Abstract
BACKGROUND
The albumin-bilirubin (ALBI) score was validated as a prognostic indicator in patients with liver disease and hepatocellular carcinoma. Incorporating platelet count in the platelet-albumin-bilirubin (PALBI) score improved validity in predicting outcome of patients undergoing resection and ablation.
AIM
To evaluate the PALBI score in predicting outcome of acute variceal bleeding in patients with cirrhosis.
METHODS
The data of 1517 patients with cirrhosis presenting with variceal bleeding were analyzed. Child Turcotte Pugh (CTP) class, Model of End-stage Liver Disease (MELD), ALBI and PALBI scores were calculated on admission, and were correlated to the outcome of variceal bleeding. Areas under the receiving-operator characteristic curve (AUROC) were calculated for survival and rebleeding.
RESULTS
Mean age was 52.6 years; 1176 were male (77.5%), 69 CTP-A (4.5%), 434 CTP-B (29.2%), 1014 CTP-C (66.8%); 306 PALBI-1 (20.2%), 285 PALBI-2 (18.8%), and 926 PALBI-3 (61.1%). Three hundred and thirty-two patients died during hospitalization (21.9%). Bleeding-related mortality occurred in 11% of CTP-B, 28% of CTP-C, in 21.8% of PALBI-2 and 34.4% of PALBI-3 patients. The AUROC for predicting survival of acute variceal bleeding was 0.668, 0.689, 0.803 and 0.871 for CTP, MELD, ALBI and PALBI scores, respectively. For predicting rebleeding the AUROC was 0.681, 0.74, 0.766 and 0.794 for CTP, MELD, ALBI and PALBI scores, respectively.
CONCLUSION
PALBI score on admission is a good prognostic indicator for patients with acute variceal bleeding and predicts early mortality and rebleeding.
Keywords: Variceal bleeding, Platelet-albumin-bilirubin score, Albumin-bilirubin score, Rebleeding
Core tip: This study describes a comparative analysis of the performance of different scoring systems in a large number of patients with acute variceal bleeding. The platelet-albumin-bilirubin score performed better in predicting short-term outcome and the incidence of rebleeding compared with the other 4 scoring systems, the Child Pugh score, albumin-bilirubin score and Model of End-stage Liver Disease and its modification for acute variceal bleeding.
INTRODUCTION
Acute variceal bleeding is a frequent, ominous complication of liver cirrhosis and portal hypertension and is responsible for high morbidity and mortality[1].
The Child-Turcotte-Pugh (CTP) and Model of End-stage Liver Disease (MELD) scores are two of the most important models for predicting the survival of upper gastrointestinal bleeding. The CTP score was originally developed to be a prognostic score in patients with cirrhosis and portal hypertension undergoing surgery for variceal bleeding[2]. The limitations of the CTP score in assessing liver functions in patients with upper gastro-intestinal tract (GIT) bleeding are the subjective assessment of encephalopathy and amount of ascites, together with the interrelated variables such as ascites and serum albumin, besides the parameters that are scored based on arbitrarily defined cutoff points[3,4].
The MELD score was initially developed to determine prognosis following a trans jugular intra-hepatic porto-systemic shunt procedure, and is widely used in liver transplant settings to prioritize donor liver allocation[5,6]. Johnson et al[7] developed the albumin-bilirubin (ALBI) score, which depends on two laboratory variables; bilirubin and albumin, omits the subjective CTP variables ascites and hepatic encephalopathy, and results are expressed as three grades with three different cutoff points[7]. Roayaie et al[8] proposed modifying the ALBI score by including the platelet count as an indicator of portal hypertension.
In this study, we aimed to determine the value of the platelet-albumin-bilirubin (PALBI) score in predicting the outcome of patients with cirrhosis presenting with acute variceal bleeding.
MATERIALS AND METHODS
This retrospective study included 1517 patients with cirrhosis presenting with acute variceal bleeding who were admitted to the National Liver Institute Hospital. The study was approved by the institutional review board (IRB number IRB00003413).
Inclusion criteria
This study included patients with acute variceal bleeding. Acute upper gastrointestinal bleeding was considered in patients with liver cirrhosis presenting with hematemesis, defined as either one or more than one episode of vomiting either fresh blood or a coffee ground-like material, or reported or observed melena, with a drop in hemoglobin, and blood in the nasogastric tube.
All patients were managed in the emergency unit and subjected to the following: (1) Resuscitation to maintain hemodynamic stability (systolic blood pressure above 80-90 mmHg); (2) Blood transfusion using type and cross-matched packed red cells and plasma as required to increase hematocrit to 25%-30% or hemoglobin to above 9 g/dL; (3) Vaso-active drugs as required and according to requirement (octreotide or terlipressin); and (4) Antibiotic prophylaxis was given in the form of I.V. cefotaxime 1 g/12 h for up to 5 d, unless acute infection, especially spontaneous bacterial peritonitis, was diagnosed, which was treated accordingly.
Urgent endoscopy was performed within the first six hours. The diagnosis of variceal hemorrhage was considered when active bleeding from an esophageal or gastric varix was observed or when a sign of recent bleeding, such as a “white nipple”, was observed. Variceal hemorrhage was inferred when varices were the only pathology found, with blood present in the stomach. Patients with other causes of acute upper gastrointestinal bleeding were not considered for this analysis.
Esophageal varices were managed by band ligation or injection sclerotherapy if banding was not feasible. Bleeding from gastric varices was managed by injection of tissue adhesive (histoacryl) injection.
Variceal bleeding was considered to have been controlled if the following criteria were met: Stable blood pressure (no reduction in systolic pressure exceeding 20 mmHg, once the blood pressure had stabilized); a stable hemoglobin concentration (> 9 g/dL), measured twice daily; and a hematocrit above 30% (measured hourly during the first 12 h and every 2 to 6 h thereafter, depending on the patient’s hemodynamic status), with a transfusion requirement of no more than two units in a 2-h period and fewer than four units within the first 4 h after endoscopic therapy.
Patients were followed for 5 d after the control of acute bleeding for occurrence of rebleeding. Rebleeding was defined as the occurrence of new hematemesis or melena after a period of 24 h or more from the 24-h point of stable vital signs and hematocrit/hemoglobin following an episode of acute bleeding[9]. In patients with significant rebleeding, defined as frank hematemesis, new onset of melena, fresh blood in nasogastric tube aspirate, or hemodynamic compromise, with a decrease in hemoglobin level of > 2 g/dL, re-endoscopy was performed.
The CTP class, MELD, ALBI, MELD-Acute variceal bleeding (MELD-AVB) and PALBI scores were calculated from admission labs, and were correlated with control of bleeding, rebleeding, and in-hospital mortality. (1) The CTP score was calculated numerically as previously described including bilirubin, albumin, international normalized ratio (INR), and presence and grade of ascites and encephalopathy. CTP class was A if the score was 5-6, B if the score was 7-9, and C if the score was 10 or higher[2]; (2) The MELD score was calculated as: 0.957 × loge (creatinine mg/dL) + 0.378 × log (bilirubin mg/dL) + 1.1 20 × loge (INR) + 0.643[5]; (3) The ALBI score was calculated as: = (log10 bilirubin × 0.66) + (albumin × -0.085) where bilirubin is in μmol/L and albumin in g/L. ALBI was categorized into three grades: ALBI-1 (≤ −2.60), ALBI-2 (> 2.60 to −1.39), ALBI-3 (> −1.39)[6]; (4) MELD-AVB was adapted from the basic MELD score through this equation logit, -5.312 + 0.207 * MELD; bootstrapped R2, 0.3295; and (5) PALBI score was calculated as: (2.02 × Log10 bilirubin) + [-0.37 × (Log10 bilirubin)2] + (-0.04 × albumin) + (-3.48 × Log10 platelets) + [1.01 (Log10 platelets)2] where bilirubin is in μmol/L and albumin in g/L, and platelet count in 1000/μL. PALBI was categorized as: PALBI 1 (score ≤ 2.53), PALBI 2 (score > 2.53 and ≤ 2.09), and PALBI 3 (score > 2.09)[7].
The areas under the receiving-operator characteristic curve (AUROC) were calculated for survival and rebleeding.
Statistical analysis
Data were collected and entered into the computer using SPSS program version 23 for statistical analysis (IBM Corp., Armonk, NY, United States). Continuous data were expressed as the mean ± SD and the median with minimum and maximum. Categorical data were expressed as the frequency (percentage). A comparison between the chosen variables and control of bleeding, rebleeding, and mortality was performed. Univariate analysis included the Fisher's exact test or Chi-square test for categorical variables and the analysis of variance for continuous variables. Multivariate logistic regression using the stepwise selection method was performed starting from the variables with P < 0.01 in the univariate analysis. ROC curve analyses were performed to determine the value of CTP class, MELD, ALBI, MELD-AVB and PALBI scores in predicting the in-hospital mortality and the control of bleeding. AUROCs with 95% confidence intervals were calculated and compared. Also, the AUROCs were tested for significance using DeLong test. The sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, positive predictive value, and negative predictive value with 95% confidence intervals were reported at the best cutoff value. P < 0.05 was considered statistically significant.
RESULTS
This analysis contains the data of 1517 patients who presented with acute variceal bleeding. There were 1176 males (77.5%), and mean patient age was 52.6 ± 10.3 years.
Three hundred and thirty-two (21.9%) patients died during hospitalization, and 364 (23.9%) developed hepatic encephalopathy during admission.
All patients received resuscitation, blood as needed, antibiotics, and vasoactive drugs. Endoscopy was performed as soon as feasible, and the mean time between admission and endoscopy was 5.6 ± 1.9 h (median 4 h) (Table 1). The mean number of blood units transfused was 2.8 ± 1.1 units, and the mean duration of hospitalization was 5 d. The baseline characteristics of the patients on admission are shown in Table 1.
Table 1.
Characteristics of all studied participants
| Variable | Number/mean (%) | Median | SD |
| Age (yr) | 52.6 | 52 | 10.3 |
| Male:Female | 1176 (77.5):341 (22.5) | - | - |
| In-hospital mortality | 332 (21.9) | - | - |
| Serum albumin (g/dL) | 2.4 | 2.4 | 0.6 |
| Serum total bilirubin (μmol/L) | 64.98 | 30.78 | 99.18 |
| Serum creatinine (mg/dL) | 1.3 | 1 | 0.97 |
| International normalized ratio (INR) | 1.7 | 1.6 | 0.53 |
| Hemoglobin level (g/dL) | 9.5 | 9.4 | 2.35 |
| Hematocrit | 28.8 | 29 | 6.25 |
| Platelet count (× 103/mm3) | 116 | 104 | 56 |
| Blood units transfused | 2.8 | 2 | 1.1 |
| Time to first endoscopy (h) | 5.6 | 4 | 1.9 |
| Duration of admission (d) | 5 | 4 | 3.3 |
| MELD score | 15.2 | 14.8 | 3.2 |
SD: Standard deviation; MELD: Model of End-stage Liver Disease.
Endoscopy revealed that 1283 patients (84.57%) had esophageal varices as the source of bleeding. Seven hundred and eighty-five patients (51.74%) had band ligation alone; 301 patients (19.84%) had sclerotherapy as a single treatment modality, while 197 (12.9%) had combined treatment modalities. Gastric varices were present in 366 patients, and were the only source of bleeding in 165. Histoacryl injection was conducted in 271 patients, in 165 as the only therapeutic intervention and with band ligation of esophageal varices in 106. Sixty-nine patients (4.54%) received conservative medical treatment (Table 2).
Table 2.
Treatment modalities
| Treatment modality | n (%) |
| Band ligation | 785 (51.8) |
| Sclerotherapy | 301 (19.9) |
| Fundal varix (histoacryl injection alone) | 165 (10.8) |
| Combined treatment | 197 (13) |
| Conservative treatment | 69 (4.5) |
Sixty-nine patients were CTP class A (4.5%), 434 were CTP class B (29.2 %) and 1014 were CTP class C (66.8%). 692 (46%) had ascites and 364 (24%) presented with hepatic encephalopathy. Twenty-six patients were ALBI grade 1 (1.6%); 669 were ALBI grade 2 (44.1%), and 822 were ALBI grade 3 (54.1%). Using the PALBI score to classify patients, 306 patients were PALBI grade 1 (20.2%), 285 patients were PALBI grade 2 (18.8%), and 926 patients were PALBI grade 3 (61%). Table 3 shows the patient classification using the different scores.
Table 3.
Patients distribution according to Child Turcotte Pugh, Albumin-bilirubin, Model of End-stage Liver Disease and Platelet-albumin-bilirubin scores
| Class | No. of patients (%) | Bleeding mortality (%) |
| CTP A | 69 (4.5) | 0 |
| CTP B | 434 (29.2) | 11 |
| CTP C | 1014 (66.8) | 28 |
| MELD < 12 | 186 (12) | 0 |
| MELD 12-20 | 353 (23.5) | 16.3 |
| MELD > 20 | 978 (64.5) | 31.9 |
| ALBI grade 1 | 26 (1.7) | 0 |
| ALBI grade 2 | 669 (44.1) | 7.2 |
| ALBI grade 3 | 822(54.1) | 34.5 |
| MELD-AVB < 11 | 159 (10.5) | 0 |
| MELD-AVB 11-19 | 370 (24.4) | 14.3 |
| MELD-AVB > 19 | 988 (65.1) | 36.3 |
| PALBI grade 1 | 306 (20.2) | 0 |
| PALBI grade 2 | 285(18.8) | 21.8 |
| PALBI grade 3 | 926 (61) | 34.4 |
PALBI: Platelet-albumin-bilirubin score; ALBI: Albumin-bilirubin; MELD: Model of End-stage Liver Disease; CTP: Child Turcotte Pugh; MELD-AVB: MELD-acute variceal bleeding.
The incidence of early rebleeding (within 1 wk) was 3.12% and the incidence of recurrent bleeding (after 1 wk) was 8.9%. The predictors of rebleeding are shown in Table 4.
Table 4.
Predictors of rebleeding
| Parameter | OR | 95%CI | P value |
| PALBI | 3.987 | 1.994-7.775 | < 0.001 |
| Conservative therapy | 2.473 | 1.237-4.822 | < 0.001 |
| Previous beta blockers | 0.387 | 0.194-0.755 | < 0.001 |
| ALBI | 3.214 | 1.607-6.267 | < 0.01 |
| Time to endoscopy | 1.572 | 1.086-3.065 | < 0.01 |
| Ascites | 2.319 | 1.160-4.522 | < 0.05 |
| Spleen size | 1.961 | 1.181-3.824 | < 0.05 |
| Diabetes | 1.631 | 1.116-3.180 | < 0.05 |
| Platelet count | 0.445 | 0.223-0.868 | < 0.05 |
| INR | 1.618 | 1.109-3.155 | < 0.05 |
| Bilirubin | 1.981 | 1.291-3.863 | < 0.05 |
| Albumin | 0.613 | 0.457-0.897 | < 0.05 |
ALBI: Albumin-bilirubin; PALBI: Platelet-albumin-bilirubin score; INR: International normalized ratio.
In-hospital mortality among CTP classes A, B and C were 0%, 11% and 28%, among ALBI grades 1, 2 and 3 were 0%, 7.2% and 34.5%, and among PALBI grade 1, 2, and 3 were 0%, 21.8% and 34.4%, respectively (Table 3).
Table 5 shows the predictors of mortality, where PALBI grade showed the highest odds ratio.
Table 5.
Multivariate analysis: Predictors of in-hospital mortality
| Parameter | OR | 95%CI | P value |
| PALBI | 4.187 | 2.093-8.164 | < 0.001 |
| MELD-AVB | 3.842 | 2.983-7.431 | < 0.01 |
| ALBI | 3.153 | 1.576-6.148 | < 0.001 |
| MELD | 2.981 | 1.490-5.812 | < 0.001 |
| CTP | 2.144 | 1.072-4.180 | < 0.01 |
| Bilirubin | 1.981 | 1.015-3.862 | < 0.01 |
| Albumin | 0.269 | 0.134-0.524 | < 0.01 |
| Age | 1.718 | 1.034-3.350 | < 0.05 |
| Ascites | 1.547 | 1.173-3.016 | < 0.05 |
| Encephalopathy | 1.869 | 1.124-3.644 | < 0.05 |
| Hematocrit | 0.191 | 0.095-0.372 | < 0.05 |
| Platelet count | 0.543 | 0.321-0.853 | < 0.05 |
| INR | 1.923 | 1.061-3.749 | < 0.05 |
| Creatinine | 1.561 | 1.180-3.043 | < 0.05 |
PALBI: Platelet-albumin-bilirubin score; ALBI: Albumin-bilirubin; MELD: Model of End-stage Liver Disease; CTP: Child Turcotte Pugh; MELD-AVB: MELD-acute variceal bleeding; INR: International normalized ratio.
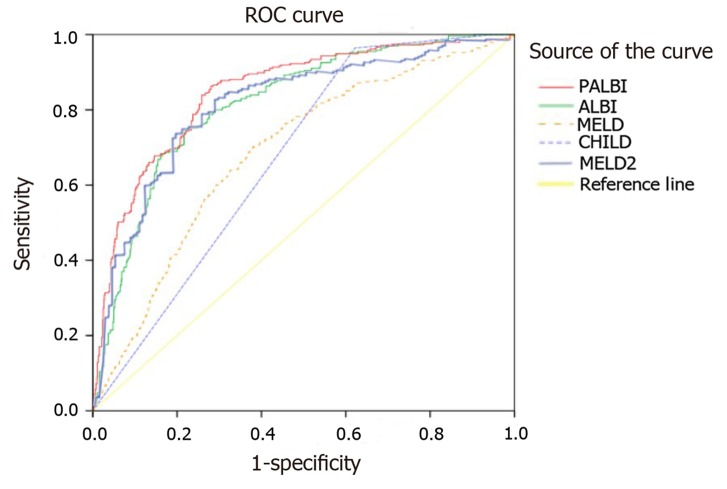
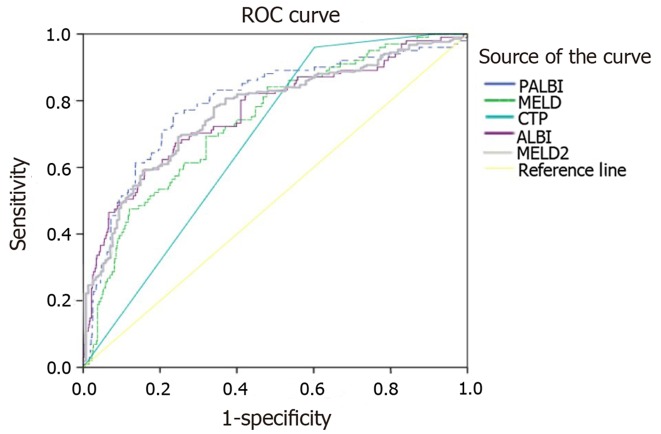
The AUROC for predicting survival following acute variceal bleeding was 0.668, 0.689, 0.803, 0.849 and 0.871 for CTP, MELD, ALBI, MELD-AVB and PALBI scores, respectively (Figure 1). PALBI score showed a significantly higher performance than MELD, ALBI and CTP (Table 6). For predicting rebleeding, the AUROC was 0.681, 0.74, 0.766, 0.769 and 0.794 for CTP, MELD, ALBI, MELD-AVB and PALBI scores, respectively (Figure 2). The performance of PALBI was significantly higher than that of MELD-AVB, MELD, ALBI and CTP (Table 6).
Figure 1.
The AUROCs of the platelet-albumin-bilirubin score, albumin-bilirubin, Model of End-stage Liver Disease, Child Turcotte Pugh and Model of End-stage Liver Disease-acute variceal bleeding scores for predicting outcome of acute variceal bleeding. PALBI: Platelet-albumin-bilirubin score; ALBI: Albumin-bilirubin; MELD: Model of End-stage Liver Disease; CTP: Child Turcotte Pugh; MELD-AVB: MELD-acute variceal bleeding.
Table 6.
Area under the receiver operating characteristic curve values of different scores to predict the outcome of acute variceal bleeding and the incidence of rebleeding
| Predicting outcome of acute variceal bleeding | |||||
| Score | CTP | MELD | ALBI | MELD-AVB | PALBI |
| AUROC | 0.668 | 0.689 | 0.803 | 0.849 | 0.871 |
| P value1 | < 0.01 | < 0.01 | < 0.01 | 0.043 | - |
| Predicting rebleeding | |||||
| Score | CTP | MELD | ALBI | MELD-AVB | PALBI |
| AUROC | 0.681 | 0.74 | 0.766 | 0.769 | 0.794 |
| P value1 | < 0.01 | < 0.05 | 0.052 | 0.032 | - |
P values are tested with Delong test between each consecutive test. PALBI: Platelet-albumin-bilirubin score; ALBI: Albumin-bilirubin; MELD: Model of End-stage Liver Disease; CTP: Child Turcotte Pugh; MELD-AVB: MELD-acute variceal bleeding; INR: International normalized ratio.
Figure 2.
The AUROCs of the platelet-albumin-bilirubin score, albumin-bilirubin, Model of End-stage Liver Disease, Child Turcotte Pugh and Model of End-stage Liver Disease-acute variceal bleeding scores for predicting rebleeding. PALBI: Platelet-albumin-bilirubin score; ALBI: Albumin-bilirubin; MELD: Model of End-stage Liver Disease; CTP: Child Turcotte Pugh; MELD-AVB: MELD-acute variceal bleeding.
DISCUSSION
The present study found a mortality rate of 21.9% due to variceal bleeding. Randomized, controlled trials have shown that mortality due to variceal bleeding in cirrhosis has decreased over the past 3 decades from about 50% to 20%-30%, but this figure is still remarkably high. Hence, stratifying the risk for mortality is paramount[10]. The best method to stratify risk is not clear. In this study we report the important predictive value of the PALBI score.
The PALBI score, proposed by Roayaie et al[8] was initially used for the assessment of patients with HCC undergoing resection or ablation. It was later validated in several studies in predicting the outcome of interventions for the management of HCC[11,12]. This report, however, evaluates the predictive power of the PALBI score in a large cohort of patients with cirrhosis presenting with acute variceal bleeding, in comparison to ALBI, MELD and CTP scores. In the overall analysis, PALBI score performed significantly better than ALBI, MELD score and CTP classification.
The performance of CTP and MELD scores in predicting survival of patients with upper gastrointestinal bleeding is comparable[13,14]. The better performance of ALBI in the current study was most probably due to omitting the subjective factors (ascites and encephalopathy) in the CTP score. The MELD score also includes creatinine that may be affected temporarily during gastrointestinal tract bleeding. Additionally, the INR results, as noted by Lisman et al[15] showed great variation among seven different European laboratories and Trotter et al[16] also confirmed such a variation in INR levels among 14 different laboratories in the United States. However, the adapted version for variceal bleeding showed significantly better performance compared with the basic version.
The performance of PALBI, an updated version of ALBI, in predicting mortality was significantly better than the ALBI score possibly because the PALBI score includes platelet count which reflects the effect of portal hypertension; the main cause of acute variceal bleeding. In other scenarios as testing the prognostic performance after radiofrequency ablation, ALBI has been proved to be superior to PALBI[17]. Thus, it appears that ALBI has a better prognostic power in patients with minimal liver dysfunction, whereas PALBI appears to be of more value in stratifying risk for portal hypertension.
The present study is the first to evaluate the performance of the PALBI score in predicting in-hospital mortality after variceal bleeding. The performance of the ALBI score in predicting the in-hospital mortality of acute upper gastrointestinal bleeding was previously tested by Zou et al[18]. Their estimated AUROC result for the ALBI score was in agreement with the current study. However, they found the performance of ALBI comparable to the CTP and MELD scores. However, it is worth noting that in their study the cohort was much smaller than the present cohort (631 vs 1517) and unlike the current study not all patients underwent endoscopy and hence the source of bleeding was not restricted to variceal bleeding.
The incidence of early rebleeding during hospitalization (within 1 wk) among our patients was 3.12%. Several studies reported overall rebleeding rates of 2.56%, 3.2%, 6.1%, 3.9%[19-23]. PALBI was significantly better than MELD, CTP and ALBI in predicting rebleeding. If the PALBI score could replace the CTP score and MELD, it would be easier and quicker to identify candidates for an early transjugular intra-hepatic porto-systemic shunt procedure. Furthermore, the use of PALBI score allows for better survival stratification within a CTP class. PALBI is a purely objective score incorporating both liver function and portal hypertension and is not subject to the inconsistencies of CTP resulting from the inclusion of ascites and encephalopathy.
Despite the limitation of being a retrospective single-center study, the large number of patients with all patients undergoing endoscopy and bleeding confirmed to be from varices, provides further validity to our findings.
In conclusion, the PALBI score is a simple, objective score that may be a good option for predicting in-hospital rebleeding and mortality in patients with acute variceal bleeding. We recommend future prospective studies to further validate the PALBI score and its value in predicting long-term prognosis.
ARTICLE HIGHLIGHTS
Research background
In 1964, the CTP score was proposed to assess patients with portal hypertension related to gastrointestinal tract bleeding and was used later to assess patients with cirrhosis in general. Many doubts have been raised recently regarding the performance of the CTP score as a subjective scoring system with abrupt points and overlapping parameters. Recently, new scoring systems such as the ALBI and PALBI scores were proposed which use linear predictive equations to overcome the disadvantages of the CTP score.
Research motivation
To identify a reliable prognostic score to predict the short-term outcome of patients with acute variceal bleeding.
Research objectives
Scoring systems with more specific parameters and using linear predictive equations showed better performance than subjective point-based scoring systems.
Research methods
We retrospectively analyzed the data of a large number of patients with acute variceal bleeding and their short-term outcome.
Research results
The PALBI score is a simple, objective score that is considered a good option for predicting in-hospital rebleeding and mortality in patients with acute variceal bleeding in comparison to other scoring systems. However, we still recommend performing a prospective study to better analyze the performance of these scoring systems.
Research conclusions
The PALBI score could be used to predict the short-term outcome and the incidence of rebleeding in patients with acute variceal bleeding.
Research perspectives
Performing a prospective large-scale multicenter study to test the performance of these scores in different management settings.
Footnotes
Institutional review board statement: The study was approved by the institutional review board (IRB number IRB00003413).
Informed consent statement: Informed consent was obtained from all patients.
Conflict-of-interest statement: Imam Waked received grants/research supports or speaker’s honoraria from Abbvie, Marcyrl, MSD, Mylan, Onxio, and Pharco. The authors report no other conflicts of interest in this work.
Manuscript source: Unsolicited manuscript
Peer-review started: September 19, 2019
First decision: October 14, 2019
Article in press: January 14, 2020
Specialty type: Gastroenterology and Hepatology
Country of origin: Egypt
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Garbuzenko DV, Mura VL S-Editor: Dou Y L-Editor: Webster JR E-Editor: Wu YXJ
Contributor Information
Omar Elshaarawy, Department of Hepatology and Gastroenterology, National Liver Institute, Menoufia University, Shebin Elkom 32511, Egypt.
Naglaa Allam, Department of Hepatology and Gastroenterology, National Liver Institute, Menoufia University, Shebin Elkom 32511, Egypt.
Eman Abdelsameea, Department of Hepatology and Gastroenterology, National Liver Institute, Menoufia University, Shebin Elkom 32511, Egypt. eabdelsameea@liver-eg.org.
Asmaa Gomaa, Department of Hepatology and Gastroenterology, National Liver Institute, Menoufia University, Shebin Elkom 32511, Egypt.
Imam Waked, Department of Hepatology and Gastroenterology, National Liver Institute, Menoufia University, Shebin Elkom 32511, Egypt.
Data sharing statement
No additional data are available.
References
- 1.Lebrec D. Life, death, and varices. Gut. 2001;49:607–608. doi: 10.1136/gut.49.5.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 3.van Dam GM, Gips CH, Reisman Y, Maas KW, Purmer IM, Huizenga JR, Verbaan BW. Major clinical events, signs and severity assessment scores related to actual survival in patients who died from primary biliary cirrhosis. A long-term historical cohort study. Hepatogastroenterology. 1999;46:108–115. [PubMed] [Google Scholar]
- 4.Shetty K, Rybicki L, Carey WD. The Child-Pugh classification as a prognostic indicator for survival in primary sclerosing cholangitis. Hepatology. 1997;25:1049–1053. doi: 10.1002/hep.510250501. [DOI] [PubMed] [Google Scholar]
- 5.Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864–871. doi: 10.1053/he.2000.5852. [DOI] [PubMed] [Google Scholar]
- 6.Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D'Amico G, Dickson ER, Kim WR. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–470. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 7.Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, O'Beirne J, Fox R, Skowronska A, Palmer D, Yeo W, Mo F, Lai P, Iñarrairaegui M, Chan SL, Sangro B, Miksad R, Tada T, Kumada T, Toyoda H. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33:550–558. doi: 10.1200/JCO.2014.57.9151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roayaie S, Jibara G, Berhane S, Tabriz-ian P, Park JW, Yang J, Yan L, Han G, Izzo F, Chen M, Blanc JF, Kudo M, Roberts LR, Sherman M, Johnson P. 851 PALBI-An Objective Score Based on Platelets, Albumin Bilirubin Stratifies HCC Patients Undergoing Resection & Ablation Better than Child's Classification. Hepatology. 2015;62(SUPPL 1):624A–690A. [Google Scholar]
- 9.Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, Austin A, Ferguson JW, Olliff SP, Hudson M, Christie JM Clinical Services and Standards Committee of the British Society of Gastroenterology. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015;64:1680–1704. doi: 10.1136/gutjnl-2015-309262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fortune BE, Garcia-Tsao G, Ciarleglio M, Deng Y, Fallon MB, Sigal S, Chalasani NP, Lim JK, Reuben A, Vargas HE, Abrams G, Lewis MD, Hassanein T, Trotter JF, Sanyal AJ, Beavers KL, Ganger D, Thuluvath PJ, Grace ND, Groszmann RJ Vapreotide Study Group. Child-Turcotte-Pugh Class is Best at Stratifying Risk in Variceal Hemorrhage: Analysis of a US Multicenter Prospective Study. J Clin Gastroenterol. 2017;51:446–453. doi: 10.1097/MCG.0000000000000733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hansmann J, Evers MJ, Bui JT, Lokken RP, Lipnik AJ, Gaba RC, Ray CE., Jr Albumin-Bilirubin and Platelet-Albumin-Bilirubin Grades Accurately Predict Overall Survival in High-Risk Patients Undergoing Conventional Transarterial Chemoembolization for Hepatocellular Carcinoma. J Vasc Interv Radiol. 2017;28:1224–1231.e2. doi: 10.1016/j.jvir.2017.05.020. [DOI] [PubMed] [Google Scholar]
- 12.Liu PH, Hsu CY, Hsia CY, Lee YH, Chiou YY, Huang YH, Lee FY, Lin HC, Hou MC, Huo TI. ALBI and PALBI grade predict survival for HCC across treatment modalities and BCLC stages in the MELD Era. J Gastroenterol Hepatol. 2017;32:879–886. doi: 10.1111/jgh.13608. [DOI] [PubMed] [Google Scholar]
- 13.Peng Y, Qi X, Dai J, Li H, Guo X. Child-Pugh versus MELD score for predicting the in-hospital mortality of acute upper gastrointestinal bleeding in liver cirrhosis. Int J Clin Exp Med. 2015;8:751–757. [PMC free article] [PubMed] [Google Scholar]
- 14.Chalasani N, Kahi C, Francois F, Pinto A, Marathe A, Bini EJ, Pandya P, Sitaraman S, Shen J. Model for end-stage liver disease (MELD) for predicting mortality in patients with acute variceal bleeding. Hepatology. 2002;35:1282–1284. doi: 10.1053/jhep.2002.32532. [DOI] [PubMed] [Google Scholar]
- 15.Lisman T, van Leeuwen Y, Adelmeijer J, Pereboom IT, Haagsma EB, van den Berg AP, Porte RJ. Interlaboratory variability in assessment of the model of end-stage liver disease score. Liver Int. 2008;28:1344–1351. doi: 10.1111/j.1478-3231.2008.01783.x. [DOI] [PubMed] [Google Scholar]
- 16.Trotter JF, Olson J, Lefkowitz J, Smith AD, Arjal R, Kenison J. Changes in international normalized ratio (INR) and model for endstage liver disease (MELD) based on selection of clinical laboratory. Am J Transplant. 2007;7:1624–1628. doi: 10.1111/j.1600-6143.2007.01822.x. [DOI] [PubMed] [Google Scholar]
- 17.Ho SY, Liu PH, Hsu CY, Chiou YY, Su CW, Lee YH, Huang YH, Lee FY, Hou MC, Huo TI. Prognostic Performance of Ten Liver Function Models in Patients with Hepatocellular Carcinoma Undergoing Radiofrequency Ablation. Sci Rep. 2018;8:843. doi: 10.1038/s41598-018-19251-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zou D, Qi X, Zhu C, Ning Z, Hou F, Zhao J, Peng Y, Li J, Deng H, Guo X. Albumin-bilirubin score for predicting the in-hospital mortality of acute upper gastrointestinal bleeding in liver cirrhosis: A retrospective study. Turk J Gastroenterol. 2016;27:180–186. doi: 10.5152/tjg.2016.15502. [DOI] [PubMed] [Google Scholar]
- 19.Khan A, Mannan F, Din Ru. Outcome of endoscopic band ligation for oesophageal variceal bleed in patients with chronic liver disease. Gomal J Med Sci. 2013;11:84–87. [Google Scholar]
- 20.Kuran S, Oğuz D, Parlak E, Asil M, Ciçek B, Kiliç M, Dişibeyaz S, Sahin B. Secondary prophylaxis of esophageal variceal treatment: Endoscopic sclerotherapy, band ligation and combined therapy--long-term results. Turk J Gastroenterol. 2006;17:103–109. [PubMed] [Google Scholar]
- 21.Petrasch F, Grothaus J, Mössner J, Schiefke I, Hoffmeister A. Differences in bleeding behavior after endoscopic band ligation: a retrospective analysis. BMC Gastroenterol. 2010;10:5. doi: 10.1186/1471-230X-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hameed K, Saeed A, Khan Y, Khan IM, Javed M. Endocopic band ligation: an ideal procedure to manage bleeding oesophageal varices. Ann Pak Inst Med Sci. 2007;3:234–237. [Google Scholar]
- 23.de Franchis R Baveno VI Faculty. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63:743–752. doi: 10.1016/j.jhep.2015.05.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No additional data are available.