Abstract
Background
Pituicytoma is a rare; slow-growing primary tumour originating from the glial cells of the neurohypophysis. It was classed as a low-grade (grade I) central nervous system tumour by the World Health Organization in 2007. We present the case of a 71-year-old man with a previous history of sellar meningioma who underwent surgical resection of pituicytoma by transphenoidal hypophysectomy.
Method
We conducted a literature search using Medline EMBASE and the Cochrane Database of Systematic Reviews using the Ovid search engines. Key words searched were ‘pituitary gland’, ‘pituicytoma’, ‘neurohypophysis’. Patient records and imaging were obtained from the Royal Stoke University Hospital database.
Results
A 71-year-old man with a background of sellar meningioma 16 years previously was found to have a pituitary fossa tumour on surveillance magnetic resonance imaging. Differential diagnosis was pituitary adenoma. Endoscopic transphenoidal hypophysectomy was performed. Histology was consistent with pituicytoma. As a result of this histology from his initial tumour was re-examined and was amended to pituicytoma, indicating a recurrence.
Conclusion
Pituicytoma is a benign, slow growing lesion of the posterior pituitary. Brat et al diagnosed it as a distinct entity in 2000 and it was listed as a World Health Organization classification grade I tumour in 2007. It can be mistaken for pituitary adenoma owing to its similar clinical presentation. Complete excision of the tumour by transphenoidal hypophysectomy is an effective management for pituicytoma as demonstrated in this case.
Keywords: Hypophysectomy, Pituitary gland, Skull base, Pituitary gland, Posterior, Neurosurgery
Background
Pituicytoma is a rare, well-circumscribed, solid benign lesion of the pituitary gland. The World Health Organization established this tumour as a grade 1 central nervous system tumour in 2007.1 It presents a complex diagnostic challenge owing to its similarity both radiologically and pathologically to a pituitary adenoma. We present the case of a 71-year-old man with previous history of a suprasellar meningioma 16 years previously, who was found to have a recurrent pituitary tumour on a routine surveillance scan. This report identifies the difficulties in diagnosing pituicytoma and also addresses its tendency to recur which, in this case, was at a late stage.
Case history
A 71-year-old man had undergone a right craniotomy and excision of the suprasellar meningioma under the neurosurgical team 16 years previously. Following this procedure, he suffered a visual field defect and pan hypopituitarism for which he was taking growth hormone, thyroxine, testosterone and hydrocortisone. He presented to his routine annual follow-up appointment with otolaryngology. Initially he had been having annual surveillance magnetic resonance imaging (MRI), but this was extended to two- and four-yearly over time. As it was now 16 years after meningioma resection and he was due to have an MRI scan, it was decided that if appearances were stable then this would be his final scan.
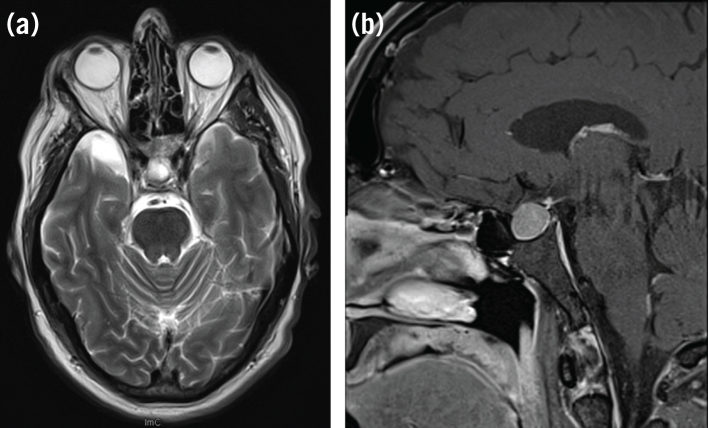
The MRI scan unexpectedly demonstrated a homogeneously enhancing sellar lesion which was extending into the suprasellar measuring approximately 14 × 13 × 15mm and creating a mild pressure effect on the optic chiasm (Fig 1a,b). The appearances were consistent with a pituitary adenoma but given the patient’s previous history of sellar meningioma a recurrence of the original lesion was also considered likely.
Figure 1.
Preoperative magnetic resonance imaging, T2-weighted. (a) Axial image demonstrating hyperintense sellar lesion. (b) T1-weighted contrast enhanced sagittal showing sellar lesion.
This case was discussed in the regional skull base multidisciplinary team meeting. Options for management were presented to the patient. These consisted of, first, a conservative approach with continued observation of this likely slow-growing tumour. The patient was aware that, given the natural history of the tumour, further growth would be expected potentially putting his remaining vision at risk. The second option would be that of an endoscopic transnasal transphenoidal resection of the pituitary tumour. The final option given was that of radiotherapy; however, in view of the tumours proximity to the optic apparatus this posed a risk of radiation-related injury. The patient opted for surgical excision. The procedure was carried out without complication and it was thought that complete resection was achieved. Postoperative recovery was uneventful.
Macroscopic histology demonstrated multiple cream and brown fragments in aggregate measuring 15mm. Microscopic histology showed tumour comprising of plump spindle cells arranged a fascicular pattern. The tumour was rich in vasculature. The tumour was found positive for vimentin, S100 protein and bcI2. It was negative for synaptophysin, chromogranin and glial fibrillary acidic protein. Ki 67 proliferation index was low 3% and thyroid transcription factor 1 (TTF-1) was strongly positive. TTF-1 positivity, together with the other tumour characteristics, led to the diagnosis of pituicytoma, a rare pituitary tumour.
As a result of these histological findings, the patient’s initial histology from 1996 was re-examined and it was found that both tumours had the same characteristics., This led to amendment of the diagnosis from meningioma to pituicytoma, a tumour that was not classified at the time of the original resection.
After 24 months of postoperative follow-up with yearly MRI scans there has been no sign of recurrence. The patient, who already suffered panhypopituitarism, continued on his preoperative medications.
Discussion
Pituicytoma is a benign, slow growing lesion of the posterior pituitary. Brat et al diagnosed it as a distinct entity in 2000.2 The WHO classification listed pituicytoma as a grade I tumour in 2007, describing it as a rare, solid, low-grade, spindle cell, glial neoplasm of adults that originates in the neurohypophysis or infundibulum, which can be intrasellar or suprasellar.1
Clinical features
Pituicytoma, like other pituitary tumours, can present with various symptoms dependant on their size and location. Suprasellar pituicytomas may present with headache and visual disturbance such as bitemporal hemianopia. Those in the sellar are more likely to suffer from endocrine symptoms such as hypopituitarism. Rarely patients present with memory loss and fatigue, or as in this case as an incidental finding.3
Differential diagnosis
This case study reveals how pituicytoma can create a diagnostic challenge owing to the non-specific nature of the tumour characteristics both clinically and radiologically, together with its rare nature. The risk of misdiagnosis is highlighted in this case report, where the pituitary lesion was thought to be either pituitary adenoma or a meningioma. Other potential differentials include granular cell tumours craniopharyngioma, pilocytic astrocytoma, germ cell tumour and metastatic tumours.4
Imaging
Radiologically pituicytomas have non-specific features that could be mistaken as other sellar pathologies particularly pituitary adenoma. Computed tomography will usually reveal an enhancing solid homogenous mass in the sellar or suprasellar region.1 Pituicytomas visualised on MRI are hypointense on T1-weighted images and hyper-intense on T2-weighted images. A 2014 study by Feng et al identifies the common appearances of all reported cases of pituicytoma on MRI and reports that we should be able to preoperatively diagnose pituicytoma based on these. These features include a mass arising in the suprasellar region, almost certainly in the midline with no attachment to dura. The mass is generally vascular, with no calcification or cystic component.5
Histology
Pituicytomas are composed of elongated spindle cells or stellate cells with oval or elongated irregular nuclei. Immunohistochemistry demonstrates staining for vimentin, S-100 protein and glial fibrillary acidic protein. Neuroendocrine markers such as synaptophysin and chromogranin are generally present. Ki67, a protein acting as a marker for cell proliferation, is low approximately 2%. TFT-1 provides a diagnostic utility in distinguishing pituicytomas and other sellar tumours such as granular cell tumour and spindle cell. Meningiomas, conversely, are TFT-1 negative.6
Management
Management of pituicytomas, for the main stay is surgical. Complete excision of the tumour by endoscopic transphenoidal hypophysectomy is an effective management for pituicytoma as demonstrated in this case. Subtotal excision of the lesion is associated with a high risk of recurrence.3 Radiotherapy or stereotactic radiotherapy have been used postoperatively but there is limited follow-up on these patients to establish its efficacy.7
Pituicytomas are rich in vasculature. This is another reason why we need to consider them in diagnosis of a pituitary lesion, as it may affect operating field. Some surgeons advocate preoperative embolisation to help reduce the bleeding and therefore provide a clearer field to achieve complete resection.7
Prognosis
Pituicytomas have no known risk of malignant transformation. They do have a strong risk of recurrence, especially if surgical resection is incomplete and, in these cases, recurrence happens soon afterwards. Our case report raises some interesting uncertainties; first with regards to long-term follow-up for these patients and second to the natural history of this tumour.
Conclusion
Pituicytomas are rare tumours of the neurohypophysis,1–4 which present a diagnostic challenge. Surgical resection by endoscopic transphenoidal hypophysectomy is the mainstay of management. It is important, however, to appreciate the vascular nature of these tumours and the complications that this presents for complete resection. It is therefore ideal to have a preoperative diagnosis of pituicytoma and, as a result, to have the option of considering preoperative embolisation. Although we are far from understanding the entire natural history of this tumour, this report provides us with some further information about its long-term behaviour and highlights the pitfalls of diagnosis.7
References
- 1.Louis DN, Ohgaki H, Wiestler OD. et al. The 2007 WHO Classification of Tumours of the Central Nervous System. Acta Neuropathol 2007; : 97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brat DJ, Scheithauer BW, Staugaitis SM. et al. Pituicytoma: a distinctive classification of tumours of the central nervous system. Acta Neuropathol 2007; : 97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kowalski RJ, Prayson RA, Mayberg MR. Pituicytoma. Ann Diagn Pathol 2004; : 290–294. [DOI] [PubMed] [Google Scholar]
- 4.Teti C, Castelletti L, Allegretti L. et al. Pituitary image: pituicytoma. Pituitary 2015; : 592–597. [DOI] [PubMed] [Google Scholar]
- 5.Feng M, Carmichael J, Bonert V. et al. Surgical management of pituicytomas: case series and comprehensive literature review. Pituitary 2014; : 399–413. [DOI] [PubMed] [Google Scholar]
- 6.Reifenberger G, Blumcke I, Pietsch T, Paulus W. Pathology and classification of tumors of the nervous system. Tonn J, Westphal M, Rutka J, Grossman SA. (). Neuro-Oncology of CNS Tumors. Berlin: Springer; 2010. . 3–72. [Google Scholar]
- 7.Pirayesh A, Buslei R, Saegar W, Fahlbusch R. Pituicytoma: overview of treatment strategies and outcome. Pituitary 2012; : 227–236. [DOI] [PubMed] [Google Scholar]