Abstract
Background
Reports of direct comparisons between operative techniques for anal fissure are variable in their results. These reports are either subject to selection bias (in non‐randomized studies) or observer bias (in all studies) or have inadequate numbers of patients enrolled to answer the question of efficacy.
Objectives
To determine the best technique for fissure surgery.
Search methods
The Cochrane Central Register of Controlled Trials and MEDLINE (1965‐2011), Medline (Pubmed) and Embase were searched March to 2011. The list of cited references in all included reports and several study authors also were helpful in finding additional comparative studies.
A total of four new trials were included in this update of the review.
Selection criteria
All reports in which there was a direct comparison between at least two operative techniques were reviewed and when more than one report existed for any given pair, that report was included. All studies must also be randomised. If crude data were not presented in the report, the authors were contacted and crude data obtained.
Data collection and analysis
The two most commonly used end points in all reported studies were treatment failure and post‐operative incontinence both to flatus and faeces. These are the only two endpoints included in the meta‐analysis.
Main results
Four trials, encompassing 406 patients were included in this update, with now a total of 2056 patients in the review from 27 studies that describe and analyze 13 different operative procedures. These operative techniques used by these studies include closed lateral sphincterotomy, open lateral internal sphincterotomy, anal stretch, balloon dilation, wound closure, perineoplasty, length of sphincterotomy and fissurectomy. Two new procedures in the update, similar to anal stretch were described‐ sphincterolysis and controlled intermittent anal dilatation. A new comparison was described, comparing the effects of unilateral internal sphincterotomy and bilateral internal sphincterotomy.
Manual Anal stretch has a higher risk of fissure persistence than internal sphincterotomy and also a significantly higher risk of minor incontinence than sphincterotomy. The combined analyses of open versus closed partial lateral internal sphincterotomy show little difference between the two procedures both in fissure persistence and risk of incontinence
Unilateral internal sphincterotomy was shown to be more likely to result in treatment failure compared to bilateral internal sphincterotomy, but there is no significant difference in the risk of incontinence.
Sphincterotomy was less likely to result in treatment failure when compared to fissurectomy, but there was no significant difference when considering post‐operative incontinence.
When comparing sphincterotomy to sphincterolysis, there was no significant difference between the two procedures both in treatment failure and risk of incontinence; the same is the case when comparing sphincterotomy with controlled anal dilation.
Authors' conclusions
Manual anal stretch should probably be abandoned in the treatment of chronic anal fissure in adults. For those patients requiring surgery for anal fissure, open and closed partial lateral internal sphincterotomy appear to be equally efficacious. More data are needed to assess the effectiveness of posterior internal sphincterotomy, anterior levatorplasty, wound suture or papilla excision. Bilateral internal sphincterotomy shows promise, but needs further research into its efficacy.
Plain language summary
This review assesses the usefulness surgery for anal fissure, a painful ulcer at the anal opening, by comparing the efficacy of various surgical procedures and how likely they are to result in complications.
Does surgery provide a long term cure for anal fissure? Yes, in better than 90% of patients having recommended operative procedures. Such operations include principally partial division of the anal sphincter, or controlled dilation of the narrowed anal opening. The technique for cutting the muscle has been refined in recent years and appears to improve cure and diminish the risk of bowel control problems. The method of achieving controlled anal dilation needs further investigation.
Can surgery cause anal incontinence? In the past, definitely, though in a minority of patients, and certain procedures were more prone to cause this complication. In recent years the risk appears to be diminishing as operative procedures have improved and is now a risk of less than 5%. Usually, in those affected individuals, there are only problems controlling flatus.
Summary of findings
Background
Anal fissure is an ulcer in the squamous epithelium of the anus located just distal to the muco‐cutaneous junction and usually in the posterior midline. It typically causes pain during defecation and for one to two hours afterwards (Goligher 1975). Atypical fissures may be multiple or off the midline, or be large and or irregular. These may be caused by inflammatory bowel disease, local or systemic malignancy, venereal infection, trauma, tuberculosis, or chemotherapy. The etiology of the typical or benign fissure is not so clear, nor are there accepted methods for fissure prevention. The most consistent finding in typical fissures is spasm of the internal anal sphincter, so severe that the pain caused by fissure is thought to be due to ischaemia (Schouten 1994). Relief of the spasm has been associated with relief of pain and healing of the fissure without recurrence. Historically the most common approach for relieving the spasm is surgical. Operative techniques commonly used for fissure in ano include: anal stretch, open lateral sphincterotomy, closed lateral sphincterotomy, posterior midline sphincterotomy and to a lesser extent dermal flap coverage of the fissure. Reports of direct comparisons between these techniques are variable in their results and for the most part under powered (Nelson 1999). Morbidity from these procedures, being principally incontinence, were once thought to be extremely rare (Abcarian 1980), but has in other reports, been found to be substantial (Garcia 1996), further emphasizing the importance of correct operative choice. These reports are either subject to selection bias (in non‐randomised studies) or observer bias (in all studies) or have inadequate numbers of patients enrolled to answer the question of efficacy. An analysis of the combined reports was therefore undertaken to determine if a preferred technique for fissure surgery can be elucidated.
Objectives
To assess the efficacy and morbidity of various operative procedures for anal fissure, in order to determine the best technique for fissure surgery.
Methods
Criteria for considering studies for this review
Types of studies
Studies in which participants were randomised to one of two operative procedures are the foci of this review. In this review update only randomised trials were considered eligible for inclusion and meta‐analysis. Studies that compared any surgical procedure to any non‐surgical procedure are included in the companion Cochrane review on non‐surgical therapy for anal fissure and will not be presented here.
Types of participants
Participants in this review are patients with chronic anal fissure. Chronic anal fissures are typically described as an anal fissure which lasts more than six weeks, with characteristic features such as a sentinel pile or hypertrophied anal papillae. It is common practice among surgeons reporting this disease not to operate on acute fissures or fissure in children, or atypical fissures (multiple, irregular, off the midline or not associated with sphincter spasm). This series of restrictions were stated in some reports, but not all.
Types of interventions
In this update, the specific operative procedures included are sphincterolysis, controlled intermittent anal dilatation, closed lateral internal sphincterotomy, unilateral internal sphincterotomy, bilateral internal sphincterotomy, and fissurectomy. Studies included in the previous update, compared the following operative procedures: anal stretch, open lateral internal sphincterotomy, closed lateral internal sphincterotomy, posterior midline sphincterotomy, dermal flap coverage of the fissure, anterior levatorplasty, pneumatic balloon anal dilation, radio frequency sphincter division, fissurectomy and, as surgical adjuncts to sphincterotomy, primary surgical wound closure or excision of anal skin tags (papillae).
Types of outcome measures
The two most significant end points are fissure treatment failure (which is used synonymously with persistence of anal pain or bleeding, and/or fissure recurrence) and post operative incontinence (minor incontinence to flatus or anal seepage, and major incontinence to faeces). All drop‐outs were considered to be treatment failures.
Search methods for identification of studies
For the prior update and this update, the following search strategies were used, searches conducted through January 2008, and March 2011 respectively
NEL 025 Search strategy Cochrane Central Register of Controlled Trials #1 anal fissure 178 edit delete #2 MeSH descriptor Fissure in Ano explode all trees 116 edit delete #3 fissure in ano 134 edit delete #4 (#1 OR #2 OR #3) 188 edit delete #5 surgery 68440 edit delete #6 anal sphincterotomy 102 edit delete #7 anal fissure therapy 117 edit delete #8 fissure therapy 263 edit delete #9 (#5 OR #6 OR #7 OR #8) 68617 edit delete #10 (#4 AND #9), from 2005 to 2007 41 edit delete
NEL 025 Search strategy Embase 2005‐2008
#28 #17 and #21 and #26 and (PY:EMBV = 2005‐2008) 77 #27 #17 and #21 and #26 290 #26 #22 or #23 or #24 or #25 1212663 #25 fissure therapy 503 #24 anal fissure therapy 2 #23 anal sphincterotomy 32 #22 surgery 1212488 #21 #18 or #19 or #20 1215 #20 fissure‐in‐ano 46 #19 explode "anus‐fissure" / all SUBHEADINGS in DEM,DER,DRM,DRR 1156 #18 anal fissure 620 Searches and results below from saved search history SS for RCT/CCT Embase Nov 2005 #17 #12 not #16 1665210 #16 #14 not #15 2675100 #15 #13 and #14 476674 #14 (ANIMAL or NONHUMAN) in DER 3151774 #13 HUMAN in DER 5823446 #12 #9 or #10 or #11 2665088 #11 (SINGL* or DOUBL* or TREBL* or TRIPL*) near ((BLIND* or MASK*) in TI,AB) 86449 #10 (RANDOM* or CROSS?OVER* or FACTORIAL* or PLACEBO* or VOLUNTEER*) in TI,AB 471851 #9 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 2452728 #8 "SINGLE‐BLIND‐PROCEDURE"/ all subheadings 6660 #7 "DOUBLE‐BLIND‐PROCEDURE"/ all subheadings 64218 #6 "PHASE‐4‐CLINICAL‐TRIAL"/ all subheadings 596 #5 "PHASE‐3‐CLINICAL‐TRIAL"/ all subheadings 7423 #4 "MULTICENTER‐STUDY"/ all subheadings 38817 #3 "CONTROLLED‐STUDY"/ all subheadings 2422081 #2 "RANDOMIZATION"/ all subheadings 22563 #1 "RANDOMIZED‐CONTROLLED‐TRIAL"/ all subheadings 119188
NEL 025 Search strategy Medline
#22 #11 and #15 and #20 and (PY:MEDS = 2005‐2007) 42 #21 #11 and #15 and #20 182 #20 #16 or #17 or #18 or #19 1660251 #19 fissure therapy 507 #18 anal fissure therapy 5 #17 anal sphincterotomy 44 #16 surgery 1660014 #15 #12 or #13 or #14 1537 #14 fissure‐in‐ano 124 #13 explode "Fissure‐in‐Ano" / all SUBHEADINGS in MIME,MJME,PT 1387 #12 anal fissure 686 Searches and results below from saved search history SS for RCT‐CCT at Medline (2006) #11 #7 not #10 661352 #10 #8 not (#8 and #9) 115717 #9 (humans ) in MESH 59 #8 (animals ) in MESH 115718 #7 #1 or #2 or #3 or #4 or #5 or #6 663193 #6 trial in TI 67043 #5 randomly in AB 114694 #4 (clinical trials) in MESH 139726 #3 placebo in AB 100149 #2 randomised in AB 153863 #1 clinical‐trial in pt 432798
For prior editions of this review the search strategy below was used.
The Cochrane Central Register of Controlled Trials Register (CENTRAL), 2005 issue 1, and the National Library of Medicine online PubMed search engine (www.nlm.nih.gov) was used to locate all published reports from 1965 to February, 2005 using the key words: surgery, anal fissure. English language was not a restriction in the search. Additional search terms included "anal sphincterotomy", "anal fissure therapy" and "fissure therapy". The list of cited references in all included reports also was helpful in finding additional comparative studies.
Data collection and analysis
All reports in which there was a direct comparison between at least two operative techniques were reviewed. If crude data were not presented in the report, the authors were contacted and crude data obtained.
Revman Analysis is used to evaluate the randomised studies only.
Results
Description of studies
The update search yielded 110 studies, of which 6 met the required criteria for the review. The studies included in the review had to be randomised, and directly compare at least two operative techniques. Of these 6 studies, one was excluded due to an excessive drop‐out rate (Hancke 2009) (an update of a previously published included study (Hancke 2003) in which 40% of the participants were lost to follow up), and the other, published only in abstract form and not yet submitted for full publication, due to lack of randomisation details Bouchard 2010. Efforts were made to contact the authors in the latter case; however, further information could not be obtained. For this update, four new studies have been added, bringing the total number of studies in this review to 27. 406 new patients have been included, with a total of 2056 patients and 13 operative procedures in the review.
The terminology used to describe endpoints varied from report to report. Some were used synonymously in this review, such as fissure recurrence, fissure persistence and need to re operate upon a fissure patient. Also Incontinence was stratified in many reports from soiling, to incontinence to flatus to incontinence to solid stool, whereas most other reports just reported minor incontinence, which is used synonymously with incontinence to flatus and seepage in this review. Anorectal manometry was performed after surgery in some reports (Olsen 1987; Marby 1979; Fischer 1976; Arroyo 2004; Hancke 2003; Renzi 2007) and correlated with other endpoints. Time to return to employment was reported in few studies (Jensen 1984;Marby 1979; Saad 1992; Yucel 2009). Duration of post operative pain and time to healing were rarely reported. One excluded study randomised subjects to postoperative Sitz baths and how it effected fissure healing (Gupta 2007), but with identical surgical procedures for all participants. Another excluded study was reclassified as a retrospective report, since surgeons were described as routinely allowed to change the procedure based upon the operative findings (Hawley 1969) after randomizations. The number of times this occurred in that report was not mentioned in the text. A total of seven reports compared anal stretch to internal sphincterotomy. The rate of incontinence varied from 0% to 27% in the anal stretch group and 0% to 20% in the sphincterotomy group. Interestingly the rate of persistence in those reports comparing open and closed sphincterotomy varied from only from 0% to 9%, though incontinence in these reports also varied from 1% to 30%. There were five reports comparing open and closed lateral internal sphincterotomy. There were three reports that looked at different lengths of sphincterotomy, two comparing sphincterotomy to the dentate line with the somewhat shorter division of sphincter to the level of the fissure apex (Mentes 2005; Elsebae 2007), and a third (Mentes 2008) included in this group though the comparison was somewhat different: division to the fissure apex or sufficient sphincter division to achieve a 30 mm anal aperture. There was one report that provided data comparing posterior midline sphincterotomy to lateral sphincterotomy (Saad 1992). There are several randomised studies comparing unique procedures, operations reported in RCTs only once and not yet published in subsequent studies, such as comparing sphincterotomy with dermal flap advancement (Leong 1995), anterior levatorplasty to sphincterotomy (Ellis 2004), suture of the sphincterotomy site (Aysan 2004), removal of hypertrophied papillae (Gupta 2003), fissurectomy versus sphincterotomy (Wang 2005) .
The four included studies in this update prospectively randomised the patients to operative techniques. One of reports compared fissurectomy with sphincterotomy (Mousavi 2009). One report compared closed sphincterotomy with sphincterolysis (a digital restricted dilation that the author felt involved the rupture of a fibrous band) (Gupta 2008), whilst another compared lateral internal sphincterolysis with controlled intermittent anal dilatation (Yucel 2009). The fourth study compared unilateral internal sphincterotomy with bilateral sphincterotomy (Pujahari 2010).
These are added to the pre‐existing groupings from the previous review, which included anal stretch versus (open, closed, posterior) sphincterotomy, open versus closed lateral sphincterotomy, posterior midline versus lateral internal sphincterotomy, pneumatic balloon dilation versus sphincterotomy, sphincterotomy versus fissurectomy, and variance of the length of internal sphincter division from the length of the fissure to the level of the dentate line.
Complications reported sporadically included post‐operative wound pain, post‐operative bleeding, urinary retention, post‐operative sepsis, constipation, and peri‐anal haematoma. Again the focus of this review will be only on minor anal incontinence.
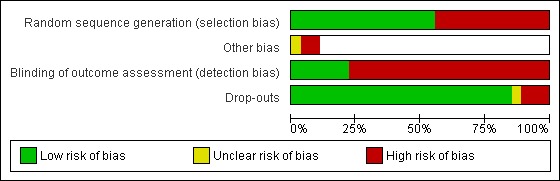
Risk of bias in included studies
The principal quality grading in this review was separation of reports in which patients were randomised to operative technique versus those reports which were retrospective reviews of experience with two or more techniques (Giebel 1989; Garcia 1996; Pernikoff 1994; Hoffman 1970; Abcarian 1980; Oueidat 1999; Collopy 1979; Bekheit 1974; Barisone 2004; Ektov 1986). Non‐randomized studies were excluded from the meta‐analysis.
Method of randomizations. In the original review, of the nine studies classified as randomised controlled trials an adequate method of randomizations was described in four: pulling classification cards once surgery had been determined to be necessary (Boulos 1984; Kortbeek 1992; Marby 1979); and use of a random number table (Fischer 1976). Randomization by hospital registration number (even or odd) is an inadequate technique (Jensen 1984; Weaver 1987); and insufficient or missing descriptions of the randomizations method were also deemed to confer a high risk of bias (Leong 1995; Olsen 1987; Saad 1992). In the five randomised trials of the first update, three specified an adequate randomizations method (Arroyo 2004; Gupta 2003; Wiley 2004), and the remaining two did not specify the method (Aysan 2004; Ellis 2004). In the nine randomised trials of the second update, five specified an adequate randomizations method (Filingeri 2005; Hancke 2003; Mentes 2005; Mentes 2008; Renzi 2007), two used inadequate methods such as hospital number (Elsebae 2007; Ram 2007) and in two the method was not stated (Kang 2008; Wang 2005). Of four new studies in this update, the randomisation method was adequate in three (Gupta 2008; Pujahari 2010; Yucel 2009) and not stated in one (Mousavi 2009).
Allocation concealment was assessed for each included study but was deemed either inadequate or insufficiently described in every case. Clearly the operating surgeon cannot be blinded to the operative procedure, but the problem is compounded when trial designers, patient case selectors, intervention implementers, and outcome assessors are the same people. Allocation concealment is not presented in the risk of bias tables or figures.
Outcome assessor blinding. Only six studies report that physicians examining patients for recurrence or complications were blinded as to the patient's operative classification (Filingeri 2005; Fischer 1976; Gupta 2003; Marby 1979; Mentes 2005; Wiley 2004).
Drop‐outs. Completeness of follow‐up is an additional quality measure: drop‐outs or losses to follow‐up should correctly be analysed as treatment failures; though a drop out rate of up to 10% has been regarded as acceptable in this review. Most studies have no drop‐outs at all (Arroyo 2004; Aysan 2004; Boulos 1984; Ellis 2004; Elsebae 2007; Fischer 1976; Gupta 2003; Hancke 2003; Jensen 1984; Kortbeek 1992; Leong 1995; Olsen 1987; Ram 2007; Saad 1992; Yucel 2009) or only a small number (Gupta 2008; Kang 2008; Mentes 2005; Mentes 2008; Pujahari 2010; Renzi 2007; Wang 2005; Wiley 2004). The drop‐out rate was high in three studies (Filingeri 2005; Marby 1979; Weaver 1987) and indeterminate in one (Mousavi 2009).
Length of follow‐up proved to be a major determinant of study quality in the Cochrane review of medical therapy for anal fissure (Nelson 2006), though healing of the fissure has in general been sustained after surgical sphincterotomy (Rotholtz 2005) when compared to medical therapy (Nelson 2006). In this review only two studies (Marby 1979; Weaver 1987) give cause for concern regarding the length of follow‐up. In (Marby 1979) only 31 of 156 patients were evaluated at 12 months; while in (Weaver 1987) a large percentage of patients could not have been followed‐up at 12 months because the paper was written too soon, although a 12 month endpoint was specified in the methods. A significant number of randomised patients were not followed long enough to attain the date at which endpoint determination was to have occurred according to the methods sections in these two repots. Follow‐up was to the specified endpoint date for all patients in other randomised studies, though this specified endpoint varied from report to report.
Among the randomised studies heterogeneity is detected in the combined analysis of anal stretch versus partial lateral internal sphincterotomy. The study by (Marby 1979) seems to be responsible for this, since removal of it from the meta‐analysis eliminates the heterogeneity. Scrutiny of this report reveals several problems. First is a 24% drop‐out rate. In addition the mean follow‐up time compared to the range of follow‐up times implies a significant skewing; with only 20% of patients being evaluated at 12 months and thus many patients being followed‐up for too little time to accurately determine the endpoints. Furthermore there is another variable inserted between the two groups besides operation and that is anaesthesia: the stretch group had general anaesthesia and the sphincterotomy group local anaesthesia. Other difficulties with this study relate to the indications for operation. The presenting symptom of fissure is, except in very unusual circumstances, anal pain on defecation, and all treatments are directed only toward pain relief (Goligher 1975). Yet 27% of patients in this series did not have pain as a presenting symptom. Also, for the sphincterotomy group to have worse outcome results than the stretch group implies that the sphincterotomies were not adequately performed in this study when compared to other reports. This is further demonstrated by the post‐operative manometric examinations reported by (Marby 1979). The cases in which healing of the fissure did not occur had significantly elevated sphincter pressure in 14 of 17 cases, denoting incomplete sphincterotomy. These same authors did a subsequent randomised trial (Weaver 1987), which had results that differed markedly from the first trial. The anaesthesia was now the same in both groups and perhaps the sphincterotomy was more complete, though this was not directly evaluated as it was in some other reports (Fischer 1976; Jensen 1984; Marby 1979; Olsen 1987). However significant problems with drop‐outs and follow‐up persist in this second report. The drop‐out rate was 14% and again looking at the mean and range of follow‐up, a large percentage of the patients could not have been seen at 12 months because the paper was written too soon, though this endpoint was specified in the methods. For all these reasons it is reasonable to consider analysis of the studies in the absence of the reports by (Marby 1979) and (Weaver 1987), when looking at anal stretch and sphincterotomy both in their effectiveness in curing anal fissure and in the risk of minor fecal incontinence after surgery.
The Graphic representation of Risk of bias is shown in the Figures (Figure 1; Figure 2)
1.
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
Summary of findings for the main comparison. Sensitivity Analysis; Stretch versus Sphincterotomy excluding Marby & Weaver for fissure in ano.
| Sensitivity Analysis; Stretch versus Sphincterotomy excluding Marby & Weaver for fissure in ano | ||||||
| Patient or population: patients with fissure in ano Settings: Intervention: Sensitivity Analysis; Stretch versus Sphincterotomy excluding Marby & Weaver | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Sensitivity Analysis; Stretch versus Sphincterotomy excluding Marby & Weaver | |||||
| Persistance of the Fissure | Study population | OR 4.42 (1.75 to 11.18) | 328 (5 studies) | ⊕⊕⊕⊝ moderate1 | ||
| 37 per 1000 | 145 per 1000 (63 to 300) | |||||
| Medium risk population | ||||||
| 33 per 1000 | 131 per 1000 (56 to 276) | |||||
| Minor incontinence to flatus | Study population | OR 5.73 (2.31 to 14.2) | 309 (5 studies) | ⊕⊕⊝⊝ low1,2 | ||
| 34 per 1000 | 168 per 1000 (75 to 333) | |||||
| Medium risk population | ||||||
| 38 per 1000 | 185 per 1000 (84 to 359) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 4 of the 5 studies included in this analysis had some level of selection and/or detection bias. 2 Incontinence assessment was variable among studies.
Summary of findings 2. Open versus closed partial lateral internal sphincterotomy for fissure in ano.
| Open versus closed partial lateral internal sphincterotomy for fissure in ano | ||||||
| Patient or population: patients with fissure in ano Settings: Intervention: Open versus closed partial lateral internal sphincterotomy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Open versus closed partial lateral internal sphincterotomy | |||||
| Persistence of the anal fissure | Study population | OR 1 (0.4 to 2.48) | 336 (5 studies) | ⊕⊕⊕⊕ high | ||
| 60 per 1000 | 60 per 1000 (25 to 137) | |||||
| Medium risk population | ||||||
| 35 per 1000 | 35 per 1000 (14 to 83) | |||||
| Minor incontinence to flatus | Study population | OR 0.87 (0.41 to 1.83) | 336 (5 studies) | ⊕⊕⊕⊝ moderate1 | ||
| 101 per 1000 | 89 per 1000 (44 to 171) | |||||
| Medium risk population | ||||||
| 86 per 1000 | 76 per 1000 (37 to 147) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Incontinence assessment variable among studies.
Seven randomised studies compared the efficacy of manual anal stretch to some form of internal sphincterotomy, comprising 385 subjects (Fischer 1976; Jensen 1984; Olsen 1987; Marby 1979; Saad 1992; Weaver 1987; Ram 2007) . The Peto Odds Ratio for all seven studies looking at persistence of the fissure is 1.55 (favouring sphincterotomy), 95% confidence interval 0.85‐2.86. All these reports also looked at minor or flatus incontinence as a complication of each procedure. The Peto Odds Ratio and 95% confidence intervals are 4.03, 2.04‐7.46 (favouring sphincterotomy). Significant heterogeneity was detected in the analysis of efficacy in Metaview (p=0.03, I2=58%). When two studies were deleted from the Metaview analysis (for reasons discussed below (Marby 1979; Weaver 1987) the heterogeneity disappeared (p=0.51, I2= 0%), and the overall effect for efficacy became significant, favouring sphincterotomy (OR = 3.35, 95% CI = 1.55‐7.26). There was no heterogeneity detected in the analysis of minor incontinence (p=0.17, I2=0%, 95% CI = 0‐74%) with or without the above two studies.
Five randomised studies compared open partial lateral internal sphincterotomy to closed or subcutaneous partial lateral internal sphincterotomy (Boulos 1984; Kortbeek 1992; Arroyo 2004; Wiley 2004;Filingeri 2005), comprised of 299 subjects. The same two endpoints were assessed: persistence of the fissure and partial or flatus incontinence. The Peto Odds Ratio for fissure persistence is 1.00 (0.4 ‐ 2.48) and for flatus incontinence is 0.87 (0.41 ‐ 1.83) (favouring closed sphincterotomy). No statistical heterogeneity is seen (P= 0.82, I2=0, 0‐0%; 0.93, I2=0, 0‐11%). Obviously neither result is statistically significant.
Four reports have at last looked at how the sphincter is actually divided, two comparing lateral sphincterotomy extending cephalad either to the base of the fissure, or somewhat longer, to the dentate line (Elsebae 2007;Mentes 2005). The third compared sphincter division to the level of the base of the fissure, or to achieve a specific aperture of the anal canal: 30 mm (Mentes 2008). Though not the same as division to the dentate line, this was included in that randomizations category assuming, based upon this reviewer's experience, that achieving this aperture would require a slightly more extensive sphincterotomy than just to the base of the fissure. The longer sphincterotomy was associated with a significantly lower risk of treatment failure (0.15, 0.03‐0.69) in a combined analysis. Incontinence was scored on a Wexner scale and found not to be significantly different between the two groups (‐0.10, ‐0.34 ‐ 0.14), reported only in the two Mentes reports (Mentes 2005; Mentes 2008). In any case these scores represent quite a low risk of incontinence. Thus sphincter division to the dentate line or to achieve an aperture of 30 mm appears to be the most efficacious procedure. Statistical heterogeneity was not present in either analysis (for efficacy, p=0.85, I2=0, 0‐0). For bilateral sphincterotomy, see below.
One report randomised patients either to sphincterotomy or dermal flap coverage of the anal fissure (Leong 1995). Three strata of outcome were reported from dissatisfied to satisfied to excellent. The outcome was generally better in the flap group (though not significantly so (p=0.23 by chi square). However the only recurrences developed in the flap group, in 3 of twenty patients. Incontinence was not seen in either group.
One report assessed the efficacy of anterior levatorplasty in the treatment of anterior fissure in women who also had rectocoele, postulating a completely different pathophysiology for a fissure in this position, and compared it in a RTC to the gold standard procedure, lateral internal sphincterotomy (Ellis 2004). 54 subjects participated in the trial, 25 randomised to sphincterotomy and 29 to levatorplasty. Fissure healing occurred in all patients except one (sphincteroplasty), showing no significant difference between procedures, with continence and pain scores that also did not differ.
Surgical adjuncts to sphincterotomy have also been studied in RCTs, hoping to hasten pain relief. In the first, anal papillae were excised during sphincterotomy, or left in situ and patients followed up to 27 months in 140 subjects, 70 in each group. Satisfaction was increased in those having papillae excision (p=0.001) (Gupta 2003). In another study, after sphincterotomy, 39 subjects were randomised either to have the anal wound dressed open (n=17) or sutured shut (n=22), hoping to hasten wound healing. This has been avoided in the past, fearing the high likelihood of surgical wound infection. However paradoxically wound infection was rare in the sutured group (1 of 22) and in 4 of 17 in the open group., and wound healing was more than twice as fast (15.05 days versus 33.94 days, p<0.001) (Aysan 2004). Total wound complications occurred in 9/22 in the sutured group and 9/17 of the open group. A second study looked at partial versus no suturing of the lateral internal sphincterotomy incision (Kang 2008) and also found more wound complications when the sphincterotomy wound is left open (7/45 versus 1/45 in a partially closed wound). In the combined analysis the advantage of closure approached significance (0.35, 0.13‐1.00). As the sphincterotomy was the same in all cases the fissure healing and incontinence risk were no different in the (Kang 2008) study.
One report looked at a method of anal dilation using a pneumatic balloon rather than manual dilation (Renzi 2007), analysed separately as the final aperture achieved is smaller with the balloon. When compared to open sphincterotomy there was no significant difference in fissure healing (1.47, 0.29‐7.37) or incontinence risk (0.1, 0.0‐1.91) among 49 participants, though the trend was towards less incontinence with balloon dilation, just the opposite of what was found with manual dilation.
One report looked at combining methods of sphincter release, performing anal dilation on all participants, but adding sphincterotomy to those randomised to combined procedures (Hancke 2003). There were insignificant trends toward the combined procedure in preventing treatment failure (OR=1.45. CI=0.44‐4.86) and towards dilation alone in preventing wound complications (0.50, 0.11‐2.23), in a study of 60 patients with chronic fissure. A long term follow up of these patients was recently published in this review but not included, as 40% of the participants were lost to follow up (Hancke 2009).
One report compared what appeared to be a sphincterotomy with fissurectomy (Wang 2005). The author was very helpful in embellishing the surgical aspects of the Chinese published article. Sphincterotomy was less likely to result in treatment failure among 50 randomised participants (10.76, 1.31‐88.47).
(Saad 1992) assessed three procedures in a randomised trial, two of which were posterior (n=21) and lateral (n=20) sphincterotomy, (the third being anal stretch, n=37), the only study to randomized to these two procedures and the results demonstrated little difference between these two procedures both in efficacy (no recurrence in the posterior sphincterotomy and one in the lateral, p=0.964) and incontinence (two incontinence in the posterior sphincterotomy and one in the lateral, p=0.994).
Among the studies added in this update: One study was added to the category which compared fissurectomy with sphincterotomy, comprising a total of 162 patients (Wang 2005, Mousavi 2009). Both studies showed that sphincterotomy was significantly less likely to result in treatment failure among 162 randomised participants, compared to fissurectomy (8.07 [1.42, 45.84]). Only Mousavi 2009 used incontinence as an outcome measure, with a total of 62 randomised participants. There was an insignificant difference between sphincterotomy and fissurectomy regarding incontinence risk, although the trend was towards control.
A novel variant on sphincterotomy was explored by Pujahari 2010, who compared unilateral internal sphincterotomy to bilateral internal sphincterotomy. In 219 participants, bilateral internal sphincterotomy was significantly less likely to result in treatment failure. (6.91 [1.97, 24.22]). For incontinence, however, there was no significant difference between the two interventions, though the trend favoured the control.
A new comparison was created between closed sphincterotomy and sphincterolysis (Gupta 2008). There was no significant difference in treatment failure (1.71 [0.38, 7.66]) or incontinence risk (3.00 [0.12, 75.74]) among the 85 participants.
One report looked at controlled anal dilatation compared to lateral internal sphincterotomy (Yucel 2009). There were no significant trends towards either intervention in preventing treatment failure (0.63 [0.9, 4.24]) in a study of 40 patients with chronic fissures. As there were no cases of incontinence in either operative technique, there is no significant difference between the interventions regarding the effect on incontinence.
Discussion
A total of thirteen operative techniques are included in the review:
Full anal stretch (that is a stretch using 6 or more fingers)
open lateral internal sphincterotomy,
closed lateral internal sphincterotomy,
pneumatic balloon dilation of the anal canal,
fissurectomy,
papilla resection,
sphincterotomy wound closure,
anterior levatorplasty,
flap coverage of the fissure
posterior midline sphincterotomy
bilateral sphincterotomy
sphincterotolysis
controlled anal dilation
In addition, length of sphincterotomy has varied in some studies, and a new instrument, radio frequency bistoury, used to do an closed versus open sphincterotomy (Filingeri 2005) and two major endpoints of these procedures ascertained: fissure persistence and incontinence to flatus, as well as a minor endpoint: sphincterotomy wound healing.
Of the procedures, anal stretch, open sphincterotomy, closed sphincterotomy, sphincterotomy length and sphincterotomy wound closure have been reported more than once and so can be subjected to combined analyses.
Unlike pharmacologic clinical trials, the exposure variable in surgical trials, such as the technique of sphincterotomy, may vary considerably, not just in radial location and incision size, but in depth as well. This variation may be due to variable patient anatomy, anaesthetic techniques, surgical experience and other factors. The conclusions regarding stretch are therefore valid, particularly since stretch is being compared to all forms of sphincterotomy, and not necessarily to a "gold standard" sphincterotomy. Thus differences between anal stretch and sphincterotomy are probably underestimated. It should be noted that as the "Full" manual anal stretch has fallen out of favour, the incidence of even minor incontinence has fallen considerably among the RCTs reported, especially in the last two updates of this review, not exceeding 5% in any study arm, except in (Renzi 2007), and usually less, even for traditional or control arms such as lateral internal sphincterotomy.
Manual anal stretch has a higher risk of fissure persistence than internal sphincterotomy and also a significantly higher risk of minor incontinence than sphincterotomy. The recent report of the benefit of balloon dilation, which is done to a smaller aperture (3.0 cm) and more gradually than manual anal stretch, are encouraging, (Renzi 2005), and a subsequent RCT supports this finding (Renzi 2007). The combined results of open versus closed partial lateral internal sphincterotomy show little difference between the two procedures both in fissure persistence and risk of incontinence
Of the operative techniques included in this update of the review, controlled intermittent anal dilatation, sphincterolysis and bilateral internal sphincterotomy are procedures previously unseen in literature. When grouping these interventions, however, we encountered problems when determining which categories sphincterolysis (Gupta 2008) and controlled anal dilatation Yucel 2009 should fall into, being rather more refined and restrained than the older "Full" or manual dilation. Sphincterolysis is the process of fragmenting the internal sphincter fibres with the finger. A finger is inserted along the left lateral side of the anal canal, and by means of delicate, but firm pressure, fibres were fractured. Controlled intermittent anal dilatation is performed under general anaesthesia. An anal speculum is placed into the anal canal, and slowly dilated to a diameter of 4.8cm. Over the next 20 seconds, the speculum is relaxed, and this sequence is repeated 15 times over a 5 minute period. Although both techniques could be thought of as variants of the anal stretch method, we decided to create new groups for both interventions, as they are fundamentally new techniques.
The four studies added to this review have not affected the conclusions from the prior review. The technique of bilateral internal sphincterolysis may gain popularity in the future as it has a better treatment success when compared to unilateral internal sphincterolysis, but further research must be undertaken in this field. The best method of anal dilation has yet to be determined, as the three techniques described in this review are so far only presented in single reports, and in each case compared only to sphincterotomy.
Authors' conclusions
Implications for practice.
Manual anal stretch should probably be abandoned in the treatment of chronic anal fissure in adults. For those patients requiring surgery for anal fissure, open and closed partial lateral internal sphincterotomy appear to be equally efficacious. It is less clear whether posterior sphincterotomy should be performed as the primary treatment of anal fissure. For the greatest chance of cure, the sphincterotomy should be performed to the level of the dentate line or to achieve an anal canal aperture of 30 mm. This rigorous measure of sphincterotomy appears to be associated with a diminished risk of incontinence when compared to previous reports. Pneumatic balloon dilation to roughly this aperture may prove a method of dilation that is safer than manual dilation and as efficacious as sphincterotomy.
Implications for research.
The treatment choices for chronic anal fissure in adults are rapidly expanding, as medical alternatives to surgery are examined. The appropriate choice of the "gold standard" procedure for fissure treatment is key to the evaluation of any new therapy in clinical trials. Since there is not yet any established standard of non‐surgical therapy, partial lateral internal sphincterotomy (open or closed) should be the standard therapy control in such studies. More randomised trials of posterior sphincterotomy compared to lateral sphincterotomy, and bilateral sphincterotomy compared to unilateral sphincterotomy are needed to resolve efficacy as well as whether dermal flap coverage of the fissure should be considered as an alternative to sphincterotomy. The issue of incontinence after fissure therapy lingers, with some very high rates being reported in the past. The incidence of this is very dependant on the ascertainment method (Casillas 2004). Yet paradoxically patient satisfaction with surgical therapy remains very high (Hyman 2004; Mentes 2006). This paradoxical disparity is the greatest research issue related to fissure and benign anorectal disease in general. At least one author posits that it could be resolved by more rigorous pre‐surgical continence assessment (Ammari 2004).
What's new
| Date | Event | Description |
|---|---|---|
| 28 September 2011 | New search has been performed | New searches performed and new RCT's included in this version. Conclusions remain the same |
| 28 September 2011 | New citation required but conclusions have not changed | New searches performed and new RCT's included in this version. Conclusions remain the same |
History
Protocol first published: Issue 3, 2000 Review first published: Issue 3, 2001
| Date | Event | Description |
|---|---|---|
| 15 June 2011 | New search has been performed | New RCT's added this update, conclusions remain the same as previous version. |
| 26 January 2009 | New citation required and conclusions have changed | This version is the third update of the review, first published in 2001 issue 3 |
| 15 July 2008 | New citation required but conclusions have not changed | Substantive amendment |
| 15 July 2008 | New search has been performed | Converted to new review format. |
Notes
This update include 4 new trials
Acknowledgements
none
Data and analyses
Comparison 1. Anal Stretch and partial internal sphincterotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Persistence of the anal fissure | 7 | 493 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.55 [0.85, 2.86] |
| 2 Minor incontinence to flatus | 7 | 493 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 4.03 [2.04, 7.96] |
1.1. Analysis.

Comparison 1 Anal Stretch and partial internal sphincterotomy, Outcome 1 Persistence of the anal fissure.
1.2. Analysis.

Comparison 1 Anal Stretch and partial internal sphincterotomy, Outcome 2 Minor incontinence to flatus.
Comparison 2. Open versus closed partial lateral internal sphincterotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Persistence of the anal fissure | 5 | 336 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.00 [0.40, 2.48] |
| 2 Minor incontinence to flatus | 5 | 336 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.87 [0.41, 1.83] |
2.1. Analysis.
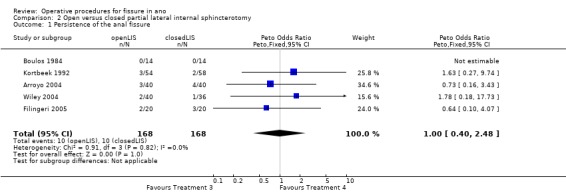
Comparison 2 Open versus closed partial lateral internal sphincterotomy, Outcome 1 Persistence of the anal fissure.
2.2. Analysis.

Comparison 2 Open versus closed partial lateral internal sphincterotomy, Outcome 2 Minor incontinence to flatus.
Comparison 3. Length of Sphincterotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Treatment Failure | 3 | 228 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.03, 0.69] |
| 2 Anal Incontinence Score | 3 | 138 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.34, 0.14] |
3.1. Analysis.
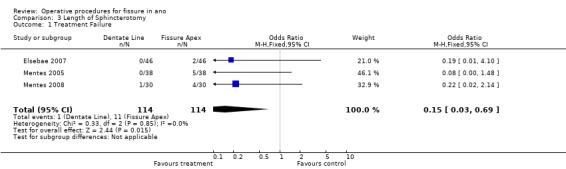
Comparison 3 Length of Sphincterotomy, Outcome 1 Treatment Failure.
3.2. Analysis.

Comparison 3 Length of Sphincterotomy, Outcome 2 Anal Incontinence Score.
Comparison 4. Pneumatic Balloon Dilation versus LIS.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Treatment Failure | 1 | 49 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.29, 7.37] |
| 2 Persistant Anal Incontinence | 1 | 49 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.00, 1.92] |
4.1. Analysis.
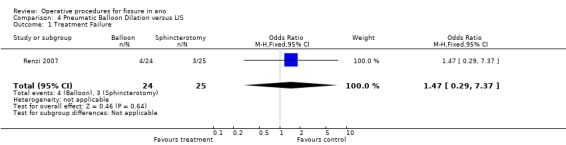
Comparison 4 Pneumatic Balloon Dilation versus LIS, Outcome 1 Treatment Failure.
4.2. Analysis.
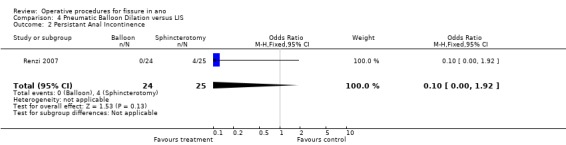
Comparison 4 Pneumatic Balloon Dilation versus LIS, Outcome 2 Persistant Anal Incontinence.
Comparison 5. Fissurectomy vs. Sphincterotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Treatment Failure | 2 | 162 | Odds Ratio (M‐H, Fixed, 95% CI) | 8.07 [1.42, 45.84] |
| 2 Incontinence | 1 | 62 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.70 [0.26, 123.78] |
5.1. Analysis.

Comparison 5 Fissurectomy vs. Sphincterotomy, Outcome 1 Treatment Failure.
5.2. Analysis.

Comparison 5 Fissurectomy vs. Sphincterotomy, Outcome 2 Incontinence.
Comparison 6. Partial wound closure versus no closure in LIS.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Treatment failure | 1 | 90 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.10, 4.10] |
| 2 Incontinence | 1 | 90 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Total Wound Complications | 2 | 129 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.13, 1.00] |
6.1. Analysis.

Comparison 6 Partial wound closure versus no closure in LIS, Outcome 1 Treatment failure.
6.2. Analysis.
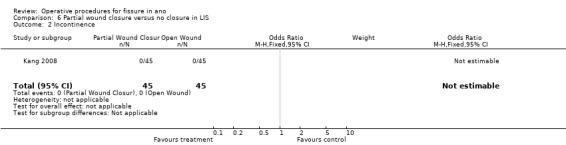
Comparison 6 Partial wound closure versus no closure in LIS, Outcome 2 Incontinence.
6.3. Analysis.
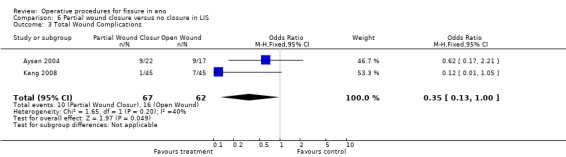
Comparison 6 Partial wound closure versus no closure in LIS, Outcome 3 Total Wound Complications.
Comparison 7. Unilateral Internal Sphincterotomy (UIS) vs. Bilateral Internal Sphincterotomy (BIS).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Treatment failure | 1 | 219 | Odds Ratio (M‐H, Fixed, 95% CI) | 6.91 [1.97, 24.22] |
| 2 Incontinence | 1 | 219 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.36, 11.26] |
7.1. Analysis.
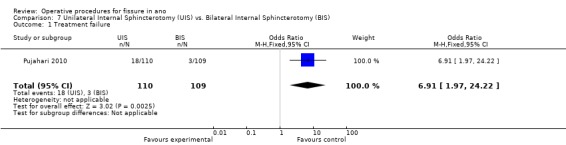
Comparison 7 Unilateral Internal Sphincterotomy (UIS) vs. Bilateral Internal Sphincterotomy (BIS), Outcome 1 Treatment failure.
7.2. Analysis.

Comparison 7 Unilateral Internal Sphincterotomy (UIS) vs. Bilateral Internal Sphincterotomy (BIS), Outcome 2 Incontinence.
Comparison 8. Closed Sphincterotomy vs. Sphincterolysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Treatment failure | 1 | 85 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.71 [0.38, 7.66] |
| 2 Incontinence | 1 | 85 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.00 [0.12, 75.74] |
8.1. Analysis.

Comparison 8 Closed Sphincterotomy vs. Sphincterolysis, Outcome 1 Treatment failure.
8.2. Analysis.

Comparison 8 Closed Sphincterotomy vs. Sphincterolysis, Outcome 2 Incontinence.
Comparison 9. Controlled‐Intermittent Anal Dilatation (CIAD) vs. Lateral Internal Sphincterotomy (LIS).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Treatment failure | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.09, 4.24] |
| 2 Incontinence | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
9.1. Analysis.

Comparison 9 Controlled‐Intermittent Anal Dilatation (CIAD) vs. Lateral Internal Sphincterotomy (LIS), Outcome 1 Treatment failure.
9.2. Analysis.

Comparison 9 Controlled‐Intermittent Anal Dilatation (CIAD) vs. Lateral Internal Sphincterotomy (LIS), Outcome 2 Incontinence.
Comparison 10. Sensitivity Analysis; Stretch versus Sphincterotomy excluding Marby & Weaver.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Persistance of the Fissure | 5 | 328 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.42 [1.75, 11.18] |
| 2 Minor incontinence to flatus | 5 | 309 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.73 [2.31, 14.20] |
10.1. Analysis.

Comparison 10 Sensitivity Analysis; Stretch versus Sphincterotomy excluding Marby & Weaver, Outcome 1 Persistance of the Fissure.
10.2. Analysis.
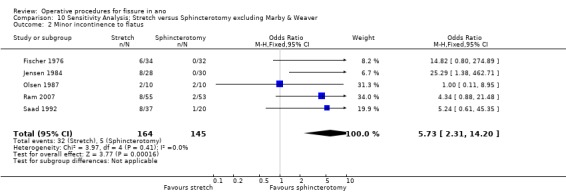
Comparison 10 Sensitivity Analysis; Stretch versus Sphincterotomy excluding Marby & Weaver, Outcome 2 Minor incontinence to flatus.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Arroyo 2004.
| Methods | Randomized Controlled Trial | |
| Participants | Chronic anal fissure | |
| Interventions | Open (40) versus "closed" (40) lateral internal sphincterotomy under local anaesthesia | |
| Outcomes | Persistance, recurrence, healing up to 2 years and manometry pre‐operative, and at each f/u: 20 days, 6 months, 1 year, 2 years Continence assessment by Wexner score | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | adequate |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | not stated |
| Drop‐outs All outcomes | Low risk | zero |
Aysan 2004.
| Methods | Randomized Controlled Trial | |
| Participants | Patients with chronic fissure | |
| Interventions | After Sphincterotomy, primary wound closure versus open b\packing | |
| Outcomes | Wound infection, wound healing time, bleeding | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | randomisation method not specified |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | not stated |
| Drop‐outs All outcomes | Low risk | zero |
Boulos 1984.
| Methods | Randomized controlled trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Open (14) versus subcutaneous (14) partial lateral internal sphincterotomy | |
| Outcomes | Persistence of the fissure and incontinence to flatus | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | pulling classification cards once surgery had been determined to be necessary |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | zero |
Ellis 2004.
| Methods | Randomized controlled trial | |
| Participants | 54 Women with anterior chronic fissure and rectocoele | |
| Interventions | Anterior perineoplasty versus sphincterotomy | |
| Outcomes | Pain score, healing, continence score, manometry pre‐ and post operative, patient satisfaction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | randomisation method not specified |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | zero |
Elsebae 2007.
| Methods | RCT | |
| Participants | Patients with Chronic anal fissure | |
| Interventions | Lateral internal sphincterotomy either to the dentate line or the apex of the fissure in 92 patients | |
| Outcomes | Healing at 4 and 18 weeks. timing of continence assessment was uncertain | |
| Notes | Among 61 women, 21 had anterior fissures, 6 had multiple fissure. Among 47 men, there were 6 with anterior fissures and 9 with multiple fissures. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | inadequate |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | zero |
Filingeri 2005.
| Methods | RCT | |
| Participants | CAF | |
| Interventions | Open (20) vs. Closed using RFA (20) internal sphincterotomy | |
| Outcomes | Healing | |
| Notes | 5 drop outs not analysed as ITT All healed at 30 d | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | specified and adequate randomisation method |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | adequate |
| Drop‐outs All outcomes | High risk | 5/40 = 12.5% |
Fischer 1976.
| Methods | Randomized controlled trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Anal stretch (34) versus lateral subcutaneous sphincterotomy (32) | |
| Outcomes | Persistence of the fissure and incontinence to flatus | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | random number table |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | physicians examining for recurrence or complications were blinded to patient operative classification |
| Drop‐outs All outcomes | Low risk | zero |
Gupta 2003.
| Methods | Randomized controlled trial | |
| Participants | Patients with chronic fissure and anal papilae | |
| Interventions | Sphincterotomy plus or minus excision of associated anal papillae | |
| Outcomes | Satisfaction score, wound related symptoms | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | adequate |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | physicians examining for recurrence / complications were blinded to patient operative classification |
| Drop‐outs All outcomes | Low risk | zero |
Gupta 2008.
| Methods | Randomised Controlled Trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Closed sphincterotomy (43) versus Sphincterolysis (42) | |
| Outcomes | Incontinence, fissure healing | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | adequate |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | 4/85 = 4.7% |
Hancke 2003.
| Methods | RCT | |
| Participants | CAF | |
| Interventions | Anal dilation, fissure excision plus or minus sphincterotomy | |
| Outcomes | healing at 3 months of the fissure and post‐operative flatus incontinence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | specified and adequate randomisation method |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | zero |
Jensen 1984.
| Methods | Randomized controlled trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Anal stretch (28) versus lateral subcutaneous sphincterotomy (30) | |
| Outcomes | Persistence of the fissure and incontinence to flatus | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | randomisation by hospital registration number ‐ inadequate |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | zero |
Kang 2008.
| Methods | RCT | |
| Participants | CAF | |
| Interventions | Open LIS followed by partial skin suture or leaving entirely open n=90; 45@ | |
| Outcomes | Pain, wound healing, incontinence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | randomisation method not specified |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | 4/90 = 4.4% |
Kortbeek 1992.
| Methods | Randomized controlled trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Open (54) versus closed (58) partial lateral internal anal sphincterotomy | |
| Outcomes | Persistence of the fissure and incontinence to flatus Open sphincterotomy Persistence risk = 0.06; incontinence risk = 0.07 Closed sphincterotomy persistence risk = 0.03; incontinence risk = 0.09 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | pulling classification cards once surgery had been determined to be necessary |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | zero |
Leong 1995.
| Methods | Randomized controlled trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Dermal flap advancement versus sphincterotomy | |
| Outcomes | Satisfaction, recurrence and incontinence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | specified method ‐ inadequate |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | zero |
Marby 1979.
| Methods | Randomized controlled trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Anal stretch (78) versus lateral subcutaneous sphincterotomy | |
| Outcomes | Persistence of the fissure | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | pulling classification cards once surgery had been determined to be necessary |
| Other bias | High risk | ‐ insufficient length of follow‐up: only 31 of 156 patients evaluated at 12 months ‐ confounding variable: different anaesthetic for different surgical groups ‐ selection criteria: 27% of patients did not present with anal pain on defecation ‐ also, cases in which healing of the fissure did not occur had significantly elevated sphincter pressure in 14 of 17 cases, denoting incomplete sphincterotomy |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | physicians examining for recurrence / complications were blinded to patient operative classification |
| Drop‐outs All outcomes | High risk | drop out rate 24% |
Mentes 2005.
| Methods | RCT | |
| Participants | CAF | |
| Interventions | Length of sphincter division: to the apex of the fissure or dentate line | |
| Outcomes | pain scores, manometry and anal incontinence scores. Fissure healing at 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | specified and adequate randomisation method |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | adequate |
| Drop‐outs All outcomes | Low risk | 4/80 = 5% |
Mentes 2008.
| Methods | RCT | |
| Participants | CAF | |
| Interventions | Length of sphincter division: to apex or to achieve 30 mm aperture | |
| Outcomes | healing of the fissure, incontinence score, aperture size over time. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | specified and adequate randomisation method |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | 3/61 = 4.9% |
Mousavi 2009.
| Methods | Randomised Controlled Trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Fissurectomy (30) versus Lateral internal sphincterotomy (32) | |
| Outcomes | Persistence of pain/bleeding, fissure recurrence, major and minor incontinence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | not stated |
| Other bias | Unclear risk | not stated if groups are comparable at baseline |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Unclear risk | indeterminate |
Olsen 1987.
| Methods | Randomized controlled trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Anal stretch (10) versus lateral subcutaneous internal sphincterotomy (10) | |
| Outcomes | Persistence of the fissure and incontinence to flatus Anal stretch persistence risk = 0.30; incontinence risk = 0.20 Sphincterotomy persistence risk = 0.10; incontinence risk = 0.20 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | inadequate |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | zero |
Pujahari 2010.
| Methods | Randomised Controlled Trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Unilateral internal sphincterotomy (110) versus Bilateral internal sphincterotomy (109) | |
| Outcomes | Major and minor incontinence, fissure recurrence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | sealed envelopes |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | not stated |
| Drop‐outs All outcomes | Low risk | 8/219 = 3.7% |
Ram 2007.
| Methods | RCT | |
| Participants | 108 Patients with Chronic anal fissure | |
| Interventions | 4 finger Anal dilation or left lateral internal sphincterotomy | |
| Outcomes | Healing (or recurrence), satisfaction or minor incontinence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | randomisation by hospital registration number ‐ inadequate |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | zero |
Renzi 2007.
| Methods | RCT | |
| Participants | CAF | |
| Interventions | Pneumatic balloon dilation vs. closed LIS | |
| Outcomes | ultrasound, manometry, pain and continence scores, persistence and recurrence of the fissure at 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | specified and adequate randomisation method |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | 4/49 = 8.2% |
Saad 1992.
| Methods | Randomized controlled trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Anal stretch (37) versus lateral sphincterotomy (20) versus midline sphincterotomy (21) | |
| Outcomes | Persistence of the fissure and incontinence to flatus Anal stretch persistence risk = 0.08, incontinence risk 0.24. Lateral sphincterotomy persistence risk = 0.05; incontinence risk = 0.05 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | inadequate |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | zero |
Wang 2005.
| Methods | RCT | |
| Participants | Patients with chronic anal fissure who had failed conservative management | |
| Interventions | PML Sphincterotomy (50) vs. Fissurectomy and ?Pectinotomy? (50). | |
| Outcomes | Healing time and "success" rate | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | randomisation method not specified |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | Low risk | 10/100 = 10% (borderline) |
Weaver 1987.
| Methods | Randomized controlled trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Anal stretch (59) versus lateral subcutaneous internal sphincterotomy (39) | |
| Outcomes | Persistence of the fissure and major incontinence Anal stretch persistence risk = 0.05; incontinence risk = NS Sphincterotomy persistence risk = 0.05; minor incontinence risk = NS | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | randomisation by hospital registration number ‐ inadequate |
| Other bias | High risk | insufficient length of follow‐up |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | inadequate |
| Drop‐outs All outcomes | High risk | drop out rate 14% |
Wiley 2004.
| Methods | Randomized controlled trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Open (41) versus closed (38) sphincterotomy | |
| Outcomes | Persistence of the fissure, continence scores, pain scores, complications | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | adequate |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | adequate |
| Drop‐outs All outcomes | Low risk | 3/80 = 3.8% |
Yucel 2009.
| Methods | Randomised Controlled Trial | |
| Participants | Patients with chronic anal fissure | |
| Interventions | Controlled‐intermittent anal dilation (20) versus Lateral internal sphincterotomy (20) | |
| Outcomes | Fissure healing, pain, bleeding | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | sealed envelopes |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | not stated |
| Drop‐outs All outcomes | Low risk | zero |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abcarian 1980 | non randomised study, LIS vs PMS |
| AlRaymoony 2001 | RCT of anaesthetic technique but measured outcome neither cure nor incontinence |
| Barisone 2004 | non‐randomized study, LIS vs PMS |
| Bekheit 1974 | non‐randomized study, AS vs. LIS vs PMS |
| Bouchard 2010 | Randomisation information unclear as only abstract available at present. |
| Cho 2005 | non‐randomized study of "controlled sphincterotomy vs. LIS |
| Collopy 1979 | non‐randomized study of AS vs. sphincterotomy |
| Ektov 1986 | non‐randomized study of open vs. closed sphincterotomy |
| Garcia 1996 | non‐randomized study of open vs. closed sphincterotomy |
| Giebel 1989 | non‐randomized study of AS vs.LIS |
| Gupta 2007 | RCT of post‐operative sitz bath for chronic fissure with identical operations performed in both groups |
| Gupta2006 | RCT of Acute Fissure. No surgery performed |
| Hancke 2009 | Excessive dropout rate (40% from the 2003 included study to this one) |
| Hawley 1969 | Randomization routinely broken at surgeons discretion in a study of AS vs. LIS vs. PMS |
| Hoffman 1970 | non‐randomized study of AS vs. LIS vs. PMS |
| Lewis 1988 | non‐randomized study of open versus closed sphincterotomy |
| Oueidat 1999 | non‐randomized study of AS vs. LIS vs. PMS |
| Pernikoff 1994 | non‐randomized study of open versus closed sphincterotomy |
Contributions of authors
RLN is the sole author of all previous versions of this review, where all aspects of the review were performed by RLN.
This update was prepared by RLN with the collaboration of the other named authors, students at the University of Sheffield School of Medicine as part of the Master Class Symposium. Each author participated in study identification, data abstraction and final conclusions. SE was responsible for Sumary of Findings. WB, risk of bias. IP data entry and analysis. AC & TP Text updating. RLN supervised and finished.
Sources of support
Internal sources
none, Not specified.
External sources
none, Not specified.
Declarations of interest
None known
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Arroyo 2004 {published data only}
- Arroyo A, Perez F, Seerrano P, Candela F, Calpena R. Open versus closed lateral sphincterotomy performed as an outpatient procedure under local anesthesia for chronic anal fissure: prospective randomized study of clinical and manometric results. J. Am Coll. Surg. 2004;199:361‐367. [DOI] [PubMed] [Google Scholar]
Aysan 2004 {published data only}
- Aysan E, Aren A, Ayar E. Lateral internal sphincterotomy incision: suture or not? A prospective randomized controlled trila. Am Surg. 2004;187:291‐294. [DOI] [PubMed] [Google Scholar]
Boulos 1984 {published data only}
- Boulos PB, Araujo JG. Adequate internal sphincterotomy for chronic anal fissure: subcutaneous or open technique? Br J Surg. Br J Surg 1984;71:360‐362. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ellis 2004 {published data only}
- Ellis CN. Anterior levatorplasty for the treatment of chronic anal fissures in females with a rectocele: a randomized controlled trial. Dis. Colon & Rectum 2004;47:1170‐1173. [DOI] [PubMed] [Google Scholar]
Elsebae 2007 {published data only}
- Elsebae MA. A study of fecal incontinence in patients with chronic anal fissure: prospective, randomized, controlled trial of the extent of internal anal sphincter division during lateral sphincterotomy. World J Surg 2007;31:2052‐57. [DOI] [PubMed] [Google Scholar]
Filingeri 2005 {published data only}
- Filingeri V, Gravante G. A prospective randomized trial between subcutaneous lateral internal sphincterotomy with radiofrequency bistoury and conventional Parks' operation in the treatment of anal fissure. Eur. Rev for Med. and Pahrmacol. Sciences 2005;9(3):175‐8. [PubMed] [Google Scholar]
Fischer 1976 {published data only}
- Fischer M, Thermann M, Trobisch M, Sturm R, Hamelmann H. Treatment of primary‐chronic anal fissure through anal stretch or sphincterotomy [Die Behandlung der primar‐chronischen analfissur durch dehnung des analkanales oder sphincterotomie]. Langenbeck's Arch Chir 1976;343:35‐44. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gupta 2003 {published data only}
- Gupta PJ, Kalaskar S. Removal of hypertrophied anal papillae and fibrous anal polyps increases patients satisfaction after anal fissure surgery. Tech Coloproctology 2003;7:155‐158. [DOI] [PubMed] [Google Scholar]
Gupta 2008 {published and unpublished data}
- Gupta PJ, Kalaskar S, Heda P. Closed lateral internal sphincterotomy versus anal sphincterolysis for chronic anal fissure. Coloproctology 2008;30:242‐8. [Google Scholar]
Hancke 2003 {published data only}
- Hancke E, Schwaner S. Chronische Analfissur ‐ operative behandlung mit analdilatation, excision der analfissure versus laterale sphinkterotomie [Chronische Anafissur ‐ oerative behandlung mit analdilatation, excision der analfissure versus laterale sphinkterotomie]. Coloproctology 2003;25:95‐105. [Google Scholar]
Jensen 1984 {published data only}
- Jensen SL, Lund F, Nielsen OV, Tange G. Lateral subcutaneous sphincterotomy versus anal dilatation in the treatment of fissure in ano in outpatients: a prospective randomized study. Br Med J. Br Med J 1984;289:528‐530. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kang 2008 {published data only}
- Kang GS, Kim BS, Choi PS, Kang DW. Evaluation of healing and complications after lateral internal sphincterotomy for chronic anal fissure: marginal suture of the incision vs. open left incision: prospective, randomized, controlled study. Dis. Colon & Rectum 2008;51:329‐33. [DOI] [PubMed] [Google Scholar]
Kortbeek 1992 {published data only}
- Kortbeek JB, Langevin JM, Khoo RE, Heine JA. Chronic fissure‐in‐ano: a randomized study comparing open and subcutaneous lateral internal sphincterotomy. Dis. Colon & Rectum. Dis Colon Rectum 1992;35:835‐837. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Leong 1995 {published data only}
- Leong AF, Seow‐Choen F. Lateral sphincterotomy compared with anal advancement flap for chronic anal fissure.. Dis Colon Rectum 1995;38:69‐71. [MEDLINE: ; 95112698 UI] [DOI] [PubMed] [Google Scholar]
Marby 1979 {published data only}
- Marby M, Alexander‐Williams J, Buchman P, Arabi Y, Kappas A, Minervini S, Gatehouse D, Keighley MR. A randomized controlled trial to compare anal dilatation with lateral subcutaneous sphincterotomy for anal fissure. Dis Colon & Rectum. Dis Colon Rectum 1979;22:308‐311. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mentes 2005 {published data only}
- Mentes BB, Ege B, Leventoglu S, Oguz M, Karadag A. Extent of lateral internal sphincterotomy: up to the dentate line or up to the fissure apex. Dis. Colon & Rectum 2005;48:365‐70. [DOI] [PubMed] [Google Scholar]
Mentes 2008 {published data only}
- Mentes BB, Guener MK, Leventoglu S, Akyuerek N. Fine tuning of the extent of lateral internal sphincterotomy: spasm controlled vs. up to the fissure apex.. Dis. Colon & Rectum 2008;51:128‐133. [DOI] [PubMed] [Google Scholar]
Mousavi 2009 {published and unpublished data}
- Mousavi SR, Sharifi M, Mehdikhah Z. A comparison between the results of fissurectomy and lateral internal sphincterotomy in the surgical management of chronic anal fissure. J Gastrointest Surg 2009;13:1279‐82.. [DOI] [PubMed] [Google Scholar]
Olsen 1987 {published data only}
- Olsen J, Mortensen PE, Krogh‐Petersen I, Christiansen J. Anal sphincter function after treatment of fissure‐in‐ano by lateral subcutaneous sphincterotomy versus anal dilatation. A randomized study. Int. J Colorectal Dis. Int J Colorectal Dis 1987;2:155‐157. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Pujahari 2010 {published and unpublished data}
- Pujahari AK. Unilateral versus bilateral lateral internal sphincterotomy: a randomized controlled trial for chronic anal fissure in ano. Tropical Gastroenterology 2010;31(1):69‐71. [PubMed] [Google Scholar]
Ram 2007 {published data only}
Renzi 2007 {published data only}
- Renzi A, Izzo D, Sarno G, Talento P, Torelli F, Izzo G, Martino N. Clinical, manometric, and ultrasonographic results of pneumatic balloondilatation vs. lateral internal sphincterotomy for chronic anal fissure: a prospective, randomized, controlled trial.. Dis Colon Rectum 2008;51(1):121‐7. [DOI] [PubMed] [Google Scholar]
Saad 1992 {published data only}
- Saad AM, Omer A. Surgical treatment of chronic fissure‐in‐ano: a prospective randomized study. East Afr. Med J. East Afr Med J 1992;69:613‐615. [MEDLINE: ] [PubMed] [Google Scholar]
Wang 2005 {published data only}
- Wang ZY, Sun JH, Chen XJ. Prospective randomized trial of optimum anal canal release treatment for chronic anal fissure. J Chinese Integr. Med 2005;3(3):190,206. [DOI] [PubMed] [Google Scholar]
Weaver 1987 {published data only}
- Weaver RM, Ambrose NS, Alexander‐Williams J, Keighley MR. Manual dilatation of the anus vs lateral subcutaneous sphincterotomy in the treatment of chronic fissure in ano. Results of a prospective, randomized clinical trial. Dis. Colon & Rectum. Dis Colon Rectum 1987;30:420‐423. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wiley 2004 {published data only}
- Wiley M, Day P, Rieger N, Stephens J, Moore J. Open vs. Closed lateral internal sphincterotomy for idiopathic fissure‐in‐ano: a prospective randomized controlled trial. Dis. Colon & Rectum 2004;47:847‐852. [DOI] [PubMed] [Google Scholar]
Yucel 2009 {published and unpublished data}
- Yucel T, Gonullu D, Oncu M, Koksoy FN, Ozkan SG, Aycan O. Comparison of controlled‐intermittent anal dilatation and lateral internal sphincterotomy in the treatment of chronic anal fissures: a prospective randomized study. Internation Journal of Surgery 2009;7(3):228‐31. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Abcarian 1980 {published data only}
- Abcarian H. Surgical correction of chronic anal fissure: results of lateral internal sphincterotomy vs. Fissurectomy ‐‐ midline sphincterotomy. Dis Colon & Rectum. Dis Colon Rectum 1980;23:31‐36. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
AlRaymoony 2001 {published data only}
- Al‐Raymoony AE. Surgical treatment of analfissures under local anaesthesia. Saudi Med. J 2001;22(2):114‐116. [PubMed] [Google Scholar]
Barisone 2004 {published data only}
- Barisone P, Ippolitti M, Dezzani C, Abbo L, Aimo I. Trattamento chirurgico della [Trattamento chirugico della ragade anale: confronto tra la sfinterotomia laterale aperta e sfinterotomia posteriore con analplatica]. Chirurgia 2004;17:43‐6. [Google Scholar]
Bekheit 1974 {published data only}
- Bekheit F. Anal fissure: comparative study of various lines of treatment in 125 cases. J Egypt. Med Assoc. J Egypt Med Assoc 1974;57:365‐372. [MEDLINE: ] [PubMed] [Google Scholar]
Bouchard 2010 {published and unpublished data}
- Bouchard D, Souffran M, Devulder F, Ganansia R, Castinel A, Staumont G, Sudaca J, Soudan D, Pigot F, Guvot P, Abramowitz L. Diseases of the colon and rectum conference: annual meeting of the American Society of Colon and Rectal Surgeons, ASCRS Minneapolis, MN United States. Conference publication. 2010.
Cho 2005 {published data only}
- Cho DY. Controlled lateral sphincterotomy for chronic anal fissure. Dis. Colon & Rectum 2005;48:1037‐41. [DOI] [PubMed] [Google Scholar]
Collopy 1979 {published data only}
- Collopy B, Ryan P. Comparison of lateral subcutaneous sphincterotomy with anal dilation in the treatment of fissure in ano. Med J Aust 1979;2:461‐462. [MEDLINE: ] [PubMed] [Google Scholar]
Ektov 1986 {published data only}
- Ektov VN, Nalivkin AI, Kriachkov AA, Lakatosh KO. Selection of the most effective method of lateral subcutaneous sphincterotomy in the treatment of fissure in ano. Vestn Khir. Vestn Khir 1986;136:37‐41. [MEDLINE: ] [PubMed] [Google Scholar]
Garcia 1996 {published and unpublished data}
- Garcia‐Aguilar J, Belmonte C, Wong WD, Lowry AC, Madoff RD. Open vs closed sphincterotomy for chronic anal fissure: long term results. Dis. Colon & Rectum. Dis Colon Rectum 1996;39:440‐443. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Giebel 1989 {published data only}
- Giebel GD, Horch R. Treatment of anal fissure: a comparison of three different forms of therapy. Nippon Hokan. Nippon Hokan 1989;58:126‐133. [MEDLINE: ] [PubMed] [Google Scholar]
Gupta 2007 {published data only}
- Gupta PJ. Effects of warm water sitz bath on symptoms of post‐anal aphincterotomy in chronic anal fissure ‐ a randomized and controlled study. World J Surg 2007;31:1480‐84. [DOI] [PubMed] [Google Scholar]
Gupta2006 {published data only}
- Gupta PJ. Randomized controlled study comparing sitz bath and no sitz bath treatments with acute anal fissure. ANZ J Surg 2006;76:718‐21. [DOI] [PubMed] [Google Scholar]
Hancke 2009 {published and unpublished data}
- Hancke E, Rikas E, Schwaner S, Völke K. Fissurectomy versus fissurectomy and lateral internal sphincterotomy for idiopathic chronic fissure in ano. A prospective, randomized trial 5 years postoperatively [Fissurexzision versus fissurexzision und laterale interne sphinkterotomie bei der chronischen analfissur. Eine prospektive, randomisierte studie 5 jahre postoperativ]. Coloproctology 2009;31:1‐9. [Google Scholar]
Hawley 1969 {published data only}
- Hawley P. The treatment of chronic fissure in ano; a trial of methods. Br J Surg. Br J Surg 1969;56:915‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hoffman 1970 {published data only}
- Hoffman DC, Goligher JC. Lateral subcutaneous internal sphincterotomy in treatment of anal fissure. Br Med J. Br Med J 1970;3:673‐5. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewis 1988 {published data only}
- Lewis TH, Corman ML, Prager ED, Robertson WG. Long term results of open and closed sphincterotomy for anal fissure. Dis. Colon & Rectum. Dis Colon Rectum 1988;31:368‐371. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Oueidat 1999 {published data only}
- Oueidat D. A comparative sutdy in anal fissure treatment. J Med. Libanaise 1999;47(3):164‐68. [PubMed] [Google Scholar]
Pernikoff 1994 {published data only}
- Pernikoff BJ, Eisenstat TE, Rubin RJ, Oliver GC, Salvati EP. Reappraisal of partial lateral internal sphincterotomy. Dis. Colon & Rectum. Dis Colon Rectum 1994;37:1291‐1295. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Additional references
Ammari 2004
- Ammari FF, Bani‐Hani KE. Faecal incontinence in patients with anal fissure: a consequence of internal sphincterotomy or a feature of the condition?. Surgeon 2004;2:225‐229. [DOI] [PubMed] [Google Scholar]
Casillas 2004
- Casillas S, Hull TL, Zutshi M, Trzcinski R, Bast JF, Xu M. Incontinence after lateral internal sphincterotomy: Are we underestimating it?. Dis. Colon & Rectum 2005;48:504. [DOI] [PubMed] [Google Scholar]
Goligher 1975
- Goligher JC, Duthie HL, Nixon HH. Surgery of the Rectum, Anus & Colon. 3rd Edition. London: Balliere & Tindall, 1975. [Google Scholar]
Hyman 2004
- Hyman N. Incontinence after lateral internal sphincterotomy: a prospective study and quality of life assessment. Dis. Colon & Rectum 2004;47:35‐38. [DOI] [PubMed] [Google Scholar]
Mentes 2006
- Mentes BB, Tezcaner T, Yilmaz U, Leventoglu S, Oguz M. Results of lateral internal sphincterotomy for chronic anal fissure with particular reference to quality of life.. Dis Colon Rectum 2006;49(7):1045‐51. [DOI] [PubMed] [Google Scholar]
Nelson 1999
- Nelson RL. Meta‐analysis of operative techniques for fissure‐in‐ano. Dis Colon Rectum 1999;42(11):1424‐1431. [MEDLINE: ; 20030806 UI] [DOI] [PubMed] [Google Scholar]
Nelson 2006
- Nelson R. Non‐surgical therapy for anal fissure. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858] [DOI] [PubMed] [Google Scholar]
Renzi 2005
- Renzi A, Brusciano L, Pescatori M, Izzo D, Napoletano V, Rossetti G, Genio G, Genio A. Pneumatic balloon dilation for chronic anal fissure: a prosepctive clinical endosonographic and manometric study. Dis. Colon & Rectum 2005;48:121‐126. [DOI] [PubMed] [Google Scholar]
Rotholtz 2005
- Rotholtz NA, Bun M, Mauri MV, Bosio R, Peczan CE, Mezzadri NA. Long‐term assessment of fecal incontinence after lateral interanl sphincterotomy. Tech. Coloproctology 2005;9:115‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schouten 1994
- Schouten WR, Briel JW, Auwerda JJA. Relationship between anal pressure and anodermal blood flow. Dis Colon Rectum 1994;37:664‐669. [MEDLINE: ; 94298415] [DOI] [PubMed] [Google Scholar]


