Abstract
Background
The family of patients undergo profound anxiety when their family member is undergoing major oncological surgery. In this study, we evaluated the effectiveness of periodic intraoperative text messages regarding the status of ongoing surgery in reducing anxiety levels among the patients’ family members.
Materials and Methods
Family members of 60 patients (one for each patient) who were undergoing major oncological surgery lasting more than 1 h were recruited and randomized into two groups (30 patients each). Group 1 (no SMS group) did not receive any text message while Group 2 (SMS group) received periodic intraoperative text messages. Respondents aged less than 16 years, those with associated psychiatric illnesses, and those who did not consent to the study were excluded. Anxiety among family members was assessed using the Visual Analogue Scale for Anxiety (VAS-A) and Anxiety component of Hospital Anxiety and Depression Scale (HADS-A) at five different periods; (P1) 1 day prior to surgery (P2) at separation from family at the operation theatre (P3) 1 h after commencement of surgery (P4) immediately after completion of surgery, and (P5) 1 day after surgery.
Results
The mean VAS-A and HADS-S scores between both the groups did not show a statistically significant difference for P1, P2 and P5 assessment periods (preoperative period, separation in operation theatre, post-operative period). However, mean VAS-A and HADS-A scores were significantly higher for Group 1 compared to Group 2 during P3 and P4 periods, 1 h after commencement of surgery and completion of surgery, respectively.
Conclusion
Periodic text messages updating the status of ongoing surgery helps to reduce anxiety for family members of patients undergoing oncological surgery during the intraoperative period.
Keywords: Intra-operative, Text message, Anxiety
Introduction
Musculoskeletal malignancies are distressful due to its prolonged duration of disease, expensive treatment cost, complex and extensive nature of surgery, and risk of relapse and poor survival. Thus, these patients and their family members are normally under profound psychological stress and anxiety. Anxiety may lead to headache, insomnia, vertigo, lack of concentration, impulsiveness, and irritability [1], thus, affecting the family member’s ability as a caregiver to function normally while taking care of the patient. Hence, psychological distress and anxiety among family members of the patients should not be neglected or dealt with superficially.
As a standard operating procedure, when a patient is admitted for surgery, the surgeon and his team members would explain in detail the nature of the disease, treatment options, surgery to be conducted, and expected complications of the surgery to the patients and their family members. They would also be available during the postoperative period, to respond to the queries of patient and family members. However, during the intraoperative period there is minimal communication between the surgical team and the patient’s family [2]. Providing timely information about the status and progress of the ongoing surgery would help reduce anxiety among family members in the waiting room [3].
Intraoperative text messages are shown to reduce parental anxiety for children undergoing posterior spinal fusion surgery for adolescent idiopathic scoliosis [4]. However, there is a scarcity of literature on the role of such intraoperative interactions in reducing distress for family members of patients undergoing surgery for musculoskeletal malignancies. This study aims to contribute to the literature on this topic of study.
Materials and Methods
This is a randomized single-blinded prospective study. Family members of 60 patients (one family member for each patient) undergoing major orthopaedic oncology surgery (lasting for more than 1 h) were recruited and randomized into two groups (30 patients each). Personal phone numbers were recorded from members of both the groups and both the groups were blinded to the variables in this study. Group 1 (No SMS group) did not receive any text messages, while Group 2 (SMS group) received periodic intraoperative text messages. Respondents of less than 16 years of age, those with associated psychiatric or mental illnesses, and those who did not consent to this study were excluded.
Anxiety among family members was assessed using Visual Analogue Scale for Anxiety (VAS-A) and Anxiety component of Hospital Anxiety and Depression Scale (HADS-A) at five different periods; (P1) 1 day prior to surgery (P2) at separation of patient from the family at the operation theatre (P3) 1 h after commencement of surgery, (P4) immediately after completion of surgery, and (P5) 1 day after surgery. VAS-A measures subjective anxiety of respondents from a scale of 0 to 10 [0 = no anxiety/fear, 10 = maximum or worst possible anxiety/fear]. HADS-A consists of seven questions each with scores ranging from 0 to 3 [minimum possible score = 0, maximum possible score = 21] for each question. The higher the HADS-A scores, the higher the anxiety level of the respondents. VAS-A and HADS-A are proven to be valid and reliable tools to assess anxiety levels [5, 6]. Table 1 below shows the intraoperative text messages via SMS sent to family members from Group 1. In cases of metastatic disease where pathological fracture fixation surgery was performed, messages two and three were replaced with messages notifying that the fracture has been fixed.
Table 1.
Sequence of SMS’s sent to Group 1 family members
| Messages | Description |
|---|---|
| Message 1 | The surgery has started |
| Message 2 | The tumour has been completely resected |
| Message 3 (if any) | The reconstruction has been completed |
| Message 4 | We are closing the wound |
| Message 5 | Surgery has been completed, patient will be sent to the recovery zone |
The relevant demographic data (age, level of education, employment status, and any previous experience waiting for surgery) of respondents from both the groups, clinical data regarding tumour location and type of surgery performed, and the VAS-A and HADS-A scores from both groups during five different time periods were tabulated into the Microsoft Excel spreadsheet (Microsoft Excel 2010, Redmond, Washington). Statistical analysis was performed using SPSS software version 16 (Chicago, IL). Chi-square test, Fisher’s exact test, and independent sample t tests were used to analyze statistical variations between the groups. Conclusions were then drawn based on the significance of the results (p < 0.05 was considered statistically significant).
Results
The demographics of the patients and the relationships of the respondents to the patients and the VAS-A and HADS-A scores are presented in Table 2. The mean age for family members in Group 1 was 38 ± 4.8 years compared to 40 ± 4.6 years for Group 2 (p = 0.104). The relationship of the respondents to the patients is shown in Fig. 1 and the types of lesions operated on in both groups is shown in Fig. 2, it is similar in both groups. The types of surgery performed in both groups are similar and shown in Fig. 3. Other than that, no significant statistical difference was noted between two groups for other demographic parameters such as level of education, working status and previous experience of waiting for surgery. In addition to that, the location of tumour, type of surgery performed, and the duration of surgery was also not significantly different between both groups (Table 3).
Table 2.
Showing the demographic details of the patients and participants
| ID | Patient | Participant (family member) | Anxiety Score | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Age | Diagnosis | Surgery | Relationship with patient | Age | HADS | VAS | |||||||||
| P1 | P2 | P3 | P4 | P5 | P1 | P2 | P3 | P4 | P5 | |||||||
| Group 1: SMS | ||||||||||||||||
| 1 | F | 30 | Ewing sarcoma | Resection reconstruction | Husband | 30 | 12 | 13 | 17 | 10 | 10 | 7 | 7 | 9 | 5 | 4 |
| 2 | F | 50 | Pleomorphic sarcoma | Resection reconstruction | Son/daughter | 18 | 3 | 5 | 7 | 3 | 0 | 3 | 4 | 6 | 3 | 2 |
| 3 | F | 15 | Fibromatosis | Resection reconstruction | Mother | 45 | 15 | 14 | 8 | 4 | 3 | 8 | 8 | 5 | 2 | 2 |
| 4 | F | 40 | Pleomorphic sarcoma | Resection | Mother | 40 | 16 | 5 | 5 | 0 | 0 | 7 | 3 | 3 | 2 | 1 |
| 5 | F | 21 | Haemangioma | Resection | Father | 55 | 17 | 12 | 12 | 11 | 10 | 9 | 8 | 8 | 6 | 5 |
| 6 | M | 73 | Squamous cell carcinoma | Resection | Son/daughter | 29 | 5 | 10 | 11 | 7 | 7 | 6 | 8 | 8 | 7 | 7 |
| 7 | F | 47 | Pleomorphic sarcoma | Resection | Son/daughter | 24 | 15 | 15 | 17 | 10 | 10 | 7 | 7 | 8 | 5 | 4 |
| 8 | M | 29 | Chondrosarcoma | Resection | Mother | 43 | 17 | 18 | 17 | 13 | 10 | 8 | 8 | 9 | 5 | 5 |
| 9 | F | 48 | Epithelial sarcoma | Resection | Wife | 45 | 13 | 13 | 15 | 13 | 10 | 7 | 6 | 7 | 5 | 5 |
| 10 | M | 53 | Pathological fracture | Fracture fixation | Son/daughter | 27 | 15 | 13 | 12 | 11 | 9 | 8 | 7 | 6 | 5 | 4 |
| 11 | M | 11 | Osteosarcoma | Resection | Mother | 33 | 7 | 9 | 9 | 8 | 5 | 3 | 4 | 4 | 3 | 2 |
| 12 | P | 21 | Retroperitoneal neuroblastoma | Resection | Mother | 40 | 12 | 15 | 16 | 5 | 1 | 7 | 8 | 8 | 3 | 1 |
| 13 | P | 60 | Aseptic loosening | Fracture fixation | Son/daughter | 35 | 15 | 14 | 16 | 14 | 10 | 8 | 8 | 9 | 8 | 5 |
| 14 | M | 43 | Lipoma | Resection | Wife | 39 | 11 | 9 | 10 | 7 | 5 | 6 | 5 | 5 | 4 | 2 |
| 15 | F | 51 | GCT | Resection | Son/daughter | 31 | 8 | 8 | 7 | 7 | 7 | 4 | 4 | 3 | 3 | 3 |
| 16 | M | 51 | Pleomorphic sarcoma | Resection | Son/daughter | 32 | 8 | 7 | 6 | 6 | 7 | 4 | 5 | 4 | 3 | 3 |
| 17 | F | 32 | Rhabdomyosarcoma | Resection | Mother | 62 | 13 | 13 | 9 | 3 | 2 | 8 | 8 | 6 | 2 | 1 |
| 18 | F | 5 | Osteosarcoma | Resection reconstruction | Mother | 29 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 19 | F | 42 | Nodular PVNS | Resection | Husband | 45 | 9 | 13 | 9 | 8 | 4 | 5 | 7 | 5 | 4 | 3 |
| 20 | M | 51 | Schwannoma | Resection | Son/daughter | 31 | 2 | 5 | 3 | 3 | 2 | 1 | 3 | 2 | 2 | 1 |
| 21 | M | 53 | Pleomorphic sarcoma | Resection | Son/daughter | 28 | 10 | 5 | 8 | 2 | 2 | 6 | 4 | 5 | 2 | 1 |
| 22 | M | 65 | Lipoma | Resection | Son/daughter | 30 | 6 | 10 | 11 | 6 | 3 | 4 | 6 | 6 | 4 | 2 |
| 23 | F | 41 | GCT | Resection reconstruction | Sister | 45 | 4 | 6 | 5 | 6 | 4 | 2 | 4 | 4 | 4 | 2 |
| 24 | M | 44 | Pleomorphic sarcoma | Resection | Wife | 40 | 5 | 11 | 11 | 7 | 4 | 3 | 5 | 5 | 4 | 2 |
| 25 | M | 51 | Periprosthetic fracture | Resection reconstruction | Son/daughter | 33 | 11 | 10 | 7 | 8 | 6 | 6 | 5 | 4 | 4 | 3 |
| 26 | F | 31 | Neurofibromatosis (NF1) | Resection | Husband | 41 | 14 | 15 | 6 | 9 | 6 | 7 | 8 | 8 | 4 | 3 |
| 27 | M | 32 | Angiosarcoma | Resection | Father | 59 | 1 | 3 | 4 | 3 | 1 | 1 | 2 | 2 | 1 | 1 |
| 28 | M | 52 | Lipoma | Resection | Son/daughter | 31 | 11 | 13 | 13 | 12 | 8 | 5 | 7 | 7 | 7 | 4 |
| 29 | M | 30 | Neurofibromatosis (NF1) | Resection | Brother | 34 | 7 | 11 | 12 | 11 | 3 | 3 | 5 | 5 | 5 | 2 |
| 30 | M | 21 | Neurofibrosarcoma | Resection | Sister | 32 | 7 | 12 | 13 | 11 | 4 | 4 | 6 | 5 | 4 | 2 |
| Group 2: no SMS | ||||||||||||||||
| 31 | M | 13 | Osteosarcoma | Resection reconstruction | Mother | 46 | 1 | 6 | 10 | 11 | 6 | 2 | 4 | 5 | 7 | 5 |
| 32 | F | 64 | Pathological fracture | Fracture fixation | Son/daughter | 32 | 10 | 12 | 15 | 10 | 7 | 6 | 7 | 8 | 5 | 4 |
| 33 | F | 67 | Pleomorphic sarcoma | Resection | Others | 28 | 12 | 13 | 13 | 10 | 7 | 6 | 7 | 7 | 5 | 4 |
| 34 | F | 50 | Pathological fracture | Fracture fixation | Son/daughter | 30 | 10 | 14 | 17 | 11 | 10 | 6 | 8 | 9 | 5 | 4 |
| 35 | F | 26 | Schwannoma | Resection | Others | 27 | 6 | 8 | 9 | 5 | 5 | 6 | 7 | 5 | 5 | 3 |
| 36 | M | 45 | Pleomorphic sarcoma | Resection | Wife | 44 | 10 | 10 | 14 | 7 | 5 | 6 | 6 | 7 | 3 | 3 |
| 37 | F | 31 | Pleomorphic sarcoma | Resection reconstruction | Husband | 31 | 17 | 17 | 17 | 12 | 14 | 8 | 8 | 8 | 5 | 5 |
| 38 | F | 42 | Synovial sarcoma | Resection | Son/daughter | 22 | 15 | 17 | 17 | 10 | 6 | 8 | 8 | 8 | 5 | 3 |
| 39 | F | 19 | Ewing sarcoma | Resection | Mother | 40 | 14 | 14 | 16 | 10 | 6 | 7 | 7 | 8 | 5 | 3 |
| 40 | M | 50 | Residual soft tissue lesion | Resection | Son/daughter | 26 | 11 | 11 | 11 | 10 | 7 | 6 | 5 | 5 | 4 | 4 |
| 41 | F | 71 | Lipoma | Resection | Son/daughter | 30 | 10 | 11 | 11 | 10 | 8 | 6 | 8 | 8 | 6 | 6 |
| 42 | M | 69 | Pleomorphic sarcoma | Resection | Son/daughter | 38 | 15 | 15 | 15 | 10 | 10 | 8 | 8 | 8 | 5 | 7 |
| 43 | M | 70 | Pleomorphic sarcoma | Resection | Son/daughter | 40 | 14 | 15 | 17 | 8 | 10 | 8 | 8 | 8 | 6 | 6 |
| 44 | M | 56 | Pleomorphic sarcoma | Resection | Son/daughter | 28 | 13 | 13 | 16 | 10 | 7 | 7 | 7 | 8 | 5 | 4 |
| 45 | M | 30 | Synovial sarcoma | Resection | Sister | 28 | 11 | 11 | 15 | 8 | 7 | 6 | 6 | 8 | 6 | 4 |
| 51 | F | 17 | Osteosarcoma | Resection reconstruction | Mother | 51 | 13 | 15 | 20 | 15 | 13 | 7 | 8 | 10 | 8 | 7 |
| 47 | F | 9 | Haemangioma | Resection | Mother | 32 | 10 | 15 | 10 | 15 | 8 | 6 | 8 | 6 | 8 | 6 |
| 48 | F | 22 | Osteochondroma | Resection reconstruction | Mother | 55 | 6 | 6 | 6 | 5 | 5 | 3 | 3 | 4 | 3 | 3 |
| 49 | M | 13 | Ewing sarcoma | Resection reconstruction | Mother | 52 | 6 | 7 | 6 | 5 | 3 | 3 | 4 | 3 | 3 | 1 |
| 50 | M | 53 | Aseptic loosening | Fracture fixation | Wife | 48 | 16 | 19 | 21 | 11 | 6 | 8 | 9 | 10 | 5 | 4 |
| 51 | M | 18 | Ewing sarcoma | Resection | Mother | 41 | 17 | 21 | 21 | 4 | 3 | 8 | 10 | 10 | 3 | 2 |
| 52 | F | 82 | Pathological fracture | Fracture fixation | Son/daughter | 62 | 6 | 7 | 9 | 8 | 4 | 3 | 4 | 5 | 9 | 2 |
| 53 | M | 14 | Chondroblastoma | Resection | Brother | 18 | 5 | 8 | 12 | 3 | 3 | 3 | 4 | 6 | 2 | 1 |
| 54 | M | 60 | Pleomorphic sarcoma | Resection reconstruction | Son/daughter | 29 | 12 | 15 | 13 | 8 | 6 | 6 | 8 | 6 | 4 | 3 |
| 55 | F | 33 | Synovial sarcoma | Resection | Husband | 30 | 9 | 13 | 15 | 14 | 9 | 4 | 7 | 8 | 7 | 3 |
| 56 | F | 25 | Malignant melanoma | Resection | Sister | 20 | 4 | 7 | 10 | 6 | 4 | 2 | 4 | 5 | 4 | 2 |
| 57 | M | 52 | Pathological fracture | Fracture fixation | Wife | 46 | 3 | 5 | 5 | 4 | 3 | 1 | 3 | 3 | 2 | 1 |
| 58 | F | 62 | Neurofibrosarcoma | Resection | Others | 61 | 1 | 3 | 6 | 3 | 1 | 1 | 2 | 3 | 2 | 1 |
| 59 | M | 56 | Pleomorphic sarcoma | Resection | Son/daughter | 25 | 5 | 16 | 16 | 11 | 3 | 3 | 9 | 9 | 7 | 2 |
| 60 | F | 7 | Spindle cell cancer | Resection | Father | 27 | 3 | 16 | 16 | 11 | 5 | 2 | 8 | 8 | 6 | 4 |
Fig. 1.
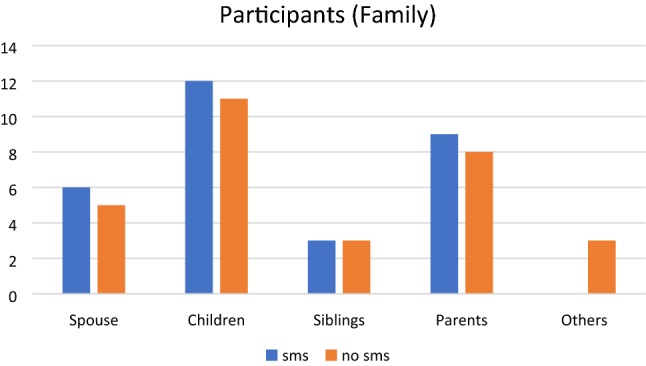
Shows the relationship of the respondents to the patient
Fig. 2.
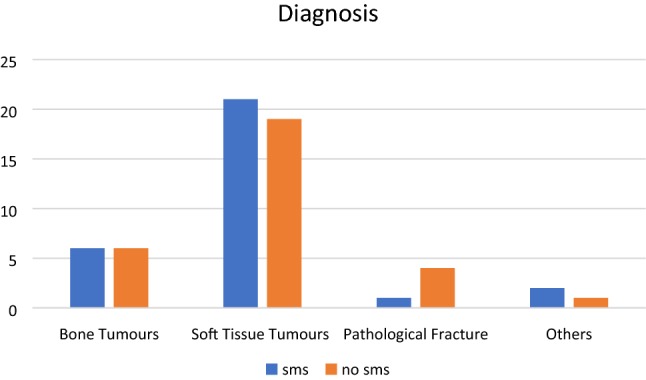
Shows the types of tumours in both groups
Fig. 3.
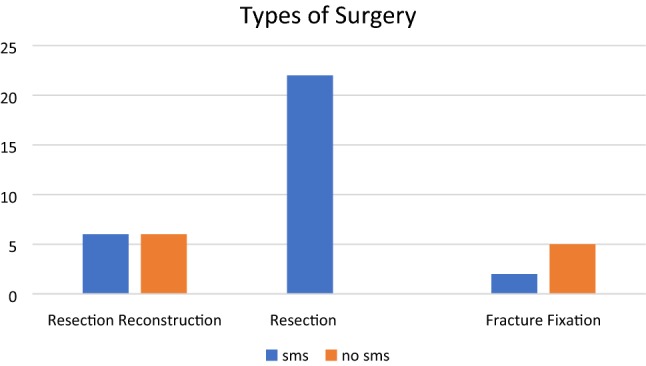
Types of surgery in both groups of patients
Table 3.
Demographic characteristics of respondent family members, location of tumour, type and duration of surgery performed for the two Groups
| Group 1 (no SMS) n = 30 |
Group 2 (SMS) n = 30 |
p | |
|---|---|---|---|
| Mean age (years) | 38 ± 4.8 | 40 ± 4.6 | 0.104 |
| Education | |||
| Level 1 (less than high school) | 2 | 1 | 0.547 |
| Level 2 (high school) | 12 | 11 | |
| Level 3 (graduation) | 13 | 17 | |
| Level 4 (post-graduation) | 3 | 1 | |
| Working status | |||
| Full time | 14 | 19 | 0.154 |
| Part time | 0 | 1 | |
| Not working | 16 | 10 | |
| Previous experience waiting for surgery | |||
| Yes | 13 | 19 | 0.124 |
| No | 17 | 11 | |
| Location of tumor | |||
| Upper extremity | 9 | 7 | 0.135 |
| Lower extremity | 20 | 17 | |
| Pelvis/axial skeleton | 1 | 6 | |
| Type of surgery | |||
| Resection only | 17 | 21 | 0.461 |
| Resection + reconstruction | 7 | 4 | |
| Fracture fixation | 6 | 5 | |
| Mean duration for surgery (minutes) | 142 ± 36.89 | 132.83 ± 38.67 | 0.351 |
The mean VAS-A and HADS-A scores between both groups did not show statistically significant difference during the preoperative period (P1), separation in operation theatre (P2), and postoperative period (P5). However, mean VAS-A and HADS-A scores were significantly lower for Group 2 (SMS Group) compared to Group 1 (No SMS Group) at 1 h after commencement of surgery (P3) and at the completion of surgery (P4) [Table 4]. Interestingly, Group 1 respondents had the highest mean VAS-A and HADS-A scores at 1 h after commencement of surgery (P3), while respondents of Group 2 had the highest mean VAS-A and HADS-A scores during separation at operation theatre (P2) (Figs. 4, 5).
Table 4.
Mean VAS-A and HADS-A scores of respondent family members between the two groups
| Period | Mean scores | Group 1 (no SMS) | Group 2 (SMS) | p |
|---|---|---|---|---|
| P1 | VAS-A | 5.26 ± 2.38 | 5.2 ± 2.31 | 0.11 |
| HADS-A | 9.5 ± 4.7 | 9.7 ± 4.8 | 0.87 | |
| P2 | VAS-A | 6.5 ± 3.1 | 5.6 ± 2.0 | 0.12 |
| HADS-A | 12 ± 4.4 | 10.4 ± 4.1 | 0.15 | |
| P3 | VAS-A | 6.8 ± 2.0 | 5.5 ± 2.3 | 0.022 |
| HADS-A | 13.3 ± 4.4 | 10.3 ± 4.4 | 0.011 | |
| P4 | VAS-A | 5.0 ± 1.8 | 3.9 ± 1.7 | 0.023 |
| HADS-A | 10.9 ± 2.8 | 7.3 ± 3.8 | 0.0001 | |
| P5 | VAS-A | 3.56 ± 1.7 | 2.8 ± 1.5 | 0.07 |
| HADS-A | 6.3 ± 2.9 | 5.16 ± 3.3 | 0.11 |
Fig. 4.
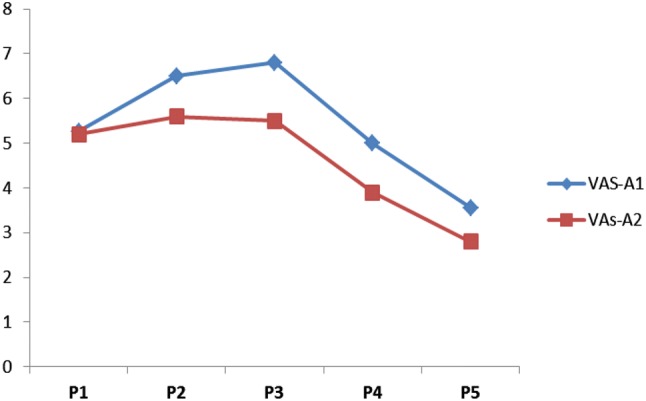
Mean VAS-A scores (y-axis) for both groups during different periods (x-axis)
Fig. 5.
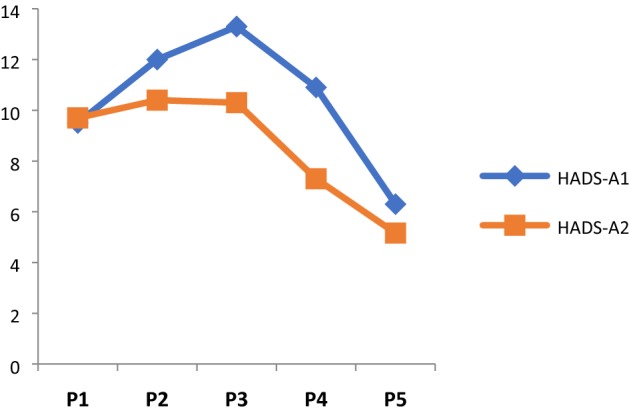
Mean HADS-A scores (y-axis) for both groups during different periods (x-axis)
For eight patients from Group 1 and six patients from Group 2, the surgery was postponed for 1 week. The anxiety assessment among family members was performed from the perioperative period up to the definitive surgery.
Discussion
Over the lengthy course of treatment, cancer patients are usually dependent on their family members for assistance with activities of daily living, regular hospital visits for treatment, for adherence to medication schedules and psychological as well as financial support. Family members of the patients tend to be drained physically, emotionally, and financially, while taking care of their loved ones. Thus, psychological distress such as anxiety and depression tend to be highly prevalent among these family members [7–9]. Patients’ recovery process might be jeopardized if the caregiving family members themselves are unable to function normally. Therefore, pacifying the mental and psychological distress of family members of cancer patients should also be emphasized for a smoother treatment and recovery.
Surgery for musculoskeletal malignancies is usually complex which explains why the family members would be highly anxious during perioperative period. Providing detailed and accurate updates during the perioperative period might help to reduce some of the fears and anxiety faced by them. The waiting period during surgery is the most stressful hospital experience for the family members [10–12]. Family members waiting during surgery would experience an increase in heart rate, increase in blood pressure [11], and emotional disturbances such as restlessness, inability to concentrate, panic reactions, and loss of control [10]. Leske et al. [11] noticed that family members who received informational progress reports during waiting hours felt more assured and experienced lesser fear or anxiety. Besides that, heart rate and mean arterial pressure were also significantly lower for them compared to family members who did not receive any progress report. Kwan et al. [4] reported that intraoperative text messages were an effective intervention to reduce parental anxiety for children undergoing posterior spinal fusion surgery for adolescent idiopathic scoliosis. However, Topp et al. [13] reported that the group which received paging devices during waiting period experienced a greater state of anxiety and greater percentage of time spent outside surgical waiting rooms compared to the group which did not receive paging devices. In another study by Trecartin et al. [14], informational report to family members did not reduce anxiety among the waiting family members. The results from these two researchers contradict with the findings of others. Watching a movie or listening to music has also been shown to reduce stress and anxiety among family members during waiting hours for surgery [15, 16].
Surgical procedures in orthopaedic oncology vary according to the nature of disease, complexity, extensiveness of the tumour, and expected complications and outcomes from the surgery. Therefore, intraoperative anxiety among family members waiting for different surgeries may vary significantly. In this study, we focused on the assessment of anxiety among family members of patients undergoing surgery for musculoskeletal malignancies.
Various methods have been used to deliver intraoperative information to the waiting family members. Kathol et al. [2] used in person progress report given 30 min after commencement of surgery and post-surgery. Meanwhile, Leske et al. [11] used single 5–10 min in person progress report halfway through the surgery. In another study, Leske et al. [17] compared the effectiveness of progress report via telephone compared to in person progress report and found the latter to be more effective. As noted earlier, Topp et al. [13] used paging devices for delivering progress report. In this study, we used text messages via SMS similar to Kwan et al. [4].
Our results showed that anxiety significantly was less during the P3 and P4 assessment periods in the group that received the SMS notifications, which reflected the psychological status of family members during intraoperative period. Demographic parameters, location of tumour, and type and duration of surgery did not show any statistically significant difference for both groups.
Conclusion
Text messages via SMS are one of the simplest and most convenient method of delivering information regarding the status of ongoing surgery to the accompanying family members which effectively reduces their anxiety levels during the perioperative period. This can be performed by a junior member of the surgical team who is not scrubbed up in the particular surgery.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rishi Ram Poudel, Email: rishipoudel2004@gmail.com.
Vivek Ajit Singh, Email: drvivek69@gmail.com.
Nor Faissal Yasin, Email: drfaissal76@gmail.com.
References
- 1.Thompson N, Irwin MG, Gunawardene WM, et al. Pre-operative parental anxiety. Anaesthesia. 1996;51(11):1008–1112. doi: 10.1111/j.1365-2044.1996.tb14992.x. [DOI] [PubMed] [Google Scholar]
- 2.Kathol DK. Anxiety in surgical patients’ families. AORN Journal. 1984;40(1):131–137. doi: 10.1016/S0001-2092(07)69436-8. [DOI] [PubMed] [Google Scholar]
- 3.O’Connell M. Anxiety reduction in family members of patients in surgery and postanesthesia care: A pilot study. Journal of Post Anaesthesia Nursing. 1989;4(1):7–16. [PubMed] [Google Scholar]
- 4.Kwan MK, Chiu CK, Gan CC, et al. Can intraoperative text messages reduce parental anxiety of children undergoing posterior spinal fusion surgery for adolescent idiopathic scoliosis? Spine. 2016;41(4):225–230. doi: 10.1097/BRS.0000000000001199. [DOI] [PubMed] [Google Scholar]
- 5.Facco E, Stellini E, Bacci C, et al. Validation of visual analogue scale for anxiety (VAS-A) in preanesthesia evaluation. Minerva Anestesiologica. 2013;79(12):1389–1395. [PubMed] [Google Scholar]
- 6.Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. Journal of Psychosomatic Research. 2002;52(2):69–77. doi: 10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 7.Pitceathly C, Maguire P. The psychological impact of cancer on patients’ partners and other key relatives: A review. European Journal of Cancer. 2003;39(11):1517–1524. doi: 10.1016/S0959-8049(03)00309-5. [DOI] [PubMed] [Google Scholar]
- 8.Friðriksdóttir N, Saevarsdóttir T, Halfdánardóttir SÍ, et al. Family members of cancer patients: needs, quality of life and symptoms of anxiety and depression. Acta Oncologica. 2011;50(2):252–258. doi: 10.3109/0284186X.2010.529821. [DOI] [PubMed] [Google Scholar]
- 9.Katende G, Nakimera L. Prevalence and correlates of anxiety and depression among family carers of cancer patients in a cancer care and treatment facility in Uganda: A cross-sectional study. African Health Sciences. 2017;17(3):868–876. doi: 10.4314/ahs.v17i3.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trimm DR, Sanford JT. The process of family waiting during surgery. Journal of Family Nursing. 2010;16(4):435–461. doi: 10.1177/1074840710385691. [DOI] [PubMed] [Google Scholar]
- 11.Leske JS. Effects of intraoperative progress reports on anxiety levels of surgical patients’ family members. Applied Nursing Research. 1995;8(4):169–173. doi: 10.1016/S0897-1897(95)80381-5. [DOI] [PubMed] [Google Scholar]
- 12.Sadeghi T, Dehghan Nayeri N, Abbaszadeh A. Factors influencing intraoperative waiting time according to the experience of Iranian families. Journal of PeriAnesthesia Nursing. 2016;31(3):217–225. doi: 10.1016/j.jopan.2014.08.146. [DOI] [PubMed] [Google Scholar]
- 13.Topp R, Walsh E, Sanford C. Can providing paging devices relieve waiting room anxiety? AORN Journal. 1998;67(4):852–854. doi: 10.1016/S0001-2092(06)62648-3. [DOI] [PubMed] [Google Scholar]
- 14.Trecartin K, Carroll DL. Nursing interventions for family members waiting during cardiac procedures. Clinical Nursing Research. 2011;20(3):263–275. doi: 10.1177/1054773811405520. [DOI] [PubMed] [Google Scholar]
- 15.Mojdeh S, Zamani M, Kooshki AM, et al. Effect of watching a movie on family members’ anxiety level during their relatives’ surgery. Iranian Journal of Nursing and Midwifery Research. 2013;18(4):329–332. [PMC free article] [PubMed] [Google Scholar]
- 16.Routhieaux RL, Tansik DA. The benefits of music in hospital waiting rooms. The Health Care Supervisor. 1997;16(2):31–40. [PubMed] [Google Scholar]
- 17.Leske JS. Intraoperative progress reports decrease family members’ anxiety. AORN Journal. 1996;64(3):424–425. doi: 10.1016/S0001-2092(06)63055-X. [DOI] [PubMed] [Google Scholar]


