Abstract
Background:
The optimal noninvasive test (NIT) for patients with diabetes and stable symptoms of coronary artery disease (CAD) is unknown.
Objective:
To assess whether a diagnostic strategy based on coronary computed tomographic angiography (CTA) is superior to functional stress testing in reducing adverse cardiovascular (CV) outcomes (CV death or myocardial infarction [MI]) among symptomatic patients with diabetes.
Methods:
The Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE; NCT01174550) was a randomized trial evaluating an initial strategy of CTA versus functional testing in stable outpatients with symptoms suggestive of CAD. We compared CV outcomes in patients with diabetes (n=1,908 [21%]) and without diabetes (n=7,058 [79%]) based on their randomization to CTA or functional testing.
Results:
Patients with diabetes (vs. without) were similar in age (median 61 vs. 60 years) and sex (female 54% vs. 52%) but had a greater burden of CV comorbidities. Patients with diabetes who underwent CTA had a lower risk of CV death/MI, compared to functional stress testing (CTA, 1.1% [10/936] vs. stress testing, 2.6% [25/972]; adjusted hazard ratio [aHR] 0.38, 95% CI 0.18–0.79; p=0.01). There was no significant difference in non-diabetics (CTA, 1.4% [50/3,564] vs. stress testing, 1.3% [45/3,494]; aHR 1.03, 95% CI 0.69–1.54, p=0.887; interaction term for diabetes p-value=0.02).
Conclusions:
In diabetics presenting with stable chest pain, a CTA strategy resulted in fewer adverse CV outcomes than a functional testing strategy. CTA may be considered as the initial diagnostic strategy in this subgroup.
Keywords: diabetes, coronary computed tomographic angiography, cardiovascular outcomes, stress testing, chest pain
Condensed abstract
The optimal noninvasive test (NIT) for patients with diabetes and stable symptoms of coronary artery disease (CAD) is unknown. We compared CV outcomes in patients with diabetes (n=1,908 [21%]) and without diabetes (n=7,058 [79%]) based on their randomization to CTA or functional testing in the PROMISE trial. In patients with diabetes, a CTA strategy resulted in a lower risk of CV death/MI than functional testing (adjusted HR 0.38, 95% CI 0.18–0.79; p=0.01). This result was not seen in patients without diabetes. CTA may be considered as the initial diagnostic strategy among stable patients with diabetes and symptoms suggestive of CAD.
Introduction
In the United States, over 29 million adults have a diagnosis of diabetes, and diabetes is an established cardiovascular (CV) risk factor (1). However, while CV disease is one of the leading causes of death and disability among patients with diabetes (2,3), evaluation of noninvasive testing (NIT) strategies to reduce CV outcomes in asymptomatic patients has not shown significant benefit from any particular NIT strategy. Among asymptomatic patients with type 1 or 2 diabetes, a strategy of screening for coronary artery disease (CAD) with coronary computed tomographic angiography (CTA) or nuclear testing versus standard of care increased subsequent processes of care (including referral to invasive coronary angiography [ICA] and revascularization) but failed to reduce CV outcomes (4,5).
To date, despite the higher prevalence and risk of CAD in patients with diabetes, there is limited evidence to guide clinicians in choosing among available NIT options. In light of these considerations, we felt that this was a clinically important subgroup to assess as the overall positive or negative results had the potential to obscure opposite findings in this important subgroup. Specifically, it is unknown whether an anatomic approach of evaluating symptoms suggestive of CAD using CTA is superior to functional stress testing in altering processes of care or reducing the risk of adverse CV outcomes. To address these knowledge gaps, we used contemporary data from the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE), a randomized trial of diagnostic evaluation strategy in stable outpatients with symptoms suggestive of CAD (6,7). We assessed symptomatic patients with and without diabetes to evaluate (a) the differences in processes of care including referral to ICA and use of CV preventative therapies following NIT; (b) differences in the risk of CV outcomes; and (c) whether the risk of CV outcomes in patients with and without diabetes is different in CTA versus functional stress testing.
Methods
Patient population
The methods and results of the PROMISE trial have been previously described (6,7). In brief, 10,003 symptomatic stable outpatients (2,144 patients with diabetes [21%] and 7,858 without diabetes [79%]) without a history of CAD were randomized to initial anatomical testing with 64-slice multi-detector CTA or functional testing of the local physician’s choice (exercise electrocardiogram [ECG], stress nuclear imaging, or stress echocardiogram). Overall, there were 8,966 patients tested as randomized with an interpretable NIT result (1,908 [21%] with diabetes and 7,058 [79%] without diabetes). For the present analysis, the population of patients with an interpretable NIT result was used. A history of diabetes was based on patient- and site-identified history of diabetes or use of anti-hyperglycemic medications.
Baseline variable and data collection
Baseline patient data on demographics, risk factor profiles, ECG findings, symptoms, and CAD risk estimates were collected for all patients. Calculation of the Framingham and Atherosclerotic Cardiovascular Disease Score (ASCVD) scores have been described previously (8,9). Test results according to site interpretation were recorded for the first NIT performed. In keeping with the pragmatic study design of the PROMISE trial, the test findings are based on site-based interpretation of the noninvasive and CTA test results.
Statistical analysis
Baseline characteristics were summarized using median (25th, 75th percentiles) for continuous variables and frequencies/percentages for categorical variables. Comparisons of patients with diabetes who were randomized to CTA versus a functional stress test were performed using the Wilcoxon rank sum test for continuous variables and chi-square test for categorical variables at a significance level of 0.05 (a similar process was conducted for patients without diabetes). Logistic regression models were used to assess the likelihood of test positivity between patients with and without diabetes. These models adjusted for NIT modality, age, and sex.
Processes of care following NIT include referral to ICA 90 days after randomization, referral to revascularization within 30 days of ICA, and medication prescription prior to or on a 60-day visit. The medications of interest included aspirin, statin, beta-blockers, and angiotensin-converting enzyme inhibitor (ACEi) or angiotensin receptor blockers (ARB).
Logistic regression models were used to compare the likelihood of each process of care between (a) patients with and without diabetes; (b) patients with diabetes randomized to CTA versus functional stress testing; and (c) patients without diabetes randomized to CTA versus functional stress testing. The association between diabetic status and ICA referral was adjusted for age, sex, and NIT result (positive/negative); the association of diabetic status and revascularization was adjusted for age, sex, and ICA result (positive/negative); and the association between diabetic history and 60-day medication prescription was adjusted for age, sex, and NIT modality. The modifying effect of diabetic status on the relationship between randomized testing strategy and each process of care was also assessed via logistic regression models that included the appropriate two-way interaction terms.
The clinical outcomes of interest included time to death/MI/unstable angina hospitalization (UAH) and CV death/MI. The relationships between diabetes history and these outcomes were assessed using Cox regression models and were adjusted for NIT modality, NIT results (positive/negative), ICA results (positive/negative/not tested, time-dependent), revascularization (time-dependent), age (time-dependent), and sex. Cox regression models were also used to evaluate the relationship between CTA versus functional stress testing by diabetic status and adjusted for NIT results (positive/negative), ICA results (positive/negative/not tested, time-dependent), revascularization (time-dependent), age (time-dependent), and sex. In addition, we conducted additional analyses to assess whether the association between disease severity (severely abnormal, moderately abnormal, mildly abnormal, and normal) and adverse events was jointly modified by initial testing modality (anatomical vs. functional) and diabetes history (yes vs. no) using Cox regression models.
We define lost to follow-up with respect to the primary outcome for this secondary analysis (death/MI/UAH) as not experiencing any component of the composite and having less than 12 months of follow-up. Overall, 1010/8966 (11%) of patients in our analysis cohort were lost to follow-up, 613/4466 (14%) of stress test patients were lost to follow-up, and 397/4500 (9%) of CTA patients were lost to follow-up; 766/7058 (11%) of patients without diabetes were lost to follow-up, and 244/1908 (13%) of patients with diabetes were lost to follow-up.
All statistical calculations were conducted using SAS 9.4 (SAS Institute, Inc., Cary, North Carolina).
Results
Baseline demographics
Patients with diabetes (n=2,144) compared to patients without diabetes (n=7,858) had similar ages and sex but a greater likelihood of having CV risk factors including hypertension, dyslipidemia, depression, and an increased body mass index (Online Table 1). The baseline characteristics between patients with diabetes who were randomized to CTA (n=936) versus functional stress testing (n=972) were well balanced (Table 1) including age, sex, and cardiac risk factors (p-value >0.05 for all). In patients without diabetes who were randomized to CTA (n=3,564) versus functional stress testing (n=3,494) (Table 1), there was a slight but statistically significant difference in age (median age 59.3 years CTA vs. 60.3 years functional stress testing; p<0.001) and racial distribution (p=0.002). Differences in the distribution of stress method among patients in the functional stress testing arm is presented in Online Table 2.
Table 1:
Patient characteristics at baseline by randomized testing modality and history of diabetes
| Diabetes(N=1908) | No Diabetes (N=7058) | |||||
|---|---|---|---|---|---|---|
| Characteristic | CTA(N=936) | Functional(N=972) | P-value | CTA(N=3564) | Functional(N=3494) | P-value |
| Age, yrs | 0.746 | <.001 | ||||
| N | 936 | 972 | 3564 | 3494 | ||
| Median (25th,75th) | 60.6 (55.0,66.3) | 60.6 (55.2,66.2) | 59.3 (54.0,65.6) | 60.3 (54.7,66.2) | ||
| Female | 500/936 (53.4%) | 525/972 (54.0%) | 0.795 | 1832/3564 (51.4%) | 1863/3494 (53.3%) | 0.107 |
| Race | 0.386 | 0.002 | ||||
| Multiracial | 10/920 (1.1%) | 5/960 (0.5%) | 45/3539 (1.3%) | 25/3470 (0.7%) | ||
| White | 712/920 (77.4%) | 748/960 (77.9%) | 3034/3539 (85.7%) | 3039/3470 (87.6%) | ||
| Black | 149/920 (16.2%) | 158/960 (16.5%) | 333/3539 (9.4%) | 316/3470 (9.1%) | ||
| Asian | 36/920 (3.9%) | 28/960 (2.9%) | 94/3539 (2.7%) | 65/3470 (1.9%) | ||
| Indian | 10/920 (1.1%) | 18/960 (1.9%) | 25/3539 (0.7%) | 10/3470 (0.3%) | ||
| Hawaiian | 3/920 (0.3%) | 3/960 (0.3%) | 8/3539 (0.2%) | 15/3470 (0.4%) | ||
| Ethnicity | 0.827 | 0.461 | ||||
| Hispanic or Latino | 109/931 (11.7%) | 110/966 (11.4%) | 234/3546 (6.6%) | 214/3469 (6.2%) | ||
| Not Hispanic or Latino | 822/931 (88.3%) | 856/966 (88.6%) | 3312/3546 (93.4%) | 3255/3469 (93.8%) | ||
| Cardiac risk factors | ||||||
| Body mass index (kg/m2) | 0.175 | 0.662 | ||||
| N | 921 | 963 | 3540 | 3465 | ||
| Median (25th,75th) | 32.7 (28.7,37.1) | 32.9 (29.4,37.6) | 28.9 (25.9,32.8) | 29.0 (25.8,32.8) | ||
| Hypertension | 747/936 (79.8%) | 778/972 (80.0%) | 0.899 | 2146/3564 (60.2%) | 2139/3494 (61.2%) | 0.387 |
| Dyslipidemia | 725/936 (77.5%) | 748/972 (77.0%) | 0.794 | 2304/3564 (64.6%) | 2293/3494 (65.6%) | 0.388 |
| Smoker (ever/never) | 464/936 (49.6%) | 488/972 (50.2%) | 0.782 | 1828/3563 (51.3%) | 1802/3493 (51.6%) | 0.812 |
| Family history of premature CAD | 297/934 (31.8%) | 282/971 (29.0%) | 0.191 | 1163/3551 (32.8%) | 1097/3481 (31.5%) | 0.267 |
| Depression | 214/936 (22.9%) | 245/971 (25.2%) | 0.226 | 671/3564 (18.8%) | 721/3494 (20.6%) | 0.056 |
| Sedentary lifestyle | 529/935 (56.6%) | 551/972 (56.7%) | 0.961 | 1650/3556 (46.4%) | 1611/3486 (46.2%) | 0.875 |
| Peripheral arterial disease or cerebrovascular disease | 67/936 (7.2%) | 71/972 (7.3%) | 0.902 | 161/3563 (4.5%) | 185/3494 (5.3%) | 0.131 |
| Metabolic syndrome | 785/936 (83.9%) | 839/972 (86.3%) | 0.133 | 888/3564 (24.9%) | 875/3494 (25.0%) | 0.902 |
| All primary presenting symptom | ||||||
| Arm or shoulder pain | 27/936 (2.9%) | 22/972 (2.3%) | 0.391 | 76/3561 (2.1%) | 99/3491 (2.8%) | 0.058 |
| Back pain | 2/936 (0.2%) | 10/972 (1.0%) | 0.024 | 36/3561 (1.0%) | 24/3491 (0.7%) | 0.139 |
| Chest pain* | 680/936 (72.6%) | 676/972 (69.5%) | 0.135 | 2642/3561 (74.2%) | 2524/3491 (72.3%) | 0.073 |
| Aching/dull | 173/680 (25.4%) | 157/676 (23.2%) | 0.342 | 669/2642 (25.3%) | 656/2524 (26.0%) | 0.582 |
| Burning/pins and needles | 58/680 (8.5%) | 69/676 (10.2%) | 0.289 | 246/2642 (9.3%) | 244/2524 (9.7%) | 0.662 |
| Crushing/pressure/squeezing/ tightness | 332/680 (48.8%) | 331/676 (49.0%) | 0.959 | 1343/2642 (50.8%) | 1239/2524 (49.1%) | 0.210 |
| Other | 215/680 (31.6%) | 201/676 (29.7%) | 0.452 | 792/2642 (30.0%) | 755/2524 (29.9%) | 0.960 |
| Fatigue or weakness | 26/936 (2.8%) | 23/972 (2.4%) | 0.570 | 98/3561 (2.8%) | 89/3491 (2.5%) | 0.596 |
| Neck or jaw pain | 5/936 (0.5%) | 6/972 (0.6%) | 0.811 | 39/3561 (1.1%) | 47/3491 (1.3%) | 0.337 |
| Palpitations | 23/936 (2.5%) | 23/972 (2.4%) | 0.897 | 83/3561 (2.3%) | 88/3491 (2.5%) | 0.604 |
| Dyspnea | 151/936 (16.1%) | 185/972 (19.0%) | 0.096 | 482/3561 (13.5%) | 528/3491 (15.1%) | 0.057 |
| Other† | 22/936 (2.4%) | 27/972 (2.8%) | 0.555 | 105/3561 (2.9%) | 92/3491 (2.6%) | 0.425 |
| Physician characterization of chest pain | ||||||
| Chest pain typicality | 0.139 | 0.722 | ||||
| Typical | 137/936 (14.6%) | 121/972 (12.4%) | 384/3564 (10.8%) | 385/3494 (11.0%) | ||
| Atypical | 724/936 (77.4%) | 753/972 (77.5%) | 2777/3564 (77.9%) | 2734/3494 (78.2%) | ||
| Non-cardiac | 75/936 (8.0%) | 98/972 (10.1%) | 403/3564 (11.3%) | 375/3494 (10.7%) | ||
| Medication use | ||||||
| Aspirin | 488/922 (52.9%) | 504/964 (52.3%) | 0.779 | 1457/3381 (43.1%) | 1385/3315 (41.8%) | 0.277 |
| Clopidogrel | 15/922 (1.6%) | 21/964 (2.2%) | 0.382 | 41/3381 (1.2%) | 47/3315 (1.4%) | 0.461 |
| Statin | 574/922 (62.3%) | 574/964 (59.5%) | 0.228 | 1399/3381 (41.4%) | 1390/3315 (41.9%) | 0.647 |
| Beta-blocker | 262/922 (28.4%) | 280/964 (29.0%) | 0.763 | 803/3381 (23.8%) | 790/3315 (23.8%) | 0.938 |
| ACEi or ARB | 633/922 (68.7%) | 656/964 (68.0%) | 0.778 | 1227/3381 (36.3%) | 1247/3315 (37.6%) | 0.261 |
| Diuretics | 310/922 (33.6%) | 378/964 (39.2%) | 0.012 | 850/3381 (25.1%) | 831/3315 (25.1%) | 0.945 |
| Oral hypoglycemic‡ | 690/936 (73.7%) | 739/972 (76.0%) | 0.245 | 0/3564 (0.0%) | 0/3494 (0.0%) | |
| Insulin‡ | 204/936 (21.8%) | 216/972 (22.2%) | 0.822 | 0/3564 (0.0%) | 0/3494 (0.0%) | |
| ECG findings | ||||||
| ECG Q waves | 51/926 (5.5%) | 61/965 (6.3%) | 0.454 | 146/3533 (4.1%) | 149/3460 (4.3%) | 0.718 |
| ECG findings that could interfere with exercise stress test interpretation | 58/926 (6.3%) | 71/966 (7.3%) | 0.349 | 208/3534 (5.9%) | 181/3459 (5.2%) | 0.234 |
| LBBB | 11/58 (19.0%) | 14/71 (19.7%) | 0.914 | 53/208 (25.5%) | 47/181 (26.0%) | 0.913 |
| ST depression | 11/58 (19.0%) | 15/71 (21.1%) | 0.761 | 48/208 (23.1%) | 36/181 (19.9%) | 0.446 |
| LVH with repolarization | 10/58 (17.2%) | 11/71 (15.5%) | 0.789 | 24/208 (11.5%) | 23/181 (12.7%) | 0.724 |
| Other | 30/58 (51.7%) | 35/71 (49.3%) | 0.784 | 84/208 (40.4%) | 75/181 (41.4%) | 0.833 |
| 10-year CVD risk | ||||||
| ASCVD (2013) | 0.356 | 0.025 | ||||
| N | 918 | 960 | 3533 | 3466 | ||
| Median (25th,75th) | 19.4 (11.6,32.3) | 20.1 (12.3,32.1) | 9.4 (5.4,15.8) | 9.9 (5.6,16.9) | ||
| Low risk (<7.5%) | 93/918 (10.1%) | 99/960 (10.3%) | 0.897 | 1378/3533 (39.0%) | 1297/3466 (37.4%) | 0.173 |
| Elevated risk (>7.5%) | 825/918 (89.9%) | 861/960 (89.7%) | 0.897 | 2155/3533 (61.0%) | 2169/3466 (62.6%) | 0.173 |
Values are n/N (%) except where indicated.
Chest pain – substernal or left anterior or Chest pain other are selected as primary symptoms. Multiple characterizations are possible.
Includes diaphoresis/sweating, dizziness/lightheaded, epigastric/abdominal pain, nausea/vomiting, syncope, and other.
Data available only for patients with diabetes mellitus.
Provider’s assessment of the likelihood that subject has significant epicardial coronary stenosis or left main stenosis. Significant = ≥70% epicardial coronary stenosis or ≥50% left main stenosis.
ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; ASCVD, Atherosclerotic Cardiovascular Disease; CAD, coronary artery disease; CASS, Coronary Artery Surgery Study; CTA, computed tomographic angiography; CVD, cardiovascular disease; ECG, electrocardiogram; LBBB, left bundle branch block; LVH, left ventricular hypertrophy.
Processes of care after NIT
Test positivity
Among patients with diabetes versus those without diabetes, there was an increased likelihood of positive NIT (15.2% vs. 11.5%, unadjusted odds ratio [OR] 1.38, 95% confidence interval [CI] 1.19–1.59; p<0.001; adjusted OR [aOR] 1.38, 95% CI 1.19–1.60; p<0.001). Testing modality did not modify the relationship between diabetes and NIT test result (interaction p-value=0.930). The distribution and details of positive test results by test modality have been published previously (10). Among the 972 patients with diabetes who underwent functional stress testing, 711 (73%) were referred for a nuclear scan, 185 (19%) were referred for an echocardiogram stress test, and only 76 (8%) were referred for an ECG stress test. Among the 76 patients referred for an ECG stress test, only 7 (9%) had a positive test (defined as ST-segment changes consistent with ischemia during stress being detected or if the stress was terminated early [< 3 min] due to reproduction of symptoms, arrhythmia, and/or hypotension). Furthermore, among those who underwent ECG stress test, 4 (5%) failed to achieve maximal stress.
Referral to ICA
Patients with diabetes, compared to patients without diabetes, were more likely to be referred for ICA within 90 days of NIT (diabetes 12.6% [240/1908] vs. without diabetes 9.3% [653/7058]) in both unadjusted (OR 1.41, 95% CI 1.21–1.65, p<0.001) and adjusted analyses (aOR 1.26, 95% CI 1.03–1.53, p=0.024). Patients undergoing CTA, compared to stress testing, had increased referral to ICA; diabetes did not modify the relationship between NIT modality and referral to ICA (adjusted interaction p-value = 0.596; Online Table 3).
Referral to revascularization
Among those receiving catheterization, patients with and without diabetes had similar likelihood of referral to revascularization within 30 days of ICA (diabetes 48.3% [116/240] vs. 45.0% [294/654], unadjusted OR 1.15, 95% CI 0.85–1.54, p=0.369; aOR 0.86, 95% CI 0.53–1.41, p=0.561). Patients undergoing CTA, compared to stress testing, had increased referral to revascularization; diabetes did not modify the relationship between NIT modality and referral to ICA (adjusted interaction p-value = 0.372; Online Table 4). The results for CTA and stress testing by invasive angiographic findings and the invasive angiographic findings by revascularization use are presented in Online Table 5.
Medication use reported at 60-day visit
Overall, patients with diabetes, compared to patients without diabetes, were more likely to have a prescription at the 60-day visit for aspirin (aOR 1.50, 95% CI 1.34–1.67, p<0.001), statin (aOR 2.19, 95% CI 1.95–2.45, p<0.001), beta-blocker (aOR 1.34, 95% CI 1.19–1.50, p<0.001), and ACEi/ARB (aOR 3.84, 95% CI 3.42–4.31, p<0.001) (Table 2).
Table 2:
Association between diabetes history and medication use reported at 60-day visit
| Proportion Using Medications(No. Reported/Sample Size) | Unadjusted* | Adjusted† | ||||
|---|---|---|---|---|---|---|
| Medication | Diabetes | No Diabetes | Odds Ratio (95% CI) | P-value | Odds Ratio (95% CI) | P-value |
| Aspirin | ||||||
| Diabetes vs. No Diabetes | 1034/1733 (59.7%) | 3110/6226 (50.0%) | 1.48 (1.33–1.65) | <0.001 | 1.50 (1.34–1.67) | <0.001 |
| Statin | ||||||
| Diabetes vs. No Diabetes | 1175/1733 (67.8%) | 3076/6226 (49.4%) | 2.16 (1.93–2.41) | <0.001 | 2.19 (1.95–2.45) | <0.001 |
| Beta-blocker | ||||||
| Diabetes vs. No Diabetes | 594/1733 (34.3%) | 1744/6226 (28.0%) | 1.34 (1.20–1.50) | <0.001 | 1.34 (1.19–1.50) | <0.001 |
| ACEi/ARB | ||||||
| Diabetes vs. No Diabetes | 1207/1733 (69.7%) | 2337/6226 (37.5%) | 3.82 (3.40–4.28) | <0.001 | 3.84 (3.42–4.31) | <0.001 |
Unadjusted model contains diabetes mellitus.
Adjusted model controls for noninvasive test modality, age, and sex.
ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; CI, confidence interval.
Diabetes did not modify the relationship between testing modality and the likelihood of having a day-60 prescription for statin (adjusted p-value =0.783) (Online Table 6). Similarly, diabetes did not modify the relationship between testing modality and the likelihood of having a day-60 prescription for aspirin (adjusted p-value = 0.907) (Online Table 6). Among patients with and without diabetes, those who had a positive NIT result had a numerically increased likelihood of being prescribed a statin by the 60-day visit and to be referred for ICA within 90 days after randomization (Online Table 7). The use of statins at 60 days was numerically higher, in both patients with and without diabetes, in the CTA arm compared to stress testing arm, when stratified by severity of results (Online Table 8).
Association between diabetes, testing modality, and outcomes
Patients with diabetes, compared with patients without diabetes, were at higher risk for death/MI/UAH (adjusted HR [aHR] 1.40, 95% CI 1.07–1.83, p=0.015) and at similar risk for CV death/MI (aHR 1.35, 95% CI 0.91–1.99, p=0.131) (Online Table 9). Diabetes did not modify the relationship between NIT result and death/MI/UAH (adjusted interaction p-value 0.179) or NIT results and CV death/MI (adjusted interaction p-value 0.884).
Diabetes significantly modified the relationship between testing modality and the outcomes of death/MI/UAH (adjusted interaction p-value = 0.096), and CV death/MI (adjusted interaction p-value = 0.02) (Figures 1 and 2). Patients with diabetes who underwent CTA, compared to functional stress testing, had a numerically lower likelihood of death/MI/UAH (CTA 3.4% [32/936] vs. 4.4% [43/972]; aHR 0.74, 95% CI 0.47–1.18; p=0.207). Diabetic patients who underwent CTA, compared to those who underwent functional stress testing, had a significantly lower risk of CV death/MI (CTA 1.1% [10/936] vs. functional stress testing 2.6% [25/972]; aHR 0.38, 95% CI 0.18–0.79; p=0.01) (Table 4). Patients without diabetes who underwent CTA, compared with functional stress testing, had a similar adjusted likelihood of death/MI/UAH (CTA 3.0% [105/3564] vs. functional stress testing 2.4% [85/3494]; aHR 1.18, 95% CI 0.88–1.57; p=0.269) and CV death/MI (CTA 1.4% [50/3564] vs. functional stress testing 1.29% [45/3494]; aHR 1.03, 95% CI 0.69–1.54; p=0.887).
Figure 1. Kaplan-Meier curves for the composite of death/myocardial infarction/unstable angina hospitalization by randomized noninvasive testing modality and diabetes history.
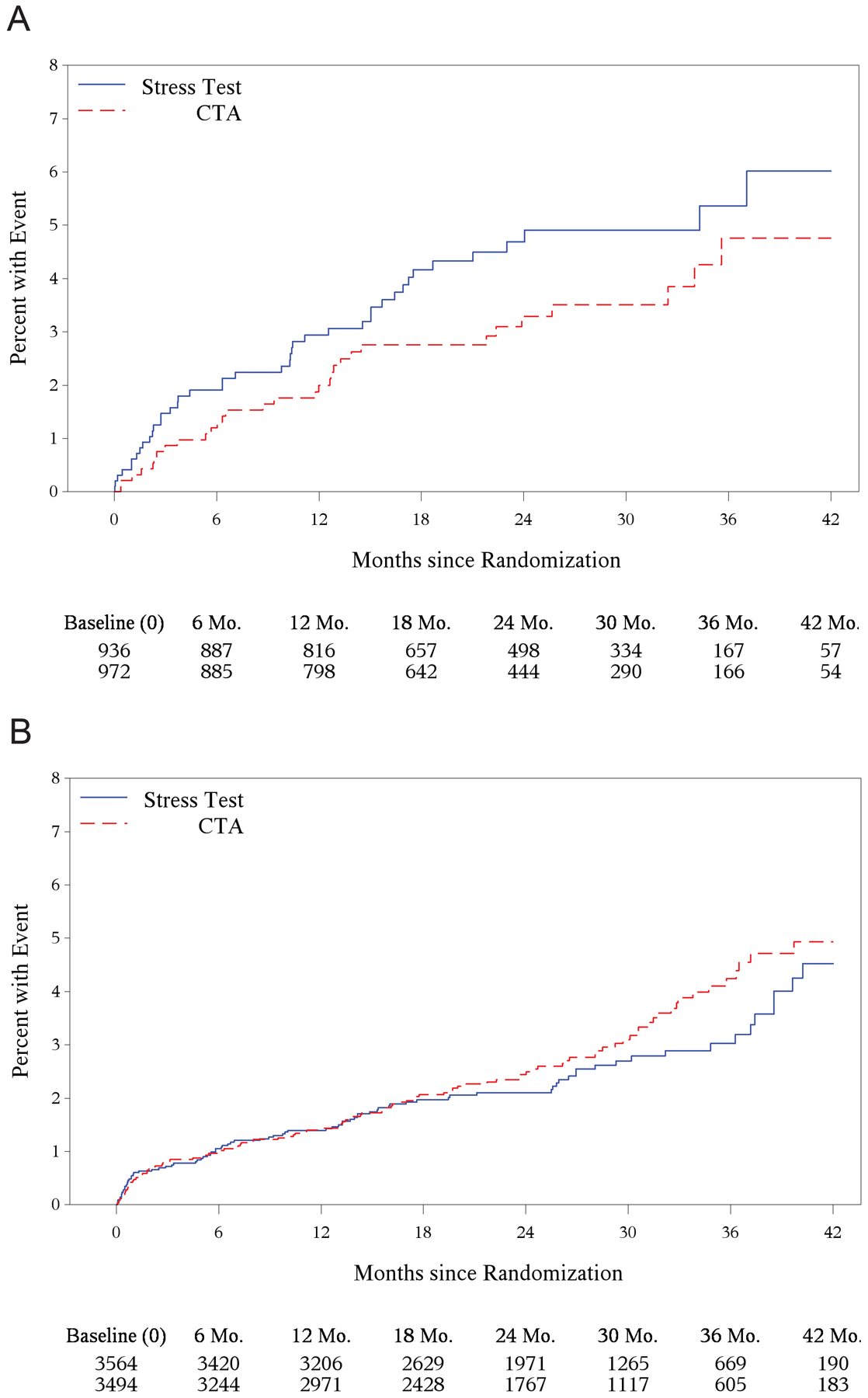
. (A) Patients with diabetes. Adjusted hazard ratio between patients randomized to CTA vs. functional testing, 0.74; 95% confidence interval, 0.47–1.18; p-value = 0.207. (B) Patients without diabetes. Adjusted hazard ratio between patients randomized to CTA vs. functional testing, 1.18; 95% confidence interval, 0.88–1.57; p-value = 0.269. CTA, computed tomographic angiography.
Figure 2. [central illustration]. Kaplan-Meier curves for the composite of cardiovascular death/myocardial infarction by randomized noninvasive testing modality and diabetes history.
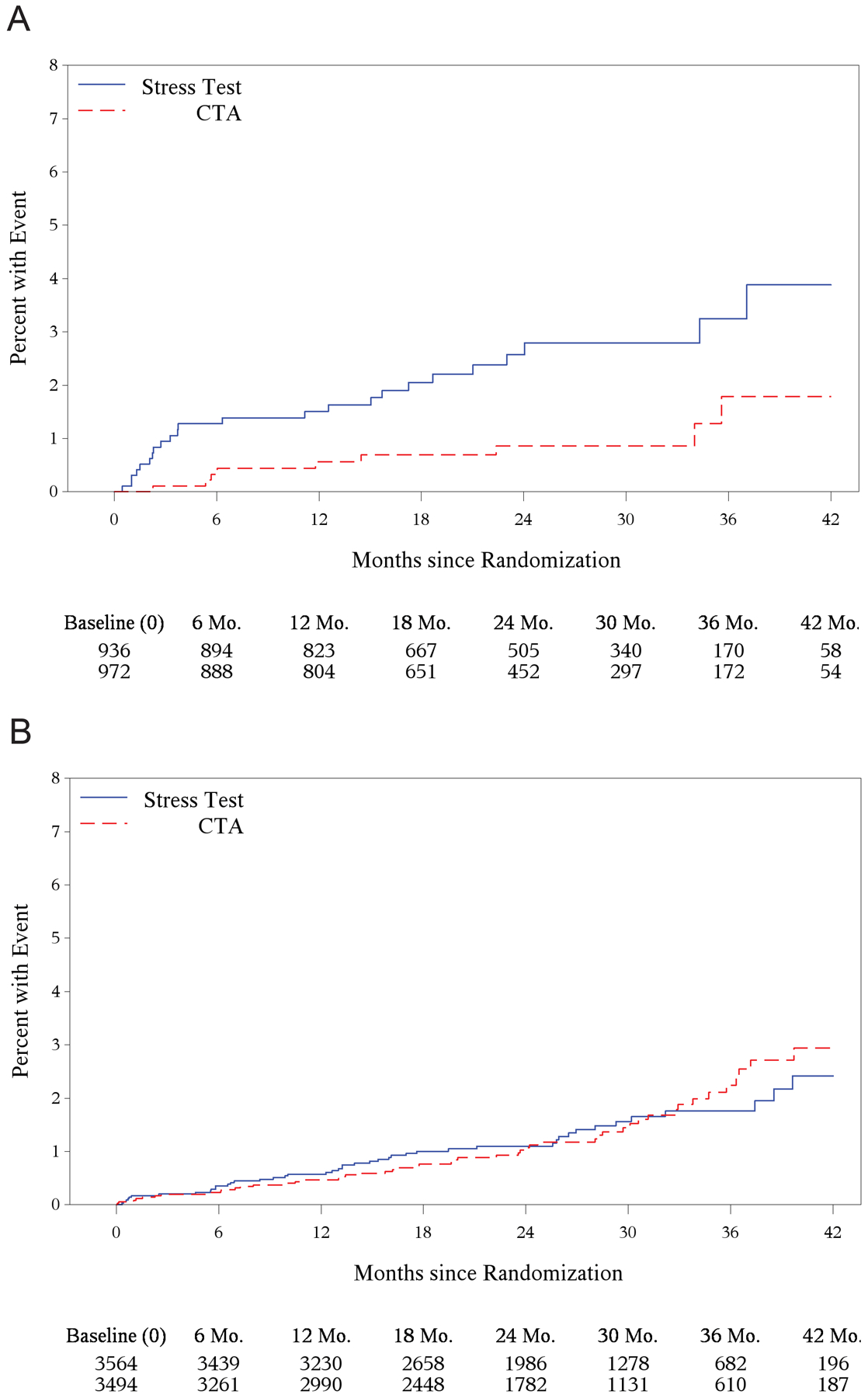
. (A) Patients with diabetes. Adjusted hazard ratio between patients randomized to CTA vs. functional testing, 0.38; 95% confidence interval, 0.18–0.79; p-value = 0.01 (B) Patients without diabetes. Adjusted hazard ratio between patients randomized to CTA vs. functional testing, 1.03; 95% confidence interval, 0.69–1.54; p-value = 0.887. CTA, computed tomographic angiography.
Among patients with diabetes having CTA, compared to those having stress tests, there was a non-significant decrease within 6 months in the number of deaths, CV deaths, and MIs; however, there was an increase in UAH among patients with diabetes having CTA compared to those having stress tests. Among patients without diabetes having CTA, compared to those having a stress test, although there was a non-significant decrease in deaths within 6 months, the remaining events were balanced between the two testing arms (Online Table 10). The overall breakdown of clinical events by individual outcome endpoints is presented in Online Table 11. Our data do not suggest that there exists a jointly modifying effect on the association between disease severity and adverse events by diabetes history (death/MI/UAH: 3-way interaction p-value: 0.1369; CV death/MI: 3-way interaction p-value: 0.9361) (Online Table 12).
Discussion
Despite the high risk of CV outcomes in patients with diabetes, the optimal NIT strategy to evaluate for symptoms suggestive of CAD in this group remains unclear. In our analysis of the PROMISE trial, we identified the following major findings: (a) diabetes influences the processes of care decisions following NIT, including increased referral to ICA and 60-day medication prescription; and (b) patients with diabetes who had a CTA, compared to functional stress testing, had a significantly reduced risk of adverse CV events (a difference not seen in patients without diabetes). These results suggest that, among patients with diabetes who have symptoms suggestive of CAD, CTA may be the preferred initial NIT modality. In patients without diabetes who have similar outcomes regardless of initial CTA versus functional stress testing, test choice is less clear.
In the PROMISE trial, diabetes was associated with an increased likelihood of positive NIT including more high-risk CTA and functional test findings (10).Yet even after adjustment for NIT result, the presence of diabetes was associated with an increased likelihood of referral to ICA. Our patients with diabetes had a higher predicted 10-year risk of adverse CV events (Framingham and ASCVD); however, the likelihood of CAD based on the Diamond-Forrester was similar. Our data suggest that these factors may be driving physician practice patterns, resulting in an increased referral to ICA even after controlling for test results. Despite this finding, referral to revascularization is similar between patients with and without diabetes. This suggests that once coronary anatomy is identified, the presence of diabetes no longer influences the decision to send a patient for revascularization, a finding that has been seen in previous registries of patients with stable angina (11). The higher use of medication at 60-day visit among patients with diabetes is likely influenced by the greater baseline use of these medications and guideline recommendations for aggressive risk factor modification (12,13).
We identified an increased risk of CV events in patients with diabetes, compared to those without diabetes, presenting with stable symptoms. Although these results align with previous reports of patients with and without diabetes who present with chest pain (14), there are some conflicting reports. The Euro Heart Survey on Coronary Revascularization (EHS-CR) prospectively enrolled patients with stable CAD (proven stenosis > 50%) undergoing ICA (11) and found that diabetes did not increase the risk of death/MI/UAH at 1 year (aHR 1.0, 95% CI 0.7–1.4), compared to those without diabetes. However, both patients with and without diabetes in our analysis had a lower event rate compared to previous research, with a 1.83% risk of CV death/MI over a median follow-up of 2 years (6). Other studies in similar populations have reported a CV death/MI risk as high as 13% over a median follow-up of 3 years (14). In comparison, our data demonstrate a good prognosis in a contemporary cohort of new onset chest pain patients with diabetes, and may result from more intensive medical management (such as use of statins) and improvements in the optimization of cardiac care.
Patients with diabetes who were assigned to an anatomic CTA testing strategy suffered significantly less CV death/MI than those assigned to a functional stress testing strategy. In contrast, no such difference was observed between the testing strategies in patients without diabetes. Furthermore, in both patients with and without diabetes, those who underwent a CTA had a greater likelihood of being referred to ICA and having increased preventive medication use at 60 days including aspirin and statins. Our results align with a recently published meta-analysis of CTA versus functional testing in patients with suspected CAD (the meta-analysis included the PROMISE study) (15). This analysis demonstrated that patients randomized to CTA, compared to functional stress testing, had an overall decreased risk of myocardial infarction (CTA 0.7% vs. 1.1%; HR 0.71, 95% CI 0.53–0.96) and increased likelihood of aspirin and statin prescription. A prior analysis of the PROMISE trial demonstrated that a majority of CV events occurred in patients with non-obstructive CAD (16). By enabling a visualization of non-obstructive CAD, CTA identifies additional at-risk patients and provides superior prognostic and discriminatory information when compared to functional stress testing. As the overall risk of subsequent CV events among stable contemporary patients with symptoms suggestive of CAD is low, the increased use of established cardio-protective therapies (as clearly influenced by CTA findings) would likely impart a greater magnitude of benefit among patients enriched for CV events – such as those with diabetes. Whether the increased referral for ICA and revascularization following CTA contributes to improved outcomes among patients with diabetes would require further exploration in a well-powered prospective randomized trial. A previous analysis demonstrated that an absence of diabetes was one of several factors associated with a higher likelihood of negative NIT results and fewer events in the PROMISE trial cohort (17). The extended follow-up results of the Scottish Computed Tomography of the Heart (SCOT-HEART) study, which randomized stable outpatients with chest pain to CTA versus standard of care, suggested that the use of CTA resulted in more correct diagnosis of CAD; this subsequently resulted in a greater use of cardio-protective therapies, which resulted in fewer clinical events among patients randomized to CTA (18). Our analysis extends on this finding by demonstrating that among patients both with and without diabetes randomized to CTA, compared to stress testing, statin use at 60 days after randomization was higher in patients with any abnormal CTA result. While prospective confirmation is required, these results suggest that physicians caring for patients who have diabetes and symptoms suggestive of CAD should consider CTA as the initial NIT modality of choice as this may yield better CV outcomes in these patients than stress testing (4).
Our findings suggest that diabetes does not modify the relationship between NIT modality and the outcome of death/MI/UAH. However, the directionality of the hazard ratio between CTA vs. functional testing in patients with diabetes and those without diabetes is consistent with the results seen in the outcome of CV death/MI (Table 3). These findings suggest a possible benefit of CTA over functional testing in patients with diabetes, but our study population was underpowered to detect this difference. Among patients with diabetes, the primary benefit of CTA over functional testing is to reduce the risk of CV events – specifically CV death/MI. Among patients across the spectrum of glycemic disorder including those with pre-diabetes (19) and those with diabetes and established CV disease (20), non-CV death forms a large burden of mortality. This competing cause of death may not necessarily be modified by the downstream treatments following NIT. This may have contributed to the absence of a statistically significant reduction in death/MI/UAH in CTA vs. functional testing in PROMISE trial patients with diabetes despite a significant reduction in CV death/MI.
Table 3:
Association between randomized non-invasive testing modality and clinical outcomes by diabetes history
| Raw Clinical Event Rate(No. of Events/Sample Size) | Unadjusted* | Adjusted† | ||||
|---|---|---|---|---|---|---|
| Clinical Endpoint | CTA | Stress Test | Hazard Ratio (95% CI) | P-value | Hazard Ratio (95% CI) | P-value |
| Death/MI/UAH | ||||||
| Interaction between diabetes and testing modality | 0.093 | 0.096 | ||||
| CTA vs. Stress Test in patients with diabetes | 32/936 (3.4%) | 43/972 (4.4%) | 0.73 (0.46–1.15) | 0.170 | 0.74 (0.47–1.18) | 0.207 |
| CTA vs. Stress Test in patients without diabetes | 105/3564 (3.0%) | 85/3494 (2.4%) | 1.15 (0.87–1.53) | 0.330 | 1.18 (0.88–1.57) | 0.269 |
| CV Death/MI | ||||||
| Interaction between diabetes and testing modality | 0.022 | 0.020 | ||||
| CTA vs. Stress Test in patients with diabetes | 10/936 (1.1%) | 25/972 (2.6%) | 0.39 (0.19–0.80) | 0.011 | 0.38 (0.18–0.79) | 0.010 |
| CTA vs. Stress Test in patients without diabetes | 50/3564 (1.4%) | 45/3494 (1.3%) | 1.03 (0.69–1.53) | 0.901 | 1.03 (0.69–1.54) | 0.887 |
Unadjusted model contains diabetes mellitus, initial noninvasive test modality, and their two-way interaction.
Adjusted model controls for noninvasive test results (positive/negative), invasive coronary angiography results (positive/negative/not tested, time-dependent), revascularization (time-dependent), age (time-dependent), and sex.
CI, confidence interval; CTA, computed tomographic angiography; CV, cardiovascular; MI, myocardial infarction; UAH, unstable angina hospitalization.
Limitations
Although our study is post-hoc and is subject to the inherent limitations of this type of analysis, evaluation of testing modality and outcomes in patients with diabetes was prespecified. The identification of reduced risk of CV death/MI in patients with diabetes associated with CTA randomization was based on small numbers. The trends toward reduced risk of death/MI/UAH and CV death/MI/UAH in patients with diabetes undergoing CTA versus functional testing reinforce the findings seen with the endpoint of CV death/MI. Failure to achieve maximal stress during an ECG stress test may also pose a limitation; however, only 5% of patients with diabetes failed to achieve maximal stress testing. Further, they are mechanistically plausible based on improved processes of care. The presence of diabetes was not formally established by HbA1c or fasting glucose testing. Data on the type, duration, and degree of control of diabetes were not available. Glycemic control during the trial and the types of antihyperglycemic medications that may have changed during the conduct of the trial are unknown. Data on risk factor control during the conduct of the trial were not collected. Slight statistical differences in some of the baseline characteristics were seen in patients without diabetes who were randomized to CTA versus functional stress testing; however, the absolute differences were small and likely not clinically relevant.
Conclusion
Among a contemporary cohort of patients with symptoms suggestive of CAD requiring testing, patients with diabetes are at increased risk of CV events compared to those without diabetes; however, the absolute risk of events is still low. Patients with diabetes who were randomized to CTA rather than functional stress testing had a reduced risk of CV events compared to those randomized to functional testing. This finding likely arises from increased use of downstream investigations and appropriate prescription of preventative therapies that may reduce CV events (such as statins). In evaluating stable patients with diabetes who have symptoms suggestive of CAD, physicians should consider these benefits of using CTA as the initial diagnostic strategy.
Supplementary Material
Clinical Perspectives.
Competency in Medical Knowledge:
Diabetes is an established marker for cardiovascular risk. In the PROMISE trial, among stable patients with diabetes who present with symptoms suggestive of coronary artery disease, those who underwent coronary computed tomographic angiography (CTA) had a reduced risk of cardiovascular death or myocardial infarction compared to patients who underwent functional stress testing. This finding was not seen in patients without diabetes.
Translational Outlook:
Patients in the PROMISE trial who underwent CTA had increased subsequent invasive evaluations and medical therapy (such as statins, aspirin, and angiotensin-converting enzyme inhibitors/angiotensin receptor blockers). This finding was also seen among patients with diabetes who underwent CTA, which may have contributed to the improvement in outcomes. Strategies to increase the use of appropriate evidence-based medical therapies such as statins in patients with diabetes who present with chest pain may represent an avenue to improve outcomes in this patient population.
Funding
This project was supported by grants R01HL098237, R01HL098236, R01HL98305, and R01HL098235 from the National Heart, Lung, and Blood Institute (NHLBI). The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents. This paper does not necessarily represent the official views of NHLBI.
Abbreviations
- CAD
coronary artery disease
- CTA
coronary computed tomographic angiography
- NIT
noninvasive test
Footnotes
Disclosures
A.S. reports receiving support from Bayer-Canadian Cardiovascular Society, Alberta Innovates Health Solution, Roche Diagnostics, and Takeda. N.J.P. reports having ownership in Freedom Health, Inc.; Physician Partners, LLC; RXAdvance, LLC; and Florida Medical Associates, LLC. M.T.L. reports receiving the American Roentgen Ray Society Scholarship. D.B.M. reports receiving grants from the National Institutes of Health, Eli Lilly and Company, Bristol-Myers Squibb, Gilead Sciences, AGA Medical Corporation, Merck & Company, Oxygen Therapeutics, and AstraZeneca, and personal fees from CardioDx, Medtronic, and St. Jude Medical. K.L.L. reports receiving grants from the National Institutes of Health. U.H. reports receiving grants from HeartFlow and Kowa Pharmaceuticals. P.S.D. reports receiving grant support from HeartFlow and service on a data and safety monitoring board for GE HealthCare. The remaining authors have nothing to disclose.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 2016;133:e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Schramm TK, Gislason GH, Kober L, et al. Diabetes patients requiring glucose-lowering therapy and nondiabetics with a prior myocardial infarction carry the same cardiovascular risk: a population study of 3.3 million people. Circulation 2008;117:1945–1954. doi: 10.1161/CIRCULATIONAHA.107.720847. [DOI] [PubMed] [Google Scholar]
- 3.Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 1998;339:229–234. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 4.Muhlestein JB, Lappé DL, Lima JA, et al. Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. JAMA 2014;312:2234–2243. doi: 10.1001/jama.2014.15825. [DOI] [PubMed] [Google Scholar]
- 5.Young LH, Wackers FJT, Chyun DA, et al. Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes: the DIAD study: a randomized controlled trial. JAMA 2009;301:1547–1555. doi: 10.1001/jama.2009.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Douglas PS, Hoffmann U, Patel MR, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 2015;372:1291–1300. doi: 10.1056/NEJMoa1415516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Douglas PS, Hoffmann U, Lee KL, et al. PROspective Multicenter Imaging Study for Evaluation of chest pain: rationale and design of the PROMISE trial. Am Heart J 2014;167:796–803.e1. doi: 10.1016/j.ahj.2014.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hemal K, Pagidipati NJ, Coles A, et al. Sex differences in demographics, risk factors, presentation, and noninvasive testing in stable outpatients with suspected coronary artery disease: insights from the PROMISE trial. JACC Cardiovasc Imaging 2016;9:337–346. doi: 10.1016/j.jcmg.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pagidipati NJ, Hemal K, Coles A, et al. Sex differences in functional and CT angiography testing in patients with suspected coronary artery disease. J Am Coll Cardiol 2016;67:2607–2616. doi: 10.1016/j.jacc.2016.03.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma A, Sekaran NK, Coles A, et al. Impact of diabetes mellitus on the evaluation of stable chest pain patients: insights from the PROMISE (Prospective Multicenter Imaging Study for Evaluation of Chest Pain) trial. J Am Heart Assoc 2017;6:pii: e007019. doi: 10.1161/JAHA.117.007019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Breeman A, Bertrand ME, Ottervanger JP, et al. Diabetes does not influence treatment decisions regarding revascularization in patients with stable coronary artery disease. Diabetes Care 2006;29:2003–2011. doi: 10.2337/dc06-0118. [DOI] [PubMed] [Google Scholar]
- 12.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129(25 Suppl 2):S1–S45. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- 13.American Diabetes Association. Standards of medical care in diabetes 2016. Cardiovascular disease and risk management. Diabetes Care 2016;39(Suppl 1):S60–S71. doi: 10.2337/dc16-S011. [DOI] [PubMed] [Google Scholar]
- 14.Junghans C, Sekhri N, Zaman MJ, Hemingway H, Feder GS, Timmis A. Atypical chest pain in diabetic patients with suspected stable angina: impact on diagnosis and coronary outcomes. Eur Heart J Qual Care Clin Outcomes 2015;1:37–43. doi: 10.1093/ehjqcco/qcv003. [DOI] [PubMed] [Google Scholar]
- 15.Chang AM, Litt HI, Snyder BS, et al. Impact of coronary computed tomography angiography findings on initiation of cardioprotective medications. Circulation 2017;136:2195–2197. doi: 10.1161/CIRCULATIONAHA.117.029994. [DOI] [PubMed] [Google Scholar]
- 16.Hoffmann U, Ferencik M, Udelson JE, et al. Prognostic value of noninvasive cardiovascular testing in patients with stable chest pain. Circulation 2017;135:2320–2332. doi: 10.1161/CIRCULATIONAHA.116.024360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fordyce CB, Douglas PS, Roberts RS, et al. Identification of patients with stable chest pain deriving minimal value from noninvasive testing: the PROMISE minimal-risk tool, a secondary analysis of a randomized clinical trial. JAMA Cardiol 2017;2:400–408. doi: 10.1001/jamacardio.2016.5501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.SCOT-HEART Investigators; Newby DE, Adamson PD, et al. Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med 2018;379:924–933. doi: 10.1056/NEJMoa1805971. [DOI] [PubMed] [Google Scholar]
- 19.Sharma A, de Souza Brito F, Sun JL, et al. Noncardiovascular deaths are more common than cardiovascular deaths in patients with cardiovascular disease or cardiovascular risk factors and impaired glucose tolerance: Insights from the Nateglinide and Valsartan in Impaired Glucose Tolerance Outcomes Research (NAVIGATOR) trial. Am Heart J 2017;186:73–82. doi: 10.1016/j.ahj.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 20.Sharma A, Green JB, Dunning A, et al. Causes of death in a contemporary cohort of patients with type 2 diabetes and atherosclerotic cardiovascular disease: insights from the TECOS trial. Diabetes Care 2017;40:1763–1770. doi: 10.2337/dc17-1091. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


