Abstract
Background:
Achilles tendon rupture leads to weakness of ankle plantarflexion. Treatment of Achilles tendon rupture should aim to restore function while minimizing weakness and complications of management.
Purpose:
To determine the influence of factors (age, sex, body mass index [BMI], weight, time from injury to operative repair, and tightness of repair) in the initial surgical management of patients after an acute Achilles tendon rupture on 12-month functional outcome assessment after percutaneous and minimally invasive repair.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
From May 2012 to January 2018, patients sustaining an Achilles tendon rupture receiving operative repair were prospectively evaluated. Tightness of repair was quantified using the intraoperative Achilles tendon resting angle (ATRA). Heel-rise height index (HRHI) was used as the primary 12-month outcome variable. Secondary outcome measures included Achilles tendon total rupture score (ATRS) and Tegner score. Stepwise multiple regression was used to create a model to predict 12-month HRHI.
Results:
A total of 122 patients met the inclusion criteria for data analysis (mean ± SD age, 44.1 ± 10.8 years; 78% male; mean ± SD BMI, 28.1 ± 4.3 kg/m2). The elapsed time to surgery was 6.5 ± 4.0 days. At 12-month follow-up, patients had an HRHI of 82% ± 16% and performed 82% ± 17% of repetitions compared with the noninjured side. Participants had a mean ATRS of 87 ± 15 and a median Tegner score of 5 (range, 1-9), with a reduction in Tegner score of 2 from preinjury levels. The relative ATRA at 12 months was –4.8° ± 3.9°. Multiple regression identified younger age (B = ±0.006; P < .001) and greater intraoperative ATRA (B = 0.005; P = .053) as predictors of more symmetrical 12-month HRHI (R 2 = 0.19; P < .001; n = 120).
Conclusion:
Age was found to be the strongest predictor of outcome after Achilles tendon rupture. The most important modifiable risk factor was the tightness of repair. It is recommended that repair be performed as tight as possible to optimize heel-rise height 1 year after Achilles tendon rupture and possibly to reduce tendon elongation.
Keywords: Achilles tendon rupture, operative repair, outcome, heel-rise
Since the 2000s, the primary outcome of Achilles tendon rupture research has expanded from complications, including rerupture,49,54 to patient-specific outcome measures,27,35,40 functional parameters,12 and tendon biomechanical characteristics.46,48 The identification of modifiable factors that influence patient recovery and guide prognostication is one of the most important steps in optimizing individualized treatment.39
Several patient characteristics may influence prognosis after Achilles tendon rupture.10,14,39,53 Older age10,39 and higher body mass index (BMI)39 have been identified as predictors of inferior outcome. There is conflicting evidence for the effect of sex, with female patients reporting more symptoms and demonstrating more variable recovery of calf muscle endurance in 1 study14 and better outcome in another.3
There are several factors involved in the initial management of an Achilles tendon rupture that may influence the outcome. One of the most prominently discussed is whether operative or nonoperative management leads to the best long-term outcome after rupture.38,44,55,56 Moreover, there is growing evidence that a larger separation between the ruptured tendon ends leads to an increased risk of tendon rerupture and worse functional outcome.25,52 Recent randomized controlled studies have shown that operative repair of Achilles tendon rupture results in significantly improved strength24,40,54 and reduced elongation17,18 compared with nonoperative treatment. The elapsed time to repair is also controversial, with improved outcome reported if repair is performed within 48 hours of injury.50 Other studies,7,42 however, show no differences in terms of outcome if surgery is performed within a week of injury.
One of the complications of Achilles tendon rupture is known to be tendon elongation.30,33 Elongation occurs from an early stage during treatment22,34,37 and correlates with decreased plantarflexion strength17,41 and heel-rise height.13 It appears that surgical repair has a greater ability to minimize the tendon elongation that occurs by approximating the tendon ends and shortening the resting length of the tendon. However, the direct influence of tightness of repair on functional outcome has yet to be determined.
The aim of this study was to determine the influence of patient-related and surgical factors (age, sex, BMI, weight, time from injury to repair, and tightness of repair) in the initial management of patients after percutaneous or minimally invasive repair for Achilles tendon rupture. We hypothesized that greater age, BMI, weight, increased time to surgery, and reduced tightness of repair would be associated with diminished heel-rise height (as measured by the heel-rise height index13 [HRHI]) at 12 months postoperatively.
Methods
This was a retrospective analysis of data collected from individuals receiving operative repair after Achilles tendon rupture. A review by a research ethics committee was not required for this study. Between May 2012 and November 2017, a total of 147 patients who sustained an Achilles tendon rupture and underwent operative repair at Princess Royal Hospital, a district general hospital, were prospectively evaluated for outcome over time. Of these patients, 122 had complete data for the primary outcome of interest in this analysis (HRHI at 12 months) and were included in this observational study. Patient characteristics are shown in Table 1.
TABLE 1.
Patient Characteristics (N = 122 Patients)a
| Age, y | 44.1 ± 10.8 |
| Sex (male:female), n | 95:27 |
| Weight, kg (n = 112) | 86.0 ± 15.6 |
| Body mass index, kg/m2 (n = 108) | 28.1 ± 4.3 |
| Elapsed time to repair, days (n = 121) | 6.5 ± 4.0 |
| Injured side (left:right), n | 62:60 |
aValues are represented as mean ± SD unless otherwise noted.
Diagnosis was established from the clinical signs of rupture: a palpable gap of the tendon at the midsubstance,28 abnormal calf squeeze test,28 and increased Achilles tendon resting angle (ATRA) compared with the noninjured ankle.8 ATRA is a quantified measure of the resting angle that has been shown to be a valid, reliable, responsive, and reproducible measure in individuals with Achilles tendon rupture.5,6,16,57 Participants with musculotendinous junction rupture as seen on imaging were excluded from this series. All operative repairs were performed by the same surgeon (M.R.C.). Patients initially underwent a percutaneous repair7; however, based upon contemporaneous audit, minor changes in the operative technique were made in an attempt to reduce complication rates. The operative technique was subsequently changed from percutaneous to minimally invasive repair.
Operative Technique
The majority of patients elected to have operative repair performed under local anesthesia. This consisted of 20 to 30 mL of 0.5% bupivacaine with 1:200,000 adrenaline injected into the site of the incisions with an additional 10 mL of 1% lignocaine, after 2% chlorhexidine skin preparation. Antibiotic prophylaxis consisted of 1 dose of 1.5 g cefuroxime/1 g flucloxacillin intravenously.7
A 1- to 2-cm longitudinal skin incision was made at the level of the palpable tendon gap. Additional “stab” incisions were made just proximal to the Achilles insertion on either side of the tendon, together with longitudinal stab incisions 3 cm and 5 cm proximal to the palpable gap on either side of the tendon. A curved mosquito clip was then used to enlarge the perforation in the fascia cruris to prevent the capture of the fascia within the suture. Next, a modified Bunnell suture was inserted across the tendon first proximally and then directed distally, using 4 strands of No. 1 Maxon suture with a Mayo needle (Wundnadeln Steril, PS204B00, Acufirm Ernst-Kratz GmbH 63303), before emerging from the incision over the rupture site. A 4-strand Kessler suture was inserted into the distal stump. With the ankle held in full plantarflexion, the sutures were tied under tension using a surgeon’s knot and 4 subsequent single throws. The lateral knot was tied first and then buried into the apposed tendon ends. Then, a medial knot was tied and a clip was applied, and the ATRA of the injured ankle was assessed with goniometry, with care taken not to touch the sterile operative field.6 The suture could then be tightened, so that the ATRA indicated greater plantarflexion than the noninjured ankle, before knot completion. Before skin closure, the knots were buried deep into the repair.
There were modifications made to the operative technique, including repair of the fascia cruris, changes in suture material, and the number of suture strands; thus, the patients were categorized into 5 groups to evaluate differences in the operative techniques (Table 2). Additionally, for patients with a short distal stump, a transosseous 2.5-mm drill hole was placed in the calcaneus, through which the distal suture was placed, and subsequently passed through the substance of the distal Achilles tendon to the incision at the rupture site.
TABLE 2.
Operative Technique Groupings
| Group | Surgical Technique | n (%) | Sural Nerve | Suture Material | No. of Strands | Distal Suture |
|---|---|---|---|---|---|---|
| 1 | Minimally invasive | 22 (18.0) | Visualized and mobilized | Absorbable monofilament | 8 | Transtendinous |
| 2 | Minimally invasive | 18 (14.8) | Visualized and mobilized | Nonabsorbable braided | 4 | Transtendinous |
| 3 | Minimally invasive | 47 (38.5) | Visualized and mobilized | Nonabsorbable braided | 6 | Transtendinous |
| 4 | Minimally invasive | 30 (24.6) | Visualized and mobilized | Nonabsorbable braided | 6 | Transtendinous |
| 5 | Minimally invasive | 5 (4.1) | Visualized and mobilized | Nonabsorbable braided | 6 | Transosseous |
Postoperative Management and Rehabilitation
Immediately after surgery, patients used a functional brace, consisting of a reinforced synthetic below-knee cast, in gravity plantarflexion. The cast was split along the midlateral lines and held in place with Velcro elasticated straps. Patients were permitted to mobilize full weightbearing on their metatarsal heads using axillary crutches. Low–molecular weight heparin thromboprophylaxis was used for 2 weeks early in the series; however, the use of this was extended to 6 weeks beginning in 2016. At the 2-week time point, patients had their skin sutures removed and commenced active plantarflexion, inversion, and eversion exercises, while they maintained the anterior shell held in place with the straps for all weightbearing for the next 4 weeks. At the 6-week time point, the anterior shell was discontinued, and patients were given a 1.5-cm heel wedge for all weightbearing activities until 3 months postoperatively; they were also referred for physiotherapy treatment. Patients typically used crutches until the 8-week time point or when they felt able to resume normal walking. Plyometric exercises and stretching were permitted at 3 months. No other restrictions were made in terms of return to activity or sports.
Evaluation
Patients were evaluated by the first author (M.R.C.) at presentation, immediately after operative repair and at 6 weeks and 3, 6, 9, and 12 months. Patients’ BMI was assessed at presentation. BMI along with sex, weight, time from injury to repair, surgical treatment technique, and tightness of repair were considered primary treatment factors of interest.
Tightness of repair was quantified using the intraoperative ATRA, as it has been found to relate to tendon length.11,57 A negative ATRA is relative ankle dorsiflexion, indicating Achilles tendon lengthening, and a positive ATRA ankle plantar flexion indicating shortening. The ATRA was measured with the patient in the prone position and the knee flexed to 90°, as described by Carmont et al.7 The ATRA was measured on the injured and noninjured sides to determine the relative ATRA.6 In addition, the ATRA was assessed immediately after surgery and at all subsequent evaluations to assess the tightness of the repair. Similar techniques have been used as a guide for the requirement of operative repair during nonoperative management protocols.11 Additionally, the dynamic form of this assessment, originally described by Matles,31 has recently been used to examine for lengthening after surgical repair.29
The HRHI was selected as the primary variable of interest because of its relationship to long-term outcomes after an Achilles tendon rupture.4 HRHI is defined as heel-rise height (injured)/heel-rise height (noninjured) and is expressed as percentage. The injured ankle was tested first. Patients were permitted to place their fingertips on the wall for balance while performing heel-rises to fatigue, keeping their knee straight. The number of repetitions performed (heel-rise repetition index) was also recorded.
Secondary outcome measures reported at the 12-month time point for descriptive purposes included Achilles tendon total rupture score (ATRS)9,36 and Tegner score.51
Statistical Analysis
All data were analyzed using SAS (Version 14; SAS Institute) with the assistance of a biostatistician. Descriptive statistics were reported using means and standard deviations as well as medians and ranges. As the aim of this study was to identify the relationships between initial management and short-/medium-term outcome, data from patient presentation (intraoperative, 6-week, and 12-month time points) are reported only for descriptive purposes in this study. Univariate linear regression was used to identify the relationship between 12-month HRHI and the variables of interest at patient presentation (age, sex, BMI, weight, time from injury to repair, and operative technique), the tightness of repair (intraoperative the ATRA), and the ATRA at 6 weeks.
Stepwise multiple regression was then used to build a model using factors of interest from the early time points to predict the 12-month HRHI. Only input factors that had a statistically significant relationship to HRHI on univariate analysis were included in the multiple regression. Input factors were inserted into the model in the order of strongest to weakest relationship. Input factors were retained in the model if the significance of the factor within the model was P < .10; otherwise, the factor was dropped from the model. The a priori level of significance was set to be ≤.05. As we were concerned that postoperative complications (ie, re-rupture, deep wound infection, and deep adhesion of the tendon) could influence functional results in the long term and affect the predictive ability of the model, we performed a sensitivity analysis, in which patients who sustained a complication were excluded from the analysis. There were several instances in which data were not collected from a given patient because of clinical constraints (time, staff demands, etc), so missing data were handled by reporting the total number of participants in each analysis.
Results
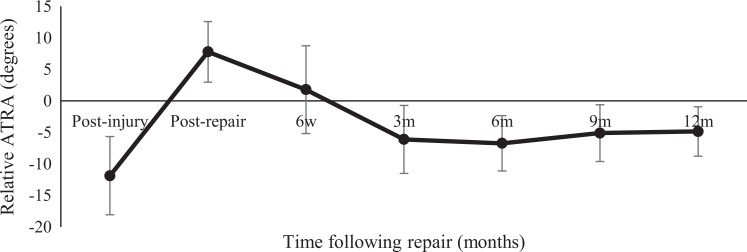
In the 122 study patients, the relative ATRA was –12° ± 6° preoperatively, 8° ± 5° intraoperatively, and 2° ± 7° at 6 weeks postoperatively. Two patients (1.6%) sustained a re-rupture.
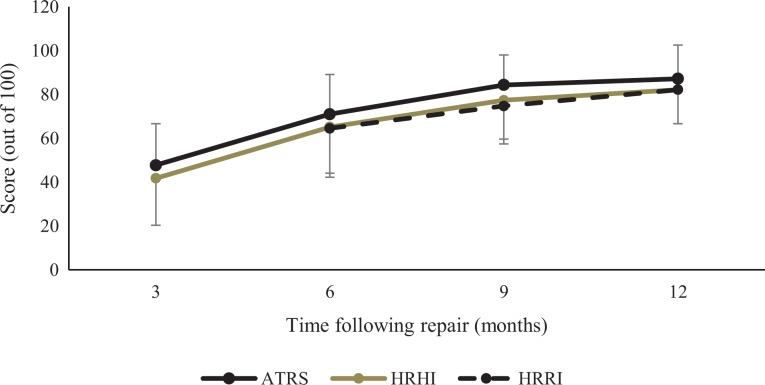
At 12 months postoperatively, patients had a mean ± SD HRHI of 82% ± 16% and performed 82% ± 17% of repetitions on the injured relative to the noninjured side during the heel-rise test (Figure 1). The relative ATRA at 12 months was –4.8° ± 3.9° (Figure 2). Patients had a mean postoperative ATRS of 87 ± 15 and a median Tegner score of 5 (range, 1-9). Patients reported a median preinjury Tegner score of 7 (range, 2-10).
Figure 1.
Achilles tendon total rupture score (ATRS) and functional outcomes for heel-rise height index (HRHI) and heel-rise repetition index (HRRI) over time. The error bars overlap for the different time points, so errors in ATRS are shown upward and for HRHI and HRRI errors are shown downward.
Figure 2.
The change in relative Achilles tendon resting angle (ATRA) over time. A positive ATRA reflects plantarflexion and a negative ATRA reflects dorsiflexion.
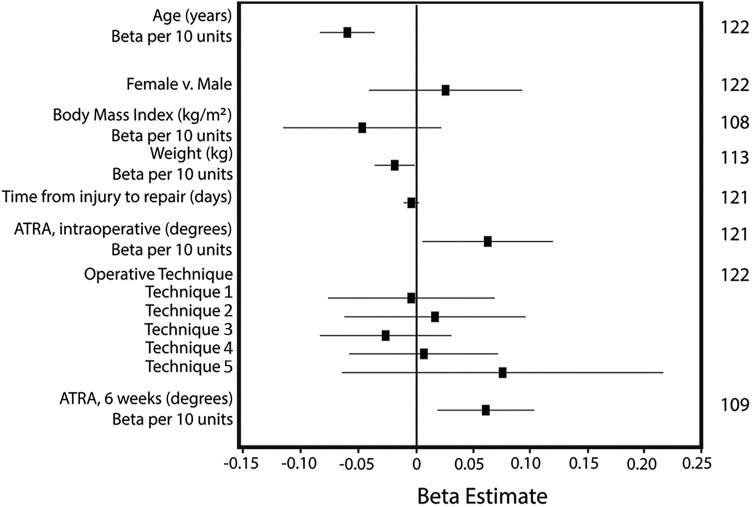
Heel-Rise Height Index
The results of the univariate analysis are shown in Figure 3. The HRHI had a statistically significant univariate relationship with age and ATRA (preoperatively, intraoperatively, and at 6 weeks postoperatively). A total of 120 patients had complete data sets and could be included in the multiple regression analysis. First, age was entered into the model, followed by intraoperative ATRA and preoperative ATRA. Preoperative ATRA was not significant (P > .1) and was accordingly dropped from the model. The final model (R 2 = 0.19; P < .001; n = 120) included age (parameter estimate = −0.006; P < .001) and intraoperative ATRA (parameter estimate = 0.005; P = .053; the parameter estimate is in ratio, not percentage, format). This model was repeated in the sensitivity analysis excluding patients who had sustained any postoperative complication. The outcome of this model was similar to that of the entire group, indicating that the presence of a postoperative complication did not affect outcome (model: R 2 = 0.21, P < .001, n = 98; for age: parameter estimate = −0.006, P < .001; for intraoperative ATRA: parameter estimate = 0.006, P = .060).
Figure 3.
Results of univariate analysis of early treatment variables on 12-month postoperative heel-rise height index (HRHI). The far-right column indicates the total number of patients included in each comparison. The beta estimate is an indicator of the effect of the variable. Points to the left of the y-axis indicate factors that negatively influence HRHI. Error bars crossing the y-axis indicate factors that are likely not statistically significant. Points falling farther from the y-axis indicate factors that have a stronger relationship to HRHI.
Discussion
The present study is the first to quantify the effect of tightness of Achilles tendon repair on 12-month postoperative heel-rise height assessment. While age continued to be the strongest predictor of heel-rise function at 12 months postrepair, tighter Achilles tendon repairs resulted in a greater heel-rise height at 12 months after surgery. The outcome from Achilles tendon rupture has been shown to be multifactorial, consisting of nonmodifiable and modifiable risk factors. Contrary to the findings of other studies,10,12 the nonmodifiable characteristics of sex or BMI were not found to be a significant indicator of heel-rise function at 12 months. Other modifiable factors included in this analysis (ie, time elapsed from injury to repair and variations in surgical technique) did not relate to heel-rise function at 12 months.
In the present study, age and intraoperative relative ATRA accounted for 19% to 21% of the variation in heel-rise height symmetry at 12 months. With every additional decade of life, the heel-rise height symmetry decreased by 6%. These findings are in agreement with those of the study by Olsson et al,39 in which age was shown to be a predictor of outcome at 12 months. In addition, for every increased degree of ATRA tightness, measured immediately after surgery, there was a 0.5% improvement in HRHI at 12 months. This translates into a 5% to 6% improvement in heel-rise height symmetry if the repair is 10° tighter at surgery.
It would be considered logical to repair the Achilles tendon in comparable tension with the noninjured side.23,27,35,40,43 Since ruptured tendons elongate during healing and rehabilitation, and lengthening leads to poor function,14,18,22,47 they would benefit from being repaired in increased plantarflexion. Repairing in greater tightness to the contralateral side is commonly performed15,19,21,26,29,42,45; however, to the best of our knowledge, this is the first study providing data to support the influence of tightness of repair on functional (heel-rise) performance. Excessive elongation of the Achilles tendon after rupture is common. In some very flexible patients, excessive tendon tightness after repair may be a problem; however, this occurs rarely. This excessive tendon tightness may limit ankle dorsiflexion.
Previously published studies12,39 have identified sex-related differences in outcome and a propensity for improved function in individuals with lower BMI. Olsson et al39 found that higher BMI was associated with greater symptoms, with a 5-unit increase in BMI leading to a 10-point reduction in ATRS. In earlier studies,1,16 female patients have been found to report more symptoms and lower ATRS scores, both in the short and in the long term. Female patients have also been reported to have inferior HRHI compared with their male counterparts after surgery.14 The present data did not reveal similar findings; however, it is reasonable that placing greater body weight on a recovering tendon would have implications for tendon healing.
This study did not show a significant relationship between time from injury to repair and heel-rise height at 12 months postsurgery. Recently, an animal study32 reported improved 6-week tendon mechanics in mice treated within 48 hours after injury. In humans, clinical studies42,50 have shown conflicting outcomes for those undergoing repair within 48 hours of injury. Svedman et al50 reported that repairs performed within 48 hours of injury lead to an improved outcome; however, other studies7,42 have found no differences in outcome if surgery is performed within a week of injury. It may be that outcomes in the first weeks postinjury are affected by time to repair, but these improvements are mitigated over time and are not reflected in longer term, functional outcomes.
In this series, a standard suture configuration consisting of a modified Bunnell and Kessler suture configuration was used initially. Over the 5.7 years of data collection, this technique was modified based upon an understanding of the current literature and contemporaneous audit. Suture materials were adjusted, as it was thought that the absorption of the suture material used in technique 1 (see Table 2) may have permitted tendon elongation, and so this was changed to a nonabsorbable suture.5 A 4-strand nonabsorbable suture was used out of concern for potential overtightness and persistent knot prominence (technique 2), but early elongation was suspected5; therefore, the number of strands of repair was increased to 6. However, at 1 year, there was no difference in patient-reported symptoms or function outcome between any of the techniques.5
The clinical and biomechanical mode of failure was noted to distal pullout and the heavy weight of patients sustaining reruptures. A subsequent change was to use a transosseous calcaneal drill hole for distal stabilization for patients >100 kg or for patients with a small distal stump (<2 cm) (technique 5); this method was similar to the one described by Bijlsma and van der Werken.2 On comparing these modifications, no association was found between the treatment technique and heel-rise performance, although the small number of patients (n = 5) treated with this technique is a limitation of the study. It is notable that 2 of these patients sustained traumatic rerupture; however, we could not determine whether this was the result of the surgical technique or characteristics of this patient group (ie, high BMI).
Strengths of this study include the following: (1) a large number of patients were evaluated over time and (2) all repairs were performed by the same surgeon. Although all patients received standardized weightbearing immobilization, physical therapy resources, and return-to-sport recommendations, it is not known if individual patients performed exactly the same physiotherapy. The focus on a patient series from a single surgeon eliminates interobserver error, increasing the value of comparisons within the cohort. It does, however, also introduce performance bias, which means that the results should be interpreted with care in comparison with other series. Although this study was a large retrospective case series, the data were prospectively collected.
Limitations of this study include the gradual introduction of outcome measures with time, as their reliability was established. This unfortunately reduced the numbers of the data set for analysis, which may be overcome in the future by multicenter or registry studies. Although the ATRA was originally considered to be an indirect measure of tendon length6 and has been shown to correlate with ultrasonographically determined tendon length,57 it actually is not a sole measure of tendon length. The ATRA could be considered to be a quantification of the overall tension in the musculotendinous unit. The influence of muscle fiber pennation and fiber length has been considered,20 which is also likely to influence the ATRA.
Conclusion
Age of the patient was the strongest predictor of outcome after an acute Achilles tendon rupture. The most important modifiable risk factor was the tightness of repair. It is recommended that repair is performed as tightly as possible to optimize heel-rise height at 1 year after surgery for Achilles tendon rupture.
Acknowledgment
The authors acknowledge Bengt Bengtsson for his help with the statistical analysis.
Footnotes
Final revision submitted December 18, 2019; accepted December 23, 2019.
One or more of the authors has declared the following potential conflict of interest or source of funding: Research bursaries were received from the British Association of Sport and Exercise Medicine and the British Orthopaedic Foot and Ankle Society (to M.R.C.). M.R.C. has received hospitality payments from Arthrex for instructing on educational courses. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the Royal Shrewsbury Hospital Research and Development/Clinical Trials Office (ref: Carmont001).
References
- 1. Aujla R, Patel S, Jones A, Bhatia M. Predictors of functional outcome in non-operatively managed Achilles tendon ruptures. Foot Ankle Surg. 2018;24(4):336–341. [DOI] [PubMed] [Google Scholar]
- 2. Bijlsma TS, van der Werken C. Operative treatment of Achilles tendon rupture: a minimally invasive technique allowing functional after-treatment. Orthopaedics and Traumatology. 2000;8(4):285–290. [Google Scholar]
- 3. Bostick GP, Jomha NM, Suchak AA, Beaupré LA. Factors associated with calf muscle endurance recovery 1 year after Achilles tendon rupture repair. J Orthop Sports Phys Ther. 2010;40(6):345–351. [DOI] [PubMed] [Google Scholar]
- 4. Brorsson A, Willy RW, Tranberg R, Silbernagel KG. Heel-rise height deficit 1 year after Achilles tendon rupture relates to changes in ankle biomechanics 6 years after injury. Am J Sports Med. 2017;45(13):3060–3068. [DOI] [PubMed] [Google Scholar]
- 5. Carmont MR, Jellers JA, Brorsson A, et al. Functional outcomes of Achilles tendon minimally invasive repair using 4- and 6- strand non-absorbable suture: a cohort comparison study. Orthop J Sports Med. 2017;5(8):2325967117723347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carmont MR, Silbernagel KG, Brorsson A, Olsson N, Maffulli N, Karlsson J. The Achilles tendon resting angle as an indirect measure of Achilles tendon length following rupture, repair and rehabilitation. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2015;2(2):49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Carmont MR, Silbernagel KG, Edge A, et al. Functional outcome of percutaneous Achilles repair: improvements in Achilles tendon total rupture score during the first year. Orthop J Sports Med. 2013;1(1):2325967113494584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Carmont MR, Silbernagel KG, Mathy A, Mulji Y, Karlsson J, Maffulli N. Reliability of Achilles tendon resting angle and calf circumference measurement techniques. Foot Ankle Surg. 2013;19(4):245–249. [DOI] [PubMed] [Google Scholar]
- 9. Carmont MR, Silbernagel KG, Nilsson-Helander K, Mei-Dan O, Karlsson J, Maffulli N. Cross cultural adaptation of the Achilles tendon total rupture score with reliability, validity and responsiveness evaluation. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1356–1360. [DOI] [PubMed] [Google Scholar]
- 10. Domej-Arverud E, Anundsson P, Hardell E, et al. Ageing, deep vein thrombosis and male gender predict poor outcome after acute Achilles tendon rupture. Bone Joint J. 2016;98(12):1635–1641. [DOI] [PubMed] [Google Scholar]
- 11. Ecker TM, Bremer AK, Krause FG, Müller T, Weber M. Prospective use of a standardized nonoperative early weightbearing protocol of Achilles rupture: 17 years of experience. Am J Sports Med. 2016;44(4):1004–1010. [DOI] [PubMed] [Google Scholar]
- 12. Grävare Silbernagel K, Brorsson A, Olsson N, Eriksson BI, Karlsson J, Nilsson-Helander K. Sex differences in outcome after an acute Achilles tendon rupture. Orthop J Sports Med. 2015;3(6):2325967115586768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Grävare Silbernagel K, Nilsson-Helander K, Thomeé E, Eriksson BI, Karlsson J. A new measurement of heel-rise endurance with the ability to detect functional deficits in patients with Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):258–264. [DOI] [PubMed] [Google Scholar]
- 14. Grävare Silbernagel K, Steele R, Manal K. Deficits in heel-rise height and Achilles tendon elongation occur in patients recovering from an Achilles tendon rupture. Am J Sports Med. 2012;40(7):1564–1571. [DOI] [PubMed] [Google Scholar]
- 15. Groetelaers RP, Janssen L, van der Velden J, et al. Functional treatment or cast immobilization after minimally invasive repair of an Achilles tendon rupture: prospective, randomized trial. Foot Ankle Int. 2014;35(8):771–778. [DOI] [PubMed] [Google Scholar]
- 16. Hansen MS, Barfod KW, Kristensen MT. Development and reliability of the Achilles tendon length measure and comparison with the Achilles tendon resting angle on patients with an Achilles tendon rupture. Foot Ankle Surg. 2017;23(4):275–280. [DOI] [PubMed] [Google Scholar]
- 17. Heikkinen J, Lantto I, Flinkkila T, et al. Soleus atrophy is common after the non-surgical treatment of Achilles tendon ruptures: a randomized controlled clinical trial comparing surgical and nonsurgical functional treatments. Am J Sports Med. 2017;45(6):1395–1404. [DOI] [PubMed] [Google Scholar]
- 18. Heikkinen J, Lantto I, Piilonen J, et al. Tendon length, calf muscle atrophy and strength deficit after acute Achilles tendon rupture: long term follow-up of patients in a previous study. J Bone Joint Surg Am. 2017;99(18):1509–1515. [DOI] [PubMed] [Google Scholar]
- 19. Hsu AR, Jones CP, Cohen BE, Davis WH, Ellington JK, Anderson RB. Clinical outcomes and complications of percutaneous Achilles repair system versus open technique for acute Achilles tendon ruptures. Foot Ankle Int. 2015;36(11):1279–1286. [DOI] [PubMed] [Google Scholar]
- 20. Hullfish TJ, O’Connor KM, Baxter JR. Gastrocnemius fascicles are shorter and more pinnate throughout the first month following acute Achilles tendon rupture. Peer J. 2019;7:e6788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kakiuchi M. A combined open and percutaneous technique for repair of tendo Achillis. Comparison with open repair. J Bone Joint Surg Br. 1995;77(1):60–63. [PubMed] [Google Scholar]
- 22. Kangas J, Pajala A, Siira P, Hämäläinen M, Leppilahti J. Early functional treatment versus early immobilization in tension of the musculotendinous unit after Achilles rupture repair: a prospective, randomized clinical study. J Trauma. 2003;54(6):1171–1180. [DOI] [PubMed] [Google Scholar]
- 23. Keller A, Ortiz C, Wagner E, Wagner P, Mococain P. Mini-open tenorrhaphy of acute Achilles tendon ruptures: medium-term follow up of 100 cases. Am J Sports Med. 2014;42(3):731–736. [DOI] [PubMed] [Google Scholar]
- 24. Lantto I, Heikkinen J, Flinkkila T, et al. A prospective randomized trial comparing surgical and nonsurgical treatments of acute Achilles tendon ruptures. Am J Sports Med. 2016;44(9):2406–2414. [DOI] [PubMed] [Google Scholar]
- 25. Lawrence JE, Nasr P, Fountain DM, Berman L, Robinson AHN. Functional outcomes of conservatively managed acute ruptures of the Achilles tendon. Bone Joint J. 2017;99(1):87–93. [DOI] [PubMed] [Google Scholar]
- 26. Liechti DJ, Moatshe G, Backus JD, Marchetti DC, Clanton TO. A percutaneous knotless technique for acute Achilles tendon ruptures. Arthrosc Tech. 2018;7(2):e171–e178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lim CS, Lees D, Gwynne-Jones DP. Functional outcome of acute Achilles tendon rupture with and without operative treatment using identical functional bracing protocol. Foot Ankle Int. 2017;38(12):1331–1336. [DOI] [PubMed] [Google Scholar]
- 28. Maffulli N. The clinical diagnosis of subcutaneous tear of the Achilles tendon. A prospective study in 174 patients. Am J Sports Med. 1998;26(2):266–270. [DOI] [PubMed] [Google Scholar]
- 29. Manegold S, Tsitsilonis S, Gehlen T, Kopf S, Duda GN, Agres AN. Alterations in structure of the muscle-tendon unit and gait pattern after percutaneous repair of Achilles tendon rupture with the Dresden instrument. Foot Ankle Surg. 2019;25(4):529–533. [DOI] [PubMed] [Google Scholar]
- 30. Maquirriain J. Achilles tendon rupture: avoiding tendon lengthening during surgical repair and rehabilitation. Yale J Biol Med. 2011;84(3):289–290. [PMC free article] [PubMed] [Google Scholar]
- 31. Matles AL. Rupture of the tendo Achilles: another diagnostic sign. Bull Hosp Joint Dis. 1975;36(1):48–51. [PubMed] [Google Scholar]
- 32. Misir A, Kizkapan TB, Arikan Y, et al. Repair within the first 48 h in the treatment of acute Achilles tendon ruptures achieves the best biomechanical and histological outcomes [published ahead of print]. Knee Surg Sports Traumatol Arthrosc. 2019. May 22 doi: 10.1007/s00167-019-05536-w [DOI] [PubMed] [Google Scholar]
- 33. Molloy A, Wood EV. Complications of treatment of Achilles tendon ruptures. Foot Ankle Clin. 2009;14(4):745–759. [DOI] [PubMed] [Google Scholar]
- 34. Mortensen HM, Skov O, Jensen PE. Separation of tendon ends after Achilles tendon repair: a prospective, randomized clinical and radiographic study. J Bone Joint Surg Am. 1999;81(7):983–990. [DOI] [PubMed] [Google Scholar]
- 35. Nilsson-Helander K, Silbernagel K, Thomeé R, et al. Acute Achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38(11):2186–2193. [DOI] [PubMed] [Google Scholar]
- 36. Nilsson-Helander K, Thomeé R, Silbernagel KG, et al. The Achilles tendon total rupture score (ATRS): development and validation. Am J Sports Med. 2007;35(3):421–426. [DOI] [PubMed] [Google Scholar]
- 37. Nyström B, Holmlund D. Separation of tendon ends after suture of Achilles tendon. Acta Orthop Scand. 1983;54(4):620–621. [DOI] [PubMed] [Google Scholar]
- 38. Ochen Y, Beks RB, van Heijl M, et al. Operative treatment versus non-operative treatment of Achilles tendon ruptures: a systematic review and meta-analysis. BMJ. 2019;364:K5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Olsson N, Petzold M, Brorsson A, et al. Predictors of clinical outcome after acute Achilles tendon ruptures. Am J Sports Med. 2014;42(6):1448–1455. [DOI] [PubMed] [Google Scholar]
- 40. Olsson N, Silbernagel KG, Eriksson BI, et al. Stable surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med. 2013;41(12):2867–2876. [DOI] [PubMed] [Google Scholar]
- 41. Pajala A, Kangas J, Siira P, Ohtonen P, Leppilahti J. Augmented compared with non-augmented surgical repair of a fresh total Achilles tendon rupture. A prospective randomized study. J Bone Joint Surg Am. 2009;91(5):1092–1100. [DOI] [PubMed] [Google Scholar]
- 42. Park YH, Jeong SM, Choi GW, Kim HJ. How early must an acute Achilles tendon rupture be repaired? Injury. 2017;48(3):776–780. [DOI] [PubMed] [Google Scholar]
- 43. Patel VC, Lozano-Calderon S, McWIlliam J. Immediate weight-bearing after modified percutaneous Achilles tendon repair. Foot Ankle Int. 2012;33(12):1093–1097. [DOI] [PubMed] [Google Scholar]
- 44. Reda Y, Farouk A, Abdelmonem I, El Shazly OA. Surgical versus non-surgical treatment for acute Achilles tendon rupture. A systematic review of the literature and meta-analysis [published ahead of print]. Foot Ankle Surg. 2019. Apr 4 doi: 10.1016/j.fas.2019.03.010 [DOI] [PubMed] [Google Scholar]
- 45. Rippstein PF, Jung M, Assal M. Surgical repair of acute Achilles tendon rupture using a “mini-open” technique. Foot Ankle Clin. 2002;7(3):611–619. [DOI] [PubMed] [Google Scholar]
- 46. Rosso C, Buckland DM, Polzer C, et al. Long-term biomechanical outcomes after Achilles tendon ruptures. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):890–898. [DOI] [PubMed] [Google Scholar]
- 47. Schepull T, Aspenberg P. Early controlled tension improves the material properties of healing human Achilles tendons after ruptures: a randomized trial. Am J Sports Med. 2013;41(11):2550–2557. [DOI] [PubMed] [Google Scholar]
- 48. Schepull T, Kvist J, Aspenberg P. Early E-modulus of healing Achilles tendons correlates with late function: similar results with or without surgery. Scand J Med Sci Sports. 2012;22(1):18–23. [DOI] [PubMed] [Google Scholar]
- 49. Soroceanu A, Sidwa F, Aarabi S, Kaufman A, Glazebrook M. Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials. J Bone Joint Surg Am. 2012;94(23):2136–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Svedman S, Juthberg R, Edman G, Ackermann PW. Reduced time to surgery improves patient reported outcome after Achilles tendon rupture. Am J Sports Med. 2018;46(12):2929–2934. [DOI] [PubMed] [Google Scholar]
- 51. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 52. Westin O, Nilsson-Helander K, Silbernagel KG, Möller M, Kälebo P, Karlsson J. Acute ultrasonography investigation to predict re-ruptures and outcomes in patients with an Achilles tendon rupture. Orthop J Sports Med. 2016;4(10):2325967116667920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Westin O, Svedman S, Senorski EH, et al. Older age predicts worse function 1 year after an acute Achilles tendon rupture: a prognostic multicentre study on 391 patients. Orthop J Sports Med. 2018;6(12):2325967118813904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Willits K, Amendola A, Bryant D, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am. 2010;92(17):2767–2775. [DOI] [PubMed] [Google Scholar]
- 55. Wu Y, Mu Y, Yin L, Wang Z, Liu W, Wan H. Complications in the management of acute Achilles tendon rupture: a systematic review and network meta-analysis of 2060 patients. Am J Sports Med. 2019;47(9):2251–2260. [DOI] [PubMed] [Google Scholar]
- 56. Yang X, Meng H, Quan Q, Peng J, Lu S, Wang A. Management of acute Achilles tendon ruptures: a review. Bone Joint Res. 2018;7(10):561–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Zellers JA, Carmont MR, Silbernagel KG. Achilles tendon resting angle relates to tendon length and function. Foot Ankle Int. 2018;39(3):343–348. [DOI] [PMC free article] [PubMed] [Google Scholar]