Abstract
Background:
The US has seen a rapid increase in synthetic opioid-related overdose deaths. We investigate Ohio, a state with one of the highest overdose death rates in 2017 and substantial numbers of deaths related to fentanyl, carfentanil, and other fentanyl analogs, to provide detailed evidence about the relationship between changes in the illicit drug market and overdose deaths.
Methods:
We investigate the illicit drug market using Ohio’s Bureau of Criminal Investigation’s (BCI) crime lab data from 2009 to 2018 that shows the content of drugs seized by law enforcement. We use Poisson regression analysis to estimate the relationship between monthly crime lab data and monthly unintentional drug overdose death data at the county level.
Results:
During this time period there has been a rapid change in the composition of drugs analyzed by the BCI labs, with a rapid fall in heroin observations, simultaneous rise in synthetic opioids, and an increase in the number of different fentanyl analogs. We find that the increased presence of fentanyl, carfentanil, and other fentanyl analogs have a strong correlation with an increase in overdose deaths. The types of opioids most associated with deaths varies by the population size of the county.
Conclusions:
Crime lab data has the potential to be used as an early warning system to alert persons who inject drugs, harm reduction services, first responders, and law enforcement about changes in the illicit opioid risk environment.
Keywords: Fentanyl, Carfentanil, Fentanyl Analogs, Overdose Deaths, Ohio
1. Introduction
The US is in the midst of a staggering opioid overdose crisis with 47,600 of 70,237 total drug overdose deaths involving opioids in 2017 (Lawrence et al., 2019). The “Triple Wave” opioid epidemic began with a rise in prescription opioid deaths in the 2000s, followed by a sharper rise in heroin deaths, and then in the last few years, a rapid rise in synthetic opioid deaths, cresting over the prior two waves (Ciccarone, 2017, 2019). The reformulation of OxyContin to the abuse-deterrent OxyNEO in 2010 likely caused a large demand shift from prescription opioids to heroin (Alpert et al., 2018; Evans et al., 2018). Starting in 2004, states began implementing electronic prescription drug monitoring programs (PDMPs) with varying enforcement levels, further reducing the availability of prescription opioids and causing a further shift towards heroin (Mallatt, 2018). Heroin prices had been low since the 1990s after Colombian-sourced heroin entered the US market (Rosenblum et al., 2014), making heroin a readily available and inexpensive substitute for many opioid consumers despite the stigma (Mars et al., 2014).
Among large parts of the eastern US, the illicit opioid market has transitioned from primarily consisting of heroin and black market prescription opioids to products marketed as heroin or black market prescription opioids, but which in fact are adulterated with or substituted by illicitly produced synthetic opioids: fentanyl, fentanyl analogs such as carfentanil, and other synthetic opioids such as U-47700 (Ciccarone et al., 2017; Mars et al., 2018a). Historically, there have been limited spikes in overdose deaths due to the substitution of heroin with fentanyl. The earliest known example in the US was a spike in overdose deaths in California in 1979 with the introduction of so-called “China White”, later determined to be 3-methylfentanyl (Henderson, 1988). New Jersey had a similar jump in fentanyl-related overdose deaths for an eight month period in 2006 (Hempstead and Yildirim, 2014). However, there is no historical precedent for the current large-scale substitution of heroin with synthetic opioids across a large part of the US for a prolonged duration. The current synthetic opioid surge appears to be driven by supply-side over demand-side forces (Ciccarone, 2019; Mars et al., 2019).
Much of our understanding of the shift to synthetic opioids comes from examining changes in the causes of death over time. However, this data only shows us the end point of illicit drug consumption providing indirect evidence of changes in the illicit drug market and consumption of opioids. We expand this understanding using Ohio as a test case. Using a unique dataset of the content of drugs seized by law enforcement from the Ohio Bureau of Criminal Investigation’s (BCI) crime labs, we are able to create a more direct estimate of changes in the illicit drug market in Ohio. Furthermore, since crime lab data has the potential to be more quickly released than mortality data, there is the potential to use this data to predict and, therefore, warn specific locations in Ohio of increasing risks in the illicit drug environment.
Our substantive contributions are to add empirical evidence to better understand the rapid and complex transition from heroin to synthetic opioids in Ohio, as well as estimate the relationship between the substances detected in state laboratories and overdose deaths. Ohio is an important state to study to better understand the opioid crisis. Ohio was the state with the second-highest drug overdose death rate in 2017 (Lawrence et al., 2019). One of the ten states tracking the presence of fentanyl analogs in overdose deaths via the State Unintentional Drug Overdose Reporting System (SUDORS), from July 2016 to June 2017, Ohio had 1,745 fentanyl analog overdose deaths of which 1,106 were attributed to one fentanyl analog: carfentanil (O’Donnell et al., 2018). The other nine states had 531 fentanyl analog overdose deaths combined, of which 130 were attributed to carfentanil.1 Ohio’s experience may be particularly useful as a lesson for other states about the ramifications of future increases in the presence of fentanyl analogs, increasing the potential for improving detection systems, and more rapidly responding to an emerging or worsening opioid crisis.
2. Methods
2.1. Data
Ohio drug seizure laboratory test data comes from the three Ohio BCI crime labs. The data contains all lab tests completed at the crime labs between January 1, 2009 and December 31, 2018 consisting of 397,815 total samples. The average time between the date of drug seizure and the testing date is approximately one month. However, a small fraction of tests may be delayed for several months.2 We use the date of drug seizure as the relevant date of drug observation. Thus, there is some data from drugs seized at the end of 2008, which we do not use, and given that we have test results through December 2018, the data should be approximately complete for drugs seized from 2009 through September 2018. The data was extensively cleaned to correct for spelling errors and ensure that there were no duplicate records.
Observations without a clear result are dropped from the analysis. These unclear tests may indicate an unknown substance, there is no controlled substance, an insufficient sample to test, the sample was not tested, there were no findings, or the test was a re-examination of a previously tested substance.3 In addition, observations are dropped if they indicate the sample looks like a particular prescription drug pill, but without testing it to know for certain. E.g. “whole tablet markings indicate Alprazolam. Not confirmed.” There were 86,809 such samples.
The BCI crime labs adopted a policy in March 2016 to not test for any minor misdemeanor amounts of cannabis, the most common illicit drug in the lab data, reducing the number of cannabis tests by approximately half compared to previous years. To ensure consistency across years, we removed any tests that solely contain cannabis or related drugs (e.g. hash) from the data (65,508 observations). However, the estimation results do not change substantially if the cannabis data is included in the estimates. Drugs are also excluded if they are likely unrelated to overdose deaths such as steroids or medications like acetaminophen. The definitions of the various drug classes used in the analysis are explained in more detail in Appendix A and are: fentanyl, carfentanil, other fentanyl analogs, heroin, prescription opioids, cocaine, benzodiazepines, synthetic cannibinoids, methamphetamines/amphetamines, other synthetic stimulants, MDMA, psychedelics, and other designer drugs. Drug samples can contain more than one drug class; i.e., if a sample contains heroin and fentanyl, it will be considered as both for the purposes of aggregating the number of heroin and fentanyl observations.
There are seven private crime labs in Ohio that are not part of BCI. We do not have access to data from these non-BCI labs. One difference between the BCI labs and the others is that the BCI labs test drugs for free (from law enforcement’s perspective), while the others charge for expedited test results. According to the BCI labs, there is no systematic difference in the types of drugs or associated crimes that the BCI labs handle versus the other labs.
The number of tests is generally consistent within a county over time, with counties that have larger populations and a higher overdose rate having more tests. The one outlier is Hamilton County, which includes Cincinnati, with far fewer tests than it should have given the number of overdose deaths and population.4 The low number of tests are due to Hamilton County generally using private instead of state labs, and we are unable to acquire data from these labs. Thus, we omit this county from the analysis.
We link the drug test data to Ohio unintentional drug overdose mortality data (for all drugs, not just opioids) from the Ohio Department of Health at the county-month level. The 2018 mortality data is preliminary and the delay between the date a drug is seized and when it is tested means that there are potential inaccuracies in the 2018 data. In addition, some of the control variables, namely the prescribed opioid morphine equivalent dose (MED) per capita for each quarter is only available starting in 2010 and the annual median income and poverty rates are only available through 2017. Thus, we restrict the sample for the estimates to the 2010 to 2017 time period, although the estimates do not change in any substantive way if we include data from 2009 and 2018 and remove the aforementioned control variables. After reducing the number of lab test observations due to the above parameters, we analyze the remaining 204,951 samples across 87 counties. We aggregate the drug test data to the county-month level. The 87 counties over the 2010–2017 time period provide 8,352 county-month observations. The mean values, standard deviations, and minimum and maximum values of each of the county-month level variables used in the estimates are reported in Appendix A, Table 3.
Table 3.
Descriptive Statistics (County-Month Level) 2010 to 2017
| Variable | Mean | Standard Deviation | Min | Max |
|---|---|---|---|---|
| Deaths | 2.4 | 5.3 | 0 | 77 |
| Number of Tests | 22.5 | 35.8 | 0 | 565 |
| Prescription Opioids | 4.5 | 8.0 | 0 | 120 |
| Heroin | 5.9 | 10.4 | 0 | 153 |
| Fentanyl | 1.2 | 3.5 | 0 | 53 |
| Carfentanil | 0.3 | 1.8 | 0 | 43 |
| Other Fentanyl Analogs | 0.3 | 1.4 | 0 | 31 |
| Cocaine | 5.1 | 10.9 | 0 | 150 |
| Benzodiazepines | 1.6 | 3.2 | 0 | 48 |
| Synthetic Cannibinoids | 0.7 | 7.8 | 0 | 473 |
| Meth/Amph | 3.5 | 7.1 | 0 | 80 |
| Other Synthetic Stimulants | 0.6 | 3.5 | 0 | 167 |
| MDMA | 0.2 | 1.1 | 0 | 35 |
| Psychedelics | 0.3 | 2.0 | 0 | 100 |
| Other Designer Drugs | 0.0 | 0.4 | 0 | 23 |
| Unemployment Rate (%*100) | 7.5 | 2.8 | 2.7 | 21.1 |
| Poverty Rate (%*100) | 14.7 | 4.6 | 4.4 | 35 |
| Median Income (1000s) | 48.7 | 10.0 | 32.0 | 107.7 |
| MED Opioids Per Capita | 2.3 | 0.8 | 0.3 | 6.0 |
| MED Suboxone Per Capita | 0.3 | 0.3 | 0 | 2.0 |
Notes: All Ohio counties except Hamilton county are included. There are 1,044 observations in each year (8,352 total). Fentanyl does not include other fentanyl analogs. Other fentanyl analogs does not include fentanyl or carfentanil. Number of Tests is the total number of tests for the illicit drug categories above, all of which are included in the estimates, and excludes, for example, cannabis. Drug categories are defined as above.
2.2. Estimation Strategy
We first present descriptive statistics on the changing pattern in drug-related deaths and in the illicit drug market in Ohio as measured by crime lab data. Next, since overdose death counts are the outcome of interest, we estimate the relationship between crime lab data and overdose deaths using a Poisson regression analysis.5 The estimates are robust to a linear regression specification and these estimation tables are available in the Supplemental Section. The number of overdose deaths6 each month in each of the 87 Ohio counties is regressed on the number of positive tests for illicit and prescription drugs from the BCI crime lab data7 each month in each of the 87 Ohio counties. The estimates include county fixed effects, month fixed effects, and county-specific linear time trends. The additional time-varying county-level controls included in the estimates are: annual poverty rates and median income,8 prescribed opioid morphine equivalent dose (MED) per capita for each quarter separated into Suboxone and non-Suboxone opioids,9 and monthly unemployment rates.10 Robust standard errors are clustered by county.
One of the goals of this study is to determine the public health value of knowing these lab tests, so even if the lab tests are not perfectly representative of the illicit drug market at a county-month level, it is an empirical question as to whether this information has valuable predictive power. That is, if we find no correlation between the test data and overdose deaths, this may be due to problems with the data. If we do find strong correlations despite the limitations of the data, then this available signal may be worth using, especially as there are so few short-term indicators of changing risk for drug overdose deaths. In addition, we are not making any causal claims about the direct effect of lab tests on mortality rates. So, for example, it may be the case that the amount of carfentanil available is relatively constant over time and law enforcement specifically targets carfentanil buyers and sellers when overdose deaths rise substantially, explaining the positive correlation between carfentanil positive lab tests and overdose deaths. Even so, the lab tests would still give us an early warning of increased risks in the illicit drug environment.
The month fixed effects control for any time trends in overdose deaths that are the same across Ohio. The county fixed effects control for any county differences that do not vary over time. The county-year linear time trends control for any county-specific linear time trends in overdose deaths. In this sense, it is a conservative estimate as, for example, if carfentanil was increasing across the whole state simultaneously and causing a similar increase in deaths, the month fixed effects would remove this state-wide change from the estimates. As shown below, at the county-level, there is large variation in the timing and extent of the emergence of various opioids, and this variation is what underpins the estimates. We control for several time-varying county-specific variables: economic controls (unemployment, poverty, median income) and the aggregate amounts of prescribed opioids per capita, which could independently cause changes in the demand, supply, or risk environment for illicit drugs. The economy is generally improving over this time period and counties with stronger improvements may have fewer overdose deaths. There has also been a decline in the amount of opioids prescribed, which could cause a spillover effect increasing the demand for illicit opioids and, therefore, overdose deaths. We separately control for the amount of Suboxone prescribed, which is one of the treatments for opioid use disorder. The amount of Suboxone prescribed has generally increased over the time period and may be associated with fewer overdose deaths.
All estimates are robust to using fentanyl-related overdose deaths as the outcome instead of overall overdose deaths, since changes in overdose deaths are largely driven by these deaths. However, from a policy perspective it may be more useful to look at whether there is an effect on all overdose deaths as people may shift their consumption of drugs from one type to another as the illicit drug market changes. In particular, if deaths are simply shifting from heroin-related to fentanyl-related, with no increase in total deaths, then the risk environment has not really changed. In addition, from a data perspective, researchers have found that opioid-related overdose deaths are under-counted (Ruhm, 2018), so looking at overall deaths avoids some possible data errors in classifying types of overdose deaths.
3. Results
3.1. Recent Trends in Overdose Deaths
Overdose deaths in Ohio have followed the Triple Wave pattern of the US as a whole: a rapid increase in prescription opioid deaths over the 2000s, followed by a more rapid increase in heroin deaths after 2010, followed by an even more rapid increase in synthetic opioid deaths after 2013. Figure 1 shows how non-fentanyl drug deaths in Ohio were steadily rising until 2013. After 2013 there was a decline in drug deaths unrelated to fentanyl or fentanyl analogs, but an increase in fentanyl-related deaths (the fentanyl deaths data includes deaths due to fentanyl and fentanyl analogs such as carfentanil, so any mention of “fentanyl” in this section should be taken to mean fentanyl or fentanyl analogs).
Fig. 1.
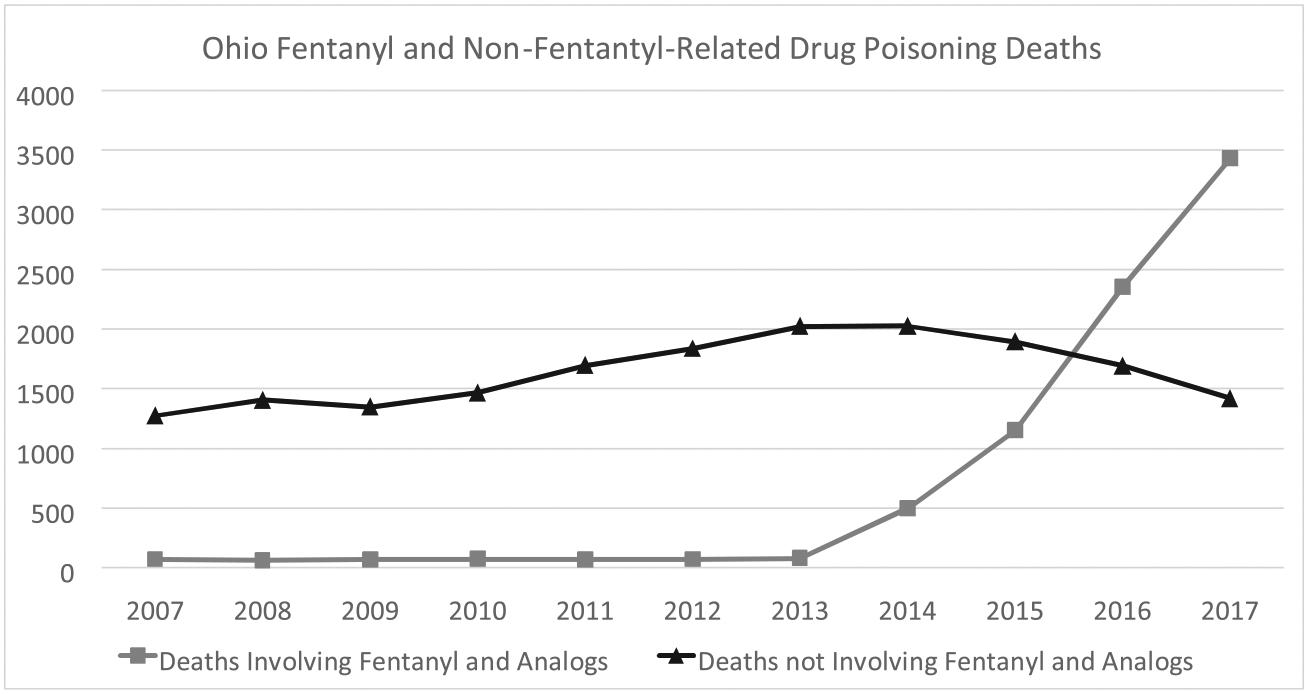
Ohio residents who died due to unintentional drug poisoning (underlying cause of death ICD-10 codes X40-X44). Fentanyl-related deaths include deaths related to fentanyl analogs and are determined by finding positive mentions of fentanyl and/or fentanyl analogs in death certificates. Data Source: Ohio Department of Health, Public Health Data Warehouse.
Supplemental Figures S1 and S2 show how heroin, cocaine, benzodiazepine, and psychostimulant (e.g. methamphetamine) related deaths have increasingly involved fentanyl as well. In 2013 there were 1,026 heroin-related deaths without fentanyl. In 2017, these fell to 267, while the number of deaths involving heroin and fentanyl increased to 720. Cocaine-related deaths have risen substantially over the last few years, but most of this increase is due to cocaine and fentanyl together. There is a similar pattern for benzodiazepine-related deaths, with a recent fall in such deaths unrelated to fentanyl and rapid increase in such deaths which also involve fentanyl. Psychostimulant deaths are somewhat distinct in that while fentanyl-involved pyschostimulant deaths have risen quickly, there is also a substantial increase in non-fentanyl related psychostimulant deaths, with less than 10 deaths per year before 2010, but increasing to 169 in 2017. This increase in psychostimulant deaths occurred at the same time as a significant increase in crime lab detections of amphetamine and methamphetamine (see Figure 2).
Fig. 2.
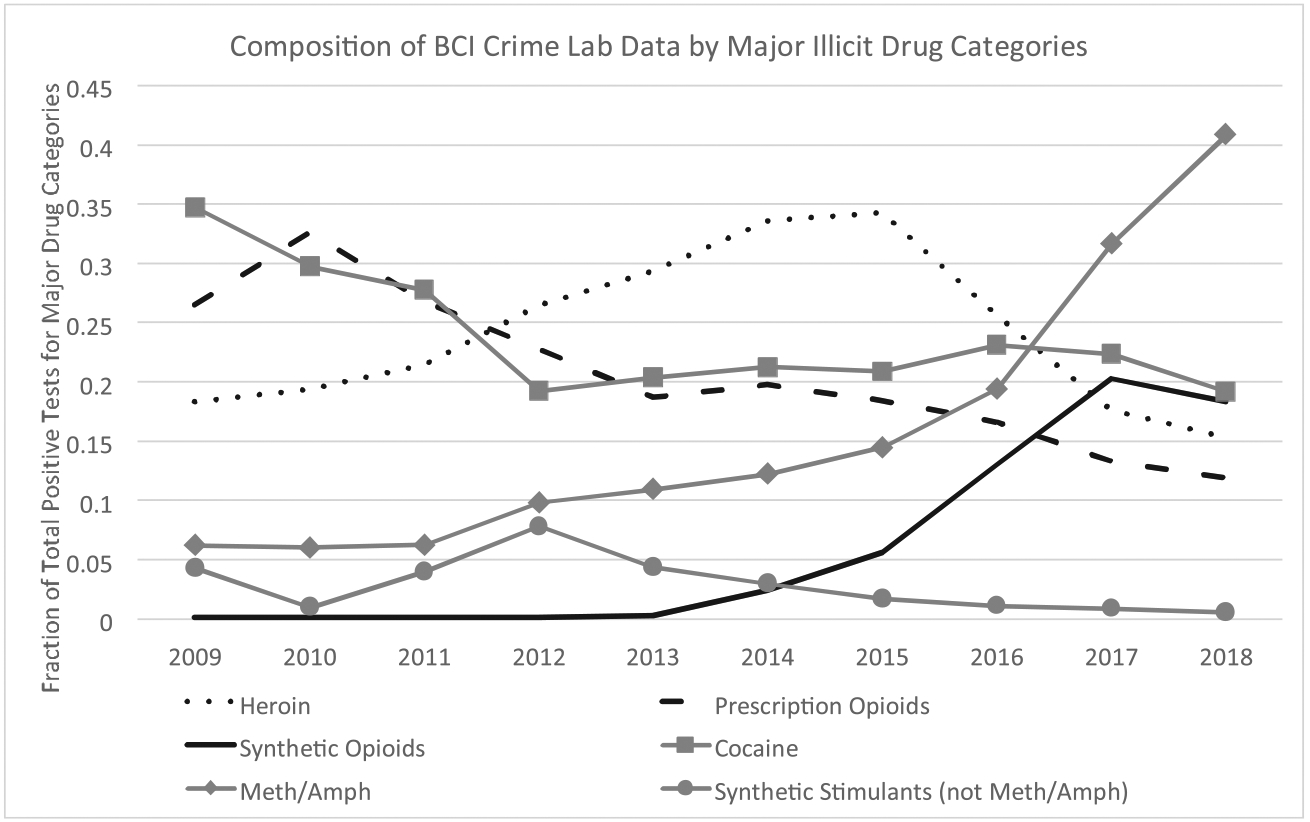
Annual fractions of positive BCI lab tests from major drug classes that contain the specified drug class. The fraction of tests is calculated as the number of drug-specific tests divided by the sum of all positive tests that can contain at least one of the major drug classes (that is fentanyl, carfentanil, other fentanyl analogs, heroin, cocaine, benzodiazepines, synthetic cannibinoids, methamphetamine/amphetamines, other synthetic stimulants (mostly cathinones), MDMA, psychedelics, and other designer drugs. Samples can test positive for multiple substances. Synthetic opioids includes fentanyl and analogs as well as other illicit synthetic opioids such as U-47700. Data Source: BCI Crime Lab Data, 2018 data is preliminary.
3.2. The Rapidly Changing Illicit Drug Market
Just as the composition of drug deaths have changed, the composition of illicit opioids analyzed in the state crime labs in Ohio has changed. Figure 2 shows that the crime lab data matches the Triple Wave, with a peak in prescription opioids in 2010, followed by a peak in heroin in 2015, and a peak in synthetic opioids in 2017. There has been a substantial increase in lab tests of methamphetamines/amphetamines since 2015, which corresponds to the timing of the increase in deaths related to these drugs.
Figure 3 shows more specifically how the composition of illicit synthetic opioids tested in crime labs has changed from 2013 to 2018. Fentanyl has seen a steady rapid increase, while 2017 was a peak year for carfentanil and other fentanyl analogs, with a sharp reduction in carfentanil in 2018. The composition of fentanyl analogs has also changed and become more complex over time. The only fentanyl analog detected in 2015 was acetyl fentanyl, which is more potent than heroin, but less potent than fentanyl. Eight new analogs appeared in 2016,11 six more appeared in 2017,12 and seven new analogs appeared in 2018.13 Other non-fentanyl synthetic opioids emerged as well: U-47700 in 2016 and U-48800, U-49900, and U-51754 in 2017.14 In addition, many crime lab samples contain more than one synthetic opioid. About 8 percent of samples with a synthetic opioid contained two or more in 2015 and 2016, 26 percent in 2017, and 19 percent in 2018. Most of these fentanyl analogs and non-fentanyl synthetic opioids have unknown potencies, exacerbating the asymmetric information problem in the illicit opioid market. That is, even if a consumer knew the exact chemical content of their drugs, they still would not be able to determine the potency.15
Fig. 3.
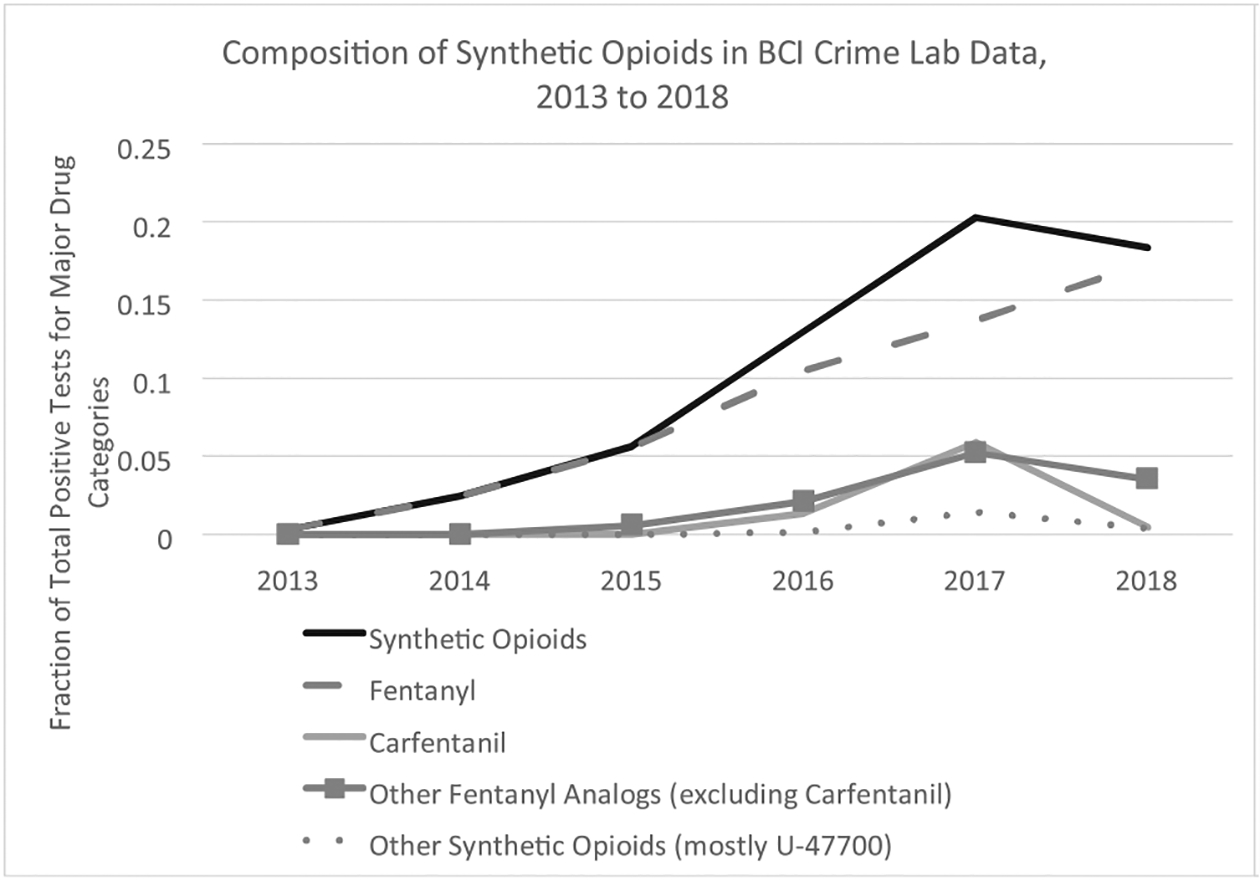
Annual fractions of positive BCI lab tests from major drug classes that contain the specified drug class. The fraction of tests is calculated as the number of drug-specific tests divided by the sum of all positive tests that can contain at least one of the major drug classes (that is fentanyl, carfentanil, other fentanyl analogs, heroin, cocaine, benzodiazepines, synthetic cannibinoids, methamphetamine/amphetamines, other synthetic stimulants (mostly cathinones), MDMA, psychedelics, and other designer drugs. Samples can test positive for multiple substances. Synthetic opioids includes fentanyl and analogs as well as other illicit synthetic opioids such as U47700. Data Source: BCI Crime Lab Data, 2018 data is preliminary.
3.3. The Connection Between Overdose Deaths and Drug Seizures
Comparing Figures 1 and 3, there is a clear positive correlation between the increase of fentanyl-related mortality and the increase of fentanyl found in BCI lab tests. However, the aggregate annual state-level counts hide the complexity of the timing of drug seizures sent to BCI labs containing synthetic opioids and overdose deaths at the county-month level. We illustrate these county-level differences in graphs of two counties of similar population size (approximately 500,000 people), Summit County in the northeast (includes Akron) and Montgomery County in southwest Ohio (includes Dayton).
Figure 4 shows the strong correlation between synthetic opioids found by the BCI crime labs and overdose deaths in Summit County. In 2014, the rise and fall in deaths begins to be correlated with the rise and fall in positive fentanyl tests. In mid-2016 there was a rapid increase in deaths at the same time as a rapid increase in positive carfentanil tests. In 2017, even though deaths fell with carfentanil detections, the level of monthly deaths is generally higher than in 2015, with less fentanyl detections, but more positive tests for fentanyl analogs.
Fig. 4.
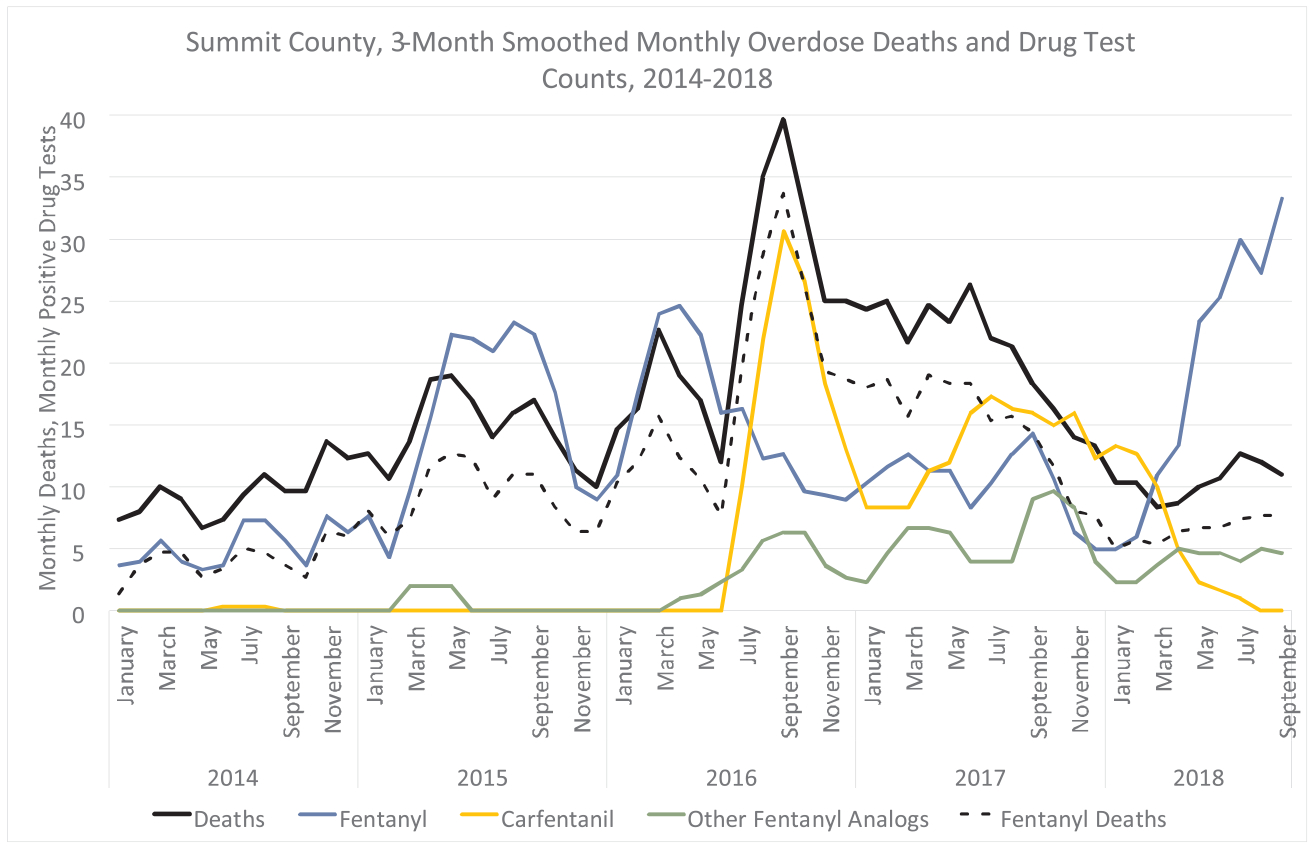
3-month smoothed count of monthly deaths of Ohio residents who died due to unintentional drug poisoning (underlying cause of death ICD-10 codes X40-X44). Fentanyl-related deaths include deaths related to fentanyl analogs and are determined by finding positive mentions of fentanyl and/or fentanyl analogs in death certificates. Drug tests and deaths are through September 2018. Fentanyl, carfentanil, and other fentanyl analog are 3-month smoothed monthly positive test counts. Fentanyl tests do not include any fentanyl analogs and other fentanyl analog tests do not include fentanyl or carfentanil. A sample can contain more than one substance. Data Source: Ohio Department of Health, Public Health Data Warehouse, and BCI Crime Labs, 2018 data is preliminary.
The graph for Montgomery County in Figure 5 shows a very different timing of events. Similar to Summit County, there are apparent correlations between positive fentanyl tests and overdose deaths. However, the peak in overdose deaths comes a year later than in Summit County, at the same time as the crime labs find a large number of samples of carfentanil and, to a lesser extent, other fentanyl analogs. In addition, there was a large amount of fentanyl found in Summit County in 2015 and a rise in deaths, while fentanyl did not appear in large quantities in Montgomery County until 2016. The patterns in overdose deaths are similar in the two counties before 2014, with close to zero fentanyl-related deaths. Thus, it is unlikely that differences in pre-existing trends in overdose deaths can explain differences in the later timing of the emergence of different synthetic opioids. In addition, given how closely the pattern of drug seizures matches the pattern of drug deaths, the graphs illustrate the potential for county-specific rapid detection systems to more nimbly address the opioid crisis.
Fig. 5.
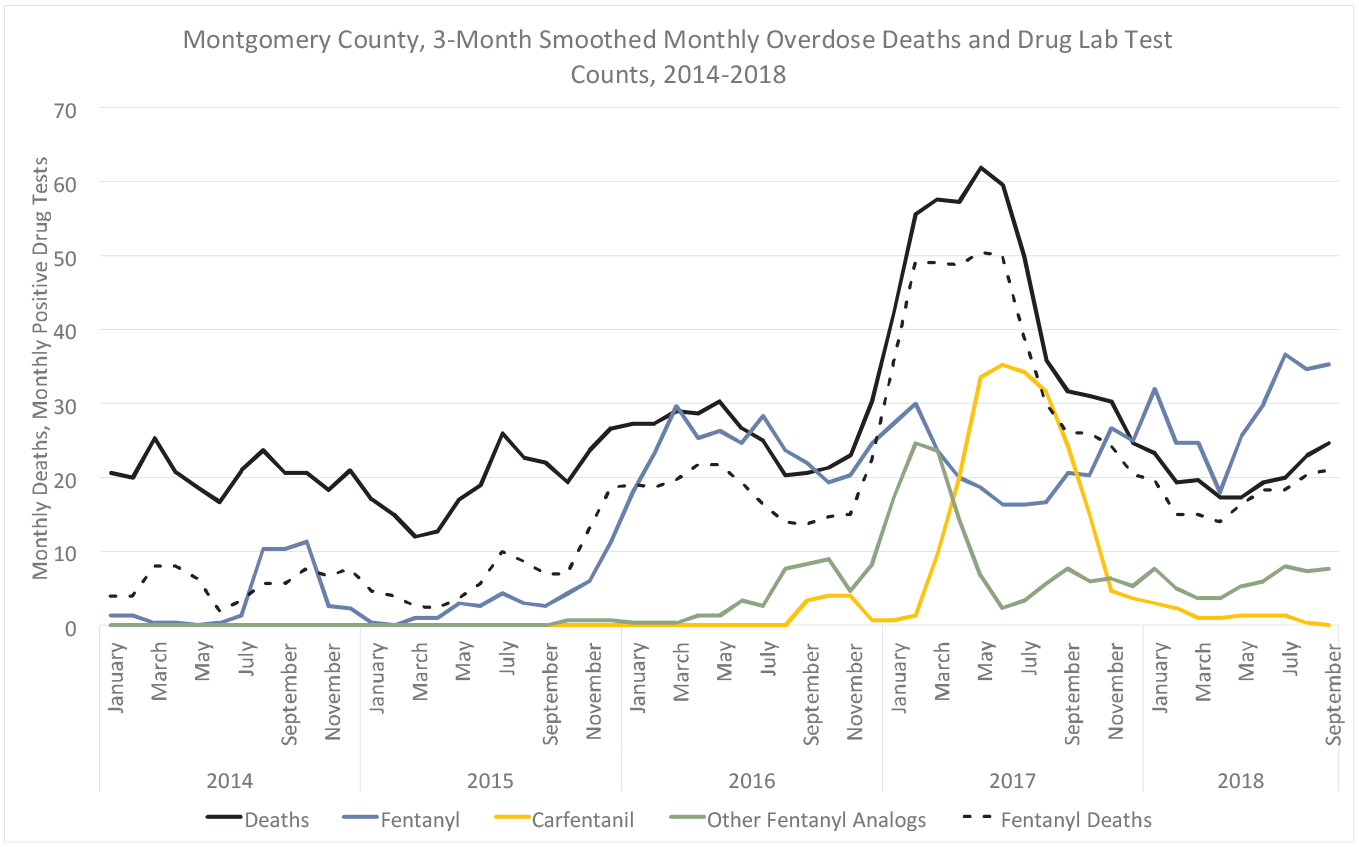
3-month smoothed count of monthly deaths of Ohio residents who died due to unintentional drug poisoning (underlying cause of death ICD-10 codes X40-X44). Fentanyl-related deaths include deaths related to fentanyl analogs and are determined by finding positive mentions of fentanyl and/or fentanyl analogs in death certificates. Drug tests and deaths are through September 2018. Fentanyl, carfentanil, and other fentanyl analog are 3-month smoothed monthly positive test counts. Fentanyl tests do not include any fentanyl analogs and other fentanyl analog tests do not include fentanyl or carfentanil. A sample can contain more than one substance. Data Source: Ohio Department of Health, Public Health Data Warehouse, and BCI Crime Labs, 2018 data is preliminary.
3.4. Estimation Results
The main estimates are presented in Table 1. Fentanyl, carfentanil, and other fentanyl analogs are positively correlated with overdose deaths at statistically significant levels. With all 87 counties included in column 1, every one additional observation of fentanyl in BCI crime lab tests in a county in a month predicts an extra 1.16 percent more deaths that month. In other words, if law enforcement finds 10 extra samples with fentanyl in a county with 20 monthly overdose deaths on average, we would expect an extra 2.4 deaths that month. Carfentanil positive tests are associated with more deaths than fentanyl: with 10 extra positive tests in a county with 20 monthly overdose deaths on average we would expect an extra 3.6 deaths that month. The coefficient for other fentanyl analogs is smaller than for fentanyl or carfentanil and has less statistical significance (5 percent compared to 1 percent for fentanyl and carfentanil). 10 more positive tests of other fentanyl analogs in a county with 20 monthly overdose deaths on average is associated with an extra 1.8 deaths that month. Summarizing, we find that changes in the presence of crime lab tests for synthetic opioids are useful as indicators of changes in the short-term risk of overdose deaths.
Table 1.
Poisson (IRR): Relationship Between Monthly BCI Crime Lab Tests and Monthly Overdose Deaths, 2010–2017
| All Counties (1) |
Small Counties (2) |
Medium Counties (3) |
Large Counties (4) |
|
|---|---|---|---|---|
| Fentanyl | 1.0116*** (0.0027) |
1.0108 (0.0144) |
1.0192** (0.0083) |
1.0114*** (0.0031) |
| Carfentanil | 1.0165*** (0.0031) |
0.9954 (0.0292) |
0.9969 (0.0300) |
1.0171*** (0.0033) |
| Other Fentanyl Analogs | 1.0086** (0.0039) |
1.0633** (0.0294) |
1.0229*** (0.0075) |
1.0099** (0.0044) |
| Heroin | 0.9990 (0.0012) |
0.9895 (0.0075) |
0.9977 (0.0053) |
0.9989 (0.0012) |
| Benzodiazepines | 0.9971** (0.0014) |
1.0039 (0.0129) |
1.0108 (0.0112) |
0.9970** (0.0014) |
| MDMA | 1.0073* (0.0040) |
0.9566 (0.0782) |
0.9853 (0.0187) |
1.0064 (0.0043) |
| Other Synthetic Stimulants (not Meth/Amph) | 0.9983* (0.0009) |
1.0134 (0.0274) |
1.0117 (0.0075) |
0.9977*** (0.0008) |
| Unemployment Rate (%*100) | 0.9537*** (0.0150) |
0.9640 (0.0400) |
0.9056** (0.0405) |
0.9537** (0.0203) |
| Poverty Rate (%*100) | 1.0244** (0.0124) |
0.9752 (0.0212) |
1.0523*** (0.0175) |
1.0186 (0.0191) |
| Median Income ($1000s) | 0.9895 (0.0084) |
0.9897 (0.0140) |
0.9779 (0.0197) |
0.9930 (0.0117) |
| MED Opioids Per Capita | 1.0217 (0.0913) |
0.7384* (0.1212) |
1.2816*** (0.1021) |
0.9554 (0.1221) |
| MED Suboxone Per Capita | 0.6980 (0.1583) |
1.3572 (0.6371) |
0.6380** (0.1311) |
1.2247 (0.8289) |
| Other Drug Tests | yes | yes | yes | yes |
| County and Month FE | yes | yes | yes | yes |
| County-Month Linear Trends | yes | yes | yes | yes |
| Observations | 8352 | 3744 | 2016 | 2592 |
| Counties | 87 | 39 | 22 | 26 |
Notes: Robust standard errors, clustered at the county level, are reported in parentheses. Coefficients are incidence rate ratios. Other drug tests control for the number of monthly positive tests of cocaine, synthetic cannibinoids, methamphetamine/amphetamines, psychedelics, and other designer drugs (each as a separate variable). See Appendix A for detailed definitions of drug categories. Each observation is at the county-month level from 2010 through 2017. Small Counties: population 50,000 or less. Medium Counties: population between 50,000 and 100,000. Large Counties: population more than 100,000.
p < 0.1.
p < 0.05.
p < 0.01.
The economic controls have some statistically significant correlations with overdose deaths: a higher poverty rate is associated with more overdose deaths, although a higher unemployment rate is associated with fewer deaths. The first finding is logical: an increase in poverty could increase the demand for illicit drugs, while the second finding is less intuitive. Unemployment rates were trending down over the period (the beginning of the time period is the end of the Great Recession with high unemployment). Counties that had large drops in unemployment over the time period happened to be smaller counties on average with few overdose deaths. Those with a smaller decrease in unemployment happened to be larger counties on average with many more deaths. Thus, the coefficient for the unemployment rate may be picking up population size differences. More or fewer MEDs of prescription opioids per capita do not have a statistically significant relationship at the 5 percent level with overdose deaths except in the restricted sample of medium sized counties in column 3 of the estimation tables, where they have the expected signs: an increase of non-Suboxone opioids is associated with more overdose deaths while an increase in Suboxone is associated with fewer overdose deaths.
The coefficients for positive tests of non-opioid drugs generally either lack statistical significance or have inconsistent relationships with overdose deaths across specifications. For example, lab tests finding benzodiazepines have a negative and statistically significant correlation with overdose deaths in Table 1, columns 1 and 4, at the 5 percent level. However, there is a positive correlation under OLS estimates, and statistical significance disappears in the robustness tables in Appendix B. Thus, although we think the estimates indicate the potential value of further research into the role of these drugs, we caution against reading too much into any specific coefficient for non-opioids.
One concern with the main estimates is that it is possible that drug sellers and consumers modify their behavior to reduce risk in response to an increasingly deadly illicit drug market, biasing the estimates towards finding a negative relationship between deaths and the amount of synthetic opioids in drug tests. However, given the short time-span of the observations, it is more likely that this negative effect is observed months later: counties with a relatively large amount of deadly synthetic opioids (and, hence, overdose deaths) in month T, may observe a relative decline in deaths in later months (T+1, T+2, etc.) as the drug market, consumer behavior, law enforcement, or harm reduction services respond to reduce the risk of overdose death.
To investigate the relationship between the timing of lab tests and overdose deaths we re-estimated the main Poisson regression changing the dependent variable to overdose death counts for the three months before and after the observed crime lab data, which is shown in Table 2. Fentanyl tests are positively correlated with contemporaneous overdose deaths and with about half the magnitude and less statistical significance, are positively correlated with future overdose deaths as well. Carfentanil tests have a different pattern, with positive statistically significant coefficients in the prior three months, and a decrease in the correlation over the next three months with a reduction in the risk of overdose death three months later. There are several possible explanations for the lag and lead pattern for carfentanil. For example: 1. the illicit drug market responded to the high number of deaths by making drugs relatively safer, 2. there is an increase in harm reduction services, law enforcement presence, and reduction in risk taking by consumers, or 3. carfentanil killed illicit drug users who are the most likely to die from an overdose in general leaving a smaller population of risky drug users later and, thus, having little apparent effect on overdose deaths later on. Other fentanyl analogs have an opposite relationship over time relative to carfentanil. Other analogs are negatively correlated with deaths two or three months prior, while the positive correlation if anything increases for the three months after. These findings indicate that more rapid testing, particularly for carfentanil, may be needed to have a meaningful impact. Fentanyl and other fentanyl analogs, however, are persistent problems allowing more time to respond to the release of crime lab data.
Table 2.
Poisson (IRR): Relationship Between Monthly BCI Crime Lab Tests and Later and Earlier Monthly Overdose Deaths, 2010–2017
| T-3 (1) |
T-2 (2) |
T-1 (3) |
T (4) |
T+1 (5) |
T+2 (6) |
T+3 (7) |
|
|---|---|---|---|---|---|---|---|
| Fentanyl | 1.0024 (0.0018) |
1.0026 (0.0021) |
1.0057*** (0.0020) |
1.0116*** (0.0027) |
1.0043* (0.0026) |
1.0056** (0.0023) |
1.0059* (0.0031) |
| Carfentanil | 1.0104*** (0.0038) |
1.0102*** (0.0031) |
1.0120*** (0.0030) |
1.0165*** (0.0031) |
1.0077*** (0.0026) |
0.9991 (0.0030) |
0.9944* (0.0032) |
| Other Fentanyl Analogs | 0.9877*** (0.0036) |
0.9876*** (0.0044) |
1.0005 (0.0045) |
1.0086** (0.0039) |
1.0111*** (0.0037) |
1.0114*** (0.0039) |
1.0117*** (0.0032) |
| Heroin | 1.0004 (0.0012) |
0.9997 (0.0008) |
0.9984* (0.0008) |
0.9990 (0.0012) |
0.9995 (0.0011) |
0.9983** (0.0008) |
0.9999 (0.0009) |
| Other Drug Tests | yes | yes | yes | yes | yes | yes | yes |
| Economic and Prescription Controls | yes | yes | yes | yes | yes | yes | yes |
| County and Month FE | yes | yes | yes | yes | yes | yes | yes |
| County-Month Linear Trends | yes | yes | yes | yes | yes | yes | yes |
| Observations | 8352 | 8352 | 8352 | 8352 | 8352 | 8352 | 8352 |
Notes: Robust standard errors, clustered at the county level (87 counties), are reported in parentheses. Coefficients are incidence rate ratios. Other drug tests control for the number of monthly positive tests of cocaine, benzodiazepines, synthetic cannibinoids, methamphetamine/amphetamines, other synthetic stimulants (mostly cathinones), MDMA, psychedelics, and other designer drugs (each as a separate variable). Each observation is at the county-month level from 2010 through 2017. Economic and prescription controls: monthly unemployment rate, quarterly MED of Suboxone and non-Suboxone opioids per capita, the annual poverty rate, and the annual median income. T+X are the monthly overdose deaths X months after the observed crime lab data and T-X are the monthly overdose deaths X months before the observed crime lab data.
p < 0.1.
p < 0.05.
p < 0.01.
There are large differences across counties and including them all in the main estimates may hide risks, particularly in smaller counties with fewer deaths. To investigate the potential for heterogeneous effects across counties, we divide the sample into counties with populations under 50,000 (39 counties), between 50,000 and 100,000 (22 counties), and 100,000 and above (26 counties).16 The main estimates are presented in the Table 1 in columns 2 to 4. Perhaps unsurprisingly, the estimates in column 1 are driven by the largest counties, which also have the most overdose deaths. Interestingly, the coefficient for carfentanil is only statistically significant in large counties. In the smallest counties, other fentanyl analogs are the only drug that is statistically significantly correlated with overdose deaths. These estimates indicate that the newly evolving fentanyl analogs may be playing a particularly dangerous role in low-population areas, which is hidden in the aggregate statistics, although we have no a priori reason for this empirical finding and leave it to future research to investigate why this may be occurring.
The robustness test estimation tables are presented in Appendix B. Table B.1 provides estimates using the fraction of tests that are positive in a county-month as independent variables instead of test counts to control for changes over time in the number of tests. Heroin lab tests do not have a statistically significant relationship with drug deaths in the main specification. However, in Table B.1, there is a negative relationship between the fraction of tests in a county-month that contain heroin and overdose deaths, statistically significant at the 1 percent level. We are unable to determine the specific underlying cause of this correlation. After 2014 the fraction of lab tests containing heroin not mixed with a synthetic opioid falls substantially while lab tests of heroin mixed with synthetic opioids and synthetic opioids in general increase. Thus, one possible explanation is that these estimates are picking up the shift from heroin to higher potency synthetic opioids.
The differences in correlations across county sizes are reinforced by linear regression estimates in robustness Table B.2 in Appendix B, where the overdose death rate per 100,000 adults is the dependent variable. These estimates should be read with some caution, as there are large standard errors when deriving death rates from small numbers of deaths, and these errors will be amplified in small counties. In column 1, which includes all counties, the coefficients for fentanyl, carfentanil, and other fentanyl analogs are all statistically significant at the 1 percent level and the magnitude of the other fentanyl analogs coefficient is larger than that for carfentanil. Given that an extra death in a small county has a much larger impact on the death rate than in a large county, and other fentanyl analogs are particularly important for explaining overdose deaths in small counties, it makes sense that they would be more strongly correlated with the overdose death rate than the overdose death count.
Aggregating all the different analogs together as if they were the same may be hiding the relatively high or low dangers of certain analogs. In Table B.3, instead of aggregating, we include separately the seven most common fentanyl analogs in the data as independent variables (acetyl, acryl, cyclopropyl, furanyl, 4-FIBF, 3-methyl, and methoxyacetyl).17 The table includes estimates by county size as well. Only acryl fentanyl, similar in potency to fentanyl but much less potent than carfentanil, has a statistically significant positive coefficient regardless of county size. These results provide more evidence of the potential to use the crime lab data for a future early warning system: the data indicates an increased risk of deaths if acryl fentanyl is found in large quantities. Acetyl and 3-methyl fentanyl are only associated with more deaths in medium sized counties, and 4-FIBF and methoxyacetyl fentanyl are only associated with more deaths in small counties.18 Cyclopropyl and furanyl fentanyl have no statistically significant relationship with overdose deaths. However, this lack of statistically significant relationships may be due to the small numbers in the crime lab data, so one should not take these estimates to mean that we should be unconcerned about future increases in the availability of these fentanyl analogs or the emergence of new fentanyl analogs. Rather, they should be seen as part of ongoing research that should be updated to include new data to find new predictors of overdose death.
4. Limitations
The BCI crime lab data, while imperfect, is to the best of our knowledge the best available indicator of the content of the illicit drug market in Ohio. However, the primary limitation in our analysis, and in research investigating illicit drug markets in general, is that the data does not provide a random sample of available and consumed illicit drugs and the demand for illicit drugs is not directly observable. In addition, the crime lab data only indicates whether a sample tests positive for particular drugs, and many samples test positive for more than one drug. There is no information about the amount of each detected substance or the proportion of the sample that is made up of each substance. One may be concerned that the estimates are biased by the BCI labs changing what they test for based on why people are dying. If this was the case, then the detection of a drug may be confounded by the timing of testing for that particular drug. For example, regarding the finding that the detection of carfentanil is positively correlated with overdose deaths, one may worry that the drug could have been around for some time, just not tested for, and the labs only started testing for carfentanil after people started dying from carfentanil. Our understanding from the BCI crime labs is that they would have tested for any known specific fentanyl analogs throughout the time period. Thus, the timing of testing should not be problematic for previously well-known fentanyl analogs such as carfentanil, acetyl fentanyl, and 3-methylfentanyl. However, as new fentanyl analogs are emerging all the time, there may be a time lag between the appearance of a new analog in Ohio and the addition of the analog to the list of substances detectable by the BCI labs. While it is unlikely that such a time lag would be related to overdose deaths in Ohio specifically in such a way as to bias the estimates, we cannot completely rule out this possibility.
Additionally, even though we control for county and month fixed effects, county-specific linear time trends, and several relevant time-varying county-level variables, there is the possibility of bias from county-specific unobserved omitted variables that are time-varying in a non-linear way, such as a sudden county-specific increase in demand for opioids. Another potential problem in interpreting the estimates is reverse-causality: changes in the composition of the drug market as measured by changes in crime lab positive tests may be affected by contemporaneous overdose deaths after including all of the controls. It does not seem plausible that an increase in overdose deaths would cause an increase in the adulteration of heroin with deadlier synthetic opioids. However, it could be the case, for example, that law enforcement may be purposefully targeting certain types of drug crimes (e.g. fentanyl) and not others based on the number of overdose deaths. That is law enforcement intensity rather than changes in the underlying illicit drug market could be the underlying unobserved variable driving the positive correlation between fentanyl/carfentanil/fentanyl analog crime lab tests and overdose deaths. Another possibility is that courts may have become more lenient towards specific types of drug crimes, e.g. via an expansion of drug courts that reduced the need for labs to test specific drugs. Given that we cannot directly observe county-specific changes in law enforcement priorities or the criminal justice system, these unobservables may be an underlying cause of the estimated relationship between BCI lab tests and overdose deaths. Other unobservables, such as a sudden increase in the population of opioid users is another potential reason for the positive correlation between synthetic opioid tests and overdose deaths, so we are hesitant to conclude that the changing illicit opioid market as measured by crime lab tests is directly causing an increase in overdose deaths. Having said that, as mentioned above, the strong correlation of overdose deaths with the BCI crime lab tests finding synthetic opioids make the lab tests a valuable resource for an early warning system regardless of the true causal relationship.
5. Discussion
The rise in fentanyl adulterated or substituted heroin represents a significant shift in the risk environment for people who inject drugs (PWID) (Ciccarone, 2017). The best evidence we have had of the increasing danger of fentanyl and other synthetic opioids is the increasing number of deaths related to these drugs. We fill some of the gap in our understanding of synthetic opioids contributing to a worsening risk environment for heroin users by providing new evidence that the illicit drug market has been changing rapidly in Ohio, which is likely a major factor in the recent surge in overdose deaths. The strong statistical relationship between overdose deaths and crime lab tests for synthetic opioids provides evidence for making this information publicly available as quickly as possible on an ongoing basis. Surveillance of the drug supply, both on an intimate as well as mass scale, may provide a way to alter the risk environment (Ciccarone, 2017). As heroin has become increasingly contaminated with synthetic opioids, people change their behavior to reduce risk (McKnight and Des Jarlais, 2018; Mars et al., 2018b). For example, there is evidence that if PWID are provided with fentanyl test strips, they take a variety of measures to decrease their risk of overdose (Peiper et al., 2019). Providing timely information about the contents of seized drugs, at the local city or county level, a relatively low-cost intervention, so that people can respond to location-specific changes in the risk of encountering evolving synthetic opioids is another promising way to help PWID take steps to reduce their chances of dying. Furthermore, the data can be used by harm reduction services, first responders, and law enforcement to more quickly respond to emerging spikes in overdose deaths. In addition, the data can alert us to new and evolving trends in the illicit drug market, such as changes in polydrug use and the recent substantial shift in the crime lab data towards methamphetamines.
Our findings are critically important from a policy perspective. Ohio’s experience with carfentanil in particular, with a surge in deaths and then a quick disappearance, should cause alarm for other states. Current public detection systems are not up to the task to respond in a timely manner. Rhode Island, for example, set up a website to provide the public with information on where overdoses are occurring to help provide the public with more information about the opioid crisis (Marshall et al., 2017).19 However, the data is only updated biannually with a significant time lag (at the end of 2018, only 2017 data was available) and little information that could help change behavior or efficiently redirect harm reduction services to counter a sudden appearance of a new deadlier opioid. Providing crime lab data quickly (e.g. within a week or month) could provide a real opportunity to have a rapid response to a rapidly changing risk environment.
Supplementary Material
Acknowledgments
We thank Dennis Cauchon, Harm Reduction Ohio, and the Ohio Bureau of Criminal Investigation (BCI) for providing crime lab data. BCI had no further role in study design; analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. Funding for this study was provided by NIH-NIDA Grant R01DA037820; NIH-NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. Mortality data are publicly available from the Ohio Department of Health. The Department specifically disclaims responsibility for any analyses, interpretations or conclusions.
Appendix A. Drug Class Definitions and Descriptive Statistics
We list below the definition of the drug classes that we created from the BCI crime lab. The drugs in the data are contained as a list of drugs in string format. We searched these strings for specific drug names to categorize below. The data was cleaned and corrected for misspellings (e.g. fentanyl is spelled as fetanyl, fenrtanyl, fenanyl, and fenatnyl) and to remove potential double counts (e.g. to ensure acetyl fentanyl was counted as a fentanyl analog, but not fentanyl itself).
Fentanyl:
Fentanyl. Does not include any fentanyl analogs.
Carfentanil:
Carfentanil.
Other Fentanyl Analogs:
Acetyl, acryl, 4-flouroisobutyryl, furanyl, 3-methyl, ortho-fluoro, tetrahydrofuran, valeryl, benzyl, butyryl, crotonyl, cyclopropyl, methoxy-acetyl, phenyl fentanyl, benzylfuranyl, benzylparaflouro, benzylparaflourocyclopropyl, nmethylnor, orthomethylacetyl, orthomethylfuranyl, and thiophene fentanyl. Does not include non-fentanyl synthetic opioids: U-47700, U-48800, U-49900, and U-51754.
Heroin:
Heroin or 6-Monoacetylmorphine
Prescription Opioids:
Buprenorphine, morphine, codeine, oxycodone, oxymorphone, hydromorphone, hydrocodone, tramadol, methadone, diphenoxylate, pentazocine, propoxyphene, tapentadol, dihydrocodeine, dextropropoxyphene, dextromethorphan, levomethorphan.
Cocaine:
Cocaine.
Benzodiazepines:
Clonazepam, alprazolam, lorazepam, diazepam, chlordiazepoxide, clorazepate, midazolam, oxazepam, triazolam, temazepam, diclazepam, etizolam, flubromazepam, flubromazolam, phenazepam, flurazepam, clonazolam.
Synthetic Cannibinoids:
65 different synthetic cannibinoids (e.g. AB-CHMINACA, AB-FUBINACA, etc.). A full list is available upon request.
Methamphetamine/Amphetamine:
Methamphetamine or amphetamine.
Other Synthetic Stimulants:
67 different cathinones (e.g. pentedrone) and amphetamine-like drugs (e.g. phentermine). A full list is available upon request.
MDMA:
MDMA, MDA, MDMC, and MDDMA.
Psychedelics:
Psilocyn, psilocybin, LSD, 4-HO-DET, 4-AcO-DMT, 5-MeO-DALT, 5-MeO-DIPT, 5-MeO-MiPT, DMT, AMT, NMT, DPT, DOB, DOI, and mescaline.
Other Designer Drugs:
25B-NBOMe, 25C-NBOMe, 25H-NBOMe, 25I-NBOMe, Bk-2C-B, 2-CB, 2-CI, and 2-CP.
Appendix B. Robustness Tables
Table B.1.
Poisson (IRR): Relationship Between Fraction of Monthly BCI Crime Lab Tests and Monthly Overdose Deaths, 2010–2017
| All Counties (1) |
Small Counties (2) |
Medium Counties (3) |
Large Counties (4) |
|
|---|---|---|---|---|
| % Fentanyl | 1.6889*** (0.2326) |
1.2333 (0.3206) |
0.9901 (0.3230) |
1.9258*** (0.3501) |
| % Carfentanil | 2.4280*** (0.7433) |
1.5532 (0.9393) |
1.1682 (0.4403) |
2.8116*** (1.0819) |
| % Other Fentanyl Analogs | 2.2510*** (0.4451) |
2.8261*** (0.8410) |
4.1513*** (1.2144) |
1.9151** (0.4928) |
| % Heroin | 0.8778*** (0.0433) |
0.9952 (0.1194) |
0.7737** (0.0906) |
0.8866* (0.0562) |
| % Benzodiazepines | 0.9907 (0.1060) |
0.8122 (0.1762) |
0.6946 (0.2043) |
1.1051 (0.1372) |
| % MDMA | 1.3058 (0.3729) |
1.2979 (0.6405) |
1.4150 (0.7079) |
1.1389 (0.4227) |
| % Other Synthetic Stimulants (not Meth/Amph) | 0.8610 (0.1037) |
1.1091 (0.2911) |
1.0809 (0.4841) |
0.8022* (0.1056) |
| Poverty Rate (%*100) | 1.0157 (0.0144) |
0.9737 (0.0209) |
1.0546*** (0.0170) |
1.0054 (0.0227) |
| Median Income ($1000s) | 0.9843* (0.0092) |
0.9904 (0.0142) |
0.9787 (0.0206) |
0.9844 (0.0133) |
| Unemployment Rate (%*100) | 0.9616** (0.0151) |
0.9606 (0.0392) |
0.9267* (0.0390) |
0.9641* (0.0186) |
| MED Opioids Per Capita | 1.0247 (0.0938) |
0.7484* (0.1278) |
1.3303*** (0.1210) |
0.9751 (0.1360) |
| MED Suboxone Per Capita | 0.7579 (0.1833) |
1.3663 (0.6529) |
0.6175** (0.1264) |
1.1645 (0.9595) |
| Other Drug Tests | yes | yes | yes | yes |
| County and Month FE | yes | yes | yes | yes |
| County-Month Linear Trends | yes | yes | yes | yes |
| Observations | 8352 | 3744 | 2016 | 2592 |
| Counties | 87 | 39 | 22 | 26 |
Notes: Robust standard errors, clustered at the county level, are reported in parentheses. Coefficients are incidence rate ratios. Other drug tests control for the number of monthly positive tests of cocaine, synthetic cannibinoids, methamphetamine/amphetamines, psychedelics, and other designer drugs (each as a separate variable). See Appendix A for detailed definitions of drug categories. Each observation is at the county-month level from 2010 through 2017. Small Counties: population 50,000 or less. Medium Counties: population between 50,000 and 100,000. Large Counties: population more than 100,000.
p < 0.1.
p < 0.05.
p < 0.01.
Table B.2.
OLS: Relationship Between Monthly BCI Crime Lab Tests and Monthly Overdose Death Rate (per 100,000 adults), 2010–2017
| All Counties (1) |
Small Counties (2) |
Medium Counties (3) |
Large Counties (4) |
|
|---|---|---|---|---|
| Fentanyl | 0.0510*** (0.0145) |
0.0514 (0.0448) |
0.0773** (0.0340) |
0.0440** (0.0182) |
| Carfentanil | 0.0904*** (0.0283) |
−0.0220 (0.1350) |
−0.0258 (0.1276) |
0.1117*** (0.0287) |
| Other Fentanyl Analogs | 0.1319*** (0.0319) |
0.3823** (0.1650) |
0.1025*** (0.0314) |
0.1450*** (0.0376) |
| Heroin | −0.0038 (0.0044) |
−0.0285* (0.0169) |
−0.0060 (0.0106) |
0.0011 (0.0028) |
| Benzodiazepines | 0.0046 (0.0100) |
−0.0035 (0.0321) |
0.0222 (0.0259) |
−0.0009 (0.0082) |
| MDMA | −0.0045 (0.0145) |
−0.1467 (0.1154) |
−0.0140 (0.0239) |
0.0016 (0.0152) |
| Other Synthetic Stimulants (Not Meth/Amph) | 0.0039 (0.0053) |
0.0182 (0.0425) |
0.0216 (0.0193) |
−0.0005 (0.0034) |
| Unemployment Rate (%*100) | −0.0755 (0.0558) |
−0.0256 (0.0842) |
−0.1972** (0.0888) |
−0.0901 (0.0676) |
| Poverty Rate (%*100) | −0.0050 (0.0299) |
−0.1010** (0.0474) |
0.1050*** (0.0331) |
0.0012 (0.0380) |
| Median Income ($1000s) | −0.0272 (0.0223) |
−0.0269 (0.0338) |
−0.0339 (0.0417) |
−0.0014 (0.0325) |
| MED Opioids Per Capita | 0.0562 (0.2738) |
−0.5098 (0.4164) |
0.7558*** (0.2003) |
−0.2588 (0.3169) |
| MED Suboxone Per Capita | −0.4955 (0.7270) |
0.8289 (1.0070) |
−1.6142** (0.6081) |
−0.8193 (2.1357) |
| Other Drug Tests | yes | yes | yes | yes |
| County and Month FE | yes | yes | yes | yes |
| County-Month Linear Trends | yes | yes | yes | yes |
| R-Squared | 0.26 | 0.18 | 0.31 | 0.58 |
| Observations | 8352 | 3744 | 2016 | 2592 |
| Counties | 87 | 39 | 22 | 26 |
Notes: Robust standard errors, clustered at the county level, are reported in parentheses. Other drug tests control for the number of monthly positive tests of cocaine, synthetic cannibinoids, methamphetamine/amphetamines, psychedelics, and other designer drugs (each as a separate variable). See Appendix A for detailed definitions of drug categories. Each observation is at the county-month level from 2010 through 2017. The death rate is calculated as the number of deaths in a county-month divided by the county population aged 18 and over from the US Census July 1st estimates for the corresponding year multiplied by 100,000. Small Counties: population 50,000 or less. Medium Counties: population between 50,000 and 100,000. Large Counties: population more than 100,000.
p < 0.1.
p < 0.05.
p < 0.01.
Table B.3.
Investigating Specific Fentanyl Analogs. Poisson (IRR): Relationship Between Monthly BCI Crime Lab Tests and Monthly Overdose Deaths, 2010–2017
| All Counties (1) |
Small Counties (2) |
Medium Counties (3) |
Large Counties (4) |
|
|---|---|---|---|---|
| Acetyl Fentanyl | 0.9975 (0.0103) |
1.0045 (0.0735) |
1.0890** (0.0394) |
0.9905 (0.0092) |
| Acryl Fentanyl | 1.0193** (0.0083) |
1.1310*** (0.0374) |
1.0513* (0.0305) |
1.0209** (0.0102) |
| Cyclopropyl Fentanyl | 1.0192 (0.0251) |
0.9942 (0.0907) |
0.9345 (0.0835) |
1.0215 (0.0241) |
| Furanyl Fentanyl | 0.9982 (0.0118) |
0.9782 (0.0576) |
0.9822 (0.0330) |
0.9995 (0.0134) |
| 3-Methyl Fentanyl | 1.0082 (0.0076) |
0.9374 (0.0711) |
1.0184*** (0.0060) |
1.0070 (0.0302) |
| 4-FIBF | 0.9611 (0.0326) |
1.1233** (0.0635) |
1.0209 (0.2158) |
0.9544 (0.0336) |
| Methoxyacetyl Fentanyl | 0.9470 (0.0357) |
1.7185** (0.3799) |
1.1291 (0.0981) |
0.9395 (0.0388) |
| Fentanyl | 1.0123*** (0.0025) |
1.0047 (0.0136) |
1.0140* (0.0085) |
1.0123*** (0.0030) |
| Carfentanil | 1.0176*** (0.0031) |
1.0025 (0.0327) |
1.0070 (0.0265) |
1.0184*** (0.0032) |
| Other Uncommon Fentanyl Analogs |
0.9517 (0.0306) |
0.9523 (0.1613) |
0.9205 (0.1409) |
0.9654 (0.0332) |
| Heroin | 0.9988 (0.0011) |
0.9908 (0.0073) |
0.9973 (0.0051) |
0.9987 (0.0011) |
| County and Month FE | yes | yes | yes | yes |
| Other Drug Tests | yes | yes | yes | yes |
| County-Month Linear Trends | yes | yes | yes | yes |
| Economic and Prescription Controls | yes | yes | yes | yes |
| Observations | 8352 | 3744 | 2016 | 2592 |
Notes: Robust standard errors, clustered at the county level (87 counties), are reported in parentheses. Coefficients are incidence rate ratios. Other drug tests control for the number of monthly positive tests of cocaine, benzodiazepines, synthetic cannibinoids, methamphetamine/amphetamines, other synthetic stimulants (mostly cathinones), MDMA, psychedelics, and other designer drugs (each as a separate variable). Uncommon fentanyl analogs are those with less than 100 positive tests in the BCI crime lab data. Each observation is at the county-month level from 2010 through 2017. Economic and prescription controls: monthly unemployment rate, quarterly MED of Suboxone and non-Suboxone opioids per capita, the annual poverty rate, and the annual median income. Small Counties: population 50,000 or less. Medium Counties: population between 50,000 and 100,000. Large Counties: population more than 100,000.
p < 0.1.
p < 0.05.
p < 0.01.
Appendix C. Supplementary Data
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.drugalcdep.2019.107779.
Footnotes
These “fentanyl analogs” do not include fentanyl itself. The other states are Kentucky, Maine, Massachusetts, New Hampshire, New Mexico, Oklahoma, Rhode Island, West Virginia and Wisconsin. The comparison of Ohio to these other states may be limited by differences across states in the accuracy of the SUDORS data.
For example, in crime lab data for tests completed for only the third quarter of 2018, approximately half of the sample were from July, August and September (the third quarter), another 40 percent of the sample were seized in May or June, and about 8 percent were from earlier dates.
We cannot link observations to see which were re-tested. These re-tests make up a small part of the sample.
Hamilton County, the third most populous, with a population of about 800,000 had 342 BCI crime lab tests with a positive result between 2009 and 2018. This number is similar to the 335 tests for Henry County with only approximately 27,000 people and one-hundredth the number of overdose deaths. Summit County with a population of over 500,000 had 12,150 BCI crime lab tests and about half the overdose deaths of Hamilton County.
A negative binomial regression to correct for potential overdispersion gives similar estimates.
Underlying cause of death ICD-10 codes X40-X44, unintentional drug overdose deaths.
Specific drug classes and included drugs are explained in Appendix A.
From the US Census Small Area Income and Poverty Estimates (SAIPE).
From the Ohio Automated RX Reporting System Quarterly County Data. The Suboxone classification includes buprenorphine/naloxone combinations, but not buprenorphine-only drugs such as Butrans and Subutex.
From the US Bureau of Labor Statistic.
Acryl, carfentanil, 4-flouroisobutyryl, furanyl, 3-methyl, ortho-fluoro, tetrahydrofuran, and valeryl fentanyl.
Benzyl, butyryl, crotonyl, cyclopropyl, methoxy-acetyl, phenyl fentanyl.
Benzylfuranyl, benzylparaflouro, benzylparaflourocyclopropyl, nmethylnor, orthomethylacetyl, orthomethylfuranyl, and thiophene fentanyl.
We do not include these non-fentanyl synthetic opioids in the estimates below. However, the estimates are unaffected if they are included and there is no statistically significant relationship between the presence of these opioids and overdose deaths.
See, for example, Suzuki and El-Haddad (2017). Of the 21 fentanyl analogs they compare, 12 have unknown potencies.
Populations are from the Ohio Department of Development’s 2010 Census Population counts for each county.
These are all the fentanyl analogs with at least 100 positive tests in the BCI crime lab data.
The coefficients for acetyl and methoxyacetyl are not robust to different estimation specifications. In OLS estimates in Supplemental Table S4, acetyl fentanyl has a negative correlation with deaths and methoxyacetyl has no statistically significant relationship with deaths.
The Rhode Island website is www.PreventOverdoseRI.org. A similar opioid monitoring website has been implemented for Staten Island, sidrugprevention.org.
References
- Alpert Abby, Powell David, Pacula Rosalie Liccardo, 2018. Supply-side drug policy in the presence of substitutes: Evidence from the introduction of abuse-deterrent opioids. American Economic Journal: Economic Policy 10 (4), 1–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D, 2017. Fentanyl in the US heroin supply: a rapidly changing risk environment. International Journal of Drug Policy 46, 107–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D, 2019. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. International Journal of Drug Policy 71, 183–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone Daniel, Ondocsin Jeff, Mars Sarah G., 2017. Heroin uncertainties: Exploring users perceptions of fentanyl-adulterated and -substituted ‘heroin’. International Journal of Drug Policy 46, 146–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans William N, Ethan Lieber, and Patrick Power 2018. How the reformulation of OxyContin ignited the heroin epidemic. NBER Working Paper No. 24475
- Hempstead Katherine, Yildirim Emel O., 2014. Supply-Side Response To Declining Heroin Purity: Fentanyl Overdose Episode In New Jersey. Health Economics 23 (6), 688–705. [DOI] [PubMed] [Google Scholar]
- Henderson Gary L., 1988. Designer drugs: past history and future prospects. Journal of Forensic Science 33 (2), 569–575. [PubMed] [Google Scholar]
- Mallatt Justine 2018. The effect of prescription drug monitoring programs on opioid prescriptions and heroin crime rates, Available at SSRN 3050692.
- Marshall BDL, Yedinak JL, Goyer J, Green TC, Koziol JA, Alexander-Scott N, 2017. Development of a Statewide Publicly Accessible Drug Overdose Surveillance and Information System. American Journal of Public Health 107 (11), 1760–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars Sarah G., Rosenblum Daniel, Ciccarone Daniel, 2019. Illicit fentanyls in the opioid street market: desired or imposed? Addiction 114 (5), 774–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars Sarah G., Ondocsin Jeff, Ciccarone Daniel, 2018a. Sold as heroin: perceptions and use of an evolving drug in Baltimore** MD. Journal of Psychoactive Drugs 50 (2), 167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars SG, Ondocsin J, Ciccarone D, 2018b. Toots, tastes and tester shots: user accounts of drug sampling methods for gauging heroin potency. Harm Reduction Journal 15 (1), 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars Sarah G., Bourgois Philippe, Karandinos George, Montero Fernando, Ciccarone Daniel, 2014. Every never I ever said came true: Transitions from opioid pills to heroin injecting. International Journal of Drug Policy 25 (2), 257–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKnight C, Des Jarlais DC, 2018. Being hooked up during a sharp increase in the availability of illicitly manufactured fentanyl: Adaptations of drug using practices among people who use drugs (PWUD) in New York City. International Journal of Drug Policy 60, 82–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell JK, Matthew Gladden R, Mattson CL, Kariisa M, 2018. Overdose Deaths with Carfentanil and Other Fentanyl Analogs Detected - 10 States, July 2016 - June 2017. Morbidity and Mortality Weekly Report 67 (27), 767–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiper Nicholas C., Clarke Sarah Duhart, Vincent Louise B., Ciccarone Dan, Kral Alex H., Zibbell Jon E., 2019. Fentanyl test strips as an opioid overdose prevention strategy: findings from a syringe services program in the Southeastern United States. International Journal of Drug Policy 63, 122–128. [DOI] [PubMed] [Google Scholar]
- Rosenblum D, Unick GJ, Ciccarone D, 2014. The entry of Colombian-sourced heroin into the US market: The relationship between competition, price, and purity. International Journal of Drug Policy 25 (1), 88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhm CJ, 2018. Corrected US opioid-involved drug poisoning deaths and mortality rates, 1999–2015. Addiction 113 (7), 1339–1344. [DOI] [PubMed] [Google Scholar]
- Lawrence S, Seth P, Kariisa M, Wilson N, Baldwin G, 2019. Drug and opioid-involved overdose deaths-United States, 2013–2017. Morbidity and Mortality Weekly Report 67 (5152), 1419–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki Joji, El-Haddad Saria, 2017. A review: fentanyl and non-pharmaceutical fentanyls. Drug and Alcohol Dependence 171, 107–116. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


