Several case reports and cohort studies have examined the use of (1,3)-beta-d-glucan measurement with cerebrospinal fluid to diagnose fungal meningitis. This systematic review aims to characterize the evidence regarding cerebrospinal fluid (1,3)-beta-d-glucan measurement to detect fungal meningitis. We searched PubMed for (1,3)-beta-d-glucan and each of several distinct fungi, cerebrospinal fluid, and meningitis. Summary data including diagnostic performance (where applicable) were recorded.
KEYWORDS: (1,3)-beta-d-glucan; Coccidioides meningitis; cryptococcal meningitis; Exserohilum rostratum; Histoplasma meningitis; cerebrospinal fluid; fungal meningitis
ABSTRACT
Several case reports and cohort studies have examined the use of (1,3)-beta-d-glucan measurement with cerebrospinal fluid to diagnose fungal meningitis. This systematic review aims to characterize the evidence regarding cerebrospinal fluid (1,3)-beta-d-glucan measurement to detect fungal meningitis. We searched PubMed for (1,3)-beta-d-glucan and each of several distinct fungi, cerebrospinal fluid, and meningitis. Summary data including diagnostic performance (where applicable) were recorded. A total of 939 records were examined via a PubMed search. One hundred eighteen records remained after duplicates were removed, and 104 records were excluded, as they did not examine cerebrospinal fluid, included animals, or focused on nonfungal infections. Fourteen studies were included in this systematic review. A variety of fungi, including species of Candida, Aspergillus, Exserohilum, Cryptococcus, Histoplasma, and Coccidioides, were studied, although most were case reports. Diagnostic accuracy was examined in 5 studies. Cerebrospinal fluid (CSF) (1,3)-beta-d-glucan measurement showed >95% sensitivity in the corticosteroid injection-related outbreak of Exserohilum rostratum. One study in Histoplasma meningitis found 53% (53/87) sensitivity and 87% (133/153) specificity, while another study of Cryptococcus meningitis found 89% (69/78) sensitivity and 85% (33/39) specificity. CSF (1,3)-beta-d-glucan testing may be useful, primarily as a nonspecific marker of fungal meningitis. Although the FDA black box warning states that Cryptococcus spp. do not make (1,3)-beta-d-glucan, the current evidence shows that (1,3)-beta-d-glucan is detectable in cryptococcal meningitis. Organism-specific testing should be used in conjunction with (1,3)-beta-d-glucan measurement.
INTRODUCTION
Meningitis may be caused by a diverse group of fungal pathogens, including molds, yeast, and dimorphic fungi. Symptoms such as headache, neck stiffness, and fever commonly occur, but their frequency varies by the type of fungi involved; typically, symptoms are subacute. Yet, fungal meningitis is often underrecognized as a cause of meningitis worldwide. For instance, cryptococcal meningitis is the most common cause of fungal meningitis worldwide and is the most common cause of meningitis in sub-Saharan Africa (1). Cryptococcal meningitis carries an average cost per case of $103,236, with an average length of hospitalization of 70.6 days in the United States (2). In Uganda, the estimated cost of initial diagnosis and treatment of cryptococcal meningitis in Uganda is $5.6 million (1). Candida meningitis is common in preterm infants and in persons with central nervous system (CNS) ventriculostomies or immunocompromised states (3). Further, although molds such as Exserohilum rostratum or Aspergillus species are generally uncommon causes of meningitis, iatrogenic outbreaks or sporadic cases may be devastating. Finally, endemic fungi such as Coccidioides or Histoplasma spp. are important causes of meningitis within their regions of endemicity (ever expanding due to a number of circumstances) (2, 4, 5).
Despite the importance of fungal pathogens as causes of meningitis, improved diagnostic tools are urgently needed in many cases. Classically, fungal meningitis is detected by culture or direct visualization of the fungus in cerebrospinal fluid (CSF) samples. While culture in many cases is fairly accurate, results often take at least 7 days, and so clinical utility is limited. The cryptococcal antigen (CrAg) lateral flow assay (LFA; Immuno-Mycologics, Norman, OK, USA) is the most rapid, effective way to diagnose cryptococcal meningitis, with sensitivity and specificity generally being >99% in CSF in testing of over 600 samples (6). While good performance has been noted for antigen detection in meningitis due to Coccidioides and Histoplasma spp., the diagnostic performance of antigen detection is less clear for Blastomyces meningitis (7–14).
Given that for many types of fungal meningitis, diagnostic testing is inadequate, new diagnostic tests are needed. One test of interest is the detection of the polysaccharide glucose polymer 1,3-beta-d-glucan (BDG), a component of the fungal cell wall (15). Several studies have been conducted to evaluate the efficacy of this test on serum samples to diagnose invasive fungal infections, and more recently, studies have investigated the use of BDG testing on CSF (16–19). Although a review of BDG testing discussed CSF BDG testing for some fungal pathogens, a systematic review of CSF BDG testing has not been completed to date (18). This review aims to examine previous studies and reports of CSF BDG use in fungal meningitis to better understand the diagnostic utility of CSF BDG.
MATERIALS AND METHODS
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis of Diagnostic Test Accuracy (PRISMA–DTA) statement (20).
Search strategy.
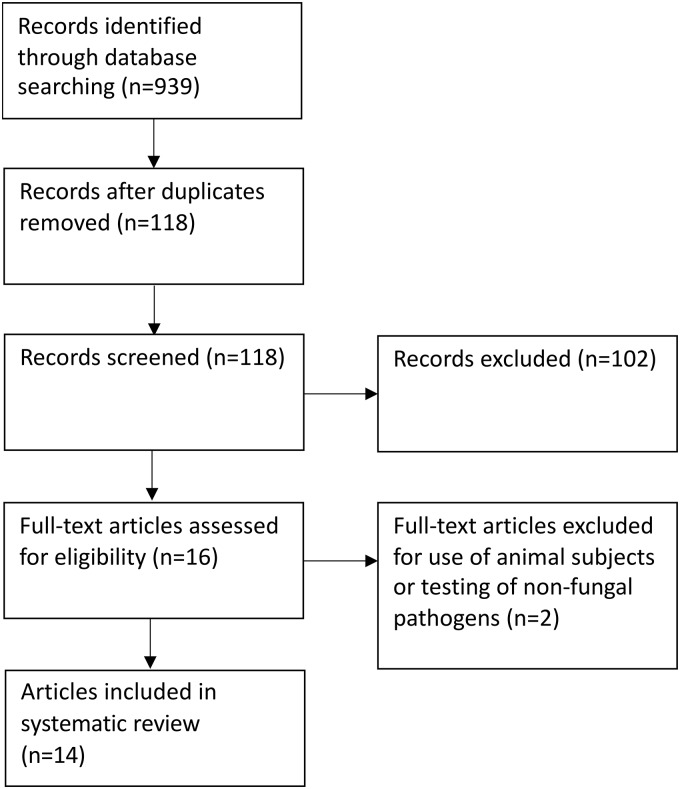
We searched PubMed (from inception until 7 February 2019) without any language restrictions using the terms “1,3 beta-d-glucan” AND each of the following: histoplasmosis, Histoplasma capsulatum, Cryptococcus, Cryptococcus neoformans, Cryptococcus gattii, cryptococcosis, coccidioidomycosis, Coccidioides immitis, blastomycosis, Blastomyces dermatitidis, aspergillosis, Aspergillus flavus, Aspergillus fumigatus, Aspergillus niger, mucormycosis, Mucor mucedo, Candida, Candida albicans, candidiasis, Exserohilum, Exserohilum rostratum, Talaromyces, Talaromyces marneffei, Fusarium, Fusarium oxysporum, Paracoccidioides, Paracoccidioides brasiliensis, Paracoccidioides lutzii, phaeohyphomycosis, Scedosporium, Scedosporium prolificans, sporotrichosis, Sporothrix schenckii, meningitis, and cerebrospinal fluid (Fig. 1).
FIG 1.
Flow chart of the study selection process demonstrating the number of records identified through PubMed queries. After duplicate records were removed, 118 studies were screened, and 104 studies were excluded based on the previously outlined criteria, which left a total of 14 records for this study.
Inclusion and exclusion criteria.
Studies were included in the systematic review if they involved human subjects and measured BDG levels in CSF. Studies were excluded if they involved animal subjects or did not measure BDG in CSF (e.g., measured blood only). Due to the relative lack of cohort trials, case reports were also included.
Study selection and data extraction.
Two authors (C.D. and N.C.B.) independently reviewed the studies and selected them for use in the review. The following data were then extracted from each study as available: details of publication (authors, country, and year of publication), organism(s) involved, study objective, number of patients, details of the diagnostic test, sensitivity and specificity, population, diagnosis of meningitis, intervention, follow-up period, control, and outcomes. No statistical analysis was completed, as a meta-analysis was not deemed feasible given the available studies.
RESULTS
The literature search produced 939 records, of which 118 remained after duplicates were removed. One hundred two studies were excluded due to not measuring CSF BDG levels. Sixteen full-text publications were examined, of which one additional study was excluded due to nonhuman subjects being included and another excluded due to its focus on Nocardia spp. rather than on fungal pathogens. Thus, of the 14 studies that were included in this systematic review (Fig. 1), 13 studies were from the United States, while one study included subjects from Uganda and South Africa. The causes of fungal meningitis examined in the studies are diverse and included Cryptococcus, Coccidioides, Histoplasma, Aspergillus, Exserohilum, and Candida spp. Eight studies were case reports or series, while seven were case-control studies. None of the studies included interventions based on BDG. Six of the studies determined diagnostic accuracy, although the cutoff level of CSF BDG used was not uniform. Twelve studies used the Fungitell assay (21–32). Two studies did not specify the method of BDG measurement (Table 1).
TABLE 1.
Characteristics of studies reporting the use of beta-d-glucan measurement in cerebrospinal fluid as a diagnostic test for fungal meningitisa
| Outcome(s) measured | No. of controls | No. of cases | Organism | Study type or objective | Country/ies | Type of study | Cohortb |
|---|---|---|---|---|---|---|---|
| CSF BDG persistence | NA | 1 | Candida tropicalis | Descriptive | USA | Case report | Ceccarelli et al. (21) |
| CSF BDG | NA | 1 | Aspergillus spp. | Descriptive | USA | Case report | Chen et al. (34)c |
| Sensitivity | 66 | 108 (41 definite, 67 probable) | Exserohilum rostratum | Diagnostic accuracy and response to treatment | USA | Case-control | Litvintseva et al. (22) |
| CSF BDG | NA | 1 | Candida sp. | Descriptive | USA | Case report | Lyons et al. (33)c |
| NA | NA | 5 | Unknown | Descriptive | USA | Case series | Lyons et al. (23) |
| NA | 66 | 9 | Cryptococcus spp., Histoplasma spp., Exserohilum spp. | Diagnostic accuracy | USA | Case-control | Lyons et al. (32) |
| Specificity, sensitivity | 153 | 47 | Histoplasma spp. | Diagnostic accuracy | USA | Case-control | Myint et al. (24)d |
| Specificity, sensitivity, decline over time | 39 | 78 | Cryptococcus spp. | Diagnostic accuracy and response to treatment | Uganda, South Africa | Case-control | Rhein et al. (25) |
| Specificity, sensitivity, PPV, NPV, decline over time | 11 | 26 | Coccidioides spp. | Diagnostic accuracy | USA | Case-control | Stevens et al. (26) |
| CSF BDG | 19 | 5 (n = 3, Aspergillus spp.; n = 1, Histoplasma sp.; n = 1, Cryptococcus sp.) | Aspergillus spp., Histoplasma sp., Cryptococcus sp. | Descriptive | USA | Case-control | Mikulska et al. (27) |
| Sensitivity, specificity | 135 | 28 (n = 1, Aspergillus spp.; n = 27, Exserohilum spp.) | Exserohilum rostratum, Aspergillus sp. | Diagnostic accuracy | USA | Case-control | Malani et al. (28) |
| CSF BDG | NA | 9 (n = 7, Candida spp.; n = 2, Aspergillus spp.) | Candida spp., Aspergillus spp. | Descriptive | USA | Case series | Salvatore et al. (29) |
| CSF BDG | NA | 1 | Phaeohyphomycosis (exact pathogen unclear) | Descriptive | USA | Case report | Nelson et al. (30) |
| CSF BDG | NA | 2 | Aspergillus spp. | Descriptive | USA | Case series | Morgand et al. (31) |
CSF, cerebrospinal fluid; BDG, beta-d-glucan; NA, not available; PPV, positive predictive value; NPV, negative predictive value.
Sensitivity/specificity values are reported in Table 2 when available.
Study did not specify the assay used; all others reported use of the Fungitell assay.
This study had among its controls 13 cases of other fungal meningitis including meningitis due to Cryptococcus (n = 5), Blastomyces (n = 3), Candida (n = 2), Aspergillus (n = 2), and Coccidioidomyces (n = 1).
Candida.
Ceccarelli et al. described persistent CSF BDG levels in a case of meningitis due to Candida tropicalis on proper treatment in the setting of negative CSF culture (21). Lyons et al. described the use of CSF BDG to monitor treatment efficacy in Candida albicans meningitis, finding a level of 500 pg/ml in CSF versus 74 pg/ml in serum (33). The positive CSF BDG levels preceded Candida albicans CSF culture growth. Myint and colleagues described two cases of Candida meningitis as part of a larger study of Histoplasma meningitis; one case had a CSF BDG level of 234 pg/ml, while the other had a level of <31 pg/ml (24). Finally, Salvatore and colleagues examined seven cases of Candida meningitis in children (n = 4, Candida albicans; n = 2, Candida krusei; n = 1, Candida parapsilosis), and two cases of Aspergillus meningitis were also included (29). This study described a median CSF BDG value of 230 pg/ml on initial testing and a decrease to <31 pg/ml in all successfully treated cases (29).
Aspergillus.
Salvatore and colleagues examined one proven and one possible case of Aspergillus meningitis (29). Mikulska and colleagues reported five patients with invasive CNS fungal infections, of which three were due to Aspergillus (27). The mean CSF BDG level for the three cases of Aspergillus meningitis was 383 pg/ml versus 41 pg/ml for 19 controls (27). Chen et al. reported a case of ventriculitis due to Aspergillus fumigatus which had elevated CSF BDG levels that seemed to rise in correlation with severity of magnetic resonance imaging (MRI) and clinical findings (34). Morgand and colleagues reported two cases of CNS infection due to Aspergillus spp. (n = 1 each of Aspergillus fumigatus and Aspergillus flavus), in which serum and CSF Aspergillus galactomannan antigen testing were negative, serum BDG was negative, and CSF BDG was positive (31). The previously noted paper by Myint and colleagues also reported two cases of Aspergillus meningitis, each with CSF BDG levels of >500 pg/ml (24).
Exserohilum spp. and other pathogens related to contaminated methylprednisolone.
Exserohilum rostratum gained notoriety as a potential human pathogen related to the widespread outbreak in the United States due to contaminated methylprednisolone acetate vials (22). Among 233 CSF specimens, including 28 proven cases of histopathological evidence of a fungal pathogen of fungal meningitis (n = 27 E. rostratum, n = 1 A. fumigatus), Malani et al. found a sensitivity of 96% (27/28) and a specificity of 95% (128/135) using a BDG cutoff of 80 pg/ml and a reference standard of any CSF culture or PCR positive (28). Control CSF samples were obtained from persons exposed to contaminated methylprednisolone. When the reference standard was liberalized to include 17 probable cases of fungal meningitis (e.g., signs or symptoms felt to be highly suggestive of fungal meningitis), the sensitivity was 84% (38/45), and the specificity was 95% (128/135) (28). Litvintseva et al. (22) examined 41 cases of definite E. rostratum meningitis and 66 controls (27 exposed to contaminated methylprednisolone without meningitis, nine with bacterial meningitis, eight with viral meningitis, 1 with toxoplasmosis, and 21 without a known infection) related to the same outbreak. Sensitivity and specificity were 100% (41/41) and 98% (65/66), respectively, using a cutoff value of 138 pg/ml, and they were 99% (40/41) and 98% (65/66) at a cutoff of 230 pg/ml, respectively (22). If 67 additional probable cases were included (108 cases total), sensitivity was 68% (73/108) and 65% (70/108) at cutoff values of 138 pg/ml and 230 pg/ml, respectively, with a specificity of 98% (65/66) in both cases (22). PCR was only 29% sensitive among cases of definite or probable E. rostratum meningitis (31/108) (22). Table 2 summarizes the diagnostic performace of CSF BDG measurement for various fungi based on the currently available evidence. The authors also noted that CSF BDG declined during testing of serial samples of 16 case patients who improved with treatment (22). In 3 patients, the CSF BDG level did not decline with treatment, and these patients all experienced worse clinical outcomes (22). Of note, this study did not use the cutoff value (80 pg/ml) listed on the package insert. Last, Lyons and colleagues reported that three of five cases of from the same outbreak (without a confirmed fungal etiology) had an elevated CSF BDG, with one that decreased with antifungal treatment (23); in another study, they reported two cases of E. rostratum meningitis with CSF BDG levels of 797 and 1,524 pg/ml, respectively (32).
TABLE 2.
Beta-d-glucan diagnostic performance on cerebrospinal fluid in fungal meningitis by cohort
| Organism(s) | % (no./total no.) for: |
CSF BDG concn cutoff used (pg/ml)a | |
|---|---|---|---|
| Sensitivity | Specificity | ||
| Exserohilum rostratum (23) | 100 (41/41) | 98 (65/66) | 138 |
| 99 (40/41) | 98 (65/66) | 230 | |
| Exserohilum rostratum, Aspergillus species (30)b | 96 (27/28) | 95 (128/135) | 80 |
| Histoplasma capsulatum (26) | 53 (25/47) | 87 (133/153) | 80 |
| Cryptococcus neoformans (27) | 89 (69/78) | 85 (33/39) | 80 |
| Coccidioides species (28) | 96 (25/26) | 82 (9/11) | 31 |
The clinically recommended cutoff value is 80 pg/ml.
Multiple organisms included in the cohort.
Nelson and colleagues reported a case of a cerebral mycotic aneurysm presumed to be due to phaeohyphomycosis with symptom onset 17 days after a methylprednisolone infection (30). Although microbiological and molecular techniques were negative for a fungal pathogen, the CSF BDG level was >500 pg/ml (30). The patient received 32 weeks of antifungal treatment and was well a year after symptoms began (30).
Cryptococcus.
Rhein and colleagues examined CSF BDG in 78 subjects with cryptococcal meningitis and 39 controls suspected to have other forms of meningitis; all subjects were HIV infected, with low CD4 counts (25). The median CSF BDG levels were 343 pg/ml among cases and 37 pg/ml among controls (25). CSF BDG sensitivity was 89% (69/78), and specificity was 85% (33/39) using a cutoff value of 80 pg/ml (25). Additionally, the sensitivity improved to 98% when the initial fungal burdens were above or equal to 10,000 CFU/ml (25). Interestingly, CSF BDG levels did decrease more rapidly than did cryptococcal antigen levels (25). Among six cases of cryptococcal meningitis, Lyons and colleagues found that five cases had detectable CSF BDG (though all were <80 pg/ml). Among 66 persons without CNS fungal infections, the median CSF BDG level was 13.5 pg/ml (range, <4 to 109 pg/ml), well below 80 pg/ml, the typical cutoff used clinically (32). Myint and colleagues described five cases of cryptococcal meningitis as part of a larger study of Histoplasma meningitis, and three of the five cases had CSF BDG levels above 80 pg/ml (82, 221, and 500 pg/ml) (24). Mikulska and colleagues also reported one case of BDG measurement in cryptococcal meningitis (27).
Histoplasma.
Myint and colleagues (24) examined 47 persons with meningitis caused by Histoplasma capsulatum, including 9 confirmed via CSF culture, 33 probable via detection of Histoplasma antigen by enzyme immunoassay (EIA) or anti-Histoplasma antibodies in the CSF by immunodiffusion (ID) or complement fixation (CF), 5 possible with pulmonary or disseminated histoplasmosis with CSF pleocytosis but without laboratory confirmation of CNS involvement and no alternative etiology for the CSF pleocytosis, and 153 controls. They found CSF BDG levels of ≥80 pg/ml in 25/47 cases, with a median of 85 pg/ml among cases and a median of <31 pg/ml among controls (24). The sensitivity and specificity of CSF BDG were 53% (25/47) and 87% (133/153), respectively (24). Interestingly, 13 subjects with other fungal meningitis were among the controls (referred to in the paragraph related to the particular pathogen throughout the manuscript), with a median CSF BDG level of 82 pg/ml. Seven of those 13 controls with other fungal meningitis had CSF BDG levels of >80 pg/ml, and if those 13 subjects were excluded, specificity for Histoplasma meningitis rose to 91% (127/140) (24). Mikulska and colleagues (27) reported one case of BDG measurement in Histoplasma meningitis (282 pg/ml), as did Lyons and colleagues (110 pg/ml) (32).
Coccidioides.
Stevens et al. tested 26 CSF samples from 21 patients with confirmed coccidioidal meningitis and 11 control CSF samples (from 11 subjects). Any positive CSF coccidioidal antibody or culture in a subject with clinical meningitis was used as the reference standard (26). A cutoff value of 31 pg/ml was used. Sensitivity was 96% (25/26), specificity was 82% (9/11), the positive predictive value was 93% (25/27), and the negative predictive value was 90% (9/10) (26). Performance with a cutoff of 80 pg/ml was not given, and exact CSF BDG values are not given here. Interestingly, some samples maintained positive CSF BDG levels for up to 8 years (26). One case of Coccidioides meningitis was also described by Myint and colleagues in their histoplasmosis study, in which the CSF BDG level was <31 pg/ml (24).
Blastomyces.
The study by Myint and colleagues (24) looking at CSF BDG diagnostic performance for Histoplasma meningitis described three cases of Blastomyces meningitis; all were CSF culture negative. Case one had a positive CSF Blastomyces antigen and bronchoalveolar lavage fluid culture with Blastomyces sp., and the CSF BDG level was 79 pg/ml. Case two also had positive CSF and urine Blastomyces antigen tests; postmortem leptomeningeal tissue Grocott’s stain was consistent with Blastomyces, and the CSF BDG level was 176 pg/ml. Case three had a positive Blastomyces urine antigen result and bronchoalveolar lavage fluid culture, a negative CSF Blastomyces antigen test, and a CSF BDG level of 61 pg/ml (24).
DISCUSSION
Fungal meningitis is caused by several organisms, and testing accuracy varies with each organism. Delay in diagnosis and treatment leads to poor outcomes. While not specific for any particular cause of fungal meningitis, CSF BDG measurement may hold some utility as a marker of fungal disease, particularly in cases of subacute meningitis without clear etiologies.
This systematic review of the currently available studies of CSF BDG measurement has several limitations, primarily related to the small overall numbers of studies available, small overall numbers of cases (aside from Exserohilum, Histoplasma, and Cryptococcus spp.), and study heterogeneity. Due to the small numbers of studies and different CSF BDG cutoff values used, we felt that a meta-analysis could not be performed. Further, we can only comment on the specific fungi examined by the included studies and so cannot comment on the utility of CSF BDG measurement for other fungal causes of meningitis. In addition, we are not able to comment on the role of common causes of false-positive serum BDG results, such as bowel surgery treatment with immunoglobulin, albumin, or other blood products filtered through cellulose filters containing BDG, patients undergoing hemodialysis with cellulose membranes, or the use of certain antibiotics, as none of the studies addressed these issues (35–38).
In Candida meningitis, only case reports were available; thus, we cannot comment on diagnostic performance for CSF BDG measurement in this disease. Yet, some authors posited that CSF BDG may have a role in monitoring treatment response given the poor diagnostic performance of fungal culture. CSF BDG measurement in preterm infants with known Candida disease at other sites has also been considered. Whether or not CSF BDG can be relied upon in this situation is uncertain.
In meningitis due to Aspergillus or Blastomyces spp., though CSF BDG may be positive, its diagnostic performance (e.g., sensitivity, specificity, etc.) is unclear. CSF BDG measurement showed perhaps the most promise in a formal diagnostic study in persons with CNS infection due to Exserohilum rostratum. Yet, although one study found sensitivity and specificity at >98% (at higher cutoffs than typical), another study could not replicate these findings (22, 28).
Cryptococcus spp. are often thought not to have sufficient BDG levels to cause positive test results based on a small study of seven subjects without HIV infection with pulmonary cryptococcosis and negative plasma BDG levels; in cryptococcal meningitis, this is clearly not true (25, 39). In the only study to systematically investigate CSF BDG in cryptococcal meningitis, sensitivity was 89% (69/78) (25). Although CSF BDG was not as effective as a cryptococcal antigen, it may have some role in differentiating immune reconstitution inflammatory syndrome (IRIS) from true relapse of disease, as it cleared quickly from the CSF in one study (25). This finding, however, has not been duplicated, and the ability of CSF BDG to differentiate IRIS from relapse is conjecture at this point. Probably the most important take-home point in regard to Cryptococcus and CSF BDG is that a positive CSF BDG may, in fact, be due to Cryptococcus spp. (e.g., one should not presume noncryptococcal fungal disease on the basis of a positive CSF BDG result alone). CSF cryptococcal antigen remains the test of choice for cryptococcal meningitis.
The performance of CSF BDG was inadequate for meningitis due to both Histoplasma spp. (sensitivity, 53%) and Coccidioides spp. (specificity, 82%). Interestingly, a positive CSF BDG was noted up to 8 years after initial diagnosis in some cases of coccidioidomycosis meningitis, as opposed to its rapid clearance with cryptococcal meningitis (24, 26). Yet, the use of 31 pg/ml as a cutoff value in this study makes this finding (and the overall accuracy of the test) difficult to interpret for Coccidioides meningitis.
One advantage of the CSF BDG test compared to waiting for fungal cultures is that the turnaround time is relatively brief. Of the studies examined in this systematic review, only one study had information on the length of time needed to process CSF BDG. This study demonstrated that assays performed by Beacon Diagnostics Laboratory had a turnaround time of 48 to 96 h for CSF BDG (29). In Kansas City, a local laboratory typically gets results back to our facility in ∼48 h.
Clinically, the role of monitoring CSF BDG during treatment has been demonstrated to be potentially useful in some settings. Rhein and colleagues showed that CSF BDG decreased more rapidly than did the CSF cryptococcal antigen during treatment (25). Litvintseva and colleagues also studied this effect and found that CSF BDG levels declined with treatment except in patients who had poor clinical outcomes in their study of Exserohilum rostratum cases (22). Clearly, additional data are needed to draw stronger conclusions; however, in cases of fungal meningitis with high CSF BDG levels at baseline, it may be reasonable to track levels with any repeat lumbar puncture to assess treatment response. Whether or not this also indicates that antifungal therapy prior to CSF BDG measurement might decrease levels is unclear, though this would be theoretically possible. None of the studies comment on the timing of antifungal therapy relative to initial CSF BDG testing.
Despite our intensive search, we found no reported cases of measuring CSF BDG in patients with meningitis caused by Talaromyces, Fusarium, Paracoccidioides, or Scedosporium spp. or sporotrichosis.
Future studies must address potential causes of false-positive BDG results, and particular focus should be given to those causes of fungal meningitis without adequate current methods of diagnosis if feasible. Further, any study of CSF BDG for fungal meningitis should report test performance using the approved cutoff of 80 pg/ml, even if other experimental cutoffs are reported as well. In one case, one of the few indications of ongoing infection was an elevated CSF BDG level, suggesting a possible role as a screening test in persons without a clear cause of subacute meningitis (30). One may consider CSF BDG measurement as a screening tool for fungal meningitis broadly, but to do so, one must also recognize inadequate specificity for any particular fungal etiology as well as inferior performance for some more specific tests, such as cryptococcal antigen testing, and uncertainty for many types of fungal meningitis. Thus, the use of CSF BDG measurement should be considered with caution and should not replace more specific testing.
ACKNOWLEDGMENTS
This publication was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under awards K23NS110470 and R01NS086312.
The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in the writing of the manuscript or the choice to submit the manuscript. L.J.W. reports that he is the medical director, president, and founder of MiraVista Diagnostics. N.C.B. and D.R.B. received research funding from the National Institutes of Health during the completion of this study. The other authors declare no conflicts of interest.
C.D. was involved in the literature search, data collection, data interpretation, writing, and figures. L.J.W., T.M., and D.R.B. performed a critical review of the manuscript and data interpretation. N.C.B. was involved in the literature search, data collection, data interpretation, writing and revision of the manuscript, and study design.
REFERENCES
- 1.Rajasingham R, Smith RM, Park BJ, Jarvis JN, Govender NP, Chiller TM, Denning DW, Loyse A, Boulware DR. 2017. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis 17:873–881. doi: 10.1016/S1473-3099(17)30243-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Charalambous LT, Premji A, Tybout C, Hunt A, Cutshaw D, Elsamadicy AA, Yang S, Xie J, Giamberardino C, Pagadala P, Perfect JR, Lad SP. 2018. Prevalence, healthcare resource utilization and overall burden of fungal meningitis in the United States. J Med Microbiol 67:215–227. doi: 10.1099/jmm.0.000656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gottfredsson M, Perfect JR. 2000. Fungal meningitis. Semin Neurol 20:307–322. doi: 10.1055/s-2000-9394. [DOI] [PubMed] [Google Scholar]
- 4.Stockamp NW, Thompson GR III. 2016. Coccidioidomycosis. Infect Dis Clin North Am 30:229–246. doi: 10.1016/j.idc.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Bradsher RW. 1996. Histoplasmosis and blastomycosis. Clin Infect Dis 22(Suppl 2):S102–S111. doi: 10.1093/clinids/22.Supplement_2.S102. [DOI] [PubMed] [Google Scholar]
- 6.Boulware DR, Rolfes MA, Rajasingham R, von Hohenberg M, Qin Z, Taseera K, Schutz C, Kwizera R, Butler EK, Meintjes G, Muzoora C, Bischof JC, Meya DB. 2014. Multisite validation of cryptococcal antigen lateral flow assay and quantification by laser thermal contrast. Emerg Infect Dis 20:45–53. doi: 10.3201/eid2001.130906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wheat LJ, Kohler RB, Tewari RP, Garten M, French ML. 1989. Significance of Histoplasma antigen in the cerebrospinal fluid of patients with meningitis. Arch Intern Med 149:302–304. doi: 10.1001/archinte.1989.00390020044009. [DOI] [PubMed] [Google Scholar]
- 8.Bloch KC, Myint T, Raymond-Guillen L, Hage CA, Davis TE, Wright PW, Chow FC, Woc-Colburn L, Khairy RN, Street AC, Yamamoto T, Albers A, Wheat LJ. 2018. Improvement in diagnosis of Histoplasma meningitis by combined testing for Histoplasma antigen and immunoglobulin G and immunoglobulin M anti-Histoplasma antibody in cerebrospinal fluid. Clin Infect Dis 66:89–94. doi: 10.1093/cid/cix706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bariola JR, Perry P, Pappas PG, Proia L, Shealey W, Wright PW, Sizemore JM, Robinson M, Bradsher RW Jr. 2010. Blastomycosis of the central nervous system: a multicenter review of diagnosis and treatment in the modern era. Clin Infect Dis 50:797–804. doi: 10.1086/650579. [DOI] [PubMed] [Google Scholar]
- 10.Kassis C, Zaidi S, Kuberski T, Moran A, Gonzalez O, Hussain S, Hartmann-Manrique C, Al-Jashaami L, Chebbo A, Myers RA, Wheat LJ. 2015. Role of Coccidioides antigen testing in the cerebrospinal fluid for the diagnosis of coccidioidal meningitis. Clin Infect Dis 61:1521–1526. doi: 10.1093/cid/civ585. [DOI] [PubMed] [Google Scholar]
- 11.Wheat LJ, Batteiger BE, Sathapatayavongs B. 1990. Histoplasma capsulatum infections of the central nervous system. A clinical review. Medicine (Baltimore) 69:244–260. doi: 10.1097/00005792-199007000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Wheat J, Myint T, Guo Y, Kemmer P, Hage C, Terry C, Azar MM, Riddell J, Ender P, Chen S, Shehab K, Cleveland K, Esguerra E, Johnson J, Wright P, Douglas V, Vergidis P, Ooi W, Baddley J, Bamberger D, Khairy R, Vikram HR, Jenny-Avital E, Sivasubramanian G, Bowlware K, Pahud B, Sarria J, Tsai T, Assi M, Mocherla S, Prakash V, Allen D, Passaretti C, Huprikar S, Anderson A. 2018. Central nervous system histoplasmosis: multicenter retrospective study on clinical features, diagnostic approach and outcome of treatment. Medicine (Baltimore) 97:e0245. doi: 10.1097/MD.0000000000010245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bamberger DM, Pepito BS, Proia LA, Ostrosky-Zeichner L, Ashraf M, Marty F, Scully E, Wheat LJ. 2015. Cerebrospinal fluid Coccidioides antigen testing in the diagnosis and management of central nervous system coccidioidomycosis. Mycoses 58:598–602. doi: 10.1111/myc.12366. [DOI] [PubMed] [Google Scholar]
- 14.Walkty A, Keynan Y, Karlowsky J, Dhaliwal P, Embil J. 2018. Central nervous system blastomycosis diagnosed using the MVista Blastomyces quantitative antigen enzyme immunoassay test on cerebrospinal fluid: a case report and review of the literature. Diagn Microbiol Infect Dis 90:102–104. doi: 10.1016/j.diagmicrobio.2017.10.015. [DOI] [PubMed] [Google Scholar]
- 15.Tsoni SV, Brown GD. 2008. Beta-glucans and dectin-1. Ann N Y Acad Sci 1143:45–60. doi: 10.1196/annals.1443.019. [DOI] [PubMed] [Google Scholar]
- 16.Alexander BD, Smith PB, Davis RD, Perfect JR, Reller LB. 2010. The (1,3){beta}-d-glucan test as an aid to early diagnosis of invasive fungal infections following lung transplantation. J Clin Microbiol 48:4083–4088. doi: 10.1128/JCM.01183-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Odabasi Z, Mattiuzzi G, Estey E, Kantarjian H, Saeki F, Ridge RJ, Ketchum PA, Finkelman MA, Rex JH, Ostrosky-Zeichner L. 2004. Beta-d-glucan as a diagnostic adjunct for invasive fungal infections: validation, cutoff development, and performance in patients with acute myelogenous leukemia and myelodysplastic syndrome. Clin Infect Dis 39:199–205. doi: 10.1086/421944. [DOI] [PubMed] [Google Scholar]
- 18.McCarthy MW, Petraitiene R, Walsh TJ. 2017. Translational development and application of (1→3)-beta-d-glucan for diagnosis and therapeutic monitoring of invasive mycoses. Int J Mol Sci 18:1124. doi: 10.3390/ijms18061124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lyons JL, Zhang SX. 2016. Current laboratory approaches to diagnosis of CNS fungal infections. Future Microbiol 11:175–177. doi: 10.2217/fmb.15.138. [DOI] [PubMed] [Google Scholar]
- 20.McInnes MDF, Moher D, Thombs BD, McGrath TA, Bossuyt PM, Clifford T, Cohen JF, Deeks JJ, Gatsonis C, Hooft L, Hunt HA, Hyde CJ, Korevaar DA, Leeflang MMG, Macaskill P, Reitsma JB, Rodin R, Rutjes AWS, Salameh J-P, Stevens A, Takwoingi Y, Tonelli M, Weeks L, Whiting P, Willis BH, Group atP-D. 2018. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA 319:388–396. doi: 10.1001/jama.2017.19163. [DOI] [PubMed] [Google Scholar]
- 21.Ceccarelli G, Ghezzi MC, Raponi G, Brunetti G, Marsiglia C, Fallani S, Novelli A, Venditti M. 2016. Voriconazole treatment of Candida tropicalis meningitis: persistence of (1,3)-beta-d-glucan in the cerebrospinal fluid is a marker of clinical and microbiological failure: a case report. Medicine (Baltimore) 95:e4474. doi: 10.1097/MD.0000000000004474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Litvintseva AP, Lindsley MD, Gade L, Smith R, Chiller T, Lyons JL, Thakur KT, Zhang SX, Grgurich DE, Kerkering TM, Brandt ME, Park BJ. 2014. Utility of (1–3)-beta-d-glucan testing for diagnostics and monitoring response to treatment during the multistate outbreak of fungal meningitis and other infections. Clin Infect Dis 58:622–630. doi: 10.1093/cid/cit808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lyons JL, Roos KL, Marr KA, Neumann H, Trivedi JB, Kimbrough DJ, Steiner L, Thakur KT, Harrison DM, Zhang SX. 2013. Cerebrospinal fluid (1,3)-beta-d-glucan detection as an aid for diagnosis of iatrogenic fungal meningitis. J Clin Microbiol 51:1285–1287. doi: 10.1128/JCM.00061-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Myint T, Chow FC, Bloch KC, Raymond-Guillen L, Davis TE, Wright PW, Woc-Colburn L, Khairy RN, Street AC, Yamamoto T, Albers A, Wheat LJ, Hage CA. 2018. Detection of (1,3)-beta-d-glucan in cerebrospinal fluid in Histoplasma meningitis. J Clin Microbiol 56:e00663-18. doi: 10.1128/JCM.00663-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rhein J, Bahr NC, Morawski BM, Schutz C, Zhang Y, Finkelman M, Meya DB, Meintjes G, Boulware DR. 2014. Detection of high cerebrospinal fluid levels of (1→3)-beta-d-glucan in cryptococcal meningitis. Open Forum Infect Dis 1:ofu105. doi: 10.1093/ofid/ofu105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stevens DA, Zhang Y, Finkelman MA, Pappagianis D, Clemons KV, Martinez M. 2016. Cerebrospinal fluid (1,3)-beta-d-glucan testing is useful in diagnosis of coccidioidal meningitis. J Clin Microbiol 54:2707–2710. doi: 10.1128/JCM.01224-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mikulska M, Furfaro E, Del Bono V, Raiola AM, Di Grazia C, Bacigalupo A, Viscoli C. 2013. (1–3)-Beta-d-glucan in cerebrospinal fluid is useful for the diagnosis of central nervous system fungal infections. Clin Infect Dis 56:1511–1512. doi: 10.1093/cid/cit073. [DOI] [PubMed] [Google Scholar]
- 28.Malani AN, Singal B, Wheat LJ, Al Sous O, Summons TA, Durkin MM, Pettit AC. 2015. (1,3)-Beta-d-glucan in cerebrospinal fluid for diagnosis of fungal meningitis associated with contaminated methylprednisolone injections. J Clin Microbiol 53:799–803. doi: 10.1128/JCM.02952-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Salvatore CM, Chen TK, Toussi SS, DeLaMora P, Petraitiene R, Finkelman MA, Walsh TJ. 2016. (1→3)-β-d-Glucan in cerebrospinal fluid as a biomarker for Candida and Aspergillus infections of the central nervous system in pediatric patients. J Pediatric Infect Dis Soc 5:277–286. doi: 10.1093/jpids/piv014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nelson G, Fermo O, Thakur K, Felton E, Bang J, Wilson L, Rhee S, Llinas R, Johnson K, Sullivan D. 2014. Resolution of a fungal mycotic aneurysm after a contaminated steroid injection: a case report. BMC Res Notes 7:327. doi: 10.1186/1756-0500-7-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morgand M, Rammaert B, Poiree S, Bougnoux ME, Tran H, Kania R, Chretien F, Jouvion G, Lortholary O. 2015. Chronic invasive Aspergillus sinusitis and otitis with meningeal extension successfully treated with voriconazole. Antimicrob Agents Chemother 59:7857–7861. doi: 10.1128/AAC.01506-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lyons JL, Thakur KT, Lee R, Watkins T, Pardo CA, Carson KA, Markley B, Finkelman MA, Marr KA, Roos KL, Zhang SX. 2015. Utility of measuring (1,3)-β-d-glucan in cerebrospinal fluid for diagnosis of fungal central nervous system infection. J Clin Microbiol 53:319–322. doi: 10.1128/JCM.02301-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lyons JL, Erkkinen MG, Vodopivec I. 2015. Cerebrospinal fluid (1,3)-β-d-glucan in isolated Candida meningitis. Clin Infect Dis 60:161–162. doi: 10.1093/cid/ciu737. [DOI] [PubMed] [Google Scholar]
- 34.Chen TK, Groncy PK, Javahery R, Chai RY, Nagpala P, Finkelman M, Petraitiene R, Walsh TJ. 2017. Successful treatment of Aspergillus ventriculitis through voriconazole adaptive pharmacotherapy, immunomodulation, and therapeutic monitoring of cerebrospinal fluid (1→3)-β-d-glucan. Med Mycol 55:109–117. doi: 10.1093/mmy/myw118. [DOI] [PubMed] [Google Scholar]
- 35.Szyszkowitz A, Zurl C, Herzeg A, Berger A, Gemes G, Mitteregger M, Pruller F, Prattes J, Zollner-Schwetz I, Valentin T, Hoenigl M, Krause R. 2018. Serum 1,3-beta-d-glucan values during and after laparoscopic and open intestinal surgery. Open Forum Infect Dis 5:ofy296. doi: 10.1093/ofid/ofy296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ogawa M, Hori H, Niiguchi S, Azuma E, Komada Y. 2004. False-positive plasma (1→3)-beta-d-glucan test following immunoglobulin product replacement in an adult bone marrow recipient. Int J Hematol 80:97–98. doi: 10.1532/ijh97.04030. [DOI] [PubMed] [Google Scholar]
- 37.Nagasawa K, Yano T, Kitabayashi G, Morimoto H, Yamada Y, Ohata A, Usami M, Horiuchi T. 2003. Experimental proof of contamination of blood components by (1→3)-β-d-glucan caused by filtration with cellulose filters in the manufacturing process. J Artif Organs 6:49–54. doi: 10.1007/s100470300008. [DOI] [PubMed] [Google Scholar]
- 38.Liss B, Cornely OA, Hoffmann D, Dimitriou V, Wisplinghoff H. 2016. 1,3-β-d-Glucan contamination of common antimicrobials. J Antimicrob Chemother 71:913–915. doi: 10.1093/jac/dkv419. [DOI] [PubMed] [Google Scholar]
- 39.Miyazaki T, Kohno S, Mitsutake K, Maesaki S, Tanaka K, Ishikawa N, Hara K. 1995. Plasma (1→3)-beta-d-glucan and fungal antigenemia in patients with candidemia, aspergillosis, and cryptococcosis. J Clin Microbiol 33:3115–3118. doi: 10.1128/JCM.33.12.3115-3118.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]