Abstract
Introduction:
Adults who engage in regular physical activity have lower rates of morbidity and mortality than those who do not. Exercise videogames may offer an attractive, sustainable alternative or supplement to traditional modes of exercise. This study compared exercise videogames with standard exercise modalities for improving uptake and maintenance of moderate to vigorous physical activity, and health risk indices.
Study design:
A three-arm clinical RCT including 12 weeks of supervised laboratory-based moderate to vigorous physical activity followed by 6 months follow-up.
Setting/participants:
This study was conducted at a university affiliated hospital research lab. Healthy, sedentary adults were eligible.
Interventions:
This study compared a 12-week program of supervised exercise videogames versus standard exercise (e.g., treadmill) versus control. Data were collected from January 2012 to September 2017 and analyzed in 2018.
Main outcome measures:
The primary outcome was weekly minutes of moderate to vigorous physical activity at end of treatment, assessed at 3 and 6 months post-intervention by using self-report and accelerometer data. Health risk indices (e.g., HbA1c, lipids) were also assessed.
Results:
Participants (N=283) had an average age of 46.2 ±13.5 years; 79% were female. At end of treatment, those in the exercise videogame arm engaged in 30 minutes/week more moderate to vigorous physical activity compared with standard exercise and 85 more minutes/week than controls (all p<0.05). Exercise videogame participants had greater reductions in cholesterol, HbA1c, and body fat versus other groups. Reductions in cholesterol were twice as large in exercise videogame versus standard participants.
Conclusions:
Exercise videogames produced greater uptake and maintenance of moderate to vigorous physical activity compared with standard exercise and improvements in multiple health risk indices. Exercise videogames may promote sustainable physical activity with significant health benefits.
Trial registration:
This study is registered at www.clinicaltrials.gov NCT03298919.
INTRODUCTION
Physical inactivity is a major leading cause of preventable death among Americans.1 National guidelines recommend that adults engage in at least 30 minutes of moderate-intensity or 20 minutes of vigorous-intensity aerobic physical activity (PA) on 5 or more days per week, or a combination of both.2–4 Despite the numerous health benefits associated with moderate to vigorous PA (MVPA) and health risks associated with inactivity,5–12 only about half of U.S. adults self-report being sufficiently active to meet national guidelines,13,14 and rates drop below 10% when measured by accelerometer.15 Even among those who initiate a PA program, long-term adherence is a challenge, with approximately half stopping within the first 6 months.16–20 There is a great need for effective approaches that not only encourage PA uptake but also promote maintaining these behaviors.
A growing body of research has begun to examine physically interactive videogames that require substantial body movement and exertion for continued play. These exercise videogames (EVGs), also called active videogames, include platforms such as the Nintendo Wii, Xbox 360 Kinect, and dance simulation products. Studies have demonstrated that playing EVGs elicits greater energy expenditure compared with rest and inactive (sedentary) videogames,21–24 and some EVGs have evidenced energy expenditure commensurate with MVPA—similar to walking and cycling, at approximately 3–6 METs,25,26 increasing energy expenditure up to 300% above resting levels.27 In addition, EVGs have been reported to result in an enjoyable exercise experience, even when working at higher intensities.28–30 These findings suggest that EVGs may present a viable, practical, and attractive alternative to traditional modes of exercise. Although promising, most EVG research has been conducted with children and adolescents, with relatively few studies in adults,31,32 and adult studies are often limited to the acute effects of EVGs on energy expenditure.24,33–37 Longitudinal studies in adults have tended to focus on elderly populations and have examined the effect of EVGs on outcomes, such as balance,38–42 cognition,43 and depression.44 Few studies have examined cardiovascular outcomes, most being small pilot studies (see review by Street et al.).32
The goals of this study were to examine the effect of EVGs on (1) time spent in MVPA following a 12-week supervised laboratory intervention, (2) cardiovascular health risk indices, and (3) maintenance of MVPA after the conclusion of the intervention. Study hypotheses were (1) at week 12, EVG and standard exercise participants will engage in significantly more minutes of MVPA than controls, (2) at week 12, EVG participants will engage in significantly more MVPA than standard participants, (3) adherence to recommended PA will be greater in the EVG arm than in the standard arm, (4) at follow-up, EVG participants will engage in significantly more MVPA than standard participants, (5) both EVG and standard groups will show significantly greater improvement in cardiovascular health risk indices than controls, and (6) EVG participants will show greater improvement in these measures than standard participants.
METHODS
Study Population
The Wii Heart Fitness study is a three-arm RCT using a parallel design. Advertisements were placed on Internet sites and local radio stations, and as flyers in local retail outlets. Ads requested “generally healthy adults” who did not exercise regularly and were interested in a healthier lifestyle. Individuals calling in response to advertisements were screened for eligibility. Eligible individuals attended an in-person orientation session and provided written informed consent. Consented individuals attended a second visit to complete baseline assessments and receive randomization assignments that were generated by the study biostatistician and delivered to the study research assistant via e-mail on the day of the randomization visit.
Participants were randomized (1:1 ratio) into a 12-week program of (1) EVGs using the Nintendo Wii and X-Box 360 Kinect, (2) standard aerobic exercise equipment including treadmills and stationary bikes, or (3) weekly mailed health and wellness materials (control). The randomization scheme was generated in R, version 3.1.0, based on a permuted block randomization procedure with small, random sized blocks. The sequence was generated by the study statistician. Assessments were conducted at baseline (prior to randomization), at end of treatment (EOT; EOT=week 12), with follow-up assessments at 3 and 6 months after EOT (6 and 9 months after enrollment). All procedures were approved by the Miriam Hospital IRB. Details regarding study design and rationale are published elsewhere.45
Eligible participants were aged >18 years, currently participating in <60 minutes of moderate or 30 minutes of vigorous PA per week, and willing to commit to the demands of the study protocol. Exclusion criteria included BMI >40, current or planned pregnancy, recent (<6 months) hospitalization, hypertension, cardiovascular or pulmonary disease, diabetes, and orthopedic conditions that interfere with PA. To avoid contamination, individuals were also excluded if they used an EVG at home (Figure 1).
Figure 1. CONSORT diagram.
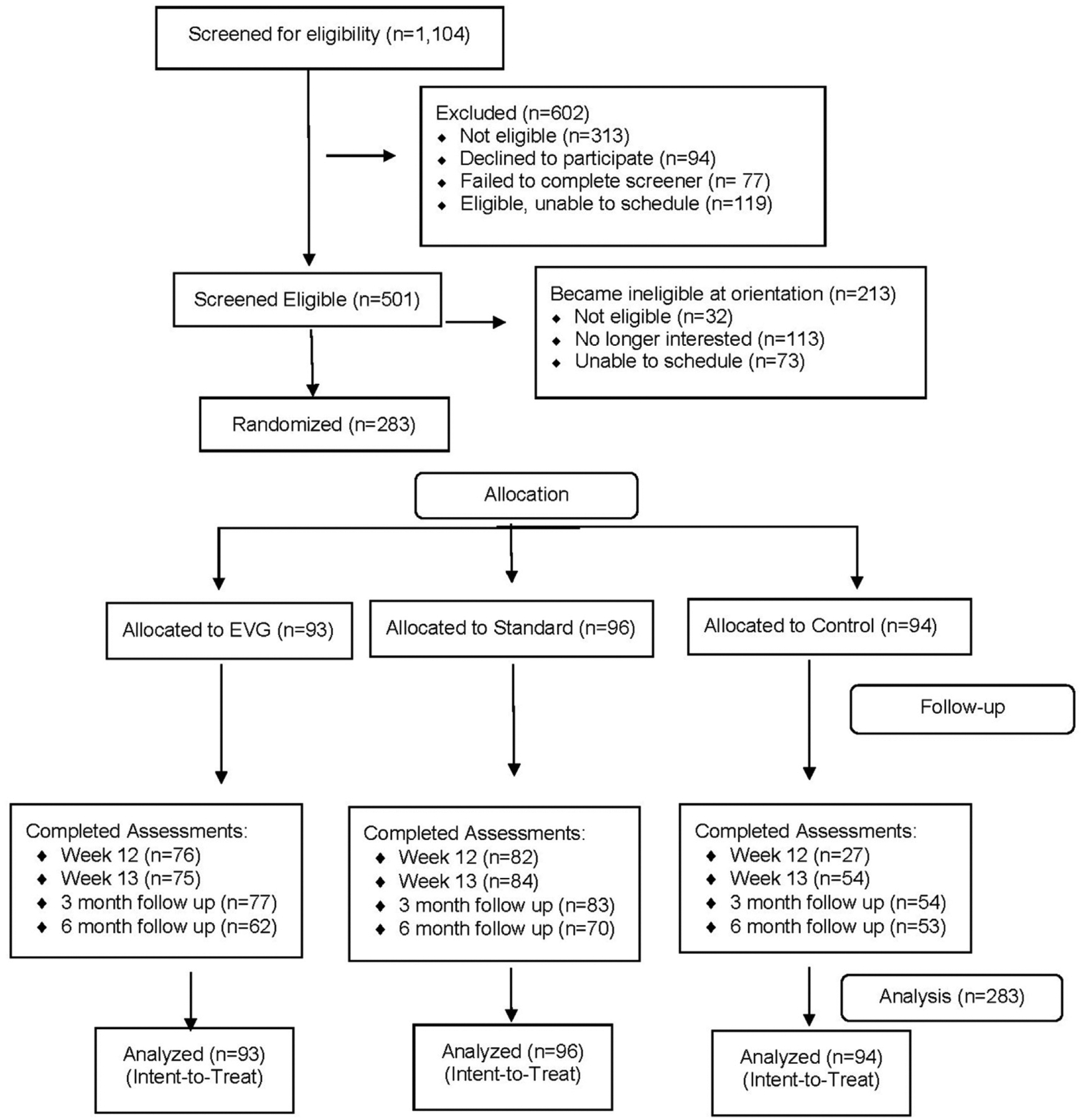
EVG, exercise video games.
Measures
The goal for both EVG and standard interventions was to increase MVPA to meet national guidelines for aerobic PA.3 Heart rate (HR) was recorded using an HR monitor (Polar RS400) worn by each participant at every session. The target HR range was calculated by using the Karvonen Formula,46 and participants were instructed to exercise in a perceived exertion range of “fairly light” to “somewhat hard” (11 – 13 on the Borg perceived exertion scale).47 HR was continuously monitored during each session, and if HR fell below the moderate-intensity range, study staff encouraged the participant to increase their speed or intensity or both.
Participants randomized to EVG arm attended 12 weeks of 50-minute EVG sessions, held three times a week in a hospital-based lab. Each session included 5- to 10-minute warm-up and cool-down components, and ≅ 40 minutes of moderate- to vigorous-intensity exercise, using a variety of EVGs available for the Xbox 360 (Kinect) and Wii platforms. Participants selected games from those offered by the study and were permitted up to two changes of game within each session. All games were focused on aerobic exercise training to produce a moderate- or vigorous-intensity exercise response during game play.
Participants in the standard exercise program arm attended sessions in a lab that was equipped with treadmills and stationary bicycles. Sessions followed the same protocol for session duration (50 minutes), including warm up and cool down periods.
Control participants were mailed print materials weekly for 12 weeks on a variety of general health-related topics (e.g., back health, sun protection, health screenings). Materials included health-oriented books (e.g. Eat This Not That) and printed pamphlets from reliable sources (e.g., American Heart Association, American Diabetes Association). They were also sent items (e.g., sun screen, stress balls, hand sanitizers) that were relevant to the printed materials. No PA promotion materials were provided, and participants were asked to continue their normal activity levels.
An important study goal was to examine whether individuals would maintain PA after the laboratory-based program. Procedures to facilitate maintenance were implemented at EOT. After week 12, EVG participants were given a game console (Kinect or Wii) and EVGs of their choice to facilitate home practice. Standard exercise participants were given a print-based PA program, a list of local gyms, walking trails and other local PA resources, and a pedometer. Control participants received health promotion printed materials monthly during this maintenance period.
Demographic information collected at baseline included age, sex, race/ethnicity, marital status, education, employment status, and household income.
MVPA (minutes/week) was measured at baseline, EOT (week 12), 1-week post-EOT (week 13) and both 3- and 6-month follow-up, using the interviewer-administered 7-day Physical Activity Recall (PAR) interview by study staff blind to participant randomization assignment.48,49 Staff recorded session attendance and total exercise time. The primary outcome was PAR.48,49 The PAR is a reliable, validated instrument sensitive to change in PA.50–53 To avoid confounding session attendance during the final week of the lab-based intervention (week 12), PAR data were collected at week 12 (EOT) and week 13 (1-week post-EOT). All participants wore an Actigraph Motion Monitor (model GTX3) for a 7-day period prior to each assessment point.
Resting HR and blood pressure were recorded at each assessment visit. Dual energy x-ray absorptiometry was used at baseline and EOT to obtain body composition data including body fat (trunk, total, and percentage).54 Height was measured at baseline and weight was measured at all assessment points using a calibrated balance beam scale. BMI was calculated as weight (kg)/height in meters squared (m2). Waist and hip circumference were measured at each assessment point. Blood samples for lipid profile assay (i.e., total cholesterol, high- and low-density lipoproteins [LDL], and triglycerides) and HbA1c were drawn by a phlebotomist at a hospital-based laboratory at baseline and EOT. Using the Balke protocol, a sub-maximal exercise tolerance test (maximal oxygen uptake [VO2] submax) was conducted to assess participant’s estimated cardiorespiratory fitness at baseline and EOT, using time on treadmill as the outcome variable.55
Dietary patterns were assessed at baseline, EOT, and both 3-month and 6-month follow-up using the Rate Your Plate (RYP) instrument,56 which is a 24-item tool capturing information on fat intake, animal and dairy protein, fruit, vegetables, whole grains, snacks, and sweets. Scores range from 24 to 72, with higher scores indicating better diet quality. Details of quality control and other process measures are published elsewhere.45
The primary outcome for this study was weekly minutes of MVPA at EOT. Effect sizes for the EVG arm were based on data from the previous pilot study.57 Effect sizes for the standard and control arms were based on previous studies.58–61 The anticipated mean minutes MVPA reported at EOT would be 124.6 (SD=39.27) for EVG, 71.5 (SD=67.3) for standard, and 41.3 (SD=41.6) for controls. Eighty-three participants randomized to each arm at baseline would provide sufficient power (>80%) to detect a difference in MVPA among all three arms, using a two-tailed significance level α=0.05. The total of 249 participants randomized at baseline included adjustment for 20% attrition. Because effect estimates for the EVG arm were based on pilot data,57 the targeted recruitment sample size was increased to 100 per arm. Recruitment started January 15, 2012 and was completed on September 20, 2016. Follow-ups were completed on September 30, 2017.
Statistical Analysis
Between-group differences in baseline demographics and PA were examined using ANOVA for continuous variables, chi-square tests for categorical variables, and non-parametric tests for skewed data. Variables not balanced by randomization were adjusted for in subsequent analyses. Differences in the number of sessions attended and length of exercise sessions between EVG and standard were compared using ANOVA.
Self-reported PA is subject to high variation, and normalizing transformations (e.g., natural logarithm) failed to bring the data toward normality. Therefore, the median minutes/week of MVPA was modeled using a series of quantile regression models (model median outcomes instead of mean). Median minutes/week of MVPA was regressed on group and baseline value of the outcome. Models were run separately for EOT and follow-up data. Model specification allowed for all pairwise comparisons (EVG versus standard, EVG versus control, standard versus control).
Longitudinal models implemented with generalized estimating equations with robust SEs were used to test between-group differences in the odds of meeting American College of Sports Medicine criteria for MVPA at EOT and follow-up.
Finally, self-reported MVPA minutes (PAR) were validated against ActiGraph data at each follow-up using Spearman rank correlations. Between-group differences in objectively measured MVPA were tested using a similar analytic approach.
A series of longitudinal mixed effects regression models, with subject-specific intercepts to adjust for repeated measures within participant over time were used to test group effects on secondary outcomes, including cardiorespiratory fitness (estimated VO2max) and cardiovascular risk indicators (resting HR, peak exercise HR, waist/hip circumference, blood lipids). Models for physiologie outcomes were further adjusted for changes in diet (RYP instrument).
All analyses were conducted on the intent-to-treat sample, with all randomized participants included in the analysis. Models used a likelihood-based approach to estimation and thus made use of all available data without directly imputing missing outcomes. Analysis was carried out using SAS, version 9.3, and significance value was set at α=0.05.
RESULTS
Participants (N=283) were predominantly female (79.1%), employed (79.6%), white (81.5%), and married/partnered (60.8%). Average participant age was 46.2 years (SD=13.5, range, 20–79) and median MVPA was 30 minutes/week (IQR, 0–90). There were no significant between-group effects on baseline demographics or PA levels (p>0.05) (Table 1). In the EVG condition, the most frequently played games used the Xbox 360 Kinect. Titles (and percentage of all games played) included Your Shape Fitness Evolved (34.45%), Kinect Adventures (23.07%), Zumba (20.29%), Kinect Sports (15.85%), and The Biggest Loser (5.28%).
Table 1.
Baseline Descriptives by Group (N=283)
| Variable | Control, n (%) (n=94) | Standard, n (%) (n=96) | EVG, n (%) (n=93) | All, n (%) |
|---|---|---|---|---|
| Gender, % female | 74 (78.7) | 74 (77.9) | 75 (80.6) | 223 (79.1) |
| Employed, %yes | 77 (84.6) | 72 (77.4) | 70 (76.9) | 219 (79.6) |
| Marital status, married/partnered | 58 (65.2) | 54 (60.7) | 52 (56.5) | 164 (60.8) |
| Education, at least some college | 80 (88.9) | 79 (89.8) | 83 (91.2) | 242 (90.0) |
| Ethnicity, % Hispanic | 4 (5.7) | 7 (8.6) | 8 (10.5) | 19 (8.4) |
| Race, % white | 78 (85.7) | 77 (82.8) | 70 (76.1) | 225 (81.5) |
| Age, years, mean (SD) | 47.8 (11.3) | 45.7 (15.0) | 45.1 (14.0) | 46.2(13.5) |
| MVPA m i n utes/week (PAR), mean (SD) | 51.7 (76.8) Median=27.5 |
54.9 (90.9) Median=30 |
63.8 (72.5) Median=40 |
56.7 (80.4) Median=30 |
Note: Frequency counts and percentages presented. There were no significant between-group differences at baseline (p>0.05). EVG, exercise video games; MVPA, moderate to vigorous physical activity; PAR, 7 Day Physical Activity Recall assessment.
Participants in EVG and standard conditions did not differ with respect to mean number of sessions over 12 weeks or length of exercise sessions (p>0.05). EVG participants attended an average of 27.11 (SD=9.81) sessions and standard participants attended an average of 27.45 (SD=7.85) sessions during the 12-week intervention. Participant retention was 88%, with no differences between groups.
Unadjusted median minutes/week of MVPA by arm over time and unadjusted secondary (physiologic outcomes) are presented in Table 2. The adjusted models show significant between-group differences in median minutes/week of MVPA at EOT. Median minutes/week of MVPA among EVG participants at EOT was 85 minutes greater than that of controls (β=85.67, 95% CI=36.97, 134.38). Similarly, standard participants engaged in significantly greater minutes at EOT compared with control (β=55.67, 95% CI=7.66, 103.70). Models show that EVG participants had significantly greater median MVPA compared with standard at EOT (β=30.00, 95% CI=4.46, 64.46).
Table 2.
Unadjusted MVPA and Secondary (Physiological) Outcomes Over Time by Group
| Variable | Control | Standard | EVG |
|---|---|---|---|
| Self-reported minutes/week of MVPA | 28 (82.5) | 30 (90) | 40 (100) |
| Baseline | 105 (185) | 150 (100) | 210 (110) |
| EOT | 90 (163.75) | 107 (97.5) | 150 (155) |
| Week 13 follow-up | 105 (217.5) | 108 (142.5) | 125 (185) |
| LDL cholesterol (mg/dl) | |||
| Baseline | 139.80 (46.88) | 138.52 (41.31) | 138.41 (47.95) |
| EOT | 145.53 (45.17) | 142.86 (39.92) | 139.29 (46.99) |
| HDL cholesterol (mg/dl) | |||
| Baseline | 55.32 (13.50) | 56.24 (14.71) | 55.79 (16.82) |
| EOT | 56.59 (12.99) | 55.50 (13.72) | 55.07 (14.63) |
| Total cholesterol (mg/dl) | |||
| Baseline | 194.11 (36.36) | 191.36 (39.21) | 193.85 (42.07) |
| EOT | 194.52 (32.21) | 191.47 (32.69) | 190.55 (36.55) |
| Triglycerides (mg/dl) | |||
| Baseline | 106.50 (56.41) | 108.46 (60.19) | 112.54 (82.77) |
| EOT | 102.30 (50.93) | 103.51 (50.89) | 107.28 (64.37) |
| A1c (mmol/mol) | |||
| Baseline | 5.47 (0.37) | 5.46 (0.38) | 5.49 (0.35) |
| EOT | 5.49 (0.37) | 5.48 (0.37) | 5.46 (0.35) |
| % Body fat | |||
| Baseline | 39.60 (6.58) | 38.99 (6.93) | 39.28 (7.27) |
| EOT | 39.02 (6.88) | 38.55 (6.83) | 39.30 (7.11) |
| % Trunk fat | |||
| Baseline | 39.83 (6.59) | 38.53 (7.67) | 39.36 (7.76) |
| EOT | 39.12 (6.94) | 37.98 (7.76) | 39.65 (7.98) |
| Resting diastolic BP (mmHg) | |||
| Baseline | 71.79 (13.90) | 71.75 (14.42) | 68.05 (13.00) |
| EOT | 67.31 (15.60) | 70.81 (13.34) | 68.94 (8.82) |
| Resting systolic BP (mmHg) | |||
| Baseline | 120.03 (21.84) | 120.72 (22.73) | 116.32 (21.32) |
| EOT | 122.65 (14.68) | 119.42 (18.43) | 115.94 (18.43) |
| Diet (RYP: raw score) | |||
| Baseline | 54.47 (6.43) | 54.84 (7.50) | 55.73 (5.42) |
| EOT | 55.68 (5.87) | 56.16 (7.30) | 57.81 (5.40) |
| Waist circumference (cm) | |||
| Baseline | 96.65 (12.29) | 93.75 (14.85) | 95.81 (14.98) |
| EOT | 96.33 (15.15) | 93.13 (12.79) | 95.77 (13.96) |
| Hip circumference (cm) | |||
| Baseline | 109.82 (10.52) | 107.03 (10.30) | 107.15 (15.73) |
| EOT | 108.47 (11.05) | 105.28 (10.55) | 106.91 (12.14) |
Note: Mean (SD) are presented. There were no significant between-group differences at baseline (p>0.05).
BP, blood pressure; cm, centimeters; EOT, end of treatment; EVG, exercise video games; HDL, high density lipoprotein cholesterol; LDL, low density lipoprotein cholesterol; mg/dl, milligrams per deciliter; mmHg, millimeters of mercury; mmol/mol, millimoles per mole; MVPA, moderate to vigorous physical activity; RYP, Rate Your Plate dietary assessment.
When considering follow-up MVPA outcomes at 1-week post EOT (Week 13), EVG outperformed both control (β=74.13, 95% CI=30.31, 117.95) and standard (β=52.78, 95% CI=13.81, 91.74) with no significant differences between standard and control. At 6 months, EVG participants had significantly greater median minutes/week of MVPA compared with control (β=16.00, 95% CI=0.91, 75.91). There was no difference in MVPA at 6 months between standard and control and a trend for EVG versus standard (β=8.31, 95% CI= −7.81,64.43).
At EOT, 80.3% of EVG participants were meeting national guidelines for PA (≥150 minutes/week of MVPA) vs 69.3% of standard and 33.3% of controls. At 1-week post EOT, these rates dropped to 57.3%, 29.8%, and 25.9% of EVG, standard and controls, respectively. At 6 months, these rates were 47.5%, 35.7%, and 40.7% for EVG, standard, and controls, respectively. These constitute significant between-group differences at both EOT and 1-week post-EOT and are presented in Figure 2. Analysis of objectively measured MVPA (ActiGraph) showed significant correlations with self-reported MVPA (ρ=0.30, p<0.001 at baseline, ρ=0.25, p<0.001 at EOT and ρ=0.60, p<0.001 at follow-up) but no significant between-group differences at EOT or follow-up (p>0.05). The authors note that although correlations at baseline and EOT were significant, they were also modest in size.
Figure 2. AORs for between group differences in meeting national guidelines for MVPA.
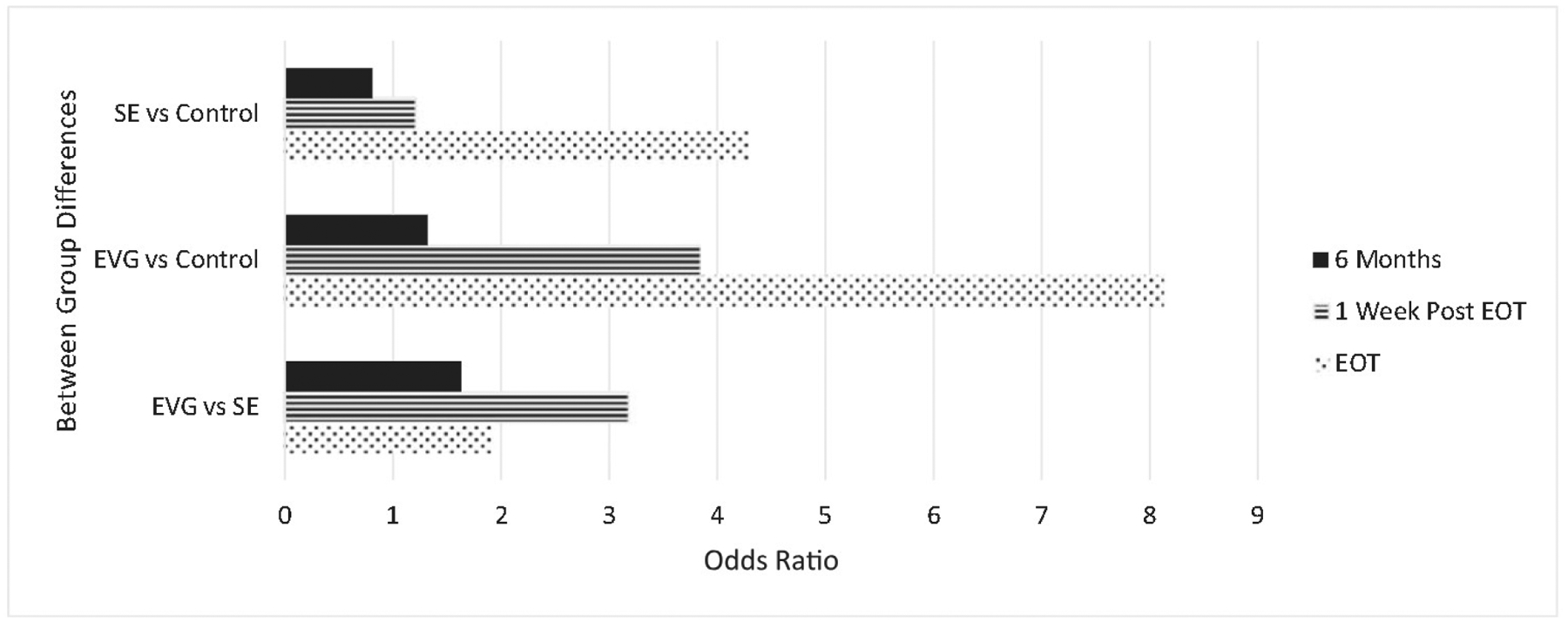
EOT, end of treatment; EVG, exercise video games; MVPA, moderate to vigorous physical activity.
Models of secondary outcomes at EOT suggest significant differences between EVG and control with respect to LDL cholesterol (β= −13.67, SE=6.88, p=0.04), HbA1c (β= −0.06, SE=0.04, p=0.02), trunk fat (β= −502.41, SE=287.54, p=0.05), total fat (β= −940.76, SE=481.59, p=0.05), percentage body fat (β= −1.05, SE=0.45, p=0.02; Table 2), and diet (β=2.00, SE=0.90, p=0.02). There were significant differences between EVG and standard in diet (RYP; β=1.48, SE=0.86, p=0.05). Differences between EVG and standard groups for LDL cholesterol, and percentage body fat were not significant. There were no differences between standard and control on these variables (p>0.05). With respect to fitness testing (VO2 submax) at EOT, standard participants had significantly higher time on treadmill versus control (p=0.002) and versus EVG (p=0.014).
DISCUSSION
The Wii Heart Fitness trial is the first longitudinal trial to examine the (1) effects of EVGs on both the uptake and maintenance of PA and (2) effects on measures of cardiovascular risk. The results are exciting, demonstrating change in all the hypothesized directions, providing support for continued inquiry in diverse samples, and a need for investigation of potential mechanisms of action (i.e., mediators) responsible for differences in PA uptake between EVG and standard approaches.
This study demonstrated that use of EVGs resulted in significantly more participation in MVPA compared with standard modes of exercise following a 12-week supervised intervention, and that EVGs continued to outperform standard exercise modes through a 6-month follow-up period. At EOT, EVG participants were nearly twice as likely to be meeting or exceeding national guidelines for PA compared with those given in the standard intervention. These differences were not explained by differences in program attendance. Differences at week 13 (1 week after EOT) were more dramatic, with EVG participants being over three times more likely to meet national guidelines for MVPA resulting from a rapid decline in the standard intervention group. These differences in meeting national guidelines persisted through the final follow-up, with the standard intervention group approximating the control group at the final follow-up visit.
Gamification, the process of adding enhancements that provide motivational affordances to create a game-like experience, may promote psychological changes and enhance behavioral outcomes.62 These enhancements typically include features such as awarding points, leaderboards, badges, levels, rewards, feedback, and challenges. A study by Patel and colleagues63 showed that a PA intervention for adults and their families was significantly more effective in increasing walking when gamification was incorporated into the intervention. Those given the game-based intervention walked an average of 1 mile per day more than controls. Similar to the study by Patel, the current study found that although PA diminished during the follow-up period among participants, MVPA continued to remain significantly higher among those in the EVG arm than in the comparison arms. Moreover, unlike the study by Patel, the present trial did not incentivize PA participation or offer rewards beyond what were programmed into the games themselves (e.g., points, additional levels). Thus, it appears that EVGs may be a sustainable as well as efficacious method for promoting PA participation. Although gamification principles have been used for health and fitness interventions and apps, results of these studies have been inconsistent, and most studies have not incorporated behavioral theory to aid in understanding how and why games may work to promote PA or behavior change more broadly.64–66 Research has suggested that the relative impact of these features may differ depending on the user, the context, and the behavior target in question.64 By using features of gamification, EVGs may assist in the internalization of motivation for PA. Additional work is needed to understand the constructs and behavioral principles underlying the observed differences in PA uptake between EVG and standard exercise modalities. Further research is also needed to understand which features of EVGs have the most impact on PA engagement, for which individuals, and the development of intrinsic motivation that generalizes to outside-of-game PA, thus leading to sustainability.
Equally important to achieving PA goals, it is necessary to establish whether individuals will voluntarily engage in EVGs with frequency and duration sufficient to produce changes in health and fitness.67 Population participation levels in PA are low, and among those who begin a program of PA, maintenance is also low, suggesting that PA has not proven to be an intrinsically motivating activity for the majority of the population.16,17,20,68,69 The present study demonstrated maintenance of PA in a real-world environment that also provided some accountability. Accountability and associated social support are known to promote maintenance of health behaviors including PA.70 EVGs are designed to be enjoyable, but their hedonic value does not rely solely on direct enjoyment of PA per se. Thus, EVGs may contribute to increasing engagement in PA through mechanisms such as enjoyment and intrinsic motivation. Participants randomized to EVGs also showed improvement in indices of cardiovascular risk including LDL cholesterol and body fat (trunk, total, and percentage), compared with controls.
HbA1c level is continuously related to risk of all-cause, cardiovascular, and ischemic heart disease mortality, with lowest rates seen in those with HbA1c concentrations below 5.0%.71,72 For HbA1c values of less than 5.0%, 5.0% to 5.5%, 5.5% to 6.0%, 6.0% to 6.5%, and more than 6.5%, the multivariable-adjusted hazard ratios for coronary heart disease are 0.96, 1.00, 1.23, 1.78, and 1.95, respectively.73 In this study, those in the EVG condition were able to diminish HbA1c levels below 5.5%, changing the hazards of coronary heart disease by at least 23% based on epidemiologic evidence across the whole population of those who do not have diabetes.71
In addition, multiple studies have traced linear relationships between LDL levels and major adverse cardiac events up to levels below 70 mg/dL to support the clinical relevance of the current findings.74 From this meta-analysis, every 0.5 mmol/L (19 mg/dL) decrease in LDL cholesterol levels was associated with a 12% decrease in the 5-year risk of cardiovascular disease (one third of that effect, based on results of this study, would be an approximately 4% lowering of the 5-year risk).
PA guidelines are given for the promotion of health or regression of disease course. Demonstrating that PA guidelines can be met and maintained using EVGs further supports the benefits of PA and provides individuals with a new vehicle for being physically active to enhance their health. Although individuals in the standard condition walked longer in the EOT fitness walking test compared with EVG participants, it is likely the result of a practice effect resulting from specificity of training, because most of the standard participants in this trial used treadmill walking as their primary exercise mode. A recent study of dance-based EVGs in 12 women also showed improvements in physiological health markers, such as total serum cholesterol, triglycerides, and LDL cholesterol.75 Recent reviews76 have suggested that EVGs may provide an effective means of reducing both cardiovascular risk factors and risk of type 2 diabetes, although studies to date tend to be small, with inconsistent results and frequently poor or moderate méthodologie quality that limit the ability to draw conclusions about the specific impact of EVGs on each risk factor among different populations and disease conditions.
Limitations
Anticipated limitations included differential dropout between groups, a possible lack of change in health risk indices if the participants did not achieve the MVPA goals, and the artificial environment of a lab-based study versus in-home EVG use. Differential dropout did not occur, the EVG and standard groups did achieve the MVPA goals, and improvements were seen in health risk indices. It is important to note that although the lab-based portion of the intervention provided a “clean and controlled” environment to promote exercise initiation, it also provided a supportive environment for the uptake of PA in a structured setting. It remains unclear whether and to what extent individuals might take up regular exercise using EVGs in a different or less structured environment (e.g., at home). Thus, it is unclear whether results obtained in this study would generalize to a larger population of individuals who might buy and use EVGs at home without any laboratory training. In this study, changes in cholesterol were more pronounced among females than males, suggesting that exercise using EVGs may have differential effects in different groups, although additional work is needed to examine the effects of EVGs among diverse groups of people.
CONCLUSIONS
The Wii Heart Fitness trial is the first study to examine the potential of EVGs for uptake and longer-term maintenance of PA. Results indicated significantly greater participation in MVPA among those in the EVG group compared with standard exercise and controls. EVG participants also showed greater improvements in some cardiovascular risk compared with controls. Physical inactivity is a significant public health issue that requires multifaceted approaches including innovative strategies to incorporate PA in daily routines. This study is an important and timely evaluation of EVG for PA adoption and cardiovascular outcomes among adults. To date, this is a first large-scale rigorous RCT using objective measures and a long-term follow-up to establish the benefits of a technology that is rapidly growing. EVGs were found to be effective, providing critical support in the fight against obesity and cardiovascular diseases.
ACKNOWLEDGMENTS
This trial is funded through a grant from NIH, National Heart, Lung, and Blood Institute (# ROI HL109116) to Dr. Bock.
All authors contributed substantially to the writing of this manuscript. In addition, Dr. Dunsiger was primarily responsible for the statistical analyses, Drs. Tilkemeier and Wu provided medical supervision, and Drs. Bock, Ciccolo, Serber, and Marcus were responsible for the trial design.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Bauer UE, Briss PA, Goodman RA, Bowman BA, Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384 (9937):45–52. 10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- 2.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8): 1423–1434. 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 3.HHS. 2008 Physical Activity Guidelines for Americans. Hyattsville, MD: HHS; 2008. https://health.gov/paguidelines/pdf/paguide.pdf. Accessed March 1, 2018. [Google Scholar]
- 4.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7): 1334–1359. 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 5.Samitz G, Egger M, Zwahlen M. Domains of physical activity and all-cause mortality: systematic review and dose-response meta-analysis of cohort studies. Int J Epidemiol 2011;40(5): 1382–1400. 10.1093/ije/dyr112. [DOI] [PubMed] [Google Scholar]
- 6.Nocon M, Hiemann T, Muller-Riemenschneider F, et al. Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabii. 2008;15(3):239–246. 10.1097/HJR.0b013e3282f55e09. [DOI] [PubMed] [Google Scholar]
- 7.Satt elm air J, Pertman J, Ding EL, et al. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011;124(7):789–795. 10.161/CIRCULATIONAHA.110.010710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore SC, Lee IM, Weiderpass E, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med. 2016; 176(6):816–825. 10.1001/jamainternmed.2016.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jakicic JM. The effect of physical activity on body weight. Obesity (Silver Spring). 2009;17(suppl 3):S34–S38. 10.1038/oby.2009.386. [DOI] [PubMed] [Google Scholar]
- 10.Woodcock J, Franco OH, Orsini N, Roberts I. Non-vigorous physical activity and all-cause mortality: systematic review and meta-analysis of cohort studies. Int J Epidemiol. 2011;40(1):121–138. 10.1093/ije/dyq104. [DOI] [PubMed] [Google Scholar]
- 11.Jefferis BJ, Whincup PH, Lennon L, Wannamethee SG. Longitudinal associations between changes in physical activity and onset of type 2 diabetes in older British men: the influence of adiposity. Diabetes Care. 2012;35(9): 1876–1883. 10.2337/dcl1-2280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eliassen AH, Hankinson SE, Rosner B, Holmes MD, Willett WC. Physical activity and risk of breast cancer among postmenopausal women. Arch Intern Med. 2010;170(19): 1758–1764. 10.1001/archinternmed.2010.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-term Trends in Health. Hyattsville, MD: National Center for Health Statistics; 2017. www.cdc.gov/nchs/data/hus/hus16.pdf. Accessed March 1, 2018. [PubMed] [Google Scholar]
- 14.Katzmarzyk PT, Lee IM, Martin CK, Blair SN. Epidemiology of physical activity and exercise training in the United States. Prog Cardiovasc Dis. 2017;60(1):3–10. 10.1016/j.pcad.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 15.Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S. adults: compliance with the Physical Activity Guidelines for Americans. Am J Prev Med 2011;40(4):454–461. 10.1016/j.amepre.2010.12.0l6. [DOI] [PubMed] [Google Scholar]
- 16.Williams NH, Hendry M, France B, Lewis R, Wilkinson C. Effectiveness of exercise-referral schemes to promote physical activity in adults: systematic review. Br J Gen Pract. 2007;57(545):979–986. 10.3399/096016407782604866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morgan O Approaches to increase physical activity: reviewing the evidence for exercise-referral schemes. Public Health. 2005;119(5):361–370. 10.1016/j.puhe.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 18.Fjeldsoe B, Neuhaus M, Winkler E, Eakin E. Systematic review of maintenance of behavior change following physical activity and dietary interventions. Health Psychol 2011;30(1):99–109. 10.1037/a0021974. [DOI] [PubMed] [Google Scholar]
- 19.Spark LC, Reeves MM, Fjeldsoe BS, Eakin EG. Physical activity and/or dietary interventions in breast cancer survivors: a systematic review of the maintenance of outcomes. J Cancer Surviv. 2013;7(1):74–82. 10.1007/s11764-012-0246-6. [DOI] [PubMed] [Google Scholar]
- 20.Dishman RK, Ickes W, Morgan WP. Self-motivation and adherence to habitual physical activity. J Appi Soc Psychol. 1980; 10 (2): 115–132. 10.1111/j.1559-1816.1980.tb00697.x. [DOI] [Google Scholar]
- 21.Fitzgerald SG, Cooper RA, Thorman T, et al. The GAMECycle exercise system: comparison with standard ergometry. J Spinal Cord Med. 2004;27(5):453–459. 10.1080/10790268.2004.11752237. [DOI] [PubMed] [Google Scholar]
- 22.Graves LE, Ridgers ND, Williams K, et al. The physiological cost and enjoyment of Wii Fit in adolescents, young adults, and older adults. J Phys Act Health. 2010;7(3):393–401. 10.1123/jpah.7.3.393. [DOI] [PubMed] [Google Scholar]
- 23.Lanningham-Foster L, Foster RC, McCrady SK, et al. Activity-promoting video games and increased energy expenditure. J Pediatr. 2009; 154 (6):819–823. 10.1016/j.jpeds.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Howe CA, Barr MW, Winner BC, Kimble JR, White JB. The physical activity energy cost of the latest active video games in young adults. J Phys Act Health. 2015; 12(2): 171–177. 10.1123/jpah.2013-0023. [DOI] [PubMed] [Google Scholar]
- 25.Miyachi M, Yamamoto K, Ohkawara K, Tanaka S. METs in adults while playing active video games: a metabolic chamber study. Med Set Sports Exerc. 2010;42(6):1149–1153. https://doi.oig/10.1249/MSS.0b013e3181c51c78. [DOI] [PubMed] [Google Scholar]
- 26.Bosch PR, Poloni J, Thornton A, Lynskey JV. The heart rate response to Nintendo Wii boxing in young adults. Cardiopulm Phys Ther J. 2012;23(2): 13–29. 10.1097/01823246-201223020-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sween J, Wallington SF, Sheppard V, et al. The role of exergaming in improving physical activity: a review. J Phys Act Health. 2014; 11 (4):864–870. 10.1123/jpah.2011-0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moholdt T, Weie S, Chorianopoulos K, Wang AI, Hagen K. Exergaming can be an innovative way of enjoyable high-intensity interval training. BMJ Open Sport Exerc Med. 2017;3(1):e000258 10.1136/bmjsem-2017-000258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barry G, van Schaik P, MacSween A, Dixon J, Martin D. Exergaming (XBOX Kinect) versus traditional gym-based exercise for postural control, flow and technology acceptance in healthy adults: a randomised controlled trial. BMC Sports Sci Med Rehabii 2016;8(1):25 10.1186/s13102-016-0050-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glen K, Eston R, Loetscher T, Parfitt G. Exergaming: feels good despite working harder. PloS One. 2017;12(10):e0186526 10.1371/journal.pone.0186526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.DuttaN Pereira MA. Effects of active video games on energy expenditure in adults: a systematic literature review. J Phys Act Health. 2015; 12 (6):890–899. 10.1123/jpah.2013-0168. [DOI] [PubMed] [Google Scholar]
- 32.Street TD, Lacey SJ, Langdon RR. Gaming your way to health: a systematic review of exergaming programs to increase health and exercise behaviors in adults. Games Health J. 2017;6(3):136–146. 10.1089/g4h.2016.0102. [DOI] [PubMed] [Google Scholar]
- 33.Leatherdale ST, Woodruff SJ, Manske SR. Energy expenditure while playing active and inactive video games. Am J Health Behav. 2010;34 (1):31–35. 10.5993/AJHB.34.L4. [DOI] [PubMed] [Google Scholar]
- 34.Garn AC, Baker BL, Beasley EK, Solmon MA. What are the benefits of a commercial exergaming platform for college students? Examining physical activity, enjoyment, and future intentions, J Phys Act Health. 2012;9(2):311–318. https://doi.org/10,1123/jpah.9.2.311. [DOI] [PubMed] [Google Scholar]
- 35.O’Donovan C, Hussey J. Active video games as a form of exercise and the effect of gaming experience: a preliminary study in healthy young adults. Physiotherapy. 2012;98(3):205–210. 10.1016/j.physio.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 36.Guzman JF, Lopez-Garcia J. Acute effects of exercise and active video games on adults’ reaction time and perceived exertion. Eur J Sport Sci. 2016; 16(8): 1197–1203. 10.1080/17461391.2016.1186744. [DOI] [PubMed] [Google Scholar]
- 37.Sanders GJ, Peacock CA, Barkley JE, et al. Heart rate and liking during “Kinect Boxing” versus “Wii Boxing”: the potential for enjoyable vigorous physical activity videogames. Games Health J. 2015;4(4):265–270. 10.1089/g4h.2014.0068. [DOI] [PubMed] [Google Scholar]
- 38.Choi SD, Guo L, Kang D, Xiong S. Exergame technology and interactive interventions for elderly fall prevention: a systematic literature review. Appi Ergon. 2017;65:570–581. 10.1016/j.apergo.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 39.Chao YY, Scherer YK, Wu YW, Lucke KT, Montgomery CA. The feasibility of an intervention combining self-efficacy theory and Wii Fit exergames in assisted living residents: a pilot study. Geriatr Nurs. 2013;34(5):377–382. 10.1016/j.gerinurse.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 40.Agmon M, Perry CK, Phelan E, Demiris G, Nguyen HQ. A pilot study of Wii Fit exergames to improve balance in older adults. J Geriatr Phys Ther. 2011;34(4):161–167. 10.1519/JPT.0b013e3182191d98. [DOI] [PubMed] [Google Scholar]
- 41.Studenski S, Perera S, Hile E, et al. Interactive video dance games for healthy older adults. J Nutr Health Aging. 2010;14(10):850–852. 10.1007/s12603-010-0119-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nagano Y, Ishida K, Tani T, Kawasaki M, Ikeuchi M. Short and long-term effects of exergaming for the elderly. Springerplus. 2016;5(1):793 10.1186/s40064-016-2379-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anderson-Hanley C, Arciera PJ, Brickman AM, et al. Exergaming and older adult cognition: a cluster randomized clinical trial. Am J Prev Med. 2012;42(2): 109–119. 10.1016/j.amepre.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 44.Rosenberg D, Depp CA, Vahia IV, et al. Exergames for subsyndromal depression in older adults: a pilot study of a novel intervention. Am J Geriatr Psychiatry. 2010;18(3):221–226. 10.1097/JGP.0b013e3181c534b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bock BC, Thind H, Dunsiger SI, et al. Exercise videogames for physical activity and fitness: design and rationale of the Wii Heart Fitness trial. Contemp Clin Trials. 2015;42:204–212. 10.1016/j.cct.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Karvonen MJ, Kentala E, Mustala O. The effects of training on heart rate; a longitudinal study. Ann Med Exp Biol Fenn. 1957;35(3):307–315. [PubMed] [Google Scholar]
- 47.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. 10.1249/00005768-198205000-00012. [DOI] [PubMed] [Google Scholar]
- 48.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985; 121(1):91–106. 10.1093/oxfordjournals.aje.al13987. [DOI] [PubMed] [Google Scholar]
- 49.Blair SN, Haskell WL, Ho P, et al. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985;122(5):794–804. 10.1093/oxfordjournals.aje.al14163. [DOI] [PubMed] [Google Scholar]
- 50.Conway JM, Seale JL, Jacobs DR Jr., Irwin ML, Ainsworth BE. Comparison of energy expenditure estimates from doubly labeled water, a physical activity questionnaire, and physical activity records. Am J Clin Nutr. 2002;75(3):519–525. 10.1093/ajcn/75.3.519. [DOI] [PubMed] [Google Scholar]
- 51.Dubbert PM, Vander Weg MW, Kirchner KA, Shaw B. Evaluation of the 7-day physical activity recall in urban and rural men. Med Sci Sports Exerc. 2004;36(9): 1646–1654. 10.1249/01.MSS.0000139893.65189.F2. [DOI] [PubMed] [Google Scholar]
- 52.Hayden-Wade HA, Coleman KJ, Sallis JF, Armstrong C. Validation of the telephone and in-person interview versions of the 7-day PAR. Med Sci Sports Exerc. 2003;35(5):801–809. 10.1249/01.MSS.0000064941.43869.4E. [DOI] [PubMed] [Google Scholar]
- 53.Washburn RA, Jacobsen DJ, Sonko BJ, Hill JO, Donnelly JE. The validity of the Stanford Seven-Day Physical Activity Recall in young adults. Med Sci Sports Exerc. 2003;35(8): 1374–1380. 10.1249/01.MSS.0000079081.08476.EA. [DOI] [PubMed] [Google Scholar]
- 54.Andreoli A, Scalzo G, Masala S, Tarantino U, Guglielmi G. Body composition assessment by dual-energy X-ray absorptiometry (DXA). Radiol Med. 2009; 114(2):286–300. 10.1007/s11547-009-0369-7. [DOI] [PubMed] [Google Scholar]
- 55.American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2013. [DOI] [PubMed] [Google Scholar]
- 56.Gans KM, Hixson ML, Eaton CB, Lasater TM. Rate Your Plate: a dietary assessment and educational tool for blood cholesterol control. Nutr Clin Care. 2000;3(3): 163–169. 10.1046/j-1523-5408.2000.00045.x. [DOI] [Google Scholar]
- 57.Serber ER, Ciccolo J, Palmer K, Cobb V, Tilkemeier PL, Bock BC. The feasibility of exercise videogames for cardiovascular risk reduction among adults: a pilot for “Wii heart fitness”. J Sports Med Phys Fitness. 2016;56(3):319–327. [PubMed] [Google Scholar]
- 58.Marcus BH, Lewis BA, Hogan J, et al. The efficacy of moderate-intensity exercise as an aid for smoking cessation in women: a randomized controlled trial. Nicotine Tob Res. 2005;7(6):871–880. 10.1080/14622200500266056. [DOI] [PubMed] [Google Scholar]
- 59.Marcus BH, Lewis BA, King TK, et al. Rationale, design, and baseline data for Commit to Quit II: an evaluation of the efficacy of moderate-intensity physical activity as an aid to smoking cessation in women. Prev Med. 2003;36(4):479–492. 10.1016/S0091-7435(02)00051-8. [DOI] [PubMed] [Google Scholar]
- 60.Marcus BH, Albrecht AE, King TK, et al. The efficacy of exercise as an aid for smoking cessation in women: a randomized controlled trial. Arch Intern Med. 1999; 159(11): 1229–1234. 10.1001/archinte.159.11.1229. [DOI] [PubMed] [Google Scholar]
- 61.Marcus BH, King TK, Albrecht AE, Parisi AF, Abrams DB. Rationale, design, and baseline data for Commit to Quit: an exercise efficacy trial for smoking cessation among women. Prev Med. 1997;26(4):586–597. 10.1006/pmed.1997.0180. [DOI] [PubMed] [Google Scholar]
- 62.Huotari K, Hamari J. Defining gamification: a service marketing perspective. Proceeding of the 16th International Academic MindTrek Conference; 2012. 10.1145/2393132.2393137. [DOI] [Google Scholar]
- 63.Patel MS, Benjamin EJ, Volpp KG, et al. Effect of a game-based intervention designed to enhance social incentives to increase physical activity among families: the BE FIT randomized clinical trial. JAMA Intern Med. 2017; 177(11):1586–1593. 10.1001/jamainternmed.2017.3458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hamari J, Koivisto J, Sarsa H. Does gamification work? A literature review of empirical studies on gamification. 47th Hawaii International Conference on System Sciences (HICSS); 2014. 10.1109/HICSS.2014.377. [DOI] [Google Scholar]
- 65.Lister C, West JH, Cannon B, Sax T, Brodegard D. Just a fad? Gamification in health and fitness apps. JMIR Serious Games. 2014;2(2):e9 10.2196/games.3413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Edwards EA, Lumsden J, Rivas C, et al. Gamification for health promotion: systematic review of behaviour change techniques in smartphone apps. BMJ Open. 2016;6(10):e012447 10.1136/bmjopen-2016-012447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Weiler R, Stamatakis E, Blair SN. Physical inactivity is associated with earlier mortality–the evidence is incontrovertible. Br J Gen Pract. 2011;61(593):719–720. 10.3399/bjgp11X613061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Carlson SA, Fulton JE, Schoenbom CA, Loustalot F. Trend and prevalence estimates based on the 2008 Physical Activity Guidelines for Americans. Am J Prev Med. 2010;39(4):305–313. 10.1016/j.amepre.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 69.CDC. Prevalence of self-reported physically active adults–United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57(48):1297–1300. [PubMed] [Google Scholar]
- 70.Kwasnicka D, Dombrowski SU, White M, Sniehotta F. Theoretical explanations for maintenance of behaviour change: a systematic review of behaviour theories. Health Psychol Rev. 2016;10(3):277–296. 10.1080/17437199.2016,1151372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Khaw KT, Wareham N, Luben R, et al. Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of European prospective investigation of cancer and nutrition (EPIC-Norfolk). BMJ 2001;322 (7277): 15–18. 10.1136/bmj.322.7277.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Matsushita K, Blecker S, Pazin-Fillio A, et al. The association of hemoglobin Ale with incident heart failure among people without diabetes: the Atherosclerosis Risk in Communities Study. Diabetes. 2010;59(8):2020–2026. 10.2337/db10-0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. New Engl J Med. 2010;362(9):800–811. 10.1056/NEJMoa0908359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J.. 2017;38(32):2459–2472. 10.1093/eurheartj/ehxl44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Amorim MGS, de Oliveira MD, Soares DS, et al. Effects of exergaming on cardiovascular risk factors and adipokine levels in women. J Physiol Sci. 2018;68(5):671–678. 10.1007/s12576-017-0581-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Höchsmann C, Schiipbaeh M, Schmidt-Trucksäss A. Effects of exergaming on physical activity in overweight individuals. Sports Med. 2016;46(6):845–860. 10.1007/s40279-015-0455-z. [DOI] [PubMed] [Google Scholar]


