Abstract
Purpose:
Sickle cell disease (SCD) is associated with high acute healthcare utilization. The purpose of this study was to examine whether Medicaid expansion in California increased Medicaid enrollment, increased hydroxyurea prescriptions filled, and decreased acute healthcare utilization in SCD.
Methods:
Individuals with SCD (≤ 65 years and enrolled in Medicaid for ≥ 6 total calendar months any year between 2011 and 2016) were identified in a multisource database maintained by the California Sickle Cell Data Collection Program. We describe trends and changes in Medicaid enrollment, hydroxyurea prescriptions filled, and emergency department (ED) visits and hospital admissions before (2011-2013) and after (2014-2016) Medicaid expansion in California.
Results:
The cohort included 3,635 individuals. Enrollment was highest in 2014 and lowest in 2016 with a 2.8% annual decease post-expansion. Whereas < 20% of the cohort had a hydroxyurea prescription filled, the percentage increased by 5.2% annually after 2014. The ED visit rate was highest in 2014 and decreased slightly in 2016, decreasing by 1.1% annually post-expansion. Hospital admission rates were similar during the pre- and post-expansion periods. Young adults and adults had higher ED and hospital admission rates than children and adolescents.
Conclusions:
Medicaid expansion does not appear to have improved enrollment or acute healthcare utilization among individuals with SCD in California. Future studies should explore whether individuals with SCD transitioned to other insurance plans or became uninsured post-expansion, the underlying reasons for low hydroxyurea utilization, and the lack of effect on hospital admissions despite a modest effect on ED visits.
Keywords: sickle cell disease, healthcare utilization, Medicaid expansion, hydroxyurea, health disparity
INTRODUCTION
Sickle cell disease (SCD) is an inherited blood disorder that predominantly affects racial minorities in the United States. An estimated one in every 365 African American and one in every 16,305 Hispanic births are affected by SCD.1,2 Medicaid is the major source of health insurance coverage for individuals with SCD, with an estimated 70% of children and 50% of adults being covered under Medicaid or Medicaid administered programs.3 As of September 2019, 37 states and the District of Columbia opted to expand Medicaid to low-income individuals under the Patient Protection and Affordable Care Act (ACA).4 Medicaid expansion resulted in significant reductions in the rates of the uninsured and gains in Medicaid enrollment among the general population in expansion compared to non-expansion states.5 However, Medicaid enrollment gains post-expansion vary across racial and ethnic groups and low-income African Americans and Hispanics continue to have higher uninsured rates than low-income Whites.6-8 Whether Medicaid expansion has increased Medicaid enrollment among individuals with SCD, who are highly dependent on Medicaid for health insurance coverage, is unknown.
It is also unknown if increased access to preventive healthcare services through Medicaid expansion decreased acute healthcare utilization in SCD. Acute healthcare utilization, defined as hospital admissions and emergency department (ED) visits, is high in SCD.3,9-11 Specifically, publically insured adults with SCD have higher acute healthcare visits (≥3 visits per year) than the privately insured (1.8 visits per year) and the uninsured (1.4 visits per year).9 There is also concern that, with Medicaid expansion, newly enrolled beneficiaries might have significant unmet health needs (pent-up demand) and, accordingly, exhibit a high level of acute healthcare utilization.12 Whether this is true among individuals with SCD is unknown. It is also unknown if access to health insurance through Medicaid expansion increased hydroxyurea prescribing and utilization among individuals with SCD. Hydroxyurea is a standard of care disease modifying therapy indicated for individuals with hemoglobin SS and sickle/beta zero thalassemia genotypes.13 and is associated with a reduction in acute healthcare utilization,14-16 National estimates indicate that approximately 75% of individuals with SCD have hemoglobin SS or sickle/beta zero thalassemia genotypes,17 and would, therefore, be eligible for hydroxyurea. Yet, hydroxyurea is neither optimally prescribed18 nor optimally utilized.19-21 The purpose of this study was to examine whether Medicaid expansion under the ACA increased Medicaid enrollment, increased hydroxyurea prescriptions filled, and decreased acute healthcare utilization among individuals with SCD in California. The study focused on individuals with SCD in California because California maintains a statewide surveillance program for SCD and expanded Medicaid coverage in 2014 under the ACA to low-income individuals.22
METHODS
Study Design
Individuals with SCD in California were identified in a multisource database created by the California Sickle Cell Data Collection (SCDC) program. The SCDC program gathers data from (1) the Office of Statewide Health Planning and Development administrative data sources [hospital discharge (PDD) and ED], (2) State of California vital records death files, and (3) Medicaid (in California, called ‘Medi-Cal’) and other state-run insurance programs (such as California Children Services and/or Genetically Handicapped Persons’ Program) claims and enrollment files. The SCDC program then links these data at the individual-level and applies a validated case definition for SCD to identify a statewide cohort with data from 2004 through 2016.23 The SCD case definition includes the presence of three or more separate healthcare visits over any five year period with an ICD-9/10-CM code for SCD.24 The databases and linkage process have been previously described.25,26
Individuals with SCD were included in this study if they were (1) enrolled in Medi-Cal or other state-run programs at any time between 2011-2016 for six or more total calendar months in the year and (2) were ≤ 64 years of age at the close of 2016. The period 2011 to 2016 was chosen because 2016 is the most recent year for which data are available and allows for a three-year comparison before and after Medi-Cal expansion. Individuals > 64 years of age were excluded because most are covered predominantly by Medicare. Although a portion of individuals ≤ 64 years of age might also be covered by Medicare due to disability, this analysis included only Medicaid claims.
Participant Level Measures
Demographics
Age (at end of 2016), race/ethnicity, and sex were determined from the Medi-Cal eligibility file. Cohort participants were grouped by age into children (≤ 11 years), adolescents (12-21 years), young adults (22-34 years), and adults (35-64 years). Death and age at death were recorded from a combination of hospital discharge disposition codes and vital records data.
Medi-Cal Enrollment
A cohort participant was considered to be enrolled in Medi-Cal for any single year if enrolled for a total of six or more calendar months in the year. The number of cohort participants enrolled annually is reported by cohort and age group. Average annual percent change in Medi-Cal enrollment during the pre-Medi-Cal expansion period (2011-2013) was compared to the post-Medi-Cal expansion period (2014-2016). The average annual percent change in enrollment was calculated according to equation (1):
| Equation,1 |
Hydroxyurea Prescriptions Filled
Claims for hydroxyurea prescriptions filled and billed to Medi-Cal were used. The National Drug Codes are included in Supporting Information Table S1. We calculated the annual percentage of cohort participants who had at least one hydroxyurea claim per year for the cohort and by age group. Average annual percent change in claims during the pre-expansion (2011-2013) was compared to post-expansion (2014-2016) period. Average annual percent change for hydroxyurea claims was calculated using equation (1).
Acute Healthcare Utilization
The number of ED visits and hospital admissions were drawn from the ED file and state administrative hospital discharge data rather than from Medi-Cal claims, as the former are more consistently coded and complete. Annual ED visit and hospital admission rates were calculated per 10,000 Medi-Cal beneficiaries who meet the SCD case definition for the cohort and by age group, using equations (2a) and (2b).
| Equation,2a |
| Equation,2b |
Average annual percent change in ED visit and hospital admission rates during the pre-expansion (2011-2013) were compared to post-expansion (2014-2016) period. Average annual percent change for ED visit and hospital admission rates were calculated using equation (1).
Statistical Analysis
Descriptive statistics were used to describe participant characteristics, Medi-Cal enrollment, hydroxyurea prescriptions filled, and acute healthcare utilization measures. Analyses were performed using SAS version 9.4.
RESULTS
Participant characteristics
During 2011 and 2016, 3635 individuals, ≤ 64 years of age and meeting the case definition for SCD, were enrolled in Medi-Cal. Of these individuals, 72% (n=2613) were continuously enrolled in Medi-Cal for at least six months of each year during 2011 and 2016. Table 1 shows the cohort’s demographic characteristics at the end of 2016. The cohort was 56% female and 78% African American. During the study period, 7.3% (n=265) of the cohort died. Although 69% of deceased individuals were adults (35-64 years), 24% were young adults (22-34 years).
TABLE 1.
Cohort demographic characteristics
| N= 3635 | n | % |
|---|---|---|
| Age group (years) | ||
| ≤11 | 476 | 13.1 |
| 12-21 | 680 | 18.7 |
| 22–34 | 1145 | 31.5 |
| 35–64 | 1334 | 36.7 |
| Sex | ||
| Female | 2039 | 56.1 |
| Male | 1596 | 43.9 |
| Race | ||
| African American | 2847 | 78.3 |
| White | 146 | 4.0 |
| Hispanic | 167 | 4.6 |
| Asian/Pacific Islander | 108 | 3.0 |
| Other/ Unknown | 367 | 10.1 |
| Deceased | ||
| Cohort | 265 | 7.3 |
| ≤11 years | 5 | 1.9 |
| 12-21 years | 13 | 4.9 |
| 22–34 years | 64 | 24.2 |
| 35-64 years | 183 | 69.0 |
Medi-Cal Enrollment
Figure 1 shows the trends in the number of cohort participants enrolled in Medi-Cal for the full cohort and by age group. The number of cohort participants enrolled annually increased during 2011 through 2014, was highest in 2014 (n=3,256) and then decreased and was lowest in 2016 (n=2,991). Medi-Cal enrollment was highest in 2014 and then decreased in 2015 and 2016 across all age groups, except adolescents (12-21 years). Medi-Cal enrollment was lowest in 2016 across all age groups, except children (≤ 11years).
FIGURE 1.
Number of Participants Enrolled in Medi-Cal by year (2011-2016), by Study Cohort and age group
During the pre-expansion period (2011-2013), the number of cohort participants enrolled in Medi-Cal increased by 0.6% annually. In contrast, during the post-expansion (2014-2016) period the number of enrolled cohort participants decreased by 2.8% annually, resulting in a net decrease of 3.4% between the pre- and post-expansion periods (Table 2). The decrease in the number of enrollees post-expansion was due to more individuals exiting than newly enrolling in Medi-Cal during this period. The gap between “newly enrolled” and “dis-enrolled” participants continued to increase post-expansion and was 0.3% in 2014, −2% in 2015, and −7.4% in 2016.
TABLE 2.
Average annual percent change for Medi-Cal enrollment, hydroxyurea prescriptions filled, and acute healthcare utilization
| Age group in years |
Average annual percent change pre-expansion (2011-2013) |
Average annual percent change post-expansion (2014-2016) |
Net Percent Change |
|---|---|---|---|
| Number of Medi-Cal enrolled participants | |||
| Cohort | 0.6 | −2.8 | −3.4 |
| ≤11 | 4.1 | −1.9 | −6.0 |
| 12-21 | 0.0 | −1.6 | −1.6 |
| 22-34 | 0.8 | −2.8 | −3.6 |
| 35-64 | −0.3 | −3.7 | −3.4 |
| Percent of hydroxyurea prescriptions filled | |||
| Cohort | 0.6 | 5.9 | 5.2 |
| ≤11 | 14.1 | 17.6 | 3.5 |
| 12-21 | 7.3 | 7.0 | −0.3 |
| 22-34 | −2.7 | 3.2 | 5.9 |
| 35-64 | −3.3 | 1.8 | 5.2 |
| Emergency department visit rate | |||
| Cohort | 0.5 | −1.1 | −1.6 |
| ≤11 | 0.7 | −5.6 | −6.2 |
| 12-21 | 2.4 | 1.8 | −0.6 |
| 22-34 | 1.0 | −0.9 | −1.9 |
| 35-64 | −0.4 | −0.9 | −0.5 |
| Hospital admission rate | |||
| Cohort | −1.2 | −1.4 | −0.2 |
| ≤11 | −0.3 | −0.1 | 0.2 |
| 12-21 | 3.1 | 2.5 | −0.6 |
| 22-34 | −0.2 | −3.1 | −2.9 |
| 35-64 | −3.2 | −1.3 | 1.9 |
The decrease in enrollment post-expansion was across all age groups and was higher among young adults (−2.8%) and adults (−3.7%) than children (−1.9%) and adolescents (−1.6%). However, children had the highest net decrease in the number of enrolled participants between the pre- and the post-expansion periods at 6%.
Hydroxyurea Prescriptions Filled
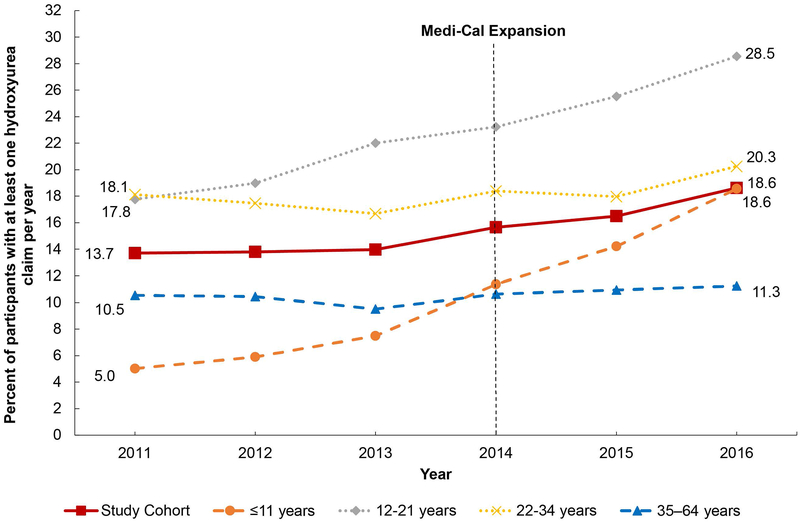
Although the percentage of study cohort participants with at least one hydroxyurea claim per year increased between 2011 and 2016, it never rose above 20% for the cohort (Figure 2). Adolescents had the highest percentage of hydroxyurea claims during the study period, reaching 28.5% in 2016, followed by young adults (20.3%). Children had the lowest percent of hydroxyurea claims in 2011, however, their claims increased during the study period reaching 18.6% in 2016. Adults had a low percentage of hydroxyurea claims during the study period reaching a maximum of 11.3% in 2016.
FIGURE 2.
Percent of Participants with at least one Hydroxyurea Claim by Year (2011-2016), by Study Cohort and Age Group
Hydroxyurea claims increased by 0.6% annually during the pre-expansion compared to 5.9% increase during the post-expansion period among the cohort, resulting in a net increase of 5.2% between the pre- and post-expansion periods (Table 2). Young adults and adults had higher net gains in the percent of hydroxyurea claims at 5.9% and 5.2%, respectively, compared to children (3.5%). Adolescents had a slight net decrease in hydroxyurea claims (−0.3%).
Trends in Acute Healthcare Utilization
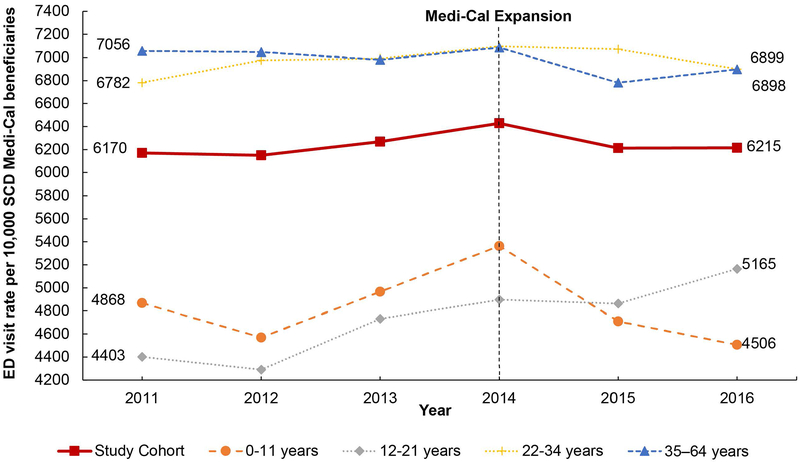
The annual rate of ED visits per 10,000 SCD Medi-Cal beneficiaries was lowest in 2012, increased in 2013, was highest in 2014, then decreased in 2015 and 2016 (Figure 3). From 2011 to 2016, the ED visit rate was consistently highest among young adults and adults compared to other age groups. Children and adolescents had a similar trend in ED visit rate between 2011 and 2014 with a decrease in 2011, followed by an increase in 2013 and 2014. During 2015 and 2016, the ED visit rate increased among adolescents and decreased among children.
FIGURE 3.
Emergency Department (ED) Visit Rate per 10,000 Medi-Cal Beneficiaries with Sickle cell Disease (SCD) by Year (2011-2016), by Study Cohort and Age Group
The ED visit rate increased by 0.5% annually during the pre-expansion period and decreased by 1.1% annually during the post-expansion period, resulting in a net decrease of 1.6% between the pre- and post-expansion periods (table 2). The ED visits not resulting in a hospital admission decreased by a net of 2.4%, whereas ED visits resulting in a hospital admission decreased by a net of 0.7% between the pre and post-expansion periods. The highest increase in ED visits during the pre-expansion period was among adolescents (2.4%). Post-expansion, the ED visit rate among adolescents continued to increase, however, the increase was 1.8% annually, resulting in a net decrease of 0.6% between the pre- and post-expansion periods. The highest net decrease in the ED visit rate was among children (−6.2%).
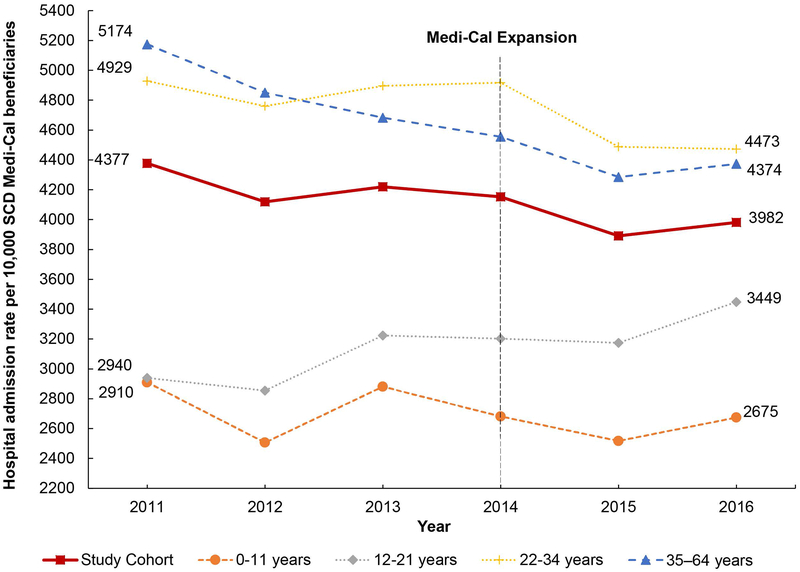
The rate of hospital admissions decreased between 2011 and 2016 (Figure 4). A slight increase compared to the previous year was observed in 2013 and in 2016. This trend was across all age groups, except among young adults whose hospital admission rates decreased in 2016. Similar to the trend for ED visit rates, hospital admission rates were highest among young adults and adults compared to other age groups. Unlike the trend observed for ED visit rates, adolescents had consistently higher hospital admission rates compared to children and their admission rates continued to increase between 2013 and 2016.
FIGURE 4.
Hospital Admission Rate per 10,000 Medi-Cal Beneficiaries with Sickle cell Disease (SCD) by Year (2011-2016), by Study Cohort and Age Group
Hospital admissions decreased at a similar rate during the pre-expansion (−1.2%) and post-expansion (−1.4%) periods (Table 2). Young adults had the highest percent decrease in rate of hospital admissions during the post-expansion period (−3.1%), resulting in a net decrease of 2.9% between the pre- and post-expansion periods. Although the average annual percent change in hospital admission rate continued to increase in the post- expansion period among adolescents, there was a net decrease of 0.6% in hospital admissions between the pre- and post-expansion periods. Among children and adults, the percent decrease in the annual hospital admission rate was larger in the pre- compared to the post-expansion period resulting in a net increase of 0.2% and 1.9%, respectively.
DISCUSSION
This is the first study, that the authors’ are aware of, that describes trends and compares Medicaid enrollment, hydroxyurea prescriptions filled, and acute healthcare utilization pre- and post-Medicaid expansion in a state-level cohort of individuals with SCD. Our findings reveal that the gains observed in Medi-Cal enrollment post-expansion among the general population in California22 did not extend to individuals with SCD in the state. Following expansion, Medi-Cal enrollment among the general population nearly doubled (from 8.6 million in 2013 to more than 13.5 million in 2016), resulting in approximately one-third of the population in California being covered under Medi-Cal.22 In contrast, Medi-Cal enrollment among the study cohort decreased in the post-expansion period. Furthermore, most enrollment gains among the general population in California were among low-income individuals, aged 19-64 years.22 In contrast, our results show that the young adult and adult groups had greater enrollment loses during the post-expansion period compared to the other age groups.
It is difficult to determine the causes of this difference in enrollment among individuals with SCD compared to the general population. Although the decrease in enrollment in this study can be explained, in part, by deaths among the cohort (Table 1), it does not completely account for the difference in enrollment. One hypothesis is the existence of substantial disparity in access to Medi-Cal enrollment among individuals with SCD compared to the general population in California. Alternatively, it is possible that most individuals with SCD were already enrolled in Medi-Cal before the expansion in 2014 with little opportunity for enrollment gains following expansion. In fact, 88% of our cohort was enrolled in Medi-Cal in 2013. Our findings also show that more individuals dis-enrolled rather than newly enrolled in Medi-Cal, post-expansion. Whether the individuals who dis-enrolled from Medi-Cal then enrolled in other health plans or became uninsured is unknown. It is possible that some cohort participants benefitted from other provisions of the ACA, including extended dependent coverage and newly required coverage by private insurance of people with pre-existing conditions, or access to employer-based insurance or new marketplace plans (Covered California)28 and, as a result, dis-enrolled from Medi-Cal for these plans. The Kaiser Family Foundation estimates that the percent of Black population in California decreased by 1% in 2014 compared to 201329 and its also possible that some individuals with SCD might have left California.
There are three main findings related to hydroxyurea from this study. First, the overall percent of individuals with SCD with at least one hydroxyurea prescription filled per year remained below 20% from 2011 through 2016 and was lower than 30-35% range reported among Medicaid enrolled children and adults in other studies.30-32 Given that the study criteria included at least one prescription claim per year, hydroxyurea is covered by Medi-Cal, and the 2014 National Heart, Lung, and Blood Institute (NHLBI) guidelines recommend that all individuals with hemoglobin SS and sickle/beta zero thalassemia genotypes, age nine months and older, be offered hydroxyurea,13 our study reveals a substantial low utilization of hydroxyurea among the cohort. Although we could not determine the percentage of study cohort participants who would be eligible for hydroxyurea based on their genotype, we anticipate that 60-75% of the cohort would have been eligible for hydroxyurea given estimates of the incidence and prevalence of hemoglobin SS and Sickle/beta zero thalassemia genotypes in SCD in California33 and nationally.17
Second, despite the overall low percentage of hydroxyurea prescriptions filled, we found a trend towards an increase in hydroxyurea prescriptions filled when comparing the pre- and post-expansion periods. Our finding is similar to other studies that found a trend towards increased hydroxyurea claims after 2014.18,31 However, this increase might be attributable to the release of the 2014 NHBLI guidelines13 rather than to Medi-Cal expansion.
Third, we found a difference in the percent increase in hydroxyurea prescriptions filled by age group. The highest increase in hydroxyurea prescriptions filled post-expansion was observed among young adults and adults at 5.9% and 5.2%, respectively. These findings are in contrast to other studies that reported no significant change in hydroxyurea claims among adults after 2014.18 We also found that hydroxyurea prescriptions filled among children increased by 3.5%. This finding is similar to other studies that reported an increase in hydroxyurea claims among Medicaid enrolled children.18,31
Overall, we found a substantial underutilization of hydroxyurea in our cohort. However, the data reported were on prescriptions filled and not adherence to hydroxyurea, which might be even lower in this cohort. In the absence of data on prescription rates, SCD genotype, other SCD modifying therapies, and individual compliance, it is difficult to determine the causes for low claims among the study cohort and whether they are due to healthcare clinicians under-prescribing hydroxyurea to eligible individuals28 or to individuals underutilization of hydroxyurea due to lack of knowledge, negative attitudes and beliefs regarding hydroxyurea and its benefits,19,20,34 or recall barriers to taking the medication.21
Trends in acute care visits varied by type of service (hospital admissions and ED visits) and by age group. The ED visit rates decreased by a net of 1.6% from the pre- to post-expansion periods. Our findings are similar to earlier research on ED utilization in California that anticipated a decrease in ED visits following Medi-Cal expansion with better access to ambulatory care12 and in contrast to national trends that showed an increase in ED visits during the three-years following Medicaid expansion.35 Whether the decrease in ED visit rates is the result of better access to preventive ambulatory healthcare is difficult to determine in the absence of data about ambulatory healthcare utilization by the cohort. On the other hand, trends in hospital admission rates did not change significantly in the pre- compared to the post-expansion period. This could also just reflect the general trend of decreased hospital admissions and control of healthcare costs. By age group, acute healthcare visit rates were higher among young adults and adults than children and adolescents. This finding is similar to other studies that found higher acute healthcare utilization among young adults compared to children.22,23,26 However, when comparing the pre- and post-expansion periods, our results indicate that young adults might have benefited the most compared to the other age groups from Medi-Cal expansion in California. Despite a reduction in enrollment among this age group in the post-expansion period, young adults concurrently had the highest decrease in hospital admissions, the second highest decrease in ED visits, and the highest increase in hydroxyurea prescriptions filled compared to the other age groups.
Limitations and Conclusions
The study has several limitations. First, change in healthcare coverage by alternative plans, such as employer-based insurance or new ACA marketplace plans (Covered California) was not assessed. It is possible that some individuals with SCD dis-enrolled from Medi-Cal for these plans. Future research should explore coverage across multiple insurance plans to identify gaps in coverage among individuals with SCD over time. Second, determination of whether individuals had dual Medicaid and Medicare eligibility was not explored. Finally, the lack of genotype data impacted our ability to determine cohort participants who would be eligible for hydroxyurea. Despite these limitations, the study is the first, to the authors’ knowledge, that describes enrollment pre- and post-expansion of Medi-Cal, hydroxyurea prescriptions filled, and acute healthcare utilization rates among a large, state-level cohort of individuals with SCD. Future research should explore the factors contributing to the low hydroxyurea fill rate among individuals with SCD in California, specifically whether it resulted from under-prescribing by clinicians or under-filling of prescriptions by individuals with SCD. Whereas we found a trend toward deceased ED visits post- compared to pre-expansion, future research should examine ED utilization concurrently with ambulatory care visits to determine whether Medicaid expansion improves access to preventive ambulatory services for individuals with SCD. Overall, these findings have important implications for clinicians and policy makers to address the potential disparities in Medi-Cal enrollment and the hydroxyurea prescriptions fill rates among individuals with SCD.
Supplementary Material
Hydroxyurea National Drug Codes (NDC) searched for in California Medi-Cal claims data
Acknowledgments
The authors would like to thank Heather K. Amato, MPH, for assisting with data extraction.
Conflict of Interest statement
Mariam Kayle was supported by funding from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR #H133P130013; PI Heinemann) during this research. She is supported by funding form the Centers for Disease Control and Prevention (1 NU58DD000004-01-00).
The Sickle Cell Data Collection Program receives support from The CDC Foundation; Pfizer, Inc.; Sanofi, Inc.; Global Blood Therapeutics; and The Doris Duke Charitable Foundation.
Paula Tanabe is supported by funding from the National Heart, Lung and Blood Institute (U01HL133964, UH3 -HL137856-01) and the Agency for Healthcare Research and Quality (RHS024501A).
Robert I. Liem is supported by funding from the National Heart, Lung and Blood Institute (5R01HL136480).
Sherif Badawy is supported by funding from the Agency for Healthcare Research and Quality (K12HS023011).
Marsha Treadwell is supported by funding from the National Heart, Lung and Blood Institute (U01HL134007), the Agency for Healthcare Research and Quality (U18HS025297), the Health Resources and Services Administration (U1EMC27862), and is a consultant to Global Blood Therapeutics.
The content is solely the responsibility of the authors and does not necessarily represent the official views of any of the funding agencies.
Abbreviations table
- SCD
Sickle cell disease
- ED
Emergency department
- ACA
Patient Protection and Affordable Care Act
- SCDC
California Sickle Cell Data Collection Program
- ICD-9/10-CM
International Classification of Diseases, Ninth and Tenth Revisions, Clinical Modification
- NHLBI
National Heart, Lung, and Blood Institute
Footnotes
Data Sharing Statement
The data that support the findings of this study are subject to third party restrictions. Data use agreements maintained by the California Sickle Cell Data Collection Program do not allow the sharing of data.
REFERENCES
- 1.Hassell KL. Population estimates of sickle cell disease in the U.S. Am J Prev Med. 2010;38(4 Suppl):S512–521. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Data & Statistics on Sickle Cell Disease. https://www.cdc.gov/ncbddd/sicklecell/data.html. Updated August 9, 2017 Accessed June 30, 2019.
- 3.Lanzkron S, Carroll CP, Haywood C Jr. The burden of emergency department use for sickle-cell disease: an analysis of the national emergency department sample database. Am J Hematol. 2010;85(10):797–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Status of State Action on the Medicaid Expansion Decision. Henry Kaiser Family Foundation; August 1, 2019 [Google Scholar]
- 5.Antonisse L, Garfield R, Rudowitx R, Artiga S. The Effects of Medicaid Expansion under the ACA: Updated Findings from a Literature Review (Issue Brief No.###). March 28, 2018. https://www.kff.org/medicaid/issue-brief/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-literature-review-march-2018/. [Google Scholar]
- 6.Buchmueller TC, Levinson ZM, Levy HG, Wolfe BL. Effect of the Affordable Care Act on Racial and Ethnic Disparities in Health Insurance Coverage. Am J Public Health. 2016;106(8):1416–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yue D, Rasmussen PW, Ponce NA. Racial/Ethnic Differential Effects of Medicaid Expansion on Health Care Access. Health Serv Res. 2018;53(5):3640–3656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wehby GL, Lyu W. The Impact of the ACA Medicaid Expansions on Health Insurance Coverage through 2015 and Coverage Disparities by Age, Race/Ethnicity, and Gender. Health Serv Res. 2018;53(2):1248–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brousseau DC, Owens PL, Mosso AL, Panepinto JA, Steiner CA. Acute care utilization and rehospitalizations for sickle cell disease. JAMA. 2010;303(13):1288–1294. [DOI] [PubMed] [Google Scholar]
- 10.Carroll CP, Haywood C Jr., Fagan P, Lanzkron S. The course and correlates of high hospital utilization in sickle cell disease: Evidence from a large, urban Medicaid managed care organization. Am J Hematol. 2009;84(10):666–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carroll CP, Haywood C Jr., Lanzkron SM. Examination of the Patient and Hospitalization Characteristics of 30-Day SCD Readmissions. South Med J. 2016;109(9):583–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lo N, Roby DH, Padilla J, et al. Increased service use following Medicaid expansion is mostly temporary: evidence from California’s low income health program. Policy Brief UCLA Cent Health Policy Res. 2014(Pb2014-7):1–8. [PubMed] [Google Scholar]
- 13.National Heart, Lung, and Blood Institute, Expert Panel. Evidence-Based Managment of Sickle Cell Disease, Expert Panel Report. 2014. https://www.nhlbi.nih.gov/sites/default/files/media/docs/sickle-cell-disease-report%20020816_0.pdf. Accessed 07/12/2019.
- 14.Lanzkron S, Strouse JJ, Wilson R, et al. Systematic review: Hydroxyurea for the treatment of adults with sickle cell disease. Ann Intern Med. 2008;148(12):939–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Quarmyne MO, Dong W, Theodore R, et al. Hydroxyurea effectiveness in children and adolescents with sickle cell anemia: A large retrospective, population-based cohort. Am J Hematol. 2017;92(1):77–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Strouse JJ, Lanzkron S, Beach MC, et al. Hydroxyurea for sickle cell disease: a systematic review for efficacy and toxicity in children. Pediatrics. 2008;122(6):1332–1342. [DOI] [PubMed] [Google Scholar]
- 17.Saraf SL, Molokie RE, Nouraie M, et al. Differences in the clinical and genotypic presentation of sickle cell disease around the world. Paediatr Respir Rev. 2014;15(1):4–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Su ZT, Segal JB, Lanzkron S, Ogunsile FJ. National trends in hydroxyurea and opioid prescribing for sickle cell disease by office-based physicians in the United States, 1997-2017. Pharmacoepidemiol Drug Saf. 2019;28(9):1246–1250. [DOI] [PubMed] [Google Scholar]
- 19.Haywood C Jr., Beach MC, Bediako S, et al. Examining the characteristics and beliefs of hydroxyurea users and nonusers among adults with sickle cell disease. Am J Hematol. 2011;86(1):85–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sinha CB, Bakshi N, Ross D, Krishnamurti L. From trust to skepticism: An in-depth analysis across age groups of adults with sickle cell disease on their perspectives regarding hydroxyurea. PLoS One. 2018;13(6):e0199375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Badawy SM, Thompson AA, Lai JS, Penedo FJ, Rychlik K, Liem RI. Adherence to hydroxyurea, health-related quality of life domains, and patients’ perceptions of sickle cell disease and hydroxyurea: a cross-sectional study in adolescents and young adults. Health Qual Life Outcomes. 2017;15(1):136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McConville S The Medi-Cal Program. Public Policy Institute of California; 2017. [Google Scholar]
- 23.Snyder AB, Zhou M, Theodore R, Quarmyne MO, Eckman J, Lane PA. Improving an Administrative Case Definition for Longitudinal Surveillance of Sickle Cell Disease. Public Health Rep. 2019;134(3):274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Snyder AB, Lane PA, Zhou M, Paulukonis ST, Hulihan MM. The accuracy of hospital ICD-9-CM codes for determining Sickle Cell Disease genotype. J Rare Dis Res Treat 2(4):39–45. 2017;2(4). [PMC free article] [PubMed] [Google Scholar]
- 25.Paulukonis ST, Feuchtbaum LB, Coates TD, et al. Emergency department utilization by Californians with sickle cell disease, 2005-2014. Pediatr Blood Cancer. 2017;64(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paulukonis ST, Harris WT, Coates TD, et al. Population based surveillance in sickle cell disease: methods, findings and implications from the California registry and surveillance system in hemoglobinopathies project (RuSH). Pediatr Blood Cancer. 2014;61(12):2271–2276. [DOI] [PubMed] [Google Scholar]
- 27.Fay MP, Tiwari RC, Feuer EJ, Zou Z. Estimating average annual percent change for disease rates without assuming constant change. Biometrics. 2006;62(3):847–854. [DOI] [PubMed] [Google Scholar]
- 28.The California Health Care Landscape. Kaiser Family Foundation: The Kaiser Commission on Medicaid and the Uninsured;August 25, 2015. [Google Scholar]
- 29.Population Distribution by Race/Ethnicity. Kaiser Family Foundation; 2017. https://www.kff.org/other/state-indicator/distribution-by-raceethnicity. Accessed 08/21/2019. [Google Scholar]
- 30.Reeves SL, Jary HK, Gondhi JP, Raphael JL, Lisabeth LD, Dombkowski KJ. Hydroxyurea Initiation Among Children With Sickle Cell Anemia. Clin Pediatr (Phila). 2019;58(13):1394–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brousseau DC, Richardson T, Hall M, et al. Hydroxyurea Use for Sickle Cell Disease Among Medicaid-Enrolled Children. Pediatrics. 2019;144(1). [DOI] [PubMed] [Google Scholar]
- 32.Candrilli SD, O’Brien SH, Ware RE, Nahata MC, Seiber EE, Balkrishnan R. Hydroxyurea adherence and associated outcomes among Medicaid enrollees with sickle cell disease. Am J Hematol. 2011;86(3):273–277. [DOI] [PubMed] [Google Scholar]
- 33.Michlitsch J, Azimi M, Hoppe C, et al. Newborn screening for hemoglobinopathies in California. Pediatr Blood Cancer. 2009;52(4):486–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Badawy SM, Thompson AA, Liem RI. Beliefs about hydroxyurea in youth with sickle cell disease. Hematol Oncol Stem Cell Ther. 2018;11(3):142–148. [DOI] [PubMed] [Google Scholar]
- 35.Singer AJ, Thode HC Jr., Pines JM. US Emergency Department Visits and Hospital Discharges Among Uninsured Patients Before and After Implementation of the Affordable Care Act. JAMA Netw Open. 2019;2(4):e192662. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Hydroxyurea National Drug Codes (NDC) searched for in California Medi-Cal claims data