Abstract
Objective:
Multiple single-center studies have reported significant reductions in major amputations among patients with diabetic foot ulcers following initiation of multidisciplinary teams. The purpose of this study was to assess the association between multidisciplinary teams (i.e., two or more types of clinicians working together) and the risk of major amputation, and to compile descriptions of these diverse teams.
Methods:
We searched PubMed, Scopus, Cumulative Index to Nursing and Allied Health, and Cochrane Central Register of Controlled Trials from inception through May 24, 2019 for studies reporting the association between multidisciplinary teams and major amputation rates for patients with diabetic foot ulcers. We included original studies if: 1) ≥50% of the patients seen by the multidisciplinary team had diabetes, 2) they included a control group, and 3) they reported the effect of a multidisciplinary team on major amputation rates. Studies were excluded if they were non-English language, abstracts only, or unpublished. We used the 5-domain Systems Engineering Initiative for Patient Safety Model, to describe team composition and function and summarized changes in major amputation rates associated with multidisciplinary team care A meta-analysis was not performed due to heterogeneity across studies, their observational designs, and the potential for uncontrolled confounding (PROSPERO no. 2017: CRD42017067915).
Results:
We included 33 studies, none of which were randomized trials. Multidisciplinary team composition and functions were highly diverse. However, four elements were common across teams: 1) Teams were composed of medical and surgical disciplines. 2) Larger teams benefitted from having a “captain” and a nuclear/ancillary team member structure. 3) Clear referral pathways and care algorithms supported timely, comprehensive care. 4) Multidisciplinary teams addressed four key tasks: glycemic control, local wound management, vascular disease, and infection. Ninety-four percent (31/33) of studies reported a reduction in major amputations following institution of a multidisciplinary team.
Conclusion:
Multidisciplinary team composition was variable, but reduced major amputations in 94% of studies. Teams consistently addressed glycemic control, local wound management, vascular disease, and infection in a timely and coordinated manner to reduce major amputation for patients with diabetic foot ulcerations. Care algorithms and referral pathways were key tools to their success.
Keywords: interdisciplinary, patient care team, healthcare team, limb salvage, limb preservation
Nearly 2 million Americans develop a diabetic foot ulcer each year; within 5 years of ulceration, 5% will undergo major amputation and 50–70% will die.1–4 Caring for patients with diabetic foot ulcer is complicated by a nexus of comorbidities including diabetes, vascular disease, neuroarthropathy, and peripheral neuropathy that cross the boundaries of usual medical or surgical care. These comorbidities, coupled with secondary infection, stymie ulcer healing, and care gaps further amplify the risk of major amputation.3,5 Experts have recommended a multidisciplinary team approach to optimally address these comorbidities in a coordinated manner and reduce major amputations.6–8
Two systematic reviews assessed the impact of multidisciplinary teams on diabetic foot ulcer outcomes.9,10 In one, three of three studies reported a decrease in major amputations.9 In the other, eight of nine reported reductions in major amputations associated with multidisciplinary team care.10 Neither of these reviews included systematic descriptions of the multidisciplinary teams.
Given the recent, global surge in multidisciplinary teams to care for patients with diabetic foot ulcers and the lack of understanding how they form and function, we conducted a systematic review using descriptive analysis of teams. In this study, we define a multidisciplinary team as two or more clinicians from different disciplines working together to care for patients with foot ulcers, where the majority of patients have diabetes. We describe consistent elements of multidisciplinary teams that may be instrumental in achieving reductions in major amputations. Descriptions may benefit clinicians who are contemplating starting a multidisciplinary clinic at their institutions, and researchers interested in interventional or comparative-effectiveness studies.
The purpose of this study is two-fold: 1) describe multidisciplinary team composition and function using a systems engineering conceptual model, and 2) summarize the impact of multidisciplinary teams on major amputations. We hypothesize that multidisciplinary teams are associated with a reduced risk of major amputation.
METHODS
We conducted this systematic review in conformity with PRISMA and MOOSE guidelines.11,12 We followed a protocol that was registered a priori with an international prospective register of systematic reviews (PROSPERO no. 2017: CRD42017067915). Because this systematic review only used results from previously published studies, it was not considered human subjects research and, as such, did not qualify for IRB review.
Search Strategy
Investigators collaborated with a medical reference librarian to develop a comprehensive search strategy using controlled vocabulary and keywords. These included: diabetic foot, foot ulcer, multidisciplinary, interdisciplinary, multispecialty, patient care team, amputation, limb salvage, and limb preservation (full search strategy available in the online Appendix, Supplemental Table I). The librarian searched the following databases from their inceptions through May 24, 2019: PubMed, Scopus, Cumulative Index to Nursing and Allied Health, and Cochrane Central Register of Controlled Trials. We augmented our database search by manually screening reference of all selected articles. We contacted corresponding authors to obtain articles that were unavailable through national and international inter-library loans. Beyond this, we had no contact with authors of identified, screened, or selected studies.
Study Selection Process
We included all original studies which met the following inclusion criteria: 1) ≥50% of the patients seen by the multidisciplinary team had diabetes, 2) included a control group, 3) reported the effect of a multidisciplinary team, defined as ≥2 types of clinicians working together, on major (above-ankle) amputation rates for patients with foot ulcers. Studies were excluded if they were written in a language other than English, published as abstracts only, or unpublished. We purposively kept our inclusion and exclusion criteria broad to encompass the experiences of as many different teams as possible and increase the generalizability of our findings. Specifically, if a group of clinicians described themselves as a team, we accepted their self-designation to capture the widest range of teams as possible. We included observational studies because these designs are more frequently used to test interventions at the system-level, rather than individual-level. Two independent reviewers screened all titles and abstracts of the identified studies for inclusion. Discrepancies were resolved by a third, independent reviewer. We repeated this process using full text articles during the second phase of screening. Three articles reported the initial effect of a single multidisciplinary team soon after team formation with more longitudinal data captured in a subsequent publication.13–18 When this occurred, we only included the article with the most longitudinal outcome data and excluded the initial article. This allowed us to give equal weights to each unique multidisciplinary team.
Theoretical Model
Prior systematic reviews did not provide descriptions of the heterogeneous teams or their functions, which we thought would be useful in understanding how multidisciplinary teams might reduce major amputation rates for patients with diabetic foot ulcers. 9,10We used the Systems Engineering Initiative for Patient Safety (SEIPS) model to systematically compile team descriptions. The SEIPS model focuses on five work system domains — people, tasks, tools and technologies, physical environment, and organizational conditions. The model describes how elements of multidisciplinary teams interact to influence processes (managing diabetic foot ulcers) and outcomes (major amputation, Figure 1).19
Figure 1.
Systems Engineering Initiative for Patient Safety (SEIPS) model, adapted to the context of multidisciplinary care teams for diabetic foot ulcers.19
Data Abstraction
The primary outcome of this review was the change in major amputation rates. We abstracted the following study attributes: publication year, design, location, sample size, length of enrollment, and whether team composition and function were reported. We abstracted the following patient attributes impacting the risk of major amputation and potentially confounding results: age, sex, race, whether a majority or all of the patients managed by the multidisciplinary team had diabetes, mean hemoglobin A1C levels, the proportion with peripheral vascular disease, the proportion with peripheral neuropathy, and whether the ulcer required hospitalization. We abstracted the following multidisciplinary team attributes, corresponding to the work system components of the SEIPS model: team composition by discipline (people); practice setting of inpatient or outpatient, and whether teams functioned in a universal healthcare system (environment); aspects of clinical care addressed (tasks); what tools and technology were used (tools and technology); and organizational changes to implement the multidisciplinary care teams (organization, Figure 1). Two reviewers independently abstracted all data using standardized, web-based forms. Reviewers met to resolve differences and clean data.
Risk of Bias Assessment
Two independent reviewers assessed the methodological quality and risk of bias for each included study using a modified Downs and Black checklist for randomized and non-randomized studies of healthcare interventions.20 Higher scores indicated higher quality studies, with a maximum modified score of 25. Scores within 3 points of each other were averaged. Otherwise, reviewers discussed discrepancies and agreed upon a final score. Studies were also assigned descriptors of study quality (excellent, good, fair, or poor) based upon the final score and previously reported ranges.21
Analysis
We created descriptions of the multidisciplinary teams using the SEIPS model; we focused on commonalities that might be necessary, core components to reduce major amputations. We constructed a summarizing Forest plot of all studies reporting odds ratios, or raw data from which odds ratios could be calculated. We also tabulated studies reporting population-based incidence rates and reported results from papers reporting high-to-low amputation ratios. A meta-analysis was not performed due to heterogeneity across studies, their observational designs, and the potential for uncontrolled confounding that might significantly bias the resulting summary statistic.
RESULTS
Our search identified 1047 distinct articles, of which 605 were excluded during title and abstract screening. The remaining 442 full-text articles were reviewed, and 33 met inclusion criteria (Figure 2).
Figure 2.
PRISMA diagram for inclusion and exclusion of studies
Study Characteristics
All 33 studies were observational, with global center representation (Table I). No randomized trials met our inclusion criteria. Twenty-six (73%) included at least 50 patients treated by their respective multidisciplinary teams.14,24–46 Length of enrollment varied greatly among the 21 studies (64%) that reported it, in terms of calendar time or time to clinical endpoints.14,17,24–32,34,36–38,40,43,44,47–49 Some studies, often those using a historically controlled (pre-post design) had unclear follow-up (Table II, with brief case and control descriptions available in the online Appendix, Supplemental Table II). The mean bias score was 15.3 (SD 1.9), and most studies (82%) ranked fair. Lack of randomization and blinding— at the level of patients, providers, and researchers—commonly detracted from study quality.
Table I.
Characteristics of the 33 included studies
| Study Characteristic | N (%) | |
|---|---|---|
| Publication Date | Before 1990 | 0 |
| 1990 – 1999 | 3 (9) | |
| 2000 – 2009 | 8 (24) | |
| 2010 - February 2019 | 22 (67) | |
| Design* | Historically controlled (pre-post) | 26 (76) |
| Retrospective cohort | 4 (12) | |
| Prospective cohort | 2 (6) | |
| Case-controlled | 2 (6) | |
| Randomized controlled | 0 | |
| Location | Europe | 18 (55) |
| South America, Asia, or Africa | 8 (24) | |
| North America | 5 (15) | |
| Australia | 2 (6) | |
| Number of patients (multidisciplinary care) | 0 – 24 | 0 (0) |
| 25 – 49 | 2 (6) | |
| 50 – 74 | 6 (18) | |
| 75 – 100 | 2 (6) | |
| >100 | 18 (55) | |
| Unknown | 5 (15) | |
| Length of enrollment | Unknown | 12 (36) |
| Until hospital discharge | 7 (21) | |
| Until ulcer healed/major amputation | 5 (15) | |
| Other | 9 (27) | |
| Bias score | 22 – 25 (excellent) | 0 (0) |
| 17 – 21 (good) | 4 (12) | |
| 12 – 16 (fair) | 27 (82) | |
| <12 (poor) | 2 (6) | |
The n for Study Design totals 34, rather than 33, because one study used both a case-control design and a retrospective cohort design. We counted it in both categories.24
Table II.
Study Descriptions
| Study | Bias Score |
Study Design | Follow up | |||||
|---|---|---|---|---|---|---|---|---|
| Prospective cohort |
Retrospective cohort |
Case-control | Historically controlled (pre-post) |
|||||
| Chung 2015 | 20 | X | Median 539 days (IQR 314 +/− 679) | |||||
| Weck 2013 | 18.5 | X | 730 days | |||||
| Laakso 2016 | 17.5 | X | Unclear | |||||
| Chiu 2011 | 17 | X | Until wound healing or amputation | |||||
| Riaz 2019 | 16.5 | X | Unclear | |||||
| Kim 2018 | 16.5 | X | Unclear | |||||
| Crihana 2014 | 16.5 | X | Duration of admission | |||||
| Setacci 2013 | 16.5 | X | 182 days | |||||
| Alexandrescu 2009 | 16.5 | X | Mean: 700 days (range 30 – 2040 days) | |||||
| Martinez- | 16 | X | Inpatient followed until discharge; outpatient and | |||||
| Gómez 2014 | inpatient followed for 730 days after admission | |||||||
| Yesil 2009 | 16 | X | 300 days after discharge | |||||
| Hedetoft 2009 | 16 | X | Unclear | |||||
| Rerkasem 2008 | 16 | X | Unclear | |||||
| Dargis 1999 | 16 | X | 730 days | |||||
| Jiménez 2017 | 15.5 | X | Until ulcer healing, sometimes longer on case-by-case basis | |||||
| Wang 2016 | 15.5 | X | Duration of hospitalization | |||||
| Plusch 2015 | 15.5 | X | Duration of hospitalization | |||||
| Cahn 2014 | 15.5 | X | Duration of hospitalization | |||||
| Denjalic 2014 | 15 | X | Followed until ulcer healing (did not follow for recurrence) | |||||
| Nather 2010 | 15 | X | Duration of admission and follow up care for surgical intervention (length of stay average 10.81–20.36 days) | |||||
| Crane 1999* | 15 | X | Duration of admission | |||||
| Hsu 2015 | 14.5 | X | Until wound healed | |||||
| Armstrong 2012 | 14.5 | X | Through wound healing, surgical post-operative care, metabolic control, and others. Timing was not reported. | |||||
| Witsø 2010 | 14.5 | X | Unclear | |||||
| Aydin 2010 | 14.5 | X | Duration of hospitalization (mean length of stay 26.9 days) | |||||
| Meltzer 2002 | 14.5 | X | Between 1 day and 1095 days, but poorly defined | |||||
| Anichini 2007 | 14 | X | Unclear | |||||
| Nason 2013 | 13.5 | X | Unclear, LOS reported for those who were hospitalized | |||||
| Holstein 2000 | 2000 | X | Until 1996 | |||||
| Gibbons 1993 | X | 365 days | ||||||
| Troisi 2016 | 11.5 | X | Unclear | |||||
| McGill 2003 | X | Unclear | ||||||
Patient Characteristics
All but two multidisciplinary teams exclusively treated those with diabetes.16,47 Most studies (22/33, or 67%) limited their recruitment to patients with ulcers severe enough to warrant hospitalization.14,24–28,30,32–34,36,38–41,43–45,47,49–51 Six studies further restricted to those requiring either revascularization, major or minor amputation, or plastic surgery reconstruction.26,32,36,38,47,50
When reported, patient characteristics were generally well balanced between those who received multidisciplinary care and those who did not. The mean patient age ranged from 56 to 76 years.14,17,24–34,38,39,41,43–47,49–51 Men composed 34–100% of patients.14,17,24–27,29–34,38–41,43–47,49,50 Five studies reported patient race; four included predominantly (>80%) white patients, and one included 100% Asian patients.14,16,29,31,51 The proportion of patients with peripheral vascular disease ranged from 42–100%.14,27,28,31–33,38,43,45–47,49,50 Three studies were entirely comprised of patients with peripheral vascular disease.27,38,47 The proportion of patients with peripheral neuropathy ranged from 64–100%.14,28,30,38,43,45,46,49,50 In the eleven studies reporting mean hemoglobin A1C values, two were less than 8%.25,28,32,33,43,45–47,49–51
Multidisciplinary Team Characteristics
People:
Team composition was highly heterogeneous, with 36 different disciplines represented on the 27 teams reporting their members.14,16,17,28–48,50–52 The average team included physicians from 5 distinct disciplines (range 3–9 physician disciplines/team). Typically, larger teams were divided into a nuclear team led by two or three physicians and ancillary team members called upon as needed. Some studies stressed that it was important to identify a team “captain” to coordinate efforts.16,32,36 Another large team reported a “learning curve,” as teamwork improved and major amputation rates fell over time.38
All but one team included physicians from medical and surgical disciplines (Table III). Endocrinology was the most common medical specialty (82%). To a lesser extent, infectious disease (37%), general medicine (30%), and physical medicine and rehabilitation (22%) specialists were involved. Most teams (85%) included two or more surgical specialties.14,16,17,29–33,35–44,47,48,50–52 Peripheral vascular surgery was the most common surgical specialty (74%), although orthopedic surgery (67%), podiatry (52%), and plastic surgery (44%) were involved frequently.
Table III.
Multidisciplinary team compositions.
| Study | Bias Score(1) |
OR for change in major amputation rate following multidisciplinary care |
Physician Disciplines | Nursing (3) & Allied Health Professionals |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medical | Surgical |
Other (2) |
|||||||||||||
| Endocrinology | General Medicine |
Infectious Disease |
PM&R | General Surgery |
Orthopedics | Vascular Surgery |
Plastic Surgery |
Podiatry | Nursing | Orthotics | Other (4) | ||||
| Chung 2015 | 20 | 0.45 (0.16, 1.24) | X | X | X | X | X | X | X | ||||||
| Weck 2013 | 18.5 | 0.28 (0.20, 0.40) | X | X | X | ||||||||||
| Laakso 2017 | 17.5 | 0.47 (0.27, 0.82) | X | X | X | X | X | X | |||||||
| Chiu 2011 | 17 | 0.09 (0.03, 0.29) | X | X | X | ||||||||||
| Alexandrescu 2009 | 16.5 | 0.47 (0.20, 1.08) | X | X | X | X | X | X | X | X | X | X | |||
| Crihana 2014 | 16.5 | 0.25 (0.07, 0.90) | X | X | X | X | X | ||||||||
| Kim 2018 | 16.5 | 1.14(0.59, 2.20) | X | X | X | ||||||||||
| Riaz 2019 | 16.5 | 0.29 (0.20, 0.42) | X | X | X | X | X | ||||||||
| Dargis 1999 | 16 | 0.39(0.04, 3.55) | X | X | X | X | X | ||||||||
| Hedetoft 2009 | 16 | * | X | X | X | X | |||||||||
| Martinez-Gómez 2014 | 16 | 0.47 (0.33, 0.68) | X | X | X | X | X | X | X | ||||||
| Rerkasem 2008 | 16 | 0.27 (0.08, 0.97) | X | X | X | X | X | X | |||||||
| Williams 2018 | 16 | −368/100,000 | X | X | X | X | X | ||||||||
| Yesil 2009 | 16 | 0.56 (0.34, 0.93) | X | X | X | X | X | X | X | X | X | X | |||
| Cahn 2014 | 15.5 | 0.49 (0.25, 0.94) | X | X | X | X | X | ||||||||
| Wang 2016 | 15.5 | 0.27 (0.13, 0.57) | X | X | X | X | X | X | |||||||
| Jiménez 2017 | 15.5 | −1.6/100,000/year | X | X | X | X | X | X | X | X | X | ||||
| Nather 2010 | 15 | 0.37 (0.21, 0.66) | X | X | X | X | X | X | X | X | |||||
| Armstrong 2012 | 14.5 | ** | X | X | X | X | X | ||||||||
| Aydin 2010 | 14.5 | 0.53 (0.25, 1.15) | X | X | X | X | X | X | |||||||
| Hsu 2015 | 14.5 | 0.28 (0.13, 0.60) | X | X | X | X | X | X | X | X | X | ||||
| Meltzer 2002 | 14.5 | 0.16 (0.07, 0.37) | X | X | X | X | X | ||||||||
| Witsø 2010 | 14.5 | −160/100,000/year | X | X | X | X | X | X | X | X | |||||
| Anichini 2007 | 14 | −3.2/100,000 | X | X | X | X | X | X | |||||||
| Holstein 2000 | 13.5 | −20.3/100,000 | X | X | X | X | X | X | |||||||
| Nason 2013 | 13.5 | 0.61 (0.23, 1.62) | X | X | X | X | X | ||||||||
| McGill 2003 | 9.5 | 0.19 (0.13, 0.27) | X | X | X | X | X | ||||||||
| Total (%) | 22 (82) |
8 (30) |
10 (37) |
6 (22) |
6 (22) |
18 (67) |
20 (74) |
12 (44) |
14 (52) |
14 (52) |
15 (56) |
8 (30) |
8 (30) |
||
Studies are ordered based on bias scores, with higher quality studies listed first.
Other physician-based disciplines included: anesthesiology & pain services, cardiology, cardiovascular surgery, dermatology, emergency medicine, interventional angiography, microbiology, neurology, psychology, and radiology
Nursing disciplines spanned: general nursing, nurse case management, diabetic foot nursing, vascular nursing, and wound care nursing
Other allied health professions included: diabetes educators, medical quality, nutrition, occupational therapy, pharmacy, physical therapy, plaster technicians, prothestics, and social work
Hedetoft and colleagues reported an increase in the high-to-low (major-to-minor) amputation ratio from 0.46 to 0.55 following introduction of a multidisciplinary team.
Armstrong and colleagues reported a reduction in the high-to-low (major-to-minor) amputation ratio from 0.35 to 0.27 following introduction of a multidisciplinary team.
In general, the roles of nurses and allied health professionals were less well documented. Team tasks, such as use of negative pressure wound therapy and casting, suggest these disciplines were under reported. The involvement of nurses was explicitly stated in 15 studies (56%), including general nursing, wound care nursing, and nurse case management.14,16,31,35,37–39,42–44,46,48,50–52 The contributions of allied health professionals were cited in 14 studies (52%), with even broader discipline involvement: casting, diabetes education, medical quality, nutrition, occupational therapy, orthotics, pharmacy, physical therapy, prosthetics, and social work.29–31,34,36–38,40,43,44,47,48,51,52 Of these, orthotics was the allied health professional discipline most commonly included on teams (8/28, or 30%).
Tasks:
Despite varied compositions, teams consistently addressed four key clinical tasks: glycemic control, local wound management, vascular disease, and infection (Table IV). Twenty-six teams (79%) addressed three or more of these key factors. Regarding local wound management, most (29/32, 91%) were able to surgically debride and perform minor amputations, in addition to non-surgical interventions such as bedside debridement and off-loading.14,16,17,25,27–48,50–52 When addressing vascular disease, most teams (24/32, 75%) were able to revascularize patients as needed, in addition to performing diagnostic testing and medical management.14,16,17,26–28,31,32,35–41,43–48,51–53 Tasks associated with medical management of vascular disease, such as diagnosis and treatment of dyslipidemias, anti-platelet therapy, and smoking cessation were not well described in the majority of the articles. Only one mentioned smoking cessation as an explicit task.40 Eleven teams directly addressed patient education.24,29,35–37,39,40,44,48,51,52 One study commented that team members would reinforce each other’s recommendations, sending a consistent message and increasing patient adherence.50
Table IV.
Four key clinical tasks addressed by multidisciplinary teams
| Study | Bias score (1) |
OR for major amputation |
Key clinical task | # tasks addressed |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Glycemic control |
Wound care | Infection | Vascular Disease | ||||||
| Surgical | Non-surgical | Revascularization | Diagnostic/ Medically managed |
||||||
| Chung 2015 | 20 | 0.45 (0.16, 1.24) | X | X | X | X | X | X | 4 |
| Weck 2013 | 18.5 | 0.28 (0.20, 0.40) | X | X | X | X | X | 4 | |
| Laakso 2017 | 17.5 | 0.47 (0.27, 0.82) | X | X | X | X | X | X | 4 |
| Chiu 2011 | 17 | 0.09 (0.03, 0.29) | X | X | X | X | X | 3 | |
| Alexandrescu 2009 | 16.5 | 0.47 (0.20, 1.08) | X | X | X | X | X | X | 4 |
| Crihana 2014 | 16.5 | 0.25 (0.07, 0.90) | X | X | X | X | X | 4 | |
| Setacci 2013 | 16.5 | 0.70 (0.50, 0.96) | X | X | X | X | X | 3 | |
| Kim 2018 | 16.5 | 1.14 (0.59, 2.20) | X | X | X | X | X | 3 | |
| Riaz 2019 | 16.5 | 0.29 (0.20, 0.42) | X | X | X | X | X | 3 | |
| Dargis 1999 | 16 | 0.39 (0.04, 3.55) | X | X | X | X | 3 | ||
| Hedetoft 2009 | 16 | * | X | X | X | 2 | |||
| Martinez-Gómez 2014 | 16 | 0.47 (0.33, 0.68) | X | X | X | X | X | 4 | |
| Rerkasem 2008 | 16 | 0.27 (0.08, 0.97) | X | X | X | X | X | 3 | |
| Williams 2018 | 16 | −368/100,000 | X | X | X | X | 2 | ||
| Yesil 2009 | 16 | 0.56 (0.34, 0.93) | X | X | X | X | X | X | 4 |
| Cahn 2014 | 15.5 | 0.49 (0.25, 0.94) | X | X | X | X | 3 | ||
| Wang 2016 | 15.5 | 0.27 (0.13, 0.57) | X | X | X | X | X | 3 | |
| Jiménez 2017 | 15.5 | −1.6/100,000/yr | X | X | X | X | X | X | 4 |
| Crane 1999 | 15 | 0.30 (0.10, 0.92) | X | X | 2 | ||||
| Denjalic 2014 | 15 | 0.49 (0.30, 0.78) | X | X | X | X | 3 | ||
| Nather 2010 | 15 | 0.37 (0.21, 0.66) | X | X | X | X | X | X | 4 |
| Armstrong 2012 | 14.5 | ** | X | X | X | X | X | 3 | |
| Aydin 2010 | 14.5 | 0.53 (0.25, 1.15) | X | X | X | X | X | X | 4 |
| Hsu 2015 | 14.5 | 0.28 (0.13, 0.60) | X | X | X | X | X | 3 | |
| Meltzer 2002 | 14.5 | 0.16 (0.07, 0.37) | X | X | X | X | X | X | 4 |
| Witsø 2010 | 14.5 | −160/100,000/yr | X | X | X | X | X | X | 4 |
| Anichini 2007 | 14 | −3.2/100,000 | X | X | X | X | X | 3 | |
| Gibbons 1993 | 13.5 | 0.22 (0.10, 0.47) | X | X | X | 2 | |||
| Holstein 2000 | 13.5 | −20.3/100,000 | X | X | X | X | X | X | 4 |
| Nason 2013 | 13.5 | 0.61 (0.23, 1.62) | X | X | X | X | X | X | 4 |
| Troisi 2016 | 11.5 | −8.8/100,000 | X | X | 1 | ||||
| McGill 2003 | 9.5 | 0.19 (0.13, 0.27) | X | X | X | 2 | |||
| Total (%) | 27 (84) | 28 (88) | 29 (91) | 20 (63) | 24 (75) | 27 (84) | Mean= 3.22 | ||
Studies are ordered based on bias scores, with higher quality studies listed first.
Hedetoft and colleagues reported a reduction in the high:low (major:minor) amputation ratio from 0.56 to 0.46 following introduction of a multidisciplinary team.
Armstrong and colleagues reported a reduction in the high:low (major:minor) amputation ratio from 0.35 to 0.27 following introduction of a multidisciplinary team.
Studies stressed that individual tasks performed by multidisciplinary teams could, and often did, happen in standard practice. However, performing all tasks for all patients, especially in a coordinated and expedited manner, was not facilitated using the standard practice model. Multidisciplinary teams credited their improved outcomes to the combination of 1) consistently and synchronously addressing all contributing factors, and 2) providing timely 15 care.16,27,32,35,39,41,48,50
Teams held standing meetings or rounded together to coordinate and expedite care. Typically, meetings were held weekly.27,33,41,43,47 Some larger teams met weekly with the nuclear team and convened the whole team less frequently.33,41 One team stressed “Continuous Multidisciplinary Activity,” or daily interactions between team members to improve multidisciplinary work beyond meetings.16 In addition to focusing on individual patient care, meetings were used to address access and resource allocation.39 One team dedicated a portion of these meetings to review the care plans of high-utilization patients.16
Tools and Technology:
Teams used basic tools to assist with communication and coordination, not advanced technology. The most common tool was a care algorithm.24–28,30–32,34,39,43,45,46,48 This tool helped ensure teams were providing comprehensive care in an agreed upon order, by designated disciplines. Usually, care algorithms were constructed with input from team members prior to initiating multidisciplinary team care.31,34,39,46,48 Algorithms varied greatly in the amount of detail and complexity they contained, with more detailed and complex algorithms tending to be more prescriptive 24–28,30–32,34,39,43,45,46,48 One team used existing guidelines as a general framework, tailoring details to their specific team and system.17 Another stressed innovation when designing their algorithm, an approach which resulted in a combined group- and home-based patient educational program they thought was much more effective than their previous standard lectures and pamphlets.39 Another used the algorithm to not only address physiological factors but facilitate inpatient-to-outpatient transitions.28 One team designated a nurse to implement the algorithm and track patients’ care through them.39 Another used patient-tailored care algorithms as a metric of accountability among team members.33 Tools utilized less frequently included: standardized documentation templates and order sets, antibiotic algorithms, and patient pamphlets.39,43,44,52
Within individual disciplines, advanced technologies were employed. These included endovascular revascularization protocols, advanced plastic surgery closures, and wound vacuums.26,30,32,38
Environment:
Teams functioned in inpatient (9, 27%),14,24–26,33,37,41,44,45 outpatient (6, 18%),29,31,35,46,49,52 or both settings (18, 55%).16,17,27,28,30,32,34,36,38–40,42,43,47,48,50,51,53 Some described starting in either the inpatient or outpatient setting and then expanding to encompass both as their teams became more established. This facilitated continuity of care, which the multidisciplinary teams highly valued.43 When caring for inpatients, co-locating patients on the same ward facilitated team rounding.33,43 Most studies (28/33, 85%) took place within universal healthcare systems.14,16,17,25,27–30,32,34,35,37–44,48–53
Organization:
Teams worked with existing resources and focused on changing system organization to improve patient outcomes.39,41,46 Before initiating multidisciplinary team care, organizational changes focused on two areas: within-team organization, and the interface between the team and other healthcare providers. Within-team organizational change included developing care algorithms and rules of conduct between team members, including: who would “captain” the team, which discipline would serve as the primary admitting service, and how consults would be called.16,32,34,36,39,44,48 Two outpatient teams grouped patients who required surgical consultation on the same day, increasing the efficient consultation of ancillary, surgical team members.40,42 Two teams incorporated a priori systems for improvement, either through annual audit-and-feedback or a patient registry.34,48
Prior to initiating care, multidisciplinary teams met with specialists and primary care providers within their healthcare systems to establish clear referral pathways.16,17,27,28,35,42,50,52,53 Consensus among specialists was needed so that patients referred to specialists who were not part of the multidisciplinary team would be redirected to the team.42,52 Meetings with primary care providers focused on advertising the multidisciplinary teams and introducing referral pathways. 16,28,35,42,52 Rapid triage was emphasized. One team guaranteed new patient evaluation within 24 hours.35 Others developed telephone triage lines for referring providers so that new patients could be seen in an appropriate timeframe and setting (e.g. outpatient clinic or hospital admission).16,27 Recognizing that the specialists involved in these multidisciplinary teams were a limited resource, some teams focused on educating primary care providers on how to care for less complicated diabetic foot ulcers so that the multidisciplinary teams could focus on patients with severe ulcerations.35,53 These efforts included clear parameters to refer to specialty care and pre-referral work-ups.35 Two teams noted a steady increase in referrals over time, which expanded outside initial catchment areas.16,52
Major Amputation Rates
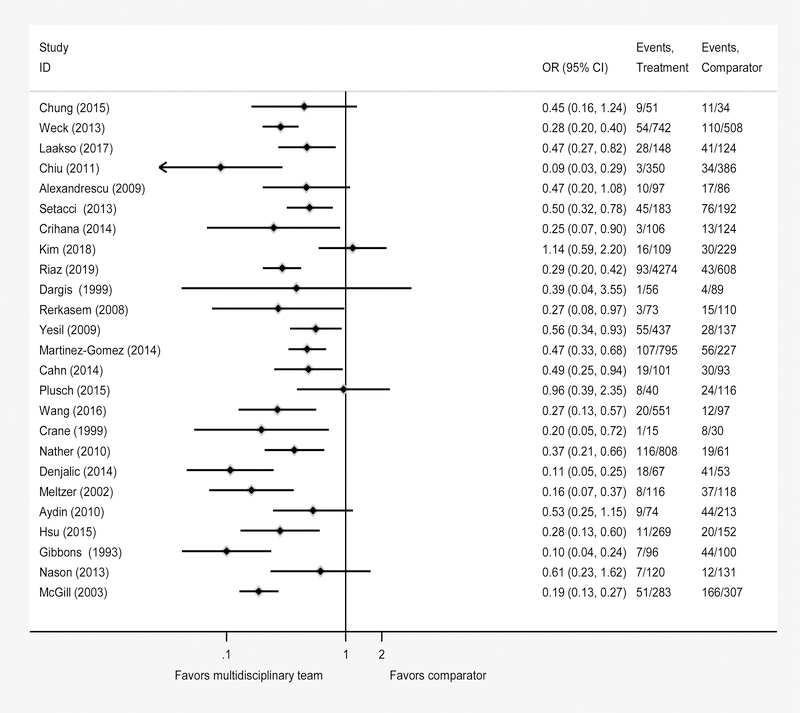
All but two studies (31/33, or 94%) reported a decrease in major amputations associated with multidisciplinary teams. Twenty-five studies reported odds ratios, or raw data from which odds ratios could be calculated.14,24–34,38–49,51 Of these, the absolute percent change in major amputations associated with multidisciplinary teams ranged from a 2% increase45 (OR 1.14, 95% CI 0.59–2.20) to a 51% absolute or 89% relative reduction (OR 0.11, 95% CI 0.05–0.25; Figure 3).25 Six studies reported changes in incidence rates;16,17,35,37,52,53 all of these took place within national healthcare systems, involved stable populations, and reported decreases in major amputation rates associated with multidisciplinary teams (Table V). Two studies used the high-to-low (major-to-minor) amputation ratio.36,50 One of these reported a decrease from 0.35 to 0.27 following introduction of a multidisciplinary care team.36 The other reported an increase from 0.46 to 0.55.50
Figure 3.
Forest plot of the estimated odds ratios for the change in major amputation rates following initiation of multidisciplinary care compared to standard care for 25 of the 33 included studies for which odds ratios could be calculated.
Table V.
Decrease in incidence rates of major amputations associated with multidisciplinary teams for patients with diabetic foot ulcers
| Study, Country | Bias score (1) |
Incidence of major amputation /100,000 inhabitants with diabetes Controls |
Incidence of major amputation/100,000 inhabitants with diabetes Multidisciplinary Teams |
Decrease in incidence with multidisciplinary teams |
|---|---|---|---|---|
| Williams 2018, United Kingdom | 16 | 412* | 44* | 368* |
| Jiménez 2017, Spain | 15.5 | 6.1** | 4.5** | 1.6** |
| Witsø 2010, Norway | 14.5 | 400*** | 240*** | 160*** |
| Anichini 2007, Italy | 14 | 6.3 | 3.1 | 3.2 |
| Holstein 2000, Denmark | 13.5 | 27.2 | 6.9 | 20.3 |
| Troisi 2016, Italy | 11.5 | 37.5 | 28.7 | 8.8 |
Studies are ordered based on bias scores, with higher quality studies listed first.
Williams and colleagues expressed the incidence of major amputation based on 100,000 inhabitants with diabetes, adjusted for age and sex.
Jiménez and colleagues expressed the incidence of major amputation based on 100,000 general inhabitants per year.
Witsø and colleagues expressed the incidence of major amputation based on 100,000 inhabitants with diabetes per year.
DISCUSSION
Despite heterogeneous team composition and function, multidisciplinary teams are associated with significant reductions in major amputations for patients with diabetic foot ulcers. Although we were unable to perform a meta-analysis, the direction of the association between multidisciplinary teams and major amputation is clear. Thirty-one of 33 studies found multidisciplinary teams were associated with fewer major amputations for patients with diabetic foot ulcers. Consistent reductions in major amputations across studies and diverse teams also contribute to the robustness of the finding. Multidisciplinary teams embedded in a variety of healthcare systems and composed of different provider combinations were able to reduce major amputations by collaboratively and efficiently addressing underlying factors.
Multidisciplinary team care is an effective strategy for the highest risk patients, especially those with 1) ulcers severe enough to warrant hospitalization, and 2) underlying peripheral vascular disease (i.e. the majority of patients served by multidisciplinary teams included in this review). It is consistent with expert opinion guidelines suggesting a tiered approach to care based on ulcer severity.7,54,55 In this model, primary care is responsible for preventing foot ulcers. Relatively straightforward ulcers can be managed locally with collaboration between primary care and populous specialties with wide geographic distributions, such as podiatry. Large multidisciplinary teams, like those included in this review, are in tertiary care centers and reserved for patients with severe ulcers. This model depends on effective triage so that patients receive the appropriate level of care.56
Our review includes descriptions of how multidisciplinary teams integrate into their broader healthcare organizations and provides evidence to support aspects of this tiered model. Teams educated primary care providers and other local healthcare professionals to screen and care for patients with minimally complex ulcers. They also focused on streamlined triage into their highly-specialized multidisciplinary teams for patients with severe ulcers. These results support health services research within the U.S. and England demonstrating decreased major amputation rates in systems with effective referral pathways.57,58 What is lacking is an understanding of how best to leverage these resource-intense, multidisciplinary teams. Subsequent investigations should focus on identifying the severity threshold for initiating multidisciplinary team care, which is likely to fluctuate based on available resources.
We were able to identify common elements of successful multidisciplinary teams using a health systems engineering conceptual model. Commonalities between these successful teams are important to identify because they may represent core elements, or facets of multidisciplinary team care that are necessary to reduce major amputations.59 Clinicians starting a multidisciplinary team may want to incorporate these elements, and researchers may opt to investigate which common elements are necessary, core elements, for success. With this in mind, we noted the following. 1) Teams were composed of medical and surgical disciplines. 2) Larger teams benefitted from having a “captain” and a nuclear/ancillary team member structure. 3) Clear referral pathways and care algorithms supported timely, comprehensive care. Each of the preceding elements addressed work system conditions that enabled the multidisciplinary teams to perform their tasks consistently, collaboratively, and rapidly. 4) Multidisciplinary teams addressed four key tasks: glycemic control; local wound management, including surgical debridement and minor amputation; diagnosis and management of vascular disease, including revascularization; and diagnosis and management of infection. Prior studies also suggested coordination facilitated by referral pathways and care algorithms (consistent element 3), as well as comprehensively addressing all comorbidities contributing to ulceration (consistent element 4), are tactics used by teams to reduce major amputation rates.57,60
The most notable limitation of our study is the quality of included studies, with the majority being ranked fair. This precluded our ability to perform a meta-analysis. It also introduced potential bias favoring multidisciplinary teams. Most studies used a historically controlled (pre-post) design, with controls receiving care before cases. In some studies, this difference was substantial and may have biased results; the formation of a multidisciplinary team may have occurred soon after increased utilization of endoscopic revascularizations or other advanced technologies. These technologies may have partially accounted for reductions in major amputations that were attributed solely to the multidisciplinary team. However, we do not think that this could entirely account for our findings as some studies utilized more robust designs, and some historically controlled (pre-post) studies took place over relatively brief periods where secular trends would be less influential. Another concern is that, as teams’ reputations and capacities increased, they cared for patients with less severe ulcers than controls. This may bias results towards multidisciplinary care, depending on how controls were selected. However, this potential bais should not exist in the six population-based studies, all of which reported a decreased incidence of major amputation following institution of multidisciplinary teams (Table V). We understand that studies of major shifts in care delivery, such as new multidisciplinary teams, are difficult to design. Treatment diffusion and lack of blinding make controlled study designs difficult. A step-wise wedge approach may offer a viable and ethically appropriate option.61 Pre/post study design using historical controls can improve rigor using interrupted time series analysis.62 We would welcome future studies incorporating these methods. In addition to improving study design, adjusting for confounders with multivariate statistical modeling would have improved study quality. All reported odds ratios were unadjusted, raising the potential that differences in comorbidities between treatment and control groups could confound results. This concern is somewhat assuaged by generally well balanced treatment and control groups, among those studies reporting comorbidities. Another limitation was the exclusion of non-English language articles, although our intent was to perform a systematic review that would best inform efforts to improve the care of patients with diabetic foot ulcers in the United States. The global representation of English-language articles speaks to the widespread uptake of multidisciplinary team care for patients with diabetic foot ulcers. Our search identified 115 non-English language studies, some of which may have met the remaining inclusion criteria and reported a negative association between multidisciplinary teams and major amputation. Our results should be applied cautiously to settings outside of Europe and North America, where the excluded, non-English speaking articles may be more relevant. Finally, publication bias may have resulted in an overly favorable conclusion that multidisciplinary teams reduce the risk of major amputation for patients with diabetic foot ulcer.
CONCLUSION
Multidisciplinary teams— especially those able to address glycemic control, local wound management, vascular disease, and infection— are associated with a reduce the risk of major amputation for patients with severe diabetic foot ulcerations. Further studies are needed to clarify core elements of these teams and the thresholds of patient severity served by these resource- intense, highly effective teams.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to thank Stephen Johnson and Mary Hitchcock, research librarians at the University of Wisconsin School of Medicine and Public Health Ebling Library, for assisting us in developing our search strategy and for performing searches. BLS, SK, and MBB received funding through the National Institutes of Health and the University of Wisconsin Institute for Clinical and Translational Research to conduct this study (NIH UL1TR000427 and NIH KL2TR000428).
This study was presented, in part, at a poster session at 2018 IDWeek, San Francisco, California, October 3–7, 2018.
REFERENCES
- 1.Margolis DJ, Malay DS, Hoffstad OJ, Leonard CE, MaCurdy T, de Nava Karla López, et al. Incidence of diabetic foot ulcer and lower extremity amputation among Medicare beneficiaries, 2006 to 2008: Data Points #2. Data Points Publication Series; Rockville (MD); 2011. [PubMed] [Google Scholar]
- 2.Brennan MB, Allen GO, Ferguson PD, McBride JA, Crnich CJ, Smith MA. The association between geographic density of infectious disease physicians and limb preservation in patients with diabetic foot ulcers. Open Forum Infect Dis 2017;4:ofx015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brennan MB, Hess TM, Bartle B, Cooper JM, Kang J, Huang ES, et al. Diabetic foot ulcer severity predicts mortality among veterans with type 2 diabetes. J Diabetes Complica tions 2017;31:556–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walsh JW, Hoffstad OJ, Sullivan MO, Margolis DJ. Association of diabetic foot ulcer and death in a population-based cohort from the United Kingdom. Diabet Med. 2016;33:1493–8. [DOI] [PubMed] [Google Scholar]
- 5.Prompers L, Schaper N, Apelqvist J, Edmonds M, Jude E, Mauricio D, et al. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study. Diabetologia 2008;51:747–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fitzgerald RH, Mills JL, Joseph W, Armstrong DG. The diabetic rapid response acute foot team: 7 essential skills for targeted limb salvage. Eplasty 2009;9:e15. [PMC free article] [PubMed] [Google Scholar]
- 7.Rogers LC, Andros G, Caporusso J, Harkless LB, Mills JL Sr, Armstrong DG. Toe and flow: essential components and structure of the amputation prevention team. J Vasc Surg 2010;52:23S–27S. [DOI] [PubMed] [Google Scholar]
- 8.Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJ, Armstrong DG, et al. 2012. Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis 2012;54:e132–73. [DOI] [PubMed] [Google Scholar]
- 9.Khan N, Sapsed S Diabetes foot complication: assessing primary and secondary outcomes of multidisciplinary team versus standard care (a systematic review). Int J Diabetes Dev Ctries 2017;37:129–36. [Google Scholar]
- 10.Buggy A, Moore Z. The impact of the multidisciplinary team in the management of individuals with diabetic foot ulcers: a systematic review. J Wound Care 2017;26:324–39. [DOI] [PubMed] [Google Scholar]
- 11.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [PMC free article] [PubMed] [Google Scholar]
- 13.Aksoy DY, Gurlek A, Cetinkaya Y, Oznur A, Yazici M, Ozgur F, et al. Change in the amputation profile in diabetic foot in a tertiary reference center: efficacy of team working. Exp Clin Endocrinol Diabetes 2004;112:526–30. [DOI] [PubMed] [Google Scholar]
- 14.Aydin K, Isildak M, Karakaya J, Gurlek A. Change in amputation predictors in diabetic foot disease: effect of multidisciplinary approach. Endocrine 2010;38:87–92. [DOI] [PubMed] [Google Scholar]
- 15.Williams DT, Majeed MU, Shingler G, Akbar MJ, Adamson DG, Whitaker CJ. A diabetic foot service established by a department of vascular surgery: an observational study. Ann Vasc Surg 2012;26:700–6. [DOI] [PubMed] [Google Scholar]
- 16.Williams DT, Powell-Chandler A, Qureshi Q, Zaidi A, Whitaker CJ. Improved limb salvage for patients with vascular disease and tissue loss associated with new model of provision targeted at the diabetic foot. Diabetes Res Clin Pract 2018;135:50–7. [DOI] [PubMed] [Google Scholar]
- 17.Jiménez S, Rubio JA, Álvarez J, Ruiz-Grande F, Medina C. Trends in the incidence of lower limb amputation after implementation of a Multidisciplinary Diabetic Foot Unit. Endocrinol Diabetes Nutr 2017;64:188–97. [DOI] [PubMed] [Google Scholar]
- 18.Rubio JA, Aragón-Sánchez J, Jiménez S, Guadaliz G, Albarracín A, Salido C, et al. Reducing major lower extremity amputations after the introduction of a multidisciplinary team for the diabetic foot. Int J Low Extrem Wounds 2014;13:22–6. [DOI] [PubMed] [Google Scholar]
- 19.Carayon P, Schoofs Hundt A, Karsh BT, Gurses AP, Alvarado CJ, Smith M, et al. Work system design for patient safety: the SEIPS model. QualSaf Health Care 2006;15:i50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hooper P, Jutai JW, Strong G, Russell-Minda E. Age-related macular degeneration and low-vision rehabilitation: a systematic review. Can J Ophthalmol 2008;43:180–7. [DOI] [PubMed] [Google Scholar]
- 22.Hingorani A, LaMuraglia GM, Henke P, Meissner MH, Loretz L, Zinszer KM, et al. The management of diabetic foot: A clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg. 2016;63:3S–21S. [DOI] [PubMed] [Google Scholar]
- 23.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- 24.Crane M, Werber B. Critical pathway approach to diabetic pedal infections in a multidisciplinary setting. J Foot Ankle Surg 1999;38:30–3. [DOI] [PubMed] [Google Scholar]
- 25.Denjalić A, Beĉulić H, Jusić A, Beĉulić L. Evaluation of the surgical treatment of diabetic foot. Med Glas (Zenica) 2014;11:307–12. [PubMed] [Google Scholar]
- 26.Gibbons GW, Marcaccio EJ Jr., Burgess AM, Pomposelli FB Jr, Freeman DV, Campbell DR, et al. Improved quality of diabetic foot care, 1984 vs 1990. Reduced length of stay and costs, insufficient reimbursement. Arch Surg 1993;128:576–81. [DOI] [PubMed] [Google Scholar]
- 27.Setacci C, Sirignano P, Mazzitelli G, Setacci F, Messina G, Galzerano G, et al. Diabetic foot: surgical approach in emergency. Int J Vasc Med 2013;2013:296169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weck M, Slesaczeck T, Paetzold H, Muench D, Nanning T, von Gagern G, et al. Structured health care for subjects with diabetic foot ulcers results in a reduction of major amputation rates. Cardiovasc Diabetol 2013;12:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dargis V, Pantelejeva O, Jonushaite A, Vileikyte L, Boulton AJ. Benefits of a multidisciplinary approach in the management of recurrent diabetic foot ulceration in Lithuania: a prospective study. Diabetes Care 1999;22:1428–31. [DOI] [PubMed] [Google Scholar]
- 30.Crihana V Improving outcomes in diabetic foot surgery after the implementation of measures for diagnosis and treatment. Journal of Translational Medicine and Research 2014;19:70–7. [Google Scholar]
- 31.Meltzer DD, Pels S, Payne WG, Mannari RJ, Ochs D, Forbes-Kearns J, et al. Decreasing amputation rates in patients with diabetes mellitus. An outcome study. J Am Podiatr Med Assoc 2002;92:425–8. [DOI] [PubMed] [Google Scholar]
- 32.Chiu CC, Huang CL, Weng SF, Sun LM, Chang YL, Tsai FC. A multidisciplinary diabetic foot ulcer treatment programme significantly improved the outcome in patients with infected diabetic foot ulcers. J Plast Reconstr Aesthet Surg 2011; 64:867–72. [DOI] [PubMed] [Google Scholar]
- 33.Cahn A, Elishuv O, Olshtain-Pops K. Establishing a multidisciplinary diabetic foot team in a large tertiary hospital: a workshop. Diabetes Metab Res Rev 2014;30:350–3. [DOI] [PubMed] [Google Scholar]
- 34.Martínez-Gómez DA, Moreno-Carrillo MA, Campillo-Soto A, Carrillo-García A, Aguayo-Albasini JL. Reduction in diabetic amputations over 15 years in a defined Spain population. Benefits of a critical pathway approach and multidisciplinary team work. Rev Esp Quimioter 2014;27:170–9. [PubMed] [Google Scholar]
- 35.Anichini R, Zecchini F, Cerretini I, Meucci G, Fusilli D, Alviggi L, et al. Improvement of diabetic foot care after the Implementation of the International Consensus on the Diabetic Foot (ICDF): results of a 5-year prospective study. Diabetes Res Clin Pract 2007;75:153–8. [DOI] [PubMed] [Google Scholar]
- 36.Armstrong DG, Bharara M, White M, Lepow B, Bhatnagar S, Fisher T, et al. The impact and outcomes of establishing an integrated interdisciplinary surgical team to care for the diabetic foot. Diabetes Metab Res Rev 2012;28:514–8. [DOI] [PubMed] [Google Scholar]
- 37.Holstein P, Ellitsgaard N, Olsen BB, Ellitsgaard V. Decreasing incidence of major amputations in people with diabetes. Diabetologia 2000;43:844–7. [DOI] [PubMed] [Google Scholar]
- 38.Alexandrescu V, Hubermont G, Coessens V, Philips Y, Guillaumie B, Ngongang C, et al. Why a multidisciplinary team may represent a key factor for lowering the inferior limb loss rate in diabetic neuro-ischaemic wounds: application in a departmental institution. Acta Chir Belg 2009;109:694–700. [DOI] [PubMed] [Google Scholar]
- 39.Rerkasem K, Kosachunhanun N, Tongprasert S, Khwanngern K, Matanasarawoot A, Thongchai C, et al. Reducing lower extremity amputations due to diabetes: the application of diabetic-foot protocol in Chiang Mai University Hospital. Int J Low Extrem Wounds 2008;7:88–92. [DOI] [PubMed] [Google Scholar]
- 40.Nason GJ, Strapp H, Kiernan C, Moore K, Gibney J, Feeley TM, et al. The cost utility of a multi-disciplinary foot protection clinic (MDFPC) in an Irish hospital setting. Ir J Med Sci 2013;182:41–5. [DOI] [PubMed] [Google Scholar]
- 41.Laakso M, Honkasalo M, Kiiski J, Ala-Houhala M, Haapasalo H, Laine HJ, et al. Re-organizing inpatient care saves legs in patients with diabetic foot infections. Diabetes Res Clin Pract 2017;125:39–46. [DOI] [PubMed] [Google Scholar]
- 42.McGill MN, Constantino M, Bolton T, Palmer E, Yue D. Diabetes Amputation Program: a structured systematic approach. Diabetic Foot Journal 2003;6:172–6. [Google Scholar]
- 43.Yesil S, Akinci B, Bayraktar F, Havitcioglu H, Karabay O, Yapar N, et al. Reduction of major amputations after starting a multidisciplinary diabetic foot care team: single centre experience from Turkey. Exp Clin Endocrinol Diabetes 2009;117:345–9. [DOI] [PubMed] [Google Scholar]
- 44.Nather A, Siok Bee C, Keng Lin W, Xin-Bei Valerie C, Liang S, Tambyah PA, et al. Value of team approach combined with clinical pathway for diabetic foot problems: a clinical evaluation. Diabet Foot Ankle 2010;1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kim CH, Moon JS, Chung SM, Kong EJ, Park CH, Yoon WS, et al. The changes of trends in the diagnosis and treatment of diabetic foot ulcer over a 10-Year period: single center study. Diabetes Metab J 2018;42:308–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Riaz M, Miyan Z, Waris N, Zaidi SIH, Tahir B, Fawwad A, et al. Impact of multidisciplinary foot care team on outcome of diabetic foot ulcer in term of lower extremity amputation at a tertiary care unit in Karachi, Pakistan. Int Wound J 2019;epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chung J, Modrall JG, Ahn C, Lavery LA, Valentine RJ. Multidisciplinary care improves amputation-free survival in patients with chronic critical limb ischemia. J Vasc Surg 2015;61:162–9. [DOI] [PubMed] [Google Scholar]
- 48.Hsu CR, Chang CC, Chen YT, Lin WN, Chen MY. Organization of wound healing services: The impact on lowering the diabetes foot amputation rate in a ten-year review and the importance of early debridement. Diabetes Res Clin Pract 2015;109:77–84. [DOI] [PubMed] [Google Scholar]
- 49.Plusch D, Penkala S, Dickson HG, Malone M. Primary care referral to multidisciplinary high risk foot services - too few, too late. J Foot Ankle Res 2015;8:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hedetoft C, Rasmussen A, Fabrin J, Kolendorf K. Four-fold increase in foot ulcers in type 2 diabetic subjects without an increase in major amputations by a multidisciplinary setting. Diabetes Res Clin Pract 2009;83:353–7. [DOI] [PubMed] [Google Scholar]
- 51.Wang C, Mai L, Yang C, Liu D, Sun K, Song W, et al. Reducing major lower extremity amputations after the introduction of a multidisciplinary team in patient with diabetes foot ulcer. BMC Endocr Disord 2016;16:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Witsø E, Lium A, Lydersen S. Lower limb amputations in Trondheim, Norway. Acta Orthop 2010;81:737–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Troisi N, Baggiore C, Landini G, Michelagnoli S. How daily practice changed in an urban area after establishing a multidisciplinary diabetic foot program. J Diabetes 2016;8:594–5. [DOI] [PubMed] [Google Scholar]
- 54.Wennberg L, Widgren S, Axelsson R, Gerok-Andersson K, Åkerlund B. Multidisciplinary diabetic foot care in Sweden - A national survey. Diabetes Res Clin Pract 2019;149:126–31. [DOI] [PubMed] [Google Scholar]
- 55.Barshes NR, Sigireddi M, Wrobel JS, Mahankali A, Robbins JM, Kougias P, et al. The system of care for the diabetic foot: objectives, outcomes, and opportunities. Diabet Foot Ankle 2013;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shih CD, Shin L, Armstrong D 4 Building Blocks for a Successful Limb Preservation Program. Podiatry Management. 2018(November/December ):113–8. [Google Scholar]
- 57.Wrobel JS, Robbins JM, Charns MP, Bonacker KM, Reiber GE, Pogach L. Diabetes-related foot care at 10 Veterans Affairs medical centers: must do’s associated with successful microsystems. Jt Comm J Qual Patient Saf 2006;32:206–13. [DOI] [PubMed] [Google Scholar]
- 58.Paisey RB, Abbott A, Levenson R, Harrington A, Browne D, Moore J, et al. Diabetes- related major lower limb amputation incidence is strongly related to diabetic foot service provision and improves with enhancement of services: peer review of the South-West of England. Diabet Med 2018;35:53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wrobel JS, Charns MP, Diehr P, Robbins JM, Reiber GE, Bonacker KM, Haas LB, Pogach L. The relationship between provider coordination and diabetes-related foot outcomes. Diabetes Care2003;26:3042–7. [DOI] [PubMed] [Google Scholar]
- 61.Zhan Z, van den Heuvel ER, Doornbos PM, Burger H, Verberne CJ, Wiggers T, et al. Strengths and weaknesses of a stepped wedge cluster randomized design: its application in a colorectal cancer follow-up study. J Clin Epidemiol 2014;67:454–61. [DOI] [PubMed] [Google Scholar]
- 62.Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr 2013;13:S38–44. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.