Abstract
Background
In the context of a variable condition such as asthma, patient recognition of deteriorating control and knowing what prompt action to take is crucial. Yet, implementation of recommended self-management strategies remains poor.
Aim
To explore how patients with asthma and parents/carers of children with asthma develop and establish recommended self-management strategies for living with asthma, and how clinicians can best support the process.
Design and setting
A qualitative study in UK primary care.
Method
Patients with asthma and parents/carers of children with asthma from 10 general practices were purposively sampled (using age, sex, and duration of asthma) to participate in focus groups or interviews between May 2016 and August 2016. Participants’ experiences of health care, management of asthma, and views on supported self-management were explored. Interviews and focus group sessions were audio-recorded and transcribed verbatim. Iterative thematic analysis was conducted, guided by the research questions and drawing on habit theory in discussion with a multidisciplinary research team.
Results
A total of 49 participants (45 patients; 4 parents/carers) took part in 32 interviews and five focus groups. Of these, 11 reported using an action plan. Patients learnt how to self-manage over time, building knowledge from personal experience and other sources, such as the internet. Some regular actions, for example, taking medication, became habitual. Dealing with new or unexpected scenarios required reflective abilities, which may be supported by a tailored action plan.
Conclusion
Patients reported learning intuitively how to self-manage. Some regular actions became habitual; dealing with the unexpected required more reflective cognitive skills. In order to support implementation of optimal asthma self- management, clinicians should consider both these aspects of self-management and support, and educate patients proactively.
Keywords: asthma, habits, health planning, personalised asthma action plans, primary health care, self-management
INTRODUCTION
Asthma is a chronic respiratory disease affecting approximately 339 million people worldwide.1 Asthma disrupts the lives of individuals as poorly controlled symptoms lead to reduced quality of life, absence from work and school, and a substantial burden on healthcare provision. For example, 6.4 million primary care consultations and 93 000 hospital admissions occur annually in the UK.2 Evidence from 270 randomised controlled trials demonstrates that supported self-management for asthma can improve asthma control and reduce unscheduled care across a broad range of demographic, cultural, and healthcare contexts.3
Self-management is defined as:
‘… the tasks that individuals must undertake to live with one or more chronic conditions. These tasks include having the confidence to deal with medical management, role management, and emotional management of their conditions.’ 4
In the context of a variable condition such as asthma, recognising deteriorating control and knowing what prompt action to take is crucial and potentially life saving, as highlighted by the National Review of Asthma Deaths.5 Health professionals can support patients to self-manage in a number of ways: providing information about the condition and access to regular review; advising on how to monitor the disease course; and through the provision of a personal asthma action plan, which recommends when and how to adjust treatment and/or seek timely help during deterioration.6
Barriers to implementing supported asthma self-management operate at the organisational, professional, and patient level.7 For success, practices have to embrace supported self-management within their routines,8 and professionals need the appropriate skills.9 Though effective self-management interventions include provision of action plans as a core component3,10 they are poorly implemented in practice,11,12 and there is concern that professionals’ clinical focus on action plans does not match the advice patients want about ‘living with asthma’.13 As part of the IMPlementing IMProved Asthma self-management as Routine (IMP2ART) programme of work, the authors aimed to explore how patients and carers develop and establish their self-management strategies for living with asthma, and to understand how health professionals could best support the process. The authors’ interest specifically included, but was not limited to, understanding the role of an action plan from the perspective of individuals with asthma.
How this fits in
| Despite knowledge that supported self-management for asthma improves asthma control, and reduces visits to out-of-hours and accident and emergency departments, it remains poorly implemented. By improving understanding of how individual self-management strategies develop, the authors sought to identify ways to improve implementation of asthma self-management support in primary care. In the present study, patients learnt how to self-manage over time intuitively; some regular actions became habitual whereas dealing with the unexpected required more reflective cognitive skills. Patients may also be more receptive at diagnosis and following an asthma attack; therefore, clinicians should consider adapting their routines and offering support accordingly. |
METHOD
Semi-structured interviews and focus group sessions with individuals with asthma and parents/carers of children with asthma were undertaken between May 2016 and August 2016.
Sampling and recruitment
Participants from 10 general practices serving demographically diverse regions across the UK (Grampian, Kent, Lothian, and Yorkshire) were recruited. Participating practices identified patients aged ≥12 years or parents/carers of children aged 5–11 years with ‘active asthma’ on their practice database and invited a random sample (n = 100) of potential participants. ‘Active asthma’ was defined as a coded diagnosis of asthma and having had a prescription for asthma medication in the previous year.14 A clinician from the practice screened the list for eligibility. Patients were excluded if unable to give consent (for example, because of cognitive impairment, chronic obstructive pulmonary disease, or attending a clinic for severe/difficult asthma) or for significant clinical or social reasons (for example, being on a palliative register or recently bereaved).
Potential participants completed an expression-of-interest form that included questions regarding age, sex, duration of asthma, current treatment, asthma control, and whether they had, or used, an asthma action plan. Responses were used to purposively sample individuals with a range of demography, and experiences of asthma and self-management. The authors did not have access to electronic health records and relied on participant reporting of asthma action plan ownership. Participants received an information leaflet providing study details before data collection. Written informed consent was obtained before arranging an interview or focus group session, according to patient preference.
Data collection
Interviews were conducted face-to-face at local general practices or participants’ homes, with the option of a telephone interview available if preferred. Focus group sessions were conducted at the practice or community venue. Interviews and focus group sessions were conducted by one author: a researcher and clinician trained in qualitative methodology. Focus group sessions were supported by an additional researcher who took notes. Interviews and focus group sessions were audio-recorded and transcribed verbatim with anonymity preserved.
Topic guides
Topic guides were developed by the multidisciplinary research team (including qualitative researchers, GPs, a health psychologist, and individuals with asthma) and piloted with members of a patient and public involvement (PPI) group that provided feedback. Discussions elicited what patients understood by self-management, and explored existing self-management strategies employed by individuals and how these behaviours had evolved. Participants were subsequently shown an exemplar asthma action plan to assist those who had not previously received one. Experiences of health care and relationships with professionals were explored, and views on supported self-management, including barriers and ways of overcoming the barriers, were discussed.
Data analysis
An interpretive thematic approach to analysis was used15 guided by the research objectives of understanding how self-management strategies are developed by patients and carers, how they can be supported by health professionals, and specifically the role of action plans. Transcripts were read using NVivo (version 10) and initial thoughts were noted. After an initial tranche of interviews had been coded, four researchers, working independently, conducted thematic analysis with selected transcripts. Emerging themes were discussed with the wider research team and an initial coding framework agreed. The coding framework was reviewed and updated iteratively as more data were collected and analysed. The final coding framework represented a mix of themes that had been proposed in advance and combined with other themes that were generated during the analysis.15 The consolidated criteria for reporting qualitative research (COREQ) guided reporting.16
Interpretation
Data were approached from a realist perspective, allowing consideration of the motivations and meanings of participants’ experiences.15 To aid interpretation, findings were discussed with the multidisciplinary steering group, which included experienced qualitative and health services researchers, clinicians, and PPI colleagues. As themes emerged from the data, relevant theory, for example, habit theory, was used to guide interpretation of data where applicable.17
RESULTS
A total of 49 participants were recruited (45 patients; 4 parents/carers of patients). Of these, 32 completed individual interviews; 18 interviews were conducted face-to-face and 14 by telephone. Seventeen participants contributed to five focus groups. Interviews lasted 45–60 minutes and each focus group lasted 60–90 minutes. No participants withdrew and no repeat interviews were undertaken.
Participant characteristics are shown in Table 1. Female participants outnumbered males and young adults were under-represented (there were none at all in the 16–25 year age group). Two participants were of non-white ethnic backgrounds. Asthma control varied and only one-third of participants reported having an action plan.
Table 1.
Characteristics of participants (N = 49)
| Characteristics | Interviews, n (N = 32) | Focus groups, n (N = 17) |
|---|---|---|
| Sex, female (71.4%) | 22 | 13 |
|
| ||
| Age, years | ||
| <16 | 4 | 0 |
| 16–25 | 0 | 0 |
| 26–45 | 9 | 3 |
| 46–65 | 13 | 8 |
| >65 | 6 | 6 |
|
| ||
| Parent/carer | 4 | 0 |
|
| ||
| Non-white ethnic background | 2 | 0 |
|
| ||
| Asthma onset in adulthood | 18 | 12 |
|
| ||
| Asthma attack within the past year | 9 | 6 |
|
| ||
| Symptoms occurring less than every month | 12 | 8 |
|
| ||
| Reported using SABA regularly | 7 | 4 |
|
| ||
| Had never received a personal action plan | 21 | 11 |
|
| ||
| Owned a personal action plan and used it | 8 | 3 |
SABA = short-acting bronchodilator.
Participants’ understanding of self-management regarding their asthma
Several participants described self-management as ‘keeping on top’ of their asthma. Medical management, such as knowledge of the condition and treatment, was commonly discussed, for instance participant (P)14, who had symptoms from an early age but no diagnosis until her 40s, described self-management as:
‘Understanding what it is I have and how it can sort of manifest itself, what it’s like to have an attack and, most importantly, how to deal with it when I do.’
(P14, female [F], aged 46–65 years, adult-onset asthma)
Social and emotional aspects of self-management were less commonly described, though participant 18, who had experienced a life-threatening asthma attack, identified how for them self-management was both emotional and medical management:
‘I just kind of deal with it and get on with it and try not to let it fluster me or anybody else. Because it’s like I can feel internally when things are … when it’s getting worse, I just go on to medication so I just kind of live with it and get on with it.’
(P18, male [M], aged 46–65 years, adult-onset asthma)
Participants who learnt how to self-manage their asthma over time
Many participants described how they had learnt to self-manage asthma over time. The experience of living with asthma led to a better understanding of how to manage the condition:
‘I’ve had enough experience of it all and over a long enough period that I feel I kind of have sort of internalised it all and memorised it all.’
(P14, F, aged 46–65 years, adult-onset asthma)
As time went by and experience of asthma grew, individuals mentioned different sources of information and advice, though for many the lived experience was most important. Participant 30, who described himself as ‘probably not the best asthmatic in the world’, was frustrated by the impact asthma had on his exercise ability. He found the advice from health professionals to be of limited value and had learnt most from experience:
‘From years of coping and living with it, it sort of becomes second nature … I know how far I can push it before I need to stop and take my inhaler … it’s just instinct now.’
(P30, M, aged 26–45 years, childhood-onset asthma)
This was echoed by others who were ‘conscious of what sets it [asthma] off’ (P21, focus group [FG]3, F, aged 46–65 years, adult-onset asthma) and had learnt to recognise and avoid triggers. Participant 6 described how her asthma ‘increased its severity ridiculously’ after a change in location, requiring several hospital admissions. She explained how she had subsequently achieved better control:
‘I think it’s living with it, I think it’s one of those things you get used to your personal triggers … you’ll go into environments and you think, “oh, I’m not going to cope with this” or you won’t put yourself in an environment where it might trigger something. Or you’ll make sure that your inhalers are next to you, just in case.’
(P6, FG2, F, aged 26–45 years, childhood-onset asthma)
Participant factors that influenced self-management
Developing asthma self-management skills over time was influenced by a range of patient factors. Age was an important factor. For example, participant 19 described the challenges of self-managing medication experienced by her teenage child:
‘Being the average teenage boy, he forgets things. I’ve lost count of the number of times he left his inhaler behind … he used to have at least six inhalers, in various different locations to prevent him from forgetting it … One in the PE bag, one in the car glove box, one in the kitchen, one in his bedroom, one in his schoolbag, etc., it wasn’t a problem I ever had.’
(P19, F, aged 46–65 years, early-onset asthma)
Other individual circumstances, including comorbidities, social, or family considerations, also impacted how individuals self-managed. One participant described how living with multiple health conditions had made it difficult to prioritise her asthma:
‘To get my asthma under control would be amazing … I think the fact that I have other health issues, it seems to be a case of juggling, trying to keep on top of things, and that can be hard.’
(P1, F, aged 46–65 years, adult-onset asthma)
Self-management behaviours also differed according to severity of symptoms and the individual’s perceived sense of control shaped by previous experience. Some participants felt very able to manage their asthma and able to deal with most eventualities. Others were less confident and chose to seek professional advice after small changes in asthma control. The self-management strategies of participant 62 were strongly influenced by a past hospital admission for a respiratory illness:
‘At the minute any slight wheeze or a cough or I start sneezing, that’s it, I’m there [the GP] because I got such a scare last year … I think I’m probably a bit less confident because I look back to last year and I think could I have done anything differently?’
(P62, F, aged 46–65 years, adult-onset asthma)
Others were more confident to self-manage a change in symptoms though still had a point at which they would seek help. For example, participant 11, who had experienced no recent asthma attacks, explained what she did if her asthma worsened:
‘It just tends to really be to double the inhaler and if it doesn’t start shifting then go and see the doctor.’
(P11, F, aged >65 years, childhood-onset asthma)
Healthcare factors that influenced self-management
The relationship with health professionals, principally from primary care, was a regular feature for each participant, though the strength of influence varied. Participant 40, a schoolteacher who had lived with asthma since childhood, felt they ‘learnt the hard way’, relating a history of requiring rescue steroid tablets to regain asthma control. With time, her experiences, supported by professional advice, helped her to limit attack frequency:
‘As I’ve become older, I’ve become more aware of the triggers that might cause an attack. Through the help from doctors and asthma nurses and things I became a bit more aware.’
(P40, F, aged 26–45 years, childhood-onset asthma)
Similarly, this interaction between experience and professional support helped participant 28 to feel confident in managing her asthma:
‘It’s taken a long time through trial and error and talking and ringing and being ill and getting better and having different people give you information at different times. And you’ve just got to gradually build up this font of knowledge.’
(P28, F, aged 46–65 years, adult-onset asthma)
Self-management strategies at a given point in time
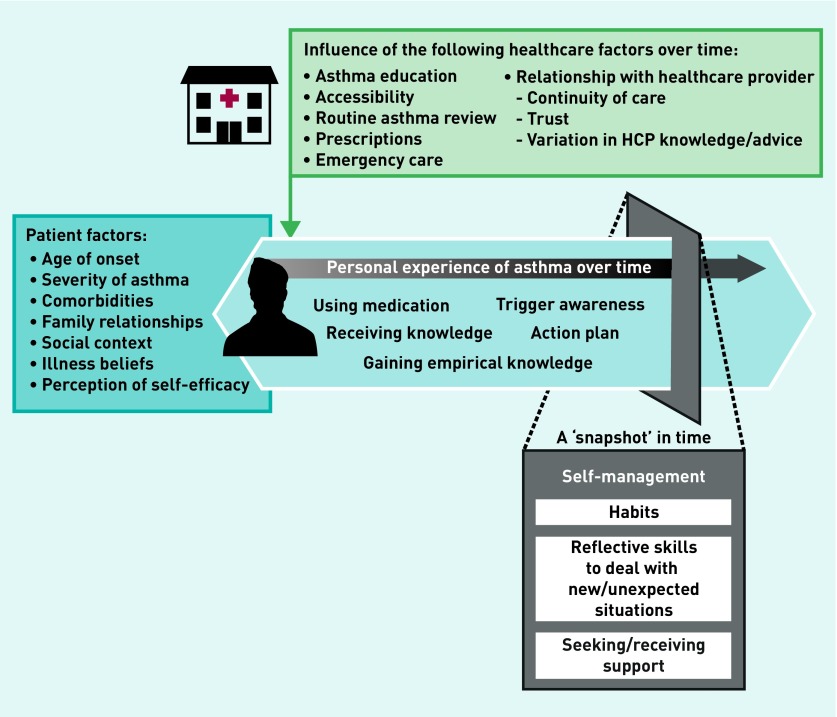
Figure 1 illustrates how self-management behaviours and skills develop over time. The evolution of self-management skills, influenced by patient and healthcare factors, are illustrated in the schema and described in the following sections.
Figure 1.
Schema illustrating how self-management behaviours and skills may develop.
The personal experience of asthma is commonly built up over time, shaped by individual-related factors and healthcare support. At any given time, an individual can draw on different skills to self-manage effectively, which can be thought of as automated actions (or ‘habits’), and other reflective skills required to process new or uncommon situations. HCP = healthcare professional.
A ‘snapshot’ in time distinguishes self-management strategies that have become habits from the reflective cognitive strategies that may influence response to less predictable and unexpected events.
Repeated actions form habits
Some participants described how aspects of self-management had become ‘habits’. For instance, the parents of a child aged between 5–11 years who had frequent symptoms and a recent asthma attack said:
‘Both my husband and I have grown up having our parents taking inhalers every day. And it almost becomes like brushing your teeth every morning, it’s just one of those things we know she has to do to prevent the asthma attack. Eventually repetition has just made it easier for us.’
(P48, parent of a child aged between 5–11 years)
Despite having achieved good asthma control by avoiding dust (‘I’m careful when I’m around dust, emptying a vacuum cleaner bag, things like that’), participant 21 continued to keep an inhaler available as a programmed part of her self-management:
‘I’ve not used my inhaler for, it must be, about 8 years now but I always keep one just in case it strikes.’
(P21, FG3, F, aged 46–65 years, adult-onset asthma)
Not everyone had developed helpful habits:
‘I don’t always take it [the inhaler] twice in the morning and twice in the evening. And it’s not until it catches up with me during the day that I then think “well, maybe I should start taking it like I’m supposed to” so I do.’
(P30, M, aged 26–45 years, childhood-onset asthma)
‘I dinnae take my inhalers. Maybe if I did take them, I maybe would find there is a difference but it’s just getting into that habit.’
(P47, F, aged >65 years, adult-onset asthma)
Cognitive management to deal with new or unexpected situations
Dealing with new or unexpected situations, for example, a deterioration in asthma control, required reflective abilities that could be put into action when needed.
When describing an action plan, participant 12, a retired nurse, said:
‘You would be in a panic, but I think to have something in front of you to say “this is what’s happening to me, I need to do it now”.’
(P12, F, aged >65 years, adult-onset asthma)
Participant 36, who did not have an action plan, commented:
‘… in the event of an asthma attack it [personal asthma action plan] gives you a nice flowchart, so you don’t immediately ring 999 and waste their time. You can see there are other things and, you know, maybe it might just calm you a bit and take you through it.’
(P36, F, aged 46–65 years, adult-onset asthma)
Matching support to evolving behaviours and skills
Several participants identified the limitation of routine reviews, highlighting the advantage of consultations when symptoms meant asthma was ‘fresh in your mind’. One participant, participant 45, explained that he would be more receptive to support when he was struggling:
‘If you get the letter perhaps when you’ve got a chest infection and you’re feeling all sorry for yourself, perhaps you would think “hmm, it might be a good thing to actually go and get this reviewed” but when you’re feeling absolutely fine you just don’t do it.’
(P45, M, aged 46–65 years, childhood-onset asthma)
Other participants felt that receiving good self-management support around the time of diagnosis was most useful:
‘We also said it [receiving information] should always start sooner, you know, that the valuable time is probably the first 3 months after you’ve been diagnosed.’
(P23, FG3, M, aged 46–65 years, adult-onset asthma)
Participant 13, diagnosed with asthma as a young adult, ‘felt quite confident’ in his ability to self-manage because he had been given the information and explanation that he needed at the time of diagnosis:
‘I would say that she [the nurse] actually gave me the information that I needed, telling me that I can train and be a very good athlete but it will have a negative effect further on my life if I wouldn’t be taking the medication. And also explaining to me how to actually take the medication, based on which inhaler it would be.’
(P13, M, aged 26–45 years, adult-onset asthma).
DISCUSSION
Summary
In this qualitative study, participants described developing self-management skills and strategies over time through a mixture of experiential learning and receiving information from others, including health professionals. Individuals described some self-management behaviours becoming like a ‘habit’, while other situations, notably new or unexpected events, required more cognitive decision making that could be supported by an action plan.
Individuals require different skills and strategies to self-manage effectively. Some regular actions become automatic; influencing these self-management behaviours may be best achieved at ‘windows of opportunity’ at diagnosis and after an asthma attack. Dealing with new or unexpected scenarios requires reflective abilities; accessing a tailored action plan at these times may be particularly helpful. To implement optimal asthma self-management, clinicians should consider these varied aspects of self-management and adapt their routines and support accordingly.
Strengths and limitations
A strength of this study was the broad sample of participants recruited from different backgrounds across 10 different practices from four UK regions. Males, young adults, parents of children with asthma aged 5–11 years, and individuals from black and minority ethnic backgrounds were under-represented, resulting in fewer viewpoints from those in harder-to-reach groups. Resources were not available to allow participants to comment on transcripts, though involving PPI colleagues in discussions ensured a patient perspective throughout.
Researchers’ attitudes influenced design, data collection, and analysis. Having primary care experience enabled the interviewing author to bring an in-depth understanding of the challenges of implementing asthma self-management to the interviews, which helped knowledgeable and holistic enquiry; however, the interviewer’s background interests and assumptions may have meant that some patient suggestions were not fully expanded upon, for example, if a suggestion was felt to be impractical in the context of primary care. Having close support and weekly meetings enabled balanced interpretation from the multidisciplinary research team.
A thematic analysis was conducted as planned and identified common ideas across the interviews and focus group sessions. How participants self-managed asthma and learnt new skills over time were well described to the extent that the authors felt data saturation had been achieved on these themes. Patient and practice factors that influenced self-management were also well covered, though these topics are potentially very broad and some relevant suggestions may have been missed.
The common-sense model and habit theories were introduced in response to emerging themes and were not used to develop the topic guides; therefore, some aspects of these concepts may not have been explored.18 The authors acknowledge that the behaviours identified in this study may not meet the health psychology definitions of ‘habit’. Nonetheless, habit formation has been demonstrated as beneficial in recognising and addressing behaviour change in long-term conditions,9 and was found to be a useful theory to help interpret the present findings and offer practical implications for how to optimise the delivery of supported self-management.
Comparison with existing literature
The common-sense model of self-regulation outlines the processes that influence individuals’ behaviours when coping with chronic illness.20–22 The participants in the present study described a process of learning to self-manage asthma over time that resonates with this framework. Individuals with asthma characterise their illness based on their own understanding of disease and test coping behaviours in a process of ‘self-regulation’.
Though the common-sense model of self-regulation describes how individuals initiate coping behaviours for their chronic condition, it offers less insight into how coping behaviours are maintained.23 Participants in the present study talked about certain self-management behaviours becoming a ‘habit’. In lay discourse, ‘habit’ is understood as a frequently completed behaviour,24 yet, ‘habits’ are not just frequently completed, but also crucially initiated automatically and associated with a ‘context cue’.25 Once formed, a habit is likely to be automatically triggered when the context cue is encountered.
Though habits are initially formed with the intention of achieving a goal, as habits intensify, the association between the intended goal and the habitual behaviour reduces, meaning that individuals perform behaviours independently of their intended goals.19
Interpreting asthma self-management using habit theory offers two valuable insights, which may inform professionals seeking to support participants in establishing good self-management, develop good, healthy ‘habits’, and break bad, unhelpful ‘habits’.
Helping patients develop good habits
Supporting individuals to develop healthy ‘habits’ has been described as (relatively) straightforward for health professionals and easy for patients to adopt;19 the self-management behaviour should be repeated in the same context until it becomes automatic.19,26 Patients should choose both the behaviour they wish to adopt and the context in which they will perform the behaviour, for example, an event like brushing teeth.19 In the context of asthma self-management, ideally the behaviour is chosen following shared decision making, with the health professional offering their expertise on the best (medical) strategies for self-management.
Self-management behaviours develop over time, with key opportunities to help individuals to develop healthy self-management habits. Potentially the most valuable time is at the point of diagnosis, when an individual is at the beginning of understanding their illness, and self-management behaviours are yet to be developed. This aligns with the British Thoracic Society/Scottish Intercollegiate Guidelines Network asthma guideline, which emphasises the importance of delivering supported self-management, not just medication, at the point of an asthma diagnosis.10 The provision of an action plan jointly completed before establishing regular medication and tailored to the individual’s situation can be used to promote habit formation by encouraging the development of intentions with behaviour.27
Supporting patients to break unhelpful habits
Habit theory helps to understand how unhelpful or ineffective self-management strategies can be identified and influenced. Overuse of a short-acting bronchodilator (SABA) inhaler is a common example of an ineffective asthma self-management behaviour and is a marker of poor asthma control.5 Identifying SABA overuse and suggesting an alternative strategy (regular use of an inhaled corticosteroid) is recommended;10,28 however, breaking the ‘SABA habit’ requires different strategies for developing new habits.19,26 For example, strategies offering advice in how (not just why) to change habitual behaviour19 and avoiding contextual cues that trigger a ‘bad’ habit are widely recommended,26,29 but the success of these approaches in the context of SABA use will require further research. The importance of training healthcare professionals to use behaviour change techniques has already been demonstrated;9 data from the present study suggest that these skills will need to encompass addressing unhelpful habits.
The role of action plans
Recommended self-management relies not only on maintaining regular behaviours but also the ability to monitor change and respond with reflective actions, which can be aided by a personalised asthma action plan. Yet, action plans do not always resonate with individuals who have asthma13 and the realisation that some self-management behaviours become habitual may help understand why. In the present study, it was at the point of an asthma attack, which for many was an uncommon and often unexpected event, that there was value in written advice that could be consulted when needed. An action plan could act as a decision-making aid in a time of crisis but should be tailored to individuals’ circumstances and preferences. Some of the participants in the present study were confident to increase medication and monitor the situation, but others described seeking help from a health professional at the first sign of worsening symptoms.
Implications for research and practice
Two timepoints emerged as moments when self-management support should be prioritised: the point of diagnosis and after an asthma attack. First, self-management education (with an action plan) has value early after diagnosis as coping strategies are beginning to form. The present findings suggest that health professionals should endeavour to ‘get in early’ by providing high-quality, patient-centred education and help shape habits from the outset. This approach resonates with the structured education programmes provided for patients newly diagnosed with diabetes, though recent reviews have highlighted the need for ongoing support accessible throughout the diabetes journey.30 Second, a worsening of asthma control could represent a ‘window of opportunity’ when an individual may be more receptive to advice and self-management support.26,29 A post-attack follow-up review, as widely recommended,5,10,28 offers a chance to review behaviours and potentially help patients break ineffective self-management ‘habits’ and promote new strategies.
Improving the provision of self-management support within healthcare settings requires organisational strategies that fit with existing practice routines.8 Scheduling time for education and self-management support when a diagnosis is first made and having strategies in place to ensure follow-up after unscheduled consultations, in addition to annual reviews, could improve timely provision of action plans and warrants further research. Digital options for monitoring asthma and patient-accessible sections of the electronic health record may offer solutions for greater sharing and accessibility.8 Policymakers and NHS managers can support this by considering how to promote or incentivise comprehensive self-management support at specific timepoints, with consistent messages delivered by all members of the healthcare team.
Acknowledgments
The authors would like to thank the wider IMPlementing IMProved Asthma self-management as Routine (IMP2ART) team for their support and advice during the project: Audrey Buelo, Nicola McCleary, Brian McKinstry, and Aziz Sheikh, University of Edinburgh; Sandra Eldridge, Chris Griffiths, and Chris Newby, Queen Mary University of London; Neil Wright, University of Oxford; Anne-Louise Caress, University of Manchester; Elisabeth Ehrlich, Asthma UK Centre for Applied Research; Bethan Haskins, Canterbury and Coastal Clinical Commissioning Group; Rob Horne, University College London; Steven Julious, University of Sheffield; Lorna McKee, University of Aberdeen; Amanda Andrews and Monica Fletcher, Education for Health; Ceri Phillips and Deborah Fitzsimmons, University of Swansea; Francis Appiagyei, Tanith Hjelmbjerg, David Price, Dermot Ryan, Derek Skinner, and Erica Vince-Lawer, Optimum Patient Care. The authors are grateful to Lesley Gardner and Rosemary Porteous for transcribing the audio recordings and Dawn Cattanach for refining the schema graphic.
Funding
This research was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care North Thames at Bart’s Health NHS Trust (NIHR CLAHRC North Thames) (grant ref: RP-DG-1213-10008). The views expressed in this article are those of the author(s) and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care. Luke Daines was supported by an academic clinical fellowship from the Scottish School of Primary Care.
Ethical approval
This study received ethical approval from South Central — Berkshire Research Ethics Committee (ref: 16/SC/0024) and was conducted in accordance with NHS Lothian research management approval (ref: 2016/0031).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
Hilary Pinnock and Luke Daines are on the British Thoracic Society/Scottish Intelligence Guidelines Network (SIGN) asthma guideline development committee and Hilary Pinnock has led work on supported self-management in the 2016 update of the guideline.
Discuss this article
Contribute and read comments about this article:
REFERENCES
- 1.Global Asthma Network The global asthma report. 2018 http://www.globalasthmareport.org/Global%20Asthma%20Report%202018.pdf (accessed 3 Mar 2020). [Google Scholar]
- 2.Mukherjee M, Stoddart A, Gupta RP, et al. The epidemiology, healthcare and societal burden and costs of asthma in the UK and its member nations: analyses of standalone and linked national databases. BMC Med. 2016;14(1):113. doi: 10.1186/s12916-016-0657-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pinnock H, Parke HL, Panagioti M, et al. Systematic meta-review of supported self-management for asthma: a healthcare perspective. BMC Med. 2017;15(1):64. doi: 10.1186/s12916-017-0823-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adams K, Greiner AC, Corrigan JM, editors. The 1st annual Crossing the Quality Chasm Summit: a focus on communities. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 5.Levy M, Andrews R, Buckingham R, et al. Why asthma still kills The National Review of Asthma Deaths (NRAD) 2014 https://www.rcplondon.ac.uk/sites/default/files/why-asthma-still-kills-full-report.pdf (accessed 3 Mar 2020).
- 6.Pearce G, Parke HL, Pinnock H, et al. The PRISMS taxonomy of self-management support: derivation of a novel taxonomy and initial testing of its utility. J Health Serv Res Policy. 2016;21(2):73–82. doi: 10.1177/1355819615602725. [DOI] [PubMed] [Google Scholar]
- 7.Pinnock H, Epiphaniou E, Pearce G, et al. Implementing supported self-management for asthma: a systematic review and suggested hierarchy of evidence of implementation studies. BMC Med. 2015;13:127. doi: 10.1186/s12916-015-0361-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morrow S, Daines L, Wiener-Ogilvie S, et al. Exploring the perspectives of clinical professionals and support staff on implementing supported self-management for asthma in UK general practice: an IMP2ART qualitative study. NPJ Prim Care Respir Med. 2017;27(1):45. doi: 10.1038/s41533-017-0041-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCleary N, Andrews A, Buelo A, et al. IMP2ART systematic review of education for healthcare professionals implementing supported self-management for asthma. NPJ Prim Care Respir Med. 2018;28(1):42. doi: 10.1038/s41533-018-0108-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scottish Intercollegiate Guidelines Network, British Thoracic Society SIGN 158 British guideline on the management of asthma A national clinical guideline. 2019 https://www.sign.ac.uk/assets/sign158.pdf (accessed 3 Mar 2020).
- 11.Wiener-Ogilvie S, Pinnock H, Huby G, et al. Do practices comply with key recommendations of the British Asthma Guideline? If not, why not? Prim Care Respir J. 2007;16(6):369–377. doi: 10.3132/pcrj.2007.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gagné ME, Boulet LP. Implementation of asthma clinical practice guidelines in primary care: a cross-sectional study based on the Knowledge-to-Action Cycle. J Asthma. 2018;55(3):310–317. doi: 10.1080/02770903.2017.1323919. [DOI] [PubMed] [Google Scholar]
- 13.Ring N, Jepson R, Hoskins G, et al. Understanding what helps or hinders asthma action plan use: a systematic review and synthesis of the qualitative literature. Patient Educ Couns. 2011;85(2):e131–e143. doi: 10.1016/j.pec.2011.01.025. [DOI] [PubMed] [Google Scholar]
- 14.NHS England 2019/20 General Medical Services (GMS) contract: guidance and audit requirements for GMS contract. 2019 https://www.england.nhs.uk/publication/2019-20-general-medical-services-gms-contract-quality-and-outcomes-framework-qof (accessed 3 Mar 2020).
- 15.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 16.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 17.Reeves S, Albert M, Kuper A, Hodges BD. Why use theories in qualitative research? BMJ. 2008;337:a949. doi: 10.1136/bmj.a949. [DOI] [PubMed] [Google Scholar]
- 18.Daly J, Willis K, Small R, et al. A hierarchy of evidence for assessing qualitative health research. J Clin Epidemiol. 2007;60(1):43–49. doi: 10.1016/j.jclinepi.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 19.Gardner B, Lally P, Wardle J. Making health habitual: the psychology of ‘habit-formation’ and general practice. Br J Gen Pract. 2012 doi: 10.3399/bjgp12X659466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leventhal H, Leventhal EA, Contrada RJ. Self-regulation, health, and behavior: a perceptual-cognitive approach. Psychol Health. 1998;13(4):717–733. [Google Scholar]
- 21.Leventhal H, Brissette I, Leventhal E. The common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behaviour. Abingdon: Routledge; 2003. pp. 42–65. [Google Scholar]
- 22.Brownlee S, Leventhal H, Leventhal EA. Regulation, self-regulation, and construction of the self in the maintenance of physical health. In: Boekaerts M, Pintrich PR, Zeidner M, editors. Handbook of self-regulation. Cambridge, MA: Academic Press; 2000. pp. 369–416. [Google Scholar]
- 23.Leventhal H, Phillips LA, Burns E. The Common-Sense Model of Self-Regulation (CSM): a dynamic framework for understanding illness self-management. J Behav Med. 2016;39(6):935–946. doi: 10.1007/s10865-016-9782-2. [DOI] [PubMed] [Google Scholar]
- 24.Gardner B. Habit as automaticity, not frequency. Eur Health Psychol. 2012;14(2):32–36. [Google Scholar]
- 25.Gardner B. A review and analysis of the use of ‘habit’ in understanding, predicting and influencing health-related behaviour. Health Psychol Rev. 2015;9(3):277–295. doi: 10.1080/17437199.2013.876238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lally P, Gardner B. Promoting habit formation. Health Psychol Rev. 2013;7(Suppl 1):S137–S158. [Google Scholar]
- 27.Sniehotta FF. Towards a theory of intentional behaviour change: plans, planning, and self-regulation. Br J Health Psychol. 2009;14(Pt 2):261–273. doi: 10.1348/135910708X389042. [DOI] [PubMed] [Google Scholar]
- 28.Global Initiative for Asthma Global strategy for asthma management and prevention. 2019 Updated 2019. https://ginasthma.org/wp-content/uploads/2019/06/GINA-2019-main-report-June-2019-wms.pdf (accessed 3 Mar 2020).
- 29.Verplanken B, Wood W. Interventions to break and create consumer habits. J Public Policy Mark. 2006;25(1):90–103. [Google Scholar]
- 30.Captieux M, Pearce G, Parke HL, et al. Supported self-management for people with type 2 diabetes: a meta-review of quantitative systematic reviews. BMJ Open. 2018;8(12):e024262. doi: 10.1136/bmjopen-2018-024262. [DOI] [PMC free article] [PubMed] [Google Scholar]