When governments in Asia and Canada imposed quarantine measures at the height of the severe acute respiratory syndrome (SARS) epidemic, most experts—particularly in the US—decried the tactics as outdated and ineffective (Nat. Med. 9, 487; 2003). With fresh data from the SARS outbreaks, however, many now say that isolating even a small percentage of those who have been exposed to the illness—but who are not yet ill—could help quell an outbreak.
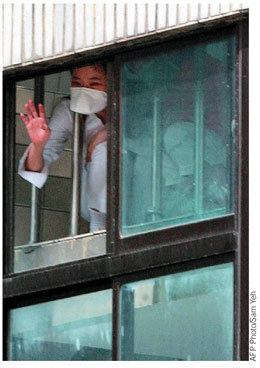
A grounded hospital employee waves from a window at the Taipei Municipal Hoping Hospital in April. Governments of many countries instituted mandatory quarantines during the SARS epidemic.
AFP Photo/Sam Yeh
“We're now reinventing a fourteenth-century public health tool, and we have to do it in the context of the twenty-first century,” says Martin Cetron, deputy director of the Division of Global Migration and Quarantine at the US Centers for Disease Control and Prevention (CDC). “Quarantine doesn't have to be airtight and under armed guard to be effective.”
Based on a model of quarantine's impact on smallpox transmission, Cetron says that isolating just 50% of those exposed to the smallpox virus could significantly reduce disease transmission. This is in stark contrast to the 90–95% experts had previously cited.
The CDC reported in October that only a third of the 30,000 Beijing residents quarantined during the SARS outbreak faced significant risk of contracting the flu-like illness (MMWR 52, 1037–1040; 2003). According to the report, only residents who came into direct contact with a symptomatic patient were later infected; those who had cared for a SARS patient carried the highest risk.
At least in the case of SARS, therefore, experts say quarantines can be implemented more efficiently by focusing on a smaller swath of the population: those who have had direct contact with an ill patient.
“For quarantine to be an important tool, it's most useful if people are infectious prior to the onset of symptoms—and we don't have any evidence that that's the case with SARS,” says Donald Low, microbiologist-in-chief at Mt. Sinai Hospital in Toronto. There is no data to support that someone infected with SARS can transmit the coronavirus during the incubation period—the time between exposure to the virus and the onset of symptoms. Patients become infectious as they enter the advanced and more symptomatic stages of the disease, giving scientists a window of several days in which to diagnose and isolate infected people.
For that reason, Low says he now favors increased self-monitoring for early-onset symptoms, such as fever. Mathematical models can help provide a better understanding of when an infected person begins spreading SARS, Low adds.
Another factor is the virus' mode of transmission. The World Health Organization says SARS is transmitted almost exclusively through direct contact with infectious droplets. But not everyone is ready to accept that analysis.
Even if a tiny percentage of infections are transmitted through the air or some means other than droplet spread, says James Koopman, a University of Michigan epidemiologist, it could completely alter the virus' transmission pattern. Koopman is developing a model to address the relative significance of different transmission patterns.
“It could be that less than 5% of all transmissions are airborne,” says Koopman. “But it may be that stopping that 5% is more important than stopping all the other 95%.”


