Effective concentration of tranexamic acid can be achieved within 1 hour after oral administration in postpartum women.
OBJECTIVE:
To evaluate the pharmacokinetics of tranexamic acid after oral administration to postpartum women.
METHODS:
We conducted a single-center pharmacokinetic study at Teaching Hospital—Jaffna, Sri Lanka, on 12 healthy postpartum women who delivered vaginally. After oral administration of 2 g of immediate-release tranexamic acid 1 hour after delivery, pharmacokinetic parameters were measured on plasma samples at 0, 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 5, 6, 8, 10, and 12 hours. Plasma tranexamic acid concentrations were determined by high-performance liquid chromatography. The outcome measures were maximum observed plasma concentration, time to maximum plasma concentration, time to reach effective plasma concentration, time period effective serum concentration lasted, area under the curve for drug concentration, and half-life of tranexamic acid.
RESULTS:
The mean maximum observed plasma concentration was 10.06 micrograms/mL (range 8.56–12.22 micrograms/mL). The mean time to maximum plasma concentration was 2.92 hours (range 2.5–3.5 hours). Mean time taken to reach the effective plasma concentration of 5 micrograms/mL and the mean time this concentration lasted were 0.87 hours and 6.73 hours, respectively. Duration for which plasma tranexamic acid concentration remained greater than 5 micrograms/mL was 5.86 hours. Half-life was 1.65 hours. Area under the curve for drug concentration was 49.16 micrograms.h/mL (range 43.75–52.69 micrograms.h/mL).
CONCLUSION:
Clinically effective plasma concentrations of tranexamic acid in postpartum women may be achieved within 1 hour of oral administration. Given the promising pharmacokinetic properties, we recommend additional studies with larger sample sizes to investigate the potential of oral tranexamic acid for the treatment or prophylaxis of postpartum hemorrhage.
Postpartum hemorrhage is one of the major complications in obstetrics and one of the leading causes of maternal mortality worldwide, especially in developing countries, where it accounts for 25% of maternal deaths.1,2 The use of intravenous tranexamic acid is recommended for the treatment of postpartum hemorrhage if oxytocin and other uterotonics fail to stop bleeding or if it is thought that the bleeding may be partly due to trauma.3 Intravenous administration of tranexamic has been shown to be safe and effective in trauma and surgery, with no apparent increase in vascular occlusive events.4 One of the main barriers to rapid treatment with tranexamic acid is the need for intravenous injection.5
The effective plasma concentration of tranexamic acid that has been shown to cause significant inhibition of systemic fibrinolysis in adults is 5–10 micrograms/mL, with near maximal inhibition between 10 and 15 micrograms/mL.6 At a minimum concentration of 5 micrograms/mL, tranexamic acid has been shown to increase the clot lysis time from 6 to 16 minutes.7
Our study was designed to investigate the pharmacokinetics of oral tranexamic acid, a key step toward considering its use, especially in low-resourced countries, in an oral form for treatment or prophylaxis of postpartum hemorrhage.
METHODS
The study was conducted at the University Obstetric Unit, Teaching Hospital—Jaffna, after obtaining ethical approval from Ethics Review Committee of the Faculty of Medicine, University of Jaffna. All procedures performed were in accordance with good clinical practice. The study cohort comprised 12 healthy postpartum women aged 24–33 years who delivered singleton neonates vaginally.8 Recruited participants were screened for contraindications to tranexamic acid: past and current history of intravascular clotting, hemorrhagic events, and procoagulant disorders. None of the pregnancies had been complicated by pregnancy-related medical disorders, and patients with any preexisting comorbidities were not studied.
In addition to history and examination, electrocardiogram, liver function and renal function tests, full blood count, and coagulation profile were performed during the screening process. Written informed consent was obtained from all participants.
All participants underwent routine active management of the third stage, with intravenous oxytocin 10 international units after delivery of the neonate, delayed cord clamping, and controlled cord traction to deliver the placenta. Blood loss was estimated by weighing swabs and blood collected in a waterproof drape on the labor ward.
An arterial line was established to obtain blood; 1 hour after delivery, all study participants were administered the same preparation of 2 g of immediate-release tranexamic acid orally with 50 mL of water, which corresponds in strength to 1 g of intravenous tranexamic acid used to treat postpartum haemorrhage.5,9 The tranexamic acid preparation was supplied by the Teaching Hospital—Jaffna, and all participants were monitored for 24 hours for adverse effects.
Blood samples (1.8 mL) were collected in tubes containing 0.2 mL of 3% sodium citrate at 0, 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 5, 6, 8, 10, and 12 hours after administration of tranexamic acid and were immediately transported to the Biochemistry Laboratory, Faculty of Medicine, University of Jaffna, where the tranexamic acid assay was carried out. Within 1 hour of collection, samples were centrifuged at 2,000g for 15 minutes at room temperature, and supernatants were stored at −70°C until analysis.
During the analysis, samples were pretreated with leucine dehydrogenase, and plasma tranexamic acid concentration was determined by Shimadzu 10Avp high-performance liquid chromatography using ortho-phthalaldehyde derivatization as previously described.10–13 Samples were analyzed on an Ultra C18 5 micrometer 4.6×150-mm column, and the tranexamic acid derivative was detected fluorometrically (Fluorometer Shimadzu RF-10Axl).
Samples for quality control were prepared with a known quantity of standard tranexamic acid added to analyte-free human plasma. Peak area for the high-performance liquid chromatography assay was well correlated for plasma concentration from 0 micrograms/mL to 15 micrograms/mL. The accuracy of the assay method was between 97% and 99%. Descriptive statistics were calculated from plasma concentration compared with time data for single-dose pharmacokinetic parameters: maximum observed plasma concentration and time to maximum plasma concentration and their SDs using SPSS Statistics 23.
The linear trapezoidal method was used to calculate the area under the curve for drug concentration. Geometric means were calculated to estimate the time pharmacologically effective drug concentrations were reached and the duration for which the pharmacologically effective concentrations lasted. Elimination half-life for tranexamic acid was calculated as a parameter describing the linear terminal slope of the log concentrations.
RESULTS
A total of 12 postpartum women participated in this study. The mean age of the participants was 29 years, with a range of 24–33 (Table 1). None of the participants developed any adverse effects during the observational period. Among the 12 participants, the mean maximum observed plasma concentration was 10.06 micrograms/mL (range 8.56–12.22 micrograms/mL). The maximum observed plasma concentration was greater than 10 micrograms/mL in eight participants. The mean time to maximum plasma concentration was 2.92 hours (range 2.5–3.5 hours) (Fig. 1 and Box 1).
Table 1.
Demographics of the Participants
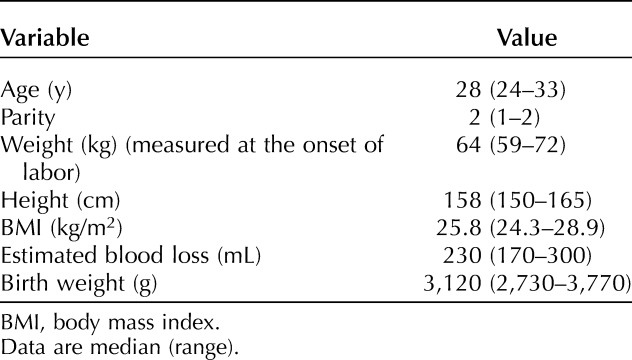
Fig. 1. Mean plasma concentration of tranexamic acid in micrograms/mL vs time curve after a single dose of 2 g of oral tranexamic acid in postpartum women. Error bars represent the range.

Muhunthan. Oral Tranexamic Acid in Postpartum Women. Obstet Gynecol 2020.
Box 1.
Pharmacokinetic Values
-
Cmax: 10.06 micrograms/mL
Range: 8.56–12.22 micrograms/mL
-
Tmax: 2.92 h
Range: 2.5–3.5 h
-
AUC0–12: 49.16 micrograms.h/mL
Range: 43.75–52.69 micrograms.h/mL
% deviation from the mean: 92.5–111%
T1/2: 1.65 h
-
Mean time course of concentration 5 micrograms/mL or greater (h)
Initial: 0.87
Final: 6.73
Duration: 5.86
Cmax, maximum observed plasma concentration; Tmax, time to maximum plasma concentration; AUC0–12, area under the curve for drug concentration; T1/2, half-life.
Because the effective plasma concentration of tranexamic acid that has been shown to cause significant inhibition of systemic fibrinolysis in adults is 5–10 micrograms/mL, we have presented the time course of plasma concentrations of tranexamic acid of 5 micrograms/mL and greater.6,7 After administration, the mean time taken to reach the plasma concentration of 5 micrograms/mL was 0.87 hours and lasted until 6.73 hours after the administration of the drug. The duration for which plasma tranexamic acid concentration remained greater than 5 micrograms/mL was 5.86 hours. Half-life was 1.65 hours. Area under the curve for drug concentration was 49.16 micrograms.h/mL, with a range of 43.75–54.69 micrograms.h/mL between individual patients, with percentage deviations of 92.5–111%.
DISCUSSION
We found that pharmacologically effective concentrations could be achieved within 1 hour of administration of 2 g oral tranexamic acid in postpartum women. Being able to achieve pharmacologically effective concentrations of 5 micrograms/mL and greater in postpartum women with the above oral dose within 1 hour was encouraging, because the World Health Organization guideline recommends the use of tranexamic acid within a 3-hour of window from birth.4 Though not comparable with intravenous administration of tranexamic acid, where effective plasma concentration is reached immediately, orally administered tranexamic acid shows potential to be effective in the management of postpartum hemorrhage.
This effective concentration is supported by a recent meta-analysis that concluded that the plasma tranexamic acid concentrations in adults from 10 micrograms/mL to 15 micrograms/mL provide near maximal inhibition of fibrinolysis, and concentrations from 5 micrograms/mL to 10 micrograms/mL provide significant inhibition of systemic fibrinolysis in adults.6,7 Further, this effective concentration lasted for almost 6 hours.
The maximum observed plasma concentration of 10.06±0.79 micrograms/mL is lower than the previously reported plasma concentrations of 13–14.8 micrograms/mL after a single oral-dose regimen in nonpregnant patients.9,14 This may be a result of the higher volume of distribution in postpartum women. The elimination half-life of 1.65 hours is shorter than previously reported values of 2–3 hours for nonpregnant patients.15 Because 95% of tranexamic acid is excreted by the kidneys, an increase of glomerular filtration rate by 50% during pregnancy may explain this observation.9,16 The main limitations of our study were its small sample size and relatively low body mass index of the study participants.
Given the promising pharmacokinetic properties, we recommend additional studies with larger sample sizes to investigate the potential of oral tranexamic acid for the treatment or prophylaxis of postpartum hemorrhage.
Footnotes
Supported by a university research grant (Ref: URG/2014/07) from the University of Jaffna, Sri Lanka.
Financial Disclosure The authors did not report any potential conflicts of interest.
The authors thank the obstetric registrars Mahendran Thanuya and Rajendraseelan Thuvarathipan, from Teaching Hospital—Jaffna, for assisting us in blood sample collection and monitoring participants for adverse effects; laboratory technicians Kirubahary Sritharan, Mahalingam Sutharsan, Kulasingam Thayananthan, and Thayalini Sukirthan for performing all the laboratory blood assays; and Nagaraja Varathan from the Department of Mathematics and Statistics for their help in the statistical and mathematical calculations.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/B775.
REFERENCES
- 1.Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 2016;387:462–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trends in maternal mortality: 1990 to 2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva (Switzerland): World Health Organization; 2015. [Google Scholar]
- 3.WHO recommendation on tranexamic acid for the treatment of postpartum haemorrhage. Geneva, Switzerland: World Health Organization; 2017. [PubMed] [Google Scholar]
- 4.CRASH-2 Collaborators. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomized, placebo-controlled trial. Lancet 2010;376:23–32. [DOI] [PubMed] [Google Scholar]
- 5.WOMAN Trial Collaborators. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with postpartum haemorrhage (WOMAN): an international, randomized, double-blind, placebo-controlled trial. Lancet 2017;389:2105–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Picetti R, Shakur-Still H, Medcalf RL, Standing JF, Roberts I. What concentration of tranexamic acid is needed to inhibit fibrinolysis? A systematic review of pharmacodynamics studies. Blood Coagul Fibrinolysis 2019;30:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dai L, Bevan D, Rangarajan S, Sorensen B, Mitchell M. Stabilization of fibrin clots by activated prothrombin complex concentrate and tranexamic acid in FVIII inhibitor plasma. Haemophilia 2011;17:e944–8. [DOI] [PubMed] [Google Scholar]
- 8.Committee for Medicinal Products for Human Use (CHMP). Guideline on the investigation of bioequivalence. London, UK: European Medicines Agency; 2010. [Google Scholar]
- 9.Pilbrant A, Schannong M, Vessman J. Pharmacokinetics and bioavailability of tranexamic acid. Eur J Clin Pharmacol 1981;20:65–72. [DOI] [PubMed] [Google Scholar]
- 10.Godel H, Graser T, Földi P, Pfaender P, Fürst P. Measurement of free amino acids in human biological fluids by high-performance liquid chromatography. J Chromatogr 1984;297:49–61. [DOI] [PubMed] [Google Scholar]
- 11.Uhe AM, Collier GR, McLennan EA, Tucker DJ, O'Dea K. Quantitation of tryptophan and other plasma amino acids by automated precolumn o-phthalaldehyde derivatization sensitive high performance liquid chromatography: improved sample preparation. J Chromatogr 1991;564:81–91. [DOI] [PubMed] [Google Scholar]
- 12.Ohshima T, Misono H, Soda K. Properties of crystalline leucine dehydrogenase for Bacillus sphaericus. J Biol Chem 1978;253:5719–25. [PubMed] [Google Scholar]
- 13.Beckett PR, Hardin DS, Davis TA, Nguyen HV, Wray-Cahen D, Copeland KC. Spectrophotometric assay for measuring branched-chain amino acid concentrations: application for measuring the sensitivity of protein metabolism to insulin. Anal Biochem 1996;240:48–53. [DOI] [PubMed] [Google Scholar]
- 14.Moore KA, Morin I, Marenco T, Lavigne J, Morelli G. Pharmacokinetic studies of two novel oral formulations of tranexamic acid therapy for heavy menstrual bleeding. Am J Ther 2012;19:190–8. [DOI] [PubMed] [Google Scholar]
- 15.Eriksson O, Kjellman H, Pilbrant Pharmacokinetics of tranexamic acid after intravenous administration to normal volunteers. Eur J Clin Pharmacol 1974;7:375–80. [DOI] [PubMed] [Google Scholar]
- 16.Cheung KL, Lafayette RA. Renal physiology of pregnancy. Adv Chronic Kidney Dis 2013;20:209–14. [DOI] [PMC free article] [PubMed] [Google Scholar]


