Abstract
The concept of sleep health (adequate sleep duration and continuity, regular timing, satisfaction with sleep, and ability to maintain wakefulness during the day) is consistent with a definition of health as more than the absence of disease. Yet past research on women's sleep focused primarily on biological influences (e.g., hormonal fluctuations) or specific sleep disorders. We reviewed the literature on sleep health in women of childbearing age from the perspectives of health promotion and the social ecological model and identified needs for future research and intervention. At least 40% of women of childbearing age report inadequate sleep, and sleep is associated with short- and long-term health and performance outcomes. Numerous sociodemographic, psychosocial, role, familial, and community factors contribute to sleep, but few studies have addressed the contributions of these factors to sleep health in women of childbearing age, aside from those who are pregnant. Understanding these factors may assist in identifying women at particular risk for sleep difficulty; some may be modifiable, and other may signal the need for sleep interventions tailored to specific circumstances. Low-income women and those in ethnic and racial minority groups are at particular risk for disparities in sleep health. There is a need for research that addresses these factors and the development of interventions at the individual, family, and community levels to promote sleep health. Screening and intervention to promote health sleep and decrease sleep difficulty should be a standard of care in clinical, community, and workplace settings frequented by women.
Keywords: sleep, childbearing, women, health disparities, sleep health, prevention
Introduction
Sleep health (adequate sleep duration and sleep continuity, regular timing, satisfaction with sleep, and ability to maintain wakefulness during the day)1 is critical to health and well-being. This perspective, in contrast to a focus on sleep disorders, frames sleep as a target of health promotion, rather than focusing only on primary sleep disorders. Yet past research on women's sleep emphasized the contributions of reproductive hormonal fluctuations (i.e., menstruation, menopause, pregnancy, and the postpartum period),2 the effects of treatment of disease (e.g., breast cancer) on sleep, or specific sleep disorders, such as insomnia. Although these are important, focusing solely on these factors oversimplifies the multidimensional nature of sleep health and fails to account for the family, social, and environmental context in which sleep occurs, as described in the social ecological model.3–6
The purposes of this narrative, a summary of a presentation at the 2018 NIH Conference on Sleep and the Health of Women are to discuss (1) influences on sleep in women of childbearing age from a biobehavioral and social ecological perspective, (2) needs for future research, and (3) needs for intervention regarding sleep health of women of childbearing age.
Characteristics of Sleep Health in Women of Childbearing Age
Data from the U.S. National Health and Nutrition Survey (NHANES) on women between the ages of 15 and 44 years7 and a study of Canadian women8 revealed that more than half reported getting adequate sleep, whereas nonpregnant women were more likely to report short or very short sleep than pregnant women. Although the exact percentages were not reported, at least 40% of women of childbearing age report inadequate sleep, whereas 21% of the overall sample report trouble sleeping, with higher rates in nonpregnant women.7 This rate was lower than the rate of difficulty sleeping (27%) in the National Sleep Foundation poll of women between 18 and 64 years.9 Nevertheless, these data emphasize the need for attention to sleep health and understanding factors that contribute to it, as well as the consequences of sleep health, in women of childbearing age.
NHANES data indicate that 4.9% of women of childbearing age report having a diagnosed sleep disorder,7 rates considerably lower than population-based estimates. One in four women have insomnia,10 and 9%–23% may have sleep-disordered breathing,11 although these data did not separate younger women from postmenopausal women who have higher rates of sleep apnea and may overestimate the rate in women of childbearing age. The discrepancies in these data emphasize the need for more comprehensive screening and treatment for sleep disorders during the childbearing years, especially because the negative consequences of sleep often begin to emerge during this period (e.g., obesity, prehypertension, prediabetes, and other conditions).
Factors That Contribute to Sleep Health
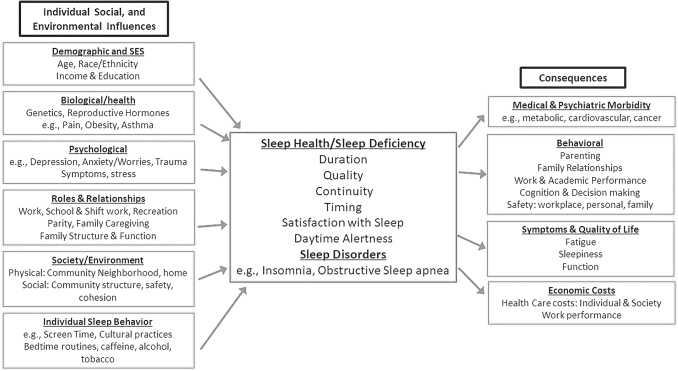
Contributors to sleep health and its inverse-sleep deficiency (less than adequate sleep duration and continuity, irregular timing, and poor sleep quality) include individual biological and behavioral factors, health and disease, family/social, lifestyle, and physical and social environmental factors, as depicted in Figure 1. These putative factors and sleep-related outcomes are drawn from the broad literature on sleep health, but few studies have addressed the sleep of women of childbearing age from a comprehensive perspective. Women of childbearing age are usually accomplishing life tasks, such as completing education, developing and fulfilling work and career plans, and raising families.12 These demands may influence sleep health, but sleep health may also influence how women effectively accomplish their roles and responsibilities. Women also report stress and worries that may contribute to poor sleep.13,14 Improved understanding of factors contributing to sleep health is needed to guide interventions for women of childbearing age.
FIG. 1.
Individual, social, and environmental influences on sleep health and sleep deficiency and its consequences.
Race, ethnicity, and socioeconomic status contribute to sleep health. Black women had consistently shorter sleep than white women in both the United States and Canada,7,8 whereas women of Mexican descent7 in the United States and women of Asian or Arab backgrounds had worse sleep than white women.8 However, Amyx et al. reported that Black and Mexican American women were less likely than others to report sleep difficulty to a health care provider—a finding that may reflect either failure of health providers to screen for sleep disorders or lack of recognition by these women of the negative consequences of sleep disorders. These findings mirror the growing body of evidence regarding disparities in sleep health. Yet, to date, research on women of childbearing age is limited.
Several small studies focused predominantly on sleep of women of childbearing age with diverse racial/ethnic backgrounds in two Northeastern U.S. communities. Among African American women between the ages of 21 and 50 years (a subset of data from a larger group of women),15 74% had poor sleep quality as measured by the Pittsburgh Sleep Quality index (Nam et al., unpublished data), whereas 60% of a group of low-income urban racially and ethnically diverse women had poor sleep quality,16 and 70% of a third group of similar mothers of young children reported poor sleep quality.14 Taken together, these findings suggest significant sleep deficiency in these women.
Consistent with past studies, psychological distress, including anxiety, depression, and trauma symptoms, was common in ethnically and racially diverse women and closely associated with sleep quality.16 Low-income minority mothers of young children reported high levels of stress and worries about finances and other concerns that interfered with their sleep. Most also reported co-sleeping with their children, a behavior that may contribute to poor sleep quality for all involved,14 whereas comorbidity, back pain, and other discomforts, and low levels of social cohesion were also associated with poor sleep quality (Nam et al., unpublished data).14,15 Among minority women, the average body mass index of 31 (Nam et al., unpublished data)14,15 and Berlin Questionnaire scores suggest high risk for sleep apnea, but none of these women had been evaluated for this problem. Taken together, these findings suggest that low-income minority women are at especially high risk for poor sleep health.
Qualitative interviews with racially and ethnically diverse mothers revealed that they understood the importance of sleep health for themselves and their children. They learned and used both effective and noneffective sleep promotion strategies from their families and were interested in learning to improve sleep for themselves and their children.14 Although these findings underscore the interrelationships among sleep in family members as described in the literature, for example,17 the primary emphasis of these studies was on children's sleep health, rather than the parent or mother's sleep.
Research Needs Related to Sleep Health in Women of Childbearing Age
Despite growth in understanding of sleep health, there has been relatively little focus on sleep health and sleep disorders in women of childbearing age aside from pregnancy, the postpartum, and the peri-menopause/menopause in the population overall. There is a pressing need to characterize sleep health and the prevalence of sleep disorders within this developmental period and to fully understand the factors that contribute to sleep health and its consequences at the individual, family/relational, and community levels, as suggested in Figure 1. There is a particular need for understanding of disparities in sleep health. Although a detailed review of the literature is beyond the scope of this report, examples of areas for research are detailed in Table 1 and briefly described here.
Table 1.
Research Needs Regarding Sleep Health in Women of Childbearing Age
| Characterize sleep health (duration, quality, timing, and sleep disorders) in women of childbearing age (including those who are not pregnant!) |
| Understand the multilevel biological, behavioral, social, and environmental influences on women's sleep in addition to the contributions of hormonal fluctuations |
| Examine the influence of family roles, caregiving, and relationships on women's sleep |
| Develop and test interventions to promote sleep health from a health promotion and population health perspective |
| Explain the contributions of multidimensional aspects of sleep health to important health outcomes in women |
| Understand sleep and sleep needs of low-income and minority women who are at particular risk for negative health outcomes |
| Consider differences in rural vs. urban environments as influences on sleep health |
| Examine the effects of community, workplace, and social interventions and policies on sleep health in women |
| Evaluate the efficacy and effectiveness of behavioral interventions to promote sleep health, as well as the effects of efforts to improve sleep deficiency |
| Conduct implementation science and health services research to ascertain the best ways to assure the reach, implementation, adoption, and maintenance of sleep health interventions for women of childbearing age |
At the biological level, there is an ongoing need to understand gender differences in “omics,” neurotransmitters, and other biological mechanisms that may explain sleep/wake patterns, as well as the contributions of stress.18 Despite recommendations to examine the effects of lifestyle and social factors on women's sleep, based on National Sleep Foundation data ∼10 years ago,9 little is known about these contributors, especially among women of childbearing age. Research is also needed that considers the family as a unit and the ways in which family members interact with one another, especially regarding daily routines, including activity, sleep, and nutrition. Although these considerations have primarily focused on children,19 routines may also be beneficial to parents.
Given growing evidence of disparities in sleep health and sleep-related outcomes, such as metabolic and cardiovascular conditions, there is also a pressing need to consider the specific needs of low-income and racially and ethnically diverse women, including characterizing sleep and influencing factors and developing, testing, and delivering sleep interventions for these women. Although efficacious behavioral strategies are available to address insomnia and sleep duration, few studies have addressed these interventions for women of childbearing age or the contexts in which they live. It may be particularly important to address social and environmental influences due to high levels of stress and frequent economic adversity that may contribute to noise, crowded or unsafe environments that may influence sleep. Cultural influences may also play an important role and may be beneficial or deleterious to sleep health but may also influence the feasibility and acceptability of traditional sleep health interventions.
At the community and population health levels, there is a need to design and evaluate the effects of messaging and educational efforts designed to raise awareness and knowledge about the importance and nature of adequate sleep and ways of managing self- and family sleep behaviors. This should also include best venues or modalities with which to disseminate this information for specific populations of women and their families. Finally, as in other areas of sleep science, the application of implementation science and health services research methods are needed to assure the widespread reach, adoption, implementation and maintenance of efficacious sleep health promotion strategies specific to the needs of women.
Implications for Practice and Community Health Promotion
Although limited, extant knowledge regarding sleep in women of childbearing age has important implications for clinical practice and public health (Table 2). From a clinical perspective, there is a need to include sleep assessment as a standard of care in clinical settings where women of childbearing age receive health care (e.g., gynecological/women's health settings and primary care). It is important to address all of the dimensions of sleep health, including sleep duration, timing, continuity, satisfaction, and daytime sleepiness and alertness, as well as signs of primary sleep disorders (e.g., snoring). Evaluation for prevalent primary sleep disorders, especially insomnia, and sleep-disordered breathing, is especially important for those at highest risk. For example, women with anxiety, depression, or trauma-related disorders may be at especially high risk for insomnia, and women who are obese are at high risk for sleep-disordered breathing. Women who are raising young children or those with other caregiving responsibilities and those who work evening or night shifts are also at particular risk for sleep deficiency and circadian rhythm disorders. The inclusion of brief screening questions in the electronic medical record may assist clinicians. There is also a need for protocols that assist in identifying women at risk and criteria for treatment and referral.
Table 2.
Strategies to Promote Sleep Health in Women of Childbearing Age
| Make it a standard of care to assess and intervene (including follow-up) in women's health and primary care clinical encounters for sleep concerns: sleep duration and maintenance, timing, quality, satisfaction, sleepiness/alertness, and signs of specific sleep disorders |
| Incorporate sleep promotion into public health, community, and primary care settings: focus on importance of adequate sleep and practical strategies |
| Emphasize obtaining 7–8 hours of daily sleep and regular sleep patterns |
| Raise awareness about the outcomes of sleep health |
| Include sleep hygiene strategies—bed time behavior, home environment, rituals, and decrease caffeine |
| Reduce screen time |
| Consider the potential impact of stress and emotional distress on sleep |
| Promote work/life/caregiver balance |
| Promote sleep health in the workplace, including strategies for shift workers |
| Target low-income and minority women who may be at particular risk for sleep deficiency |
| Incorporate principles of sleep health when working with family members (e.g., children) |
| Address sleep from the perspective of family interactions |
From a population health perspective, public service announcements and community education in churches, childcare centers, fitness centers, colleges and universities, and workplace settings frequented by women may assist in raising awareness about the importance of sleep health and practical strategies to extend sleep and regularize bedtimes. Raising awareness about efficacious behavioral approaches (e.g., reducing screen time, regular bedtimes with bedtime rituals, relaxation approaches, and reducing caffeine) may contribute to improvements in sleep health. Workplace health promotion programs may also facilitate sleep health and improve worker productivity and health outcomes, although these practices have not been studied specifically in women.20
Conclusions
Women of childbearing age are at risk for sleep deficiency due to multiple biological, behavioral, social, and environmental factors, and sleep deficiency may contribute to short- and longer-term health outcomes. There is a need for research that improves understanding of these factors and clinical and population-based interventions to address sleep health.
Acknowledgements
The author acknowledges the contributions of Lois Sadler, PhD, RN, FAAN, Professor, Yale School of Nursing and Soohyun Nam, PhD, RN, Associate Professor, Yale School of Nursing to the development of this presentation and the resulting article.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
References
- 1. Buysse DJ. Sleep health: Can we define it? Does it matter? Sleep 2014;37:9–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nowakowski S, Meers JM. Cognitive behavioral therapy for insomnia and women's health: Sex as a biological variable. Sleep Med Clin 2019;14:185–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Centers for Disease Control. The social ecological model: A framework for prevention. Centers for Disease Control, 2007. Available at: www.cdc.gov/violenceprevention/overview/social-ecologicalmodel.html Accessed January24, 2015
- 4. Grandner MA. Addressing sleep disturbances: An opportunity to prevent cardiometabolic disease? Int Rev Psychiatry 2014;26:155–176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Dev Psychol 1986;22:723–742 [Google Scholar]
- 6. Rosa EM, Tudge J. Urie Bronfenbrenner's theory of human development: Its evolution from ecology to bioecology. J Family Theory Rev 2013;5:243–258 [Google Scholar]
- 7. Amyx M, Xiong X, Xie Y, Buekens P. Racial/ethnic differences in sleep disorders and reporting of trouble sleeping among women of childbearing age in the United States. Mat Child Health J 2017;21:306–314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vezina-Im LA, Lebel A, Gagnon P, Nicklas TA, Baranowski T. Individual correlates of sleep among childbearing age women in Canada. Behav Sleep Med 2019;17:634–645 [DOI] [PubMed] [Google Scholar]
- 9. Baker FC, Wolfson AR, Lee KA. Association of sociodemographic, lifestyle, and health factors with sleep quality and daytime sleepiness in women: Findings from the 2007 National Sleep Foundation “Sleep in America Poll”. J Women's Health (2002) 2009;18:841–849 [DOI] [PubMed] [Google Scholar]
- 10. Kessler RC, Berglund PA, Coulouvrat C, et al. Insomnia and the performance of US workers: Results from the America insomnia survey. Sleep 2011;34:1161–1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jehan S, Auguste E, Zizi F, et al. Obstructive sleep apnea: Women's perspective. J Sleep Med Disord 2016;3. [PMC free article] [PubMed] [Google Scholar]
- 12. McGoldrick M. Women and the family lifecycle. In: McGoldrick M, Carter EA, Garcia-Preto N, eds. Expanding family life cycle: Individual, family, and social perspectives, 5th ed. Boston: Pearson, 2016:45–62 [Google Scholar]
- 13. Zambrano DN, Mindell JA, Reyes NR, Hart CN, Herring SJ. “It's not all about my baby's sleep”: A qualitative study of factors influencing low-income African American mothers' sleep quality. Behav Sleep Med 2016;14:489–500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Caldwell BA, Redeker NS, Ordway M, Sadler NS. Parent perspectives on sleep and sleep habits among young children living in economic adversity. J Pediatric Health Care 2020;34:10–22 [DOI] [PubMed] [Google Scholar]
- 15. Nam S, Whittemore R, Jung S, Latkin C, Kershaw T, Redeker NS. Physical neighborhood and social environment, beliefs about sleep, sleep hygiene behaviors, and sleep quality among African Americans. Sleep Health 2018;4:258–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Caldwell BA, Redeker NS. Sleep patterns and psychological distress in women living in an inner city. Res Nurs Health 2009;32:177–190 [DOI] [PubMed] [Google Scholar]
- 17. Meltzer LJ, Montgomery-Downs HE. Sleep in the family. Pediatr Clin North Am 2011;58:765–774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McEwen BS, Karatsoreos IN. Sleep deprivation and circadian disruption: Stress, allostasis, and allostatic load. Sleep Med Clin 2015;10:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Buxton OM, Chang AM, Spilsbury JC, Bos T, Emsellem H, Knutson KL. Sleep in the modern family: Protective family routines for child and adolescent sleep. Sleep Health 2015;1:15–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Redeker NS, Caruso CC, Hashmi SD, Mullington JM, Grandner M, Morgenthaler TI. Workplace interventions to promote sleep health and an alert, healthy workforce. J Clin Sleep Med 2019;15:649–657 [DOI] [PMC free article] [PubMed] [Google Scholar]