Dear Editor,
We retrospectively analyzed the microbiological spectrum and evaluated the factors associated with infection-related mortality in renal recipients with acute respiratory distress syndrome (ARDS) within 6 months after transplantation, according to the Berlin definition of ARDS [1], over the 10-year period from 2004 to 2014. Patient demographic and clinical data were collected, and laboratory data were collected at the onset of ARDS.
During the study period, 1,369 patients underwent renal transplantation and 72 developed ARDS caused by pneumonia. The leading cause of end-stage renal disease was glomerulonephritis (58.3 %). Mean patient age was 39.2 years, and average duration between transplantation and ARDS onset was 97.5 days. The predominant causative agents were bacteria (73.8 %), cytomegalovirus (12.7 %), and fungi (7.9 %). Twenty-eight and 11 patients had at least one acute rejection episode and one major infection before ARDS was diagnosed, respectively. Hepatitis B virus infection was found in 13.9 % of all these patients. Hospital mortality was 33.3 % overall. Ten (13.9 %) patients had mild, 38 (52.8 %) moderate, and 24 (33.3 %) severe ARDS; mortality was 4.2, 41.7, and 54.2 %, respectively (P = 0.005, Fig. 1).
Fig. 1.
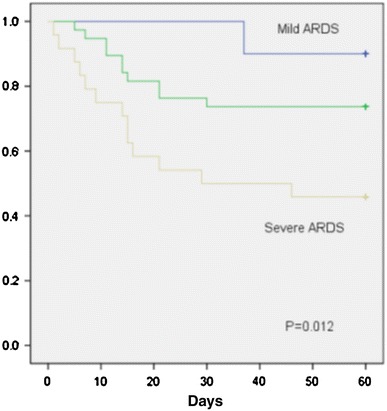
Cumulative survival according to ARDS severity category in the Berlin definition. Blue line indicates mild ARDS, green line moderate ARDS, and gray line severe ARDS. The three groups were compared using the log-rank test (P = 0.012)
The independent determinants of mortality were use of tacrolimus [odds ratio (OR) 7.7 (95 % confidence interval, CI 1.5–38.4), P = 0.013], serum creatinine level >1.5 mg/dL [OR 5.8 (95 % CI 1.6–20.4), P = 0.006], and severe ARDS [OR 5.0 (95 % CI 1.5–17.1), P = 0.01] at onset of ARDS, as shown in Table S1. White blood cell (WBC) count <10,000/mm3 (P = 0.043), which was significantly associated with mortality on univariate analysis, did not however remain significant on multivariate analysis.
The present study shows high incidence of ARDS (5.3 %) and mortality (33.3 %), in line with another study from China conducted by Tu et al. [2], who reported a mortality rate of 26.7 % in renal recipients with ARDS.
We revealed that use of tacrolimus had 7.7-fold greater mortality than cyclosporine-based immunosuppression, in line with an earlier study [3] suggesting that tacrolimus was associated with a significantly higher percentage of Pneumocystis carinii and cytomegalovirus infections. We also identified increased serum creatinine as a 5.8-fold greater risk factor for mortality, in accordance with a study [4] which reported high serum creatinine level to be a mortality determinant in renal recipients with respiratory failure due to pneumonia. We found severe ARDS to be significantly associated with mortality, in line with a study [5] suggesting that severe ARDS was a risk factor for higher mortality in patients with malignancies.
In conclusion, infection-related mortality in renal transplant patients with ARDS was associated with high serum creatinine level, severe ARDS, and use of tacrolimus.
Electronic supplementary material
Below is the link to the electronic supplementary material.
References
- 1.Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, Brochard L, Brower R, Esteban A, Gattinoni L, Rhodes A, Slutsky AS, Vincent JL, Rubenfeld GD, Thompson BT, Ranieri VM. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med. 2012;38:1573–1582. doi: 10.1007/s00134-012-2682-1. [DOI] [PubMed] [Google Scholar]
- 2.Tu GW, Ju MJ, Zheng YJ, Zhu DM, Xu M, Rong RM, Zhu TY, Luo Z. An interdisciplinary approach for renal transplant recipients with severe pneumonia: a single ICU experience. Intensive Care Med. 2014;40:914–915. doi: 10.1007/s00134-014-3296-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reichenberger F, Dickenmann M, Binet I, et al. Diagnostic yield of bronchoalveolar lavage following renal transplantation. Transpl Infect Dis. 2001;3:2–7. doi: 10.1034/j.1399-3062.2001.003001002.x. [DOI] [PubMed] [Google Scholar]
- 4.Shih CJ, Tarng DC, Yang WC, Yang CY. Immunosuppressant dose reduction and long-term rejection risk in renal transplant recipients with severe bacterial pneumonia. Singap Med J. 2014;55:372–377. doi: 10.11622/smedj.2014089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Azoulay E, Lemiale V, Mokart D, Pène F, Kouatchet A, Perez P, Vincent F, Mayaux J, Benoit D, Bruneel F, Meert AP, Nyunga M, Rabbat A, Darmon M. Acute respiratory distress syndrome in patients with malignancies. Intensive Care Med. 2014;40:1106–1114. doi: 10.1007/s00134-014-3354-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


