CITATION
Sweetman A, Lack L, McEvoy D. Refining the measurement of insomnia in patients with obstructive sleep apnea. J Clin Sleep Med. 2019;15(12):1717–1719.
Comorbid insomnia and sleep apnea (COMISA) is a common condition which results in additive impairments to patients’ sleep and quality of life, difficult diagnostic decisions for treating clinicians, and problems with treatment adherence and effectiveness.1 Although the co-occurrence of insomnia and obstructive sleep apnea (OSA) was first reported by Guilleminaut and colleagues in 1973,2 there was a lack of research interest in the field until two articles were published in 19993 and 2001,4 reporting that 50% of patients with OSA report clinically significant insomnia symptoms, and 43% of those with insomnia fulfill minimum diagnostic criteria for OSA. Since then, there has been an exponential increase in COMISA research; investigating the prevalence, characteristics, consequences, bidirectional relationships, and the effectiveness of singular and combined treatment approaches.1,5–7
Despite this increased interest in COMISA, there has a been a surprising lack of research investigating the validity of current measures of insomnia in the presence of co-occurring OSA. Insomnia and OSA result in many shared symptoms that can complicate the measurement and diagnosis of each disorder in the presence of the other.5 For example, a diagnosis of insomnia is indicated according to the frequency, severity, timing, and chronicity of trouble falling asleep or night time awakenings, and associated daytime functional impairments.8 However, OSA commonly manifests in similar symptoms; including perceptions of nonrestorative sleep, frequent (postapneic) night time awakenings, and daytime sleepiness, fatigue, and depressive symptoms. Additionally, the International Classification of Sleep Disorders lists “insomnia” among criteria to indicate a diagnosis of OSA in the presence of an apnea-hypopnea index of 5–15 events/h.8 These shared symptoms therefore complicate the measurement and diagnosis of COMISA, and highlight the need for research investigating the validity of current insomnia measures in patients with OSA.
The Insomnia Severity Index (ISI)9 is a concise and useful self-report measure of insomnia, which has been used in several hundred cross-sectional and treatment studies. However, there has previously been a lack of data examining the validity of the ISI in the presence of co-occurring OSA. In this issue of the Journal of Clinical Sleep Medicine, Wallace and Wohlgemuth10 report a comprehensive data-driven investigation of profiles and predictors of insomnia symptoms among 630 United States veterans with newly diagnosed OSA. This study represents an important and refreshing step toward refining the use and interpretation of the ISI to appropriately detect insomnia symptoms in the presence of OSA.
The ISI includes 7 self-report items, including three nocturnal symptoms (difficulties falling sleep, staying asleep, and waking too early; range of 0–12), and four daytime symptoms (sleep dissatisfaction, daytime functioning interference, reduced quality of life, and worry/distress; range of 0–16). These items are summed to determine a patient’s “global insomnia severity” on a scale of 0–28, with cutoff of ≥ 15 indicating at least moderate clinical insomnia. As both insomnia and OSA share multiple “daytime” symptoms,1,5 patients with OSA may score highly on the four “daytime” items of the ISI in the absence of any significant nocturnal insomnia complaint, resulting in false-positive insomnia classifications, and artifactually inflated measures of “insomnia severity.”
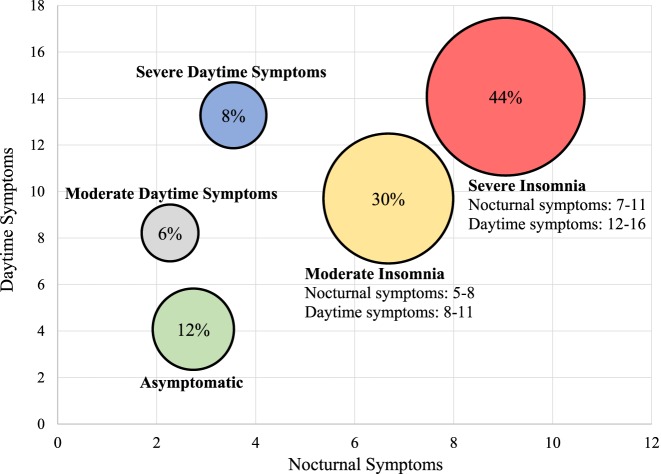
To investigate this issue, Wallace and Wohlgemuth10 performed a latent profile analysis of itemized ISI responses, and found that 74% of a sample of United States veterans with OSA were classified with “moderate” or “severe insomnia” (including both nocturnal and daytime symptoms), while the remaining 26% were divided between patients without insomnia (asymptomatic), and those with “moderate,” and “severe daytime symptoms” in the absence of nocturnal complaints (Figure 1). Importantly, Wallace and Wohlgemuth10 have identified two distinct ISI subscales among patients with OSA; indicating differential variation in nocturnal and daytime symptoms of insomnia. This paper has therefore made a critical step in using a robust dataset to highlight the potential limitations of traditional ISI scoring and interpretation in the presence of comorbid OSA, while providing an alternate and potentially more appropriate scoring system (Table 3 of Wallace and Wohlgemuth10). Further research will be required to replicate these profiles in other non-veteran population samples of patients with OSA, and to compare these ISI profiles to psychologist-determined insomnia presence and severity, and changes following treatment of the insomnia.
Figure 1. Distribution of nocturnal and daytime Insomnia Severity Index profiles in United States veterans with sleep apnea.
Distribution of insomnia profiles from Wallace and Wohlgemuth, 2019.10
The most exciting strength of this article in our view, lies in the possibility for future research and clinical use of these 5 ISI profiles in the identification and treatment of future patients with COMISA. Currently, most sleep clinics specialize in the diagnosis and treatment of OSA with continuous positive airway pressure (CPAP) therapy, while neglecting the management of insomnia. However, a large body of research suggests that poor patient acceptance and long-term adherence to CPAP therapy is partially driven by the 30% to 50% of patients with OSA who have comorbid insomnia symptoms.11–14 Understandably, patients who experience difficulties falling asleep, or prolonged nocturnal awakenings have greater difficulty in accepting and using pressurized CPAP masks throughout the night.1,4 We recently reported a randomized controlled trial in 145 patients with OSA and comorbid insomnia symptoms, which showed that treating the insomnia with cognitive and behavioral therapy for insomnia (CBT-I) improved subsequent acceptance of CPAP, and increased long-term CPAP use by 1 hour per night, compared to treatment with CPAP alone.1,15
Therefore, the adoption of psychological services directed toward the identification and treatment of insomnia will assist sleep clinics in improving treatment outcomes for patients with OSA. By using the brief ISI questionnaire9 alongside the refined cutoffs reported by Wallace and Wohlgemuth (Figure 1), it will be possible for sleep clinics around the world to efficiently identify the 30% to 50% of patients with OSA and clinically significant moderate and severe insomnia profiles who are at the highest risk of poor CPAP outcomes. As suggested by Wallace and Wohlgemuth, a more nuanced approach to the management of insomnia based on their different insomnia profiles (eg, to refer patients with OSA with “moderate” and “severe” insomnia profiles for CBT-I before, or concurrently with CPAP) may improve patient wellbeing and increase subsequent CPAP acceptance and use.16
DISCLOSURE STATEMENT
All authors have approved this manuscript. The authors report no conflicts of interest.
REFERENCES
- 1.Sweetman A, Lack LC, Catcheside PG, et al. Developing a successful treatment for co-morbid insomnia and sleep apnea. Sleep Med. Rev. 2017;33:28–38. doi: 10.1016/j.smrv.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 2.Guilleminault C, Eldridge FL, Dement WC. Insomnia with sleep apnea: a new syndrome. Science. 1973;18:856–858. doi: 10.1126/science.181.4102.856. [DOI] [PubMed] [Google Scholar]
- 3.Lichstein KL, Riedel BW, Lester KW, Aguillard RN. Occult sleep apnea in a recruited sample of older adults with insomnia. J Consult Clin Psychol. 1999;67(3):405–410. doi: 10.1037//0022-006x.67.3.405. [DOI] [PubMed] [Google Scholar]
- 4.Krakow B, Melendrez D, Ferreira E, et al. Prevalence of insomnia symptoms in patients with sleep-disordered breathing. Chest. 2001;120(6):1923–1929. doi: 10.1378/chest.120.6.1923. [DOI] [PubMed] [Google Scholar]
- 5.Luyster FS, Buysse DJ, Strollo PJ. Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6(2):196–204. [PMC free article] [PubMed] [Google Scholar]
- 6.Björnsdóttir E, Janson C, Sigurdsson JF, et al. Symptoms of insomnia among patients with obstructive sleep apnea before and after two years of positive airway pressure treatment. Sleep. 2013;36(12):1901–1909. doi: 10.5665/sleep.3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crawford MR, Turner AD, Wyatt JK, Fogg LF, Ong JC. Evaluating the treatment of obstructive sleep apnea comorbid with insomnia disorder using an incomplete factorial design. Contemp Clin Trials. 2016;47:146–152. doi: 10.1016/j.cct.2015.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Academy of Sleep Medicine . 3rd ed. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 9.Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 10.Wallace DM, Wohlgemuth WK. Predictors of Insomnia Severity Index profiles in United States veterans with obstructive sleep apnea. J Clin Sleep Med. 2019;15(12):1827–1837. doi: 10.5664/jcsm.8094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wallace DM, Sawyer AM, Shafazand S. Comorbid insomnia symptoms predict lower 6-month adherence to CPAP in US veterans with obstructive sleep apnea. Sleep Breath. 2018;22(1):5–15. doi: 10.1007/s11325-017-1605-3. [DOI] [PubMed] [Google Scholar]
- 12.Pieh C, Bach M, Popp R, Jara C, Crönlein T, Hajak G, Geisler P. Insomnia symptoms influence CPAP compliance. Sleep Breath. 2012;17(1):99–104. doi: 10.1007/s11325-012-0655-9. [DOI] [PubMed] [Google Scholar]
- 13.Wickwire EM, Smith MT, Birnbaum S, Collop NA. Sleep maintenance insomnia complaints predict poor CPAP adherence: a clinical case series. Sleep Med. 2010;11(8):772–776. doi: 10.1016/j.sleep.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 14.Philip P, Bioulac S, Altena E, et al. Specific insomnia symptoms and self-efficacy explain CPAP compliance in a sample of OSAS patients. PLoS One. 2018;13(4):e0195343. doi: 10.1371/journal.pone.0195343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sweetman A, Lack L, Catcheside PG, et al. Cognitive and behavioral therapy for insomnia increases the use of continuous positive airway pressure therapy in obstructive sleep apnea participants with co-morbid insomnia: a randomized clinical trial. Sleep. doi: 10.1093/sleep/zsz178. 2019 Aug 12. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 16.Lack L, Sweetman A. Diagnosis and treatment of insomnia comorbid with obstructive sleep apnea. Sleep Med Clin. 2016;11(3):379–388. doi: 10.1016/j.jsmc.2016.05.006. [DOI] [PubMed] [Google Scholar]