Retinal detachment is an important cause of vision loss
Retinal detachment occurs when vitreous fluid enters through a retinal tear or hole leading to separation of the retina from the choroid, similar to water behind wallpaper (Figure 1).1 Lifetime risk of retinal detachment is about 0.1% and is higher in patients who are older, have high myopia (nearsightedness greater than –6.0 diopters), have a history of ocular trauma or prior eye surgery, or a family history of retinal detachment.2–4 The importance of wearing protective eyewear during contact sports should be emphasized to patients with high myopia.4
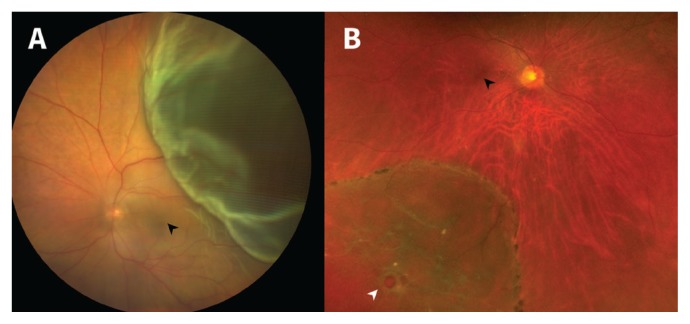
Figure 1:
(A) Fundus photograph of the left eye showing an acute retinal detachment in the superotemporal quadrant of the retina. It is elevated and bullous in appearance, and hides the underlying choroidal vessels from view. Given the proximity of the detachment to the macula (black arrowhead), a gas bubble was emergently injected into the eye to treat and preserve central vision. (B) Fundus photograph of the right eye showing a chronic retinal detachment in the inferotemporal quadrant with a retinal hole (white arrowhead) and a pigment demarcation line at the leading edge. The macula (black arrowhead) was not involved. A laser was used to treat the detachment to prevent progression of fluid toward the macula.
New-onset unilateral visual field loss associated with seeing flashing lights or floaters is retinal detachment until proven otherwise
Patients often describe the subsequent visual field loss as a dark shadow appearing in their peripheral vision that progresses centrally within hours to weeks.4
Bilateral confrontational visual field testing must be performed
Office-based confrontational visual field testing can distinguish between a bilateral field defect, which is suggestive of a central neurologic process, and a unilateral field defect, which is suggestive of an ocular cause.4
Patients with a suspected retinal detachment should be referred immediately to an ophthalmologist
A dilated eye examination can diagnose a retinal detachment and identify whether it involves the central retina (macula). If there is no involvement of the macula, the patient requires urgent intervention to prevent further progress that could affect central vision.
Treatment can restore vision
Some retinal detachments can be treated in a clinic setting by lasering the retina or by injecting a gas bubble into the eye to reattach the retina.1 After treatment, patients must maintain appropriate head posture to position the gas bubble over the retinal break and avoid air travel because bubble expansion can occur with changes in atmospheric pressure.5 Complex retinal detachments, characterized by multiple retinal tears or the presence of retinal scar tissue, are typically repaired using a pars plana vitrectomy or scleral buckling procedure in an operating room.1
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
References
- 1.Sodhi A, Leung LS, Do DV, et al. Recent trends in the management of rhegmatogenous retinal detachment. Surv Ophthalmol 2008;53:50–67. [DOI] [PubMed] [Google Scholar]
- 2.Lindsell LB, Sisk RA, Miller DM, et al. Comparison of outcomes: scleral buckling and pars plana vitrectomy versus vitrectomy alone for primary repair of rhegmatogenous retinal detachment. Clin Ophthalmol 2016;11:47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mitry D, Charteris DG, Fleck BW, et al. The epidemiology of rhegmatogenous retinal detachment: geographical variation and clinical associations. Br J Ophthalmol 2010;94:678–84. [DOI] [PubMed] [Google Scholar]
- 4.Gariano RF, Kim CH. Evaluation and management of suspected retinal detachment. Am Fam Physician 2004;69:1691–8. [PubMed] [Google Scholar]
- 5.Mills MD, Devenyi RG, Lam WC, et al. An assessment of intraocular pressure rise in patients with gas-filled eyes during simulated air flight. Ophthalmology 2001;108:40–4. [DOI] [PubMed] [Google Scholar]