Abstract
Changing lifestyles reduce the time spent by children on physical activity during the day. The result is an increasing frequency of childhood obesity, which has become one of the most common chronic diseases of childhood. Furthermore, the treatment of obesity in childhood is quite difficult, and the most common problem is non-compliance with obesity treatment. The path that will facilitate the adaptation to treatment comprises nutrition regulation and increased daily physical activity and psychological support. Diet alone leads to a significant reduction in both fat and non-fat body mass. However, adding exercise to dietary therapy improves weight loss by maintaining non-fat body mass. Even though exercise alone has little effect on weight loss, it provides a significant reduction in mortality. Moreover, regular physical exercise is also an important factor in regulating body composition during growth. However, changes in the child’s body during growth affect the motor power and performance, so it is necessary to plan the exercise according to the individual characteristics, age and sex of the child. Short-term frequent exercises are more entertaining and more accessible forms of exercise (dancing at home) for children, and enhance compliance with treatment. Starting treatment as soon as possible will also increase behavioral effectiveness and compliance. This paper focuses on the basics of exercise therapy, which is extremely beneficial for both healthy and obese children.
Keywords: Childhood, compliance to treatment, obesity, obesity treatment, physical exercise
Abstract
Değişen yaşam biçimleri çocuklarda gün içinde hareketli geçen süreyi azaltmaktadır ki, sonuç çocuklarda obezite sıklığının giderek artması ve çocukluk çağının en sık görülen kronik hastalıklarından birisi haline gelmesidir. Dahası, çocukluk döneminde obezite tedavisi oldukça zordur ve çocuklarda obezite tedavisinde uyumsuzluk en sık görülen sorundur. Tedaviye uyumu kolaylaştıracak yol sadece beslenme düzenlenmesi değil, fiziksel aktivite ile birlikte psikolojik desteğin de verilmesidir. Diyet tek başına hem yağ hem de yağ dışı vücut kütlesinde belirgin azalmaya neden olur, ancak, diyet tedavisine egzersiz eklenmesi yağ dışı vücut kütlesini koruyarak kilo kaybını artırır. Egzersiz tek başına az kilo kaybı yapsa da, ölüm oranında önemli azalma sağlar. Düzenli fiziksel egzersiz, büyüme sırasında vücut kompozisyonunun düzenlenmesi için de önemli bir etkendir. Ancak, büyüme sırasında çocukların bedeninde meydana gelen değişimler motor gücü ve performansı etkiler. Bu yüzden çocuğun bireysel özellikleri, yaşı ve cinsiyetine göre egzersiz planı yapmak gerekir. Çocuklara verilecek kısa süreli sık egzersizler daha eğlenceli ve daha erişilebilir bir egzersiz şeklidir (evde dans etmek vb.) ve tedaviye uyumu artırır. Tedavinin mümkün olan en kısa zamanda başlanması da davranış tedavisi etkinliğini ve uyumu artıracaktır. Bu yazıda hem sağlıklı hem de obez çocuklar için son derece yararı olan ve çoğunlukla ihmal edilen egzersiz tedavisinin esasları üzerinde durulacaktır.
Introduction
Although obesity has been defined as the most common health problem in modern societies; currently, it is a problem with gradually increasing frequency both in developed and developing countries. Different studies conducted in Turkey also showed similar results [the prevalence of obesity is 40.0% in men and 50.0% in women according to the Turkey Obesity and Hypertension Research (1), 38% in women and 22% in men according to the results of the Turkey Diabetes, Hypertension, Obesity and Endocrinological Diseases Prevalence Study-II (TURDEP II) (2), and 16.9% in men and 48.4% in women (total prevalence 34.3%) according to the Turkey Obesity Profile (3)].
Obesity is also considered one of the most common chronic diseases in childhood. In a study conducted in 17 countries by the World Health Organization (WHO), the prevalences of overweight and obesity were reported as 15% and 6,6%, respectively, in school-age children in Turkey (4). Considering that childhood obesity continues into adulthood, and leads to a predisposition to many chronic diseases, the importance of fighting obesity in this period is clear.
Treatment of childhood obesity is considerably difficult. Poor patient motivation and inability of parents to spare time for their children have been reported as the most important factors that cause low treatment efficiency in children and adolescents (5). Children who are stuck among courses/classes in an exam marathon with career anxiety cannot find time for physical activity and even for referring to healthcare institutions for these problems. As a result, we confront non-compliance with obesity treatment in children as the most common problem. In our previous study, non-compliance with obesity treatment was found with a rate of 63% in children in Kırıkkale, and this rate was reported as 32.5% by Akbaş et al. (6) in Istanbul in patients presenting to an adult obesity outpatient clinic (7). When the two studies were compared, it was noted that non-compliance with treatment was higher in children. Murtagh et al. (8) performed focus group discussions in obese children, and showed the obstacles to treatment success with different aspects. According to this study, continuance of the activities recommended for treatment was impossible without constant emotional support presented at individual level. Obstacles to support were defined as inability to abandon present habits, delayed recognition of the problems by parents, and negative experiences at previous presentations to healthcare institutions because of being overweight (8).
For successful treatment, the causes of obesity should primarily be identified accurately, and good team work is essential. In the treatment of obese children, cooperation of pediatricians, psychiatrists (Child-Adolescent), dieticians, and sports physicians, if possible, will provide an increase in treatment compliance and positive outcomes (9). In addition to team work, another way to enhance treatment compliance includes adjusting nutrition and providing psychological support together with physical activity (Table 1). Moreover, cooperation with families, social circles, and teachers is also essential in establishing permanent and positive behavioral changes in children.
Table 1.
Approach in long-term follow-up of obesity treatment
| 1. Reducing calorie intake |
| 2. Increasing exercise |
| 3. Motivation for behavioral modification |
| 4. Drug therapy |
| 5. Surgery |
According to the evaluation made by the United Kingdom Health Promotion Agency, as a result of examining meta-analysis studies, body weight-reducing studies applied to overweight/obese children are gathered under five main headings: a) family-based physical activity and interventions for encouraging and promoting health, b) family-based programs that consider parents the main element of change, c) family-based behavioral modification programs, d) behavioral modification programs that do not include parents, and e) exercise treatment programs alone (4). The agency reported that community education rarely influenced behavioral modifications; the most effective way to provide positive outcomes in treatment included considering the child an individual, making the child to have information and think about this issue and subsequently, choosing effective treatment methods appropriate for the child’s and family’s daily life dynamics (4).
The efficiency of behavioral therapy in the treatment of obesity is also associated with the child’s age and the degree of obesity. In a study conducted by Danielsson et al. (10), no significant reduction in body weight (BMI-score) was found in adolescents aged between 14 and 16 years as a result of 1-2–year and 3-year behavioral therapy. However, more efficient outcomes were obtained in the 6–8 years’ age group with severe obesity compared with children who had moderate obesity and the 14–16 years’ age group. These results indicate that initiating treatment as soon as possible increases the efficiency of behavioral therapy and treatment compliance (10, 11).
This article will emphasize the fundamentals of exercise treatment, which is very helpful for both healthy and obese children, and is mostly ignored.
Daily activity status in children
Changing lifestyles reduces the daily time period during which children are active. Television and computers are factors for this change, and insufficient recreation/play areas in districts of low development levels, the fact that families do not give permission for their children to play outside because of unsafe external environments, and transportation of children to school by vehicles are the main causes that lead to a reduction in physical activity. Unfortunately, a child involuntarily stuck at home burns very little energy with indoor activities (e.g. watching TV, sitting, staying in front of a screen, reading) (12). After a sedentary lifestyle is established, it is very difficult to develop behavioral modification in daily life. The parents’ behaviors and control are ineffective in increasing indoor energy expenditure, but indoor exercises that will enable the child to move with fun like playing, and interactive video games instead of TV are considered significant tools to increase activity (12).
There are numerous studies evaluating the association between physical activity and overweight and obesity in children and adolescents (13–15). These studies have found a positive correlation between reduced physical activity and overweight and obesity. Mostly, exercise (walking, swimming, running, jogging, and aerobics) and outdoor sports (volleyball, soccer, cricket, badminton and table tennis) are defined as physical activity. In these studies, children’s activity times were generally shorter than 30 minutes daily and less than 2 hours weekly (16, 17).
Physical activity tends to decrease especially in the 11–15-year age group. In most European Union countries, physical activity levels in girls aged 15 years are lower compared with the 11 years’ age group, and this proportional reduction reaches up to 60% in some other countries (18).
The Turkey Nutrition and Health Survey reported that the mean time spent by children aged between 2 and 5 years for sedentary activity (TV, computer, internet) in 2010 was 3.46 hours (3.51 hours for boys, 3.40 hours for girls). The level of regular exercise was considerably low; 58.4% of the children in the 6–11 years’ age group, 67.6% of the boys aged over 12 years, and 76.5% of the girls aged over 12 years did not exercise regularly (30 minutes or longer daily) (19).
Exercise model to recommend for children
Total and visceral adipose depots decrease, lean mass index increases, energy consumption at rest, and the insulin sensitivity of adipose tissue increases with exercise. In addition, the vessels improve endothelial function, and free fatty acids, low-density lipoprotein (LDL) cholesterol and triglyceride levels decrease, high-density lipoprotein (HDL) cholesterol increases, and metabolic and cardiovascular complications are reduced (20). Lean body mass is the most important factor that determines basal metabolism rate. Therefore, exercises that aim at increasing muscle mass are generally recommended. Exercise alone provides little weight reduction, but causes a significant reduction in mortality rates because of the above-mentioned effects.
Regular physical exercise is an important factor for the regulation of body composition during growth. However, the point to be noted is that changes occurring in children’s bodies during growth influence motor strength and performance. Therefore, exercise should be planned according to the child’s individual characteristics, age, and sex (21).
Lean body mass develops with a two-fold higher rate in boys compared with girls when transferring from early adolescence to late adolescence. In girls, however, adipose mass develops with a two-fold higher rate compared with boys. Great lean mass is important in terms of exercises that need strength including pushing and weightlifting. However, this is the exercise type that should be limited during this period; jumping or sprinting should be recommended more. Generally, exercises that increase strength are recommended at the end of somatic growth after the age of 16–18 years (late adolescence) (21).
Exercise types and examples for children (22):
Aerobic exercise: This type of exercise increases heart rate and respiratory strength. Examples include: skateboarding, paddle, dancing, basketball, soccer, volleyball, tennis, swimming, gymnastics, jumping rope, house cleaning, running, and cycling.
Muscle strengthening: climbing a rope, tree, rock, push-ups, weightlifting
Bone strengthening: Recommended to perform at least three times weekly, e.g. jumping rope, climbing mountain, walking, basketball, volleyball, running.
Extension (Strain): Causes muscles to become more elastic and there is less risk of injury, e.g. yoga, dancing, gymnastics.
In exercise recommendations for children, exercise programs corresponding to the English acronym FITT (Frequency, Intensity, Time, and Type), which means having a high level of conditioning, are recommended (Table 2) (20). Table 3 describes the intensity of exercise. Table 4 shows physical exercise programs that can be recommended by applying the FITT principles in children and adolescents, and Figure 1 shows a weekly activity pyramid.
Table 2.
Compatibility recommendations in exercise treatment in obesity (FITT) (20)
| Frequency: Frequent/each day of the week |
| Intensity: 55–90% of maximum heart rate |
| Time: 30–80 minutes |
| Should increase gradually |
| Beginning; 10 minutes of walking, 3–5 days/week |
| Continued; 60–80 min, almost every day /week |
| Type: Aerobic, resistant |
Table 3.
Exercise intensity (20)
| Intensity | % MVC | Effect on strength |
|---|---|---|
| Low | <20 | Almost none |
| Moderate | 20–50 | Rehabilitating |
| High | 50–70 | Increases muscle strength to optimal level |
| Very high | >70 | Increases muscle mass to optimal level |
MVC: maximum voluntary contraction
Table 4.
Physical exercise programs that can be recommended by applying FITT principles in children and adolescents (20, 23)
| FITT | Cardiovascular (aerobic) program | Interval program | Muscle resistance program |
|---|---|---|---|
| Frequency | ≥3/week | ≥3/week | 2–3/week |
| Intensity | Moderate-severe exercise | 3–5 min. Mild-moderate | High (50–70% MVC) |
| Interrupting for 6–8 times | |||
| 1–3 min high intensity exercise | |||
| Time | 20–60 min | Total 20–60 min | 2–3 min. per muscle group (8–20 repetitions) Total ≥30 |
| Type | Running, jumping, biking Swimming, soccer | Running, jumping swimming, biking | push-ups, climbing paddle |
| Program duration | 8–12 weeks | 6–12 weeks | 6–12 weeks |
FITT: Frequency, intensity, time, and type; MVC: Maximum voluntary contraction
Figure 1.
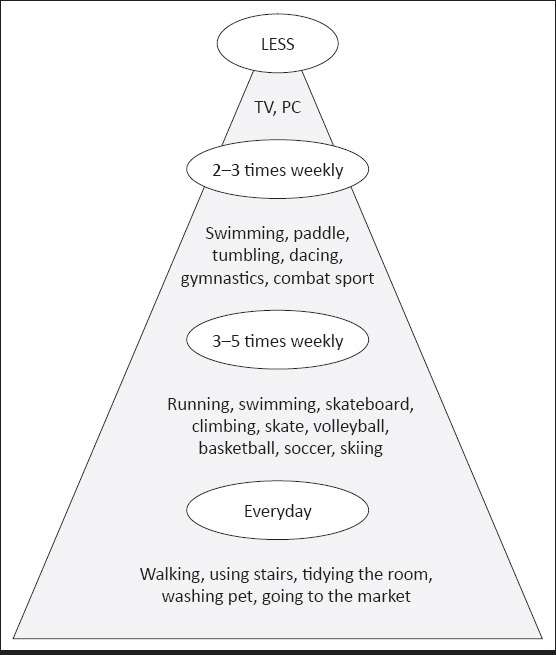
Weekly activity pyramid in children and adolescents
Addition of moderate aerobic exercise to diet therapy increases weight loss slightly. During weight loss, aerobic exercise decreases loss of lean mass, and resistance exercise enhances weight loss while preserving lean mass. Diet alone causes a marked reduction in lean body mass (LMN) in addition to reducing fat. However, aerobic exercise preserves LMV (less LMV loss occurs as BMI increases) (24). In addition, exercise may contribute to weight loss by leading to a behavioral change enabling children to pay attention to their diets.
In children, starting with very high intensity exercise may cause injuries. Therefore, one should start with low intensity exercise and the intensity should be increased gradually. Programs given to children are not different from adults. One may need to prepare more entertaining short programs for children because they may easily become bored and discontinue the program. Generally, all exercise programs should consist of a dynamic warm-up period of 10–15 minutes, an educational exercise period of 20–60 minutes, and a cooling period that includes low intensity movements (21, 24).
It has been reported that combined exercise is more efficient compared with weightlifting exercises alone in correcting insulin resistance, but resistance exercises are more efficient in increasing lean body mass in obese children (25).
It has also been reported that weightlifting exercises in overweight and obese children causes an increase in lean body mass and a reduction in body fat percentage (26). In a comparison of two groups who were made to perform 2–4 sets of resistance exercise, it was reported that both exercise types were efficient in total fat loss, but resistance exercises were more efficient in increasing lean body mass (27).
Any type of exercise provides weight loss, if it is performed for at least 4–10 hours weekly, and children may adapt better to frequent and short-term exercises. It is a more entertaining and more accessible type of exercise (e.g. dancing at home). However, the efficiency of this type of activity is controversial. Donnelly et al. (28) investigated the effect of intermittent and continuous exercise performed for 18 months on body weight and its components in obese women. In the continuous exercise group, the subjects walked for at least 30 minutes 3 days a week such that 60–75% of body O2 consumption was provided. In the intermittent exercise group, the subjects walked for 15 minutes 2 times a day for 5 days, weekly. Body weight was reduced by 2.1% in the continuous exercise group, whereas no reduction was found in the intermittent exercise group. Although the results of this study suggest that frequent short-term exercises are not efficient, it would be appropriate to encourage children to perform short-term activities rather performing no activity.
The International Association for the Study of Obesity (IASO) recommends that adults perform moderate physical activity for at least 30 minutes each day of the week to prevent chronic diseases and protect health. However, this activity level is not sufficient for weight loss or for preserving body weight. Obese individuals should perform mild-moderate exercise at least 60–90 minutes daily and normal individuals should perform moderate exercise at least 45–60 minutes daily to avoid obesity (29). Examples of moderate intensity exercise are shown in Table 5. At the beginning and in individuals with very sedentary lifestyles, one should begin with very low intensity exercise, and the intensity should be increased according to patient compliance. In children, these exercise levels should be higher; participation in moderate-high intensity physical activity at least 60 min/day is recommended (5).
Table 5.
Types of moderate exercise that can burn 150 kcal (22)
| Daily activities | Sports activities | |
|---|---|---|
| Washing or polishing a car for 45–60 min | Playing volleyball for 45–60 min | Less tiresome, more time consuming |
| Washing windows or the floor for 45–60 min | Playing with soccer ball for 45–60 min | |
| Gardening for 30–45 min | Walking 1.5 km in 35 min | |
| Using wheelchair for 30–40 min | Shooting a basketball for 30 min | |
| Pushing a wheel for 30 min for 2 km | Biking 6 km in 30 min | |
| Walking 2.5 km in 30 min | Dancing swiftly for 30 min | More tiresome, less time consuming |
| Climbing stairs for 15 min | Exercising in water for 30 min | |
| Swimming cycles for 20 min | ||
| Playing basketball for 15–20 min | ||
| Biking 5 km for 15 min | ||
| Jumping rope for 15 min | ||
| Running 2 km in 15 min |
In a meta-analysis study conducted with overweight and obese children, it was found that a 0.4% (0.1–0.7%) reduction in body fat occurred with moderate-high intensity physical activity performed for 155–180 minutes weekly, though marked weight loss was not obtained (30). In conclusion, an exercise program that included moderate exercising for 10–45 minutes 3–5 days weekly or 60–80 minutes every day in the beginning, and targeted consumption of 1000–2000 kcal, was recommended. An entertaining exercise program for at least 1 hour every day was recommended for children aged 6 years and older and free playing programs were recommended for young children (30).
The Korean Pediatric Gastroenterology Hepatology and Nutrition Obesity Group classified obesity treatment and exercise strategies in four steps (11).
Step 1: Strategies for protection against obesity will be applied and physical activity will be performed for one hour or less. Unstructured physical activity for young children and entertaining physical activities for older children.
Step 2: Structured and planned exercise under supervision for 1 hour every day.
Step 3: Specification of physical activity targets in multidisciplinary obesity treatment. Exercise plan targeting negative energy balance.
Step 4: Appropriate exercise program in addition to drug and surgical treatment options.
The Korean Group’s treatment plan according to age and the degree of obesity in children is shown in Table 6.
Table 6.
Exercise treatment strategies according to age and the degree obesity in children
| Age group | Degree of obesity | Primary option | Advanced option |
|---|---|---|---|
| Infant (≤2 years) | Weight for height ≥95th pc | Preventive precautions | Preventive precautions |
| Early childhood (2–5 y) | BMI 5–84th pc | Preventive precautions | Preventive precautions |
| BMI 85–94th pc risk Ø | Preventive precautions | Preventive precautions | |
| BMI 85–94th pc risk present | Step 1 | Step 2 | |
| BMI ≥95th pc | Step 1 | Step 3 | |
| School-age child (6–11 y) | BMI 5–84th pc | Preventive precautions | Preventive precautions |
| BMI 85–94th pc risk Ø | Preventive precautions | Preventive precautions | |
| BMI 85–94th pc risk present | Step 1 | Step 2 | |
| BMI 95–99th pc | Step 1 | Step 3 | |
| BMI ≥99th pc | Step 1 | Step 3 | |
| If the family is motivated | If appropriate | ||
| Step 2 or 3 | Step 4 | ||
| Adolescent (12–18 y) | BMI 5–84th pc | Preventive precautions | Preventive precautions |
| BMI 85–94th pc risk Ø | Preventive precautions | Preventive precautions | |
| BMI 85–94th pc risk present | Step 1 | Step 2 | |
| BMI 95–99th pc | Step 1 | Step 3 | |
| BMI ≥99th pc | Step 1 | Step 3 | |
| If the family is motivated | If appropriate | ||
| Step 2 or 3 | Step 4 |
BMI: Body mass index
In a different program, it was recommended that exercise programs in children with obesity should begin with 20 minutes three days a week, the exercise duration should be prolonged to 30–60 minutes subsequently, and exercise should be performed every day, if possible (31). It has been reported that exercises that burn 100–200 kcal/day (total energy consumption 1000 kcal/week) should be selected, and exercises should be adjusted such that joint loading is avoided, especially in individuals who have back, knee or heel pain. The same group emphasized that physical activity had to be pursued together with calorie limitation for efficient weight loss. The easiest activity for obese individuals is walking. Walking should be increased gradually up to 12 000 steps a day. One or two sets of weightlifting exercises with 8–10 repetitions that train main muscle groups 1–2 days a week are also recommended.
Physical activity and cardiovascular exercise are very important factors for controlling body weight and for health. Being thin does not guarantee perfect health. Walking to school, playing during breaks, hiking, going for a walk with a dog, and shortening screen time (less time for TV and computer) may be recommended for children in order to increase physical activity. It should be kept in mind that doing physical exercise is preventive against cardiovascular disease and cardiopulmonary risk factors, but other complications including obesity-associated osteoarthritis, reduced quality of life, social discrimination, and functional limitations persist. In other words, exercise alone is not sufficient in the prevention and treatment of obesity, and must be applied in combination with calorie reduction.
In adults, a 500 kcal negative energy balance is targeted daily in weight loss programs. The duration of exercise required is 2 hours to provide this negative energy balance. It has been reported that it is not possible for obese individuals to reach this duration regularly (25). Only two-thirds of obese individuals state that they partake in exercise for weight loss, one-fifth state that they can perform exercise for the recommended time period and at the recommended level (30 min/day/every day), and 20% state they cannot perform exercise because they feel too obese and heavy (32). Farris et al. (33) arranged a 12-week activity program that included physical exercise for two days and an entertaining activity program for one day weekly for children aged between 6 and 12 years together with their families in Arkansas. Although a significant reduction in body measurements occurred in the children at the end of this study, 51% of the children left the study. In other words, sustainability of exercise treatment is not so possible. Considering this finding, European Union 2008 Instructions included a statement recommending that school-age children should participate in moderate-high intensity physical activity at least 60 minutes daily (21).
In conclusion, treatment of obesity is difficult. Therefore, the easiest way is prevention. In prevention, the 5-2-1-0 rule (5 or more vegetables and fruit, sitting in front of the TV/computer for less than 2 hours, physical activity for at least 1 hour daily, and zero sugary drinks) seems to be the easiest recommendation (Table 7) (22, 23).
Table 7.
Feasible exercise recommendations in prevention of obesity
| 5 - 2 – 1 – 0 Rule; |
| 5 or more vegetables and fruit |
| Sitting in front of the TV/computer and inactivity for less than 2 hours |
| 1 hour of structured physical activity |
| Low-fat milk or water instead of sugary drink |
| 10 000 steps each day (2000 steps in excess daily burns 100 calorie) (difficult in children, but they should be informed) |
| Participation in moderate-high intensity physical activity at least 60 min/day weekly is recommended for children and adolescents, but this time period should be 90 minutes for reducing insulin resistance and cardiovascular risk. Glucose and glycogen are oxidized primarily with exercise, and fat oxidation begins in 90–120 minutes. |
| The benefit of exercise persists for 24–72 hours. Therefore, physical activity should be pursued for at least 3 times weekly |
| All types of exercise provide weight loss if its duration is at least 4–10 hours/week |
| Children may comply better with frequent short-term exercises |
Obesity epidemics should be evaluated well to prevent a rapid increase of this health problem in the twentieth century. Treatment of obesity is considerably long and the possibility of treatment failure is high. Therefore, treatment objectives should be specified accurately.
Physical activity is very important for healthy children as well as for obese children with chronic problems. Preparing physical activity plans according to each child’s individual health status is very important for both prevention and treatment of obesity. A few points to be noted when specifying treatment objectives, are as follows:
a) One of the frequent mistakes is to inspire patients to think that they can rapidly lose weight.
b) Making patients reach the ideal body weight is not so effective in practice.
c) At the end of treatment, patients will probably be able to lose 5–10% of their body weights.
d) Patients should be enabled to exercise and reduce the mortality risk.
e) Regular exercise should be improved gradually.
f) Acquirement of healthy eating behavior should be provided gradually.
g)Obese children should be seen on the 15th day initially and monthly thereafter. During these follow-up visits, treatment course should be discussed, the child be encouraged, and obstacles and how these obstacles can be eliminated should be discussed.
h) At each visit, the child should be weighed and the body fat percentage should be checked; even small amounts of weight loss should be discussed with the child for motivation.
i) If necessary, evaluation in terms of blood lipid profile, blood glucose level, blood pressure, fasting/postprandial insulin levels and hepatic steatosis may be recommended at follow-up visits.
In our current modern world, it is very difficult to develop a lifestyle including a behavioral model that increases physical activity in addition to diet treatment in children. In addition, the efficiency and adverse effects of dugs recommended for use in treatment of obesity, are not yet clear in children. Therefore, the important point is prevention of obesity rather than favorable treatment.
Footnotes
Peer-review: Externally peer-reviewed.
Conflict of Interest: No conflict of interest was declared by the author.
Financial Disclosure: The author declared that this study has received no financial support.
Hakem Değerlendirmesi: Dış bağımsız.
Çıkar Çatışması: Yazar çıkar çatışması bildirmemişlerdir.
Mali Destek: Yazar bu çalışma için mali destek almadığını beyan etmiştir.
References
- 1.Hatemi H, Turan N, Arık N, Yumuk V. Türkiye Obezite ve Hipertansiyon Çalışması(TOHTA) Endokrinolojide Yönelişler Dergisi. 2002;11:1–16. [Google Scholar]
- 2.Satman I, Alagöl F, Omer B, ve ark Türkiye Diyabet, Hipertansiyon, Obezite ve Endokrinolojik Hastalıklar Prevalans Çalışması-II TURDEP II:On sonuclar. Kronik Hastalıklar Oturumu, 13. Ulusal Halk SağlığıKongresi. 2010 Ekim d18-22;İzmir. [Google Scholar]
- 3.T.C. Sağlık BakanlığıTurkiye Obezite İle Mücadele Programıve Ulusal Eylem PlanıTaslağı 2008-2012 3. Ankara: Taslak; [Google Scholar]
- 4.Whitlock E, O'Connor E, Williams S, Beil T, Lutz K. Effectiveness of weight management programs in children and adolescents. Evid Rep Technol Assess (Full Rep) 2008;170:1–308. [PMC free article] [PubMed] [Google Scholar]
- 5.Befort CA, Greiner KA, Hall S, et al. Weight-related perceptions among patients and physicians:how well do physicians judge patients'motivation to lose weight? J Gen Intern Med. 2006;21:1086–90. doi: 10.1111/j.1525-1497.2006.00567.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akbaş F, Atmaca HU, Karadaş E, Yıldız İ, Ökten İN. Evaluation of data from the obesity outpatient clinic at the end of the second year as a newly formed unit in Istanbul training and research hospital. Istanbul Med J. 2013;14:253–6. [Google Scholar]
- 7.Bülbül S, Uluğ F, Şanlı C, Kırışoğlu M Obesite Hastalarının Tedaviye Uyum Durumlarının Değerlendirilmesi SözlüBildiri. VI. Ulusal Ana Çocuk SağlığıKongresi. Antalya: Kasım 16-20; 2011. [Google Scholar]
- 8.Murtagh J, Dixey R, Rudolf M. A qualitative investigation into the levers and barriers to weight loss in children:opinions of obese children. Arch Dis Child. 2006;91:920–3. doi: 10.1136/adc.2005.085712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.August GP, Caprio S, Fennoy I, et al. Prevention and treatment of pediatric obesity:an endocrine society clinical practice guideline based on expert opinion. J Clin Endocrinol Metab. 2008;93:4576–99. doi: 10.1210/jc.2007-2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Danielsson P, Kowalski J, Ekblom Ö, Marcus C. Response of severely obese children and adolescents to behavioral treatment. Arch Pediatr Adolesc Med. 2012;166:1103–8. doi: 10.1001/2013.jamapediatrics.319. [DOI] [PubMed] [Google Scholar]
- 11.Yi DY, Kim SC, Lee JH, et al. Clinical practice guideline for the diagnosis and treatment of pediatric obesity:recommendations from the Committee on Pediatric Obesity of the Korean Society of Pediatric Gastroenterology Hepatology and Nutrition. Korean J Pediatr. 2019;62:3–21. doi: 10.3345/kjp.2018.07360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maitland C, Stratton G, Foster S, Braham R, Rosenberg M. A place for play?Theinfluence of the home physical environment on children's physical activity and sedentary behaviour. Int J Behavioral Nutrition and Physical Activity. 2013;10:99. doi: 10.1186/1479-5868-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bautista-Castaño I, Sangil-Monroy M, Serra-Majem L Comitéde Nutrición y Obesidad Infantil de la Sociedad Española de Nutrición Comunitaria. Knowledge and gaps on the role of nutrition and physical activity on the onset of childhood obesity [Article in Spanish] Med Clin (Barc) 2004;123:782–93. doi: 10.1016/s0025-7753(04)74668-0. [DOI] [PubMed] [Google Scholar]
- 14.Goyal JP, Kumar N, Parmar I, Shah VB, Patel B. Determinants of Overweight and Obesity in Affluent Adolescent in Surat City, South Gujarat region, India. Indian J Community Med. 2011;36:296–300. doi: 10.4103/0970-0218.91418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patnaik S, Patnaik L, Patnaik S, Hussain M. Prevalence of overweight and obesity in a private school of Orissa, India. The Internet J Epidemiology. 2010;10:1–5. [Google Scholar]
- 16.Kotian MS, S GK, Kotian SS. Prevalence and determinants of overweight and obesity among adolescent school children of South karnataka, India. Indian J Community Med. 2010;35:176–8. doi: 10.4103/0970-0218.62587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bharati DR, Deshmukh PR, Garg BS. Correlates of overweight &obesity among school going children of Wardha city, Central India. Indian J Med Res. 2008;127:539–43. [PubMed] [Google Scholar]
- 18.European Commission Eurostat Pocketbooks. European Social Statistics, 2013 edition European Union. [Accessed, November 9 2018]. pp. 78–79. Available from: http://ec.europa.eu/eurostat/documents/3930297/5968986/KS-FP-13-001-EN.PDF/6952d836-7125-4ff5-a153-6ab1778bd4da .
- 19.T.C. Sağlık Bakanlığı, Hacettepe Üniversitesi Sağlık Bilimleri Fakültesi Beslenme ve Diyetetik Bölümü. Türkiye Beslenme ve Sağlık Araştırması. 2010. [Accessed, February 19 2020]. Available from: https://hsgm.saglik.gov.tr/depo/birimler/saglikli-beslenme-hareketli-hayat-db/Yayinlar/kitaplar/diger-kitaplar/TBSA-Beslenme-Yayini.pdf .
- 20.Takken T, Giardini A, Reybrouck T, et al. Recommendations for physical activity, recreation sport, and exercise training in paediatric patients with congenital heart disease:a report from the Exercise, Basic &Translational Research Section of the European Association of Cardiovascular Prevention and Rehabilitation, the European Congenital Heart and Lung Exercise Group, and the Association for European Paediatric Cardiology. Eur J Prev Cardiol. 2012;19:1034–65. doi: 10.1177/1741826711420000. [DOI] [PubMed] [Google Scholar]
- 21.Taşkın G, Şahin Özdemir FN. The importance of exercise on children. Gazi J Physical Education and Sport Sciences. 2018;23:131–41. [Google Scholar]
- 22.Baltacı G. Obezite ve egzersiz. Ankara: Klasmat Matbaacılık; 2018. pp. 14–8. [Google Scholar]
- 23.Amed S, Shea S, Pinkney S, Wharf Higgins J, Naylor PJ. Wayfinding the Live 5-2-1-0 Initiative-At the Intersection between Systems Thinking and Community-Based Childhood Obesity Prevention. Int J Environ Res Public Health. 2016;13:614. doi: 10.3390/ijerph13060614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Takken T, Hulzebos EH. Exercise testing and training in chronic childhood conditions. Hong Kong Physiotherapy J. 2013;31:58–63. [Google Scholar]
- 25.Akkurt S. Obezite ve egzersiz tedavisi. Turkish J Sports Medicine. 2012;47:123–30. [Google Scholar]
- 26.Dietz P, Hoffmann S, Lachtermann E, Simon P. Influence of exclusive resistance training on body composition and cardiovascular risk factors in overweight or obese children:a systematic review. Obes Facts. 2012;5:546–60. doi: 10.1159/000341560. [DOI] [PubMed] [Google Scholar]
- 27.Pagotto U, Vanuzzo D, Vicennati V, Pasquali R. Pharmacological therapy of obesity [Article in Italian] G Ital Cardiol (Rome) 2008;9:83S–93S. [PubMed] [Google Scholar]
- 28.Donnelly JE, Jacobsen DJ, Heelan KS, Seip R, Smith S. The effects of 18 months of intermittent vs continuous exercise on aerobic capacity, body weight and composition, and metabolic fitness in previously sedentary, moderately obese females. Int J Obes Relat Metab Disord. 2000;24:566–72. doi: 10.1038/sj.ijo.0801198. [DOI] [PubMed] [Google Scholar]
- 29.Saris WH, Blair SN, van Baak MA, et al. How much physical activity is enough to prevent unhealthy weight gain?Outcome of the IASO 1st Stock Conference and consensus statement. Obes Rev. 2003;4:101–14. doi: 10.1046/j.1467-789x.2003.00101.x. [DOI] [PubMed] [Google Scholar]
- 30.Atlantis E, Barnes EH, Singh MA. Efficacy of exercise for treating overweight in children and adolescents:a systematic review. Int J Obes (Lond) 2006;30:1027–40. doi: 10.1038/sj.ijo.0803286. [DOI] [PubMed] [Google Scholar]
- 31.Alleyne JM. Safe exercise prescription for children and adolescents. Paediatr Child Health. 1998;3:337–42. doi: 10.1093/pch/3.5.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention (CDC) Prevalence of leisure-time physical activity among overweight adults--United States 1998. MMWR Morb Mortal Wkly Rep. 2000;49:326–30. [PubMed] [Google Scholar]
- 33.Farris JW, Taylor L, Williamson M, Robinson C. A 12-week Interdisciplinary Intervention Program for Children who are Obese. Cardiopulm Phys Ther J. 2011;22:12–20. [PMC free article] [PubMed] [Google Scholar]


