Abstract
Objectives
The aim was to identify and describe outcomes from original published studies that present the number, nature, mechanism and severity of medically treated injuries sustained in community-level cricket.
Design
Systematic review.
Methods
Nine databases were systematically searched to December 2019 using terms “cricket*” and “injur*”. Original, peer-reviewed studies reporting injury for at least one injury descriptor (body region, nature of injury and/or mechanism of injury) in community-level cricketers of all ages were included. Qualitative synthesis, critical appraisal and descriptive summary results are reported within the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.
Results
Six studies were included: five reported hospital-treated data and one reported insurance claims data. Two had a low risk of bias. In hospital-based studies, fractures were the most frequent injury type. Upper and lower limb injuries (age ≥15 years) and injuries to the head (age <15 years) were the most common body region injured. Being struck by the ball was the most common mechanism for injury presenting to hospitals. Children were also commonly struck by equipment. One study using insurance claims data reported soft tissue injuries as the main of injury type.
Conclusion
Hospital treatment data were most prominent, which emphasised injuries of a more serious nature or requiring acute care. These injuries were primarily fractures, dislocation/sprain and strains, bruising and open wounds with the majority resulting from players being struck by the ball. Research into whether properly fitted protective equipment, at an approved standard, is worn and is effective, is recommended.
Keywords: injuries, cricket, sports
What is already known?
Compared to elite levels of the game, injury in community-level cricket is much less reported.
Medically treated injuries may be a cause of lost time from sport and work for community-level players and a negative influence on future health and well-being.
What are the new findings?
Studies reporting medically treated cricket injuries are limited and biased toward hospital data sources (five studies) compared to insurance claims data (one study). The information is dated with only two study being published in the last 5 years. More effective injury reporting is required at community levels.
Fractures, bruising and open wounds/lacerations were the most common injury types, with the majority caused by players being struck by the ball. These findings suggest that future research should consider whether properly fitted and maintained protective equipment, designed to an approved standard, is worn by players and is effective.
For children under 15 years, the head was the most commonly injured body part. Children also had many injuries from being struck by equipment (other than the ball). This finding suggests a need for close supervision of junior cricketers to ensure a safe environment together with education of these players on safe behaviour, appropriate playing techniques and need for protective equipment.
Introduction
Cricket is a non-contact, bat and ball sport played mostly in Commonwealth countries. Injuries can occur in all activities of the game, for example when bowling, batting or fielding, and from a range of causes such as being hit by the cricket ball, falling when attempting to catch or overuse/repetitive strain, particularly in bowlers.1 Protective equipment is only worn by players in high-risk activities (batting, specialist fielding positions), including leg pads, gloves and helmets. Nevertheless, participation still carries a risk of injury and monitoring of injury occurrence remains an important element of promoting safety in the game.
During the 2017/2018 season, approximately 704 000 people,2 or around 3% of the Australia population, were engaged in competitions or club-based cricket across junior or senior levels, most of whom are considered to be community level players. Since 2002, the national body for cricket in Australia, Cricket Australia (CA), and affiliated State bodies have routinely monitored injuries in their elite players.3 Although the cohort of participants at community level is substantially greater, and therefore the total public health burden from injury potentially larger, there is no routine injury surveillance system available to monitor injuries in this player group. As shown in other sports, the injury profile in elite athletes is often very different to that seen in community participants.4
Hospitals, emergency departments (EDs), general practitioners (ie, family doctor), insurers and sports or allied health clinics are all possible sources of injury data for community sports injury.5 In Australia, hospital and ED datasets offer the most readily available data on sports injury because it is coded using the 10th edition of the Australian Modification to the International Classification of Diseases (ICD-10-AM). This classification includes specification of an activity code for external causes of injury, including specific activity (eg, cricket) for sports and leisure.
It is important to identify and understand the profile of community cricket injuries because it is through this process that we can begin to assess any discernible problem. Just as important is the fact that many injuries may be acute and interruptive of sport and/or work life. At the community level, participation is more likely to be driven by enjoyment, personal fitness and social factors.6 Injury may be a barrier to current and future participation, which may have flow on health effects.7 Return to physical activity postinjury has been shown to be influenced by the degree to which the injury may affect the participant’s work–life, and hence ability to derive income.8 An examination of medically treated injuries can be used to confirmwhat current information exists around injuries in community cricketers and who is seeking treatment, which may enable better targeted prevention strategies.9
The aim of this systematic review was to identify and describe outcomes from studies that present the number, nature, mechanism and severity of medically treated injuries sustained in community level cricket. The profile of these injuries is presented together with the quality of the data reporting.
Methods
Protocol and registration
This systematic review was registered online through the International prospective register of systematic reviews (PROSPERO)10 record CRD42017079047 and is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.11
Search strategy
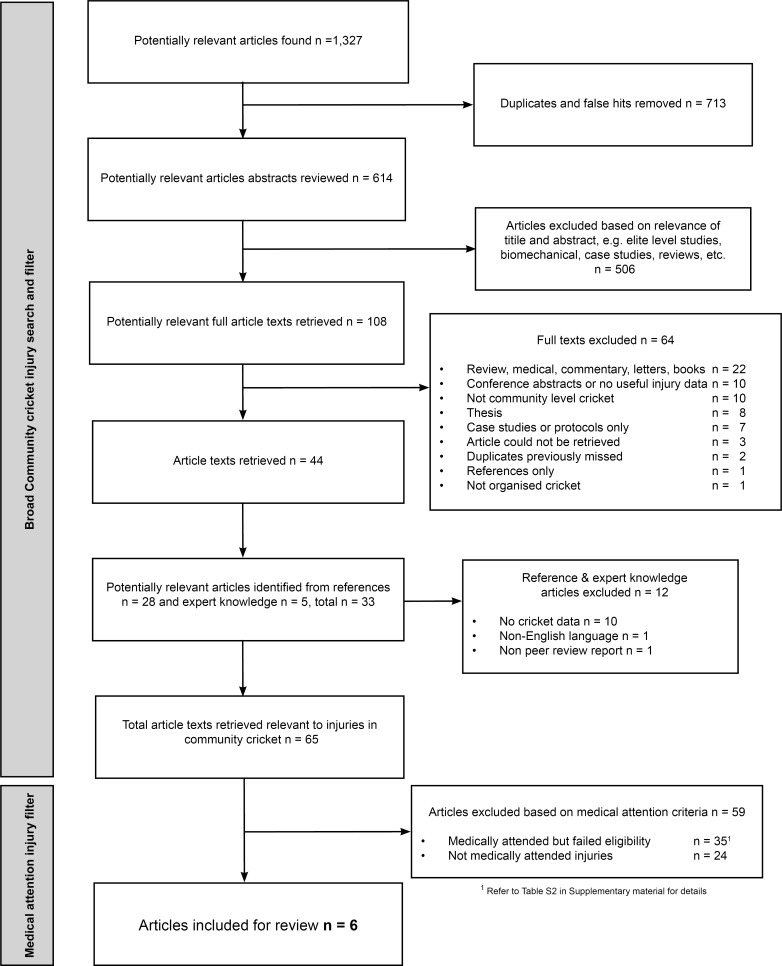
Nine databases were searched: CINAHL, MEDLINE and SPORTDiscuss (all through EBSCOHost), ScienceDirect, SCOPUS, Web of Science, PubMed, Informit and Google Scholar. Reference lists of included articles were checked for additional studies of relevance and experts (CFF and AK) were consulted for knowledge of any additional studies not already captured. The search terms were “cricket*” AND “injur*” (and synonyms/derivatives) being present in the title, abstract or keywords of a paper. Variations to the search strings were used depending on the database. An example of a search description is shown in online supplementary table S1. The initial search was conducted by GM and included all community cricket injury papers published before the 30 September 2017. Updated searches were performed by GM in April 2018, November 2018 and December 2019 with additional relevant papers included (figure 1).
Figure 1.
Search and study selection flow chart.
bmjsem-2019-000670supp001.pdf (140.6KB, pdf)
Eligibility criteria
Review of the full text identified studies that reported medical-attention data from community cricket over the past 30 years (1988–2018). The term of 30 years was considered appropriate to reflect the game and injuries that may exist in its present forms. Community cricket was defined as encompassing all organised cricket (indoor and outdoor), from junior development and club cricket up to and including premier level cricket in Australia (or its equivalent, ie, one level below state, provincial or county cricket), school cricket, including state and national representative school championships not managed by national or state cricketing bodies. Community cricket excluded high performance centres, or equivalents, where community level players may be training or playing temporarily under the auspices of higher cricketing bodies. Where the population/level of play was not presented or was unclear in the original studies, we contacted the corresponding author for clarification.
All included studies were required to report data on the number of injuries and at least one of the following variables representing core items in sports injury surveillance12:
Body region injured (eg, head, wrist)
Nature of the injury (eg, fracture, sprain, strain)
Mechanism of injury (eg, fall, hit by ball).
To enable the identification of the most frequently occurring injuries, and therein derive injury prevention priorities, studies which reported only on a specific type of injury (eg, stress fracture) or body part (eg, head) were excluded. Medical-attention studies that were excluded based on the above criteria are listed in online supplementary table S2. Case studies, editorials, reports, letters, books, reviews and conference proceedings were also excluded.
Study selection
After the initial search was completed, duplicates and false hits were removed, and two authors (GM and SOC) independently screened the titles and abstracts for eligibility. Publications were excluded only when both reviewers agreed that the title/abstract clearly confirmed the study was not relevant to the review aims. Where it was unclear, the full article was assessed. The full text of the remaining articles was examined independently by the same two authors for eligibility. Any disagreements regarding inclusion were resolved through discussion with a third author (LVF).
Critical appraisal/risk of bias
A self-developed, nine-item critical appraisal tool (table 1) was designed using elements of the Downs and Black tool13 and Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.14 A specific item regarding injury definition and injury severity (item 5; table 1) was included as being pertinent to aims of this review in line with reporting under the current and previous cricket consensus statements. Although not formally validated, two authors (GM and SOC) tested the tool with a selection of similar (but not included) papers to ensure its relevance and applicability to the types of study designs included. Modifications and explanations to the tool were agreed on prior to its evaluation of articles for this review.
Table 1.
Critical appraisal of studies
| Item | Study (first author and year) | |||||||
| Perera, 201922 |
Finch, 199820 |
Walker, 201019 |
King, 201817 |
Upadhyay, 200018 |
Forward, 198821 |
Overall % of yes | ||
| Likelihood of bias* | Low | Low | Low | Unclear | Unclear | High | ||
| 1 | Were the study aims and design described adequately and are they compatible? | Yes | Yes | Yes | Yes | Yes | Partial | 83 |
| 2 | Was the study setting, subjects, source, target population and size described adequately? | Yes | Yes | Yes | Yes | Partial | Partial | 67 |
| 3 | Was the method of data collection described adequately and did it seek to minimise information bias? | Yes | Yes | Yes | Partial | Yes | Partial | 67 |
| 4 | Has there been appropriate reporting of attrition of subjects or missing data? | Yes | Partial | Partial | Partial | Partial | Partial | 17 |
| 5 | Was there an injury definition and/or injury severity measure/definition provided and were they suitable for the study design? | Yes | Partial | Yes | Yes | Yes | Partial | 67 |
| 6 | Were the injury outcomes and exposure measures reported in a standardised, justified and reasonable manner? | Partial | Yes | Yes | Yes | Yes | Yes | 83 |
| 7 | Were limitations to the study discussed adequately? | Yes | Yes | Yes | Yes | No | No | 67 |
| 8 | Is there a summary of key results, their potential generalisability and whether they and any conclusions match the aims and/or reflect the limitations of the study? | Yes | Yes | Yes | Yes | Yes | Partial | 83 |
| 9 | Does the study explain any ethics requirements, author conflicts of interest and/or funding arrangements? | Yes | Partial | Yes | Yes | No | No | 50 |
*Items 2, 3 and 4 (shaded) used to assess the likelihood of bias.
Risk of bias assessment was based on three of the items (2, 3 and 4) relating to selection, information and attrition biases.15 16 If each of these items was answered ‘yes’, then the study was considered to have a low likelihood of bias. If one of these items was considered to have only been partially satisfied, the study was considered to have an unclear likelihood of bias. Any ‘no’ response to these items resulted in the study being considered to have a high likelihood of bias. Studies were assessed independently by two authors (GM and SOC) and where agreement could not be reached then a third author (LVF) was consulted.
Data collection and data items
Two authors (GM and SOC) independently extracted data from the eligible articles on a custom data extraction form, which included study design, country, setting and context, aims, year and timeframe, ethics, overall participant numbers, age range, gender, levels of play, facets of play (eg, batting, bowling and/or fielding), participant recruitment, data collection methods, injury definition, injury severity measure/definition, number of injuries, exposure measures, incidence, prevalence, nature (type), locations (body parts), mechanisms, severity, losses/dropouts, and number of injuries not defined. Any disagreement regarding study type, participant characteristics, measurement methods or main results was clarified by discussion with a third author (LVF).
Data synthesis/summary measures
To address the primary aim of this review and identify the number, nature, mechanism and severity of injuries in community cricket, a qualitative synthesis is presented, with tabular summaries. Further details are presented in combination, where appropriate, for the relevant summary outcomes: injury rates, prevalence/proportions, nature, body location, mechanism/setting and severity. To address the secondary aim of reporting quality, we summarised the completeness of reporting (n and %) for individual items of the critical appraisal tool to identify which areas are well addressed and which need improvement.
Results
Over 1300 articles were identified from which 65 were relevant to community cricket injury (refer to figure 1). Six articles met all inclusion criteria and were retained for analysis.
Study characteristics
Table 2 summarises the characteristics and outcomes of included studies. Three studies were specific to cricket and two studies included cricket among other sports or injury reporting. Three of the studies were based in New Zealand (NZ)17–19 and two in Australia.20 21 Three studies used ED presentation data only,18 20 21 one used hospital admission data only,19 one used both ED presentation and admission data22 and one used insurance claims data.17 One study was specific to indoor cricket,21 while the remainder of the studies did not specify so outdoor and indoor are assumed combined.
Table 2.
Study characteristics and injury outcomes from five original studies of medical-attention injuries in community cricket (n=6)
| First author, year (reference) | Setting/context and aims | Overall participants (n), age, sex | Injury data collection methods | Injury definition, SM |
No of injured (np) and injuries (ni) | EM, incidence/prevalence | Nature of injuries | Body region/part injured | Mechanism of injuries | Severity of injuries | Other information |
| Perera, 201922 | A comprehensive profile of hospital-treated cricket injuries sustained by female cricketers in Victoria, Australia, from 2002/2003 to 2013/2014. | n=668 cases overall with 547 ED presentations and 121 HA All females aged 5 years or more Top three age groups for HA: 20–24: 19.0% 10–14: 16.5% 30–34: 10.7% Top three age groups for ED: 10–14: 19.9% 15–19: 15.7% 20–25: 13.3% |
Data sourced from Victorian Injury Surveillance Unit which collects ED data under the Victorian Emergency Minimum Dataset and HA data under the Victorian Admitted Episode Dataset | ED presentation or HA. For HA, SM: <2 days bed stay or ≥2 days bed stay. |
ED np=547 HA np=121 |
Per 1000 participants Overall=1.9 (95% CI 0.8 to 4.5) |
HA: Fractures=57 (47.1%) Dislocation, sprain and strain=22 (18.2%) Injury to muscle and tendon=8 (6.6%) Superficial injury=6 (5.0%) Other unspecified=28 (23.1%) ED: Dislocation sprain and strains=199 (36.4%), fractures=92 (17.2%) Superficial injury=80 (14.6%) Open wound=46 (8.4%) Injury to muscle and tendon=38 (6.9%) Eye injury—excluding foreign body=16 (2.9%) Intracranial injury=9 (1.6%) Other unspecified=67 (11.9%) |
HA: Head=34 (28.1%) Shoulder=6 (5%) Elbow=14 (12%) Wrist/hand=21 (17.4%) Abdominal/lower back/spine/pelvis=0 Knee/lower leg=27 (22%) Ankle/foot=7 (5%) Unspecified=12 (10%) ED: Head=152 (27.8%) Shoulder=22 (4%) Elbow=33 (6%) Wrist/hand=158 (29%) Abdominal/lower back/spine/pelvis=6 (1%) Knee/lower leg=66 (12%) Ankle/foot=77 (14%) Unspecified=6 (1%) Suppressed=27 (5%) |
HA: Hit/struck/crushed by ball or bat=54 (44.6%) Fall=33 (27.3%) Overexertion and/or strenuous movements=15 (12.4%) Other unspecified=15 (12.4%) Not reported=4 (3.3%) ED: Hit/struck/crushed by ball or bat=349 (63.8%) Fall=104, (19.0%) Other unspecified=94 (17.1%) |
HA: Bed stay <2 days=95 (78.5%) Bed stay ≥2 days= 26 (21.5%) |
|
| King, 201817 | Provide retrospective analysis of moderate to serious injury and serious injury claims and related costs for five sporting codes using national insurance claims (ACC) in New Zealand from 2012 to 2016. | n=853 to 324 claims from which 60 803 moderate to serious claims (3072 cricket related), 597 serious claims (15* cricket related) Age 0–85+ years Sex: M=2864, F=208 for moderate to serious claims M=12, F=3 for serious claims* |
Retrospective analysis of data from ACC for 5 years from 2012 to 2016 | Any injury which qualified for a moderate to serious injury or serious injury claim. SM=Any injury which qualified as either a ‘moderate to serious’ or ‘serious’ injury defined by the ACC based on level of benefits and care provided. |
np cricket related: moderate to serious injury claims=3072, serious injury claims=15 | EM=NR 0.4% of all claims cricket related |
Moderate to serious claims: Soft tissue=1980 (64.4%) Fracture/dislocation=948 (30.9%) Laceration/wound=59 (1.9%) Concussion/brain injury=44 (1.4%) Deafness=15 (0.49%) Gradual onset=14 (0.46%) Dental injuries=6 (0.20%) Hernia=6 (0.20%) Serious claims: Concussion/brain injury=9 (60%) Fracture/dislocation=6 (40%) |
Moderate to serious claims: Head/neck=212 (6.9%) Upper limb=1086 (35.4%) Lower limb=1394 (45.4%) Chest/back/shoulder=72 (2.3%) Serious claims*: Head/neck=15 (56%) Lower limb=12 (44%) |
NR | 3072 moderate to serious claims. 15 serious claims |
Cricket ranked fifth for total moderate to serious injury claims but third for mean cost per claim. Cricket ranked equal third for serious injury claims but fifth for mean costs per claim. Moderate to serious claims for fracture/dislocations increased significantly over 2012–2016. |
| Walker, 201019 | Hospitalisation of cricket players in NZ from 2000 to 2005 inclusive. Identify the epidemiology of injury resulting in hospitalisation, agents and mechanisms (products and activities) associated with injury and evidence of assistance to those developing activity-specific PPE. |
n=498 cases Age range=2–80 years 0–9: 8% 10–19: 28% 20–29: 23% 30–39: 21% 40–49: 12% 50–59: 4% 60+: 3% Sex: M>F but no numbers |
Retrospective analysis of NZ’s National Minimum Dataset of public and private hospitals | ICD-10-AM codes for case hospitalised for at least one night, including bystanders injured as a direct result of cricket activity. SM=Serious non-fatal cases based on ICISS score of ≤0.941. |
np=ni=498 | EM=1 00 000 people/year and 100 000 participants/year. Population IIR=2.3 Participant IIR=39 Almost 1% of all cases were cricket related |
Fracture: 218 (44%) Sprain/strain/soft tissue: 76 (15%) Dislocation: 31 (6%) Contusion: 27 (5%) Rupture/tear: 18 (4%) Concussion: 14 (3%) Open wound: 12 (2%) Seizure: 11 (2%) Other: 90 (18%) |
Head and neck: 114 (23%)—28 fractures, 11 open wounds, 10 concussions Upper limb: 178 (36%)—111 phalanges, 32 lower arm, upper arm and shoulder 33 Lower limb: 156 (31%)—Achilles 44, tibia/fibula 27, ankle 25, knee 21 Trunk and back: 14 (3%) Not specified: 36 (7%) |
Exposure to inanimate mechanical forces: 240 (48%) —of these 144 (60%) were hit by ball and 33 (14%) hit by bat. Falls: 108 (22%) Overexertion or repetitive movements: 102 (21%) Exposure to animate objects (eg, player collisions): 34 (7%) Unspecified: 3% |
20 (4%) cases were classified as serious non-fatal, 11 due to being struck by bat or ball, 6 due to collisions with other players, 2 from falls and 1 from overexertion. | For children under 10 years who were injured under exposure to inanimate mechanical forces, 25 (72%) were struck by the bat. |
| Upadhyay, 200018 | Emergency presentations to Starship Children’s Hospital Auckland, NZ. Describe the nature of injuries sustained by children playing cricket from 1993 to April 1998. | n=60 cases Age range=9–13 years Sex NR |
Retrospective review of existing data | Injury secondary to playing cricket under ICD code E-8897 SM=NR. |
np=ni=60 | EM=NR | Fracture: 26 (43.3%) Closed head injury: 8 (13.3%) Blunt trauma: 8 (13.3%) Other: 18 (30%)—noted as soft tissue contusions, ligamentous injuries, minor lacerations and abrasions |
Head/face and neck: 16 (26.7%) Thorax/abdomen: 8 (13.3%) Upper limb: 18 (30%) Other unspecified: 18 (30%) |
Hit by ball: 31 (51.6%) Hit by bat: 12 (20%) Fall: 12 (20%) Collision with player: 3 (5%) Fall on bat handle: 1 (1.7%) Fall on stumps: 1 (1.7%) |
Two injuries were severe, both blunt abdominal trauma. 19 cases (31.6%) required operative procedures. Median range of days of stay in hospital: 1–2.5 days. 18 cases did not require admission to hospital (all other). |
Not applicable |
| Finch, 199820 | ED presentations of sports injuries in selected parts of Australia for the period 1989–1993. Describe sports injury cases presented to selected hospital EDs and redress the lack of community-based information on sports injury in Australia. | n=5 16 221 98 140 attendees to NISU EDs 51 203 <15 years old (children) 46 837 ≥15 years old (adults) not specific to cricket Gender NR |
Data collected from 74 public hospitals and medical centres on standardised collection forms throughout Australia | NR SM=NR |
np(children)=1945 ni(children)=2345 np(adults)=3408 ni(adults)=3846 |
EM=NR 3.7% of all children presenting with sports injury and 7.3% of all adults presenting with sports injury related to cricket |
Children/adult: Haematoma/bruising: 30.2 %/19.6% Fracture: 17.8 %/20.7% Laceration: 17.8%/11.8% Sprain/strain: 12.4%/26.0% Inflammation/swelling/pain: 7.5%/10.6% Superficial abrasion: 2.9%/1.2% Other: 11.4%/11.5% |
Children/adults: Head: 44.2%/16.6% Upper extremity: 33.9%/32.6% Lower extremity: 15.5%/22.8% Trunk: 3.2%/4.2% Other: 11.4 %/11.5% |
Head and facial injuries generally associated with hits with the ball or bat | 8.2% of ED presentations for children were admitted to hospital. 5.4% of ED presentations for adults were admitted to hospital. |
Not applicable |
| Forward, 198821 | Review indoor cricket injuries presenting to ED of Royal Perth Hospital, Australia, over a 6-month period. (Published in 1988—no reference to dates investigated.) | n=64 cases 19–34 years Sex: M=50, F=14 |
Recording of all indoor cricket injuries presenting in ED | NR (all indoor cricket-related injuries) SM=work time loss |
np=64 ni=65 |
EM=NR | Fractures: 19–22 (includes three bruised or fractured ribs) Grade I/II ligament strains: 10 Eye-specific damage: 6 Dislocations: 5 Bruising: 2–5 (includes three bruised or fractured ribs) Friction burns (infected): 4 Lacerations: 4 Avulsions: 2 Concussion: 1 Other: 7 |
Head and neck: 14—eye injuries 6 (43%), supraorbital ridge 4 (29%), nasal bone 3 (21%) Upper limb: 30—proximal phalanx 11 (37%) Lower limb: 18—ankle 5 (28%), knee 5 (28%) Thorax: 3—ribs 3 (100%) |
Batters most often struck on fingers by ball Wicket-keepers: 5 of 7 injuries due to being struck in eye by ball One player was struck by the bat in an argument |
No time off work: 19% <1 week off: 19% 1 week—1 month: 19% >1 month: 11% Not known: 32%. |
Activity at onset: Fielding: 72% Batting: 17% |
*There is some disparity in the reported figures of the number of serious for cricket-related injury (reported in different tables as n=15 and n=27).
ACC, Accident Compensation Corporation; ED, emergency department; EM, exposure measure; F, female; ICD-10-AM, 10th edition of the Australian Modification to the International Classification of Diseases; ICISS, International Classification Injury Severity Score; IIR, Injury Incidence Rate; M, male; NISU, National Injury Surveillance Unit; NR, not reported; NZ, New Zealand; PPE, personal protective equipment; SM, severity measure.
Critical appraisal
(table 1)summarises the critical appraisal of the studies: two recorded a low likelihood of bias,19 20 two were unclear17 18 and one recorded a high likelihood of bias.21 The overall percentage of items addressed adequately (ie, recorded yes responses) for all studies was 65%. (n=35 of 54). Item 4 (reporting of attrition and missing data) was the most incompletely answered with all studies recording partial responses. Item 9 (ethics, author conflicts and funding) recorded 50% of yes answers. All other items recorded 67% or greater proportions of yes answers.
Injury incidence rates and prevalence
The injury rate for cricket-related hospitalisation in NZ from 2000 to 2005 was 2.3 per 100 000 population per year, while for participation the injury rate for cricket-related hospitalisation was 39 per 100 000 participants per year.19 In the same NZ hospital study, almost 1% of all cases were related to cricket injury.19 An NZ study looking at insurance claims over the 2012 to 2016 period reported 0.4% of the total claims (of the five sports investigated) were due to cricket-related injury.17 A study looking at ED presentations across Australia from 1989 to 1993 reported 3.7% of children under 15 years of age and 7.3% of all adults (defined as 15 years or older) presenting with sports injuries were cricket related.20 A study looking at hospital-attended cricket injuries in females in Victoria, Australia, from 2002/2003 to 2013/2014, reported an overall injury rate of 1.9 per 1000 participants, with an overall downward trend over that time period.22
Nature of injury
Table 3 summarises the injury nature reported by the six studies. For ED presentations in NZ among children aged 9 to 13 years, fracture was the highest proportion of injuries recorded (43.3% of all cases) with both concussion/head injury and internal organ rupture as the equal second highest injury nature (13.3%).18 Of the Australian ED presentations from 1989 to 1993, for children under 15 years of age, bruising (30.2%) was the highest proportion of cricket-related injury type, with fractures (17.8%) and lacerations (17.8%) equal second.20 For adults (15 years or older), sprain and strain (combined) was the highest proportion of injury nature (26.0%), followed by fracture (20.7%) and bruising (19.6%).20 Fractures were also the most common injury nature for females in Victoria, Australia, for hospital admissions (47.1%), while dislocation, sprain, and strain were more common in ED presentations (36.4%).22 For indoor cricket injuries seen at ED, fracture was the highest proportion of injury nature (34.3%) followed by sprain (15.6%) and dislocation (10.9%).21 Fracture was the most common injury nature in hospital admissions in NZ (43.8%) with sprain (15.2%) and avulsion/dislocation (6.2%) as the next two highest injury nature proportions.19 For cricket injuries resulting in insurance claims in NZ, soft tissue injury was the highest reported injury nature (64.0%) followed by fractures (30.9%).17
Table 3.
Injury nature for studies reporting medical-attention injury in community cricket (ED presentations unless otherwise noted)
| First author, year (reference) | No of injuries | Age range | Concussion/closed head intracranial injury or seizure | Superficial injury | Eye injury | Fracture | Avulsion / dislocation |
Injury to muscle and tendon or rupture/tear | Internal organ injury | Open wound/laceration | Soft tissue | Sprain | Strain | Bruising | Overuse | Inflammation* | Abrasion/friction burn | Other/NR |
| Perera, 201922 | HA: 121 | 5–45+ years | – | 5.0% | – | 47.1% | † | 6.6% | – | – | – | 18.2%† | – | – | – | – | 23.1% | |
| ED: 547 | 5–45+ years | 1.6% | 14.6% | 2.9% | 17.2% | † | 6.9% | – | 8.4% | – | 36.4%† | – | – | – | – | 11.9% | ||
| King, 201817 | 3087** | 0–85+ years | 1.7% | – | – | 30.9% | – | – | – | 1.9% | 64.1% | – | - | – | 0.5% | – | – | 0.9% |
| Walker, 201019 | HA: 498 | 2–80 years | 5.0%‡ | – | – | 43.8% | 6.2% | 3.6% | – | 2.4% | – | – | 15.2% | 5.4% | – | – | – | 18.1% |
| Upadhyay, 200018 | 60 | 9–13 years | 13.3% | – | – | 43.3% | – | – | 13.3% | – | – | – | – | – | – | – | 30.1% | |
| Finch, 199820 | 2345 | <15 years | – | – | – | 17.8% | – | – | – | 17.8% | – | 12.4%§ | 30.2% | – | – | 2.9% | 11.4% | |
| 3846 | ≥15 years | – | – | – | 20.7% | – | – | – | 11.2% | – | 26.0%§ | 19.6% | – | – | 1.2% | 11.5% | ||
| Forward, 198821 | 65 | 19–34 years | 1.5% | – | 9.2% | 33.8%¶ | 10.8% | – | – | 6.2% | – | 15.4% | – | 6.2% | – | – | 6.2% | 10.7% |
*Includes pain and swelling.
†Dislocation, sprain and strain were combined.
‡Includes 2.2% seizures.
§Sprain and strain combined.
¶Includes bruised ribs as three cases were classifiedas bruised or fractured.
**Insurance claims.
ED, emergency department presentations; HA, hospital admission; NR, not reported.
Body regions injured
Table 4 summarises the body regions of injury in the six studies. With the exception of children aged under 15 years presenting to Australian EDs, the upper limb was the body region with to the highest proportion of injury, ranging from 33%20 to 47%.21 The lower limb injury proportion ranged from 16%20 to 35%.17 The proportion of head injury was highest in children under 15 years presenting to Australian EDs at 44%20 and 27% for ED presentations in NZ.18 For older age groups presenting to EDs or admitted to hospital, head injury ranged from 17%20 to 23%.19 Twenty-eight per cent of females of all ages required hospital treatment for head/face/neck injuries in Victoria, Australia.22 For injuries resulting in moderate to serious or serious insurance claims in NZ, head injuries represented 7% of the cases.17 Trunk and back injuries ranged from 2%17 to 13%18 across all studies.
Table 4.
Percentage of body regions for medical-attention injuries in community cricket
| First author, year (reference) | No of injuries | Head/face/neck | Upper limb | Trunk/back | Lower limb | Unspecified |
| Perera, 201922 | ||||||
| HA | 121 | 28.1 | 33.9 | – | 28.1 | 9.9 |
| ED | 547 | 27.8 | 38.9 | 1.1 | 26.1 | 6.1 |
| King, 201817 | 3087* | 7.4 | 35.2 | 2.3 | 45.5 | 9.6 |
| Walker, 201019 | 498 | 22.9 | 35.7 | 2.8 | 31.3 | 7.3 |
| Upadhyay, 200018 | 60 | 26.7 | 30.0 | 13.3 | NR | 30.0 |
| Finch, 199820 | ||||||
| Ages <15 years | 2345 | 44.2 | 33.9 | 3.2 | 15.5 | 11.4 |
| Ages ≥15 years | 3846 | 16.6 | 32.6 | 4.2 | 22.8 | 11.5 |
| Forward, 198821 | 65 | 21.5 | 46.2 | 4.6 | 27.7 | 0.0 |
*Number of claims (there were no ‘multiple locations’ injuries reported).
ED, emergency department presentations; HA, hospital admissions; NR, not reported.
Specific body parts injured were provided in three hospital-based studies.19 21 Of the upper limb injuries admitted to hospital in NZ, almost two-thirds (62%) were to the fingers. Thirty-two per cent of the lower limb injuries were to the Achilles tendon.19 Of the indoor cricket injuries presenting to EDs in Australia from 1989 to 1993, 50% of the head injuries were to the nasal bone or the bony region above the eye (supraorbital ridge) and 43% were to the eye itself. Thirty-seven per cent of upper limb injuries were to the fingers (proximal phalanx) and the ankle and knee each made up 28% of the lower limb injuries.21 Of the hospital-attended injuries in females in Victoria, Australia, the wrist and hand made up the majority of upper limb injuries in ED presentations (29%) and hospital admissions (17%), with the knee being the most common injured region of the lower limb in ED presentations (12%) and admissions (22%).22 Of the wicket-keepers injured in indoor cricket, 71% were eye injuries due to being struck by the ball.21 The study of NZ insurance claims reported that of the moderate to serious claims (n=3072) for the head/neck/face region, 31% of the claims were to the head, with 25% to nose specifically and 25% to other facial areas. For the upper limb, 41% of the claims were to the finger/thumb, 32% to the shoulder and 15% to the wrist/hand. For the lower limb, the majority of claims were for the knee (51%) and ankle (26%). In the trunk/back region, the chest (44%) was the most common claim, with back/spine (26%) and abdomen/pelvis (25%) at similar levels. For serious claims (n=27), 56% were to the head and 44% to the hip, upper leg and thigh.17
Mechanism of injury
Table 5 summarises the broad mechanisms of injury reported by four studies. Being struck by the ball was consistently the highest proportion of mechanism reported, varying from 31.4%19 to 98.4%.21 Being struck by the bat or equipment was relatively high in the ED presentations for children (23.3%)18 when compared with the hospital admission proportion of 7.2% for a broader age group (2 to 80 years); however in the same study, it was reported that for children under 10 years the proportion was 72%.19 An Australian study looking at female cricket injuries reported higher proportions of ED presentations compared with hospital admissions for being struck by the ball or bat.22 An earlier Australian study on ED presentations noted that head and facial injuries in children (<15 years) were generally associated with being hit by the ball or bat, though numerical data were not available.20 Non-specific fall and player collisions were similar across ED presentations and hospital admissions for the two NZ studies despite the age range differences.18 19
Table 5.
Broad mechanism of injury as a percentage of all medical-attention injuries in community cricket
| First author, year (reference) | No of injuries | Struck by ball | Struck by bat or equipment | Non-specific overexertion | Non-specific falls | Player collision | Other/NR |
| Perera, 201922 | |||||||
| HA | 121 | 44.6* | 12.4 | 27.3 | – | 15.7 | |
| ED | 547 | 63.8* | – | 19.0 | – | 17.2 | |
| Walker, 201019 | 498 | 28.9 | 6.6 | 20.5 | 21.7 | 6.8 | 15.5 |
| Upadhyay, 200018 | 60 | 51.7 | 23.3 | – | 20.0 | 5.0 | – |
| Forward, 198821 | 65 | 98.4 | 1.6 | – | – | – | – |
*Struck by ball or bat combined.
ED, emergency department presentations; HA, hospital admissions; NR, not reported.
Position of play when injured
One study, for indoor cricket, provided information on injuries with regard to the position of play for the injured player, with injuries occurred mainly in fielding (72%) and then batting (17%).21
Injury severity
One study identified 21.5% of hospitalised cricket-related injuries to females in Victoria, Australia, required a bed stay of two or more days.22 One study identified that 4% (n=20) of cricket-related hospital admissions were classified as serious non-fatal injuries on the International Classification Injury Severity Score (ICISS) scale. Of these, 11 were due to being struck by the ball, 6 due to collisions with other players, 2 from falls and 1 from overexertion.19 For children (aged 9–13 years) presenting to ED in NZ, 30% did not require hospital admission and 32% required operative procedures. Two children had abdominal trauma injuries that were classified as severe. The median range for days of stay in hospital for the operative cases among the children was 1 to 2.5 days.18 The severity of injuries from indoor cricket presentations to ED in Australia was measured by time off work. Equal proportions of cases required no time off work (19%), less than 1 week off work (19%) and between 1 week and 1 month off work (19%). Eleven per cent of cases required greater than 1 month off work.21 For the study that investigated moderate to serious and serious injury claims for cricket-related insurance claims in NZ, 0.5% (n=15) of claims were serious. Although not reported specifically for cricket, minor injuries accounted for 93% of all claims.
Discussion
Main findings
Data items for improved reporting
Successful injury prevention strategies should be informed by high-quality injury data. Medical-attention injuries were chosen as the focus of this review because they are costly to the public health system23 (and individuals) and because the diagnosis from a medical professional is considered to provide more accurate results than self-report data.24 25 For medical-attention community cricket injuries, we identified six studies that reported epidemiological data inclusive of all body parts/injury types. Only two studies were considered to have a low likelihood of bias, meaning that the reported results could be subject to selection and information biases.26 Two key areas are highlighted for inclusion in future original research studies: item 4 (missing data and subject attrition) and item 9 (reporting of ethical standards, conflicts of interest and funding). A further four items were only moderately well addressed and should be considered for improved reporting: item 7 (study limitations), item 5 (injury definition), item 3 (description of data collection method) and item 2 (study setting).
High prevalence of fractures and head injuries
As might be expected from the data sources, the types of injuries that were treated in hospitals/EDs were primarily fractures. Cricket is a projectile sport and it is likely that many of the fractures were due to being struck by the ball and or equipment, as has been reported in a prospective cohort study of junior players in Australia.27 Falls are another common mechanism that can lead to fracture. For injuries requiring hospital treatment, the head/face/neck was the second most common injured body region behind the upper limb. An interesting observation from the hospital data was that the overall proportions of head/face/neck cases seen in females, in Victoria, Australia, from 2002 to 2012 were similar to those reported for both sexes (but would be predominantly male) throughout Australia from 1989 to 1993.20 22 Although difficult to compare directly between the studies, it might suggest a possible issue with helmet use. Given that helmets have been shown to be protective, specifically at junior levels in cricket,28 and anecdotally against fatalities,29 we might expect to see a comparatively lower proportion in the more recent study, especially as the data used were largely from the period in which the wearing of helmets was generally mandatory for players under the age of 18 years. There may be other factors involved in the comparable proportion of head/face/neck face injuries. Other factors include improper fitting of helmets, lax regulation of wearing protective equipment, especially at training, or the injuries occurring in other aspects of the game such as in the field, where protective equipment is not normally mandated.
Another recent study based on insurance claims data from NZ reported lower proportions of head/neck/face injuries than the Australian hospital data and other earlier studies.17 The relatively low proportion of head/neck/face injuries in the insurance claim data is possibly reflective of the nature of injuries recorded in this dataset (being a no-fault claims system), rather than a clear reduction in the proportion of cases (when compared with the hospital data from earlier timeframes). Regardless of the reason for the change, 50% of these injuries were to the face. Investigation of the mechanisms for these injuries, including the use of appropriate personal protection (such as a helmet with face guard for batters/wicket-keepers and protective glasses for wicket-keepers), is needed.
Injuries over time
Besides the number and types of injuries sustained, the temporal patterns and incidence rates need to be understood. Looking at injury over time enables practitioners to identify when, what and in whom cases are increasing or decreasing, therein supporting the decisions required on prevention measures. One of the difficulties in presenting injury incidence rates, and possibly why only two studies19 22 reported these, is the requirement for an accurate denominator (risk exposure). Cricket is a sport with several, separate activities (batting, bowling and fielding) which further complicates accurate collection of exposure data. Although guidance for this data collection is presented in the consensus statements,25 30 this guidance is best suited to the elite levels of the game. Improving the consistency of injury surveillance including exposure to injury risk at a community level requires a targeted and tailored approach within those settings.6
Limitations
The type and consistency of data extracted from the articles in this review limited our ability to conduct any quantitative analysis. Due to the majority of the studies within this review being outdated, it is difficult to provide unequivocal recommendations from the data reported.
While hospital data can be a useful, routinely collected, source of acute injury data, reliance on it underestimates the overall prevalence of cricket injuries as it is likely that many will not require hospital treatment. Earlier research has reported that up to 50% of adults with a sports injury seek treatment by a community-based practitioner, including family doctors, physiotherapists or sports medicine specialists.31 32 While not included in this review due to the lack of detailed epidemiological data, two studies were identified in which the proportion of injury by sport was noted for a sports medicine clinic (wherein 3% of 6479 cases and 4% of 1682 cases in consecutive years were cricket related33 and a general practice (5% of 78 were cricket related).34 The level of organisation (eg, formal or recreational) in which the cricket was played when the injury occurred is also often not known with any accuracy, which can hamper specific advice for injury prevention policy.
In addition to limitations of the included studies, there were also limitations of the review process itself that need to be considered in understanding the results. The search strategy was deliberately broad to identify all original cricket-related studies, including reference searches and knowledge from two authors with extensive cricket research backgrounds. However, it is still possible that large studies reporting on all types of sports or other injuries could have reported on cricket, within a subgroup analysis (as similar to those that were identified).
The tool used for critical appraisal of the included studies was self-developed, based on the Downs and Black tool13 and STROBE statement,14 with reference to bias assessment from Hoy et al16 and the Cochrane Collaboration.15 While not formally validated, the items were agreed by the author team to be the minimum data for reporting and interpreting injury data in line with the study aim. It is, however, possible that the tool may overestimate or underestimate the quality of the studies reviewed.
Conclusions
From studies of medical-attention injuries in community cricket, fractures, bruising and open wounds/lacerations were identified as relatively more common than other injury types. The majority of these injuries were likely sustained by players being struck by the ball. However, the evidence on which these findings are based is largely outdated and biased toward hospital-treated cases. Head/neck and face injuries were relatively common, suggesting that further investigations of their injury mechanism and the use of appropriate personal protective equipment are needed.
Acknowledgments
GM, CFF and LVF are part of the Australian Centre for Research into Injury in Sport and its Prevention (ACRISP) at Edith Cowan University. ACRISP is one of the International Research Centres for the Prevention of Injury and Protection of Athlete Health supported by the IOC.
Footnotes
Twitter: @SiobhanOConnor3, @@CarolineFinch, @lfortington
Contributors: GM wrote the study protocol, performed the literature search, article selection, data extraction, critical appraisal and bias analysis and is the first author of the article. SOC assisted in the article selection, data extraction, critical appraisal and bias analysis as well as contributing to editing the article. DM reviewed the protocol and provided review and editing of the article. AK and CFF assisted in providing expert advice on article selection and reviewed and edited the article. LVF assisted in the study protocol, article selection, critical appraisal and bias analysis and contributed to reviewing and editing of the article.
Funding: GM is a recipient of an Australian Government Research Training Scheme fee offset scholarship and is further supported by a scholarship from JLT Sport, CA and ACRISP.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Finch CF, Elliott BC, McGrath AC. Measures to prevent cricket injuries: an overview. Sports Med 1999;28:263–72. 10.2165/00007256-199928040-00004 [DOI] [PubMed] [Google Scholar]
- 2.Cricket Australia 2017/18 Anual report, 2018. Available: https://www.cricketaustralia.com.au/media/media-releases/cricket-australia-announces-annual-results-for-2017-18/2018-10-25 [Accessed 26 Oct 2018].
- 3.Orchard J, James T, Alcott E, et al. Injuries in Australian cricket at first class level 1995/1996 to 2000/2001. Br J Sports Med 2002;36:270–4. 10.1136/bjsm.36.4.270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hägglund M, Waldén M, Ekstrand J. Injury recurrence is lower at the highest professional football level than at national and amateur levels: does sports medicine and sports physiotherapy deliver? Br J Sports Med 2016;50:751–8. 10.1136/bjsports-2015-095951 [DOI] [PubMed] [Google Scholar]
- 5.Finch C, Williams F, Ozanne-Smith J. The feasibility of improved data collection methodologies for sports injuries: Monash University accident research centre, 1995. Available: https://www.monash.edu/muarc/archive/our-publications/reports/muarc069 [Accessed 20 May 2019].
- 6.Finch CF. Injury data collection in lower leagues needs to be targeted specifically to those settings. Science and Medicine in Football 2017;1:89–90. 10.1080/24733938.2016.1256555 [DOI] [Google Scholar]
- 7.Finch C, Owen N, Price R. Current injury or disability as a barrier to being more physically active. Med Sci Sports Exerc 2001;33:778–82. 10.1097/00005768-200105000-00016 [DOI] [PubMed] [Google Scholar]
- 8.Andrew N, Wolfe R, Cameron P, et al. The impact of sport and active recreation injuries on physical activity levels at 12 months post-injury. Scand J Med Sci Sports 2014;24:377–85. 10.1111/j.1600-0838.2012.01523.x [DOI] [PubMed] [Google Scholar]
- 9.Ekegren CL, Gabbe BJ, Finch CF. Medical-attention injuries in community Australian football: a review of 30 years of surveillance data from treatment sources. Clin J Sport Med 2015;25:162–72. [DOI] [PubMed] [Google Scholar]
- 10.University of York, Centre for Reviews and Dissemination About Prospero, 2018. Available: www.crd.york.ac.uk/prospero/#aboutpage [Accessed 30 Apr 2018].
- 11.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 12.Australian Sports Injury Data Working Party. Australian Sports Injury Data Dictionary Guidelines for injury data collection and classification for the prevention and control of injury in sport and recreation, 1998. Available: http://sma.org.au/sma-site-content/uploads/2018/10/Australian-Sports-Injury-Data-Dictionary.pdf [Accessed 21 Feb 2018].
- 13.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377–84. 10.1136/jech.52.6.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Prev Med 2007;45:247–51. 10.1016/j.ypmed.2007.08.012 [DOI] [PubMed] [Google Scholar]
- 15.Higgins JPT, Green S. Cochrane Handbook for systematic reviews of interventions version 5.1.0: the Cochrane Collaberation, 2011. Available: www.handbook-5-1.cochrane.org/ [Accessed 7 Mar 2011].
- 16.Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol 2012;65:934–9. 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 17.King D, Hume PA, Hardaker N, et al. Sports-related injuries in New Zealand: National insurance (Accident Compensation Corporation) claims for five sporting codes from 2012 to 2016. Br J Sports Med 2019;53:1026–33. 10.1136/bjsports-2017-098533 [DOI] [PubMed] [Google Scholar]
- 18.Upadhyay V, Tan A. Cricketing injuries in children: from the trivial to the severe. N Z Med J 2000;113:81–3. [PubMed] [Google Scholar]
- 19.Walker HL, Carr DJ, Chalmers DJ, et al. Injury to recreational and professional cricket players: circumstances, type and potential for intervention. Accid Anal Prev 2010;42:2094–8. 10.1016/j.aap.2010.06.022 [DOI] [PubMed] [Google Scholar]
- 20.Finch C, Valuri G, Ozanne-Smith J. Sport and active recreation injuries in Australia: evidence from emergency department presentations. Br J Sports Med 1998;32:220–5. 10.1136/bjsm.32.3.220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Forward GR. Indoor cricket injuries. Med J Aust 1988;148:560–1. 10.5694/j.1326-5377.1988.tb93811.x [DOI] [PubMed] [Google Scholar]
- 22.Perera NKP, Kemp JL, Joseph C, et al. Epidemiology of hospital-treated cricket injuries sustained by women from 2002-2003 to 2013-2014 in Victoria, Australia. J Sci Med Sport 2019;22:1213–8. 10.1016/j.jsams.2019.07.010 [DOI] [PubMed] [Google Scholar]
- 23.Cassell E, Kerr E, Clapperton A, et al. Hazard Ed. 74 adult sports injury hospitalisations in 16 sports: the football codes, other team ball sports, team bat and stick sports and raquet sports. Available: https://www.monash.edu/__data/assets/pdf_file/0009/218475/haz74.pdf
- 24.Gabbe BJ, Finch CF, Bennell KL, et al. How valid is a self reported 12 month sports injury history? Br J Sports Med 2003;37:545–7. 10.1136/bjsm.37.6.545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orchard JW, Ranson C, Olivier B, et al. International consensus statement on injury surveillance in cricket: a 2016 update. Br J Sports Med 2016;50:1245–51. 10.1136/bjsports-2016-096125 [DOI] [PubMed] [Google Scholar]
- 26.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med 2007;4:e297 10.1371/journal.pmed.0040297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Finch CF, White P, Dennis R, et al. Fielders and batters are injured too: a prospective cohort study of injuries in junior club cricket. J Sci Med Sport 2010;13:489–95. 10.1016/j.jsams.2009.10.489 [DOI] [PubMed] [Google Scholar]
- 28.Shaw L, Finch CF. Injuries to junior club cricketers: the effect of helmet regulations. Br J Sports Med 2008;42:437–40. 10.1136/bjsm.2007.041947 [DOI] [PubMed] [Google Scholar]
- 29.Brukner P, Gara TJ, Fortington LV. Traumatic cricket-related fatalities in Australia: a historical review of media reports. Med J Aust 2018;208:261–4. 10.5694/mja17.00908 [DOI] [PubMed] [Google Scholar]
- 30.Orchard J, Newman D, Stretch R, et al. Methods for injury surveillance in international cricket. J Sci Med Sport 2005;8:1–14. 10.1016/S1440-2440(05)80019-2 [DOI] [PubMed] [Google Scholar]
- 31.Mummery WK, Schofield G, Spence JC. The epidemiology of medically attended sport and recreational injuries in Queensland. J Sci Med Sport 2002;5:307–20. 10.1016/S1440-2440(02)80019-6 [DOI] [PubMed] [Google Scholar]
- 32.Mitchell R, Finch C, Boufous S. Counting organised sport injury cases: evidence of incomplete capture from routine hospital collections. J Sci Med Sport 2010;13:304–8. 10.1016/j.jsams.2009.04.003 [DOI] [PubMed] [Google Scholar]
- 33.Finch CF, Mitchell DJ. A comparison of two injury surveillance systems within sports medicine clinics. J Sci Med Sport 2002;5:321–35. 10.1016/S1440-2440(02)80020-2 [DOI] [PubMed] [Google Scholar]
- 34.Jago D, Finch C. Sporting and recreational injuries. in a general practice setting. Aust Fam Physician 1998;27:389–95. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2019-000670supp001.pdf (140.6KB, pdf)