Abstract
Background
To date, many attempts are employed to increase the regenerative potential of stem cells. In this study, we evaluated the hypothesis of whether an autophagy modulation could alter differentiation potency of CD146+ cells into mature pericyte, endothelial, and cardiomyocyte lineage.
Methods
In this study, CD146+cells were enriched from the human bone marrow aspirates and trans-differentiated into mature endothelial cells, pericytes, and cardiomyocytes after exposure to autophagy stimulator (50-μM Met)/inhibitor (15-μM HCQ). The protein levels of autophagy proteins were monitored by western blotting. NO content was measured using the Griess assay. Using real-time PCR assay and western blotting, we monitored the lineage protein and gene levels. Pro-inflammatory cytokine and angiocrine factors were measured by ELISA. The fatty acid change was determined by gas chromatography. We also measured exosome secretion capacity by measuring AChE activity and real-time PCR assay.
Result
Data revealed the modulation of autophagy factors, Beclin-1, P62, and LC3 II/I ratio in differentiating CD146+ cells after exposure to Met and HCQ (p < 0.05). The inhibition of autophagy increased NO content compared to the Met-treated cells (p < 0.05). Real-time PCR analysis showed that the treatment of CD146+ cells with autophagy modulators altered the expression of VE-cadherin, cTnI, and α-SMA (p < 0.05). Met increased the expression of VE-cadherin, α-SMA, and cTnI compared to the HCQ-treated cells (p < 0.05) while western blotting revealed the protein synthesis of all lineage-specific proteins under the stimulation and inhibition of autophagy. None statistically significant differences were found in the levels of Tie-1, Tie-2, VEGFR-1, and VEGFR-2 after autophagy modulation. Fatty acid profile analysis revealed the increase of unsaturated fatty acids after exposure to HCQ (p < 0.05). The treatment of cells with HCQ increased the levels of TNF-α and IL-6 compared to the Met-treated cells. Data revealed the increase of exosome biogenesis and secretion to the supernatant in cells treated with HCQ compared to the Met groups (p < 0.05).
Conclusions
In summary, autophagy modulation could alter differentiation potency of CD146+cells which is important in cardiac regeneration.
Keywords: Human bone marrow CD146+ cells, Autophagy modulation, Nitrosative assay, Lineage-specific differentiation, Exosome activity
Background
According to WHO statistics, coronary heart disease is the main cause of human mortality in the clinical setting. Despite current advances in the decrease mortality rate in patients with coronary heart disease, further attempts and novel approaches are highly needed for the alleviation of cardiac tissue injuries [1]. Up to date, the advent of cell therapy and regenerative medicine is touted as the modern therapeutic procedures in the field of cardiovascular disease [2]. Hitherto, different types of stem cells, including embryonic stem cells, cardiac progenitor cells, mesenchymal stem cells, endothelial progenitor cells, and induced pluripotent stem cells have been used in the clinical setting. Recently, it has been documented that PCs have great regenerative potential in limb ischemia and myocardial infarction [3, 4]. PCs are a specific population that concentrically wraps vascular ECs [5]. According to recent data, a fraction of PCs exhibits extreme proliferation, and clonogenic capacity with a magnificent stemness feature, pleiotropic properties, and angiogenic potency [6]. Based on molecular analyses, multiple PC populations have the potential to express OCT4, NANOG, SOX2, CD146, alkaline phosphatase, CD44, CD73, CD90, CD105, etc. [7]. The ability of PCs to express CD146 (melanoma cell adhesion molecules) was shown before which contributes to highly proliferative rate differentiation capacity [8]. According to previously published experiments, cardiac tissue encompasses a large number of CD146+ cells inside myocardium with a trilineage potential capacity to rescue angiogenesis and replace damaged myocardium [9]. Cardiac PCs are potent to release tissue metalloproteinases to re-model the fibrous matrix in the periphery of the injured sites [10]. These features make PCs as an appropriate cell source for the alleviation of cardiac tissue injuries.
Autophagy is an intricate intracellular process that facilitates the degradation of impaired proteins and the removal of dysfunctional organelles by fusion to lysosomes and releases out of the cell. In addition to the integrity of autophagy to the bioactivity of the host cells, novel data highlighted the interaction and interplay of the autophagy signaling pathway with another signaling cascade reciprocally [11]. Scientific literature demonstrated that autophagy functions in the developmental and maturation of B lymphocytes, adipocytes, osteoblasts, keratinocytes, and erythrocytes [12–16]. Interestingly, it was revealed that autophagy inhibition resulted in ROS accumulation in hematopoietic stem cells and self-renewal capacity loss [17]. Zhang et al. showed that the promotion of autophagy in C-kit+cardiac progenitor cells, accelerated differentiation toward mature CMs after inhibition of the fibroblast growth factor signaling pathway, showing the critical role of autophagy in differentiation properties of stem cells [18, 19].
Despite PCs’ significance in hemostasis, angiogenesis, vasculogenesis, differentiation, and maturation into several cardiac cells, there is no information related to the modulation of autophagy on the differentiation potential of immature PCs. In this study, we further evaluated the hypothesis, whether an autophagy modulation could alter differentiation potency of CD146+ cells into mature PCs, ECs, and CMs.
Methods
Mononuclear cell isolation and expansion protocol
Bone marrow samples of healthy volunteers, ranging from 3 to 10 years old, referred to children hospital, an affiliated hospital to Tabriz University of Medical Sciences, were enrolled in the present study. Informed consent was obtained from the parents/legally authorized representatives of participants. Children who suspected of malignant diseases and clinical screening were referred to routine bone marrow aspiration procedures at the posterior superior iliac crest. In the current experiment, we selected the samples without any neoplastic changes, genetic, and inflammatory diseases. Briefly, bone marrow aspirates (2 ml) were used for the isolation of MNCs. To inhibit the coagulation, a 5000-IU/mL heparin was used. Blood samples were diluted with PBS (1:1 v/v) and overlaid on the same volume of Ficoll-Hypaque solution (Cat No: GE17-1440-02, Sigma-Aldrich). The samples were centrifuged at 400g for 25 min at 4 °C. MNCs at the interface fraction between the plasma and the Ficoll solution were carefully collected, washed with PBS, and re-suspended in DMEM/LG (Cat No: 31600083, Gibco, USA) culture medium. The media were supplemented with %10 FBS (Cat No: 10270, Invitrogen) and replaced every 3–4 days. By using 0.25% Trypsin-EDTA (Cat No: 25200056, Gibco, USA) solution, cells were detached.
Enrichment of CD146+ cells using magnetic-activated cell sorting
In the current study, we aimed to isolate CD146+ cells for different analyses. For this purpose, expanded bone marrow MNCs were detached using the enzymatic solution and subjected to MACS. In short, the MNCs were blocked by using 1% bovine serum albumin for 20–30 min and incubated with mouse anti-human CD146 microbead (order no: 130-093-596, Miltenyi Biotec, Germany) for 30 min at 4 °C. The cell suspensions were passed over the MACS LS column (order no: 130-042-401, Miltenyi Biotec).
Cell survival assay
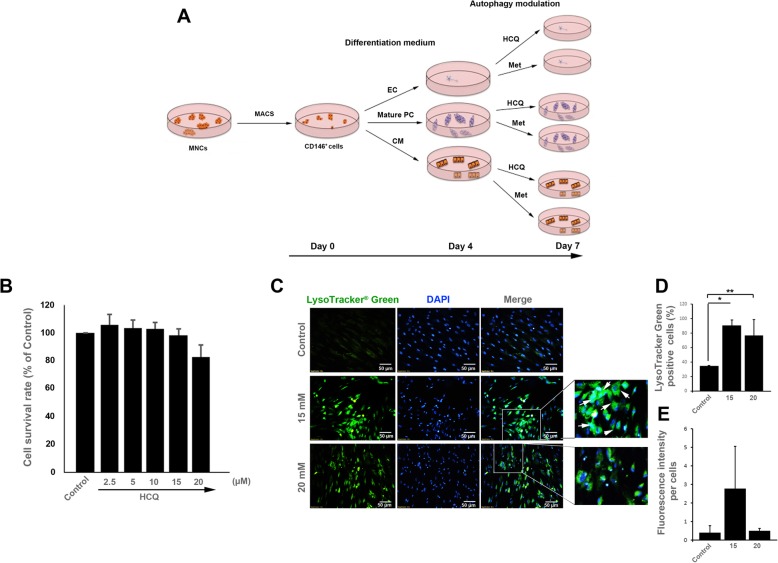
This study aimed to evaluate the effect of autophagy modulation on the differentiation capacity of CD146+ cells toward different lineages. In this regard, we performed MTT assay to select the maximum dose of autophagy blocker, HCQ, with the lowest toxic effect on CD146+ cells. In this regard, CD146+ cells were plated (2 × 104/well) in each well of 96-well plates (SPL). Cells were treated with different concentrations of HCQ (Cat No: H0915, Sigma-Aldrich) including 2.5, 5, 10, 15, and 20 μM for 72 h [20]. Thereafter, a 30-μl MTT solution was added to each well and incubated at 37 °C for 2 h followed by the addition of 200-μl dimethyl sulfoxide (Merck, Germany). The optical density was read at 620 nm by using a microplate reader (BioTek). The cell survival rate was expressed as a percentage relative to the non-treated control CD146+ cells. To stimulate autophagy, CD146+ cells were treated with a 50-mM Met (as a gift from Osveh Pharmaceutical Inc., Tehran, Iran) [21].
LysoTracker assay
To assess the inhibitory effect of HCQ on the late stage of autophagy, we performed LysoTracker staining. To this end, MNCs were seeded at a density of 104 cells per well in 8-well Chambered Cell Culture Slide (SPL) and incubated at 37 °C with 5% CO2 and 95% relative humidity. After 24 h, cells were treated with 15- and 20-μM HCQ for 72 h. After completion of autophagy modulation, cells were washed with cold PBS, 50 nM LysoTracker Green (cat no: L7526, Sigma-Aldrich) added to each well and kept for 30 min. After three times of washing with PBS, cells were stained with a 1-μg/ml DAPI (Sigma-Aldrich) solution 30 s to stain the background. The cells harboring intracellular vacuoles were visualized by using immunofluorescence microscopy (Model: BX41, Olympus).
Cell differentiation and autophagy modulation
In this study, we explored the effect of autophagy modulation on the differentiation potency of CD146+ cells in vitro. Purified CD146+ cells were cultured in the endothelium (Cat No: C-22111, Promocell, Germany), pericyte (Cat No: C-28040, Promocell, Germany), and cardiomyocyte (Cat No: 05010, STEMCELL, USA) differentiation media. Cells were maintained for 7 days in differentiation media supplemented with 2% FBS and 1% Pen-Strep solutions. On day 4, autophagy was blocked/stimulated using 15-μM HCQ and 50-μM Met (Cat No: Osveh Pharmaceutical Inc., Iran) as previously described (Fig. 1a) [21].
Fig. 1.
Schematic illustration of study design (a). MTT assay (b); Measuring CD146+ cell survival rate by MTT assay after exposure to different doses of HCQ (n = 16). Our data illustrated that 15-μM HCQ is the optimum dose for autophagy inhibition in CD146+ cells with a minimal toxic effect. LysoTracker Green staining (c–e). Fluorescence microscopy imaging confirmed that 15-μM HCQ inhibited autophagic flux (c, d (n = 100 cells) and e (n = 100 cells)). Data are expressed as mean ± SD. One-way ANOVA and Tukey post hoc test. *p < 0.05; **p < 0.01
Western blotting
Western blot analysis was done to evaluate and confirm the modulation of autophagy proteins in PC-, CM-, and EC-like cells after the modulation of autophagy. On day 7, cells were collected and lysed in ice-cold cell lysis buffer solution (NaCl, NP-40, and Tris–HCl) enriched with cocktail enzyme inhibitors. Then, the samples were sonicated at a resonance of 50 Hz for 2 min. The homogenates were centrifuged at 14,000 g for 20 min. By using the Picodrop spectrophotometer system (Model No: PICOPET01, Serial No. 000212/1), total protein content was determined in the supernatant. In this study, 100-μg proteins from each sample were resolved by 12% SDS-PAGE method and transferred to PVDF membrane. The membranes were incubated in antibody solution (LC3: Cat No: ab51520, Abcam; P62: Cat No: SC-10117, Santa Cruz Biotechnology, Inc.; Beclin-1: Cat No: SC-48341, Santa Cruz Biotechnology, Inc.; α-actinin-2: Cat No: SC-130928, Santa Cruz Biotechnology, Inc.; α-SMA: Cat No: SC-53015, Santa Cruz Biotechnology, Inc.; vWF: Cat No: SC-365712, Santa Cruz Biotechnology, Inc.; ERK 1/2: Cat No: SC-292838, Santa Cruz Biotechnology, Inc.; pERK 1/2: Cat No: SC-16981-R, Santa Cruz Biotechnology, Inc.) at 4 °C overnight. Then, the membranes were incubated with secondary HRP-conjugated anti-IgG antibody (Cat No: sc-2357, Santa Cruz Biotechnology, Inc.) for 1 h at room temperature. The immunoreactive blots were detected using the ECL plus solution (BioRad). Immunoreactive bands were analyzed with ImageJ software (ver.1.44p, NIH). GAPDH (Cat No: sc-32233, Santa Cruz Biotechnology, Inc.) was used as an internal control group. This experiment was performed in triplicate.
NO assay
The level of NO was measured in differentiating cells after autophagy stimulation or inhibition using the Griess method. In this method, NO is converted to nitrite and nitrite produces nitrous acid in an acidic state. In the next step, the addition of sulfanilamide to a solution containing nitrous acid forms a diazonium salt and in the presence of n-(1-naphthyl) ethylenediamine dihydrochloride (C12H16Cl2N2) generates an azo dye. Briefly, an initial number of 1 × 104 cells was seeded in each well of 96-well plates (SPL). Seventy-two hours after the addition of autophagy blocker/stimulator under differentiation condition, 200 μl supernatant of each sample was mixed with 20-μl Griess A and maintained for 10 min followed by the addition of 20 μl of Griess B solution. After 2 min, the optical density of each sample was read at 450 nm using a microplate reader (BioTek) and levels of NO calculated based on sodium nitrite standard curve. Levels of NO were expressed as nM.
Measuring endothelial RTKs and pro-inflammatory cytokines
To determine the levels of inflammatory cytokines and RTKs during CD146+ differentiation into different lineages, we measured the levels of IL-6 (Cat No: DY206, R&D) and TNF-α (Cat No: DY210, R&D) in the supernatants by using ELISA according to manufacturer’s recommendation. The angiogenic status of cells was further assessed by monitoring RTK protein levels such as VEGFR-1 (Cat No: ab32152, Abcam), VEGFR-2 (Cat No: ab39256, Abcam), Tie-1 (Cat No: ab27851, Abcam), Tie-2 (Cat No: ab24859, Abcam), and Ang-1 (Cat No: 130-06, Peprotech) by ELISA assay provided by our group [22]. The final absorbance was recorded at 450 nm using a microplate reader (BioTek, USA). The concentration of each factor either in autophagy stimulated/inhibited and groups is calculated based on comparison to corresponding standard curves.
Measuring fatty acid composition by GC
The lipid profile was analyzed by the GC technique as previously described [23]. The cellular lipid was extracted by using the Bligh-Dyer method and further esterified with methanol during acetyl chloride catalysis [24]. Methyl esters were introduced to the analyzing machine to determine the fatty acid composition. The fatty acid methyl ester derivatives were separated on a Teknokroma TR CN100 column (60 × 0.25 mm) using a Buck Scientific gas chromatograph (Model 610, SRI Instruments, Torrance, USA). Tridecanoic acid (13:0) was exploited as the internal control. Peak retention times in each group were compared to the peak of standards.
Assessing paracrine potency of CD146+ cells under the modulation of autophagy
To this end, we monitored AChE touted as an exosome marker protein. In brief, supernatants were discarded after the completion of the experimental procedure and replaced by incubation with culture medium containing 1% exosome-free FBS (Invitrogen) for 48 h. Thereafter, a 20-μl culture medium was mixed with 500-μl buffer solution containing pyrophosphate (75 mM) and potassium hexacyanoferrate (2 mM) (Cat No: BXC0801, biorexfars) for 5 min at RT. Finally, a 100-μl s-butyrylthiocholine iodide was added to each sample and absorbance read at 405 nm during three different intervals. Finally, the choline esterase activity was calculated by the following formula: activity (U/l) = ∆Abs/min × 65,800.
RT-PCR assay
After a 7-day incubation with differentiation media and autophagy modulation, the total RNAs were isolated from each sample. To this end, cells were trypsinized and were washed with PBS. Then, a 1-ml Ambion TRIzol buffer (Cat No: 15596-026, Invitrogen, USA) was added to cell pellets and agitated rigidly to homogenize the samples. Next, 200-μl chloroform (Merck, Darmstadt, Germany) was added and samples centrifuged at 4 °C at 12000 rpm for 20 min. Next, the equal volume of the upper phase containing RNA was mixed with isopropanol (Sigma-Aldrich) and incubated at 4 °C for 15 min. After centrifugation, the supernatant was discarded and the pellet was dissolved in 1-ml ethanol (75% v/v) solution. Finally, the total RNA was dissolved in 50-μl DEPC-treated water and samples’ concentration determined by a Nanodrop system (Thermo Scientific). To exclude a possible genomic DNA contamination, RNA solutions were incubated with the DNase1 kit (Cat No: en0521, FermenTaz). Before real-time PCR analysis, purified RNAs were reversely transcribed using a cDNA synthesis kit (Cat No: YT4500). The qRT-PCR reaction was performed by using 1-μl cDNA, 5-μl SYBR premix Ex Taq kit (Cat No: RR820L, TaKaRa), 0.4 μl candidate gene primers, and 3.2-μl DEPC water. The qRT-PCR was performed by a Rotor-Gene Corbett System 6000. The raw data was analyzed by a convenient Pfaffl method with normalization to housekeeping gene β2-microglobulin (β2M). The experiment was conducted in triplicate. The sequences of all primers for human VE-cadherin, cTnI, α-SMA, and TPBG were outlined in Table 1.
Table 1.
The list of primers designed by Perl Primer software
| Gene | Forward | Reverse | Tm (°C) |
|---|---|---|---|
| α-SMA | 5′-GTCCACCGCAAATGCTTCTA-3′ | 5′-AAACACATAGGTAACGAGTCAG-3′ | 57 |
| VE-cadherin | 5′-ACCCAAGATGTGGCCTTTAG-3′ | 5′-GTGACAACAGCGAGGTGTAA-3′ | 60 |
| Troponin I | 5′-TTTGACCTTCGAGGCAAGTTT-3′ | 5′-CCCGGTTTTCCTTCTCGGTG-3′ | 57 |
| β2M | 5′-AGGCTATCCAGCGTACTCC-3′ | 5′-ATGTCGGATGGATGAAACCC-3′ | 58 |
| CD63 | 5′-TCCTGAGTCAGACCATAATCC-3′ | 5′-GATGGCAAACGTGATCATAAG-3′ | 63 |
| ALIX | 5′-CTGGAAGGATGCTTTCGATAAAGG-3′ | 5′-AGGCTGCACAATTGAACAACAC-3′ | 63 |
| Rab11 | 5′-CCTCAGCCTCTACGAAGCAAA-3′ | 5′-CCGGAAGTTGATCTCCTCCTG-3′ | 59 |
| Rab27a | 5′-AGAGGAGGAAGCCATAGCAC-3′ | 5′-CATGACCATTTGATCGCACCAC-3′ | 59 |
| Rab27b | 5′-GGAACTGGCTGACAAATATGG-3’ | 5′-CAGTATCAGGGATTTGTGTCTT-3′ | 59 |
Statistical analysis
In this study, data are expressed as mean ± SD. To find statistically significant differences between the groups, we performed a one-way ANOVA test. P < 0.05 was considered statistically significant. Three sets of experiments were at least performed for different analyses unless mentioned.
Results
HCQ dose selection for the subsequent analyses
The optimum dosage of HCQ to inhibit autophagy was calculated based on the MTT assay. CD146+ cells were exposed to different doses of HCQ ranging from 2.5 to 20 μM for 3 days (Fig. 1b). According to our data, a 3-day incubation of CD146+ cells with 2.5-, 5-, and 10-μM HCQ had no cytotoxic effect on cell survival rate. Data demonstrated that a slight increase in the cell survival rate from groups 2.5-, 5-, and 10-μM HCQ. The addition of 15- and 20-μM HCQ to the culture medium decreased cell viability to 98.3 and 82.7%, respectively, showing dose-dependent cytotoxicity of HCQ on the CD146+ cells (Fig. 1b). Consistent with the previous experiments, we selected 15-μM HCQ as the highest dose without toxic effect for other analyses [25].
HCQ treatment showed lysosomal accumulation inside the CD146+ cells
To further confirm the suppression of autophagy in CD146+ cells, the LysoTracker staining was done (Fig. 1c–e). According to results, the fluorescence intensity and the number of LysoTracker+ cells were increased in cells from 15-μM HCQ compared to the control non-treated cells (p < 0.05, Fig. 1c–e). We also found that the number of cells with accumulated lysosomes was increased in the 20-μM HCQ group compared to the control cells (p < 0.05, Fig. 1c–e). However, these effects were less compared to the 15-μM HCQ. We found a non-significant difference between groups 15- and 20-μM HCQ. These data showed that a 3-day incubation of CD146+ cells with HCQ at doses 15- and 20-μM HCQ could efficiently block autophagy efflux and accumulate lysosomes inside the CD146+ stem cells. According to data from MTT and IF assays, we selected 15-μM HCQ for subsequent analyses.
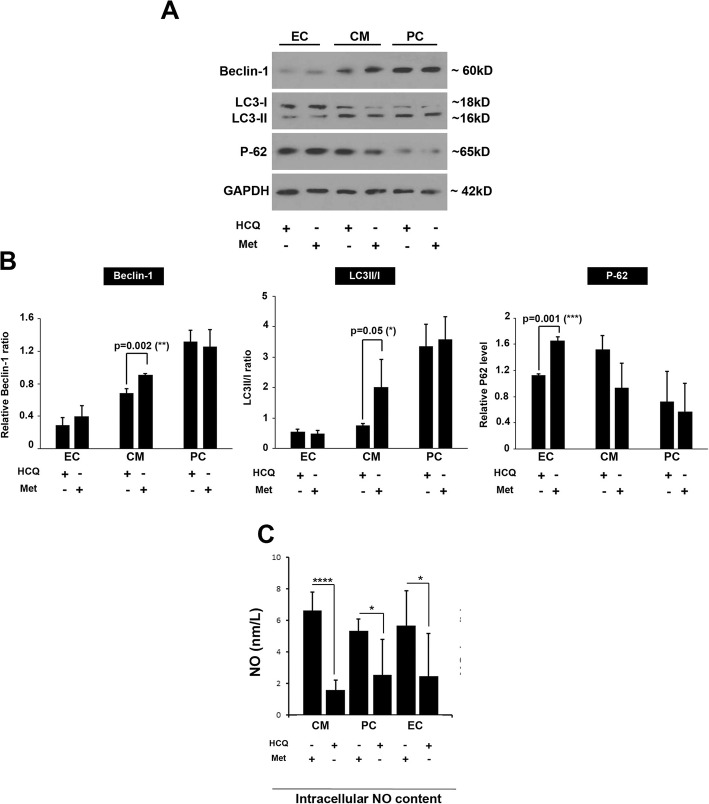
HCQ and Met changed protein levels of autophagy-related factors
Following the completion of the experimental protocol, we performed western blotting to measure protein levels of Beclin-1, P62, and LC3II/I ratio (Fig. 2a, b). We showed that the basal levels of each autophagy factor were different in CD146+ cells after being-exposed to different differentiation media. The basal level of Beclin-1 was low in CD146+ cells differentiating toward endothelial lineage compared to the other groups. In support of this notion, we found that the P62 was also low in the PC group compared to the cells exposed to CM and EC differentiation media (Fig. 2a, b). According to our data, the treatment of CD146+ cells with the Met and endothelial differentiation medium significantly increased protein levels of P62 compared to the group treated with the HCQ group (p < 0.05). No statistically significant differences were found between the two groups for the Beclin-1 level and LC3II/I ratio (p > 0.05, Fig. 2a, b). The incubation of CD146+ cells with Met and CM differentiation medium increased Beclin-1 and LC3II/I ratio compared to the HCQ-treated cells (p < 0.05). However, the levels of P62 were decreased in Met-treated cells but did not reach statistically significant levels. We found a statistically non-significant difference in the protein levels of Beclin-1, P62, and LC3II/I ratio in CD146+ cells incubated with PC differentiation medium enriched with Met or HCQ (Fig. 2a, b). According to our data, one could hypothesize that the application of autophagy modulators (Met and HCQ) in CD146+ cells committed to different lineages changes the protein levels of autophagy-related proteins differently, showing possibly different basal levels of autophagy function in different lineages.
Fig. 2.
Western blotting and NO assay (a–c). Measuring protein levels of autophagy-related factors by western blotting (a, b; n = 3). Detecting NO levels by Griess assay (c; n = 16). Data are expressed as mean ± SD. One-way ANOVA and Tukey post hoc test. *p < 0.05; ****p < 0.0001
NO production was increased after autophagy stimulation
To monitor the level of NO production in differentiation cells subjected to autophagy modulation, we performed a Griess assay. Results indicated that NO content was diminished by autophagy suppression via 15-μM HCQ compared to control-matched Met groups after incubation with CM, PC, and EC differentiation medium (p < 0.05, Fig. 2c). Overall, NO production was significantly hindered by autophagy inhibition while the stimulation of autophagy increases the NO production especially in CD146+ cells exposed to PC and EC differentiation media, showing NO production depends on the cell lineage.
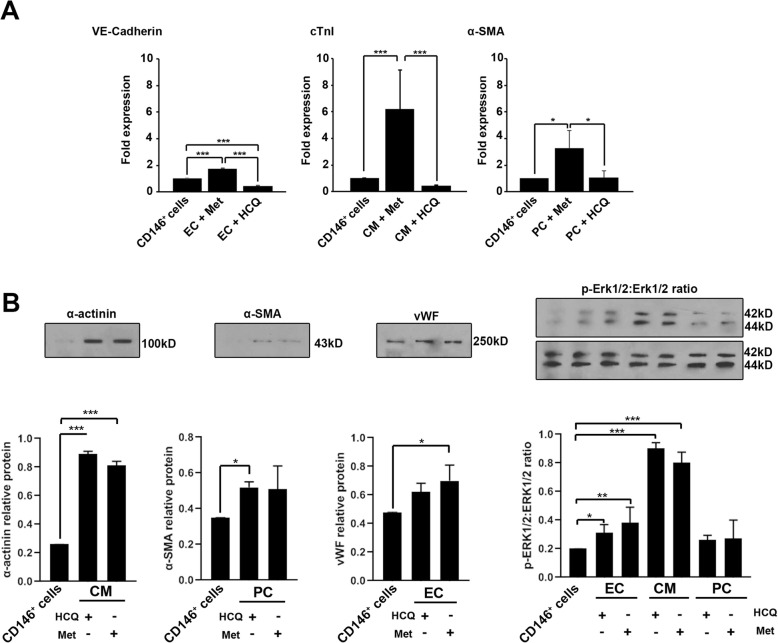
HCQ and Met altered levels of differentiation-related proteins
We performed western blotting and real-time PCR analysis to assess the differentiation potential of CD146+ cells toward different lineages (Fig. 3a, b). Real-time PCR analysis showed that the treatment of CD146+ cells with autophagy modulators altered the expression of VE-cadherin, cTnI, and α-SMA. According to our data, the incubation of CD146+ cells with Met significantly increased the expression of VE-cadherin, cTnI, and α-SMA genes compared to the control and HCQ groups (p < 0.05, Fig. 3a). We found a significant inhibition of VE-cadherin in the group received HCQ compared to the control CD146+ cells (p < 0.001, Fig. 3a) while non-significant differences were found in the mRNA levels of both cTnI and α-SMA between the HCQ and control groups. These data demonstrated that the stimulation of autophagy signaling in CD146+ cells upon treatment with differentiation medium could increase differentiation potential toward multiple lineages. Western blotting showed that the modulation of CD146+ cells with autophagy modulators (either Met or HCQ) could promote lineage-specific protein synthesis compared to the control of CD146+ cells (p < 0.05, Fig. 3b). The protein analysis of VE-cadherin showed a significant increase in differentiating cells that committed endothelial lineage after exposure to the HCQ and Met. Of note, protein levels of α-SMA and vWF increased in CD146+ cells committed to PC and CM differentiation upon treatment with Met and HCQ. The levels of α-SMA and vWF reached significant levels in the differentiation medium enriched with Met and HCQ, respectively (Fig. 3b). Data revealed the significant phosphorylation of Erk1/2 in all cells exposed to differentiation media upon autophagy stimulation and inhibition (p < 0.05, Fig. 3b). Despite a slight increase in Erk1/2 phosphorylation of CD146+ cells exposed to PC lineage, these changes did not reach statistically significant differences.
Fig. 3.
Real-time PCR assay and western blotting (a, b). Measuring the effect of autophagy modulation on the differentiation capacity of human bone marrow CD146+ cells via real-time PCR assay (a; n = 3). Data demonstrated that autophagy stimulation increased the mRNA level of endothelial VE-cadherin, cardiac cTnI, and pericyte α-SMA after autophagy stimulation compared to non-treated CD146+cells (a). Western blotting assays were used to monitor lineage protein levels after autophagy modulation (b; n = 3). One-way ANOVA and Tukey post hoc test. *p < 0.05; **p < 0.01; ***p < 0.001; and ****p < 0.0001
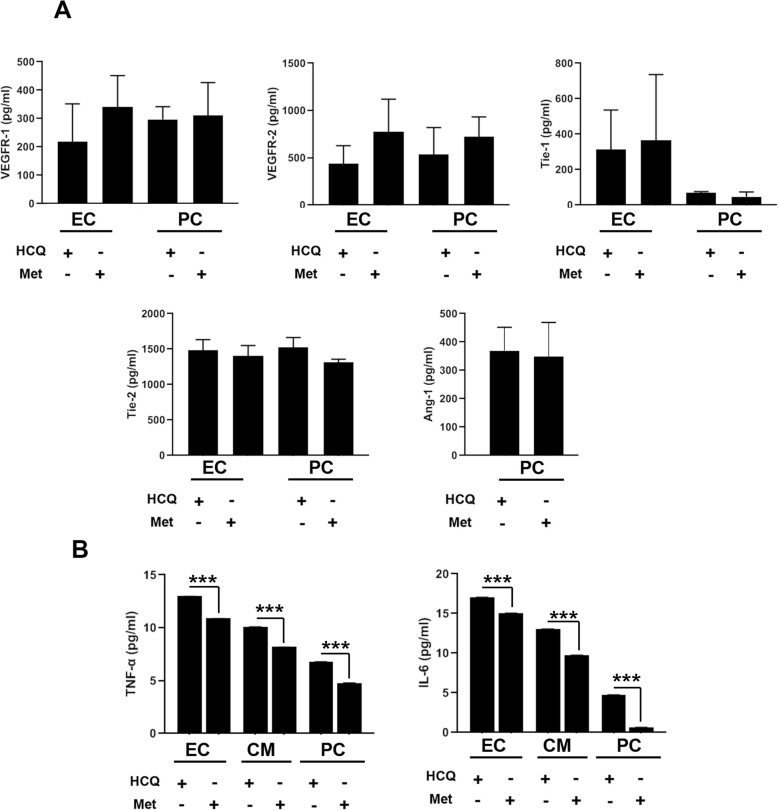
Autophagy modulation effect on RTK levels and pro-inflammatory cytokines
Cell surface RTK levels, VEGFR-1, VEGFR-2, Tie-1, Tie-2, and ligand Ang-1 were monitored by using ELISA. We found an increase in protein level for Tie-1, Tie-2, VEGFR-1, and VEGFR-2 under autophagy stimulation compared to the condition cells received HCQ (Fig. 4a). Despite slight changes, the protein levels of RTKs and Ang-1 did not reach statistically significant differences. Also, it seems that autophagy modulation for 72 h could not alter the potency of CD146+ cells to synthesize Ang-1 (Fig. 4a). To the assessment of the correlation between autophagy and the inflammatory process, we measured TNF-α and IL-6 (Fig. 4b). Data showed that autophagy induction by 50-μM Met diminished either TNF-α or IL-6 levels in CD146+ cells incubated in EC and PC and CM differentiation media compared to the control-matched group exposed to the 15-μM HCQ (Fig. 4b). According to data, we found that the CD146+ cells had a magnificent TNF-α and IL-6 synthesis capacity when committed to the endothelial lineage rather than PC and CM destination (Fig. 4b). Data showed that the promotion of autophagy by Met, although it did not, changes the RTKs and Ang-1 levels but could affect pro-inflammatory status via the reduction of TNF-α and IL-6 cytokines.
Fig. 4.
ELISA assay (a, b). Measuring protein levels of VEGFR-1, VEGFR-2, and Tie-1, Tie-2, and Ang-1 after autophagy modulation (a; n = 3). It seems that autophagy stimulation could increase differentiation potential, but these changes did not reach statistically significant levels. The effect of autophagy stimulation/inhibition on the inflammatory status of differentiating CD146+ cells (b; n = 3). It seems that autophagy stimulation could decrease significantly the production of TNF-α and IL-6 after treatment with 50-μM Met. Student t test. ***p < 0.001
Fatty acid profile was changed during the autophagy modulation in differentiating CD146+ cells
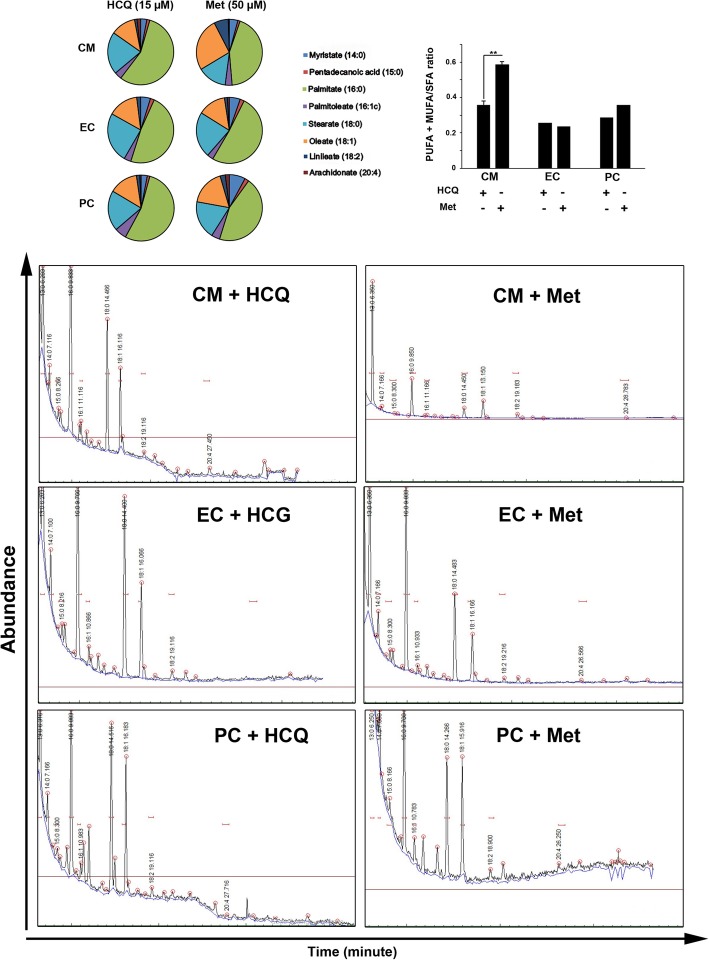
In the current experiment, we measured the level of PUFA (Linoleate18:2 and Arachidonate 20:4), MUFA (Palmitoleate 16:1, Oleate 18:1), and SFA acids (Myristate 14:0, Pentadecanoic acid 15:0 and Palmitate 16:0 and Stearate 18:0) by GC analysis to monitor the ratio of unsaturated and saturate fatty acids in CD146+ cells exposed to autophagy stimulation and inhibition (Fig. 5). Data showed the increase of PUFA +MUFA: SFA ratio in CD146+ cells after the inhibition of autophagy by HCQ. We found a 2.53-fold increase in the fatty acid ratio in the CM group exposed to 50-μM Met compared to HCQ-treated CM during differentiation (p < 0.05, Fig. 5). Similar to the CM group, a 1.24-fold increase was found in the PUFA + MUFA/SFA ratio in PC after exposure to the Met in comparison with the HCQ. In contrast, we noted that the exposure of CD146+ cells to endothelial medium enrich with Met decreased this ratio (Fig. 5). Therefore, the application of autophagy modulators during differentiation of CD146+ cells toward different lineages such as EC, PC, and CM could alter the cellular fatty acid composition.
Fig. 5.
Fatty acid analysis. Gas chromatography fatty acid analysis indicated that the ratio of PUFA + MUFA/SFA was increased after autophagy stimulation in the CM group (n = 3). Student t test. **p < 0.01
Autophagy modulation altered the exosome biogenesis
To further assess the modulation of autophagy on exosome biogenesis, AChE activity and the expression of genes including CD63, ALIX, Rab11, Rab27a, and Rab27b were measured. Data revealed the increase of exosome secretion to the supernatant in cells treated with HCQ compared to the Met groups (Fig. 6a). These data demonstrated that the treatment of CD146+ cells with autophagy blockers, 15-μM HCQ, increases exosome abscission and activates paracrine activity. A similar pattern was found in the expression of CD63, ALIX, Rab11, Rab27a, and Rab27b (Fig. 6b). Despite induction in molecular pathways in exosome biogenesis, localization, and abscission of HCQ-treated cells; however, these changes did not reach statistically significant changes.
Fig. 6.
Exosome biogenesis assay (a and b). Measuring AChE in supernatant cell culture (a). Data showed that autophagy stimulation by Met decreased AChE activity compared to the HCQ groups. Real-time PCR analysis revealed the expression of CD63, Alix, Rab11, Rab27a, and Rab27b in stimulated autophagy groups compared to HCQ-treated cells (b; n = 3). These values did not reach significant levels. Student t test. *p < 0.05; **p < 0.01; ***p < 0.001
Discussion
The combinatorial cell therapy is touted as an intriguing approach to reach efficient results in terms of cardiac regeneration after myocardial infarction [26]. Therefore, the study of multiple differentiation capacity of distinct stem cells or progenitors could enable us in concomitant promotion of angiogenesis and cardiomyogenesis [27]. More than a decade, studies have suggested that different signaling pathways, such as autophagy, are involved to commence a novel cell-fate acquisition in different cell types [28]. Due to a lack of sufficient data, we reasoned that pharmacological modulation of autophagy (either stimulation or inhibition) in bone marrow-derived CD146+ cells would modulate the differentiation capacity and further change regenerative capacity. To this end, 72-h incubation of CD146+ cells with 15-μM HCQ revealed significant accumulation of intracellular vacuoles determined by LysoTracker staining, showing successful lysosomal dysfunction and autophagic inhibition [29]. In this study, we noted 72-h incubation of differentiating CD146+ cells with 50-μM Met-induced protein synthesis of Beclin-1, and an increase in LC3-II/LC3-I ratio compared to the HCQ-treated groups. In contrast to CD146+ cells committed to endothelial lineage, a concurrent decrease in p62 in cells from PC and CM groups showed the completion of autophagic response after the exposure to the Met, while the current results showed contradictory P62 changes after autophagy modulation in progenitor cells oriented toward endothelial lineage. One reason for this discrepancy would be that the treatment of cells with lineage-specific factors could alter or blunt the normal function of the autophagic signaling pathway effector [30]. Therefore, one could hypothesize that the treatment of human bone marrow CD146+ cells could alter cellular levels of main autophagic regulators such as Beclin-1, P62, and LC3II/I ratio. In support of this statement, the inhibition of the insulin growth factor receptor could perturb autophagic response by modulation of protein kinase C [31]. According to the existence of different growth factors in the differentiation medium, it is logical to suppose that modulation of autophagy-related factors varies depending on the cell phenotype and activation of signaling pathways.
Interestingly, analysis of nitrosative stress showed significantly higher NO levels in groups treated with autophagy inhibitor HCQ compared to the Met-treated CD146+ cells. According to the results from the MTT test and NO analysis, it seems that 72-h incubation of CD146+ cells with autophagy inhibitor committed to different lineages could reduce cell viability via the nitrosative stress [32]. Considering different levels of NO in EC, PC, and CM, it seems that progenitor cells respond differently to autophagy modulation upon differentiation to different lineages [33]. According to our result, the production of NO is induced in a condition enriched with Met compared to the HCQ group. According to data from real-time PCR analysis and NO assay, one could hypothesize that the induction of autophagy could trigger the differentiation capacity of CD146+ toward EC, PC, and CM in the genomic levels. The lack of significant changes in protein levels of lineage-specific factors may point to the necessity for prolonged incubation periods at the proteomic level. The differentiation capacity of CD146+ cells was also monitored after autophagy modulation. Real-time PCR analysis showed the potency of 50-μM Met to upregulate the mRNA expression of lineage-specific factors such as endothelial VE-cadherin, cardiac cTnI, and PC α-SMA compared to the control of CD146+ cells and HCQ-treated groups. Western blotting also exhibited an increase in protein levels of lineage-specific factors such as α-actinin, α-SMA, and vWF factor after modulation of autophagy compared to the control group. These changes were following the phosphorylation of Erk1/2 in which groups received Met and HCQ showed a more Erk1/2 phosphorylation rate compared to the control cells [34]. According to the previous data, the modulation of autophagic response, either stimulation or inhibition, could induce the same enzymatic activity in different levels [34, 35]. The increase of cellular lineage-specific factors in HCQ-treated cells in comparison with control CD146+ cells could be related to the abolition of protein clearance after autophagy flux inhibition. However, more mechanistic investigations are needed to address the importance of autophagic status on the cellular distribution of specific factors.
We found that simultaneous autophagy modulation of human bone marrow CD146+ cells committed to PC, EC, and CM lineages altered fatty acid profile in which an increased PUFA + MUFA/SFA ratio in Met-treated group was achieved compared to the HCQ counterpart. These data showed that the supplementation of differentiation culture medium with 50-μM Met shifted the differentiating CD146+ cell fatty acid profile from saturated to unsaturated status. Previous studies declared that the reduction of saturated fatty acids, notably palmitic acid, seems a strategic approach to increase autophagic flux [36]. This study showed the increase of MUFA and PUFA in differentiating CD146+ cells after autophagic stimulation.
To find the possible cross-talk between the RTKs and autophagy status, we measured the levels of VEGFR-1 and -2 and Tie-1 and -2. Despite a slight increase in the level of VEGFR-1 and -2 and Tie-1 and -2 in cells exposed to the Met, these values did not reach statistically significant levels. Further analysis of CD146+ cells after autophagy modulation showed a close interplay between autophagy and pro-inflammatory status [37]. We showed that the supplementation of differentiation media with 50-μM Met reduced inflammatory TNF-α and IL-6 production. Previous data confirmed that the promotion of autophagic response is a way to reduce pro-inflammatory status in the target cells [38]. The existence of the same pattern in the promotion of nitrosative status and inflammatory cytokine production could indirectly indicate that the inhibition of autophagy in progenitor cells could abort the survival rate after transplantation to the target sites [39]. There are controversies regarding the potency of inflammatory status on the differentiation capacity of stem cells [40, 41]. Liu et al. showed that prolonged pro-inflammatory status could abrogate the differentiation capacity of stem cells [40]. In contrast, Pourgholaminejad and co-workers highlighted the potency of cytokine in accelerating MSC differentiation capacity [41]. Although the incubation of CD146+ cells with Met decreased inflammation rate, this modulation did not alter differentiation capacity toward three lineages in vitro compared to the condition exposed to the HCQ. Another interesting data from this experiment was the potency of Met to alter the biosynthesis of MUFA and PUFA in CD146+ cells committed to the CM lineage but not EC and PC phenotypes. It seems that autophagy stimulation/inhibition could alter the synthesis of MUFA, PUFA, and SFA in a specific condition. Hurley and co-workers investigated that the addition of oleic acid, but not SFA such as palmitic acid, could promote the differentiation of rat skeletal muscle cells in vitro via engaging peroxisome proliferator-activated receptors alpha or gamma [42].
This study aimed also to define the interplay between the autophagy and paracrine activity in CD146+ cells by monitoring the exosome secretion capacity. Our data showed the exosome secretion capacity indicated by supernatant AChE activity and stimulation of different genes involved in exosomes synthesis, transfer, and abscission in HCQ-treated cells. It seems that the inhibition of autophagy in differentiating cells promotes paracrine activity in vitro [43]. Commensurate with data from the current experiment and previous studies, it seems that the inhibition of autophagy and fatty acid change could alter the paracrine ability of progenitor and differentiating cells and increase of PUFA and MUFA is efficient in the secretion of exosomes [44].
Conclusion
In conclusion, it seems that the modulation of autophagy could alter the differentiation potential and exosome secretion of human CD146+ cells in vitro.
Acknowledgements
The authors thank the stem cell research center personnel for guidance and help.
Abbreviations
- MTT
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide
- DAPI
4′,6-Diamidino-2-phenylindole
- AChE
Acetylcholine esterase
- α-SMA
Alpha-smooth muscle actin
- Ang-1
Angiopoietin-1
- cTnI
Cardiac troponin-I
- CMs
Cardiomyocytes
- CD146
Melanoma cell adhesion molecules
- GC
Chromatography
- ECs
Endothelial cells
- ELISA
Enzyme-linked immunosorbent assay
- FBS
Fetal bovine serum
- GC
Gas chromatography
- HCQ
Hydroxychloroquine
- IL-6
Interleukin 6
- DMEM/LG
Low-content glucose Dulbecco’s modified Eagle medium
- MACS
Magnetic-activated cell sorting
- Met
Metformin
- MUFA
Monounsaturated fatty acid
- MNCs
Mononuclear cells
- PCs
Pericytes
- PBS
Phosphate-buffered saline solution
- PUFA
Polyunsaturated fatty acid
- ROS
Reactive oxygen species
- RT-PCR
Real-time PCR
- RTKs
Receptor tyrosine kinases
- SFA
Saturated fatty acid
- TNF-α
Tumor necrosis factor alpha
- Tie-1
Tyrosine-protein kinase receptor-1
- Tie-2
Tyrosine-protein kinase receptor-2
- VE-cadherin
Vascular endothelial—cadherin
- VEGFR-1
Vascular epithelial growth factor receptor-1
- VEGFR-2
Vascular epithelial growth factor receptor-2
Authors’ contributions
M.H., J.R., and M.D. performed the experiments. A.H. collected the samples. R.R. and M.N. supervised the study. The author(s) read and approved the final manuscript.
Funding
This work was supported by a grant (IR.TBZMED.REC.1397.636) from the Tabriz University of Medical Sciences.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
All procedures in this study were conducted under the European Medicines Agency’s (EMA) pediatric committee (EudraCT number: 2011-004074-28) and conducted according to the 2000 revised principles of the Declaration of Helsinki (ClinicalTrials.gov identifier: NCT01765283 ). Informed consent was obtained from the parents/legally authorized representatives of participants. Local Ethics Committee, Tabriz University of Medical, approved all phases of this study (IR.TBZMED.REC.1397.636).
Consent for publication
None applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Reza Rahbarghazi and Mohammad Nouri contributed equally to this work.
Contributor Information
Reza Rahbarghazi, Email: Rezarahbardvm@gmail.com.
Mohammad Nouri, Email: Nourimd@yahoo.com.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2016 update a report from the American Heart Association. Circulation. 2016;133(4):e38–e48. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Gorjipour F, Hosseini-Gohari L, Alizadeh Ghavidel A, Hajimiresmaiel SJ, Naderi N, Darbandi Azar A, et al. Mesenchymal stem cells from human amniotic membrane differentiate into cardiomyocytes and endothelial-like cells without improving cardiac function after surgical administration in rat model of chronic heart failure. J Cardiovasc Thorac Res. 2019;11(1):35–42. doi: 10.15171/jcvtr.2019.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katare R, Riu F, Mitchell K, Gubernator M, Campagnolo P, Cui Y, et al. Transplantation of human pericyte progenitor cells improves the repair of infarcted heart through activation of an angiogenic program involving micro-RNA-132. Circ Res. 2011;109(8):894–906. doi: 10.1161/CIRCRESAHA.111.251546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Avolio E, Meloni M, Spencer HL, Riu F, Katare R, Mangialardi G, et al. Combined intramyocardial delivery of human pericytes and cardiac stem cells additively improves the healing of mouse infarcted hearts through stimulation of vascular and muscular repair. Circ Res. 2015;116(10):e81–e94. doi: 10.1161/CIRCRESAHA.115.306146. [DOI] [PubMed] [Google Scholar]
- 5.Shaw I, Rider S, Mullins J, Hughes J, Péault B. Pericytes in the renal vasculature: roles in health and disease. Nat Rev Nephrol. 2018;14(8):521. doi: 10.1038/s41581-018-0032-4. [DOI] [PubMed] [Google Scholar]
- 6.Psaltis PJ, Simari RD. Vascular wall progenitor cells in health and disease. Circ Res. 2015;116(8):1392–1412. doi: 10.1161/CIRCRESAHA.116.305368. [DOI] [PubMed] [Google Scholar]
- 7.Avolio E, Madeddu P. Discovering cardiac pericyte biology: from physiopathological mechanisms to potential therapeutic applications in ischemic heart disease. Vasc Pharmacol. 2016;86:53–63. doi: 10.1016/j.vph.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 8.Cathery W, Faulkner A, Maselli D, Madeddu P. Concise review: the regenerative journey of pericytes toward clinical translation. Stem Cells. 2018;36(9):1295–1310. doi: 10.1002/stem.2846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herrmann M, Bara J, Sprecher C, Menzel U, Jalowiec J, Osinga R, et al. Pericyte plasticity–comparative investigation of the angiogenic and multilineage potential of pericytes from different human tissues. Eur Cell Mater. 2016;31:236–249. doi: 10.22203/eCM.v031a16. [DOI] [PubMed] [Google Scholar]
- 10.Frangogiannis NG. The extracellular matrix in ischemic and nonischemic heart failure. Circ Res. 2019;125(1):117–146. doi: 10.1161/CIRCRESAHA.119.311148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Song S, Tan J, Miao Y, Li M, Zhang Q. Crosstalk of autophagy and apoptosis: involvement of the dual role of autophagy under ER stress. J Cell Physiol. 2017;232(11):2977–2984. doi: 10.1002/jcp.25785. [DOI] [PubMed] [Google Scholar]
- 12.Miller BC, Zhao Z, Stephenson LM, Cadwell K, Pua HH, Lee HK, et al. The autophagy gene ATG5 plays an essential role in B lymphocyte development. Autophagy. 2008;4(3):309–314. doi: 10.4161/auto.5474. [DOI] [PubMed] [Google Scholar]
- 13.Simon AK, Obba S, Zhang H, Riffelmacher T. Autophagy in the hematopoietic system. Washington DC: American Society of Hematology; 2019. [Google Scholar]
- 14.Mizushima N, Levine B. Autophagy in mammalian development and differentiation. Nat Cell Biol. 2010;12(9):823–830. doi: 10.1038/ncb0910-823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ke D, Ji L, Wang Y, Fu X, Chen J, Wang F, et al. JNK1 regulates RANKL-induced osteoclastogenesis via activation of a novel Bcl-2-Beclin1-autophagy pathway. FASEB J. 2019;33(10):11082–11095. doi: 10.1096/fj.201802597RR. [DOI] [PubMed] [Google Scholar]
- 16.Baerga R, Zhang Y, Chen P-H, Goldman S, Jin SV. Targeted deletion of autophagy-related 5 (atg5) impairs adipogenesis in a cellular model and in mice. Autophagy. 2009;5(8):1118–1130. doi: 10.4161/auto.5.8.9991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hou J, Han Z, Jing Y, Yang X, Zhang S, Sun K, et al. Autophagy prevents irradiation injury and maintains stemness through decreasing ROS generation in mesenchymal stem cells. Cell Death Dis. 2013;4(10):e844–e84e. doi: 10.1038/cddis.2013.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang J, Liu J, Liu L, McKeehan WL, Wang F. The fibroblast growth factor signaling axis controls cardiac stem cell differentiation through regulating autophagy. Autophagy. 2012;8(4):690–691. doi: 10.4161/auto.19290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amini H, Rezaie J, Vosoughi A, Rahbarghazi R, Nouri M. Cardiac progenitor cells application in cardiovascular disease. J Cardiovasc Thorac Res. 2017;9(3):127–132. doi: 10.15171/jcvtr.2017.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ye H, Chen M, Cao F, Huang H, Zhan R, Zheng X. Chloroquine, an autophagy inhibitor, potentiates the radiosensitivity of glioma initiating cells by inhibiting autophagy and activating apoptosis. BMC Neurol. 2016;16(1):178. doi: 10.1186/s12883-016-0700-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zolali E, Rezabakhsh A, Nabat E, Jaberi H, Rahbarghazi R, Garjani A. Metformin effect on endocan biogenesis in human endothelial cells under diabetic condition. Arch Med Res. 2019;50(5):304–314. doi: 10.1016/j.arcmed.2019.08.012. [DOI] [PubMed] [Google Scholar]
- 22.Hassanpour M, Rezabakhsh A, Rahbarghazi R, Nourazarian A, Nouri M, Avci ÇB, et al. Functional convergence of Akt protein with VEGFR-1 in human endothelial progenitor cells exposed to sera from patient with type 2 diabetes mellitus. Microvasc Res. 2017;114:101–113. doi: 10.1016/j.mvr.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 23.Mohammadzadeh F, Mosayebi G, Montazeri V, Darabi M, Fayezi S, Shaaker M, et al. Fatty acid composition of tissue cultured breast carcinoma and the effect of stearoyl-CoA desaturase 1 inhibition. J Breast Cancer. 2014;17(2):136–142. doi: 10.4048/jbc.2014.17.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ulmer CZ, Jones CM, Yost RA, Garrett TJ, Bowden JA. Optimization of Folch, Bligh-Dyer, and Matyash sample-to-extraction solvent ratios for human plasma-based lipidomics studies. Anal Chim Acta. 2018;1037:351–357. doi: 10.1016/j.aca.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vijayaraghavan S, Karakas C, Doostan I, Chen X, Bui T, Yi M, et al. CDK4/6 and autophagy inhibitors synergistically induce senescence in Rb positive cytoplasmic cyclin E negative cancers. Nat Commun. 2017;8:15916. doi: 10.1038/ncomms15916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang P, Wang L, Li Q, Xu J, Xu J, Xiong Y, et al. Combinatorial treatment of acute myocardial infarction using stem cells and their derived exosomes resulted in improved heart performance. Stem Cell Res Ther. 2019;10(1):1–12. doi: 10.1186/s13287-018-1105-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reddy LVK, Sen D. Regulation of cardiomyocyte differentiation, angiogenesis, and inflammation by the delta opioid signaling in human mesenchymal stem cells. Regen Eng Transl Med. 2019;5(3):252–262. doi: 10.1007/s40883-019-00100-x. [DOI] [Google Scholar]
- 28.Hassanpour M, Rezabakhsh A, Pezeshkian M, Rahbarghazi R, Nouri M. Distinct role of autophagy on angiogenesis: highlights on the effect of autophagy in endothelial lineage and progenitor cells. Stem Cell Res Ther. 2018;9(1):305. doi: 10.1186/s13287-018-1060-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amaravadi RK, Winkler J. Asymmetric bisaminoquinolines and bisaminoquinolines with varied linkers as autophagy inhibitors for cancer and other therapy. Google Patents. 2019.
- 30.Schaaf MBE, Houbaert D, Meçe O, To SK. Ganne M, Maes H, et al. Lysosomal pathways and autophagy distinctively control endothelial cell behavior to affect tumor vasculature. Front Oncol. 2019;9:171. doi: 10.3389/fonc.2019.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Renna M, Bento CF, Fleming A, Menzies FM, Siddiqi FH, Ravikumar B, et al. IGF-1 receptor antagonism inhibits autophagy. Hum Mol Genet. 2013;22(22):4528–4544. doi: 10.1093/hmg/ddt300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rezabakhsh A, Ahmadi M, Khaksar M, Montaseri A, Malekinejad H, Rahbarghazi R, et al. Rapamycin inhibits oxidative/nitrosative stress and enhances angiogenesis in high glucose-treated human umbilical vein endothelial cells: role of autophagy. Biomed Pharmacother. 2017;93:885–894. doi: 10.1016/j.biopha.2017.07.044. [DOI] [PubMed] [Google Scholar]
- 33.Boya P, Codogno P, Rodriguez-Muela N. Autophagy in stem cells: repair, remodelling and metabolic reprogramming. Development. 2018;145(4):dev146506. doi: 10.1242/dev.146506. [DOI] [PubMed] [Google Scholar]
- 34.S-y C, Chiu L-Y, Ma M-C, Wang J-S, Chien C-L, Lin W-W. zVAD-induced autophagic cell death requires c-Src-dependent ERK and JNK activation and reactive oxygen species generation. Autophagy. 2011;7(2):217–228. doi: 10.4161/auto.7.2.14212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mahli A, Saugspier M, Koch A, Sommer J, Dietrich P, Lee S, et al. ERK activation and autophagy impairment are central mediators of irinotecan-induced steatohepatitis. Gut. 2018;67(4):746–756. doi: 10.1136/gutjnl-2016-312485. [DOI] [PubMed] [Google Scholar]
- 36.Morselli E, Hernández-Cáceres MP, Toledo-Valenzuela L, Ávalos Y, Peña-Oyarzun D, Criollo A. Palmitic acid reduces the autophagic flux and insulin sensitivity through the activation of the free fatty acid receptor 1 (FFAR1) in the hypothalamic neuronal cell line N43/5. Front Endocrinol. 2019;10:176. doi: 10.3389/fendo.2019.00176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Varga ZV, Giricz Z, Liaudet L, Haskó G, Ferdinandy P, Pacher P. Interplay of oxidative, nitrosative/nitrative stress, inflammation, cell death and autophagy in diabetic cardiomyopathy. Biochim Biophys Acta. 2015;1852(2):232–242. doi: 10.1016/j.bbadis.2014.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ge Y, Huang M, Yao Y-m. Autophagy and proinflammatory cytokines: interactions and clinical implications. Cytokine Growth Factor Rev. 2018;43:38–46. doi: 10.1016/j.cytogfr.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 39.Beljanski V, Grinnemo K-H, Österholm C. Pleiotropic roles of autophagy in stem cell–based therapies. Cytotherapy. 2019. [DOI] [PMC free article] [PubMed]
- 40.Liu C, Xiong H, Chen K, Huang Y, Yin X. Long-term exposure to pro-inflammatory cytokines inhibits the osteogenic/dentinogenic differentiation of stem cells from the apical papilla. Int Endod J. 2016;49(10):950–959. doi: 10.1111/iej.12551. [DOI] [PubMed] [Google Scholar]
- 41.Pourgholaminejad A, Aghdami N, Baharvand H, Moazzeni SM. The effect of pro-inflammatory cytokines on immunophenotype, differentiation capacity and immunomodulatory functions of human mesenchymal stem cells. Cytokine. 2016;85:51–60. doi: 10.1016/j.cyto.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 42.Hurley MS, Flux C, Salter AM, Brameld JM. Effects of fatty acids on skeletal muscle cell differentiation in vitro. Br J Nutr. 2006;95(3):623–630. doi: 10.1079/BJN20051711. [DOI] [PubMed] [Google Scholar]
- 43.Shrivastava S, Devhare P, Sujijantarat N, Steele R, Kwon Y-C, Ray R, et al. Knockdown of autophagy inhibits infectious hepatitis C virus release by the exosomal pathway. J Virol. 2016;90(3):1387–1396. doi: 10.1128/JVI.02383-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jackson CL. Membrane trafficking: a little flexibility helps vesicles get into shape. Curr Biol. 2018;28(12):R706–R7R9. doi: 10.1016/j.cub.2018.04.068. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.