Abstract
Smoke inhalation leads to acute lung injury (ALI), a devastating clinical problem associated with high mortality rates. Suppressor of cytokine signaling-1 (SOCS-1) is a negative regulator of proinflammatory cytokine signaling. We have found that adenoviral gene transfer of SOCS-1 ameliorates smoke inhalation-induced lung injury in C57BL/6 mice. We also found that the release of adenosine triphosphate (ATP) was increased post smoke exposure, while oxidized ATP, an inhibitor of purinergic P2X7 receptor, suppressed smoke-induced NALP3 inflammasome assembly, caspase-1 activation, and K+ efflux. Similar to oxidized ATP, high protein level of SOCS-1 dampened the formation of NALP3 inflammasome and the activation of caspase-1 and IL-1β induced by smoke exposure in mouse alveolar macrophages. In conclusion, SOCS-1 relieves smoke inhalation-induced pulmonary inflammation and injury by inhibiting NALP3 inflammasome formation.
KEY WORDS: smoke-induced ALI, SOCS-1, NALP3 inflammasome, ATP, K+, P2X7
INTRODUCTION
Each year, burn-related injuries result in nearly 265,000 deaths globally and 3500 deaths in the USA. Ninety percent of burn-related mortality can be partially attributed to smoke inhalation-associated acute lung injury (SI-ALI). Despite advances in care and rehabilitation of patients with burns, SI-ALI-related mortality remains substantial at 21.3% in 2015 [1]. Smoke inhalation is the leading cause of acute lung injury (ALI), acute respiratory distress syndrome (ARDS), and serious respiratory failure. ALI/ARDS is also a significant clinical problem with no drug treatment currently approved by the Food and Drug Administration. Because ALI/ARDS patients entering the intensive care unit often have already developed clinical diseases, therapeutics targeting not only the initiation but also the propagation of ALI/ARDS is necessary. Therefore, understanding the molecular mechanisms of smoke-induced lung injury can help the treatment of ALI/ARDS. Yet, despite decades of intense research, the molecular mechanisms involved in the pathogenesis of smoke inhalation-induced ALI are poorly understood.
Smoke directly destroys endothelial and epithelial barrier function and aggregates mucous with sloughed airway epithelium and cellular debris, leading to airway obstruction, change in regional blood flow, increased airway microvascular permeability, exfoliation of epithelial lining, enhanced surfactant denaturation, and toxin/cytokine-mediated inflammation [2–5].
The most abundant non-parenchymal cell in the lung is alveolar macrophage, which plays a central role in maintaining normal lung structure and function in both the maintenance of immunological homeostasis and host defense [6, 7]. The inflammatory responses triggered by direct or indirect insults to the lung involve the recruitment and activation of tissue macrophages in the lung parenchyma of ALI/ARDS. Macrophages can be rapidly activated by burn injury to release proinflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α) and interleukin-1beta (IL-1β), and may therefore play important roles in burn-induced ALI [8, 9]. IL-1β is known as one of the most potent inflammatory initiating cytokines observed in patients suffering from ALI [7]. Macrophage depletion improves alveolar barrier dysfunction and lung inflammatory response caused by severe burns [10].
Suppressor of cytokine signaling 1 (SOCS-1) is a member of the cytokine signaling pathway inhibitor family, which is known as a potent negative regulator of proinflammatory cytokine signaling [11, 12]. SOCS-1 is characterized by the presence of an N-terminal proline rich domain called the central Src homology 2 (SH2) domain and a C-terminal conserved motif named the SOCS box [13]. The SOCS box can couple with SH2 domain-binding proteins to activate ubiquitin-proteasome pathway and thus function as a negative regulator of cytokine signaling [14, 15]. SOCS-1 deletion causes fatal inflammation, which can be rescued by deletion of IFNG [16]. Previously, findings indicate that SOCS-1 is critical in macrophages for preventing uncontrolled inflammation [17]. In LPS-induced ALI, downregulation of SOCS-1 by alveolar macrophages-derived miR-155, which is a proinflammatory factor blinding to 3’-UTR of SOCS-1, remarkably exaggerates lung inflammation [18]. Increased expression of Ad-SOCS-1 has been shown to protect lung from hyperoxic injury by suppressing IL-1β levels [19]. Ad-SOCS-1-infected murine exhibits a lower degree of lymphocytic inflammation and pulmonary fibrosis as well as a diminished mortality after bleomycin treatment [20]. However, the role of SOCS-1 in inflammation during smoke inhalation-induced ALI has not been revealed.
NALP3 inflammasome is a multiprotein oligomer formed by NALP3, apoptosis-associated speck-like protein containing a CARD (ASC), and pro-caspase-1. NALP3 also participates in the pathogenesis of ALI [21, 22]. ATP, an NALP3 agonist, acts on P2X7 purinergic receptor (P2RX7) to alter the permeability of the cell membrane, which results in cytosolic K+ efflux and the collapse of cation gradient [23]. A drop in cytosolic K+ level is a common and sufficient trigger for NALP3 inflammasome assembly and caspase-1 activation [24]. In response to the rising outflow of K+, the assembly of ASC specks, which are large multimeric complexes predominantly composed of dimers and oligomers of ASC, is activated. This allows pro-caspase-1 to be recruited and starts the autocatalytic event that ultimately leads to the formation of active caspase-1 heterotetramers and the conversion of inactive cytosolic pro-IL-1β to the functional form [24–27]. Recent in vitro experiment using alveolar macrophages (AMs) indicates that ROS-mediated NLRP3 inflammasome plays an essential role in burn-induced ALI [7]. Other studies suggest that SOCS-1 may suppress the activity of NALP3, resulting in attenuated encephalomyelitis (EAE) pathogenicity [28].
We therefore hypothesize that SOCS-1 exhibits important effects on smoke inhalation-induced ALI through an anti-inflammatory mechanism. To test our hypothesis, C57BL/6 mice were infected with Ad-SOCS-1 or Ad-GFP by microsprayer. Then, the degree of lung damage and the survival rates were examined after smoke inhalation. Furthermore, to reveal the anti-inflammatory mechanism of SOCS-1, we studied both the activation process of the NALP3 inflammasome assembly in response to smoke exposure and the inhibitory action of SOCS-1 on smoke-induced NALP3 inflammasome assembly, caspase-1 activation, and IL-1β expression.
MATERIALS AND METHODS
Animals
C57BL/6 male mice aged 6–8 weeks were obtained from the Zhejiang Academy of Medical Sciences. All animals were maintained under specific pathogen-free conditions.
Smoke Inhalation
Smoke inhalation was administered as previously described [29]. After induction of anesthesia with 5% chloral hydrate 0.01 ml/g (Tianjin Dingshengxin Chemical Industry Co., Ltd., China), mice were briefly placed in the smoke chamber, which was filled with smoke from 300 mg of smoldering cotton heated to 400 °C, for 15 min. During smoke exposure, the temperature in the smoke chamber did not exceed 40 °C to prevent thermal injury to the airways. All mice were returned to the cages for recovery, which was recorded as day 0. During the experimental period, mice were allowed free access to food and water.
Isolation of Mouse Lung Macrophages
Mice were euthanized to collect lung macrophages. Lungs were perfused at 37 °C with 1 ml of cold normal saline (NS) 15 times. Lung tissue was placed on a culture plate containing cold RPMI 1640 and then chopped. Cell suspension was filtered twice by a 75-μm steel mesh. Lung macrophages were centrifuged with sterile water to destroy red blood cells. Cells were washed with RPMI 1640. The suspension was then placed in lymphocyte separation medium and centrifuged to obtain lung macrophages.
Smoke Exposure to Lung Macrophages
The experimental method is similar to smoke inhalation [30]. Briefly, after isolation of mouse lung macrophages, cells were cultured in six well plates overnight. During smoke exposure, the temperature in the smoke chamber was maintained at 37 °C. The smoke was introduced to the cells at a flow rate 25 ml/min using an air sampling pump for 30 min. After completion of the exposure period, the cells were washed using 1 × PBS, and added into the new culture medium with 10% FCS with 5% CO2 in an incubator at 37 °C for 24 h. Cells were digested and collected for subsequent experiments.
Lung Histology
Twenty-four hours after smoke exposure, the mice were sacrificed and the lungs were collected. Each lung was fixed in 10% formalin and embedded in paraffin. The fixed lungs were then sectioned at 4 μm of thickness, and the tissue was dewaxed in ethanol, rehydrated, and stained with hematoxylin and eosin.
Adenoviral Vectors
Adenoviral expression vector carrying the coding sequences of the mouse SOCS-1 gene (Ad-SOCS-1) were from ABM Inc. (Richmond, CANADA). Primers were designed and synthesized by TIANGEN BIOTECH (BEIJING) Co., Ltd. SOCS-1 sense: 5’-CACGCACTTCCGCACATTCC-3′; SOCS-1 antisense: 5’-TCCAGCAGCTCGAAGAGGCA-3′. Briefly, total RNA was extracted from C57BL/6 mouse liver tissue by Trizol RNA extraction kit (Invitrogen, US). RT-PCR (Thermo Fisher Scientific, US) was used to obtain mSOCS-1 cDNA by PrimeScript®RT reagent Kit with gDNA Eraser (Takara, Japan). The mSOCS-1 cDNA was cloned into a multicloning site of pHMCMV10. The pAdHM4-SOCS-1 was constructed by ligation of I-CeuI/PI-SceI-digested pAdHM4 and I-CeuI/PI-SceI-digested pHMCMV10-mSOCS-1. To generate the virus, pAdHM4-SOCS-1 was digested with PacI and purified by phenol-chloroform extraction and ethanol precipitation. Linearized DNAs were transfected into HEK-293 cells with Lipofectamine™ 2000 (Invitrogen, US) according to the manufacturer’s instructions. The viruses were amplified in HEK-293 cells. Before virus purification, cell lysates were centrifuged to remove cell debris and digested for 30 min at 37 °C with 200 μg/ml DNase I and 200 μg/ml RNase A in the presence of 10 mM MgCl2. Viruses were purified by CsCl2 step gradient ultracentrifugation followed by CsCl2 linear gradient ultracentrifugation. The purified viruses were dialyzed against a solution containing 10 mM Tris-HCl (pH 7.5), 1 mM MgCl2, and 10% glycerol. They were then stored at − 80 °C. Viral particle (VP) and biological titers were determined by a spectrophotometrical method and by using an Adeno-X Rapid Titer kit (BD Clontech, US), respectively. The ratios of the biological-to-particle titer were 1:12 and 1:7 for Ad-SOCS-1 and Ad-GFP (control), respectively.
Immunoblotting
Lung tissue lysates or cell extracts were electrophoresed on SDS-PAGE gels (Bio-rad, China) and transferred to polyvinylidene difluoride (PVDF) membranes (Millipore, US). The membranes were washed in 1 × PBS Tween-20 for 20 min and blocked with 5% fat-free milk at room temperature for 2 h. Then they were incubated with SOCS-1 antibody, NALP3, ASC, caspase-1, active caspase-1, or GAPDH antibody (Abcam, China) in TBST containing 5% fat-free milk at 4 °C overnight on a gentle shaker. After washing with 1 × PBS Tween-20 for 20 min, the membranes were incubated with the appropriate secondary antibody (Abcam, China) in TBST containing 3% fat-free milk at room temperature for 2 h according to manufacturer’s instruction. Proteins were detected by ECL chemiluminescence (GE, Healthcare, China).
Immunoprecipitation
Immunoprecipitation was performed using the MPER™ immunoprecipitation kit (Pierce Biotechnology, US). Five hundred micrograms of protein lysate from alveolar macrophages were incubated with anti-NALP3 or anti-ASC antibody (3–5 μg) at 4 °C overnight with rocking. The immune complexes were allowed to bind to 40 μL of Recombinant Protein G Agarose beads (Invitrogen, USA) at 4 °C for 2 h, and the beads were washed three times with lysis buffer. After centrifugation, the supernatants were obtained as immunoprecipitates and dissolved in SDS-PAGE sample buffer for electrophoresis and immunoblot analysis.
Quantification of ATP in Cell Culture Supernatant
Quantification of ATP was determined by ATP Determination Kit (Thermo Fisher, US). The concentration of extracellular ATP was determined by the culture supernatant. One hundred microliters per well recombinant firefly luciferase (LLR) was added, and the solution was shaken gently. The transmitted light was detected with a luminometer (BioSystems 20/20 luminometer, TURNER), and fluorescence intensity was measured continuously for 5 min [31].
Quantification of K+ Concentration
Macrophages were seeded at a density of 1 × 106 cells per well in 12-well tissue culture dishes and maintained for 24 h. The next day, media were collected at the indicated time points, and cells were washed once with phosphate-buffered saline. Cells were lysed in 1 ml of 10% nitric acid. The extracellular (medium) and the intracellular K+ content was quantified using atomic absorbance spectroscopy [32].
Statistical Analysis
Data are expressed as mean ± SEM from three or more independent experiments. When comparing between three or more groups, differences were tested using one-way analysis of variance followed by the Bonferroni test. When comparing between two groups, we used a Student’s paired two-tailed t test.
RESULTS
Increased Survival in Ad-SOCS-1 Mice After Smoke Inhalation
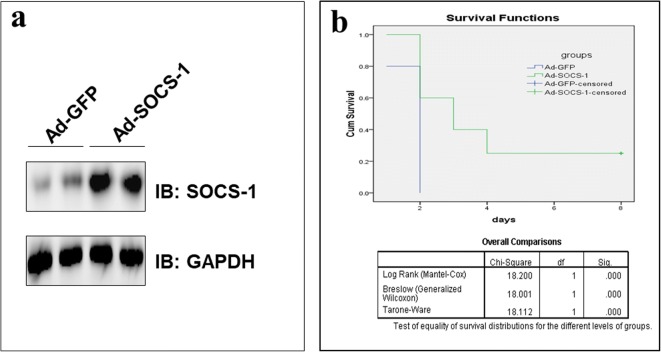
Ad-SOCS-1 or Ad-GFP (1 × 108 PFU/mouse) was delivered to C57BL/6 mice lung by a microsprayer (Penn-Century, US). Mice lungs and survival were examined after smoke exposure. The overexpression of SOCS-1 was confirmed in mice lungs 72 h after Ad-SOCS-1 infection by western blot (Fig. 1a). The results showed that transfection of SOCS-1 was successful, and the expression of SOCS-1 in the lung of the Ad-SOCS-1 group was significantly higher than that in Ad-GFP group.
Fig. 1.
Prolonged survival after smoke exposure in Ad-SOCS-1-treated mice. Ad-GFP or Ad-SOCS-1 was administered to mice lungs, and whole-lung homogenates were assessed for SOCS-1 expression by western blot 3 days later (a). After 15 min of smoke inhalation, mice survival was monitored for up to 8 days by using Kaplan-Meier method and analyzed by log-rank test (n = 20 in each group, P < 0.01 vs. the ad-GFP group) (b).
After 15 min of smoke inhalation, mice survival was monitored for up to 8 days. Three days after smoke inhalation, all Ad-GFP-administered mice died, while 60% of Ad-SOCS-1-administered mice still lived. Twenty-five percent of Ad-SOCS-1-administered mice even survived up to 8 days, at which point they were sacrificed (Fig. 1b). The results show that the high expression of SOCS-1 in vivo can significantly improve the survival rate of mice with smoke-induced lung injury.
Ad-SOCS-1 in Mice Relieved Smoke-Induced Acute Lung Injury
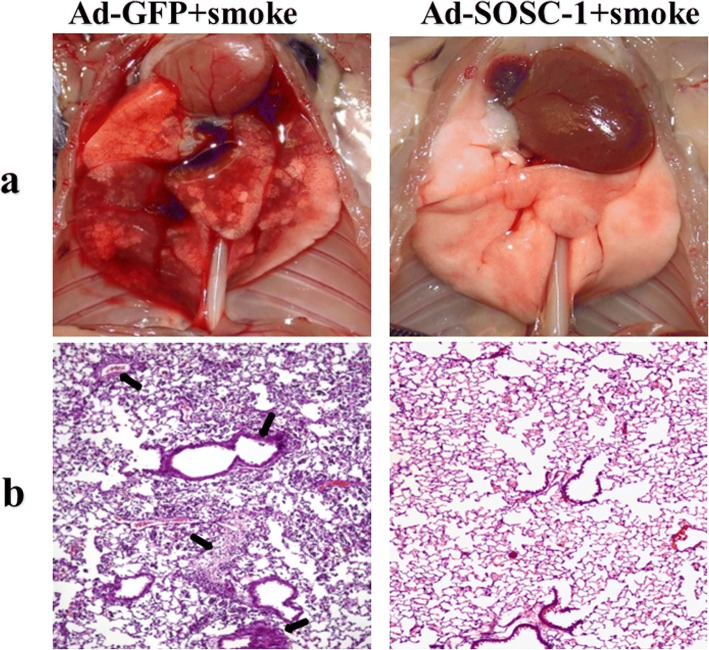
After exposure to smoke for 15 min and a day of rest, mice were sacrificed to observe the degree of lung injury in each group. Ad-GFP mice had obvious lung tissue injury after smoke exposure: lung tissues appeared darkly red with a volume expansion, and lung surface was moist with increased exudation; diffuse hyperemia and edema were visible, and congestion was obviously in some lung tissues. Conversely, in Ad-SOCS-1 mice, lung tissues appeared pink with a smooth and rosy surface; no blood, bleeding spots, congestion, or edema was observed. There was an obvious reduction in lung injury (Fig. 2a). The results showed that compared to Ad-GFP-infected mice, Ad-SOCS-1-infected mice appeared to have a lower level of lung tissue damage. Thus, SOCS-1 overexpression significantly reduces lung injury caused by smoke inhalation.
Fig. 2.
Reduced degree of smoke inhalation-induced lung injury in Ad-SOCS-1-treated mice. Mice infected with Ad-GFP or Ad-SOCS-1 were exposed to smoke for 15 min. After 1 day, a the degree of lung injury was observed in each group, and b lung tissue sections stained by H&E were observed to study morphological alternation (magnification ×400).
To further demonstrate that SOCS-1 overexpression can significantly reduce lung injury caused by smoke inhalation, lungs were isolated and lung tissue sections were stained by H&E after infection with or without smoke exposure. Mice were exposed to smoke for 15 min and sacrificed 1 day later. Under optical microscope, in the Ad-GFP mice, the capillaries in the alveolar walls showed swelling and were congested with many red blood cells. Alveolar epithelial cells were edematous. There was visible neutrophil and monocyte infiltration in the pulmonary interstitium. Hemorrhage in the alveolar spaces was found as well. On the contrary, in the Ad-SOCS-1 mice, the lung tissues in the specimens were clear and integral. The alveolar septum was thin and the wall was smooth. There was rarely neutrophil and monocyte infiltration observed in spaces (Fig. 2b). The results showed that Ad-SOCS1 mice exposed to toxic smoke had a marked decrease in immune cells infiltration. It is confirmed that SOCS-1 overexpression can significantly reduce smoke inhalation-caused lung injury.
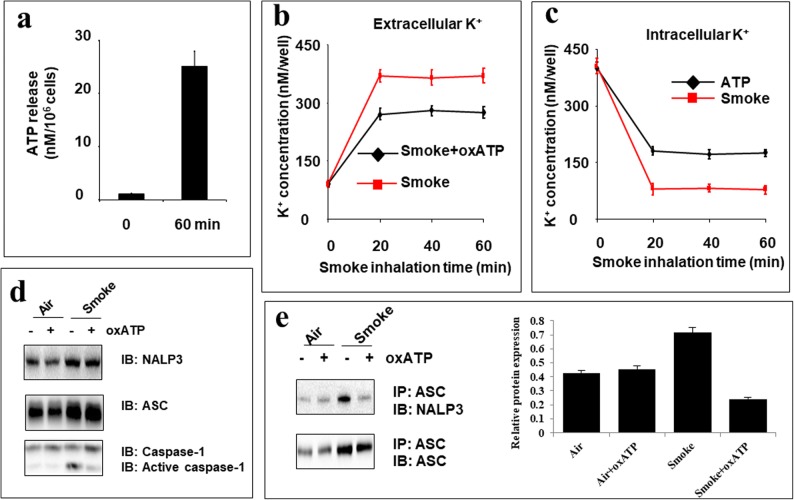
Smoke Promoted NALP3 Formation and Caspase-1 Activation via P2RX7
ATP activates the NALP3 inflammasome through P2X7 receptor mediated K+ efflux [32, 33]. To determine whether smoke exposure affects ATP, an important activator of NALP3, alveolar macrophages isolated from non-infected mice lungs were treated with or without smoke for 30 min, and the extracellular concentration of ATP was analyzed 60 min after the end of smoke treatment. Compared to non-treated macrophages, smoke-treated macrophages displayed a significant upsurge in ATP release of approximately 25 ± 2.01 nM/106 cells (Fig. 3a).
Fig. 3.
The requirement of P2RX7 in smoke exposure-induced NALP3 inflammasome assembly and caspase-1 cleavage. Alveolar macrophages were isolated from C57BL/6 mice, treated with or without oxATP, exposed to smoke for 30 min, and then analyzed for a ATP release, b extracellular, and c intracellular K+ levels, d expression of inflammasome components NALP3, ASC, and caspase-1, and e the complex formed by NALP3 and ASC. The intensity of the signals were quantified by ImageJ software for more strict and direct viewing to reflect the interaction between ASC and NALP3 (e).
To determine whether smoke affects cytoplasmic K+ level, we detected both extracellular and intracellular K+ concentrations up to 60 min after smoke exposure by atomic absorption flame photometry with or without oxidized ATP (oxATP), a P2RX7 antagonist, and observed that oxATP reduced smoke-induced K+ efflux (Fig. 3b, c). Before exposure to smoke, the extracellular K+ baseline level of macrophages was 100 nM/well (Fig. 3b), and the intracellular K+ baseline level was 400 nM/well (Fig. 3c). After exposure to smoke, there was about an 80% decrease in the intracellular K+ concentration, while the extracellular K+ level was surged to 400 nM/well. The depletion of cytoplasmic K+ was detected within 20 min and was maintained for 60 min after inhalation of smoke. These results show that smoke-induced K+ efflux through interacting with P2RX7 (Fig. 3b, c).
To determine whether P2RX7 is required for smoke-induced inflammasome activation, isolated macrophages were pretreated with oxATP and exposed to smoke or air for 30 min. Immunoblotting revealed that smoke significantly increased the protein level of NALP3, ASC, and cleaved caspase-1. OxATP reduced smoke-mediated caspase-1 activation but not smoke-induced NALP3 and ASC expression (Fig. 3d). Immunoprecipitation of cell lysates with anti-ASC antibody and the quantifications of relative protein expression analyzed by the intensity of the signals affirmed that oxATP suppresses the interaction between ASC and NALP3 enhanced by smoke (Fig. 3e). This indicates that P2RX7 is a necessary component of smoke-increased NALP3 inflammasome assembly (Fig. 3d, e).
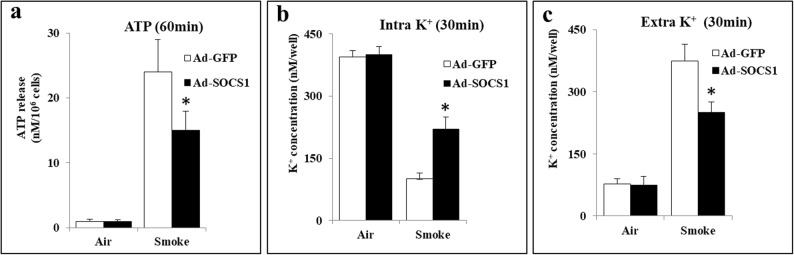
SOCS-1 Constrained Smoke-Induced NALP3 Inflammasome Assembly
To determine whether SOCS-1 reduces ATP and K+ efflux induced by smoke, alveolar macrophages isolated from Ad-SOCS-1 mice lungs were treated with or without smoke for 30 min, and the extracellular concentration of ATP was analyzed 60 min after the end of smoke treatment. Macrophages from the lungs of Ad-SOCS-1 mice showed a significant decrease in ATP release compared to Ad-GFP mice alveolar macrophages (Fig. 4a). We also detected both extracellular and intracellular K+ concentrations up to 30 min after smoke and observed that macrophages from Ad-SOCS-1-infected mice exhibited a lower degree of K+ efflux than those from Ad-GFP-infected mice (Fig. 4b, c).
Fig. 4.
Negative regulation of SOCS-1 on smoke-induced ATP and K+ efflux. Ad-GFP or Ad-SOCS-1-treated mice were exposed to smoke for 15 min and allowed to rest for 1 day. Isolated alveolar macrophages were analyzed for a ATP release and b intracellular and c extracellular K+ levels.(P < 0.01 vs. the Ad-GFP group).
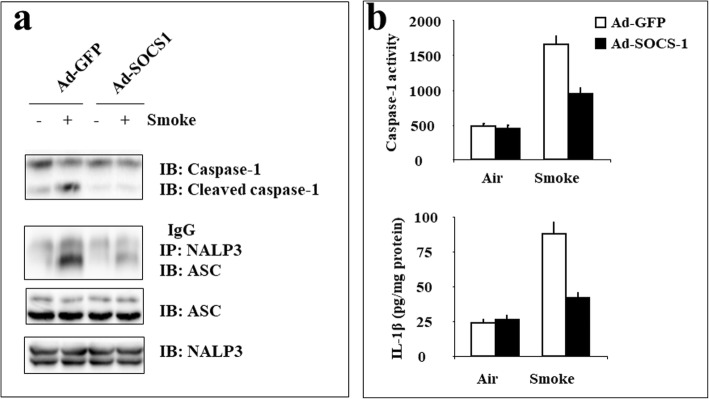
To test whether SOCS-1 exerts anti-inflammatory effect through inhibition of NALP3 inflammasome formation and consequent activation of caspase-1 and IL-1β, Ad-GFP, or Ad-SOCS-1-adminstered mice were exposed to smoke for 15 min and euthanized 1 day later to collect alveolar macrophages. Immunoblotting indicated that overexpression of SOCS-1 helped macrophages resist smoke-enhanced caspase-1 cleavage. Additionally, the amount of ASC protein pulled down with NALP3 was detected after immunoprecipitation with anti-NALP3 antibody. The results indicate that SOCS-1 repressed smoke-induced interaction between NALP3 and ASC (Fig. 5a).
Fig. 5.
Negative regulation of SOCS-1 on smoke-induced NALP3 inflammasome assembly, caspase-1 activation, and IL-1β expression. Ad-GFP or Ad-SOCS-1-treated mice were exposed to smoke for 15 min and allowed to rest for 1 day. Isolated alveolar macrophages were analyzed for a NALP3 inflammasome assembly and b caspase-1 activity and IL-1β secretion.
We also explored caspase-1 activity and IL-1β level by enzyme-linked immunosorbent assay (ELISA) and found that compared to the macrophages in smoke-treated Ad-GFP-infected mice, the macrophages in smoke-treated Ad-SOCS-1-infected mice had lower levels of both caspase-1 activity and IL-1β secretion (Fig. 5b). Our study demonstrates that SOCS-1 obstructs smoke-activated NALP3 inflammasome assembly, caspase-1 cleavage, and IL-1β secretion.
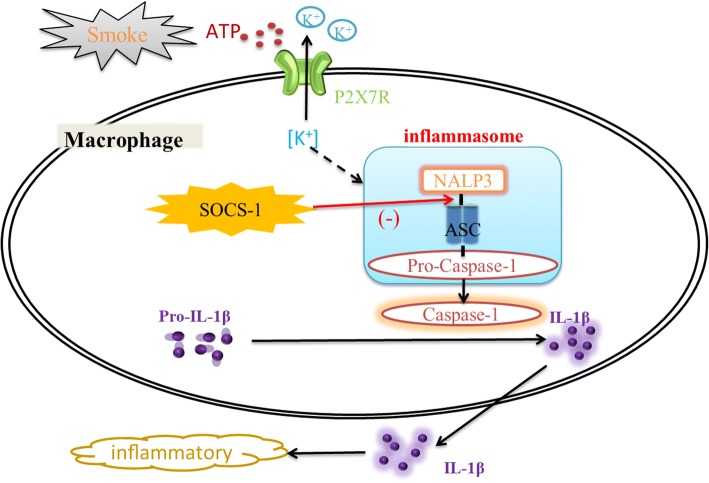
DISCUSSION
This study aims to identify the role of SOCS-1 in smoke inhalation-induced ALI. The results reveal that SOCS-1 attenuates ALI resulting from smoke exposure by suppressing macrophage-mediated inflammation. Adenovirus-mediated transfer of SOCS-1 to mice attenuates smoke exposure-induced ALI and improves the survival of mice. Additionally, smoke-enhanced ATP release promotes NALP3 inflammasome formation and caspase-1 activation through the stimulation of P2RX7-mediated K+ efflux. Finally, adenoviral gene transfer of SOCS-1 blocks ATP and K+ efflux to diminish NALP3 inflammasome assembly, caspase-1 activation, and IL-1β expression prompted by smoke in macrophages (Fig. 6).
Fig. 6.
Model of suppression of SOCS-1 to smoke-induced NALP3 inflammasome activation in alveolar macrophage. Smoke-enhanced ATP release promotes NALP3 inflammasome formation and caspase-1 and subsequent IL-1 activation through the stimulation of P2RX7-mediated K+ efflux. SOCS-1 interacts with NALP3 and ASC to diminish NALP3 inflammasome assembly, caspase-1 activation, and IL-1β expression prompted by smoke in macrophages.
Previous reports indicate that SOCS-1 plays an important role in preventing inflammation. SOCS-1 is critical for preventing lethal inflammation in T cells and macrophages, and deficiency of SOCS-1 results in spontaneous inflammation [17]. SOCS-1 in adaptive immune cells inhibits antiviral immunity, and its presence in innate/stromal cells is responsible for aggravated lung damage [34]. SOCS-1-deficient mice die within 3 weeks of birth with severe inflammation and lung damage through infiltration of inflammatory cells [20]. Compared to control mice, mice with overexpression of SOCS-1 exposed to hyperoxia show a significant amelioration in inflammation and alveolar damage [35]. As is shown in our results and other reports, smoke exposure can lead to ALI and result in inflammation and alveolar damage [36, 37]. Mice with Ad-GFP exposed to smoke all died within 3 days and the lung tissue showed lung tissue damage and immune cells invasion. However, survival rates and these pathological changes were significantly ameliorated in Ad-SOCS-1 mice. Galam et al. show that SOCS-1 overexpression inhibits ASK-1 and suppresses IL-1β levels to restore lung tissue in HALI [19]. Therefore, we speculate that ASK-1 may participate in inflammation of lung injury induced by smoke and interact with SOCS-1 in this process.
NALP3 inflammasome is activated and the inflammatory cascade is triggered with subsequent fibrosis in crystalline silica-induced lung injury [38]. Bleomycin-induced inflammation and fibrosis of ALI also require activation of NALP3 [39]. Using the mouse model of hemorrhagic shock (HS) in the lungs, HS activates lung endothelial NAD(P)H oxidase through high mobility group box 1 (HMGB1) to induce the production of reactive oxygen species (ROS). ROS then promotes association of thioredoxin-interacting protein (TXNIP) with NALP3 and subsequent activation of inflammasome and IL-1β secretion [40]. NALP3 inflammasome formation and IL-1β cleavage are induced by hyperoxia both in vivo and in vitro [32, 33, 41, 42]. In the hyperoxia-induced lung injury mice model, hyperoxia can induce ATP efflux. The elevated extracellular ATP interacts with P2X7 receptors, causing K+ efflux and activation of NALP3 inflammasome [43]. Likewise, our results show that smoke-induced ATP promotes inflammasome formation and caspase-1 activation through stimulation of P2X7 receptor-induced K+ efflux. Previous study investigating the effect of NALP3 on an inflammatory disease, EAE, demonstrates that IFNAR (the shared receptor for IFN-α and IFN-β) signaling in macrophages induces SOCS-1-mediated ubiquitination and degradation to decrease the production of mitochondrial ROS, resulting in inhibition of NALP3 inflammasome activity [28]. Our results indicate that SOCS-1 reduces NALP3 inflammasome formation through repression of the smoke-induced interaction between NALP3 and ASC, which thereby inhibits caspase-1 and IL-1β activated by NALP3. Recent reports also indicate that Cobalt protoporphyrin induces COX-2 expression by activation of P2X7 receptors, ASK-1/MAP kinases, and STAT-1 degradation signaling pathways [44]. Therefore, there may be a relationship between ASK-1 and P2RX7 that leads to the formation of NALP3 in smoke-induced ALI, which we will further investigate in the future.
In summary, SOCS-1 significantly ameliorates smoke-induced ALI. The protective mechanism of SOCS-1 from smoke-induced ALI is associated with a reduction in inflammation. These studies are the first to demonstrate that SOCS-1 is a critical regulator of smoke inhalation-induced ALI and a key mediator in inflammation protection. SOCS-1 may lead to the discovery of anchor points for new treatment strategies for smoke-induced ALI.
Funding Information
This study is supported by the National Natural Science Foundation of China (No.81470004) and Zhejiang Natural Science Foundation of China (LY18H010009) for their financial supports.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Kadri SS, Miller AC, Hohmann S, Bonne S, Nielsen C, Wells C, Gruver C, Quraishi SA, Sun J, Cai R, Morris PE, Freeman BD, Holmes JH, Cairns BA, Suffredini AF, US Critical Illness and Injury Trials Group: Smoke Inhalation-associated Acute Lung Injury (SI-ALI) Investigators (USCIIT-SI-ALI) Risk factors for in-hospital mortality in smoke inhalation-associated acute lung injury: data from 68 United States hospitals. Chest. 2016;150(6):1260–1268. doi: 10.1016/j.chest.2016.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang F, Li MY, Lan YT, Wang CB. Imbalance of Th17/Tregs in rats with smoke inhalation-induced acute lung injury. Scientific Reports. 2016;6:21348. doi: 10.1038/srep21348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rehberg S, Maybauer MO, Enkhbaatar P, Maybauer DM, Yamamoto Y, Traber DL. Pathophysiology, management and treatment of smoke inhalation injury. Expert Review of Respiratory Medicine. 2009;3(3):283–297. doi: 10.1586/ers.09.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones SW, Zhou H, Ortiz-Pujols SM, Maile R, Herbst M, Joyner BL, Jr, Zhang H, et al. Bronchoscopy-derived correlates of lung injury following inhalational injuries: a prospective observational study. PLoS One. 2013;8(5):e64250. doi: 10.1371/journal.pone.0064250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang PM, Syrkina O, Yu L, Dedaj R, Zhao H, Shiedlin A, Liu YY, Garg H, Quinn DA, Hales CA. High MW hyaluronan inhibits smoke inhalation-induced lung injury and improves survival. Respirology. 2010;15(7):1131–1139. doi: 10.1111/j.1440-1843.2010.01829.x. [DOI] [PubMed] [Google Scholar]
- 6.Crimi E, Slutsky AS. Inflammation and the acute respiratory distress syndrome. Best Practice & Research. Clinical Anaesthesiology. 2004;18(3):477–492. doi: 10.1016/j.bpa.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Han S, Cai W, Yang X, Jia Y, Zheng Z, Wang H, Li J, et al. ROS-mediated NLRP3 inflammasome activity is essential for burn-induced acute lung injury. Mediators of Inflammation. 2015;2015:720457. doi: 10.1155/2015/720457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsushima K, King LS, Aggarwal NR, De Gorordo A, D'Alessio FR, Kubo K. Acute lung injury review. Internal Medicine. 2009;48(9):621–630. doi: 10.2169/internalmedicine.48.1741. [DOI] [PubMed] [Google Scholar]
- 9.Clark CJ, Pollock AJ, Reid WH, Campbell D, Gemmell C. Role of pulmonary alveolar macrophage activation in acute lung injury after burns and smoke inhalation. Lancet. 1988;2(8616):872–874. doi: 10.1016/S0140-6736(88)92471-3. [DOI] [PubMed] [Google Scholar]
- 10.Shults JA, Curtis BJ, Boe DM, Ramirez L, Kovacs EJ. Ethanol intoxication prolongs post-burn pulmonary inflammation: role of alveolar macrophages. Journal of Leukocyte Biology. 2016;100(5):1037–1045. doi: 10.1189/jlb.3MA0316-111R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shimada K, Serada S, Fujimoto M, Nomura S, Nakatsuka R, Harada E, Iwahori K, Tachibana I, Takahashi T, Kumanogoh A, Kishimoto T, Naka T. Molecular mechanism underlying the antiproliferative effect of suppressor of cytokine signaling-1 in non-small-cell lung cancer cells. Cancer Science. 2013;104(11):1483–1491. doi: 10.1111/cas.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kubo M, Hanada T, Yoshimura A. Suppressors of cytokine signaling and immunity. Nature Immunology. 2003;4(12):1169–1176. doi: 10.1038/ni1012. [DOI] [PubMed] [Google Scholar]
- 13.Yasukawa H, Sasaki A, Yoshimura A. Negative regulation of cytokine signaling pathways. Annual Review of Immunology. 2000;18:143–164. doi: 10.1146/annurev.immunol.18.1.143. [DOI] [PubMed] [Google Scholar]
- 14.Rui L, Yuan M, Frantz D, Shoelson S, White MF. SOCS-1 and SOCS-3 block insulin signaling by ubiquitin-mediated degradation of IRS1 and IRS2. The Journal of Biological Chemistry. 2002;277(44):42394–42398. doi: 10.1074/jbc.C200444200. [DOI] [PubMed] [Google Scholar]
- 15.Cui X, Shan X, Qian J, Ji Q, Wang L, Wang X, Li M, et al. The suppressor of cytokine signaling SOCS1 promotes apoptosis of intestinal epithelial cells via p53 signaling in Crohn’s disease. Experimental and Molecular Pathology. 2016;101(1):1–11. doi: 10.1016/j.yexmp.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 16.Naka T, Tsutsui H, Fujimoto M, Kawazoe Y, Kohzaki H, Morita Y, Nakagawa R, et al. SOCS-1/SSI-1-deficient NKT cells participate in severe hepatitis through dysregulated cross-talk inhibition of IFN-gamma and IL-4 signaling in vivo. Immunity. 2001;14(5):535–545. doi: 10.1016/S1074-7613(01)00132-7. [DOI] [PubMed] [Google Scholar]
- 17.Chong MM, Metcalf D, Jamieson E, Alexander WS, Kay TW. Suppressor of cytokine signaling-1 in T cells and macrophages is critical for preventing lethal inflammation. Blood. 2005;106(5):1668–1675. doi: 10.1182/blood-2004-08-3049. [DOI] [PubMed] [Google Scholar]
- 18.Wang W, Liu Z, Su J, Chen WS, Wang XW, Bai SX, Zhang JZ, Yu SQ. Macrophage micro-RNA-155 promotes lipopolysaccharide-induced acute lung injury in mice and rats. American Journal of Physiology. Lung Cellular and Molecular Physiology. 2016;311(2):L494–L506. doi: 10.1152/ajplung.00001.2016. [DOI] [PubMed] [Google Scholar]
- 19.Galam L, Soundararajan R, Breitzig M, Rajan A, Yeruva RR, Czachor A, Harris F, Lockey RF, Kolliputi N. SOCS-1 rescues IL-1beta-mediated suppression of epithelial sodium channel in mouse lung epithelial cells via ASK-1. Oncotarget. 2016;7(20):29081–29091. doi: 10.18632/oncotarget.8543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakashima T, Yokoyama A, Onari Y, Shoda H, Haruta Y, Hattori N, Naka T, Kohno N. Suppressor of cytokine signaling 1 inhibits pulmonary inflammation and fibrosis. The Journal of Allergy and Clinical Immunology. 2008;121(5):1269–1276. doi: 10.1016/j.jaci.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 21.Goodman RB, Pugin J, Lee JS, Matthay MA. Cytokine-mediated inflammation in acute lung injury. Cytokine & Growth Factor Reviews. 2003;14(6):523–535. doi: 10.1016/S1359-6101(03)00059-5. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y, Li X, Grailer JJ, Wang N, Wang M, Yao J, Zhong R, Gao GF, Ward PA, Tan DX, Li X. Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome. Journal of Pineal Research. 2016;60(4):405–414. doi: 10.1111/jpi.12322. [DOI] [PubMed] [Google Scholar]
- 23.Surprenant A, Rassendren F, Kawashima E, North RA, Buell G. The cytolytic P2Z receptor for extracellular ATP identified as a P2X receptor (P2X7) Science. 1996;272(5262):735–738. doi: 10.1126/science.272.5262.735. [DOI] [PubMed] [Google Scholar]
- 24.Munoz-Planillo R, Kuffa P, Martinez-Colon G, Smith BL, Rajendiran TM, Nunez G. K(+) efflux is the common trigger of NLRP3 inflammasome activation by bacterial toxins and particulate matter. Immunity. 2013;38(6):1142–1153. doi: 10.1016/j.immuni.2013.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sborgi L, Ravotti F, Dandey VP, Dick MS, Mazur A, Reckel S, Chami M, Scherer S, Huber M, Böckmann A, Egelman EH, Stahlberg H, Broz P, Meier BH, Hiller S. Structure and assembly of the mouse ASC inflammasome by combined NMR spectroscopy and cryo-electron microscopy. Proceedings of the National Academy of Sciences of the United States of America. 2015;112(43):13237–13242. doi: 10.1073/pnas.1507579112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang Z, Cao J, Yu C, Yang Q, Zhang Y, Han L. Caspase-1 mediated interleukin-18 activation in neutrophils promotes the activity of rheumatoid arthritis in a NLRP3 inflammasome independent manner. Joint, Bone, Spine. 2016;83(3):282–289. doi: 10.1016/j.jbspin.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 27.Garcia K, Escobar G, Mendoza P, Beltran C, Perez C, Arancibia S, Vernal R, Rodas PI, Acuna-Castillo C, Escobar A. ATP induces IL-1beta secretion in Neisseria gonorrhoeae-infected human macrophages by a mechanism not related to the NLRP3/ASC/caspase-1 axis. Mediators of Inflammation. 2016;2016:1258504–1258510. doi: 10.1155/2016/1258504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Inoue M, Williams KL, Oliver T, Vandenabeele P, Rajan JV, Miao EA, Shinohara ML. Interferon-beta therapy against EAE is effective only when development of the disease depends on the NLRP3 inflammasome. Science Signaling. 2012;5(225):ra38. doi: 10.1126/scisignal.2002767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yamamoto Y, Enkhbaatar P, Sousse LE, Sakurai H, Rehberg SW, Asmussen S, Kraft ER, Wright CL, Bartha E, Cox RA, Hawkins HK, Traber LD, Traber MG, Szabo C, Herndon DN, Traber DL. Nebulization with gamma-tocopherol ameliorates acute lung injury after burn and smoke inhalation in the ovine model. Shock. 2012;37(4):408–414. doi: 10.1097/SHK.0b013e3182459482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang L, Zhu K, Ma Y, Xu C, Shi Q, Chen X, Su W, Zhao H. SOCS-1 ameliorates smoke inhalation-induced acute lung injury through inhibition of ASK-1 activity and DISC formation. Clinical Immunology. 2017;191:94–99. doi: 10.1016/j.clim.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 31.Okada SF, Nicholas RA, Kreda SM, Lazarowski ER, Boucher RC. Physiological regulation of ATP release at the apical surface of human airway epithelia. The Journal of Biological Chemistry. 2006;281(32):22992–23002. doi: 10.1074/jbc.M603019200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Franchi L, Kanneganti TD, Dubyak GR, Nunez G. Differential requirement of P2X7 receptor and intracellular K+ for caspase-1 activation induced by intracellular and extracellular bacteria. The Journal of Biological Chemistry. 2007;282(26):18810–18818. doi: 10.1074/jbc.M610762200. [DOI] [PubMed] [Google Scholar]
- 33.Di Virgilio F. Liaisons dangereuses: P2X(7) and the inflammasome. Trends in Pharmacological Sciences. 2007;28(9):465–472. doi: 10.1016/j.tips.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 34.Sun K, Salmon S, Yajjala VK, Bauer C, Metzger DW. Expression of suppressor of cytokine signaling 1 (SOCS1) impairs viral clearance and exacerbates lung injury during influenza infection. PLoS Pathogens. 2014;10(12):e1004560. doi: 10.1371/journal.ppat.1004560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Galam L, Parthasarathy PT, Cho Y, Cho SH, Lee YC, Lockey RF, Kolliputi N. Adenovirus-mediated transfer of the SOCS-1 gene to mouse lung confers protection against hyperoxic acute lung injury. Free Radical Biology & Medicine. 2015;84:196–205. doi: 10.1016/j.freeradbiomed.2015.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee AS, Mellins RB. Lung injury from smoke inhalation. Paediatric Respiratory Reviews. 2006;7(2):123–128. doi: 10.1016/j.prrv.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 37.Enkhbaatar P, Traber DL. Pathophysiology of acute lung injury in combined burn and smoke inhalation injury. Clinical Science (London, England) 2004;107(2):137–143. doi: 10.1042/CS20040135. [DOI] [PubMed] [Google Scholar]
- 38.Leung CC, Yu IT, Chen W. Silicosis. Lancet. 2012;379(9830):2008–2018. doi: 10.1016/S0140-6736(12)60235-9. [DOI] [PubMed] [Google Scholar]
- 39.Gasse P, Mary C, Guenon I, Noulin N, Charron S, Schnyder-Candrian S, Schnyder B, Akira S, Quesniaux VFJ, Lagente V, Ryffel B, Couillin I. IL-1R1/MyD88 signaling and the inflammasome are essential in pulmonary inflammation and fibrosis in mice. The Journal of Clinical Investigation. 2007;117(12):3786–3799. doi: 10.1172/JCI32285.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xiang M, Shi X, Li Y, Xu J, Yin L, Xiao G, Scott MJ, Billiar TR, Wilson MA, Fan J. Hemorrhagic shock activation of NLRP3 inflammasome in lung endothelial cells. Journal of Immunology. 2011;187(9):4809–4817. doi: 10.4049/jimmunol.1102093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Petrilli V, Papin S, Tschopp J. The inflammasome. Current Biology. 2005;15(15):R581. doi: 10.1016/j.cub.2005.07.049. [DOI] [PubMed] [Google Scholar]
- 42.Petrilli V, Papin S, Dostert C, Mayor A, Martinon F, Tschopp J. Activation of the NALP3 inflammasome is triggered by low intracellular potassium concentration. Cell Death and Differentiation. 2007;14(9):1583–1589. doi: 10.1038/sj.cdd.4402195. [DOI] [PubMed] [Google Scholar]
- 43.Kolliputi N, Shaik RS, Waxman AB. The inflammasome mediates hyperoxia-induced alveolar cell permeability. Journal of Immunology. 2010;184(10):5819–5826. doi: 10.4049/jimmunol.0902766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lin HY, Tsai CH, Lin C, Yeh WL, Tsai CF, Chang PC, Wu LH, Lu DY. Cobalt protoporphyrin upregulates cyclooxygenase-2 expression through a heme oxygenase-independent mechanism. Molecular Neurobiology. 2016;53(7):4497–4508. doi: 10.1007/s12035-015-9376-y. [DOI] [PubMed] [Google Scholar]