shield them from violence. Such strategies may include non-confrontation, subservience, and other conflict avoidance strategies [71].
The implications of marital power inequities for IPV in urban SSA are also evident in the positive associations between polygyny and all IPV forms. Polygyny is related to and can boost gender inequities that could promote IPV. Violence toward women can be potentiated by polygyny which often goes together and, in combination with women’s low economic power, low educational attainment, and weak decision-making power. Polygyny enhances male control over women in ways that allow and encourage violence and suppression of rights and liberties of women and girls [72,73]. Additionally, urban women who approved of wife-beating had a significantly elevated prevalence of all forms of IPV relative to their counterparts who did not. Women who approve of wife-beating in unions tend to be poorer, adolescents, or marry early. They are also often powerless and marginalized in their unions, showing inadequate capacity to safely challenge their partners and prevent their abuse or violation. One study in Kenya showed that 36% of girls married before 18 believed that a man is sometimes justified in beating his wife, compared to 20 percent of those who married later [74]. Early ages at cohabitation were associated with increased prevalence rates for IPV. Women who started to cohabit between ages 25 and 35 years had much lower adjusted prevalence rates for all three forms of IPV relative to their counterparts who began to cohabit before age 18. Doku and Asante [75] write that early marriage exacerbates power inequities in unions, putting the woman at extended risks for IPV. Girls who marry before 18 are more likely to experience domestic violence than their peers who marry later. In Peru, where more than half of women report physical or sexual violence, early age at marriage aggravated women’s risk for IPV [76].
The elevated prevalence rates for all IPV forms among women with higher numbers of living children is another critical finding. Large families can be a source of enormous pressure and frustrations that can strain unions and precipitate violence. Research shows that the cost of children is rising in SSA at a time of widespread inflation, unemployment, and growing cost of living [77]. Years of structural adjustment, poor development planning, and decline of public protection and social services have shrunk livelihood opportunities for many urban SSA families, systematically depleting their ability to maintain a decent living and resulting in hardship, poverty and deterioration in the quality of life [13]. These trends have potential to create tensions that can promote IPV [77,78]. Scholars have noted the systematic erosion of the advantages which urban areas have historically enjoyed over rural areas in Africa in terms of livelihood opportunities, social protection, health access to services, and disconnection from traditional gender norms[79–81].
Conclusion
In just a decade, the majority of SSA women will be urban dwellers. IPV remains a common public health problem and one of the most prevalent forms of violations of women's human rights globally [4,7]. Efforts to address IPV in Africa must include a strong focus on urban areas. The current multi-country study sought to understand the broader dynamics of IPV and its forms in urban SSA using representative data on urban women in the sub-region. The study showed that the prevalence of IPV is highest in conflict and post-conflict states such as DRC and Sierra Leone. It also highlights the complexities and varying influences on IPV subtypes in urban SSA. The factors associated with urban African women’s exposure to different IPV subtypes can be both similar and unique at the same time. Future research should explore the contextual and community-level factors (such as gender norms) that may be associated with IPV against urban women in Africa, as documented in previous research [82]. This study used a cross-sectional dataset and was unable to track trends and changes over time with respect to IPV forms and their correlates in SSA. This limitation notwithstanding, the study reveals some important dynamics, correlates and complexities surrounding IPV in contemporary urban SSA.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The study was supported by the International Development Center Center (IDRC) grant # IDRC-19-2287 to COI. The funder did not also have role in the study design; collection, analysis, and interpretation of data; writing of the paper; and/or decision to submit for publication.
References
- 1.World Health Organization. Understanding and addressing violence against women: Intimate partner violence. World Health Organization; 2012. [Google Scholar]
- 2.Shamu S, Abrahams N, Temmerman M, Musekiwa A, Zarowsky C. A systematic review of African studies on intimate partner violence against pregnant women: prevalence and risk factors. PloS One. 2011;6: e17591 10.1371/journal.pone.0017591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Osinde MO, Kaye DK, Kakaire O. Intimate partner violence among women with HIV infection in rural Uganda: critical implications for policy and practice. BMC Womens Health. 2011;11: 50 10.1186/1472-6874-11-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. The lancet. 2006;368: 1260–1269. [DOI] [PubMed] [Google Scholar]
- 5.Groves AK, Kagee A, Maman S, Moodley D, Rouse P. Associations between intimate partner violence and emotional distress among pregnant women in Durban, South Africa. J Interpers Violence. 2012;27: 1341–1356. 10.1177/0886260511425247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Niaz U. Women’s mental health in Pakistan. World Psychiatry. 2004;3: 60 [PMC free article] [PubMed] [Google Scholar]
- 7.Ellsberg M, Jansen HA, Heise L, Watts CH, Garcia-Moreno C. Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study. The Lancet. 2008;371: 1165–1172. [DOI] [PubMed] [Google Scholar]
- 8.Selin A, DeLong SM, Julien A, MacPhail C, Twine R, Hughes JP, et al. Prevalence and associations, by age group, of IPV among AGYW in rural South Africa. Sage Open. 2019;9: 2158244019830016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gibbs A, Dunkle K, Jewkes R. Emotional and economic intimate partner violence as key drivers of depression and suicidal ideation: A cross-sectional study among young women in informal settlements in South Africa. PloS One. 2018;13: e0194885 10.1371/journal.pone.0194885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCloskey LA, Boonzaier F, Steinbrenner SY, Hunter T. Determinants of intimate partner violence in sub-Saharan Africa: a review of prevention and intervention programs. Partn Abuse. 2016;7: 277–315. [Google Scholar]
- 11.World Health Organization. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. World Health Organization; 2013. [Google Scholar]
- 12.Dos Santos S, Adams E, Neville G, Wada Y, De Sherbinin A, Bernhardt EM, et al. Urban growth and water access in sub-Saharan Africa: Progress, challenges, and emerging research directions. Sci Total Environ. 2017;607: 497–508. 10.1016/j.scitotenv.2017.06.157 [DOI] [PubMed] [Google Scholar]
- 13.Davis M. Planet of slums. Open House Int. 8: 5. [Google Scholar]
- 14.Gage AJ. Women’s experience of intimate partner violence in Haiti. Soc Sci Med. 2005;61: 343–364. 10.1016/j.socscimed.2004.11.078 [DOI] [PubMed] [Google Scholar]
- 15.Gibbs A, Jewkes R, Willan S, Washington L. Associations between poverty, mental health and substance use, gender power, and intimate partner violence amongst young (18–30) women and men in urban informal settlements in South Africa: A cross-sectional study and structural equation model. PLoS One. 2018;13: e0204956 10.1371/journal.pone.0204956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gibbs A, Dunkle K, Jewkes R. Emotional and economic intimate partner violence as key drivers of depression and suicidal ideation: A cross-sectional study among young women in informal settlements in South Africa. PloS One. 2018;13: e0194885 10.1371/journal.pone.0194885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kruijt D, Koonings K. The rise of megacities and the urbanization of informality, exclusion and violence. Kees Koonings Dirk Kruijt Mega-Cities Polit Urban Exclusion Violence Glob South Lond Zed Books. 2009. [Google Scholar]
- 18.Turshen M. African women’s health. Africa World Press; 2000. [Google Scholar]
- 19.Oshiro A, Poudyal AK, Poudel KC, Jimba M, Hokama T. Intimate partner violence among general and urban poor populations in Kathmandu, Nepal. J Interpers Violence. 2011;26: 2073–2092. 10.1177/0886260510372944 [DOI] [PubMed] [Google Scholar]
- 20.Sambisa W, Angeles G, Lance PM, Naved RT, Curtis SL. Physical and sexual abuse of wives in urban Bangladesh: husbands’ reports. Stud Fam Plann. 2010;41: 165–178. 10.1111/j.1728-4465.2010.00241.x [DOI] [PubMed] [Google Scholar]
- 21.Decker MR, Peitzmeier S, Olumide A, Acharya R, Ojengbede O, Covarrubias L, et al. Prevalence and health impact of intimate partner violence and non-partner sexual violence among female adolescents aged 15–19 years in vulnerable urban environments: a multi-country study. J Adolesc Health. 2014;55: S58–S67. 10.1016/j.jadohealth.2014.08.022 [DOI] [PubMed] [Google Scholar]
- 22.Dim EE. Differentials and Predictors of IPV against Nigerian Women in Rural and Urban Areas. J Aggress Maltreatment Trauma. 2019; 1–23. [Google Scholar]
- 23.Machisa MT, Christofides N, Jewkes R. Structural pathways between child abuse, poor mental health outcomes and male-perpetrated intimate partner violence (IPV). PloS One. 2016;11: e0150986 10.1371/journal.pone.0150986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abrahams N, Jewkes R, Hoffman M, Laubsher R. Sexual violence against intimate partners in Cape Town: prevalence and risk factors reported by men. Bull World Health Organ. 2004;82: 330–337. [PMC free article] [PubMed] [Google Scholar]
- 25.Ellsberg M, Jansen HA, Heise L, Watts CH, Garcia-Moreno C. Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study. The Lancet. 2008;371: 1165–1172. [DOI] [PubMed] [Google Scholar]
- 26.Gibbs A, Dunkle K, Jewkes R. Emotional and economic intimate partner violence as key drivers of depression and suicidal ideation: A cross-sectional study among young women in informal settlements in South Africa. PloS One. 2018;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klomegah RY. Intimate partner violence (IPV) in Zambia: An examination of risk factors and gender perceptions. J Comp Fam Stud. 2008;39: 557–569. [Google Scholar]
- 28.Dim EE. Differentials and Predictors of IPV against Nigerian Women in Rural and Urban Areas. J Aggress Maltreatment Trauma. 2019; 1–23. [Google Scholar]
- 29.Klomegah RY. Intimate partner violence (IPV) in Zambia: An examination of risk factors and gender perceptions. J Comp Fam Stud. 2008;39: 557–569. [Google Scholar]
- 30.Machisa MT, Christofides N, Jewkes R. Structural pathways between child abuse, poor mental health outcomes and male-perpetrated intimate partner violence (IPV). PloS One. 2016;11: e0150986 10.1371/journal.pone.0150986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gibbs A, Jewkes R, Willan S, Washington L. Associations between poverty, mental health and substance use, gender power, and intimate partner violence amongst young (18–30) women and men in urban informal settlements in South Africa: A cross-sectional study and structural equation model. PLoS One. 2018;13: e0204956 10.1371/journal.pone.0204956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gibbs A, Jewkes R, Willan S, Washington L. Associations between poverty, mental health and substance use, gender power, and intimate partner violence amongst young (18–30) women and men in urban informal settlements in South Africa: A cross-sectional study and structural equation model. PLoS One. 2018;13: e0204956 10.1371/journal.pone.0204956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abrahams N, Jewkes R, Hoffman M, Laubsher R. Sexual violence against intimate partners in Cape Town: prevalence and risk factors reported by men. Bull World Health Organ. 2004;82: 330–337. [PMC free article] [PubMed] [Google Scholar]
- 34.Amegbor PM, Rosenberg MW. What geography can tell us? Effect of higher education on intimate partner violence against women in Uganda. Appl Geogr. 2019;106: 71–81. [Google Scholar]
- 35.Ahinkorah BO, Dickson KS, Seidu A-A. Women decision-making capacity and intimate partner violence among women in sub-Saharan Africa. Arch Public Health. 2018;76: 5 10.1186/s13690-018-0253-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Black E, Worth H, Clarke S, Obol JH, Akera P, Awor A, et al. Prevalence and correlates of intimate partner violence against women in conflict affected northern Uganda: a cross-sectional study. Confl Health. 2019;13: 35 10.1186/s13031-019-0219-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. The lancet. 2006;368: 1260–1269. [DOI] [PubMed] [Google Scholar]
- 38.UNICEF. Early Marriage: A Harmful Traditional Practice. New York: UNICEF, 2005. 2018. [Google Scholar]
- 39.Jewkes R. Intimate partner violence: causes and prevention. The lancet. 2002;359: 1423–1429. [DOI] [PubMed] [Google Scholar]
- 40.Kelly JT, Colantuoni E, Robinson C, Decker MR. From the battlefield to the bedroom: a multilevel analysis of the links between political conflict and intimate partner violence in Liberia. BMJ Glob Health. 2018;3: e000668 10.1136/bmjgh-2017-000668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kouyoumdjian FG, Calzavara LM, Bondy SJ, O’campo P, Serwadda D, Nalugoda F, et al. Intimate partner violence is associated with incident HIV infection in women in Uganda. Aids. 2013;27: 1331–1338. 10.1097/QAD.0b013e32835fd851 [DOI] [PubMed] [Google Scholar]
- 42.McCarthy KJ, Mehta R, Haberland NA. Gender, power, and violence: A systematic review of measures and their association with male perpetration of IPV. PloS One. 2018;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wandera SO, Kwagala B, Ndugga P, Kabagenyi A. Partners’ controlling behaviors and intimate partner sexual violence among married women in Uganda. BMC Public Health. 2015;15: 214 10.1186/s12889-015-1564-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dim EE. Differentials and Predictors of IPV against Nigerian Women in Rural and Urban Areas. J Aggress Maltreatment Trauma. 2019; 1–23. [Google Scholar]
- 45.Hellemans S, Loeys T, Buysse A, Dewaele A, De Smet O. Intimate Partner Violence Victimization Among Non-Heterosexuals: Prevalence and Associations With Mental and Sexual Well-Being. J Fam Violence. 2015;30: 171–188. 10.1007/s10896-015-9669-y [DOI] [Google Scholar]
- 46.Kouyoumdjian FG, Calzavara LM, Bondy SJ, O’Campo P, Serwadda D, Nalugoda F, et al. Risk factors for intimate partner violence in women in the Rakai Community Cohort Study, Uganda, from 2000 to 2009. BMC Public Health. 2013;13: 566 10.1186/1471-2458-13-566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Saile R, Neuner F, Ertl V, Catani C. Prevalence and predictors of partner violence against women in the aftermath of war: a survey among couples in Northern Uganda. Soc Sci Med. 2013;86: 17–25. 10.1016/j.socscimed.2013.02.046 [DOI] [PubMed] [Google Scholar]
- 48.Kilburn KN Pettifor A. Cash Transfers Conditional on Schooling Reduce IPV among Young Women in South Africa. 2019. [Google Scholar]
- 49.Benebo FO, Schumann B, Vaezghasemi M. Intimate partner violence against women in Nigeria: a multilevel study investigating the effect of women’s status and community norms. BMC Women's Health. 2018;18: 136 10.1186/s12905-018-0628-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moletsane R, Mitchell C. Researching Sexual Violence with Girls in Rural South Africa. Wiley Handb Violence Educ Forms Factors Prev. 2018; 433. [Google Scholar]
- 51.Annan J, Brier M. The risk of return: intimate partner violence in Northern Uganda’s armed conflict. Soc Sci Med. 2010;70: 152–159. 10.1016/j.socscimed.2009.09.027 [DOI] [PubMed] [Google Scholar]
- 52.Black E, Worth H, Clarke S, Obol JH, Akera P, Awor A, et al. Prevalence and correlates of intimate partner violence against women in conflict affected northern Uganda: a cross-sectional study. Confl Health. 2019;13: 35 10.1186/s13031-019-0219-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kinyanda E, Weiss HA, Mungherera M, Onyango-Mangen P, Ngabirano E, Kajungu R, et al. Intimate partner violence as seen in post-conflict eastern Uganda: prevalence, risk factors and mental health consequences. BMC Int Health Hum Rights. 2016;16: 5 10.1186/s12914-016-0079-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tlapek SM. Women’s status and intimate partner violence in the Democratic Republic of Congo. J Interpers Violence. 2015;30: 2526–2540. 10.1177/0886260514553118 [DOI] [PubMed] [Google Scholar]
- 55.Wako E, Elliott L, De Jesus S, Zotti ME, Swahn MH, Beltrami J. Conflict, displacement, and IPV: Findings from two Congolese refugee camps in Rwanda. Violence Women. 2015;21: 1087–1101. [DOI] [PubMed] [Google Scholar]
- 56.Alleyne-Green B, Kulick A, Matsuzaka S, Betancourt TS. War Violence Exposure, Reintegration Experiences and Intimate Partner Violence Among a Sample of War-Affected Females in Sierra Leone. Glob Soc Welf. 2019;6: 97–106. [Google Scholar]
- 57.Levtov RG, Barker G, Contreras-Urbina M, Heilman B, Verma R. Pathways to gender-equitable men: Findings from the international men and gender equality survey in eight countries. Men Masculinities. 2014;17: 467–501. [Google Scholar]
- 58.Bajunirwe F, Maling S, Adami H-O, Ajayi I, Volmink J, Adebamowo C, et al. Burden of depressive symptoms and non-alcohol substance abuse; and their association with alcohol use and partner violence: a cross-sectional study in four sub-Saharan Africa countries. Glob Ment Health. 2018;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Greene MC, Kane J, Tol WA. Alcohol use and intimate partner violence among women and their partners in sub-Saharan Africa. Glob Ment Health. 2017;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hatcher AM, Colvin CJ, Ndlovu N, Dworkin SL. Intimate partner violence among rural South African men: alcohol use, sexual decision-making, and partner communication. Cult Health Sex. 2014;16: 1023–1039. 10.1080/13691058.2014.924558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mthembu J, Khan G, Mabaso M, Simbayi L. Intimate partner violence as a factor associated with risky sexual behaviours and alcohol misuse amongst men in South Africa. AIDS Care. 2016;28: 1132–1137. 10.1080/09540121.2016.1146216 [DOI] [PubMed] [Google Scholar]
- 62.Zablotska IB, Gray RH, Koenig MA, Serwadda D, Nalugoda F, Kigozi G, et al. Alcohol use, intimate partner violence, sexual coercion and HIV among women aged 15–24 in Rakai, Uganda. AIDS Behav. 2009;13: 225–233. 10.1007/s10461-007-9333-5 [DOI] [PubMed] [Google Scholar]
- 63.Kirwan M, Parkhill MR, Schuetz BA, Cox A. A within-subjects analysis of men’s alcohol-involved and nonalcohol-involved sexual assaults. J Interpers Violence. 2019;34: 3392–3413. 10.1177/0886260516670179 [DOI] [PubMed] [Google Scholar]
- 64.McCarthy KJ, Mehta R, Haberland NA. Gender, power, and violence: A systematic review of measures and their association with male perpetration of IPV. PLoS One. 2018;13: e0207091 10.1371/journal.pone.0207091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sprague C, Hatcher AM, Woollett N, Sommers T, Black V. ‘They can’t report abuse, they can’t move out. They are at the mercy of these men’: exploring connections between intimate partner violence, gender and HIV in South African clinical settings. Cult Health Sex. 2016;18: 567–581. 10.1080/13691058.2015.1096420 [DOI] [PubMed] [Google Scholar]
- 66.Wandera SO, Kwagala B, Ndugga P, Kabagenyi A. Partners’ controlling behaviors and intimate partner sexual violence among married women in Uganda. BMC Public Health. 2015;15: 214 10.1186/s12889-015-1564-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kundapur R, Shetty SM, Kempaller VJ, Kumar A, Anurupa M. Violence against educated women by intimate partners in Urban Karnataka, India. Indian J Community Med Off Publ Indian Assoc Prev Soc Med. 2017;42: 147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Motsa ND, Morojele PJ. Vulnerable masculinities: Implications of gender socialisation in three rural Swazi primary schools. South Afr J Child Educ. 2019;9: 1–11. [Google Scholar]
- 69.Vyas S, Watts C. How does economic empowerment affect women’s risk of intimate partner violence in low- and middle-income countries? A systematic review of published evidence. J Int Dev. 2009;21: 577–602. 10.1002/jid.1500 [DOI] [Google Scholar]
- 70.Rahman M, Hoque MdA, Makinoda S. Intimate Partner Violence Against Women: Is Women Empowerment a Reducing Factor? A Study from a National Bangladeshi Sample. J Fam Violence. 2011;26: 411–420. 10.1007/s10896-011-9375-3 [DOI] [Google Scholar]
- 71.Riddell T, Ford-Gilboe M, Leipert B. Strategies Used by Rural Women to Stop, Avoid, or Escape From Intimate Partner Violence. Health Care Women Int. 2009;30: 134–159. 10.1080/07399330802523774 [DOI] [PubMed] [Google Scholar]
- 72.McDermott R, Cowden J. Polygyny and violence against women. Emory LJ. 2014;64: 1767. [Google Scholar]
- 73.McDermott R, Cowden J. Polygyny and Its Effects on Violence against Women. Polygyny Quest. 2015. [Google Scholar]
- 74.UNICEF. Early Marriage: A Harmful Traditional Practice. New York: UNICEF, 2005. 2018. [Google Scholar]
- 75.Doku DT, Asante KO. Women’s approval of domestic physical violence against wives: analysis of the Ghana demographic and health survey. BMC Womens Health. 2015;15: 120 10.1186/s12905-015-0276-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Flake DF. Individual, family, and community risk markers for domestic violence in Peru. Violence Women. 2005;11: 353–373. [DOI] [PubMed] [Google Scholar]
- 77.Beegle K, Christiaensen L, Dabalen A, Gaddis I. Poverty in a rising Africa. The World Bank; 2016. [Google Scholar]
- 78.Heise L, Ellsberg M, Gottemoeller M. Ending violence against women. Popul Rep. 1999;27: 1–1. [Google Scholar]
- 79.Mberu BU, Haregu TN, Kyobutungi C, Ezeh AC. Health and health-related indicators in slum, rural, and urban communities: a comparative analysis. Glob Health Action. 2016;9: 33163 10.3402/gha.v9.33163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Benebo FO, Schumann B, Vaezghasemi M. Intimate partner violence against women in Nigeria: a multilevel study investigating the effect of women’s status and community norms. BMC Womens Health. 2018;18: 136 10.1186/s12905-018-0628-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dirsuweit T, Mohamed S. Vertical and horizontal communities of practice: gender and geography in South Africa. South Afr Geogr J. 2016;98: 531–541. [Google Scholar]
- 82.Leddy AM, Lippman SA, Neilands TB, Twine R, Ahern J, Gómez-Olivé FX, et al. Community collective efficacy is associated with reduced physical intimate partner violence (IPV) incidence in the rural province of Mpumalanga, South Africa: findings from HPTN 068. J Epidemiol Community Health. 2019;73: 176–181. 10.1136/jech-2018-211357 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.