Abstract
Objective
Outpatient hysteroscopy is often accompanied by pain and discomfort along with frequent occurrence of bradycardia and hypotension. This study aimed to observe if intravenous low-dose ketamine reduces the pain scores along with lowering the incidence of bradycardia and hypotension during hysteroscopy.
Methods
This prospective, randomised, double-blind trial was conducted in operating rooms in a tertiary care hospital. In this study, we enrolled 72 patients with American Society of Anesthesiologists status I to II undergoing hysteroscopy. We randomised patients into two groups, and both groups received paracervical block. The control group received intravenous pentazocine and promethazine along with saline infusion. The ketamine group received ketamine infusion (0.75 mg kg−1 bolus followed by infusion at the rate of 10 mcg kg−1 min−1). We analysed visual analogue scale (VAS), rescue analgesic consumption, hemodynamic parameters, lowest recorded heart rate, blood pressure, level of sedation, patient’s comfort, surgeon’s satisfaction and nursing staff’s satisfaction.
Results
Analysis of the data revealed that the pain scores were similar in both the groups (p=0.493, p<0.001). Rescue analgesic was required by 47% patients in control group, compared to only 5.6% patients in ketamine group. Episodes of bradycardia and hypotension were more pronounced in the control group than in the ketamine group [77.4±10.9 vs. 78.4±5.5; 67.6±8 vs. 70.1±6 respectively] (p<0.001). Patient comfort and surgeon’s satisfaction were higher in the ketamine group, but nursing satisfaction was higher in the control group. Disorientation was present in 75% patients in the ketamine group as compared to none in the control group.
Conclusion
We concluded that low-dose ketamine in day-care hysteroscopy is an effective and safe agent.
Keywords: Ambulatory surgery, ketamine, systemic effects
Introduction
Hysteroscopy is a common and routine procedure carried out on an outpatient basis for both diagnostic and therapeutic purposes. It is regarded as a safe procedure; however, it is often associated with pain and discomfort. Pain relief for outpatient hysteroscopy has been the quest for various studies (1, 2). Associated occurrence of nausea, bradycardia and hypotension has also been reported in literature (3). Ketamine is an indirectly acting sympathomimetic drug that acts through the release of catecholamines from the adrenal medulla. By blocking the NMDA receptor, ketamine attenuates centrally mediated pain processes, thereby reducing acute pain. Because of its potential to blunt central sensitisation, ketamine provides postoperative analgesia even after infusion is stopped (3). It has anaesthetic and analgesic property, and it causes tachycardia and hypertension as side effects. These properties can be utilised for pain relief during hysteroscopy, and the side effects can be exploited to counteract the associated bradycardia and hypotension.
Low-dose ketamine is defined as a bolus dose of less than 1 mg kg−1 when administered via the intravenous (IV) route or ≤20 mcg kg−1 min−1 in continuous intravenous infusion (4).
This study aimed to observe if low-dose ketamine reduces the pain scores and decreases the incidence of bradycardia during outpatient hysteroscopy in nulliparous women. Our primary aim was to compare the intraoperative pain scores in patients undergoing outpatient hysteroscopy with or without low-dose ketamine infusion. Our secondary research questions were to determine the amount of rescue analgesic required; compare the incidence of bradycardia and hypotension in patients undergoing outpatient hysteroscopy with or without low-dose ketamine infusion; assess patient satisfaction, surgeon satisfaction and nursing staff satisfaction during recovery of patients in post-anaesthesia care unit (PACU) (5); and to observe any side effects.
Methods
The prospective, randomised double-blind study was conducted in the Department of Anaesthesiology, AIIMS, New Delhi after approval by the institute ethics committee (Ref. No. IEC-131/07.04.2017, RP-4/2017). Study was registered in Clinical Trials Registry of India - CTRI/2017/05/008516. A written informed consent was obtained from all the patients.
Inclusion criteria were American Society of Anesthesiologist Physical status I and II, nulliparous women aged 18–40 years, scheduled for hysteroscopy as a day-care procedure. Exclusion criteria before procedure were patients on analgesic medication for other ailments, patients with cardiac disorders and patients requiring general or other anaesthetic agent for some reason during the procedure.
The patients underwent pre-anaesthetic evaluation in the pre-anaesthesia clinic before being posted for surgery and were instructed to come fasting according to the standard guidelines. In the morning of surgery, intravaginal misoprostol 400 mcg was given for cervical priming. An IV access was obtained, and IV midazolam 50 mcg kg−1 was administered 10 min before the procedure as premedication.
We divided the patients into two groups based on computer-generated random numbers: control group - paracervical block with IV bolus of pentazocine (15 mg) and promethazine (12.5 mg) along with IV saline infusion; and ketamine group - paracervical block with IV ketamine 0.75 mg kg−1 bolus followed by IV infusion of ketamine at the rate of 10 mcg kg−1 min−1.
Paracervical block with IV bolus of pentazocine (15 mg) and promethazine (12.5 mg) as done in the control group is the standard departmental practice in which the paracervical block is administered by gynaecologist using 1% lignocaine with adrenaline 10–15 mL. IV saline infusion acted as a placebo. In both the groups, IV infusion with or without ketamine analgesia was immediately stopped at the end of the procedure when the hysteroscope was taken out. Bradycardia and hypotension was defined as less than 20% of the baseline recording.
Patients with Ramsay sedation score of 1 received further IV midazolam 50–100 mcg kg−1 for sedation and were excluded from study.
Any patient requiring additional analgesia during the procedure or within 2 h after the procedure (VAS>3) was given IV fentanyl 0.5 mcg kg−1, and the amount of rescue fentanyl was noted. The patients were discharged home with oral paracetamol 1 g TDS (three times a day) for analgesia. The surgical stimulation was kept constant by using a 4-mm sized hysteroscope in all cases.
The following parameters were noted:
Visual analogue score (VAS) every 15 min from onset till 2 h of procedure,
Number of patients requiring rescue analgesia in each group,
Hemodynamic parameters at the beginning and every 5 min during the procedure,
Lowest recorded heart rate and blood pressure during the procedure,
-
Level of sedation during the procedure using Ramsay sedation scale.
Anxious and agitated or restless, or both,
Co-operative, oriented and calm,
Responsive to commands only,
Exhibiting brisk response to light glabellar tap or loud auditory stimulus,
Exhibiting a sluggish response to light glabellar tap or loud auditory stimulus,
Unresponsive.
Patient’s comfort and overall experience of the anaesthesia technique in three-point scale (1=poor, 2=good, 3=excellent),
Surgeon’s satisfaction (1=poor, 2=good, 3=excellent),
Nursing staff’s satisfaction during recovery of patients in PACU (1=poor, 2=good, 3=excellent),
Any adverse effects (PONV, disorientation/delirium).
The sample size calculation was done by doing a pilot study of ten cases in each group and with an alpha error of 0.05 and power of the study 90%. To detect a minimum difference of 20% in pain score with standard deviation (SD) of 2.5, we needed a sample size of 36 in each group.
All the patients were randomised by computer-generated random numbers and subsequently divided into one of the two groups by sequentially numbered sealed opaque envelope technique prepared by the statistician.
The attending anaesthesiologist in the hysteroscopy room prepared the saline or the ketamine bolus as well as the infusion syringe in equal volume to ensure both the syringes are indistinguishable. An independent investigator who was blinded to the drug used, noted all the parameters during intraoperative and postoperative period.
Results were presented in mean (SD)/median (min–max) and frequency (%). Mean difference and 95% confidence interval opioid consumption (fentanyl) among the groups at 48 h was calculated. Continuous variables were compared amongst the groups by one-way ANOVA/Kruskal-Wallis test as appropriate and within change in the continuous variables were assessed by repeated measure ANOVA/Friedmans test as appropriate.
Statistical analysis
Categorical variables were compared amongst the groups by chi square or Fisher exact test. Other appropriate statistical analysis carried out at the time of analysis. P-value less than 0.05 was considered as statistically significant.
Results
Total of 90 patients were screened for the study, and 72 patients were enrolled as per the inclusion criteria. Two patients in the control group required IV midazolam because of poor Ramsay’s sedation score and hence were excluded from the study. Details of patient recruitment are shown in the CONSORT diagram (Figure 1). Demographic characteristics were comparable between the two groups (Table 1).
Figure 1.
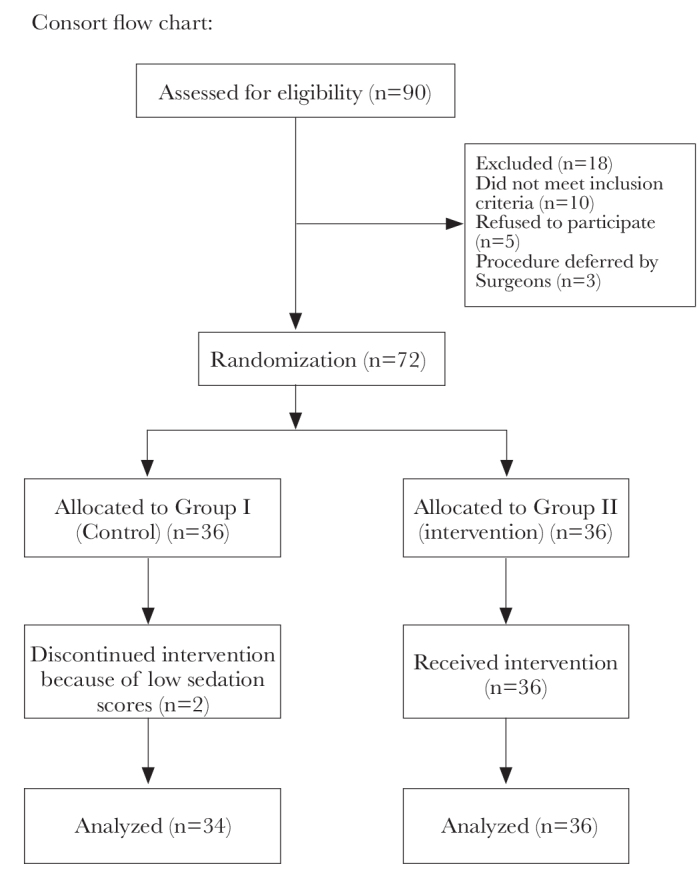
CONSORT flow diagram
Table 1.
Demographic characteristics and visual analogue scores at various time intervals (values as mean±SD)
| Variables | Control group (n=34) | Ketamine group (n=36) | p |
|---|---|---|---|
|
| |||
| Age (years) | 28±4.8 | 29.8±6.4 | 0.171 |
| Weight (kg) | 65.6±7.6 | 64.2±6.4 | 0.383 |
| VAS at 15 min | 2.9±1.3 | - | - |
| VAS at 30 min | 2.4±0.9 | - | - |
| VAS at 45 min | 2.2±0.7 | 2.0±0.9 | 0.26 |
| VAS at 60 min | 1.7±0.6 | 1.8±0.7 | 0.42 |
| VAS at 75 min | 1.5±0.5 | 1.7±0.6 | 0.15 |
| VAS at 90 min | 1.7±0.5 | 1.6±0.6 | 0.27 |
| VAS at 105 min | 1.3±0.5 | 1.7±0.5 | 0.25 |
| VAS at 120 min | 1.3±0.4 | 1.2±0.4 | 0.68 |
VAS scores: visual analogue scores; SD: standard deviation
Hysteroscopy is a short procedure. It took around 15–45 min, mean (SD) being 30.1±3.4 min in the control group and 31.9±2.9 min in the ketamine group. Pain assessment was started from the onset of the procedure and recorded every 15 min for 2 h. The VAS score at 15 and 30 min could not be assessed in the ketamine group as the patients were deeply sedated and did not respond to verbal commands during the procedure time. Thereafter, pain scores were comparable in both the groups at all time points with the overall p=0.493 (Table 1).
The number of patients requiring rescue analgesia in the form of IV fentanyl was considerably higher in the control group as compared to that in the ketamine group. Only 2 (5.6%) patients in the ketamine group required additional fentanyl as compared to 16 (47%) patients in the control group (p<0.001) (Table 2).
Table 2.
Number of patients requiring rescue analgesia and having postoperative nausea vomiting and disorientation. Values as frequency (percentage)
| Variables | Control group (n=34) f(%) | Ketamine group (n=36) f(%) | p |
|---|---|---|---|
|
| |||
| Fentanyl used | |||
| No | 18 (52.9) | 34 (94.4) | <0.001 |
| Yes | 16 (47) | 2 (5.6) | |
| PONV | |||
| No | 34 (100) | 33 (91.6) | 0.240 |
| Yes | 0 (0) | 3 (8.3) | |
| Disorientation | |||
| No | 34 (100) | 9 (25) | <0.001 |
| Yes | 0 (0) | 27 (75) | |
PONV: postoperative nausea vomiting
Trend of hemodynamic parameters in the form of heart rate (HR) and mean arterial pressures (MAP) were assessed starting from the onset of procedure (T0) till the end of procedure every 5 min. Significant bradycardia or hypotension was not seen in either group; however, the hemodynamic parameters remained more near the baseline values in the ketamine group as compared to those in the control group. The statistical analysis done on the increase or decrease of MAP and HR showed at each time point which was significantly different at many points (Table 3, Figure 2 and 3).
Table 3.
Haemodynamic trends measured as the mean arterial pressure in mmHg (MAP) and heart rate per minute (HR. min−1)
| Parameter | Group | T0 | T5 | T10 | T15 | T20 | T25 | T30 | T35 | Overall p-value |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| MAP mm Hg | Control group (mean±SD) | 78.7±4.9 | 80.1±5.5 | 84.6±5.4 | 81.6±7.1 | 78.7±5.8 | 79.3±6.4 | 78.1±6.1 | 75.5±5.5 | <0.01 |
| Ketamine group (mean±SD) | 75.4±6.6 | 79.3±6.1 | 78.3±5.4 | 75.8±5.2 | 75.6±4.9 | 75.8±4.7 | 75.9±5.2 | 75.5±5 | ||
| P-value | 0.58 | 0.03 | 0.06 | 0.20 | 0.21 | 0.24 | 0.08 | |||
|
| ||||||||||
| HR. min−1 | Control group (mean±SD) | 78.2±10.9 | 86.5±9.2 | 102.2±8.6 | 98.2±7.3 | 94.9±6.4 | 90.3±6.2 | 86.4±6.4 | 82.7±6.1 | <0.01 |
| Ketamine group (mean±SD) | 78±8.5 | 85.9±8.6 | 87.9±8.3 | 87±7.1 | 85.8±6.6 | 85.9±5.8 | 81.9±6.6 | 81.7±6.3 | ||
| p-value | 0.76 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | 0.57 | |||
Values as mean±SD (standard deviation)
Figure 2.
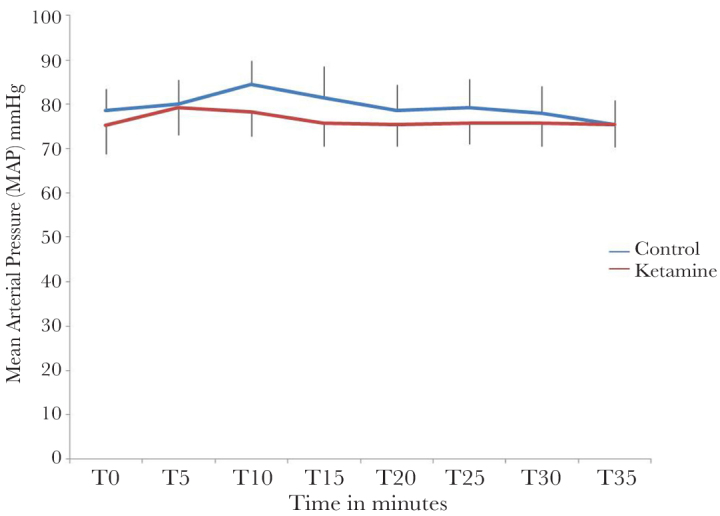
Mean arterial pressure (MAP) trend
Figure 3.
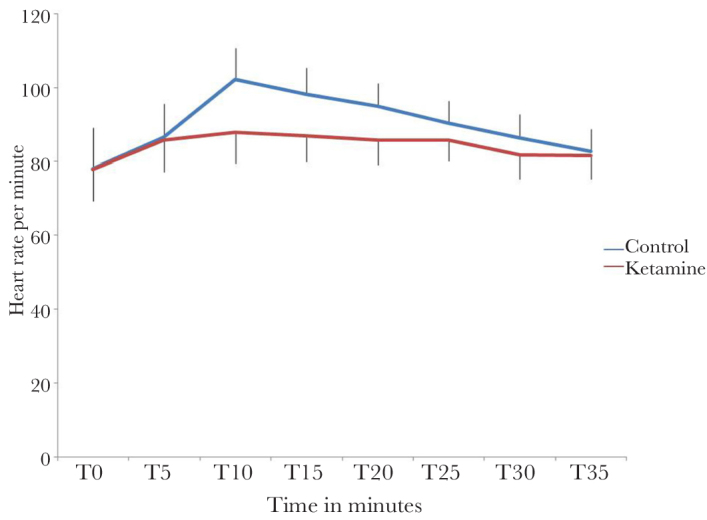
Heart rate trend
Incidence of bradycardia (as measured by lowest recordable HR) was lower in the ketamine group as supported by statistical significance. There were fewer episodes of hypotension (as measured by lowest recorded MAP) in the ketamine group as compared to those in the control group; and the result was statistically significant (p<0.001) (Table 4).
Table 4.
Lowest recorded heart rate per minute and mean arterial pressure in mmHg. Values as mean±SD
| Variables | Control group (n=34) | Ketamine group (n=36) | p |
|---|---|---|---|
|
| |||
| Lowest HR | 77.4±10.9 | 78.4±5.5 | <0.001 |
| Lowest MAP | 67.6±8 | 70.1±6 | <0.001 |
HR: heart rate; MAP: mean arterial pressure; SD: standard deviation
Ramsay sedation scores were significantly more in the ketamine group as compared to those in the control group (p<0.001). Intraoperatively, patients in the ketamine group had sedation scores of approximately 4, and therefore verbal communication could not be established to assess VAS during this period (Table 5).
Table 5.
Ramsay Sedation scores. (Values as Mean±SD minutes)
| T0 | T5 | T10 | T15 | T20 | T25 | T30 | T35 | Overall p-value | |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Control group | 1.5±0.5 | 1.8±0.4 | 2.1±0.5 | 2.4±0.5 | 2.7±0.7 | 3.1±0. | 3.4±0.8 | 3.7±0.7 | <0.001 |
| Ketamine group | 1.3±0.5 | 4.4±0.7 | 4.6±0.5 | 4.5±0.5 | 4.5±0.6 | 4.4±0.6 | 4.2±0.6 | 3.8±0.6 | |
| p | 0.24 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | 0.62 | |
T: time points in minutes; SD: standard deviation
Patients and surgeons in the ketamine group were more satisfied as compared to those in the control group as evident from the statistically significant values of satisfaction scores (p<0.001). However, nursing staff’s satisfaction was lower in the ketamine group mainly because of higher delirious state of patients requiring more nursing attention thus translating to lower satisfaction scores (Table 6).
Table 6.
Satisfaction scores in a 3 point scale (1=poor, 2=good, 3=excellent).Values as frequency (percentage)
| Satisfaction Levels | Patient | Surgeon | Nursing | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Control group (n=34) | Ketamine group (n=36) | Control group (n=34) | Ketamine group (n=36) | Control group (n=34) | Ketamine group (n=36) | |
|
| ||||||
| Poor | 30 (88.2%) | 0 (0) | 28 (82.3%) | 0 (0) | 1 (2.94%) | 14 (38.8%) |
| Good | 3 (8.8%) | 7 (19.4%) | 4 (11.7%) | 3 (8.3%) | 22 (64.7%) | 11 (30.5%) |
| Excellent | 1 (2.9%) | 29 (80.6%) | 2 (5.8%) | 33 (91.6%) | 11 (32.6%) | 11 (30.5%) |
|
| ||||||
| p | 0.001 | 0.001 | 0.001 | |||
Postoperative nausea and vomiting (PONV) was seen in 3 (8.3%) patients in the ketamine group and none in the control group (p=0.240). Delirium was present in 27 (75%) patients in the ketamine group and none in the control group (p<0.001) (Table 2).
Discussion
Hysteroscopy is a routine procedure carried out on an outpatient basis for both diagnostic and therapeutic procedures. It is often referred to as ‘office hysteroscopy’ done as an ambulatory procedure. Although considered safe, it is often associated with pain and discomfort and occasional occurrence of bradycardia and hypotension (6). Although the procedure is acceptable for 90% of patients, the use of analgesics has been shown to increase the success rate. Pain is attributed as one of the reasons for failure; and amongst the failures, around 29.4% has been attributed to inadequate analgesia (7). Moderate to severe pain has been reported to be around 5.4%–16% in outpatient hysteroscopy without anaesthesia (8, 9). Cochrane database systematic reviews report insufficient data to determine the appropriate analgesia or anaesthesia for hysteroscopy (10, 11).
The role of cervical preparation before hysteroscopy has also been extensively studied to alleviate the pain and discomfort associated with the procedure. The role of cervical priming with misoprostol, mifepristone or prostaglandins has not shown to reduce pain in routine outpatient hysteroscopy (12). Misoprostol 400 mcg is routinely given for cervical priming in our institute.
Transcervical intrauterine instillation of local anaesthetic was found to be ineffective in eliminating pain and vasovagal attacks (13). Paracervical anaesthesia alone was reported to be inadequate for pain relief, and it was observed to have higher risk of bradycardia and hypotension (14). Systematic review and meta-analysis by Cooper et al. (1) comparing the different types of local anaesthetics in reducing pain in outpatient hysteroscopy have derived paracervical injection to be superior to other forms of local anaesthesia such as intracervical and transcervical blocks or topical analgesia.
As paracervical local anaesthesia is not a complete anaesthesia by itself for outpatient hysteroscopy, in our centre, it is a routine practice to give IV pentazocine and promethazine. Pentazocine causes increase in HR and hypertension; however, it also increases cardiac work and is known to cause myocardial infarction. It is also a respiratory depressant drug, which may not be suitable for outpatient procedures. Promethazine is a sedative and a good drug to counteract postnarcotic nausea.
The size of the hysteroscope has also been implicated in causing pain and discomfort during hysteroscopy. Studies have tried to correlate the size with patient comfort. De Angelis et al. (15) have tried using a mini hysteroscope (3.3 mm) compared to a conventional hysteroscope (5 mm). They observed that with the use of small hysteroscope, the occurrence of pelvic pain significantly decreased (p<0.05). A flexible hysteroscope of 3 mm has been well tolerated by most women (16). However, even with a flexible hysteroscope, women reported of barely tolerable to severe pain around 12.4% to 3.6% respectively (17). In this study, the surgical stimulation was kept constant by using a hysteroscope of 4 mm for all cases.
Bradycardia and hypotension, also mentioned as vasovagal attacks in some studies, is seen to occur in about 5% of patients undergoing hysteroscopy (3, 18). Rigid hysteroscopes have been implicated to be more responsible for vasovagal attacks (19). On the contrary, in another study, incidence of bradycardia was more with mini hysteroscope as compared to the traditional hysteroscope (15). In our study, we did not encounter bradycardia or hypotension requiring additional pharmacological intervention, and the lowest recorded HR and MAP were more in the control group as compared to those in the ketamine group (p<0.001).
We decided to give low-dose ketamine infusion in place of pentazocine and promethazine as ketamine has the inherent property of causing hypertension and tachycardia by the release of catecholamines. Ketamine is also a respiratory stimulant unlike opioids (20). Sub-anaesthetic doses of IV ketamine (0.3 mg kg−1 or less) have been shown to blunt central pain response with low incidence of mild psychomimetic symptoms. It has also been seen to reduce perioperative opioid consumption in a wide range of surgical procedures (21). All these properties make it a near ideal drug for outpatient hysteroscopy. Low-dose ketamine is defined as a bolus dose of less than 2 mg kg−1 when given intramuscularly or 1 mg kg−1 when administered via the IV route and ≤20 mcg kg−1 min−1 in continuous intravenous infusion. It is preferably used as an adjunct to local anaesthetics, opioids or other analgesic agents (4).
Use of ketamine IV bolus infusion of 0.2 mcg kg−1 followed by an infusion of 0.1 mg kg−1 h−1 till the end of surgery for open cholecystectomy resulted in effective analgesia in the first 6 h postoperatively as compared to normal saline infusion. They had reduced pain scores and reduced opioid requirements with the use of low-dose ketamine infusion (p=0.001) (22). Ketamine in sub-anaesthetic doses has been found useful in the management of intraoperative and postoperative pain in outpatient to major abdominal surgery as evidenced by the decrease in the consumption of opiates. To be effective, it needs to be administered throughout the operative procedure (23). In our study, the number of patients requiring opioids is significantly less in the ketamine group as compared to that in the control group receiving IV pentazocine and promethazine (p<0.001).
Ketamine is known for its inherent property to cause central nervous system (CNS) symptoms like delirium, disorientation and agitation. Different studies have given conflicting results concerning the occurrence of CNS symptoms with the use of sub-anaesthetic doses of ketamine. IV ketamine in the dose of 1 ug kg−1 min−1 both intraoperatively and postoperatively was responsible for less morphine consumption and has not to been associated with any CNS disturbances (24).The use of very low-dose ketamine infusion in patients already on narcotics did not offer much advantage after major spine surgery in terms of pain relief. CNS side effects were similar as compared to placebo (25).
A triple-blinded study on low-dose ketamine (0.25 mg kg−1 bolus followed by 0.125 mg kg−1 h−1), minimal dose ketamine (0.015 mg kg−1 h−1) and placebo (normal saline) resulted in similar pain scores in all the three groups. Delirium was highest in the low-dose ketamine group as compared to that in minimal dose ketamine and placebo (26). However, in this study, 75% of patients in the ketamine group had mild delirium, which resolved in a short time without any additional medication. All patient’s condition was evaluated after 2 h before discharging to their home. It was found satisfactory, and all the patients were accompanied with attendants.
In a retrospective review of patients receiving low-dose ketamine combined with opioid for various surgical procedures observed lower pain scores but was associated with more cardiovascular side effects such as hypertension, hypotension and respiratory depression (27). We did not encounter significant hemodynamic variations with the use of low-dose ketamine, and the MAP and HR were more in the range of baseline values.
We could not assess VAS score in ketamine group at 15 and 30 min as the patients were deeply sedated and did not respond to verbal commands. Thereafter, pain scores were comparable in both the groups at all other time points. The one of the reasons of not finding statistically significant difference in VAS score could be IV bolus of 15 mg pentazocine in the control group.
However, the number of patients requiring rescue analgesia was considerably higher in the control group as compared to that in the ketamine group. This can be explained by dissociative analgesic/sedative property of ketamine that also blunts central sensitisation. It resulted into less number of patients who needed rescue analgesia in the ketamine group. Nursing staff’s satisfaction was lower in the ketamine group mainly due to higher delirious state of patients requiring more care. Both the patient’s and surgeon’s satisfaction was significantly better in the low-dose ketamine group, thus making low-dose ketamine a safe agent for outpatient hysteroscopy.
Conclusion
We concluded that low-dose ketamine in day-care hysteroscopy is an effective and safe agent.
Main Points.
Ambulatory hysteroscopy is usually accompanied by pain and discomfort with bradycardia and hypotension.
We evaluated whether intravenous low dose Ketamine reduces the rate of pain and reduces the incidence of bradycardia and hypotension during hysteroscopy.
Ketamine group had less rescue analgesic requirement, less episodes of bradycardia and hypotension, more patient comfort and surgeon’s satisfaction score.
We concluded that low-dose ketamine is an efficient and safe agent in day care hysteroscopy.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of All India Institute of Medical Sciences (Ref. No. IEC-131/07.04.2017, RP-4/2017).
Informed Consent: Written informed consent was obtained from all patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - D.G., A.S., V.D.; Design - D.G., N.N., A.S.; Supervision - D.G., N.N., D.K.B.; Resources - M.A.; Materials - D.G., A.S.; Data Collection and/or Processing - D.G., N.N., V.D.; Analysis and/or Interpretation - D.G., A.S.; Literature Search - A.S.; Writing Manuscript - D.G., A.S.; Critical Review - D.G., D.K.B., M.A.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Cooper NA, Khan KS, Clark TJ. Local anaesthesia for pain control during outpatient hysteroscopy: systematic review and meta-analvsis. Br Med J. 2010;340:c1130. doi: 10.1136/bmj.c1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’Flynn H, Murphy LL, Ahmad G, Watson AJ. Pain relief in outpatient hysteroscopy: a survey of current UK clinical practice. Eur J Obstet Gynecol Reprod Biol. 2011;154:9–15. doi: 10.1016/j.ejogrb.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Teran-Alonso MJ, De Santiago J, Usandizaga R, Zapardiel I. Evaluation of pain in office hysteroscopy with prior analgesic medication: a prospective randomized study. Eur J Obstet Gynecol Reprod Biol. 2014;178:123–7. doi: 10.1016/j.ejogrb.2014.04.030. [DOI] [PubMed] [Google Scholar]
- 4.Schmid RL, Sandler AN, Katz J. Use and efficacy of low-dose ketamine in the management of acute postoperative pain: a review of current techniques and outcomes. Pain. 1999;82:111–25. doi: 10.1016/S0304-3959(99)00044-5. [DOI] [PubMed] [Google Scholar]
- 5.Vivas JP, Reyes E, Ríos F, Lozano R, Pérez JA, Plazas M. Measurement of satisfaction with anesthetic recovery in a high complexity postanesthetic care unit: a patient perspective. Colombian J Anesth. 2018;46:279–85. doi: 10.1097/CJ9.0000000000000070. [DOI] [Google Scholar]
- 6.Bellingham FR. Outpatient hysteroscopy--problems. Aust N Z J Obstet Gynaecol. 1997;37:202–5. doi: 10.1111/j.1479-828X.1997.tb02254.x. [DOI] [PubMed] [Google Scholar]
- 7.Readman E, Maher PJ. Pain relief and outpatient hysteroscopy: a literature review. J Am Assoc Gynecol Laparosc. 2004;11:315–9. doi: 10.1016/S1074-3804(05)60042-4. [DOI] [PubMed] [Google Scholar]
- 8.Kremer C, Barik S, Duffy S. Flexible outpatient hysteroscopy without anaesthesia:a safe, successful and well tolerated procedure. Br J Obstet Gynaecol. 1998;105:672–6. doi: 10.1111/j.1471-0528.1998.tb10185.x. [DOI] [PubMed] [Google Scholar]
- 9.Glasser MH. Practical tips for office hysteroscopy and second-generation “global” endometrial ablation. J Minim Invasive Gynecol. 2009;16:384–99. doi: 10.1016/j.jmig.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 10.Kaneshiro B, Grimes DA, Lopez LM. Pain management for tubal sterilization by hysteroscopy. Cochrane Database Syst Rev. 2012;15:CD009251. doi: 10.1111/j.1471-0528.1998.tb10185.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tangsiriwatthana T, Sangkomkamhang US, Lumbiganon P, Laopaiboon M. Paracervical local anaesthesia for cervical dilatation and uterine intervention. Cochrane Database Syst Rev. 2009;21:CD005056. doi: 10.1002/14651858.CD005056.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Cooper NA, Smith P, Khan KS, Clark TJ. Does cervical preparation before outpatient hysteroscopy reduce women’s pain experience? A systematic review. BJOG. 2011;118:1292–301. doi: 10.1111/j.1471-0528.2011.03046.x. [DOI] [PubMed] [Google Scholar]
- 13.Lau WC, Tam WH, Lo WK, Yuen PM. A randomised double-blind placebo-controlled trial of transcervical intrauterine local anaesthesiain outpatient hysteroscopy. BJOG. 2000;107:610–3. doi: 10.1111/j.1471-0528.2000.tb13301.x. [DOI] [PubMed] [Google Scholar]
- 14.Lau WC, Lo WK, Tam WH, Yuen PM. Paracervical anaesthesia in outpatient hysteroscopy: a randomised double-blind placebo-controlled trial. Br J Obstet Gynaecol. 1999;106:356–9. doi: 10.1111/j.1471-0528.1999.tb08274.x. [DOI] [PubMed] [Google Scholar]
- 15.De Angelis C, Santoro G, Re ME, Nofroni I. Office hysteroscopy and compliance: mini-hysteroscopy versus traditional hysteroscopy in a randomized trial. Hum Reprod. 2003;18:2441–5. doi: 10.1093/humrep/deg463. [DOI] [PubMed] [Google Scholar]
- 16.Glasser MH. Practical tips for office hysteroscopy and second-generation “global” endometrial ablation. J Minim Invasive Gynecol. 2009;16:384–99. doi: 10.1016/j.jmig.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Bradley LD, Widrich T. State-of-the-art flexible hysteroscopy for office gynecologic evaluation. J Am Assoc Gynecol Laparosc. 1995;2:263–7. doi: 10.1016/S1074-3804(05)80106-9. [DOI] [PubMed] [Google Scholar]
- 18.Ma T, Readman E, Hicks L, Porter J, Cameron M, Ellett L, et al. Is outpatient hysteroscopy the new gold standard? Results from an 11 year prospective observational study. Aust N Z J Obstet Gynaecol. 2017;57:74–80. doi: 10.1111/ajo.12560. [DOI] [PubMed] [Google Scholar]
- 19.Agostini A, Bretelle F, Ronda I, Roger V, Cravello L, Blanc B. Risk of vasovagal syndrome during outpatient hysteroscopy. J Am Assoc Gynecol Laparosc. 2004;11:245–7. doi: 10.1016/S1074-3804(05)60207-1. [DOI] [PubMed] [Google Scholar]
- 20.Eikermann M, Grosse-Sundrup M, Zaremba S, Henry ME, Bittner EA, Hoffmann U, et al. Ketamine activates breathing and abolishes the coupling between loss of consciousness and upper airway dilator muscle dysfunction. Anesthesiology. 2012;116:35–46. doi: 10.1097/ALN.0b013e31823d010a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gorlin AW, Rosenfeld DM, Ramakrishna H. Intravenous sub-anesthetic ketamine for perioperative analgesia. J Anaesthesiol Clin Pharmacol. 2016;32:160–7. doi: 10.4103/0970-9185.182085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaur S, Saroa R, Aggarwal S. Effect of intraoperative infusion of low-dose ketamine on management of postoperative analgesia. J Nat Sci Biol Med. 2015;6:378–82. doi: 10.4103/0976-9668.160012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Himmelseher S, Durieux ME. Ketamine for perioperative pain management. Anesthesiology. 2005;102:211–20. doi: 10.1097/00000542-200501000-00030. [DOI] [PubMed] [Google Scholar]
- 24.Hadi BA, Daas R, Zelko R. A randomized, controlled trial of a clinical pharmacist intervention in microdiscectomy surgery - Low dose intravenous ketamine as an adjunct to standard therapy. Saudi Pharm J. 2013;21:169–75. doi: 10.1016/j.jsps.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Subramaniam K, Akhouri V, Glazer PA, Rachlin J, Kunze L, Cronin M, et al. Intra- and postoperative very low dose intravenous ketamine infusion does not increase pain relief after major spine surgery in patients with preoperative narcotic analgesic intake. Pain Med. 2011;12:1276–83. doi: 10.1111/j.1526-4637.2011.01144.x. [DOI] [PubMed] [Google Scholar]
- 26.Bornemann-Cimenti H, Wejbora M, Michaeli K, Edler A, Sandner-Kiesling A. The effects of minimal-dose versus low-dose S-ketamine on opioid consumption, hyperalgesia, and postoperative delirium: a triple-blinded, randomized, active- and placebo-controlled clinical trial. Minerva Anest. 2016;82:1069–76. [PubMed] [Google Scholar]
- 27.Kator S, Correll DJ, Ou JY, Levinson R, Noronha GN, Adams CD. Assessment of low-dose i.v.ketamine infusions for adjunctive analgesia. Am J Health Syst Pharm. 2016;73(5 Suppl 1):S22–9. doi: 10.2146/ajhp150367. [DOI] [PubMed] [Google Scholar]


