Abstract
Respiratory syncytial virus (RSV) is the most frequent cause of bronchiolitis. However the pathophysiology of bronchiolitis is unclear. Leukocytes, especially neutrophils, may play an important role in the pathogenesis of bronchiolitis. Whereas we have previously shown that neutrophils augment epithelial leakage and detachment in RSV infection in vitro, it is unknown whether epithelial damage occurs in vivo in infants with RSV bronchiolitis. We hypothesized that respiratory epithelial damage occurs in infants with RSV bronchiolitis and that surfactant proteins leak into the circulation. The plasma concentrations of surfactant protein-A and surfactant protein-B in infants with RSV bronchiolitis were measured by ELISA. Plasma immunoreactive surfactant protein-B in infants with RSV bronchiolitis was markedly higher than that in matching controls. Our study suggests that alveolocapillary permeability is increased in infants with RSV bronchiolitis in vivo and that surfactant protein-B may be a sensitive marker for lung injury in such infants.
Main
RSV causes significant respiratory disease, infecting almost all children during the first 2 y of life (1, 2). Indeed RSV is the most frequent cause of bronchiolitis and pneumonia in infants requiring hospitalization (3). Moreover, at least 50% of infants who have acute viral bronchiolitis because of RSV have subsequent episodes of wheezing consistent with asthma (4, 5). However, the pathophysiology of RSV bronchiolitis is unclear. RSV bronchiolitis is characterized histologically by epithelial necrosis and peribronchoalveolar infiltration with leukocytes, especially neutrophils (6, 7). We recently reported that neutrophils can augment epithelial leakage and detachment in RSV infection in vitro (8), suggesting that neutrophils and their products may have an important role in the clinical and pathologic changes occurring in RSV infection. However, it is unknown whether such epithelial damage occurs in vivo in infants with RSV bronchiolitis, as there has been no clinical measure available to detect such damage.
The alveolocapillary membrane, with a surface area approximately 50 times that of the body and only 0.1–0.2 μm thick, faces an extraordinary task in partitioning proteins of the plasma and those of the pulmonary ELF (9). We have recently shown that impairment of the alveolocapillary barrier allows increased leakage of SP-A and SP-B into the circulation in a manner that reflects lung function and injury score (9–11). Because the integrity of the bronchoalveolar epithelium is likely to be impaired in RSV bronchiolitis, we have compared the plasma concentrations of SP-A and SP-B in infants without cardiopulmonary diseases with those in infants hospitalized because of RSV bronchiolitis.
Methods
Subjects
Fifteen RSV-positive infants between 1 and 14 mo of age (6.0 ± 1.1 mo; mean ± SEM), admitted for acute bronchiolitis to Flinders Medical Center in Adelaide, South Australia, were enrolled. The RSV antigens were detected from an aliquot of nasopharyngeal aspirates by indirect immunofluorescence assay. The infants, who were healthy until the time of infection, all had a severe infection with coughing, wheezing, chest overinflation, and tachypnea. None of them required intubation or ventilation. A healthy control group of 13 infants between 1 and 24 mo of age (7.7 ± 1.7 mo), who required blood tests before minor surgery, were also enrolled. Informed consent was obtained from the parents of the infants, and the study was approved by the Clinical Investigations (Ethics) Committee at Flinders Medical Center.
Blood sampling and plasma preparation
Blood (1–2 mL) was drawn from an antecubital vein into lithium heparin tubes from patients and control infants. The blood was immediately centrifuged at 913 ×g for 5 min at 4°C (GS-6R Centrifuge, Beckman, USA). The plasma was collected and stored at −20°C or −80°C for batch analysis.
Determination of SP-A and SP-B
Our SP-A and SP-B ELISA have been previously published (9–11). Briefly, to free the SP-A and SP-B from any associated plasma or surfactant components, aliquots are first treated with EDTA, SDS, and Triton X-100. The antigens are measured by ELISA inhibition assays using antibodies Po-A and Po-B raised against alveolar proteinosis-derived SP-A and mature SP-B, respectively (9–11). All samples are assayed in duplicate at four serial dilutions. Standards, assayed in quadruplicate, are included in each ELISA plate at eight serial dilutions (ranging from 7.8 to 1000 ng/mL). Absorbance is measured using a Dynatech MR5000 reader (Dynatech Laboratories; Chantilly, VA). An AssayZap program (Biosoft; Ferguson, MO) is used to generate a standard curve (r> 0.99) and to compute the concentrations of SP-A and SP-B. The antibodies do not react with other plasma or ELF antigens, and the assays have a coefficient of variation of approximately 6%.
Antibody specificity
SP-A.
The specificity of Po-A has been described in detail elsewhere (9). Briefly, its specificity was compared by Western blotting with the MAb Pe-10 (9). The reactivity was tested under both reducing and nonreducing conditions using whole human bronchoalveolar lavage fluid, human surfactant, purified human SP-A, and human serum. The patterns of immunochemical staining obtained were indistinguishable regardless of whether Po-A or PE-10 was used and corresponded solely to immunoreactive SP-A (9).
SP-B.
The specificity of Po-B has also been described in detail elsewhere (10). Briefly, we have purified mature human SP-B and raised a polyclonal antibody that reacts strongly with the mature protein, the processing intermediate, and the SP-B precursor when separated under both reducing and nonreducing conditions. We have compared its specificity with antibodies raised against a synthetic fusion protein of the human full-length SP-B cDNA; antibodies generated against recombinant human C-terminal propeptide, residues 280–381; and finally, antibodies generated against recombinant human N-terminal propeptide, residues 24–200 (10). Our analysis suggests that plasma contains very little mature SP-B and that the major immunoreactive forms present correspond to the precursor (approximately 42 kD) and processing intermediate (approximately 25 kD) (10).
Statistical analysis
Data are given as mean ± SEM. Differences in results between groups were examined with independent-samples t test. A p value of < 0.05 was considered significant.
RESULTS
The plasma concentration of immunoreactive SP-A in the control infants (673 ± 77 ng/mL) was not different from that in the infants with RSV-positive bronchiolitis (630 ± 94 ng/mL;Fig. 1). In contrast, plasma immunoreactive SP-B was significantly higher in the infants with RSV-positive bronchiolitis (4017 ± 852 ng/mL) than that in the controls (1313 ± 104 ng/mL;p< 0.01;Fig. 1). Consistent with this, the SP-B/SP-A ratio in plasma was approximately 300% higher in the infected group. Neither the plasma concentration of immunoreactive SP-B nor the SP-B/SP-A ratio was related to age.
Figure 1.
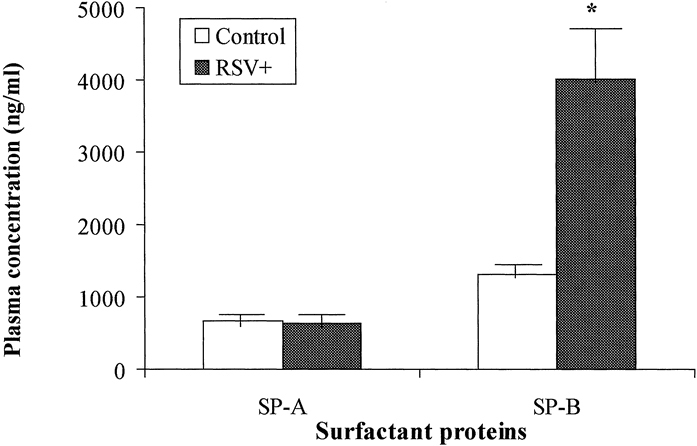
Plasma concentrations of SP-A and SP-B in control infants (n= 13) and infants with RSV-positive bronchiolitis (n= 15). Both SP-A and SP-B were determined using ELISA. The data are expressed as the mean ± SEM. *p< 0.05 compared with control group.
DISCUSSION
Our data illustrate that the plasma SP-B, but not the SP-A, concentration is elevated in RSV-positive infants with bronchiolitis. We believe that the site of leakage is the alveolocapillary barrier, inasmuch as the bronchocapillary barrier has a surface area approximately 2.5% to 5% that of the alveolocapillary barrier and is considerably thicker (several micrometers to millimeters as opposed to 0.1 to 0.2 μm). In addition, protein transport across the bronchial epithelium is usually accompanied by degradation, whereas proteins cross the alveolar epithelium largely intact (12).
Consistent with this, there is now a large body of work describing the flux of locally secreted proteins from the hypophase into the circulation (13). Moreover, because of difficulties associated with the bioavailability of orally ingested recombinant therapeutic proteins, increasing attention has been given to the use of the lung as a noninvasive means of systemic delivery. Nebulized intrapulmonary recombinant human insulin has been used (14), and recombinant human superoxide dismutase administered intratracheally to infants with respiratory distress syndrome is found in significant quantities in serum and urine within 6 h of administration (15).
In the airspaces, SP-A predominantly forms high-molecular weight oligomers (approximately 650 kD) with Stokes radii of approximately 35 nm (16). Although mature SP-B, which associates as a low Mr (approximately 18 kD) thiol-dependent homodimer (17), is normally intimately associated with complexes of surfactant phospholipids, which are possibly too large to readily breach the alveolocapillary barrier, we have previously shown that at least some of the protein is secreted into the alveolus as hydrophilic, monomeric proprotein and processing intermediate with approximate Mr of 45 kD and 25 kD, respectively (10). We have shown that these forms breach the alveolocapillary barrier more readily than SP-A (10, 11), presumably because they are smaller, and so provide a better marker of lung injury. Therefore, our finding that RSV bronchiolitis is associated with increased levels of SP-B, but not SP-A, may reflect the relative severity of the injury, the nature of the sieving properties of the lung, and the differences in the sizes of the proteins (9–11). This indicates that RSV bronchiolitis requiring hospitalization is associated with increased alveolocapillary permeability, but, at least in cases in which ventilatory support is not required, to a lesser extent to that which occurs in acute respiratory distress syndrome (9, 10). As far as we know, this is the first report identifying increased alveolocapillary permeability in infants with RSV bronchiolitis.
Consistent with the notion that our findings reflect increased alveolocapillary permeability and the difference in the sizes of SP-A and SP-B, Kerr and Paton (18) recently found that SP-A and SP-B are reduced approximately 40% and 90%, respectively, in bronchoalveolar lavage fluid harvested from children infected with RSV. This indicates that neither selective degradation nor consumption of alveolar SP-A, or increased SP-B synthesis, are likely to explain why plasma SP-B is elevated in our RSV-infected cohort, whereas SP-A is not. Indeed, increased leakage of SP-B may be a contributing factor to the decreased SP-B concentrations with regard to those of SP-A in bronchoalveolar lavage fluid harvested from children infected with RSV (18).
The mechanism of lung injury induced by RSV infection in vivo is unknown. In most cases, a common pathway involving the recruitment and activation of leukocytes, and in particular neutrophils, is thought to result in diffuse inflammatory lung injury (10). Neutrophils play an important role in lung injury in acute respiratory distress syndrome. They are also the predominant inflammatory cells in RSV infection (6, 7), and our previous in vitro study has shown that RSV infection can induce alveolar type II-like cell (A549) leakage and detachment to a certain extent, both of which are augmented by neutrophils (8). Therefore, we speculate that alveolar permeability may be increased both through the direct action of the virus, as well as through that of the neutrophils. In addition, increased work of breathing associated with airway obstruction can generate large negative alveolar pressure and cause edema (19, 20), whereas lung hyperinflation is a well-known factor increasing alveolocapillary permeability (21). However, we do not know the relative contribution of these factors to the overall alveolocapillary permeability.
Pulmonary surfactant is known to stabilize alveoli and to maintain patency of conducting airways (22–24). In a guinea-pig asthma model challenged with ovalbumin aerosol, it was shown that surfactant dysfunction developed, which might cause conducting airways to become blocked by liquid columns and thereby increase airway resistance (24). It has also been reported that RSV infection in BALB/c mice induced surfactant dysfunction, which may increase airway resistance (25). It seems that surfactant may play an important role in the pathophysiology of both RSV infection and asthma (25, 26). It has recently been shown that surfactant from infants with viral bronchiolitis has an increased minimum surface tension (27). Inasmuch as SP-B is essential for normal surface activity (28), possible leakage of SP-B into the circulation may reduce alveolar levels and contribute to the reduced surface activity observed by Dargaville and associates (27).
In summary, our study suggests that alveolocapillary permeability is increased in infants with RSV bronchiolitis in vivo. However, currently we do not know whether the circulating concentration of SP-B is related to disease severity. Further studies are required to elucidate the role of surfactant and pulmonary injury in the pathophysiology of RSV bronchiolitis.
Acknowledgements
The authors thank all the staff in the Departments of Pediatrics, Pediatric Surgery, and Anesthesia at Flinders Medical Center, for assistance in collecting clinical samples.
Glossary
- ARDS
acute respiratory distress syndrome
- ELF
epithelial lining fluid
- RSV
respiratory syncytial virus
- SP-A
surfactant protein-A
- SP-B
surfactant protein-B
Footnotes
Supported in part by The Channel Seven Children's Research Foundation of South Australia Inc. (grant no. 30, 97/98). Dr. S.Z. Wang was supported by an Australian Overseas Postgraduate Research Scholarship and Flinders University Research Scholarship.
References
- 1.Anderson LJ, Heilman CA. Protective and disease-enhancing immune responses to respiratory syncytial virus. J Infect Dis. 1995;171:1–7. doi: 10.1093/infdis/171.1.1. [DOI] [PubMed] [Google Scholar]
- 2.Openshaw PJM. Immunity and immunopathology to respiratory syncytial virus. The mouse model. Am J Respir Crit Care Med. 1995;152:S59–S62. doi: 10.1164/ajrccm/152.4_Pt_2.S59. [DOI] [PubMed] [Google Scholar]
- 3.Holberg CJ, Wright AL, Martinez FD. Risk factors for respiratory syncytial virus-associated lower airway illness in the first year of life. Am J Epidemiol. 1991;133:1135–1151. doi: 10.1093/oxfordjournals.aje.a115826. [DOI] [PubMed] [Google Scholar]
- 4.Phelan PD. Practical Paediatrics. 1994. The epidemiology of acute respiratory infections; p. 341. [Google Scholar]
- 5.Wang S-Z, Forsyth KD. Asthma and respiratory syncytial virus infection in children: is there a link? Clin Exp Allergy. 1998;28:927–935. doi: 10.1046/j.1365-2222.1998.00353.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dakhama A, Vitalis TZ, Hegele RG. Persistence of respiratory syncytial virus (RSV) infection and development of RSV-specific IgG1 response in a guinea-pig model of acute bronchiolitis. Eur Respir J. 1997;10:20–26. doi: 10.1183/09031936.97.10010020. [DOI] [PubMed] [Google Scholar]
- 7.Everard ML, Awarbrick A, Wrightham M, McIntyre J, Dunkley C, James DJ, Sewell HF, Milner AD. Analysis of cells obtained by bronchial lavage of infants with respiratory syncytial virus infection. Arch Dis Child. 1994;71:428–432. doi: 10.1136/adc.71.5.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang S-Z, Xu H, Wraith A, Bowden JJ, Alpers JH, Forsyth KD. Neutrophils induce damage to respiratory epithelial cells infected with respiratory syncytial virus. Eur Respir J. 1998;12:612–618. doi: 10.1183/09031936.98.12030612. [DOI] [PubMed] [Google Scholar]
- 9.Doyle IR, Nicholas TE, Bersten AD. Serum surfactant protein-A (SPA) levels in patients with acute cardiogenic pulmonary edema and adult respiratory distress syndrome. Am J Respir Crit Care Med. 1995;152:307–317. doi: 10.1164/ajrccm.152.1.7599839. [DOI] [PubMed] [Google Scholar]
- 10.Doyle IR, Bersten AD, Nicholas TE. Surfactant proteins-A and -B are elevated in plasma of patients with acute respiratory failure. Am J Respir Crit Care Med. 1997;156:1217–1229. doi: 10.1164/ajrccm.156.4.9603061. [DOI] [PubMed] [Google Scholar]
- 11.Doyle IR, Hermans C, Bersten A, Nicholas TE, Bersten AD. Clearance of Clara cell secretory protein (CC16) and surfactant proteins A and B from blood in acute respiratory failure. Am J Respir Crit Care Med. 1998;158:1528–1535. doi: 10.1164/ajrccm.158.5.9712097. [DOI] [PubMed] [Google Scholar]
- 12.Folkesson HG, Matthay MA, Weström BR, Kim KJ, Karlsson BW, Hastings RH. Alveolar epithelial clearance of protein. J Appl Physiol. 1996;80:1431–1445. doi: 10.1152/jappl.1996.80.5.1431. [DOI] [PubMed] [Google Scholar]
- 13.Doyle IR, Nicholas TE, Bersten AD. Partitioning lung and plasma proteins: circulating surfactant proteins as biomarkers of alveolocapillary permeability. Clin Exp Pharmacol Physiol. 1999;26:185–197. doi: 10.1046/j.1440-1681.1999.03015.x. [DOI] [PubMed] [Google Scholar]
- 14.Jendle JH, Karlberg BE. Intrapulmonary administration of insulin to healthy volunteers. Intern Med. 1996;240:93–98. doi: 10.1046/j.1365-2796.1996.502836000.x. [DOI] [PubMed] [Google Scholar]
- 15.Rosenfeld WN, Davis JM, Parton L, Richter SE, Price A, Flaster E, Kassem N. Safety and pharmacokinetics of recombinant human superoxide dismutase administered intratracheally to premature neonates with respiratory distress syndrome. Pediatrics. 1996;97:811–817. [PubMed] [Google Scholar]
- 16.Voss T, Eistetter H, Schäfer KP, Engel J. Macromolecular organization of natural and recombinant lung surfactant protein SP 28–36. J Mol Biol. 1988;201:219–227. doi: 10.1016/0022-2836(88)90448-2. [DOI] [PubMed] [Google Scholar]
- 17.Johansson J, Curstedt T, Jornvall H. Surfactant protein B: disulfide bridges, structural properties, and kringle similarities. Biochemistry. 1991;30:6917–6921. doi: 10.1021/bi00242a015. [DOI] [PubMed] [Google Scholar]
- 18.Kerr MH, Paton JY. Surfactant protein levels in severe respiratory syncytial virus infection. Am J Respir Crit Care Med. 1999;159:1115–1118. doi: 10.1164/ajrccm.159.4.9709065. [DOI] [PubMed] [Google Scholar]
- 19.Stalcup SA, Mellins RB. Mechanical forces producing pulmonary edema in acute asthma. N Engl J Med. 1977;297:592–596. doi: 10.1056/NEJM197709152971107. [DOI] [PubMed] [Google Scholar]
- 20.Pang LM, Rodriguez-Martinez F, Stalcup SA, Mellins RB. Effect of hyperinflation and atelectasis on fluid accumulation in the puppy lung. J Appl Physiol. 1978;45:284–288. doi: 10.1152/jappl.1978.45.2.284. [DOI] [PubMed] [Google Scholar]
- 21.Egan EA. Lung inflation, lung solute permeability, and alveolar edema. J Appl Physiol. 1982;53:121–125. doi: 10.1152/jappl.1982.53.1.121. [DOI] [PubMed] [Google Scholar]
- 22.Enhorning G, Duffy LC, Welliver RC. Pulmonary surfactant maintains patency of conducting airways in the rat. Am J Respir Crit Care Med. 1995;151:554–556. doi: 10.1164/ajrccm.151.2.7842219. [DOI] [PubMed] [Google Scholar]
- 23.Enhorning G, Yarussi A, Rao P, Vargas I. Increased airway resistance due to surfactant dysfunction can be alleviated with aerosol surfactant. Can J Physiol Pharmacol. 1996;74:687–691. doi: 10.1139/y96-062. [DOI] [PubMed] [Google Scholar]
- 24.Liu M, Wang L, Enhorning G. Surfactant dysfunction develops when the immunized guinea-pig is challenged with ovalbumin aerosol. Clin Exp Allergy. 1995;25:1053–1060. doi: 10.1111/j.1365-2222.1995.tb03251.x. [DOI] [PubMed] [Google Scholar]
- 25.Van Schaik SM, Vargas IDA, Welliver RC, Enhorning G. Surfactant dysfunction develops in BALB/c mice infected with respiratory syncytial virus. Pediatr Res. 1997;42:169–173. doi: 10.1203/00006450-199708000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Postle AD. Lung surfactant and asthma. Clin Exp Allergy. 1995;25:1030–1033. doi: 10.1111/j.1365-2222.1995.tb03247.x. [DOI] [PubMed] [Google Scholar]
- 27.Dargaville PA, South M, McDougall PN. Surfactant abnormalities in infants with severe viral bronchiolitis. Arch Dis Child. 1996;75:133–136. doi: 10.1136/adc.75.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Venkitaraman AR, Hall SB, Whitsett JA, Notter RH. Enhancement of biophysical activity of lung surfactant extracts and phospholipid-apoprotein mixtures by surfactant protein A. Chem Phys Lipids. 1990;56:185–194. doi: 10.1016/0009-3084(90)90101-V. [DOI] [PubMed] [Google Scholar]


