Abstract
Background
Opioid-induced constipation (OIC), the most common side effect of opioid treatment, is under-recognized and undertreated in older patients. Naldemedine, an oral, peripherally acting μ-opioid receptor antagonist (PAMORA), is approved in Japan, the United States, and the European Union for treatment of OIC in adult patients.
Objective
This integrated analysis of three phase 3 trials (COMPOSE-1, COMPOSE-2, and COMPOSE-3) evaluated the safety and efficacy of naldemedine for up to 12 weeks in a subgroup of patients aged ≥ 65 years.
Methods
Patients aged 18–80 years with chronic non-cancer pain for ≥ 3 months (treated with opioids for ≥ 3 months in COMPOSE-1 and COMPOSE-2) and OIC received oral naldemedine 0.2 mg or placebo once daily. Safety assessments included overall incidence of treatment-emergent adverse events (TEAEs), TEAEs in the gastrointestinal disorders System Organ Class, and TEAEs of opioid withdrawal or possible opioid withdrawal. Efficacy was based on the proportion of responders in COMPOSE-1 and COMPOSE-2, defined as having ≥ 3 spontaneous bowel movements/week and a ≥ 1-spontaneous bowel movement/week increase from baseline for ≥ 9 of 12 weeks and ≥ 3 of the last 4 weeks.
Results
A total of 14.8% (344/2328) of patients were aged ≥ 65 years in all studies. The incidence of TEAEs in naldemedine-treated patients aged ≥ 65 years (45.9%) was comparable to that in patients aged ≥ 65 years receiving placebo (51.6%) and in the overall naldemedine group (47.1%). The incidence of gastrointestinal disorders System Organ Class TEAEs in naldemedine-treated patients aged ≥ 65 years (20.2%) was also comparable to that in patients aged ≥ 65 years receiving placebo (16.1%) and in the overall naldemedine group (21.8%). The incidence of TEAEs of opioid withdrawal with naldemedine was 1.1% in patients aged ≥ 65 years and 1.0% overall, and the incidence of TEAEs of possible opioid withdrawal was 1.1% in patients aged ≥ 65 years and 1.7% overall. The proportion of responders was higher in naldemedine-treated patients versus placebo, both overall (50.1% vs 34.1%; p < 0.0001) and in those aged ≥ 65 years (51.8% vs 37.6%).
Conclusions
This integrated analysis confirmed that OIC treatment with naldemedine 0.2 mg was generally well tolerated and effective in patients aged ≥ 65 years with chronic non-cancer pain. Safety and efficacy results were consistent with the overall patient population.
ClinicalTrials.gov registration
Electronic supplementary material
The online version of this article (10.1007/s40266-020-00753-2) contains supplementary material, which is available to authorized users.
Key Points
| Individuals aged 65 years or older can safely use naldemedine to treat opioid-induced constipation. |
| Naldemedine is effective in improving symptoms of opioid-induced constipation in adults, regardless of age. |
Introduction
Opioid analgesic therapy is a common treatment option for chronic moderate-to-severe non-cancer and cancer pain in selected patients [1]. Opioid-induced constipation (OIC) is the most common adverse effect associated with opioid analgesic treatment and results from opioids activating µ-opioid receptors that are expressed in the enteric nervous system of the gastrointestinal (GI) tract [2]. Unlike other adverse effects associated with opioid therapy, OIC persists unabated over time, even with use of laxatives [3], and patients may skip or reduce their opioid doses in an attempt to manage such adverse effects, which can lead to inadequate pain relief [4].
Opioids are effective for treating chronic pain in older patients (≥ 65 years of age) [5]; however, evidence suggests the risk of OIC rises with age [6]. In fact, OIC is under-recognized and undertreated in the older population [7], and often does not respond to conventional laxatives [8]. Additionally, studies of nursing home residents show that OIC is associated with worse physical and mental outcomes in older patients [9, 10]. Naldemedine is an oral, once-daily, peripherally acting µ-opioid receptor antagonist (PAMORA) approved in Japan, the United States, and the European Union for the treatment of OIC in adults [11–14]. The efficacy and safety of once-daily naldemedine 0.2 mg in patients with chronic non-cancer pain and OIC have been demonstrated in three placebo-controlled phase 3 studies: two identically designed 12-week studies (COMPOSE-1 and COMPOSE-2) [15] and a 52-week study (COMPOSE-3) [16]. This analysis was conducted to characterize the safety and efficacy of naldemedine 0.2 mg once daily versus placebo for up to 12 weeks in patients aged 65 years or older in the three studies.
Methods
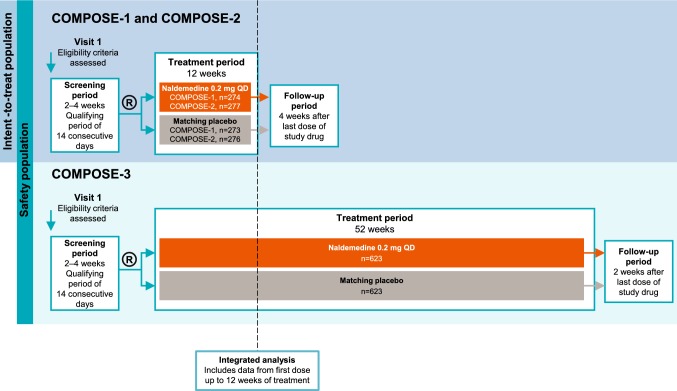
This subgroup analysis of patients ≥ 65 years of age used data from three multicenter, randomized, double-blind, placebo-controlled, parallel-group, phase 3 clinical studies that evaluated the efficacy and safety of naldemedine 0.2 mg once daily in patients with OIC and chronic non-cancer pain (Fig. 1). COMPOSE-1 (NCT01965158) and COMPOSE-2 (NCT01993940) had 12-week treatment periods and were conducted in patients not taking laxatives [15]. COMPOSE-3 (NCT01965652) had a 52-week treatment period and was conducted in patients who could be on stable laxatives [16]. For the purpose of integration, this analysis includes only data from the first dose up to 12 weeks of treatment in all three studies and does not include events reported during the follow-up periods. The studies were conducted in accordance with Good Clinical Practice Guidelines and the Declaration of Helsinki and were approved by the institutional review boards at each study center (see the electronic supplementary material, Online Resource 1). All patients provided written informed consent. Patient disposition profiles for the individual COMPOSE studies have been previously published [15, 16].
Fig. 1.
Study designs. R randomization
All three studies had key inclusion criteria, including age 18–80 years, inclusive; chronic non-cancer pain for ≥ 3 months (treated with opioid analgesics for ≥ 3 months in COMPOSE-1 and COMPOSE-2) and OIC; and receipt of a stable opioid analgesic regimen with a total daily dose of ≥ 30 mg oral morphine equivalent for ≥ 1 month before screening. In addition, participants in the COMPOSE-1 and COMPOSE-2 studies were not currently using or had discontinued laxatives and met all three of the following criteria during a 14-consecutive-day qualifying period during screening: (1) experienced four or fewer spontaneous bowel movements (SBMs) in the qualifying period; (2) reported three or fewer SBMs in any 7-day period during screening; and (3) had one or more symptoms of OIC in ≥ 25% of bowel movements, including straining, hard or lumpy stools, sensation of incomplete evacuation, or anorectal obstruction/blockage. In a 14-consecutive-day qualifying period during screening, participants in COMPOSE-3 must have experienced four or fewer SBMs in total and three or fewer SBMs in any 7-day period and patients may or may not have been on a laxative regimen at screening. The proportion of patients either on a routine laxative regimen (naldemedine 50.2%; placebo 54.0%) or not (naldemedine 30.0%; placebo 29.5%) was similar between treatment groups.
Key exclusion criteria in all three studies included evidence or history of bowel structural abnormalities, strictures, and obstructions, or history of bowel surgery; medical conditions affecting GI transit; a history of chronic constipation unrelated to opioid use; and no history of previous laxative use for OIC.
The safety and tolerability of naldemedine were assessed with data up to 12 weeks from all three studies (safety population: all randomized patients who received at least one dose of study drug and were analyzed by the treatment actually received) using the incidence of treatment-emergent adverse events (TEAEs), treatment-related TEAEs (adverse drug reactions), TEAEs in the GI disorders System Organ Class, and TEAEs of opioid withdrawal or possible opioid withdrawal. TEAEs of opioid withdrawal were defined using “drug withdrawal” per standardized Medical Dictionary for Regulatory Activities queries, and possible opioid withdrawal was defined as three or more TEAEs potentially related to opioid withdrawal syndrome with onset on the same date or occurring within 1 day. The efficacy of naldemedine compared with placebo was assessed in COMPOSE-1 and COMPOSE-2 (intent-to-treat population, including all randomized patients) based on the proportion of responders. Responders were defined as having ≥ 3 SBMs per week and a ≥ 1-SBM-per-week increase from baseline for ≥ 9 of 12 weeks and ≥ 3 of the last 4 weeks. The p value for the comparison of responders in the naldemedine versus the placebo group for the overall patient population was calculated using the Cochran–Mantel–Haenszel test; no statistical analyses were performed for subgroup comparisons.
Results
Safety
The integrated safety population included 2328 patients from the COMPOSE-1, COMPOSE-2, and COMPOSE-3 studies. The demographics and baseline medical characteristics of the integrated safety population are summarized in Table 1. Of the 1163 patients treated with naldemedine, 183 (15.7%) were aged ≥ 65 years, and of the 1165 patients who received placebo, 161 (13.8%) were aged ≥ 65 years. Most patients were white (overall 80.2%; ≥ 65 years 87.2%) and female (overall 62.0%; ≥ 65 years 57.8%). Patients’ mean duration of opioid use prior to screening was 58.1–61.8 months for the overall population and 57.6–71.3 months for patients aged ≥ 65 years, mean daily morphine equivalent dose was 122.2–126.1 mg for the overall population and 84.6–106.4 mg for patients aged ≥ 65 years, and 899 patients (38.6%) overall and 89 patients (25.9%) aged ≥ 65 years used > 100 mg morphine equivalent dose daily.
Table 1.
Baseline demographics and medical characteristics
| Attribute | Integrated safety population (COMPOSE-1/COMPOSE-2/COMPOSE-3) | Intent-to-treat population (COMPOSE-1/COMPOSE-2) | ||||||
|---|---|---|---|---|---|---|---|---|
| Overall | ≥ 65 years of age | Overall | ≥ 65 years of age | |||||
| Naldemedine 0.2 mg/day (n = 1163) |
Placebo (n = 1165) | Naldemedine 0.2 mg/day (n = 183) |
Placebo (n = 161) | Naldemedine 0.2 mg/day (n = 549) | Placebo (n = 546) | Naldemedine 0.2 mg/day (n = 83) |
Placebo (n = 85) | |
| Age | ||||||||
| Mean age, years (SD) | 53.6 (11.1) | 52.9 (10.9) | 70.3 (4.1) | 69.8 (4.0) | 53.7 (10.5) | 53.1 (11.2) | 70.1 (4.1) | 69.9 (4.1) |
| < 65 years, % (n) | 84.3 (980) | 86.2 (1004) | – | – | 84.9 (466) | 84.4 (461) | – | – |
| ≥ 65 years, % (n) | 15.7 (183) | 13.8 (161) | – | – | 15.1 (83) | 15.6 (85) | – | – |
| Female, % (n) | 60.6 (705) | 63.3 (738) | 56.8 (104) | 59.0 (95) | 59.4 (326) | 61.5 (336) | 56.6 (47) | 58.8 (50) |
| Mean BMI, kg/m2 (SD) | 31.5 (7.4)a | 31.4 (7.4)a | 30.5 (6.9) | 30.4 (5.6)b | 31.4 (7.2)c | 31.3 (7.2)d | 30.8 (7.3) | 30.6 (6.1)e |
| Region, % (n) | ||||||||
| North America | 85.8 (998) | 86.4 (1007) | 76.0 (139) | 77.6 (125) | 85.8 (471) | 85.7 (468) | 78.3 (65) | 74.1 (63) |
| Rest of world | 14.2 (165) | 13.6 (158) | 24.0 (44) | 22.4 (36) | 14.2 (78) | 14.3 (78) | 21.7 (18) | 25.9 (22) |
| Race, % (n) | ||||||||
| White | 79.4 (924) | 80.9 (943) | 87.4 (160) | 87.0 (140) | 79.8 (438) | 81.9 (447) | 89.2 (74) | 84.7 (72) |
| Black | 19.0 (221) | 16.7 (195) | 11.5 (21) | 11.2 (18) | 18.6 (102) | 15.9 (87) | 8.4 (7) | 12.9 (11) |
| Other | 1.5 (18) | 2.3 (27) | 1.1 (2) | 1.9 (3) | 1.6 (9) | 2.2 (12) | 2.4 (2) | 2.4 (2) |
| Opioid use | ||||||||
| Mean duration of opioid use, months (SD) | 61.8 (65.3) | 58.1 (56.4) | 71.3 (88.2) | 57.6 (58.0) | 61.1 (61.7) | 59.2 (57.1) | 55.6 (65.4) | 58.9 (63.8) |
| Mean daily opioid dose, MED, mg (SD) | 122.2 (134.5) | 126.1 (157.3) | 84.6 (80.4) | 106.4 (140.9) | 121.6 (120.0) | 131.8 (150.0) | 81.5 (73.8) | 122.6 (177.2) |
| Patients with daily opioid dose, % (n) | ||||||||
| 30 to 100 mg | 61.7 (717) | 61.1 (712) | 76.5 (140) | 71.4 (115) | 59.0 (324) | 58.6 (320) | 74.7 (62) | 69.4 (59) |
| > 100 mg | 38.3 (446) | 38.9 (453) | 23.5 (43) | 28.6 (46) | 41.0 (225) | 41.4 (226) | 25.3 (21) | 30.6 (26) |
| Mean duration of treatment exposure, days (SD) | 76.6 (20.8) | 77.2 (18.8) | 76.9 (20.6) | 77.6 (19.1) | 77.5 (22.0)f | 77.9 (20.4) | 76.1 (23.1)g | 77.7 (21.1) |
BMI body mass index, MED morphine equivalent dose, SD standard deviation
an = 1162
bn = 160
cn = 547
dn = 543
en = 84
fn = 542
gn = 82
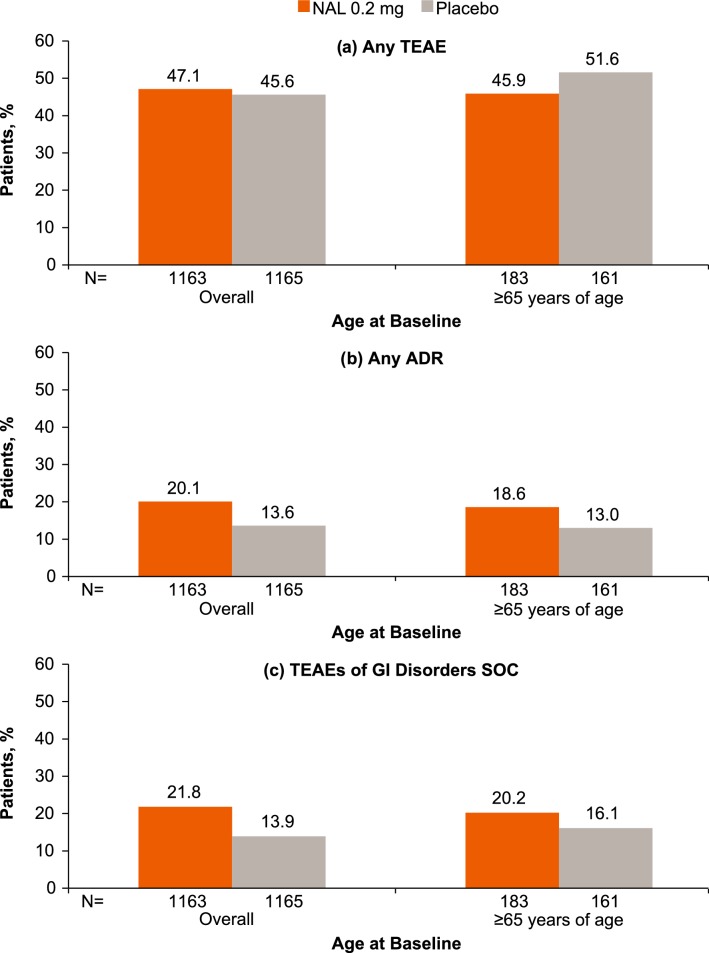
The incidence of TEAEs was similar with naldemedine in the overall patient population (47.1%) and in patients aged ≥ 65 years (45.9%) (Fig. 2a). The incidence of adverse drug reactions with naldemedine was also similar both overall (20.1%) and in patients aged ≥ 65 years (18.6%; Fig. 2b). In patients receiving placebo, the incidence of TEAEs was similar to or greater than that in patients receiving naldemedine, and the incidence of adverse drug reactions was lower than that in patients receiving naldemedine for the overall patient population and for patients aged ≥ 65 years of age.
Fig. 2.
Incidence of any TEAE (a), any ADR (b), and TEAEs of GI disorders SOC (c) by age at baseline (safety population). ADR adverse drug reaction, GI gastrointestinal, SOC system organ class, TEAE treatment-emergent adverse event
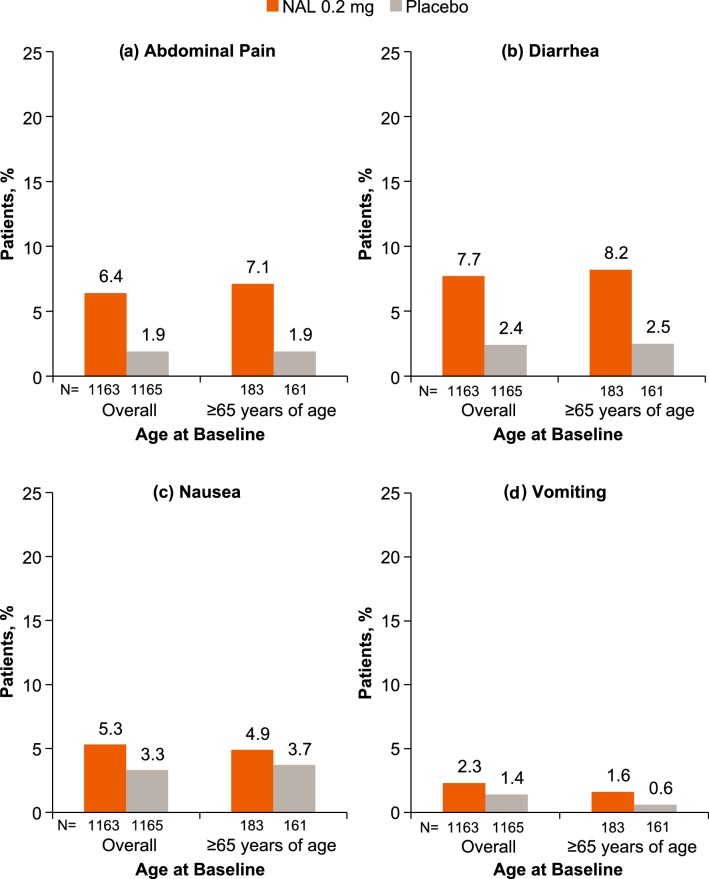
GI TEAEs were reported in 37 of 183 patients (20.2%) aged ≥ 65 years who received naldemedine and 253 of 1163 patients (21.8%) in the overall patient population who received naldemedine; a lower incidence of GI TEAEs was reported in patients receiving placebo for both the overall patient population and patients aged ≥ 65 years (Fig. 2c). The incidence of the most common GI disorders reported in patients who received naldemedine, including abdominal pain, diarrhea, nausea, and vomiting, was similar in patients aged 65 years or older to the incidence in the overall patient population (Fig. 3). Again, a lower incidence of these GI disorders was reported in patients receiving placebo for both the overall patient population and patients aged ≥ 65 years.
Fig. 3.
Incidence of abdominal pain (a), diarrhea (b), nausea (c), and vomiting (d) by age at baseline (COMPOSE-1, COMPOSE-2, and COMPOSE-3 safety population). NAL naldemedine
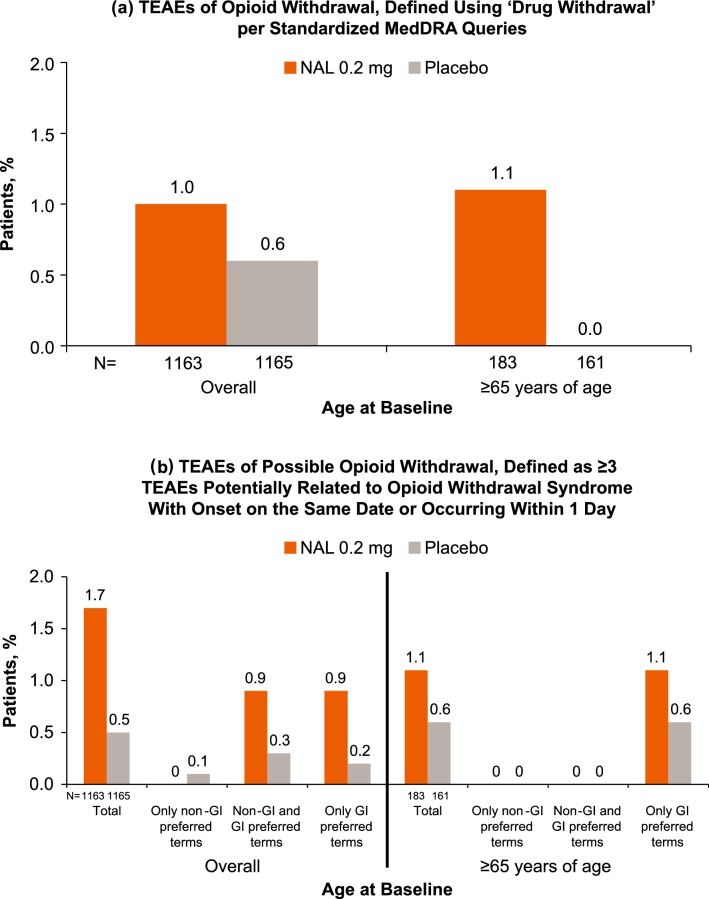
The incidence of TEAEs of opioid withdrawal and possible opioid withdrawal is shown in Fig. 4. Opioid withdrawal was reported in 12 of 1163 patients (1.0%) treated with naldemedine overall and in two of 183 patients aged ≥ 65 years (1.1%); the incidence in the placebo groups ranged from 0% to 0.6%. Overall, possible opioid withdrawal was identified in 20 of 1163 naldemedine patients (1.7%), all of which were characterized either solely or at least partially by GI symptoms.
Fig. 4.
TEAEs of opioid withdrawal (a) and possible opioid withdrawal (b) (COMPOSE-1, COMPOSE-2, and COMPOSE-3 safety population). GI gastrointestinal, MedDRA Medical Dictionary for Regulatory Activities, NAL naldemedine; TEAE treatment-emergent adverse event
There were two cases of possible opioid withdrawal identified in patients aged ≥ 65 years receiving naldemedine (1.1%), both of which were characterized solely by GI symptoms. The incidence of possible opioid withdrawal in patients receiving placebo was 0.5% in the overall patient population and 0.6% in patients aged ≥ 65 years.
Efficacy
The intent-to-treat population included 1095 patients from the COMPOSE-1 and COMPOSE-2 studies. The distribution of demographics and baseline medical characteristics in the intent-to-treat population was similar to that of the integrated safety population (Table 1). Of the 549 patients treated with naldemedine, 83 (15.1%) were aged ≥ 65 years, and of the 546 patients who received placebo, 85 (15.6%) were aged ≥ 65 years. Most patients were white (overall 80.8%; ≥ 65 years 86.9%) and female (overall 60.5%; ≥ 65 years 57.7%). Patients’ mean duration of opioid use prior to screening was 59.2–61.1 months for the overall population and 55.6–58.9 months for patients aged ≥ 65 years, mean daily morphine equivalent dose was 121.6–131.8 for the overall population and 81.5–122.6 for patients aged ≥ 65 years, and 451 patients (41.2%) overall and 47 patients (28.0%) aged ≥ 65 years used > 100 mg morphine equivalent dose daily.
Overall, there were significantly more responders in the naldemedine group [50.1% (275/549)] than in the placebo group [34.1% (186/546); difference (95% confidence interval) 16.0% (10.2–21.8); p < 0.0001]. Likewise, among patients aged ≥ 65 years, more patients in the naldemedine group [51.8% (43/83)] were responders compared with the placebo group [37.6% (32/85); difference (95% confidence interval) 12.6% (− 2.3 to 27.5)].
Discussion
This integrated analysis evaluated the safety and efficacy of naldemedine 0.2 mg once daily for 12 weeks in patients aged ≥ 65 years with chronic non-cancer pain and OIC using data from the phase 3 clinical studies. Treatment with naldemedine was shown to be generally well tolerated compared with placebo in aged patients ≥ 65 years from the COMPOSE-1, COMPOSE-2, and COMPOSE-3 clinical studies. The incidence of overall TEAEs, adverse drug reactions, and TEAEs in the GI disorders System Organ Class in patients ≥ 65 years of age was consistent with that in the overall patient population, and GI-related TEAEs occurred more frequently in the naldemedine group compared with the placebo group in the overall patient population and in patients ≥ 65 years of age. This observation is expected due to the mechanism of action of naldemedine, which reverses the effects of opioids on µ-opioid receptors in the GI tract [11]. The overall incidence of TEAEs of opioid withdrawal or possible opioid withdrawal was low in both the naldemedine and placebo treatment groups in the overall patient population and in patients ≥ 65 years of age, and all TEAEs of possible opioid withdrawal in the naldemedine group were solely or partially related to GI symptoms.
These results compare favorably with other orally available PAMORAs currently approved for the treatment of OIC. A pooled safety analysis of naloxegol studies suggested no increase in adverse events in patients aged ≥ 65 years [17], but data in Japanese patients showed higher exposure in older patients than in younger patients, although no dose adjustment is recommended [18]. Likewise, available information indicates oral methylnaltrexone is effective in patients aged ≥ 65 years, but a higher incidence of diarrhea (data not specified) was reported in older patients [19]. Results from our analysis found that diarrhea was the most commonly occurring GI disorder in patients aged ≥ 65 years receiving naldemedine; however, the incidence of diarrhea in the subgroup of patients aged ≥ 65 years (8.2%) was similar to that in the overall patient population (7.7%), which suggests that the occurrence of this adverse event in patients receiving naldemedine is not influenced by age.
Integrated data from the COMPOSE-1 and COMPOSE-2 studies showed that the proportion of responders in patients ≥ 65 years of age was consistent with the overall patient population and that the percentage of responders was higher with naldemedine than with placebo both in patients aged ≥ 65 years and in the overall patient population.
A limitation of this analysis is that it is a post hoc subgroup analysis. However, the large sample size for the integrated safety population (n = 2328), which includes patients across the COMPOSE-1, COMPOSE-2, and COMPOSE-3 clinical studies, provides a robust data set for comparison of safety and tolerability in the overall patient population versus patients aged ≥ 65 years (n = 344). The sample size for the intent-to-treat population from COMPOSE-1 and COMPOSE-2 was smaller (overall n = 1095; ≥ 65 years of age n = 168); however, the results in the subgroup of patients ≥ 65 years of age were also consistent with the overall patient population.
The results of this integrated analysis support the safety and efficacy of naldemedine in the treatment of OIC. An increase in age does not result in different tolerability and a different safety profile for naldemedine, nor is the efficacy of naldemedine affected by an increase in age.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Editorial and writing support was provided by Bina Patel, PharmD, of Peloton Advantage, LLC, an OPEN Health company.
Compliance with Ethical Standards
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committees (see the electronic supplementary material, Online Resource 1) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the studies.
Funding
These studies were sponsored by Shionogi Inc., Florham Park, NJ. BDSI owns full rights to commercialize Symproic® (naldemedine) tablets 0.2 mg in the US for opioid-induced constipation. Editorial and writing support was funded by Shionogi Inc.
Conflict of interest
James Wild received a stipend from Shionogi Inc. for review of the clinical study report. Lynn R. Webster has received honoraria for consultation from Daiichi Sankyo, Insys, Mallinckrodt, Merck, Pain Therapeutics, Pfizer, Shionogi, Teva, Trevena, and Vallon; honoraria for work on advisory boards from BDSI, Ensysce Biosciences, Mallinckrodt, Neurana Pharmaceuticals, Pfizer, and Trevena; and travel expenses from BDSI, Daiichi Sankyo, Ensysce, Elysium, Insys, Mallinckrodt, Pain Therapeutics, Pfizer, Shionogi, Teva, and Trevena. Martin Hale was a consultant to Shionogi Inc. and received a stipend for review of the clinical study report. Tadaaki Yamada is an employee of Shionogi Inc. who may or may not own stock options.
Data availability statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
- 1.Noori SA, Aiyer R, Yu J, White RS, Mehta N, Gulati A. Nonopioid versus opioid agents for chronic neuropathic pain, rheumatoid arthritis pain, cancer pain and low back pain. Pain Manag. 2019;9(2):205–216. doi: 10.2217/pmt-2018-0052. [DOI] [PubMed] [Google Scholar]
- 2.Camilleri M, Drossman DA, Becker G, Webster LR, Davies AN, Mawe GM. Emerging treatments in neurogastroenterology: a multidisciplinary working group consensus statement on opioid-induced constipation. Neurogastroenterol Motil. 2014;26(10):1386–1395. doi: 10.1111/nmo.12417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coyne KS, Margolis MK, Yeomans K, King FR, Chavoshi S, Payne KA, et al. Opioid-induced constipation among patients with chronic noncancer pain in the United States, Canada, Germany, and the United Kingdom: laxative use, response, and symptom burden over time. Pain Med. 2015;16(8):1551–1565. doi: 10.1111/pme.12724. [DOI] [PubMed] [Google Scholar]
- 4.Gupta S, Patel H, Scopel J, Mody RR. Impact of constipation on opioid therapy management among long-term opioid users, based on a patient survey. J Opioid Manag. 2015;11(4):325–338. doi: 10.5055/jom.2015.0282. [DOI] [PubMed] [Google Scholar]
- 5.Pergolizzi J, Boger RH, Budd K, Dahan A, Erdine S, Hans G, et al. Opioids and the management of chronic severe pain in the elderly: consensus statement of an International Expert Panel with focus on the six clinically most often used World Health Organization Step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone) Pain Pract. 2008;8(4):287–313. doi: 10.1111/j.1533-2500.2008.00204.x. [DOI] [PubMed] [Google Scholar]
- 6.Rosti G, Gatti A, Costantini A, Sabato AF, Zucco F. Opioid-related bowel dysfunction: prevalence and identification of predictive factors in a large sample of Italian patients on chronic treatment. Eur Rev Med Pharmacol Sci. 2010;14(12):1045–1050. [PubMed] [Google Scholar]
- 7.Chokhavatia S, John ES, Bridgeman MB, Dixit D. Constipation in elderly patients with noncancer pain: Focus on opioid-induced constipation. Drugs Aging. 2016;33(8):557–574. doi: 10.1007/s40266-016-0381-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Emmanuel A, Johnson M, McSkimming P, Dickerson S. Laxatives do not improve symptoms of opioid-induced constipation: results of a patient survey. Pain Med. 2017;18(10):1932–1940. doi: 10.1093/pm/pnw240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allen C, Zarowitz BJ, O’Shea T, Datto C, Olufade T. Clinical and functional characteristics of nursing facility residents with opioid-induced constipation. Consult Pharm. 2017;32(5):285–298. doi: 10.4140/TCP.n.2017.285. [DOI] [PubMed] [Google Scholar]
- 10.Lamas K, Karlsson S, Nolen A, Lovheim H, Sandman PO. Prevalence of constipation among persons living in institutional geriatric-care settings - a cross-sectional study. Scand J Caring Sci. 2017;31(1):157–163. doi: 10.1111/scs.12345. [DOI] [PubMed] [Google Scholar]
- 11.Symproic [package insert]. Florham Park: Shionogi Inc.; 2018.
- 12.Symproic® (naldemedine) approved for the treatment of opioid-induced constipation in Japan [press release]. 2017. http://www.shionogi.eu/media/402717/e170330_2-symproic-approved-for-treatment-of-oic-in-japan.pdf. Accessed 22 Apr 2019.
- 13.European Medicines Agency. Rizmoic (naldemedine). 2019. https://www.ema.europa.eu/en/medicines/human/EPAR/rizmoic. Accessed 24 July 2019.
- 14.Streicher JM, Bilsky EJ. Peripherally acting micro-opioid receptor antagonists for the treatment of opioid-related side effects: mechanism of action and clinical implications. J Pharm Pract. 2017:897190017732263. [DOI] [PMC free article] [PubMed]
- 15.Hale M, Wild J, Reddy J, Yamada T, Arjona Ferreira JC. Naldemedine versus placebo for opioid-induced constipation (COMPOSE-1 and COMPOSE-2): two multicentre, phase 3, double-blind, randomised, parallel-group trials. Lancet Gastroenterol Hepatol. 2017;2(8):555–564. doi: 10.1016/S2468-1253(17)30105-X. [DOI] [PubMed] [Google Scholar]
- 16.Webster LR, Nalamachu S, Morlion B, Reddy J, Baba Y, Yamada T, et al. Long-term use of naldemedine in the treatment of opioid-induced constipation in patients with chronic non-cancer pain: a randomized, double-blind, placebo-controlled phase 3 study. Pain. 2018;159(5):987–994. doi: 10.1097/j.pain.0000000000001174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tummala R, Diva U, Sostek M. Treatment with naloxegol versus placebo: safety assessment in patients aged ≥ 65 years with noncancer pain and opioid-induced constipation [abstract Sa1398] Gastroenterology. 2015;148(4 suppl 1):s-314. doi: 10.1016/S0016-5085(15)31036-2. [DOI] [Google Scholar]
- 18.Movantik [package insert]. Wilmington: AstraZeneca Pharmaceuticals; 2018.
- 19.Relistor [package insert]. Bridgewater: Salix Pharmaceuticals; 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.