Abstract
Background
With technological innovations especially newer parenchymal transection devices, improved understanding of hepatic anatomy facilitated by better imaging, and reconstructions along with experiences gained from advanced minimal invasive procedures, laparoscopic liver surgery is gaining momentum with more than 5300 reported cases worldwide. Most of the published literature comprises nonanatomical and segmental resections with only few case series having major hepatic resections performed by minimally invasive approach. Aim of this article is to share our technique and experience of total laparoscopic major hepatectomy.
Methods
It is a retrospective analysis of prospectively maintained database of 56 patients, who underwent laparoscopic major hepatectomy for various indications during 2001 to 2013.
Results
Of 56 patients operated, 37 had malignant disease and 19 had benign lesions with mean size of 6.0 ± 2.8 cm. Thirty-four patients underwent right hepatectomy and 22 left with mean age of 54.8 ± 15.3 years. Mean operating time was 227.4 ± 51.8 min with mean blood loss 265.5 ± 143.4 ml and transfusion needed in 10.7 %. Pringle’s maneuver was used in 19.6 % with mean occlusion time of 34.0 ± 11.4 min. Liver-specific complications were observed in 12.5 % and overall complications in 19.6 %. Mean resection margin length in malignant lesions was 2.1 ± 0.9 cm, with <1 cm margin noted in 5.4 %. Median hospital stay was 8 days (6–29) with readmission rate of 8.9 %, re-intervention rate of 5.3 % and 90 days mortality of 1.7 %.
Conclusion
Laparoscopic major liver resection is a formidable task. It requires considerable expertise in both, advanced laparoscopy, and liver surgery. It can be feasible, safe, and oncologically adequate in well-selected cases in experience hands.
Keywords: Laparoscopic liver surgery, Major hepatectomy, Major liver resection, Hepatocellular carcinoma, Liver resection
Introduction
A minimally invasive approach toward intra-abdominal malignancies has evolved considerably. From mere staging laparoscopy and palliative procedures, minimally invasive curative resections are increasingly being performed. Laparoscopic liver resection (LLR) although reported early in 1992 by Gagner et al.1 has progressed, albeit with slow pace. The cautious approach was partly due to complexity of surgical procedures with fear of uncontrolled bleeding, bile leak, and gas embolism along with initial doubts about its oncological adequacy and safety.
Technological innovations especially various parenchymal transection devices coupled with improved understanding of hepatic anatomy facilitated by better imaging and reconstruction methods had contributed immensely. Developments in liver transplantation also added in a way by increasing familiarity of surgeons to liver surgeries. With almost two decades of development and around 5300 reported cases worldwide,2 laparoscopic liver surgery is gaining momentum.
Most of the published literature comprises segmentectomies, nonanatomical resections along with few major hepatic resections by minimally invasive approach. In a review published in 2009 on laparoscopic liver resection, out of 2804 cases, only 9.0 % were right hepatectomy and 7.0 % left hepatectomy3 constituting 16.0 % of surgeries. In accordance with this, we aimed to share our technique and experience of laparoscopic major hepatectomies (Brisbane 2000 Nomenclature4) for benign and malignant lesions with short-term outcomes.
Materials and Methods
This is a retrospective analysis of prospectively maintained database of all patients who underwent laparoscopic major hepatectomy for various indications from 2001 to 2013, at a tertiary care teaching institute.
- Exclusion criteria
- Lesion close to portal pedicle or hepatic veins
- Child B or C status
- ASA > II
- Extended hepatic resections
- Concomitant resection of other organ
All patients were subjected to thorough preoperative workup including contrast enhanced CT; magnetic resonance imaging (MRI) was done when needed. Vascular image reconstructions and volumetric analysis were utilized wherever indicated. Liver function reserve was assessed using Child-Turcotte-Pugh (CTP) score in patients with cirrhosis. Presence of cirrhosis alone was not considered as an absolute contraindication for laparoscopic approach. There was no upper limit for size of lesion when more than 1-cm margin could be achieved. Patients requiring biliary or vascular reconstruction were not offered laparoscopic resection. Patients with cirrhosis were optimized before proceeding for surgery. All patients were kept fasting for at least 6 hour prior to surgery. Preoperatively, all patients received prophylactic antibiotic at the time of induction of anesthesia. All patients were operated under general anesthesia with endotracheal intubation. Results were analyzed on the basis of
- Primary outcomes
- All-cause mortality (90 days)
- Oncological clearance (if applicable)
- Complications (liver specific/overall)
- Secondary outcomes
- Tumor resection margins
- Number of patients requiring blood transfusion
- Total length of hospital stay (days)
- Operative time (min)
Technique
Patient is placed in supine position with split legs. The table is usually kept in reverse Trendelenberg’s position with tilt maneuverability. The operating surgeon stands between legs of the patient, while the camera surgeon is standing on right and staff nurse on left of the patient. Assistant surgeon changes his/her position according to need. Monitor is kept at head end of the patient.
We use close technique of creating pneumoperitoneum using Veress needle. Camera port is placed above umbilicus and toward right of the midline. Umbilicus is usually avoided in view of possible trauma to umbilical vein, which is usually recanalized due to elevated portal pressure in cirrhotic patients. Right hand working port (12 mm) is placed in epigastric region and left hand working port (5 mm) placed in right mid-clavicular line about 2 cm below the costal margin. Additionally, two more retraction ports (5 mm) are placed, one in right anterior axillary line and the other in left para-rectal line midway between epigastric and supra-umbilical ports. Port placement is shown in Fig. 1. Insufflation pressure is kept at 12 mmHg.
Fig. 1.
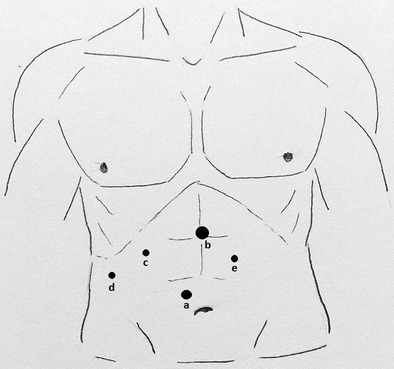
Port placement: a Camera port (10 mm) supra-umbilical slightly on right side, b right hand working port (12 mm) in epigastric region, c left hand working port (5 mm) in right mid-clavicular line about 2 cm below the costal margin, d retraction port (5 mm) in right anterior axillary line, and e retraction port in left para-rectal line midway between epigastric and supra-umbilical ports
After thorough survey of peritoneal cavity for signs of unresectable disease, we proceed with hepatic resection. We use modified anterior approach. First, falciform and round ligaments are divided using harmonic scalpel (Ethicon endo-surgery, Cincinnati, USA) or ligasure (Valleylab, Boulder, CO). Separation of falciform ligament from anterior abdominal wall is extended cranially to expose supra-hepatic, infra-diaphragmatic inferior vena cava (IVC). The divided end of the round ligament is then used to give cranial traction on liver so that porta hepatis and inferior surface of liver become clearly visible. Triangular and the coronary ligaments of the concerned side are divided last after parenchymal transection and division of hepatic veins. This maneuver of dividing these ligaments lastly helps in providing the necessary counter traction and support to liver during parenchymal division.
The next step is inflow control which is achieved by porta hepatis dissection. The liver is cranially retracted, and porta is clearly made out. Sometimes, downward retraction of duodenum is necessary to have proper exposure of porta. The peritoneal reflection along the free border of lesser omentum is incised and dissected so as to expose the common bile duct, portal vein, and hepatic artery. The cystic duct and artery are dissected in Calot’s triangle, clipped, and divided. The divided gall bladder is then used to retract liver cranially. As the dissection proceeds toward hilum, the right and left branches of portal vein and hepatic artery are identified. We generally follow extra-hepatic dissection to achieve inflow control. The concerned hepatic artery is divided first after ligating it doubly with silk suture or applying plastic locking clips (Hem-o-lok; Teleflex Medical, Research Triangle Park, NC). Next, portal vein branch is dissected and divided using vascular stapler (White cartridge, Endo GIA, Covidien, Mansfield, MA; Echelon Endopath Stapler, Ethicon Endo-Surgery). Alternately, if there is no space to apply stapler, we ligate the portal vein branch doubly using silk suture and then divide (Figs. 2 and 3). Concerned hepatic duct branches are divided during parenchymal transaction (Fig. 4). Branches to caudate lobe are carefully identified and preserved.
Fig. 2.
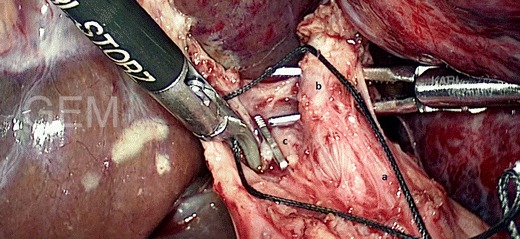
Hilar dissection in progress: a common hepatic artery, b left hepatic artery, and c clipped cystic artery origin from right hepatic artery (not visible in picture)
Fig. 3.
Hilar dissection in progress: a common hepatic duct, b left duct, and c left portal vein being transected
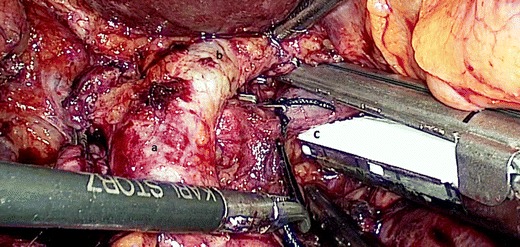
Fig. 4.
Closure of left ductal stump after parenchymal transection
Once portal supply is divided, color change becomes visible on liver surface (Fig. 5). At this stage, we reduce the insufflations pressure to 8–10 mmHg to reduce the risk of gas embolism. The transection line is marked along the liver capsule with mono-polar diathermy or harmonic scalpel. After placing stay sutures on either side of transaction line along inferior border of liver for retraction, liver parenchyma is divided for depth of 5–10 mm using harmonic scalpel. For further parenchymal transection, we use harmonic hook with bipolar diathermy and ligasure. Divided parenchymal tissue is sucked through right lateral port using routine 5-mm suction cannula. Vascular and biliary structures more than 3 mm are ligated applying titanium clips. In this way, the parenchyma is divided along the entire plane from caudal to cranial and from anterior to posterior direction.
Fig. 5.
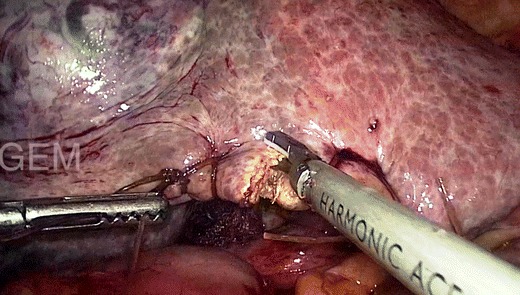
Beginning of parenchymal transection along the line of demarcation
The posterior Glisson’s capsule is now divided along the anterior surface of the vena cava while systematically clipping and dividing the small bridging veins. As the parenchymal division reaches the posterior surface of the liver, the major hepatic veins are encountered. Once the hepatic vein that is to be divided is visualized, it is dissected out clearly and its junction with IVC is identified. Vascular stapler is used to divide the hepatic vein concerned. Finally, triangular and coronary ligaments and diaphragmatic attachments are divided to complete resection. Specimen is placed in protective plastic retrieval bag and removed via Pfannenstiel incision. The fascial layers are re-approximated, the pneumoperitoneum is reintroduced, and the operative site is lavaged and examined for hemostasis and biliary tract integrity. We use argon plasma coagulator (APC) to control small ooze from cut surface of retained liver (Fig. 6). Closed drainage tube is placed in Morrison’s space, and ports are closed.
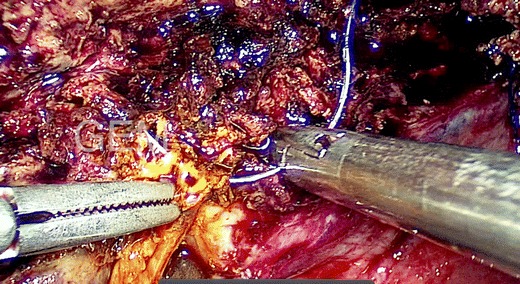
Fig. 6.
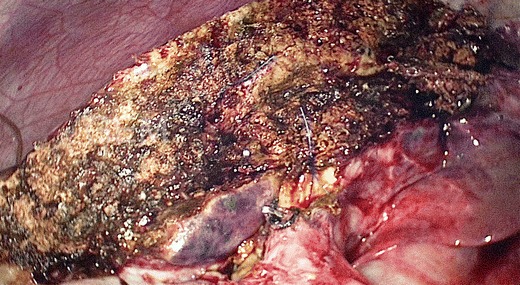
Remnant liver after parenchymal division
We do not routinely use the Pringle maneuver to control blood flow to the liver, but in selected cases, we have used selective extra-glissonian pedicle clamping with laparoscopic bulldog clamp for bleeding control.
Postoperatively, all patients were kept in ICU. Oral fluids were started after return of bowel activity, usually on first postoperative day and solids on next day. Liver enzymes, bilirubin, and coagulation parameters were accessed on daily basis. Drain was removed once output became minimal and nature becoming serous.
Statistical Analysis
All data were collected retrospectively by reviewing prospectively maintained medical records and electronic database. Variables studied include demographics, operative time and blood loss, transfusion requirements, requirement of inflow occlusion with time if applicable, conversion rate, and complications according to Clavien-Dindo classification.5 Postoperative variables like ICU and hospital stay, morbidity, and 90-days mortality along with detailed pathological analysis were included. It also includes early follow-up, readmissions, and re-interventions if applicable. GraphPad Prism 6 (GraphPad Software, Inc., CA, USA) was used for statistical analysis.
Results
Total 56 patients underwent total laparoscopic major hepatectomies out of which 34 were right-sided resections and 22 were involving left lobe. Indications and patient characteristics are shown in Table 1. Mean age of the entire cohort was 54.8 ± 15.3 years with male: female ratio of 1.5:1. Nineteen (33.9 %) patients underwent surgery for benign lesions, whereas 37 (66.0 %) patients had malignant lesions [hepatocellular cancer (HCC) 26, colorectal metastasis (CRM) 4, intrahepatic cholangiocarcinoma (ICC) 4, neuroendocrine tumors (NET) 3). Eleven patients (19.6 %) had cirrhosis due to various causes; however, all of them were classified as child A. Mean size of lesions was 6.0 ± 2.8 cm, while most of the lesions were single.
Table 1.
Patient characteristics and indications
| Sr. no | Demographic factors | |
|---|---|---|
| 1. | Age (years) | 54.8 ± 15.3 |
| 2. | Sex (M/F) | 34:22 (1.5:1) |
| 3. | Liver status (normal/CLD) | 45/11 |
| Indications | ||
| 4. | Hepatocellular carcinoma | 26 |
| 5. | Intrahepatic cholangiocarcinoma | 4 |
| 6. | Neuroendocrine tumor | 3 |
| 7. | Colorectal metastasis | 04 |
| 8. | Hemangioma | 11 |
| 9. | Biliary cystadenoma | 03 |
| 10. | Complex cyst | 05 |
| Tumor Character | ||
| 11. | Size (cm) | 6.0 ± 2.8 |
| 12. | Number (single/multiple) | 42/14 |
CLD chronic liver disease
All surgeries were performed by two senior surgeons of hepatobiliary surgery unit by following institutionally standardized approach and protocols. Mean operating time during the procedure was 227.4 ± 51.8 min, with mean blood loss of 265.5 ml ± 143.4 ml. Six patients required blood transfusion either in operating room or during immediate postoperative period. Extra-Glissonian Pringle’s maneuver (inflow control) was used in 11 patients with mean occlusion time of 34.0 ± 11.4 min. Although no untoward incidence of slipped ligature or clip happened during or after the procedures, US FDA has issued a warning regarding use of Weck Hem-O-Lok Ligating Clips for securing renal artery (http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm253237.htm). Three patients needed conversion to open approach, two in view of excessive bleeding, while one patient had extensive adhesion due to prior upper abdominal surgery; these cases were included in final analysis. Operative variables are summarized in Table 2
Table 2.
Operative variables
| Procedure | |
| Right hepatectomy | 34 |
| Left hepatectomy | 22 |
| Intra-operative | |
| Mean operating time (min) | 227.4 ± 51.8 |
| Mean blood loss (ml) | 265.5 ± 143.4 |
| Transfusion required | 6 (10.7 %) |
| Patients requiring inflow occlusion | 11 (19.6 %) |
| Conversion rate | 3 (5.3 %) |
Postoperative outcomes are described in Table 3. Median intensive care unit (ICU) stay during this study was 3 days (2–8 days). Overall complications were observed in 11 patients comprising liver-specific complications in seven along with wound infection in two, pleural effusion in one, and pneumonia with acute respiratory distress syndrome (ARDS) in one patient. Median hospital stay was 8 days (6–29). One patient died on 29th postoperative day due to bile leak, sepsis, and ARDS.
Table 3.
Postoperative outcomes
| Median ICU stay (days) | 3 (2–8) |
| Overall complications | 11 (19.6 %) |
| Liver-specific complications | 7 (12.5 %) |
| Ascites | 4 |
| Bleeding | 2 |
| Liver decompensation | 3 |
| Bile leak | 4 |
| Clavien-Dindo grade | |
| 1 | 3 |
| 2 | 4 |
| 3 | 3 |
| 4 | 0 |
| 5 | 1 |
| Median hospital stay (days) | 8 (6–29) |
| Re-admission | 5 (8.9 %) |
| Re-intervention | 3 (5.3 %) |
| 90-day mortality | 1 (1.7 %) |
| Mean resection margin (cm) | 2.1 ± 0.9 |
| <1-cm margin | 2 (5.4 %) |
Specimens resected were subjected to pathological examination by a single expert. Histological evaluation of specimen for malignant lesions (i.e., HCC, CRM, ICC, and NET) revealed a mean resection margin length of 2.1 ± 0.9 cm. Margin less than 1 cm (<1 cm) was reported in two patients.
During the early follow-up (90 days), five patients had readmissions for various reasons, out of which three required invasive intervention. First patient needed endoscopic decompression for persistent bile leak, another with biloma was managed with pig tail catheter drainage, and third one underwent secondary suturing for wound disruption.
Discussion
The experience and expertise gained during exponential growth of application of minimally invasive approach in various intra-abdominal procedures along with better transaction devices have helped to make laparoscopic liver resection a common entity worldwide today. Studies focusing on major liver resections by laparoscopic means are limited.6 – 9 The progress of LLR in Indian subcontinent is still in infancy with few case reports existing in literature.10 To our knowledge, this is the first and largest series from India till date and amongst the few in the world literature focusing on major LLR.
The hurdle for laparoscopic major liver resection lies with combined expertise needed in complex liver surgeries as well as advanced laparoscopy. Present study was conducted at tertiary level academic institution exclusively dedicated to gastrointestinal surgery and advanced laparoscopic procedures. The skills and experience achieved during other gastrointestinal and hepato-biliary procedures done earlier11 – 13 have profoundly contributed to shorten the learning curve for LLR. With the present study, authors would like to highlight certain aspects of LLR like technique, feasibility through total laparoscopic approach, safety, oncological completeness, and short-term complications.
Majority of the patients in the present study had malignant lesions (66.0 %). As most of the patients with benign lesions were offered either nonanatomical resections or segmental excisions, these were excluded from present analysis. The patients with concomitant liver cirrhosis were carefully selected, having CTP grade A, though, of late we started offering minimally invasive option to patients with early CTP grade B too. Of 26 patients with HCC, 11 had associated cirrhotic changes, while the majority of HCC occurred in normal livers. This is partly explained by high incidence of HCC in Asian subcontinent attributable to nonviral etiologies and equally significant number of hepatitis B virus (HBV) and hepatitis C virus (HCV) carriers.14 The mean size of lesions was 6 cm with largest being 13 cm and mostly was single, as multifocal lesions involving extended resections were excluded.
Of the 19 benign lesions, 11 were hemangiomas. Surgical option was exercised as most were giant in size, symptomatic, and few had rapid progression or exophytic pattern of growth making them vulnerable for rupture. Although enucleation remained the overall procedure of choice for most of hemangiomas during the same period, resection was favored in these patients owing to combination of factors like lesion occupying almost hemi-liver, planned ligation of arterial division supplying liver segments, and suspicion of malignancy. Five patients with final histology of complex cyst also underwent LLR mainly in view of atypical imaging findings like altered vascularity patterns and complex septations mimicking cancerous lesions, which otherwise hardly forms an indication for major hepatectomy.
The mean operating time in this study is 227.4 min, which is comparable to most of the published data.2 , 15 The important advantage of laparoscopic approach is reduction in blood loss. In our study, mean blood loss was 265.5 ml with transfusion required in 10.1 % of the patients. It is widely accepted today that the excess blood loss and transfusion are an independent prognostic markers for morbidity, perioperative outcome, mortality, and even recurrence after hepatectomy.16 – 18 The authors believe that the reduced blood loss in current study is mainly contributed by positive pneumoperitoneal pressure, careful patient selection, sound anatomical dissection, and judicious use of various transection and hemostatic devices. As mentioned earlier, we do not use routine inflow occlusion during parenchymal transaction. The cases mentioned were part of our initial experience as well as certain situations which mandated its use.
We had three conversions to open approach, constituting 5.3 %. Reported conversion rate for major hepatectomy worldwide varies considerably but approximately comes at 10.0 %.2 We had a little experience in assisted LLR or use of hand ports, as all completed LLR were by total laparoscopy. But, literature shows favorability of these assisted techniques in certain scenarios like assisted LLR for cirrhotics, with difficult tumor locations and in living donor hepatectomies. Hand assistance was particularly mentioned to be useful during initial learning curve.19 Authors would like to stress the importance of keeping low threshold for conversion at least during early experience, especially considering the amount of complexity involved along with required learning curve. It is advisable not to modify resection plan in view of retaining the approach for surgery.
In present study, median ICU stay is 3 days with hospital stay of 8 days and overall complications seen in 19.6 % patients with liver-specific complications in 12.5 % and early (90 days) mortality in 1.7 %. A study on major LLR by Dagher et al. has reported similar outcomes.8 The length of hospital stay has considerably improved over time at our center but still remains high compared to data from west, though comparable to studies from Asian subcontinent.20 We believe, in our scenario, that multiple factors are contributory like different sociocultural perspective of major surgery, approach/awareness toward disease, and majority of patients belonging to remote peripheral locations.
Using minimal invasive approach, we could achieve an excellent mean resection margin of 2.1 cm, with R0 resection in 95 % of the cases. LLR has also been reported to be equivalent or sometimes better in terms of attaining negative (<1 cm) margin in comparison with its open counterpart.15
Reported literature has shown many benefits of LLR approach with regard to postoperative pain, analgesic requirements, blood loss, and hospital stay while no difference in terms of morbidity, mortality, resection margin status, and overall survival.21 – 23 A review comparing benefits of LLRs with its open counterpart, comprising more than 2400 patients highlights advantages of LLR in terms of short-term outcomes, cost, and equivalent oncological clearance.20 Recently, the second international consensus conference held at Morioka supported the role of minor LLR as standard of care (IDEAL 3). It also emphasized a cautious introduction of major LLR, which still according to statement is an innovative procedure in phase of exploration (IDEAL 2b).24
Conclusion
Laparoscopic major hepatic resection requires considerable expertise in both advanced laparoscopy and liver surgery. It can be feasible, safe, and oncologically adequate in well-selected cases at experienced hands.
Acknowledgments
Conflict of Interest
None declared
References
- 1.Gagner M, Rheault M, Dubuc J. Laparoscopic partial hepatectomy for liver tumor. Surg Endosc. 1992;6:99. [Google Scholar]
- 2.Dagher I, Gayet B, Tzanis D, Tranchart H, Fuks D, Soubrane O, Han HS, Kim KH, Cherqui D, O'Rourke N, Troisi RI, Aldrighetti L, Bjorn E, Abu Hilal M, Belli G, Kaneko H, Jarnagin WR, Lin C, Pekolj J, Buell JF, Wakabayashi G. International experience for laparoscopic major liver resection. J Hepatobiliary Pancreat Sci. 2014;21(10):732–6. doi: 10.1002/jhbp.140. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen KT, Gamblin TC, Geller DA. World Review of Laparoscopic Liver Resection—2,804 Patients. Ann Surg. 2009;250(5):831–841. doi: 10.1097/SLA.0b013e3181b0c4df. [DOI] [PubMed] [Google Scholar]
- 4.The Terminology Committee of the IHPBA The Brisbane 2000 terminology of hepatic anatomy and resections. HPB. 2000;2:333–9. [Google Scholar]
- 5.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Rourke N, Fielding G. Laparoscopic right hepatectomy: surgical technique. J Gastrointest Surg. 2004;8(2):213–6. doi: 10.1016/j.gassur.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 7.Topal B, Aerts R, Penninckx F. Laparoscopic intrahepatic Glissonian approach for right hepatectomy is safe, simple, and reproducible. Surg Endosc. 2007;21(11):2111. doi: 10.1007/s00464-007-9303-z. [DOI] [PubMed] [Google Scholar]
- 8.Dagher I, O’Rourke N, Geller DA, Cherqui D, Belli G, Gamblin TC, Lainas P, Laurent A, Nguyen KT, Marvin MR, Thomas M, Ravindra K, Fielding G, Franco D, Buell JF. Laparoscopic major hepatectomy: an evolution in standard of care. Ann Surg. 2009;250(5):856–60. doi: 10.1097/SLA.0b013e3181bcaf46. [DOI] [PubMed] [Google Scholar]
- 9.Cardinal JS, Reddy SK, Tsung A, Marsh JW, Geller DA. Laparoscopic major hepatectomy: pure laparoscopic approach versus hand-assisted technique. J Hepatobiliary Pancreat Sci. 2013;20(2):114–119. doi: 10.1007/s00534-012-0553-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gadiyaram S, Shetty N. Laparoscopic resection of giant liver hemangioma using laparoscopic Habib probe for parenchymal transection. J Minim Access Surg. 2012;8(2):59–61. doi: 10.4103/0972-9941.95540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Senthilnathan P, Srivatsan Gurumurthy S, Gul SI, Sabnis S, Natesan AV, Palanisamy NV, Praveen Raj P, Subbiah R, Ramakrishnan P, Palanivelu C. Long-term results of laparoscopic pancreaticoduodenectomy for pancreatic and periampullary cancer-experience of 130 cases from a tertiary-care center in South India. J Laparoendosc Adv Surg Tech A. 2015;25(4):295–300. doi: 10.1089/lap.2014.0502. [DOI] [PubMed] [Google Scholar]
- 12.Senthilnathan P, Patel ND, Nair AS, Nalankilli VP, Vijay A, Palanivelu C. Laparoscopic Management of Choledochal Cyst-Technical Modifications and Outcome Analysis. World J Surg. 2015 Jun 12. DOI 10.1007/s00268-015-3111-8 [Epub ahead of print]. [DOI] [PubMed]
- 13.Senthilnathan P, Inamdar S, Nalankilli VP, Vijay A, Rajapandian S, Parthsarathi R, Raj P, Palanivelu C. Long-term results of hepatic hydatid disease managed using palanivelu hydatid system: Indian experience in tertiary center. Surg Endosc. 2014;28(10):2832–39. doi: 10.1007/s00464-014-3570-2. [DOI] [PubMed] [Google Scholar]
- 14.Venook AP, Papandreou C, Furuse J, de Guevara LL. The incidence and epidemiology of hepatocellular carcinoma: a global and regional perspective. Oncologist. 2010;15(4):5–13. doi: 10.1634/theoncologist.2010-S4-05. [DOI] [PubMed] [Google Scholar]
- 15.Mirnezami R, Mirnezami AH, Chandrakumaran K, Abu Hilal M, Pearce NW, Primrose JN, Sutcliffe RP. Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB (Oxford) 2011;13(5):295–308. doi: 10.1111/j.1477-2574.2011.00295.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kooby DA, Stockman J, Ben-Porat L, Gonen M, Jarnagin WR, Dematteo RP, Tuorto S, Wuest D, Blumgart LH, Fong Y. Influence of transfusions on perioperative and long-term outcome in patients following hepatic resection for colorectal metastases. Ann Surg. 2003;237(6):860–869. doi: 10.1097/01.SLA.0000072371.95588.DA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shiba H, Ishida Y, Wakiyama S, Iida T, Matsumoto M, Sakamoto T, Ito R, Gocho T, Furukawa K, Fujiwara Y, Hirohara S, Misawa T, Yanaga K. Negative impact of blood transfusion on recurrence and prognosis of hepatocellular carcinoma after hepatic resection. J Gastrointest Surg. 2009;13(9):1636–1642. doi: 10.1007/s11605-009-0963-y. [DOI] [PubMed] [Google Scholar]
- 18.de Boer MT, Molenaar IQ, Porte RJ. Impact of blood loss on outcome after liver resection. Dig Surg. 2007;24(4):259–64. doi: 10.1159/000103656. [DOI] [PubMed] [Google Scholar]
- 19.Lin NC, Nitta H, Wakabayashi G. Laparoscopic major hepatectomy: a systematic literature review and comparison of 3 techniques. Ann Surg. 2013;257:205–13. doi: 10.1097/SLA.0b013e31827da7fe. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen KT, Marsh JW, Tsung A, Steel JJ, Gamblin TC, Geller DA. Comparative benefits of laparoscopic vs open hepatic resection: a critical appraisal. Arch Surg. 2011 Mar; 146 (3):348-56. [DOI] [PubMed]
- 21.Reddy SK, Tsung A, Geller DA. Laparoscopic liver resection. World J Surg. 2011;35(7):1478–86. doi: 10.1007/s00268-010-0906-5. [DOI] [PubMed] [Google Scholar]
- 22.Xiong JJ, Altaf K, Javed MA, Huang W, Mukherjee R, Mai G, Sutton R, Liu XB, Hu WM. Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. World J Gastroenterol. 2012;18(45):6657–6668. doi: 10.3748/wjg.v18.i45.6657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tzanis D, Shivathirthan N, Laurent A, Abu Hilal M, Soubrane O, Kazaryan AM, Ettore GM, Van Dam RM, Lainas P, Tranchart H, Edwin B, Belli G, Campos RR, Pearce N, Gayet B, Dagher I. European experience of laparoscopic major hepatectomy. J Hepatobiliary Pancreat Sci. 2013;20:120–4. doi: 10.1007/s00534-012-0554-2. [DOI] [PubMed] [Google Scholar]
- 24.Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, OʼRourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schön MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J, Strasberg SM. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261(4):619–29. doi: 10.1097/SLA.0000000000001184. [DOI] [PubMed] [Google Scholar]


