Abstract
Study Design
Longitudinal co-twin control study of the Vietnam-Era Twin Registry.
Objective
To examine the association of post-traumatic stress disorder (PTSD) symptoms with incident chronic back pain (CBP), while controlling for genetic factors and early family environment.
Summary of Background Data
It is unknown whether PTSD symptoms are associated with an increased incidence of CBP.
Methods
In 2010–2012 a baseline survey was undertaken as part of a large-scale study of PTSD. Study participants completed the PTSD Symptom Checklist (PCL) and a self-report measure of CBP. In 2015–2017 a follow-up survey was sent to all 171 monozygotic (MZ) twin pairs (342 individuals) where both co-twins had no history of CBP at baseline, but only one co-twin in the pair met criteria for having current PTSD symptoms (one twin with PCL <30 and the co-twin with PCL≥30). No other inclusion/exclusion criteria were applied. CBP at 5-year follow-up was defined as back pain of duration ≥3 months in the low back or mid/upper back. Covariates included age, race, education, income, Veterans Affairs health care use, disability compensation, smoking, body mass index, and depression. Statistical analysis estimated the cumulative incidence of CBP according to baseline PTSD symptoms. Risk ratios (RRs) and 95% confidence intervals (CI) were estimated in matched-pair co-twin control analyses adjusting for familial factors.
Results
Among 227 males completing 5-year follow-up, including 91 MZ twin pairs, the mean age was 62 years. Five-year incidence of CBP in those without and with baseline PTSD symptoms was 40% and 60%, respectively. Baseline PTSD symptoms were significantly associated with incident CBP in crude and multivariable-adjusted within-pair analyses (RR 1.6 [95% CI 1.2–2.1]; p=0.002).
Conclusions
PTSD symptoms were associated with an increased incidence of CBP, without confounding by genetic factors or early family environment. PTSD symptoms may be a modifiable risk factor for prevention of CBP.
Keywords: twins, post-traumatic stress disorder, PTSD, depression, low back pain, genetics, Veterans
INTRODUCTION
Back pain is one of the most common symptoms prompting health care visits and the leading cause of years lived with disability worldwide.1,2 Mental health conditions may predispose to incident back pain,3,4 and the comorbidity of back pain with mental health conditions predicts worse overall back-related outcomes.5–8 Although the association of back pain with depression and anxiety has been extensively studied, less is known regarding the relationship between back pain and other mental health conditions, such as post-traumatic stress disorder (PTSD).
Military Veterans have a high prevalence of both PTSD and back pain.9,10 PTSD is comorbid with chronic pain in 47–59% of United States (US) military Veterans in outpatient pain clinics and post-deployment clinics,11,12 where the back is the most common individual location of chronic musculoskeletal pain. Much remains unknown about the relationship between PTSD and back pain. The association between PTSD and back pain may be due to causal links between these two conditions or their correlates, raising the possibility that treatment of one condition might prevent or improve symptoms of the other. Alternatively, PTSD and back pain may be explained by other confounding factors. Several theoretical models to explain the comorbidity of PTSD and chronic pain have suggested that the two conditions coexist due to underlying “vulnerabilities” that predispose to the development or maintenance of both conditions.13–15 Such vulnerabilities might be genetic predispositions or familial factors related to upbringing that lead to both PTSD and back pain, without a direct causal link between the two conditions. If such predispositions are a major driver of the PTSD-back pain association, treatment of PTSD symptoms would not be expected to have a direct effect on the occurrence of back pain. Twin studies of back pain indicate a heritability of 40%,16,17 with generally greater heritability for chronic back pain (CBP) than for any back pain,18 and PTSD is also moderately heritable (up to 46%19,20). These estimates suggest that shared genetic contributions to CBP and PTSD are a possible explanation for their co-occurrence, as seen in prior twin studies of depression/anxiety and CBP.21–23 However, to date, no published studies have used genetically informative samples that permit the examination of whether PTSD symptoms are a risk factor for future CBP independent of genetic factors and the early family environment.
The aim of the current study was to examine whether PTSD is associated with an increased risk of CBP at 5-year follow-up, after accounting for confounding by genetic or early family environmental influences (which henceforth we refer to collectively as ‘familial factors’).
METHODS
A challenge in conducting observational research is how best to isolate the effects of potential risk factors on an outcome by controlling for relevant confounders. Even with the most rigorous methods for multivariate statistical adjustment, there remains the potential for residual confounding due to factors which are unknown and unmeasured. An alternative approach is to use study designs that account for some of the unknown or unmeasured confounding factors. The co-twin control design using monozygotic (MZ) twins is one such approach. This design capitalizes on the fact that MZ (‘identical’) twins within a pair are perfectly matched for genetics and are also matched for ‘early’ (childhood to adolescence) family environmental factors, as well as a host of other factors which are not directly measured, but which twins share in common. This offers a degree of control for confounding that cannot be attained in conventional studies of unrelated individuals.
Study Sample
This was a longitudinal study involving members of the Vietnam-Era Twin (VET) Registry. The VET Registry was assembled from military discharge records, and includes more than 7,000 male twin pairs, both of whom served on active duty during the Vietnam era (1965–1975).24 It is the only active national twin registry in the US, and members live in all 50 states. VET Registry participants are comparable to older adult males from the US general population with respect to sociodemographic factors including educational attainment and income.25 Further details of the VET Registry construction and zygosity ascertainment are described elsewhere.26–30
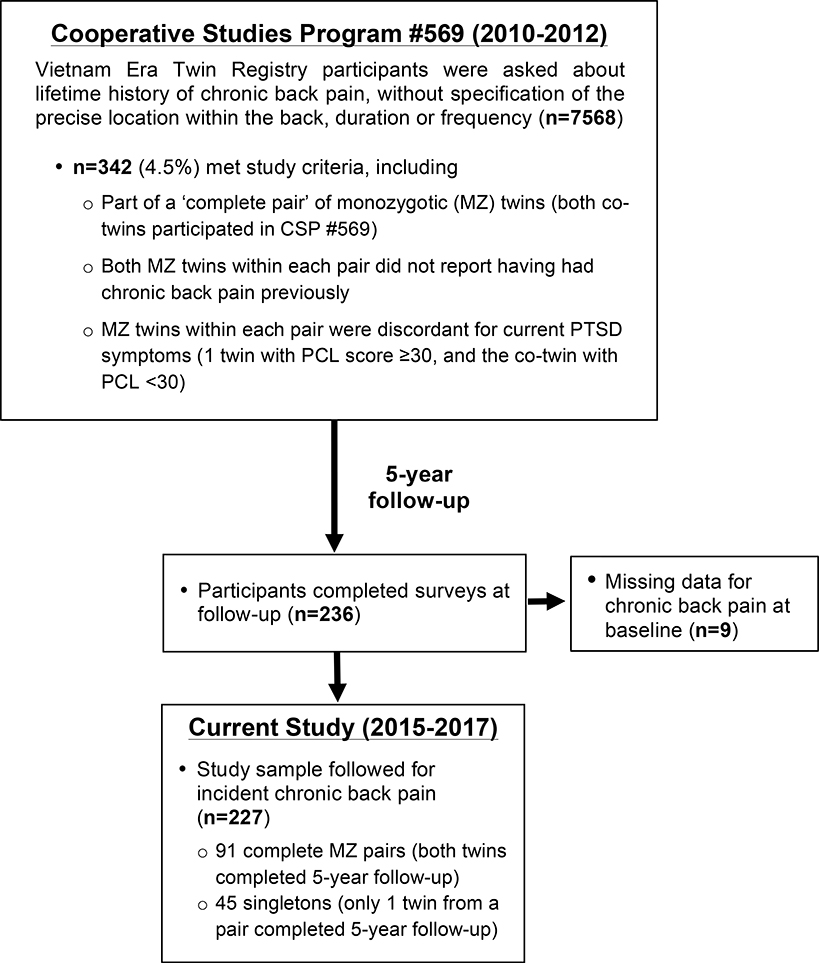
Between 2010 and 2012, living VET Registry members were invited to participate in an observational study of PTSD among Veterans (Cooperative Studies Program [CSP] #569). This included a survey obtaining information regarding a broad range of physical and mental health conditions (Figure 1). Informed consent was obtained from all participating VET Registry members as part of CSP #569, and this protocol was approved by the Veterans’ Affairs (VA) Puget Sound Institutional Review Board. During CSP #569, study participants reported whether they had ever had “chronic back pain” in the past, without specifying the precise location within the back, duration, or frequency of pain. We identified all 171 MZ twin pairs (n=342 individuals) participating in CSP #569 in which both twins within a pair (‘co-twins’) did not report having had CBP in the past, but only one co-twin in the pair met criteria for having current PTSD symptoms. MZ twin pairs were the focus of the current study to permit within-MZ-pair analyses, which by design are controlled for underlying genetic or early family environmental factors that might predispose certain individuals to having both PTSD symptoms and CBP. These participants were contacted by mail or telephone-administered surveys between 2015 and 2017, 5 years after the time of CSP #569, to complete new data collection specifically for the purposes of the current study (Figure 1). Participants were not informed of the current study’s research questions examining associations between PTSD and CBP.
Figure 1.
Flowchart of study participation. After 5-year follow-up data collection was completed, nine respondents were subsequently found to have had missing data for chronic back pain at baseline (during CSP #569). CSP #569 indicates Cooperative Studies Program #569; PCL¼ PTSD, (post-traumatic stress disorder) checklist.
Assessment of PTSD symptoms at Baseline
PTSD symptoms were assessed using the PTSD Checklist Civilian version (PCL).31 The PCL has high test-retest reliability (r=0.9632), internal consistency (α=0.9633), and concurrent validity in Veterans when compared to a formal diagnosis of PTSD.34–36 It consists of 17 Likert items that correspond to PTSD symptoms from the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). For each item, respondents report the degree to which they were bothered by symptoms in the past month, ranging from 1 (not at all) to 5 (extremely). Individual PCL items are summed to produce a summary severity score. We defined participants with PCL scores <30 as not having current PTSD symptoms, and those with PCL scores ≥30 as having current PTSD symptoms. The PCL cut point of 30 has high sensitivity (87%) and specificity (79%) compared to a reference standard of the World Health Organization Composite Diagnostic Interview diagnosis of current PTSD,36 and corresponds to the lowest number recommended for use in general population samples (30–35).37
Assessment of Covariates
We considered as confounders a selected list of baseline variables with a conceptual rationale for potentially being associated with both PTSD and back pain. Data on age and race were previously abstracted from military service records during the 1980s. Other data collected by participant self-report during CSP #569 included educational attainment, annual family income, having ever used VA health care, having ever received or applied for VA disability compensation for any health condition, current cigarette smoking, and height and weight (used to calculate body mass index [weight in kilograms/(height in meters)2]); these variables are further described elsewhere.25 Current depression symptoms were measured using the Patient Health Questionnaire (PHQ-9), a measure of depression that grades the severity of 9 depression symptoms over the past 2 weeks (range 0–27, with higher scores representing greater depression symptoms).38 A cut point of 5 or higher was used to define depression.38
Assessment of Back Pain Outcomes at 5-year Follow-up
At the 5-year follow-up, participants were asked the question “In the past 4 weeks, have you had low back pain?” anchored to a pain diagram indicating the lumbar region. Subsequent questions inquired about low back pain duration and intensity on a 0 to 10 numerical rating scale (NRS), where “0” reflects no pain and 10 reflects the worst pain possible, using question items from the minimal dataset of the US National Institutes of Health (NIH) task force on research standards for chronic low back pain.39 These questions were then asked in regards to mid/upper back pain in the past 4 weeks, also defined as ‘thoracic’ pain and accompanied by an illustration depicting the thoracic region. Participants completed the Oswestry Disability Index (ODI), accounting for back symptoms in the low back and mid/upper back over the past month. The ODI is a widely used and validated index of back pain-related functional limitations; scores range from 0–100, where 0 represents no limitations and 100 represent the most severe limitations possible.40 The primary study outcome was incident CBP (duration ≥3 months) in the low back and/or mid/upper back at 5-year follow-up. Secondary outcomes by specific region of the back included 1) low back pain of ≥3 months duration (‘incident chronic low back pain’) and mid/upper back pain of ≥3 months duration (‘incident chronic mid/upper back pain’).
Statistical Analysis
We assessed normality of continuous variables using graphical methods and found none in violation of this assumption. We compared baseline characteristics by incident CBP at 5-year follow-up. We conducted within-MZ-pair analyses using generalized linear models to examine the association of baseline PTSD symptoms with incident CBP at 5-year follow-up. This was done first by examining bivariable associations from models including baseline PSTD symptoms and incident CBP, and next in multivariable analyses adjusting for potential confounders. We identified possible confounders of the PTSD-CBP relationship by examining for ≥10% changes in parameter estimates between bivariable models and multivariable models adjusting for the potential confounding variable.41 We calculated risk ratios (RRs) and 95% confidence intervals (CIs), setting the threshold for statistical significance at p≤0.05. The same methods were applied to the secondary back pain outcomes. Sample size was determined a priori based on assumptions of a 34% incidence of CBP at 5-year follow-up using annual incidence data from a prior study of Veterans,42 two-sided α of 0.05, 80% power to detect a relative risk of CBP ≥2.0 for those with PTSD43, and a 60% response rate from the targeted group of 342 VET Registry members who were sent surveys. Analyses were conducted using STATA v.15.1 (College Station, TX).
RESULTS
Of 342 individuals contacted at 5-year follow-up, 227 (66%) returned mail surveys for the current study and comprised the longitudinal study sample (Figure 1). The sample included 91 MZ pairs (n=182) and 45 singletons. Compared to other participants of CSP #569 (n=7341), those in the current study (n=227) were more likely to report having received or having ever applied for VA disability compensation (25.9% vs. 33.3%; p=0.01), but were otherwise comparable with respect to all variables examined in this study (data not shown).
The average age of the sample was 62 years, 26% of participants were college graduates, and 52% had an annual household income greater than the US median in 2011($50,000) (Table 1).44 Those with baseline PTSD symptoms (PCL≥30) were significantly more likely than those without to report having ever used VA health care services, to have ever received or applied for a VA service-connected disability, and to have depression symptoms (PHQ score ≥5) at baseline (Table 1).
Table 1.
Characteristics of the study sample according to baseline PTSD symptoms
| Complete MZ pairs (Within-pair analysis) | ||||
|---|---|---|---|---|
| Characteristics | All (n=227) | No PTSDa (n=91) | PTSDa (n=91) | p valueb |
| Sociodemographics | ||||
| Age (mean) | 61.6 (3.0) | 61.6 (2.9) | 61.6 (2.8) | - |
| Race (white) | 213 (93.8%) | 86 (94.5%) | 86 (94.5%) | - |
| College graduatec (miss.=10) | 56 (25.6%) | 23 (26.4%) | 26 (29.6) | 0.40 |
| Income (≥$50,000)d (miss.=12) | 112 (52.1%) | 50 (57.5%) | 43 (50%) | 0.16 |
| VA health care user ever | 80 (35.2%) | 22 (24.2%) | 38 (41.8 %) | 0.006 |
| VA service-connected disability status (miss.=5)e | 74 (32.6%) | 22 (24.7%) | 39 (43.3 %) | 0.003 |
| Clinical Characteristics | ||||
| Body Mass Index (miss.=4) | 28.6 (5.1) | 28.6 (5.0) | 29.1 (4.6) | 0.27 |
| Current smoking (miss.=2) | 52 (23.1%) | 15 (16.9%) | 19 (20.9%) | 0.32 |
| Depression symptoms (PHQ ≥5.0)(miss.=1) | 35 (15.6%) | 0 | 27 (31.8%) | <0.001 |
| PTSD symptoms (PCL ≥30) | 115 (50.7%) | 0 | 91 (100%) | - |
PTSD= Post-traumatic stress disorder, miss.= missing, VA= Veterans Affairs, PHQ=Patient Health Questionnaire, PCL=PTSD checklist
PTSD symptoms (PCL≥30) vs. no PTSD symptoms at baseline (PCL<30)
From generalized linear models, restricted to complete monozygotic twin pairs (both twins in pair with covariate and PCL data). Statistical comparisons by age and race were not made due to twins within a pair sharing these features; small differences in age within a twin pair occurred due to the timing of when surveys were completed.
Completed college, vocational school, technical school, or graduate/advanced degrees
approximate median household income in the United States at the time of baseline data collection (2011)
having ever received or applied for VA disability compensation, for any health condition
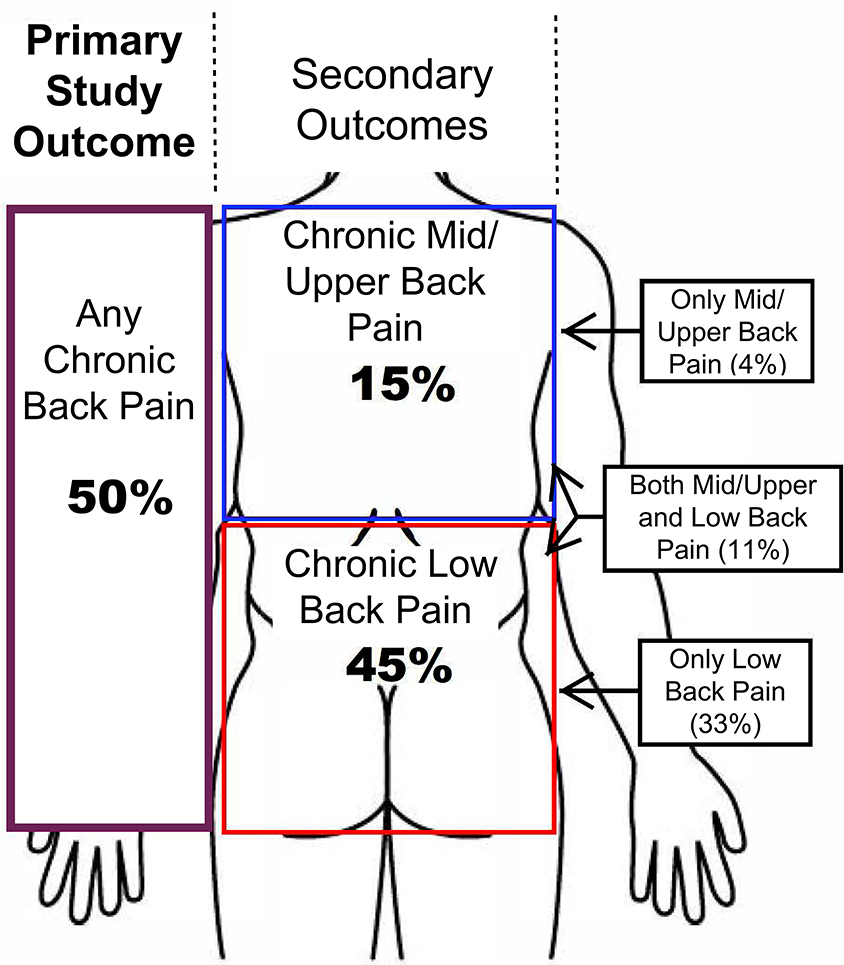
At 5-year follow-up, 110 participants (50%) reported incident CBP, the primary study outcome (Table 2, Figure 2). Of the 91 MZ pairs in the longitudinal study sample, there were 86 MZ pairs where both co-twins reported on the presence or absence of incident CBP at follow-up. Among these 86 MZ pairs, the 5-year incidence was 41% in those without baseline PTSD symptoms, and 64% in those with baseline PTSD symptoms. Mean back pain intensity in those with CBP was approximately 5 points on a 0–10 NRS scale, reflecting moderate levels of pain intensity, and mean back-related functional limitations were 24 points on a 0–100 Oswestry scale. The incidences of chronic low back pain and chronic mid/upper back pain were 45% and 15%, respectively (Table 2, Figure 2).
Table 2.
Incident chronic back pain over 5-Year follow-up (n=227)*
| n (%) with back pain outcome | Back pain intensity by locationa | Oswestry scoreb | |
|---|---|---|---|
| Primary outcome | |||
| Any chronic back painc (miss.=7) | 110 (50.0%) | 4.8 (2.0)d | 23.5 (1.6) |
| Secondary outcomes | |||
| Chronic low back pain (miss. =2) | 102 (45.3%) | 4.6 (1.9)e | 23.7 (14.5) |
| Chronic mid/upper back pain (miss.=8) | 33 (14.5%) | 5.2 (2.1)f | 25.3 (14.0) |
miss.= missing
chronic back pain defined as back pain of duration ≥ 3 months
back pain intensity (mean [SD]) on a 0 to 10 numerical pain scale with 0 being no pain and 10 being the worst pain possible.
Oswestry Disability Index (mean [SD]) on a 0 to 100 scale with 0 being no back-related functional limitations and 10 being the most severe functional limitations. Participants reported ODI items taking into account both pain in the low back, midback, and upper back regions.
In either the low back [lumbar] or mid/upper back [thoracic] regions
Scores reflect the worst pain intensity reported, between the low back and/or mid/upper back locations
Pain intensity scores for low back pain
Pain intensity scores for mid/upper back pain
Figure 2.
Incidence of chronic back pain at 5-year follow-up.
In bivariable within-pair analyses (accounting for familial factors), baseline PTSD symptoms were significantly associated with incident CBP at 5-year follow-up (RR 1.6 [95% CI 1.2–2.1]; p=0.001) (Table 3). The only covariate that met criteria for confounding using the ≥10% change-in-estimate method was VA service-connected disability (data not shown). Within-pair multivariable analyses adjusting for VA service-connected disability yielded nearly the same estimate of association as the bivariable analyses (RR 1.5 [95% CI 1.2–2.1]; p=0.002) (Table 3). Significant associations were also seen between baseline PTSD symptoms and the secondary back pain outcomes (Table 3), although the magnitude of association with incident chronic mid/upper back pain (multivariate-adjusted RR 2.7 [95% CI 1.1–6.3]; p=0.02) was larger than that with incident chronic low back pain (multivariate-adjusted RR 1.6 [95% CI 1.2–2.1]; p=0.001).
Table 3.
Baseline PTSD symptoms and risk of incident chronic back pain over 5-Year follow-up*
| Bivariable associationsa | Multivariable-adjusted associationsab | ||||
|---|---|---|---|---|---|
| n of total complete pairs | RR (95% CI) | p value | RR (95% CI) | p value | |
| Primary outcome | |||||
| Any chronic back painc | 83 | 1.6 (1.2–2.1) | 0.001 | 1.5 (1.2–2.0) | 0.002 |
| Secondary outcomes | |||||
| Chronic low back pain | 91 | 1.6 (1.2–2.1) | 0.001 | 1.6 (1.2–2.1) | 0.001 |
| Chronic mid/upper back pain | 83 | 3.7 (1.6–8.2) | 0.002 | 2.7 (1.1–6.3) | 0.02 |
n=sample size, RR= risk ratio of incident chronic back pain with baseline PTSD symptoms*
PTSD (post-traumatic stress disorder) symptoms defined as PCL≥30 at baseline. Chronic back pain is defined as back pain of duration ≥ 3 months.
Within-pair analyses of associations of PTSD symptoms with each back pain outcome, from generalized linear models in which twins are compared to their co-twins.
Adjustment for having received or applied for Veterans Affairs (VA) service connection
Back pain in either of the low back [lumbar] or mid/upper back [thoracic] regions
DISCUSSION
In this longitudinal study, baseline symptoms of PTSD were strongly associated with incident CBP at 5-year follow-up. This relationship was seen in within-MZ-pair analyses that control for genetics and early family environment, as well as unmeasured confounding factors. These results suggest that PTSD symptoms are a possible etiologic factor for CBP and not due to confounding by other factors.
Two prior longitudinal studies in clinical samples of patients with back pain have shown links with PTSD. In patients with incident low back pain in a military medical center, PTSD conferred a 3-fold greater odds of acute back pain developing into CBP at 6 months follow-up45. PTSD also predicted a 4-fold greater odds of future surgery in patients with CBP46. Our findings build upon this earlier work in 2 important ways. First, our study followed a non-clinical sample of those without back pain at baseline, establishing a clear temporal sequence of PTSD symptoms preceding the onset of CBP. Although in the military context PTSD and back pain may coexist due to combat-related physical injuries acting as the traumatic event triggering PTSD, while also directly injuring the spinal structures, this would not be expected in our study of older male Veterans who had left military service decades ago. Second, our work used a genetically informative sample that allowed us to determine that the PTSD-incident CBP association was present even after controlling for genetics, early family environment, and unmeasured confounders shared by MZ twins. These results add to findings from an earlier cross-sectional twin study by our group demonstrating that the association of PTSD and CBP persists once familial factors are accounted for,25 and are consistent with studies of pain perception which show greater sensitivity to painful stimuli in subjects with PTSD and traumatic events compared with controls,47,48 Taken together with prior work, the current findings suggest the possibility that PTSD symptoms may have causal effects on CBP. Since effective psychologic and pharmacologic treatments exist for improving PTSD symptoms,49–51 PTSD symptoms may be a potentially modifiable target of interventions to reduce the downstream risk of CBP. However, since PTSD symptoms should be treated for their mental health implications anyways, a more relevant implication for clinical practice may be that PTSD symptoms can be used to identify a subgroup of patients likely to experience future CBP; these at-risk individuals can be prepared to anticipate, respond to, and manage future back pain episodes. Such screening would be quite feasible to implement in the VA healthcare system, where PTSD symptoms are routinely screened for.52
To our knowledge, this is the first longitudinal co-twin control study to show a significant association between a psychological risk factor and incident back pain in within-MZ-pair analyses. A recent study by Pinheiro et al. found no significant associations between symptoms of depression/anxiety and incident chronic low back pain in longitudinal within-twin pair analyses, calling into question a causal effect of depression on future back pain.22 The contrasting results between our work and that of Pinheiro et al. may be because elevated PTSD symptoms affect back pain differently than do depression/anxiety. Another explanation for the null findings of Pinheiro et al. as noted by the authors was limited statistical power due to a small number of twin pairs discordant for the outcome of back pain.22 This limitation is very common in longitudinal co-twin control studies of binary outcomes, where statistical power is driven mainly by the number of outcome-discordant twin pairs with complete data for exposures, outcomes, and covariates. Our study design resulted in exposure and outcome frequencies close to 50% and adequate statistical power, despite modest within-MZ-pair sample sizes.22,23 Another potential limitation of the longitudinal co-twin control design using binary outcomes is the typical practice of restricting the baseline sample to twin pairs where both co-twins do not have the outcome at baseline, as was done in our study. Restriction to twin pairs concordant for absence of disease may define a baseline study sample that is enriched for those genetically predisposed to not having a particular disease,53 and bias towards a null association in studies of environmental risk factors for a condition. This makes our finding of a significant association between PTSD and incident chronic back pain all the more noteworthy. Multiple specific biological mechanisms have been proposed for how PTSD-related pathophysiologic changes may maintain or amplify the experience of pain, involving neurohormones, neurotransmitters, and inflammatory mechanisms, all of which are active areas of current research.54
Strengths of the current study include the longitudinal design, the unique ability of the co-twin control design to adjust for genetics and early family environment, and the use of accepted and validated measures for PTSD symptoms37 and back pain.39 Potential limitations include the use of surveys to ascertain CBP status, rather than structured interviews, and the reliance on recalled pain, the accuracy of which decreases according to the length of the recall period.55 In addition, the definition used to identify a cohort free of CBP at the study baseline did not specify a minimum duration of pain needed to count as ‘chronic’, and was formulated differently than the NIH task force-recommended questions used at 5-year follow-up.39 We expect that any such potential misclassification resulting from this would not occur differentially by current PTSD status, and therefore would have had minimal effects on our overall results, if any. Another potential limitation of our study was a low response rate at follow-up (66%), which was likely due in part to the long (5-year) follow-up period involved. Loss to follow-up could possibly create selection bias if the PTSD-back pain association differed in those lost to follow-up compared to those who completed follow-up. Since our study included US Veterans only, and the majority of participants were white, further studies will be needed to see whether our findings are generalizable to non-Veterans, non-whites, and populations outside the US.
In summary, this co-twin control analysis demonstrated strong associations (RRs 1.5–2.7) between PTSD symptoms and the development of incident CBP even after accounting for familial factors. These data suggest that PTSD symptom severity might be a potential modifiable risk factor for chronic thoracolumbar back pain.
This is the first longitudinal co-twin control study of post-traumatic stress disorder (PTSD) and back pain.
The association of PTSD symptoms with incident chronic back pain at 5-year follow-up is independent of genetic and familial factors.
PTSD symptoms may be a modifiable risk factor for chronic back pain.
Funding sources and acknowledgements
Drs. Suri, Boyko, Smith, Goldberg, Haselkorn, and William’s participation in this study was funded by VA Puget Sound Health Care System. The creation and the ongoing development, management, and maintenance of the Vietnam-Era Twin (VET) Registry (CSP #256) is supported by the Cooperative Studies Program (CSP) of the United States Department of Veterans Affairs (VA) Office of Research & Development. VET Registry data included in this article was supported by funding for CSP #569: The Course and Consequences of PTSD in Vietnam Era Twins, and a Career Development Award #1IK2RX001515 to Dr. Suri from VA Rehabilitation Research and Development. Most importantly, the authors gratefully acknowledge the continued cooperation and participation of the members of the VET Registry and their families. Without their contribution this research would not have been possible. All statements and opinions are solely of the authors and do not necessarily reflect the position or policy of the VET Registry, the VA, or the United States Government. The authors report no financial arrangements that may represent a possible conflict of interest with the work presented.
All VET Registry study procedures were approved by the Veterans’ Affairs (VA) Puget Sound Health Care System Institutional Review Board.
REFERENCES
- 1.Centers for Disease Control (CDC). National Ambulatory Medical Care Survey: 2010 Summary Tables], 2010. Available at: http://www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_namcs_web_tables.pdf. Accessed 10/8/2015, 2015.
- 2.Hoy D, March L, Brooks P, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73:968–74. [DOI] [PubMed] [Google Scholar]
- 3.Carroll LJ, Cassidy JD, Cote P. Depression as a risk factor for onset of an episode of troublesome neck and low back pain. Pain 2004;107:134–9. [DOI] [PubMed] [Google Scholar]
- 4.Croft PR, Papageorgiou AC, Ferry S, et al. Psychologic distress and low back pain. Evidence from a prospective study in the general population. Spine 1995;20:2731–7. [DOI] [PubMed] [Google Scholar]
- 5.Chou R, Shekelle P. Will this patient develop persistent disabling low back pain? Jama 2010;303:1295–302. [DOI] [PubMed] [Google Scholar]
- 6.Pincus T, Burton AK, Vogel S, et al. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine 2002;27:E109–20. [DOI] [PubMed] [Google Scholar]
- 7.Keeley P, Creed F, Tomenson B, et al. Psychosocial predictors of health-related quality of life and health service utilisation in people with chronic low back pain. Pain 2008;135:142–50. [DOI] [PubMed] [Google Scholar]
- 8.Baumeister H, Knecht A, Hutter N. Direct and indirect costs in persons with chronic back pain and comorbid mental disorders--a systematic review. Journal of psychosomatic research 2012;73:79–85. [DOI] [PubMed] [Google Scholar]
- 9.Sinnott P, Wagner TH. Low back pain in VA users. Arch Intern Med 2009;169:1338–9; author reply 9. [DOI] [PubMed] [Google Scholar]
- 10.Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. The Australian and New Zealand journal of psychiatry 2010;44:4–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alschuler KN, Otis JD. Coping strategies and beliefs about pain in veterans with comorbid chronic pain and significant levels of posttraumatic stress disorder symptoms. Eur J Pain 2011. [DOI] [PubMed] [Google Scholar]
- 12.Lew HL, Otis JD, Tun C, et al. Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: polytrauma clinical triad. J Rehabil Res Dev 2009;46:697–702. [DOI] [PubMed] [Google Scholar]
- 13.Asmundson GJ, Katz J. Understanding the co-occurrence of anxiety disorders and chronic pain: state-of-the-art. Depress Anxiety 2009;26:888–901. [DOI] [PubMed] [Google Scholar]
- 14.Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: mutual maintenance? Clinical psychology review 2001;21:857–77. [DOI] [PubMed] [Google Scholar]
- 15.Otis JD, Keane TM, Kerns RD. An examination of the relationship between chronic pain and post-traumatic stress disorder. Journal of rehabilitation research and development 2003;40:397–405. [DOI] [PubMed] [Google Scholar]
- 16.Polderman TJ, Benyamin B, de Leeuw CA, et al. Meta-analysis of the heritability of human traits based on fifty years of twin studies. Nat Genet 2015;47:702–9. [DOI] [PubMed] [Google Scholar]
- 17.Polderman TJ, Benyamin B, de Leeuw CA, et al. MaTCH (Meta-analysis of Twin Correlations and Heritability) web application], 2017. Available at: http://match.ctglab.nl/#/specific/plot1. Accessed May 25, 2017.
- 18.Ferreira PH, Beckenkamp P, Maher CG, et al. Nature or nurture in low back pain? Results of a systematic review of studies based on twin samples. Eur J Pain 2013. [DOI] [PubMed] [Google Scholar]
- 19.True WR, Rice J, Eisen SA, et al. A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry 1993;50:257–64. [DOI] [PubMed] [Google Scholar]
- 20.Sartor CE, Grant JD, Lynskey MT, et al. Common heritable contributions to low-risk trauma, high-risk trauma, posttraumatic stress disorder, and major depression. Arch Gen Psychiatry 2012;69:293–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pinheiro MB, Ferreira ML, Refshauge K, et al. Genetics and the environment affect the relationship between depression and low back pain: a co-twin control study of Spanish twins. Pain 2015;156:496–503. [DOI] [PubMed] [Google Scholar]
- 22.Pinheiro MB, Ferreira ML, Refshauge K, et al. Symptoms of Depression and Risk of Low Back Pain: A Prospective Co-Twin Study. Clin J Pain 2017;33:777–85. [DOI] [PubMed] [Google Scholar]
- 23.Fernandez M, Colodro-Conde L, Hartvigsen J, et al. Chronic low back pain and the risk of depression or anxiety symptoms: insights from a longitudinal twin study. Spine J 2017;17:905–12. [DOI] [PubMed] [Google Scholar]
- 24.Eisen S, True W, Goldberg J, et al. The Vietnam Era Twin (VET) Registry: method of construction. Acta geneticae medicae et gemellologiae 1987;36:61–6. [DOI] [PubMed] [Google Scholar]
- 25.Suri P, Boyko EJ, Smith NL, et al. Modifiable risk factors for chronic back pain: insights using the co-twin control design. Spine J 2017;17:4–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goldberg J, Curran B, Vitek ME, et al. The Vietnam Era Twin Registry. Twin research : the official journal of the International Society for Twin Studies 2002;5:476–81. [DOI] [PubMed] [Google Scholar]
- 27.Tsai M, Mori AM, Forsberg CW, et al. The Vietnam Era Twin Registry: a quarter century of progress. Twin Res Hum Genet 2013;16:429–36. [DOI] [PubMed] [Google Scholar]
- 28.Forsberg CW, Goldberg J, Sporleder J, et al. Determining zygosity in the Vietnam era twin registry: an update. Twin Res Hum Genet 2010;13:461–4. [DOI] [PubMed] [Google Scholar]
- 29.Goldberg J, True WR, Eisen SA, et al. A twin study of the effects of the Vietnam War on posttraumatic stress disorder. JAMA : the journal of the American Medical Association 1990;263:1227–32. [PubMed] [Google Scholar]
- 30.Goldberg J, Curran B, Vitek ME, et al. The Vietnam Era Twin Registry. Twin research : the official journal of the International Society for Twin Studies 2002;5:476–81. [DOI] [PubMed] [Google Scholar]
- 31.Norris FH, Hamblen JL. Standardized self-report measures of civilian trauma and PTSD In Wilson JP, Keane TM, Martin T eds. Assessing psychological trauma and PTSD. New York: Guilford Press, 2004:63–102. [Google Scholar]
- 32.Campbell KA, Rohlman DS, Storzbach D, et al. Test-retest reliability of psychological and neurobehavioral tests self-administered by computer. Assessment 1999;6:21–32. [DOI] [PubMed] [Google Scholar]
- 33.Keen SM, Kutter CJ, Niles BL, et al. Psychometric properties of PTSD Checklist in sample of male veterans. Journal of rehabilitation research and development 2008;45:465–74. [DOI] [PubMed] [Google Scholar]
- 34.Blanchard EB, Jones-Alexander J, Buckley TC, et al. Psychometric properties of the PTSD Checklist (PCL). Behaviour research and therapy 1996;34:669–73. [DOI] [PubMed] [Google Scholar]
- 35.Yeager DE, Magruder KM, Knapp RG, et al. Performance characteristics of the posttraumatic stress disorder checklist and SPAN in Veterans Affairs primary care settings. General hospital psychiatry 2007;29:294–301. [DOI] [PubMed] [Google Scholar]
- 36.Magruder K, Yeager D, Goldberg J, et al. Diagnostic performance of the PTSD checklist and the Vietnam Era Twin Registry PTSD scale. Epidemiol Psychiatr Sci 2015;24:415–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.VA. Using the PTSD Checklist for DSM-IV (PCL) ], 2013. Available at: http://www.ptsd.va.gov/professional/pages/assessments/assessment-pdf/pcl-handout.pdf. Accessed 1/7/2015, 2015.
- 38.Kroenke K, Spitzer RL, Williams JB, et al. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. General hospital psychiatry 2010;32:345–59. [DOI] [PubMed] [Google Scholar]
- 39.Deyo RA, Dworkin SF, Amtmann D, et al. Report of the NIH task force on research standards for chronic low back pain. Spine (Phila Pa 1976) 2014;39:1128–43. [DOI] [PubMed] [Google Scholar]
- 40.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine 2000;25:2940–52; discussion 52. [DOI] [PubMed] [Google Scholar]
- 41.Greenland S Modeling and variable selection in epidemiologic analysis. Am J Public Health 1989;79:340–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Suri P, Boyko EJ, Goldberg J, et al. Longitudinal associations between incident lumbar spine MRI findings and chronic low back pain or radicular symptoms: retrospective analysis of data from the longitudinal assessment of imaging and disability of the back (LAIDBACK). BMC musculoskeletal disorders 2014;15:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ferguson CJ. An Effect Size Primer: A Guide for Clinicians and Researchers. Professional Psychology: Research and Practice 2009;40:532–8. [Google Scholar]
- 44.Noss A Household Income for States: 2010 and 2011 [American Community Service Briefs], 2012. Available at: https://www.census.gov/prod/2012pubs/acsbr11-02.pdf. Accessed 1/7/2016, 2016.
- 45.Shaw WS, Means-Christensen AJ, Slater MA, et al. Psychiatric disorders and risk of transition to chronicity in men with first onset low back pain. Pain medicine (Malden, Mass 2010;11:1391–400. [DOI] [PubMed] [Google Scholar]
- 46.Dersh J, Mayer T, Theodore BR, et al. Do psychiatric disorders first appear preinjury or postinjury in chronic disabling occupational spinal disorders? Spine 2007;32:1045–51. [DOI] [PubMed] [Google Scholar]
- 47.Defrin R, Ginzburg K, Solomon Z, et al. Quantitative testing of pain perception in subjects with PTSD--implications for the mechanism of the coexistence between PTSD and chronic pain. Pain 2008;138:450–9. [DOI] [PubMed] [Google Scholar]
- 48.Tesarz J, Gerhardt A, Leisner S, et al. Distinct quantitative sensory testing profiles in nonspecific chronic back pain subjects with and without psychological trauma. Pain 2015;156:577–86. [DOI] [PubMed] [Google Scholar]
- 49.Bisson JI, Roberts NP, Andrew M, et al. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev 2013:CD003388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stein DJ, Ipser JC, Seedat S. Pharmacotherapy for post traumatic stress disorder (PTSD). Cochrane Database Syst Rev 2006:CD002795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barrera TL, Mott JM, Hofstein RF, et al. A meta-analytic review of exposure in group cognitive behavioral therapy for posttraumatic stress disorder. Clin Psychol Rev 2013;33:24–32. [DOI] [PubMed] [Google Scholar]
- 52.Spoont MR, Williams JW Jr., Kehle-Forbes S, et al. Does This Patient Have Posttraumatic Stress Disorder?: Rational Clinical Examination Systematic Review. JAMA 2015;314:501–10. [DOI] [PubMed] [Google Scholar]
- 53.Tan Q, Li W, Vandin F. Disease-Concordant Twins Empower Genetic Association Studies. Ann Hum Genet 2017;81:20–6. [DOI] [PubMed] [Google Scholar]
- 54.Scioli-Salter ER, Forman DE, Otis JD, et al. The shared neuroanatomy and neurobiology of comorbid chronic pain and PTSD: therapeutic implications. The Clinical journal of pain 2015;31:363–74. [DOI] [PubMed] [Google Scholar]
- 55.Stull DE, Leidy NK, Parasuraman B, et al. Optimal recall periods for patient-reported outcomes: challenges and potential solutions. Curr Med Res Opin 2009;25:929–42. [DOI] [PubMed] [Google Scholar]