Abstract
Acute diarrhea caused by an infectious organism is highly prevalent, particularly in developing countries, and is usually self-limiting. The condition is a major contributor to the global disease burden and is associated with a significant economic cost. The disease is common in children aged <5 years. It occurs as the result of exposure to a diarrheogenic agent that alters intestinal absorption and/or secretion, resulting in an increase in the volume of water that enters the colon beyond that which can be absorbed. Diarrhea almost always occurs by one or more of four mechanisms: disruption of osmotic forces in the intestine; disruption of normal secretory processes; disruption of epithelial cells or the epithelial tight junctions; or motility disorders.
Oral rehydration therapy (ORT) is central to the management of acute diarrhea, and is sufficient to prevent complications due to dehydration in most patients while the disease runs its course. However, ORT has no effect on the duration of the disease or frequency of bowel motions, and any agent that could meet these needs would therefore be a useful addition to ORT.
Diosmectite is a natural aluminomagnesium silicate clay with a lamellar, non-fibrous crystalline structure that gives it strong adsorbent properties. Its mechanisms of action are not yet fully understood, but are probably multiple. Diosmectite reduces inflammation, modifies mucus rheologic properties, inhibits mucolysis, and adsorbs bacteria, bacterial enterotoxins, viruses and other potentially diarrheogenic substances.
A number of studies have shown that diosmectite reduces the duration of diarrhea and decreases the frequency of bowel motions after 2 days of treatment in children with mild-to-moderate acute diarrhea. Two recent trials have indicated a reduction in stool output with diosmectite. Because of its very favorable safety profile, with no serious adverse effects, diosmectite is frequently used, mainly in European countries but also in Asia and Africa. Diosmectite should be used as an adjunct, not an alternative, to ORT and, when needed, to antibacterial therapy.
Keywords: Diarrhea, Cystic Fibrosis Transmembrane Conductance Regulator, Mucus Layer, Acute Gastroenteritis, Acute Diarrhea
Acute diarrhea is defined as a diarrheal disease consisting of the passage of unformed or watery stools three or more times per day lasting up to 14 days.[1,2] Persistent and chronic diarrhea are diarrheal diseases lasting for >14 and >30 days, respectively. Diarrhea occurs as the result of a nonspecific intestinal response to various stimuli, including infections, drugs, and inflammatory bowel disease.
Acute diarrhea is attributable to various infectious causes, although the infecting organism(s) often cannot be identified. Invasive diarrhea occurs when the infecting pathogen crosses the mucosal lining of the gastrointestinal (GI) tract. Viruses, particularly rotavirus, are the predominant pathogens associated with diarrhea in developed countries, while bacteria are the most frequent cause in developing regions.[3]
Diarrhea occurs when absorptive and secretory changes increase the volume of water that enters the colon to a level beyond its absorptive capacity. It almost always arises as a result of one or more of four basic mechanisms: osmotic diarrhea, secretory diarrhea, exudative diarrhea, and diarrhea associated with motility disorders. Osmotic diarrhea occurs when large quantities of poorly absorbed, low molecular-weight solutes in the lumen drive the transport of excessive water into the lumen via osmotic forces.[4] Secretory diarrhea develops in response to overstimulation of the secretory capacity of the intestinal tract.[1,4] It usually occurs as a result of bacterial and viral enterotoxins. In exudative diarrhea, bacterial and viral pathogens destroy epithelial cells or disrupt the tight junctions of the intestinal epithelium.[4] This allows water and electrolytes, mucus, and proteins to exude into the lumen due to the hydrostatic pressure differential, where they may accumulate and cause diarrhea. Motility disorders that accelerate intestinal transit time can decrease absorption, causing diarrhea even when the absorptive process itself is proceeding normally.[4]
Diarrhea is a major contributor to global morbidity and mortality despite recent advances in understanding of the pathogenesis, diagnosis, and treatment of enteric diseases. It is less well recognized that the consequences of some causes of infectious diarrhea can also include conditions such as irritable bowel syndrome, hemolytic-uremic syndrome, malnutrition, and Guillain-Barré syndrome.
Factors in the environment also play an important role in the pathogenesis of infectious diarrheal disease. Mass food processing and globalization of food supplies, increased international travel, and the emergence and spread of resistant bacteria are all factors that contribute to diarrheal disease being a concern for both developed and developing countries. Although there has been a sharp decline in diarrhea-associated mortality in developed countries, it is still a prevalent disease that is associated with a significant economic burden. Developing countries are particularly vulnerable to the consequences of diarrhea.[5]
Acute gastroenteritis is characterized by acute-onset diarrhea with or without vomiting, nausea, fever, and abdominal pain.[3] The symptoms and signs may be nonspecific in children. It is estimated that there are 3–5 billion cases of acute gastroenteritis caused by GI tract infection annually among children aged <5 years.[1] Previously, approximately 1.5 million children aged <5 years died each year as a consequence of acute gastroenteritis, predominantly in developing countries, but this figure has decreased considerably in the last 2 decades, mainly as a result of improved management of the condition.[1]
As gastroenteritis is typically a self-limiting condition, the main goal of therapy is to prevent complications secondary to dehydration and its associated electrolyte disturbances and metabolic acidosis.[3] Oral rehydration salt (ORS) solutions are the recommended mainstay of treatment for acute diarrhea, and are effective on their own in ≥95% of cases of mild or moderate dehydration.[1] Oral rehydration therapy (ORT) with ORS solutions has the obvious advantages over intravenous (IV) fluid rehydration of being less costly and able to be administered in many settings, including the home.[6] In cases of severe dehydration, or where ORT is contraindicated or the patient is unable to drink, IV rehydration may be required initially, with early reintroduction of ORT where possible. Continued feeding, including breast feeding, is also important for children with acute diarrhea, and this is considered feasible as soon as the first part of rehydration is finished, i.e. not more than 6–8 hours.
While ORT is central to the management of acute diarrhea, it does not reduce the frequency of bowel movements or the duration of illness.[6] Alternative or adjunctive anti-diarrheal agents that decrease the duration of diarrhea and are safe would therefore be a valuable addition in the management of diarrhea. The three main classes of anti-diarrheal drug that are used to reduce stool frequency and/or volume and duration of symptoms are anti-motility agents, anti-secretories, and adsorbents. However, it is important that any drug used to treat diarrhea, particularly in children, is safe and well tolerated, especially as it is likely to be used in the home environment without extensive physician supervision. An anti-diarrheal agent should also be able to be used in conjunction with ORT, and be effective in diarrhea of different etiologies. Anti-diarrheal agents are not usually recommended for acute diarrhea in children, mainly because of a lack of consistent efficacy data supporting their use in pediatric patients, but also because of the potential for significant and/or serious adverse effects associated with anti-motility or anti-secretory agents. Adsorbents, on the other hand, are generally well tolerated as they are not readily absorbed systemically.
Diosmectite (smectite, Smecta®; Ipsen, Boulogne-Billancourt, France) is an oral formulation of a natural aluminomagnesium silicate clay with a lamellar structure. It exhibits adsorbent properties, interacts with mucus, and has been shown to be an effective and well tolerated anti-diarrheal agent, reducing the frequency of stools and the duration of symptoms (see sections 2 and 4).
This review summarizes the pharmacodynamic activity of diosmectite underlying its anti-diarrheal properties, and evaluates the clinical evidence for the use of diosmectite in the treatment of diarrhea in children. Articles used for this review were identified within the MEDLINE database using the search terms ‘diosmectite’ and ‘smectite.’ Additional references were identified from the bibliographies of published articles.
1. Use of Medicinal Clays
1.1 History
The historical practice of geophagy has been reported on all continents going back hundreds of years, particularly in tropical regions; it is also seen in the animal kingdom in the use of salt licks and mud wallows.[7] Clays have been used systemically to prevent poisoning, to treat diarrhea and indigestion, and, topically, for the treatment of skin and mouth ulcers and parasite eradication. Soils that have historically been used for such purposes have typically been found to be rich in ‘kaolin’ minerals, particularly smectite.
1.2 Current Utilization
Clays continue to be used today in a variety of indications. In addition to their use as anti-diarrheal agents, which is the focus of this article, there has been a resurgence in the use of clays by complementary therapists for many of the indications described in section 1.1. Other uses of clays include beauty treatments, as lubricants in drilling, as sealants, and as emulsifying and bleaching agents; indeed the clay extract bentonite is used as a back-filling material in underground storage facilities for radioactive nuclear material.[8]
2. Clinical Evidence of Effectiveness of Diosmectite
Diosmectite, a powder formulation for oral suspension, is a natural clay formed from fine sheets of aluminomagnesium silicate. The non-fibrous crystalline structure of diosmectite confers significantly greater adsorbent properties than other clays used in the treatment of diarrhea.[9] Diosmectite reduces inflammation and inhibits the penetration of toxins through the mucus layer, thus intervening between the intestinal lumen and the epithelial cells (see section 4). The efficacy of diosmectite in the treatment of acute diarrhea in children has been investigated in several controlled clinical studies. Despite varying inclusion criteria and outcome parameters, results have consistently demonstrated the efficacy of diosmectite.
In the largest trial to date, 804 children aged 3 months to 5 years with acute-onset, mild-to-moderate diarrhea were randomized to receive ORS plus diosmectite 3 or 6 g/day or ORS therapy alone for 5 days.[10] Efficacy was assessed according to the total duration of diarrhea, stool frequency and consistency, incidence of vomiting and fever, the number of children with diarrhea lasting >7 days, and the number of children requiring hospitalization. Adjunctive therapy with diosmectite significantly improved frequency of stool outputs and stool consistency on days 2–5 compared with ORS alone. By day 6 of treatment, the differences in improvement between the treatment groups were not significant. Diarrhea lasting >7 days affected fewer children receiving diosmectite plus ORS than ORS alone (10.8% vs 18.1%; p < 0.01). Other outcomes such as hospital admission, and incidence and duration of vomiting and fever did not differ between treatment groups. Diosmectite was well tolerated and no treatment-related adverse events were reported. Up to 20% of children did not comply with the 5-day diosmectite regimen, including 2.8% who refused even one dose. The most commonly reported reason for the noncompliance was the unpleasant taste of the diosmectite formulation. Comparative control tolerability data were not reported.
In a placebo-controlled study, 90 boys aged 3–24 months with acute watery diarrhea and mild, moderate, or severe dehydration were randomized to receive, following rehydration therapy, diosmectite 1.5 g four times daily for 3 days or placebo.[11] Unlike the previous study, all patients completed the regimen; the treatment was administered under supervision. The mean duration of diarrhea in diosmectite recipients was significantly shorter than in placebo recipients (54 vs 73 hours; p = 0.001). The difference between the groups became statistically significant 24–48 hours after the start of treatment. Diosmectite was also associated with significantly fewer diarrheal stools overall (11.3 vs 13.8; p = 0.001). Weight gain at 24, 48, and 72 hours was significantly greater with diosmectite, despite comparable fluid and food intake between the groups. Diosmectite was well tolerated and did not interfere with normal feeding or ORT.
Two similarly designed studies in Thailand evaluated the efficacy, acceptability, and safety of diosmectite in hospitalized or outpatient pediatric patients aged 1–24 months with mild-to-moderate acute diarrhea.[12,13] In the study of hospitalized patients, infants were randomized to receive diosmectite 1.5 g every 6, 8, or 12 hours depending on bodyweight in combination with ORS (n = 32) or ORS alone (n = 30).[12] The duration of diarrhea was almost halved in diosmectite recipients (43.3 vs 84.7 hours; p < 0.005). By day 5, only 3% of infants who were receiving diosmectite continued to have diarrhea compared with 27% treated with ORS alone. In the outpatient study, 66 infants were randomized to receive rehydration plus diosmectite 1.5 g every 12 hours (n = 34) or IV or oral rehydration alone (n = 32).[13] Diarrhea had resolved in 71% of diosmectite recipients by day 3 of treatment, compared with 34% of infants receiving rehydration alone (p < 0.01). On day 5 of treatment, the incidence of diarrhea was 12% in the diosmectite group compared with 34% in the rehydration-alone group (p = 0.04). The acceptability of diosmectite was rated as ‘good’ by 88% of children in the outpatient study. There was a tendency for more patients in the diosmectite group to experience constipation in both studies; three cases in the outpatient study and two participants in the study with hospitalized infants had hardened stools. Two of the hospitalized infants refused medication because of vomiting, a difficulty resolved by moving diosmectite administration to the preprandial period.
Diosmectite combined with ORS was also shown to be more effective than ORS alone in a randomized, open-label, multicenter study involving 54 children aged 6–48 months hospitalized in Lithuania with acute diarrhea and mild or moderate dehydration.[14] Diosmectite significantly reduced the duration of diarrhea compared with ORS alone (42.3 vs 61.8 hours; p < 0.05). Electrolyte levels were also evaluated. Sodium levels increased significantly during treatment in both groups; the levels did not exceed normal levels and normalized in patients with hyponatremic dehydration, suggesting that diosmectite did not impact on the absorption of electrolytes. No treatment-related adverse effects occurred in this study.
Gilbert et al.[15] compared the efficacy of diosmectite with that of loperamide in a placebo-controlled study involving 56 children aged 2–22 months with moderate or severe diarrhea, mostly secondary to rotavirus infection. Resolution of diarrhea occurred in 3.22 and 3.07 days with diosmectite and loperamide, respectively, compared with 4.08 days for placebo; the difference between diosmectite and loperamide was not significant. Although tolerability data were not formally obtained in this study, the treating physicians reported that tolerability was ‘good’ in all cases. Currently, no other studies have directly compared the efficacy of diosmectite with anti-motility drugs, anti-secretory drugs, or other adsorbent agents.
A recent meta-analysis of randomized, controlled clinical trials included many of the clinical studies cited previously in this review (table I).[19] Six trials (n = 1076) found that diosmectite significantly reduced the duration of diarrhea by a mean −22.7 hours (95% CI −24.8, −20.6) compared with controls. Data from two trials[19] (n = 125) showed that the frequency of stools was reduced at 48–72 hours and 72–96 hours after start of treatment with diosmectite, compared with placebo; no difference between diosmectite and placebo was evident at <48 hours. The relative chance of resolution of diarrhea on day 3 of diosmectite treatment was 1.64 (95% CI 1.36, 1.98) compared with controls, which was statistically significant; the number of patients needed to treat to resolve one case of diarrhea was 4 (95% CI 3, 5). The analyses did not detect any differences between diosmectite and placebo in the incidence of vomiting or compliance with treatment. Available tolerability data indicated only a nonsignificant trend for more diosmectite than placebo recipients to experience constipation. While acknowledging the limitations inherent in any meta-analysis, and the methodologic limitations of the included studies, the investigators concluded that the results of the meta-analysis were promising and suggested that some children with acute diarrhea may benefit from using diosmectite. However, they also cautioned that if diosmectite is to be used, then patients, parents, and physicians need to be mindful that the focus is not removed from appropriate rehydration, electrolyte, and nutritional therapies. The investigators also noted that further well conducted research is needed to determine which patients (e.g. age, invading pathogen type, outpatient vs inpatient) will gain the greatest clinical benefit, the most effective dosing regimen, the cost effectiveness or otherwise of therapy, and the tolerability of diosmectite.
Table I.
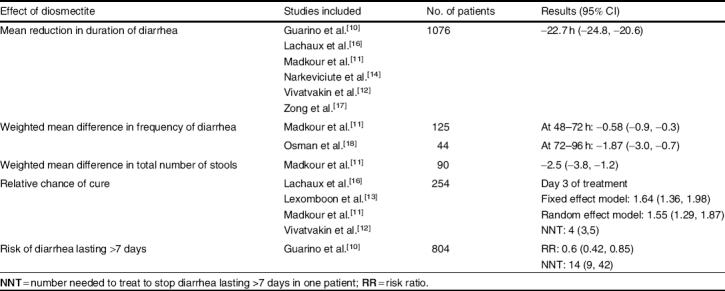
Significant clinical effects of diosmectite compared with controls in randomized controlled trials[19]
Very recently, two randomized, parallel, double-blind, placebo-controlled studies in Peru (n = 300) and Malaysia (n = 302) were undertaken to examine the efficacy of diosmectite for reducing stool output in children aged 1–36 months with acute diarrhea.[20] Inclusion criteria included ≥3 watery stools/day for <72 hours and a weight : height ratio ≥0.8. In addition to ORT (WHO formula), patients received diosmectite (6 g/day in children aged 1–12 months and 12 g/day in children aged 13–36 months) for ≥3 days, followed by half doses until complete recovery. Stool output was significantly lower with diosmectite, particularly among rotavirus-positive children. In pooled data, a mean stool output of 94.5 ± 74.4 g/kg was observed in the diosmectite group versus 104.1 ± 94.2 g/kg in the placebo group (p = 0.002).[20]
3. Pathophysiology of Diarrhea
3.1 Microcellular Changes and Mechanisms in Diarrhea
3.1.1 Inflammatory Response to Enteric Pathogens
Intestinal epithelial cells can trigger a large immune response to pathogenic organisms.[21–23] Adhesion or invasion of enteric pathogens stimulates an inflammatory response in the adjacent intestinal mucosa via a number of different mechanisms (figure 1). Bacterial invasion results in the coordinated expression and upregulation of proinflammatory cytokines by epithelial cells.[24] It has also been demonstrated that when intestinal epithelial cells are infected by microbes, for example, enteropathogenic Escherichia coli (EPEC), an inflammatory response mediated by nuclear factor-κB is activated.[23] Indeed, many enteric pathogens are capable of activating inflammatory responses.[21]
Fig. 1.
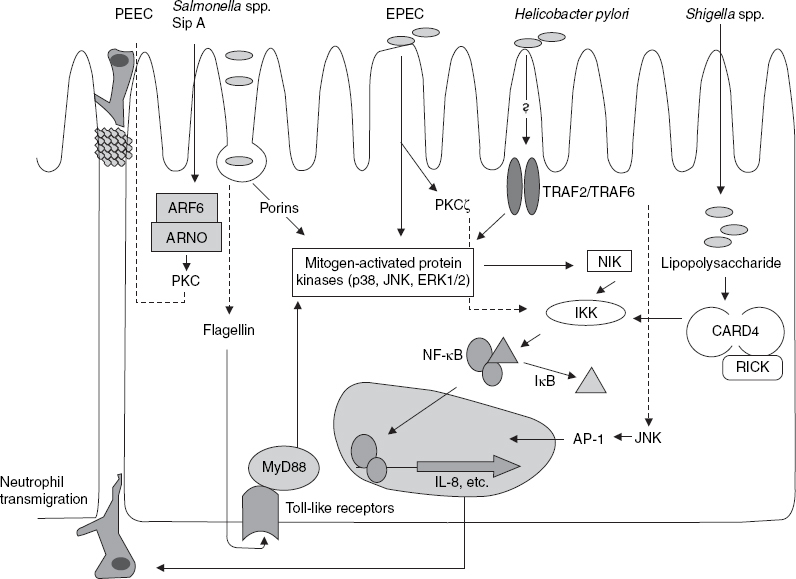
The main enteric pathogen-induced proinflammatory pathway, which results in nuclear factor-κB (NF-κB)-mediated transcription of interleukin (IL)-8. Secreted IL-8 and other factors such as pathogen-elicited epithelial-derived chemoattractant (PEEC) stimulate the transepithelial migration of neutrophils to the lumen, where they target pathogens for destruction. The precise bacterial components involved in inducing an inflammatory response and the details of the signaling pathways involved have not been determined for all pathogens, but mitogen-activated protein kinases play a fundamental role in many of these pathways. Pathogen-associated molecular patterns (e.g. lipopolysaccharide and flagellin) induce a response by binding to cognate toll-like receptors to elicit a response. Non-IL-8-mediated proinflammatory pathways are also present in epithelial cells (reproduced from Berkes et al.,[21] with permission). AP-I = activating protein 1; ARF6 = adenosine diphosphate (ADP) ribosylation factor 6; ARNO = ARF nucleotide-binding site opener; CARD4 = caspase recruitment domain protein 4; EPEC = enteropathogenic Escherichia coli; ERK = extracellular signal-regulated kinase; IκB = inhibitory protein κβ; IKK = Iκβ kinase; JNK = c-Jun NH2 terminal kinase; MyD88 = myeloid differentiation primary response protein 88; NIK = NF-κB-inducing kinase; PKC = protein kinase C; RICK = receptor-interacting protein (RIP)-like interacting caspase-like apoptosis regulatory protein kinase; Sip A = Salmonella invasion protein A; TRAF = tumor necrosis factor (TNF) receptor-associated factor.
3.1.2 Alterations to Fluid and Electrolyte Secretion
Secretion of chloride is the main determinant of hydrationin the lumen. The main chloride transporters affected by pathogens are the cystic fibrosis transmembrane conductance regulator (CFTR) and calcium-driven chloride channels. Cholera enterotoxin, E. coli types I and II heat labile enterotoxins, and Clostridium difficile, for example, activate CFTR via induction of cyclic adenosine monophosphate (cAMP), which stimulates electrogenic chloride secretion, ultimately leading to diarrhea. Chloride secretion can also be stimulated via cyclic guanosine monophosphate (cGMP)-mediated pathways by heat-stable enterotoxins produced by enteroaggregative E. coli or enterotoxigenic E. coli (ETEC).[25] Nonbacterial pathogens, especially rotavirus, have also been associated with production of the viral glycoprotein enterotoxin NSP4, which is associated with intracellular calcium-driven chloride secretion.[26]
3.1.3 Role of Mucus
Pathogens can trigger an inflammatory response at the level of the intestinal mucosa itself[22,24] causing disruption of the intestinal barrier, which results in heightened crossing by macromolecules, including antigens, thereby probably facilitating a self-perpetuating process of mucosal inflammation.[22] This inflammation can destroy the mucosa and cause diarrhea.
3.1.4 Role of Enterocytes
Colonic epithelial cells may be ‘programmed’ to provide chemotactic and activating signals to nearby immune and inflammatory cells following a pathogenic invasion. Furthermore, tumor necrosis factor (TNF)-α and interleukin (IL)-1 produced by neighboring cells within the epithelial microenvironment following microbial invasion stimulate the production of proinflammatory cytokines by epithelial cells, amplifying the mucosal inflammatory response.
3.1.5 Role of Cytokines/Endotoxins
Bacterial invasion has been shown to result in the coordinated expression and upregulation of proinflammatory cytokines by epithelial cells.[24] Many pathogens produce endotoxins, which can also contribute to the pathophysiology of acute diarrhea by disruption of calcium-, cAMP-, and cGMP-mediated fluid and electrolyte secretion, alteration of the tight junction barrier function, and activation of inflammatory pathways.[21,4]
3.1.6 Alteration of Cellular Tight Junction
The tight junctions of epithelial cells can be disrupted by enteric pathogens either by alteration of the cellular cytoskeleton or by affecting specific tight junction proteins.[21] C. difficile, EPEC, C. perfringens, Bacteroides fragilis, and Vibrio cholera are all known to interfere with the tight junction barrier.[21]
4. Mechanisms of Action of Diosmectite
There are, up to now, three broad mechanisms by which diosmectite is thought to help in the treatment of diarrhea, all of which ultimately involve disruption of the interaction between the intestinal lumen and intestinal epithelial cells. First, diosmectite reduces inflammation; secondly, it binds with the mucus barrier, altering its rheologic properties and inhibiting mucolysis; and thirdly, it adsorbs toxins, other compounds, and infectious agents that can damage the mucus lining.
4.1 Anti-Inflammatory Activity
The anti-inflammatory mechanism of diosmectite probably involves inhibition of proinflammatory markers. Diosmectite has demonstrated significant anti-inflammatory activity in an experimental rat model of hapten-induced colitis.[27] Furthermore, the level of anti-inflammatory action was comparable to that of established treatments such as sulfasalazine. Possible anti-inflammatory mechanisms include adsorption of luminal antigens produced during the inflammation process, an increase in colonic mucin levels, and modulation of cytokine production by mucosal cells; several effects on proinflammatory cytokines have been demonstrated that contribute to the anti-inflammatory effects of diosmectite (see section 4.4).
4.2 Interactions with Mucus
Diosmectite binds to the mucus layer in the intestines where it induces physicochemical changes in mucopolysaccharides that alter their rheologic properties.[28,29] Droy et al.[29] showed that pretreating rats with diosmectite provided protection against morphologic damage caused by bile salts, an effect believed to be related to reduced penetration of toxins through the mucus layer.
Rateau et al.[30] investigated the effect of diosmectite in a rabbit ileum model in which mucolysis was controlled by sucrase and protease enzymes produced by pathogenic bacteria. Diosmectite inhibited mucolysis and reduced destruction of the luminal surface membranes of most epithelial cells in animals infected with EPEC. Diosmectite did not influence mucus levels in uninfected animals. In anesthetized rats, diosmectite protected the adherent gastric mucus layer from pepsin-induced mucolysis when administered 30 minutes prior to pepsin challenge.[31] When given up to 16 hours prior to pepsin challenge, diosmectite was able to prevent gastric mucosal hemorrhage and histologic epithelial damage. Mucin degradation was also significantly reduced in rats that received diosmectite 30 minutes or 2 hours before pepsin challenge, but the reduction was not significant when diosmectite was administered 16 hours before pepsin challenge. Diosmectite was also found to effectively increase the thickness of the mucus layer in rats shortly after administration. The thickness was greatest at the 30-minute measurement, and had declined to 8% of that maximum 16 hours after administration. The histologic findings suggest that diosmectite mixes with the adherent mucus, rather than forming two separate layers. In addition to binding to the mucus layer, diosmectite may also inhibit the actions of pepsin, as there was evidence of inhibition of pepsin-induced mucolysis in rats that received diosmectite.
It is believed that diosmectite exerts its action on mucus, at least in part, by binding to mucins, thereby protecting them from damage resulting from the presence of inflammation.[27] Diosmectite significantly increased colonic expression of mucin 2, the main secretory gel-forming mucin in the colon. However, the effect is post-transcriptional, as the mucin-2 gene messenger RNA level was unchanged by diosmectite in vivo.
4.3 Adsorption of Toxins
Data from in vivo animal studies and in vitro experiments indicate that diosmectite is able to protect the intestinal mucosa by adsorbing bacteria, bacterial toxins, viruses, and other intestinal irritants.[9,11] Increased gastric emptying associated with administration of a trichothecene mycotoxin was reduced in mice when they were pretreated with diosmectite 4 days earlier, or when diosmectite was incubated with the toxin for 24 hours prior to administration. However, diosmectite had no effect on gastric emptying when it was administered concurrently with the toxin (and with no prior incubation). Diosmectite administered on its own also had no effect on gastric emptying, indicating the effect was dependent on the presence of the toxin.[9] The fact that incubating the toxin with diosmectite in vitro prior to administration was effective in preventing accelerated gastric emptying suggests that diosmectite may be able to adsorb the toxin. However, the findings that diosmectite is normally eliminated within 16 hours and that protection was conferred when diosmectite was administered 4 days before the toxin[9] support an additional mechanism independent of adsorption of the toxin by smectite in the stomach.
The ability of diosmectite to adsorb E. coli and V. cholera heat-labile toxins, ETEC heat-stable toxins, and enterohemorrhagic E. coli verotoxin has been investigated in cell cultures and newborn mice.[32] At the pH of intestinal chyme, diosmectite efficiently adsorbed labile toxins by hydrogen bonding, preventing fixation of the toxins to cellular membrane receptors. Diosmectite adsorbed verotoxin in an acidic environment, but not at an alkaline pH. Stable toxin was only slightly adsorbed.
Diosmectite has been shown to completely bind C. difficile toxins A, B, and C and C. perfringens enterotoxin in vitro at dilutions of 1 : 2–1 : 16, with partial binding observed at greater dilutions.[33] C. difficile endotoxin was >99% bound to diosmectite at dilutions of 1 : 2–1 : 32. The same study also demonstrated that diosmectite had no effect on bacterial growth or the effect of metronidazole in vitro. The ability of diosmectite to minimize the effects of C. difficile enterotoxin B has also been observed in McCoy cell lines.[34] That study also showed that diosmectite was able to eliminate toxic effects of enterotoxins from B. fragilis when incubated in the HT29-C1 human colon adenocarcinoma cell line.
Clark et al.[35] investigated adsorption of rotavirus and coronavirus in vitro by a variety of adsorptive agents. Diosmectite was not one of the agents included in the investigation. However, given that all of the tested agents showed excellent virus-adsorbing properties, it is tempting to speculate that diosmectite may also possess such capabilities.
4.4 Interactions with Cytokines
Compared with controls, diosmectite significantly reduced levels of IL-1β and inhibited the increased synthesis of myeloperoxidase normally seen in colitic rats.[27] This is suggestive of decreased neutrophil infiltration and activation of monocytes, which would be consistent with a decrease in the antigenic load. This scenario was further supported by decreased levels of inducible nitric oxide synthase and histologic findings.
Diosmectite may also modulate the mucosal inflammatory response. Using the HT29 human epithelial cell line as a model for the interface between diosmectite and the colonic epithelium, the same investigators found that diosmectite dose dependently inhibited basolateral secretion of IL-8 by intestinal epithelial cells in response to lipopolysaccharide stimulation.[27] IL-8 is one of the important proinflammatory cytokines released by epithelial cells following penetration of endotoxic or endotoxin-bearing pathogens. Diosmectite also dose dependently reduced IL-1β levels produced by human monocytic cell line THP-1 cells in response to lipopolysaccharide stimulation, suggesting that diosmectite may have potentially greater anti-inflammatory activity if the integrity of the epithelium is impaired. However, it must be noted that these findings are from in vitro studies.
Further evidence of the ability of diosmectite to act from the luminal side of the intestinal epithelium to reduce the consequences of inflammation arises from a study investigating the effect of apical diosmectite on the intestinal dysfunction induced by basal TNFα.[36] Incubation of monolayers of the intestinal cell line HT29-19A with TNFα and interferon-γ altered the intestinal barrier function, resulting in a paracellular leakage in the epithelial layer. Addition of diosmectite completely restored the barrier capacity of the epithelial layer, as measured by a significant reduction in ionic conductance and mannitol and horseradish peroxidase fluxes. Furthermore, diosmectite was found to have no effect on permeability in the absence of TNFα.
4.5 Interaction with Digestive Fluids
Diosmectite has been found to decrease gastric, but not jejunal or colonic, motility in dogs from day 3 of treatment in the absence of diarrhea-producing stimuli.[37] When cholera toxin was also administered, diosmectite administered 3 days later appeared to restore the cholera toxin-induced disruption of GI cyclical activity. Mannitol infusion on its own disrupted gastric and jejunal cyclical migrating motor complexes, which stimulated colonic motility activity and resulted in diarrhea 45–60 minutes after the start of the infusion. When the mannitol infusions were administered 3 or 6 days after diosmectite initiation, disruption of gastric and jejunal activity persisted, but the disturbances in colonic motility were absent, and development of diarrhea was delayed by >7 hours. The investigators postulated that diosmectite probably enhanced fluid absorption by some mechanism. The differing effects suggest that diosmectite may have different mechanisms on different sections of the GI tract under various conditions.
4.6 Effect on Intestinal Permeability
In addition to the pre-clinical evidence, the effect of diosmectite on intestinal permeability has been investigated in children with acute gastroenteritis.[38] Patients received diosmectite 1.5–6 g three or four times daily depending on their bodyweight, or placebo. Diosmectite significantly improved urinary mannitol clearance 2 days after treatment, compared with placebo. This finding that the intestinal absorption of mannitol was superior in diosmectite recipients suggests that the absorptive capability of the intestine had been increased by diosmectite.
4.7 Effect on Secretory Mechanisms
Diosmectite altered the net ion fluxes and fluid changes in favor of absorption, and consequently counteracted microbial-induced water excretion, in rabbit ileal mucosa exposed to ETEC.[30] These effects are believed to be secondary to reduced bacterial mucolysis and diminished destruction of the luminal surface membranes of the intestinal epithelium by the microbial pathogens. Chloride and magnesium adsorption were increased and bicarbonate secretion was decreased by diosmectite; goblet cell degradation was ameliorated. Increased absorption of magnesium indicated that the cellular integrity was preserved. These findings could contribute to the anti-diarrheal effects of diosmectite in infectious diarrhea in humans.
5. Discussion
Diosmectite is available in more than 50 countries and is frequently used with good effect to reduce the duration of diarrhea. However, it is currently not recommended by the WHO for routine use in children with acute diarrhea because of the additional costs and efficacy of ORT.[39] The WHO recently recommended use of zinc as an adjunct therapy to ORT in the treatment of acute diarrhea in children.[39] To date, no studies have shown whether concomitant use of diosmectite will affect zinc absorption. However, it should be noted that because of the adsorbent properties of diosmectite it should be administered at a different time to other medications. Although no cost-effectiveness studies have been published, it is possible that the additional cost of diosmectite is offset by the reduced duration of disease and length of hospital stay and time spent by parents looking after children with diarrhea. It has also been proposed that diosmectite might be useful for managing infectious diarrhea where extensive use of antibacterial agents has led to the emergence of multi-resistant organism strains.[13]
The precise process(es) by which diosmectite acts to decrease diarrhea have yet to be established and appear to be quite complex. Impairment of the structure or function of the intestinal mucosa always occurs with infectious diarrhea[14] and the anti-diarrheal properties of diosmectite probably include protection against damage to the intestinal mucosa by diarrheogenic agents. Current data suggest that multiple mechanisms may contribute to the anti-inflammatory effect, but it is likely that the decrease in proinflammatory cytokines reported in several studies is secondary to effects that occur in the lumen. Diosmectite is not absorbed from the lumen into the epithelial cells[40] and, therefore, probably inhibits some pathogens in the lumen that induce inflammation of the gut wall. Proposed mechanisms by which diosmectite acts at the luminal level include increased thickness of the mucus layer, absorption of or binding to endotoxins, absorption of proteins and antigens associated with inflammation, increase in colonic mucin, and decreased mucolysis[11] (which may also be secondary to enterotoxin adsorption). As previously mentioned (in section 4.2), Rateau et al.[30] determined that diosmectite inhibits mucolysis caused by EPEC infection. In their study, they acknowledge that smectite may have inhibited mucolysis by adsorbing enterotoxins, thereby masking their action on the goblet cells. Diarrhea is probably decreased by the anti-inflammatory effects of diosmectite resulting in amelioration of increased fluid secretion normally associated with inflammation. Changes in the absorptive properties of the intestine in the presence of diosmectite may also alter fluid and electrolyte secretion and absorption, which may also contribute to the anti-diarrheal effects.[37]
While it is tempting to deduce from these data that diosmectite acts as a physical barrier to proinflammatory mechanisms, there are data showing that diosmectite can provide anti-diarrheal activity several days after administration (by which time it would have been eliminated from the intestinal lumen), suggesting that there is also likely to be a reinforcing effect of the natural defense mechanisms contributing to the overall anti-inflammatory effect.[9]
A significant effect of diosmectite on stool output was also recently demonstrated as a primary outcome in two placebo-controlled trials in young children with acute diarrhea.[20] Although not designed with this aim, these studies showed that diosmectite was particularly effective in rotavirus-positive children. This effect could be related to both the higher stool output in rotavirus-positive patients and to the pharmacologic properties of diosmectite. It may also be related to the fact that a pharmacologic effect is more likely demonstrated when symptoms are more pronounced. An additional reason may be that rotavirus itself induces a secretory process at the enterocyte level that could be counteracted by diosmectite.
Oral antibacterials may also be indicated for patients with diarrhea, and diosmectite should not be considered a replacement for antibacterial therapy where it is indicated (e.g. in invasive diarrhea).[12,13] Furthermore, because of the effects of diosmectite on the GI system, other orally administered drugs may be inadequately absorbed when given concomitantly. Therefore, a delay of 60–90 minutes between administration of diosmectite and oral antibacterials or any other orally administered agents that rely on absorption is recommended. ORT, on the other hand, is not adversely affected when administered concomitantly with diosmectite.[14]
6. Conclusion
Diosmectite has demonstrated adsorbent and anti-inflammatory activity in both in vivo and in vitro studies. There are several mechanisms by which diosmectite can treat diarrhea. Diosmectite reduces inflammation, probably via a direct modulatory effect on cytokine production by mucosal cells. It can bind with the mucus barrier and alter its rheologic properties, inhibiting mucolysis and increasing colonic mucin. Diosmectite has also been shown to adsorb toxins and other compounds that can damage the mucus lining, including bacterial enterotoxins and viruses, and it enhances the absorptive capability of the gut in vivo.
Although ORT remains the cornerstone of treatment for mild-to-moderate acute diarrhea, several controlled clinical trials in children with mild-to-moderate acute diarrhea have provided evidence that diosmectite significantly reduces stool output, the duration of diarrhea, stool frequency, the time to improved stool consistency, and the incidence of protracted cases of diarrhea (i.e. >7 days). Because of its lack of systemic absorption, diosmectite is also well tolerated, even by very young children. It can be administered as an adjunct to ORT without affecting its absorption or efficacy, but antibacterial agents need to be administered at least 60–90 minutes before or after diosmectite. The efficacy of diosmectite has been assessed mainly in eight controlled studies in children in developed and developing countries with mild-to-moderate acute diarrhea, both in hospital and ambulatory settings. Studies to determine the cost effectiveness of diosmectite in combination with ORT would also be useful.
Acknowledgements
The preparation of this manuscript was supported by Ipsen, France. Editorial assistance for the development of this manuscript was provided by John McKeogh, Wolters Kluwer Health Medical Communications. C. Dupont has received honoraria for lectures, for the current review, and for previous clinical trials with Ipsen. B. Vernisse has no conflicts of interest that are directly relevant to the content of this review.
References
- 1.Alam NH, Ashraf H. Treatment of infectious diarrhea in children. Pediatr Drugs. 2003;5(3):151–65. doi: 10.2165/00128072-200305030-00002. [DOI] [PubMed] [Google Scholar]
- 2.Gadewar S, Fasano A. Current concepts in the evaluation, diagnosis and management of acute infectious diarrhea. Curr Opin Pharmacol. 2005;5(6):559–65. doi: 10.1016/j.coph.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Thapar N, Sanderson IR. Diarrhoea in children: an interface between developing and developed countries. Lancet. 2004;363(9409):641–53. doi: 10.1016/S0140-6736(04)15599-2. [DOI] [PubMed] [Google Scholar]
- 4.Field M. Intestinal ion transport and the pathophysiology of diarrhea. J Clin Invest. 2003;111(9):931–43. doi: 10.1172/JCI18326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dalby-Payne J, Elliott E. Gastroenteritis in children. Clin Evid. 2004;12:443–54. [PubMed] [Google Scholar]
- 6.Provisional Committee on Quality Improvement: Subcommittee on Acute Gastroenteritis Practice parameter: the management of acute gastroenteritis in young children. Pediatrics. 1996;97(3):424–36. [PubMed] [Google Scholar]
- 7.Wilson MJ. Clay mineralogical and related characteristics of geophagic materials. J Chem Ecolog. 2003;29(7):1525–47. doi: 10.1023/A:1024262411676. [DOI] [PubMed] [Google Scholar]
- 8.Dies J, Miralles L, Tarrasa F, et al. Thermoluminescence response of calcic bentonite subjected to conditions of high nuclear waste underground storage. Radiat Prot Dosimetry. 2002;100(1–4):389–94. doi: 10.1093/oxfordjournals.rpd.a005896. [DOI] [PubMed] [Google Scholar]
- 9.Fioramonti J, Fargeas MJ, Bueno L. Action of T-2 toxin on gastrointestinal transit in mice: protective effect of an argillaceous compound. Toxicol Lett. 1987;36(3):227–32. doi: 10.1016/0378-4274(87)90190-1. [DOI] [PubMed] [Google Scholar]
- 10.Guarino A, Bisceglia M, Castellucci G, et al. Smectite in the treatment of acute diarrhea: a nationwide randomized controlled study of the Italian; Society of Pediatric Gastroenterology and Hepatology (SIGEP) in collaboration with primary care physicians. J Pediatr Gastroenterol Nutr. 2001;32(1):71–5. doi: 10.1097/00005176-200101000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Madkour AA, Madina EM, El-Azzouni OE, et al. Smectite in acute diarrhea in children: a double-blind, placebo-controlled clinical trial. J Pediatr Gastroenterol Nutr. 1993;17(2):176–81. doi: 10.1097/00005176-199308000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Vivatvakin B, Jongpipatvanich S, Harikul S, et al. Control study of oral rehydration solution (ORS)/ORS+dioctahedral smectite in hospitalized Thai infants with acute secretory diarrhea. Southeast Asian J Trop Med Public Health. 1992;23(3):414–9. [PubMed] [Google Scholar]
- 13.Lexomboon U, Harikul S, Lortholary O. Control randomized study of rehydration/rehydration with dioctahedral smectite in ambulatory Thai infants with acute diarrhea. Southeast Asian J Trop Med Public Health. 1994;25(1):157–62. [PubMed] [Google Scholar]
- 14.Narkeviciute I, Rudzeviciene O, Leviniene G, et al. Management of Lithuanian children’s acute diarrhea with Gastrolit solution and dioctahedral smectite. Eur J Gastroenterol Hepatol. 2002;14(4):419–24. doi: 10.1097/00042737-200204000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Gilbert B, Lienhardt A, Palomera S, et al. The efficacy of smectite in acute infantile diarrhea, compared to a placebo and loperamide. Ann Pediatr (Paris) 1991;38(9):633–6. [PubMed] [Google Scholar]
- 16.Lachaux A, Danzon A, Collet JP, et al. Acute infantile diarrhoea: role of treatment with smectite as complement to rehydration. Randomised double-blind study. Int Rev Pediatr. 1986;163:29–31. [Google Scholar]
- 17.Zong S, Chao YM, Qu Y, et al. Study on Smecta therapy for acute diarrhea in infants. J Tianjing Med Univ. 1997;3:60–3. [Google Scholar]
- 18.Osman GAH, Mahomoud SAR, El-Shakankiry HM, et al. An adsorbent! Role in the management of acute diarrhea in infants and children. Ain Shams Med J. 1992;13:10. [Google Scholar]
- 19.Szajewska H, Dziechciarz P, Mrukowicz J. Meta-analysis: smectite in the treatment of acute infectious diarrhea in children. Aliment Pharmacol Ther. 2006;23(2):217–27. doi: 10.1111/j.1365-2036.2006.02760.x. [DOI] [PubMed] [Google Scholar]
- 20.Dupont C, Kok Foo JL, Garnier P, et al. Oral diosmectite reduces stool output and diarrhea duration in children with acute watery diarrhea [online]. Available from URL: http://www.cghjournal.org/inpress [Accessed 2009 Feb 24] [DOI] [PubMed]
- 21.Berkes J, Viswanathan VK, Savkovic SD, et al. Intestinal epithelial responses to enteric pathogens: effects on the tight junction barrier, ion transport, and inflammation. Gut. 2003;52(3):439–51. doi: 10.1136/gut.52.3.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Droy-Lefaix MT, Bueno L. Inflammatory cascade and diarrhea: a new approach. Acta Endoscopica. 2003;33(5):773–80. doi: 10.1007/BF03002623. [DOI] [Google Scholar]
- 23.Hecht G, Savkovic SD. Review article: effector role of epithelia in inflammation: interaction with bacteria. Aliment Pharmacol Ther. 1997;11(Suppl.3):64–8. doi: 10.1111/j.1365-2036.1997.tb00810.x. [DOI] [PubMed] [Google Scholar]
- 24.Jung HC, Eckmann L, Yang S-K, et al. A distinct array of proinflammatory cytokines is expressed in human colon epithelial cells in response to bacterial invasion. J Clin Invest. 1995;95(1):55–65. doi: 10.1172/JCI117676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amieva MR. Important bacterial gastrointestinal pathogens in children: a pathogenesis perspective. Pediatr Clin North Am. 2005;52(3):749–77. doi: 10.1016/j.pcl.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 26.Dong Y, Zeng CQ, Ball JM, et al. The rotavirus enterotoxin NSP4 mobilizes intracellular calcium in human intestinal cells by stimulating phospholipase C-mediated inositol 1,4,5-trisphosphate production. Proc Natl Acad Sci U S A. 1997;94(8):3960–5. doi: 10.1073/pnas.94.8.3960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gonzalez R, de Medina FS, Martinez-Augustin O, et al. Anti-inflammatory effect of diosmectite in hapten-induced colitis in the rat. Br J Pharmacol. 2004;141(6):951–60. doi: 10.1038/sj.bjp.0705710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moré J, Benazet F, Fioramonti J, et al. Effects of treatment with smectite on gastric and intestinal glycoproteins in the rat: a histochemical study. Histochem J. 1987;19(12):665–70. doi: 10.1007/BF01676173. [DOI] [PubMed] [Google Scholar]
- 29.Droy MT, Drouet Y, Geraud G, et al. Spinnability: a new approach to intestinal stress and its therapy. Gastroenterol Clin Biol. 1985;9:119–21. [PubMed] [Google Scholar]
- 30.Rateau JG, Morgant G, Droy-Priot MT, et al. A histological, enzymatic and water-electrolyte study of the action of smectite, a mucoprotective clay, on experimental infectious diarrhea in the rabbit. Curr Med Res Opin. 1982;8(4):233–41. doi: 10.1185/03007998209109772. [DOI] [PubMed] [Google Scholar]
- 31.Leonard A, Droy-Lefaix MT, Allen A. Pepsin hydrolysis of the adherent mucus barrier and subsequent gastric mucosal damage in the rat: effect of diosmectite and 16, 16 dimethyl prostaglandin E2. Gastroenterol Clin Biol. 1994;18(6–7):609–16. [PubMed] [Google Scholar]
- 32.Brouillard MY, Rateau JG. Adsorption potency of 2 clays, smectite and kaolin on bacterial enterotoxins: in vitro study in cell culture and the intestine of newborn mice. Gastroenterol Clin Biol. 1989;13(1):18–24. [PubMed] [Google Scholar]
- 33.Weese JS, Cote NM, deGannes RV. Evaluation of in vitro properties of di-tri-octahedral smectite on clostridial toxins and growth. Equine Vet J. 2003;35(7):638–41. doi: 10.2746/042516403775696384. [DOI] [PubMed] [Google Scholar]
- 34.Martirosian G, Rouyan G, Zalewski T, et al. Dioctahedral smectite neutralization activity of Clostridium difficile and Bacteroides fragilis toxins in vitro. Acta Microbiol Pol. 1998;47(2):177–83. [PubMed] [Google Scholar]
- 35.Clark KJ, Sarr AB, Grant PG, et al. In vitro studies on the use of clay, clay minerals and charcoal to adsorb bovine rota virus and bovine coronavirus. Vet Microbiol. 1998;63(2–4):137–46. doi: 10.1016/S0378-1135(98)00241-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mahraoui L, Heyman M, Plique O, et al. Apical effect of diosmectite on damage to the intestinal barrier induced by basal tumour necrosis factor. Gut. 1997;40(3):339–43. doi: 10.1136/gut.40.3.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fioramonti J, Droy-Lefaix MT, Bueno L. Changes in gastrointestinal motility induced by cholera toxin and experimental osmotic diarrhea in dogs: effects of treatment with an argillaceous compound. Digestion. 1987;36(4):230–7. doi: 10.1159/000199423. [DOI] [PubMed] [Google Scholar]
- 38.Dupont C, Moreno JL, Barau E, et al. Effect of diosmectite on intestinal permeability changes in acute diarrhea: a double-blind placebo-controlled trial. J Pediatr Gastroenterol Nutr. 1992;14(4):413–9. doi: 10.1097/00005176-199205000-00007. [DOI] [PubMed] [Google Scholar]
- 39.USAID, UNICEF, World Health Organization. Diarrhoea treatment guidelines [online]. Available from URL: http://whqlibdoc.who.int/publications/2005/a85500.pdf [Accessed 2009 Feb 2]
- 40.European Patent Office. European patent application [online]. Available from URL: https://publications.european-patient-office.org/PublicationServer/getpdf.jsp?cc=EP&pn=1747775&ki=A1


