Background
Subtotal cholecystectomy (STC) is a resection of the portion of the gallbladder performed due to hazardous inflammatory pathology or (and) non-standard relationships between the gallbladder and extrahepatic bile ducts, typically. Only 72 research papers – 67 case series (≥5), two cohort studies, and three reviews – were published on indications, outcomes, and technicalities of STC between 1985 and 2017. No recognised classification of technical variants of laparoscopic STC exists.
Technique
Figures 1, 2 and 3 depict four variants and five technical modalities (subvariants) of laparoscopic STC. To achieve a surgical tunnel of safety (when possible), distally from cystic pedicle for STC-1A and STC-1B (and even for STC-1C), is important. The drawings are useful for describing the technicalities of the STC – a variant and the extent of it. Surgical actions for branches of the cystic artery and remnant mucosa, type of completion of STC (fenestrating or reconstituting) and patterns of parahepatic drainage, are not features of this STC classification. They, as well as the number and size of gallstones removed, should be documented in the operation note (Fig 4).
Figure 1.
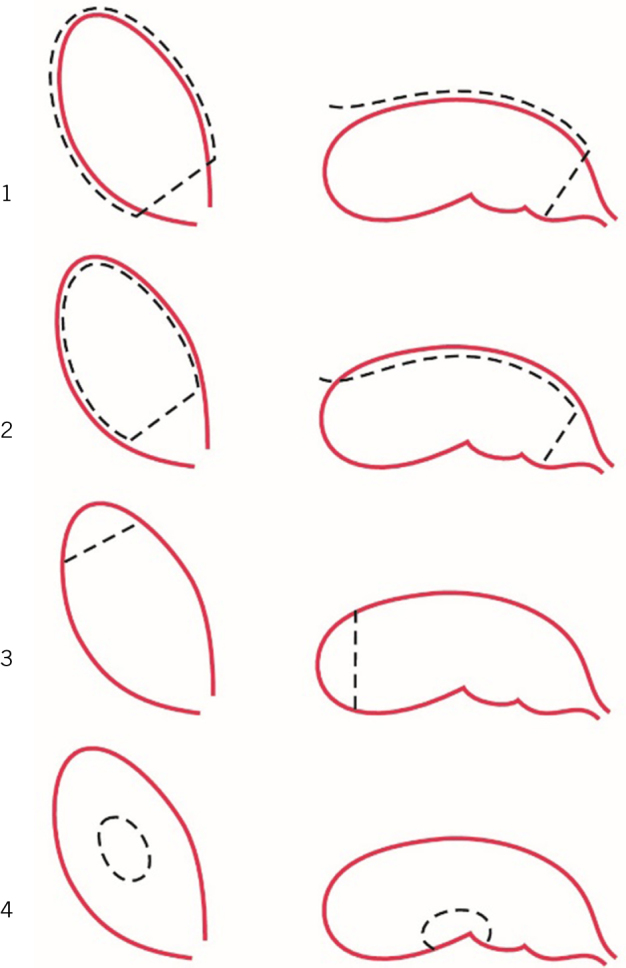
Four variants of laparoscopic STC:1) a circular excision of a considerable portion of the gallbladder (commonest; 80% of 61 laparoscopic STCs performed).2) a longitudinal removal of a considerable portion of the visceral wall of the gallbladder (18%).3) fundectomy (2% or less; in case of a solid inflammatory mass around the body and neck of the gallbladder in a high-risk patient).4) wedge resection of the gallbladder (possible variant, if the gallbladder is true intrahepatic). The dashed lines illustrate incisions or an approximate site of transection of the gallbladder.
Figure 2.

STC-1: three technical modalities (subvariants).1A) fundus-down first, circular transection of the proximal portion of the gallbladder second.1B) transection of proximal portion of the gallbladder first, body-fundus-up second.1C) visceral wall first, hepatic wall second. The arrowed lines illustrate the direction of detachment of gallbladder from the cystic plate.
Figure 3.

STC-2: two technical modalities (subvariants).2A) excision of the visceral wall, just.2B) transection of the cystic duct, excision of the visceral wall (and a part of the hepatic wall) of the gallbladder.
Figure 4.

Retrieved specimen of a resected portion of the gallbladder with approximately 350 gallstones of small, moderate and large sizes: laparoscopic 85-90% STC-1B, reconstituting type, achieved utilising Vicryl Endoloop® ligature.
Discussion
These schemes of STC are practical when a surgeon considers conversion from laparoscopic cholecystectomy to laparoscopic STC in challenging surgical circumstances. Some modalities of STC require advanced laparoscopic skills. It is a new synthesis of numerous technical details described by surgeons over the past 120 years and personal experience in laparoscopic biliary surgery – acute in the absolute majority of the cases. It has an added value to well-known terminologies.1,2,3,4,5
References
- 1.Bornman PC, Terblanche J. Subtotal cholecystectomy: for the difficult gallbladder in portal hypertension and cholecystitis. Surgery 1985; : 1–6. [PubMed] [Google Scholar]
- 2.Khan TF. Modified subtotal cholecystectomy: a procedure for the difficult gall bladder. Med J Malaysia 1992; 65–68. [PubMed] [Google Scholar]
- 3.Michalowski K, Bornman PC, Krige JE. et al. Laparoscopic subtotal cholecystectomy in patients with complicated acute cholecystitis or fibrosis. Br J Surg 1998; 904–906. [DOI] [PubMed] [Google Scholar]
- 4.Henneman D, da Costa DW, Vrouenraets BC. et al. Laparoscopic partial cholecystectomy for the difficult gallbladder: a systematic review. Surg Endosc 2013; 351–358. [DOI] [PubMed] [Google Scholar]
- 5.Strasberg SM, Pucci MJ, Brunt LM, Deziel DJ. Subtotal cholecystectomy - “fenestrating” vs “reconstituting” subtypes and the prevention of bile duct injury: definition of the optimal procedure in difficult operative conditions. J Am Coll Surg 2016; 89–96. [DOI] [PubMed] [Google Scholar]


