Abstract
Introduction
Cancer Immunotherapy has recently emerged as a promising and effective modality to treat different malignancies. Antigenic profiling of cancer tissues and determination of any pre-existing immune responses to cancer antigens may help predict responses to immune intervention in cancer. NY-ESO-1, a cancer testis antigen is the most immunogenic antigen to date. The promise of NY-ESO-1 as a candidate for specific immune recognition of cancer comes from its restricted expression in normal adult tissue but frequent occurrence in multiple tumors including melanoma and carcinomas of lung, esophageal, liver, gastric, prostrate, ovarian, and bladder.
Main body
This review summarizes current knowledge of NY-ESO-1 as efficient biomarker and target of immunotherapy. It also addresses limitations and challenges preventing a robust immune response to NY-ESO-1 expressing cancers, and describes pre-clinical and clinical observations relevant to NY-ESO-1 immunity, holding potential therapeutic relevance for cancer treatment.
Conclusion
NY-ESO-1 induces strong immune responses in cancer patients but has limited objective clinical responses to NY-ESO-1 expressing tumors due to effect of competitive negative signaling from immune-checkpoints and immune-suppressive tumor microenvironment. We propose that combination therapy to increase the efficacy of NY-ESO-1 specific immunotherapeutic interventions should be explored to unleash the immune response against NY-ESO-1 expressing tumors.
Keywords: Cancer immunotherapy, Cancer testis antigen, Cancer vaccine, Immune checkpoint inhibitors, NY-ESO-1, Tumor microenvironment
Introduction
Carcinogenesis may often lead to the expression of neo-antigens recognized, under certain conditions, by the immune system [1]. However, expression of tumor-associated antigens (TAA) does not commonly lead to effective tumor cell eradication due to inconsistent expression, immunological tolerance, lack of restriction to transformed tissues, low affinity of the TCR to the MHC/peptide complex or immunosuppressive microenvironment [2]. Different from most TAA, cancer testis antigens (CTA) are considered highly immunogenic due to their unique set of characteristics including restricted expression in immune privileged organs, stable expression on tumor tissues and ability to encode immunogenic antigens to cancer [3]. To date, an estimated 250 proteins associated with CTA group have been documented [4]. Of these, NY-ESO-1 is a particularly promising target for immunotherapy due to its high and frequent expression in malignancies and its ability to elicit potent integrated natural humoral and cellular responses [5]. This has led to a number of pre-clinical studies and clinical trials (completed and ongoing) exploring the potential efficacy of immunotherapeutic strategies against NY-ESO-1 expressing tumors [6]. Here, we aim to provide an in-depth perspective on NY-ESO-1 as an efficient target for immunotherapy and describe its immunogenicity limitation and challenges that need to be addressed to unleash a robust immune response against cancers. Furthermore, this review will provide detailed perspectives on pre-clinical and clinical advances with relation to NY-ESO-1 that may have therapeutic potential in combination with standard therapies.
Structure, expression and regulation of NY-ESO-1
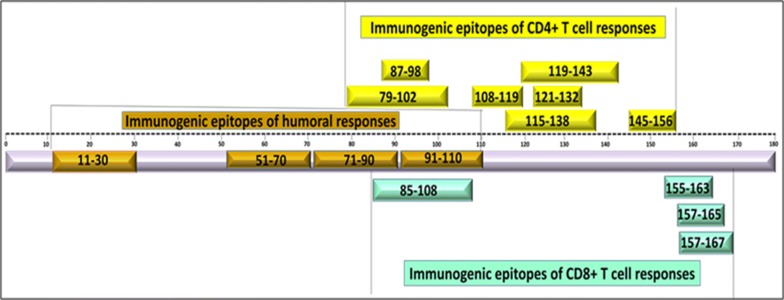
NY-ESO-1 belongs to Cancer Testis 6 antigen (CT6) family encoded by CTAG1 gene. Its gene maps to the Xq28 region of the X chromosome. Structurally, it is 180 amino acid long protein of 18 kDa, containing epitopes of humoral and cellular responses in its glycine rich N terminal region and an extremely hydrophobic C terminal region [7–9] (Fig. 1).
Fig. 1.
Schematic representation of amino acids representing immunogenic epitopes against anti-NY-ESO-1 antibody, CD4+ and CD8+ T cell responses. Naturally occurring anti-NY-ESO-1 antibodies are mostly mapping to soluble N-terminus region while the cellular responses are mapping to the C-terminus region [139]
In healthy individuals, the expression of NY-ESO-1 appears early at fetal level with germ cells of testis and ovaries expressing this antigen at 13–18 weeks, plateauing at 22–24 weeks and then decreasing rapidly [10]. Therefore, NY-ESO-1 is only expressed in immune privileged organs such as testis and placenta (in spermatogonia/oogonia). Since, testis/placenta do not express MHC alleles, NY-ESO-1 expression is lost during spermatid differentiation. Therefore, it is not expressed in normal healthy tissues. This is an important parameter as any therapeutic potential against NY-ESO-1 will not be restricted by implications of normal tissue damage [5].
In cancers, NY-ESO-1 expression is a consequence of epigenetic event that involves tightly controlled recruitment and sequential interaction of histone deacetylases, histone methyltransferase, DNA methyltransferases, and transcription factors. Mechanistically, formation of multi-protein complexes between HDAC1-mSin3A-NCOR1, Dnmt3b-HDAC1-Egr1and Dnmt1-PCNA-UHRF1-G9a have been reported as main players of NY-ESO-1 regulation [11].
Factors affecting NY-ESO-1 expression
The expression of NY-ESO-1 in cancers is a well-documented phenomenon with studies reporting that approximately 75% of cancer patients express this antigen at some stage during the course of their illness [12]. However, since tumor characteristics evolve during the course of the disease, it is important to understand that factors such as tumor stage, grade and therapeutic interventions are critical factors directing the expression of NY-ESO-1 in tumors [5, 13, 14]. For e.g. with respect to grade, NY-ESO-1 expression can vary from 0% in grade 1 to 44% in grade 4. Similarly, stage wise, variable expression of NY-ESO-1 has been reported in premalignant lesions, early stage and metastatic tumors [15, 16]. Global data indicates that in majority of tumors, NY-ESO-1 is frequently expressed in metastatic, high grade/advanced stage tumors and is as such associated with poor prognosis [17–21].
In addition to this, studies have also observed relationship between clinical course of disease and NY-ESO-1 expression. For e.g. patients with disease remission show variable patterns with some patients exhibiting antigen loss while others showing stable expression over time [12]. It is postulated that this variable expression pattern may be a result of interrelated tumor-immune dynamics including intra-tumoral heterogeneity, immuno-editing, or reduced tumor cell proliferation [5]. On the other hand, there are reports that therapeutic interventions such as radiotherapy or de-methylating agents enhance the release of NY-ESO-1 antigen from the tumor, and this in itself may play a critical role in directing tumor dynamics [22, 23].
Other factors such as culturing and detection methods are associated with its expression analysis and reporting. For e.g. NY-ESO-1 expression is usually higher in cell lines due to well-controlled homogenous culture conditions [24, 25]. Similarly, detection methods are an important parameter as this has direct effect on reporting of NY-ESO-1 expression. For e.g. reverse transcriptase PCR (RT PCR) and tissue microarray have been reported to give higher false positive/negative results due to variation in the homology/binding affinity of detection antibodies. Immunohistochemistry (IHC), on the other hand is considered a gold standard as its allows localized detection of NY-ESO-1 antigen in the cytoplasm of the tumor tissues [14]. Although, NY-ESO-1 antigen is always localized in the cytoplasm, some limited studies have also reported simultaneous expression of NY-ESO-1 in both nucleus and cytoplasm of tumor tissues. It is unclear if this simultaneous expression, observed in certain cancers, is a stable trait or varies over time [26–28].
Immunogenicity of NY-ESO-1
NY-ESO-1 humoral responses
The discovery of NY-ESO-1 was based on its capacity to induce detectable antibody response in cancer patients. Since its discovery, a large number of studies have documented aberrant expression of NY-ESO-1 in variable frequencies ranging from 10 to 50% among solid tumors, 25–50% of melanomas, and up to 80% in synovial sarcomas [7, 26–36]. A large scale serological study by Oshima et al. on 1969 specimens from patients with different cancer types reported highest frequency in esophageal cancer (32%), followed by lung cancer (13%), hepatocellular cancer (11%), prostate and gastric cancer (10%), colorectal cancer (8%) and breast cancer (7%) indicting the variable pattern of antibody response in different cancer types [37].
The predictive/prognostic utility of NY-ESO-1 antibody has been investigated by correlating the antibody levels with patient responses. Valuable observations with respect to antibody responses and tumor burden have been reported. Various studies have reported a pattern of antibody increase with disease progression that decreases with effective treatment [38]. For e.g. a study focusing on NY-ESO-1 antibody in 363 gastric cancers patients showed that NY-ESO-1 antibody was detected in 3.4% (6/176) of stage I, 4.4% (2/45) of stage II, 25.3% (17/67) of stage III and 20.0% (16/75) of stage IV gastric cancer patients, resulting in an overall detection rate of 11.1% (41 of 363). Interestingly, the study observed that patients who underwent surgery and did not suffer a subsequent relapse displayed consistent decreases or complete disappearance of NY-ESO-1 antibody from their sera [39]. Similarly, a study on 155 CRC patients (stage III or IV) reported that out of 24.5% of NY-ESO-1 antibody positive patients, 59 patients exhibited sera conversion after change in their clinical status. This is important evidence indicating correlation between clinical status and NY-ESO-1 humoral response [40].
Another study reported that out of 689 ovarian cancer patients tested, 19.0% that tested positive for NY-ESO-1 antibody exhibited higher stage/grade at presentation with more serous histology. These patients were found to have fewer complete responses to primary therapy with worse outcomes. Interestingly, the study observed that NY-ESO-1 positive patients on antigen-specific immunotherapy exhibited improved response and overall survival indicating that immune dynamics in NY-ESO-1 patients is modulated towards a better clinical trajectory using NY-ESO-1 specific targeted therapy [41].
Studies investigating the utility of NY-ESO-1 antibody as surrogate marker of response in cancers such as multiple myeloma, melanoma, gastric cancer, hepatocellular carcinoma, bladder, prostate cancer etc. have also been performed with promising results [35, 38, 39, 42–44]. For e.g. in synovial sarcoma, strong NY-ESO-1 expression is observed while in spindle cell neoplasms, NY-ESO-1 expression is rare. It is suggested that this distinct expression profile can help to distinguish these two types of sarcomas diagnostically [45]. Similarly, studies have suggested that NY-ESO-1 expression can serve as a sensitive and specific diagnostic biomarker in myxoid and round cell liposarcoma [46–48].
However, it should be noted that circulating antibodies against NY-ESO-1 cannot mediate direct anti-tumor responses. Instead, these antibodies facilitate the formation of immune complexes, with NY-ESO-1 protein, for effective cross presentation by dendritic cells [44]. It is well understood that, in NY-ESO-1 expressing tumors, key anti-tumor responses involve integrated antibody, CD4+ and CD8+ T cell responses leading to robust immune response with significant clinical benefit [49–52]. Interestingly, clinical trials have shown that, therapeutic interventions against NY-ESO-1(for e.g. vaccination) are capable of robust immune response and tumor control as compared to naturally occurring responses [53, 54]. This is an important understanding as it provides evidence that therapeutic boosting of humoral and cellular responses is a key control for NY-ESO-1 expressing tumors.
NY-ESO-1 cellular responses
Structurally, the epitopes for cellular response in NY-ESO-1 are clustered within its central (80–110 aa) and C terminal region (157–170 aa) [8, 9, 55] (Fig. 1). These epitopes are considered highly immunogenic with capability of eliciting potent CD4+ and CD8+ T cell responses [54]. A number of clinical trials have evidenced on the role of NY-ESO-1 cellular responses in driving therapeutic benefits in patients. For e.g. immunization in patients with NY-ESO-1 specific peptides has shown to induce potent CD8+ T cell responses leading to regression and disease stabilization in such patients [51, 56–58]. Another study on full length NY-ESO-1 protein vaccine showed induction of integrated humoral and cellular responses with clinical benefit and overall/progression free survival [55].
Factors limiting immunogenic potential of NY-ESO-1
Although, a highly promising therapeutic antigen, there are several factors that limit the induction of efficient responses against NY-ESO-1 expressing tumors including (a) tumor evasion from immune recognition, (b) inefficient induction of high affinity adaptive immunity and (c) tumor induced immunosuppression [59–63]. A number of studies have documented these factors in limiting control of NY-ESO-1 expressing tumors. For e.g. Lotta von Boehmer et al. evidenced this in a case of NY-ESO-1 expressing melanoma patient who was started on anti-NY-ESO-1 specific vaccines for tumor control. Though immune responses were boosted initially in the patient, some lesions continued to grow. On the other hand, with lesions still progressing, the expression of NY-ESO-1 on tumor cells was found to be lost with reduced specific CD8+ T cell response. Subsequent immunizations were unable to boost or recall these specific cellular responses. The study postulated that NY-ESO-1-specific immunological pressure/persistence of NY-ESO-1 negative cells lead to tumor evasion and ultimately tumor progression [60]. This complex relationship between NY-ESO-1 expressing tumors and the immune system has been demonstrated in other studies as well [64]. For e.g. in murine xenograft models of multiple myeloma, adoptive transfer of NY-ESO-1157-165/HLA-A*02:01-specific T cells was performed. Despite encouraging results for four mice, disease persistence was observed in two of the mice. The study reported a selective loss of HLA-A*02:01 expression indicating that loss of heterozygosity in MHC was the factor leading to immune escape against NY-ESO-1 specific intervention [65]. Similarly, biopsy analysis of 17 melanoma patients, who had relapsed after NY-ESO-1 protein vaccination showed that 11/17 patients exhibited either NY-ESO-1 or HLA class I downregulation, indicating that alteration in tumor phenotype can lead to immune evasion and relapse [59].
On the other hand, several intrinsic and extrinsic immune suppressive mechanisms are reported to be involved in modulation of NY-ESO-1 specific immune responses. These include activation of immune checkpoints such as PD-1, CTLA-4 etc. and infiltration of suppressive cells such as regulatory T cells (Tregs), myeloid-derived suppressor cells (MDSC), various cytokines and chemokines [65–68]. Many studies have documented the restrictive abilities of these cells in CD4+ T cell activation and CD8+ priming thus limiting cellular responses against NY-ESO-1 [69–72]. For e.g. NY-ESO-1 positive patients with high frequencies of circulating CD25+ high/FOXP3+ Tregs and CD14+/CD11b+/HLA-DR−/low MDSCs exhibited poor response to therapeutic intervention. On the other hand, patients with low MDSCs and higher tumor infiltrating lymphocytes (TIL), were showed improved prognosis [71, 73, 74]. Similarly, Tregs depletion by anti-CD25 antibodies has been shown to enhance anti-tumor responses in murine models [75, 76]. Furthermore, therapeutic interventions targeting checkpoint molecules (for e.g anti-PD-1, anti-CTLA-4) work by blocking negative pathways and enhancing anti-NY-ESO-1 specific immunity [67, 77–81].
Therefore, It is clear that various factors influence and direct NY-ESO-1 mediated responses. Thus, immunotherapeutic interventions keeping these factors in perspective could facilitate potentiation of anti-NY-ESO-1 immunogenicity.
Current pre-clinical and clinical trials of NY-ESO-1 antigen
The potential of NY-ESO-1 antigen to generate integrated humoral and cellular responses have paved the way for various pre-clinical studies and clinical trials. Most studies are focused on generation of NY-ESO-1-specific TCR gene transduced T lymphocytes, humanized engineered antibodies and combination of NY-ESO-1 petides/proteins with biological agents such as oncolytic viruses and antibody drug conjugate natural dendritic cells, gene modified viruses/bacterial vectors etc. (Tables 1, 2) [82].
Table 1.
Completed clinical trials targeting New York esophageal squamous cell carcinoma-1(NY-ESO-1) antigen
| Immunotherapeutic strategy | Adjuvant/interventions | Indications | Phase | Trial ID |
|---|---|---|---|---|
| NY-ESO-1 protein vaccine | CpG 7909 | Advanced prostate cancer | 1 | NCT00292045 |
| Cholesteryl pullulan(CHP) + CHP HER2 + OK-432 | Esophageal cancer, lung cancer, stomach cancer, breast cancer, ovarian cancer | 1 | NCT00291473 | |
| Glucopyranosyl lipid adjuvant stable emulsion (GLA-SE) | Melanoma, ovarian cancer, sarcoma non-small cell lung cancer, breast cancer | 1 | NCT02015416 | |
| Recombinant Fowl-Pox virus vector | Fallopian tube cancer, ovarian cancer, peritoneal cavity cancer | 2 | NCT00112957 | |
| Recombinant canarypox virus vector (ALVAC) 2 + TRIad of Co-stimulatory molecules B7-1, ICAM- and LFA-3. | Fallopian tube cancer, ovarian cancer, peritoneal cavity cancer | 1 | NCT00803569 | |
| ISCOMATRIX | Melanoma | 2 | NCT00518206 | |
| Imiquimod | Malignant melanoma | 1 | NCT00142454 | |
| NY-ESO-1 peptide vaccine | Montanide, montanide + carboxymethylcellulose, polyinosinic-polycytidylic acid, and poly-l-lysine (Poly-ICLC) | Epithelial ovarian cancer, fallopian tube cancer, primary peritoneal cancer | 1 | NCT00616941 |
| CpG 7909 + montanide ISA-51 | Stage III/IV;resected Stage II, III, or IV non-small cell lung cancer or esophageal cancer | 1 | NCT00199836 | |
| None | Prostate cancer | 1 | NCT00616291 | |
| CpG 7909, CpG 7909 + montanide ISA 720 | All NY-ESO-1 expressing tumors | 1 | NCT00819806 | |
| BCG vaccine, sargramostim | Bladder cancer | 1 | NCT00070070 | |
| Resiquimod | Melanoma | 1 | NCT00470379 | |
| NY-ESO-1 TCR | Palliative radiation therapy | Sarcoma | 1 | NCT02319824 |
| NY-ESO-1 specific monoclonal antibody | Resiquimod and/or carboxymethylcellulose, polyinosinic-polycytidylic acid, and poly-l-lysine (poly-ICLC) | Advanced malignancies | 1 and 2 | NCT00948961 |
Table 2.
On-going clinical trials targeting New York esophageal squamous cell carcinoma-1 (NY-ESO-1) antigen
| Immunotherapeutic strategy | Adjuvant/interventions | Indications | Phase | Trial ID |
|---|---|---|---|---|
| Anti-NY-ESO-1 TCR | Cyclophosphamide | Synovial sarcoma, melanoma, esophageal cancer, ovarian cancer, lung cancer, bladder cancer, liver cancer | 1 | NCT02869217 |
| Cyclophosphamide + transforming growth factor-beta receptor II (TGFbDNRII)-transduced autologous tumor infiltrating lymphocytes | Adult solid neoplasm | 1 and 2 | NCT02650986 | |
| Cyclophosphamide | Bone Sarcoma, soft tissue sarcoma, melanoma, liver cancer, esophageal cancer, breast cancer, thyroid cancer, ovarian cancer | 1 | NCT03159585 | |
| None | Advanced malignant solid tumors | 1 | NCT03047811 | |
| Cyclophosphamide, fludarabine | Bladder carcinoma, breast cancer, esophagus carcinoma, lung cancer, melanoma, multiple myeloma, neuroblastoma, ovarian cancer, synovial sarcoma, other metastatic solid cancers | 1 | NCT02457650 | |
| Aldesleukin, cyclophosphamide, decitabine | Recurrent fallopian tube carcinoma, recurrent ovarian carcinoma, recurrent primary peritoneal carcinoma | 1 | NCT03017131 | |
| Cyclophosphamide | Lung cancer, non-small cell lung cancer | NCT03029273 | ||
| Pembrolizumab | Multiple myeloma | 1 | NCT03168438 | |
|
NY-ESO-1 TCR + NY-ESO-1 peptide Vaccine |
Aldesleukin, cyclophosphamide, fludarabine phosphate, nivolumab | Neoplasms | 1 | NCT02775292 |
|
NY-ESO-1 TCR+ NY-ESO-1 protein vaccine |
Cyclophosphamide, fludarabine phosphate, aldesleukin, radiation | Solid tumors | 1 | NCT02366546 |
| NY-ESO-1 protein vaccine | Atezolizumab, guadecitabine, carboxymethylcellulose, polyinosinic-polycytidylic acid, and poly-l-lysine (Poly ICLC) |
Recurrent fallopian tube carcinoma Recurrent ovarian carcinoma Recurrent primary peritoneal carcinoma |
1 and 2 | NCT03206047 |
| NY-ESO-1 peptide vaccine | Montanide ISA-51, polyinosinic-polycytidylic acid, and poly-l-lysine (Poly ICLC), Cyclophosphamide, Fludarabine, Interleukin-2 | Melanoma | 2 | NCT02334735 |
Pre-clinical studies on plasmid DNA vaccine, encoding NY-ESO-1 epitopes, has shown induction of prophylactic anti-tumor cytotoxic T cell immune responses in vivo [83]. SCIB2, a DNA vaccine, encoding human IgG1 antibody, with 16 NY-ESO-1 epitopes (nested within the four regions of NY-ESO-1 covering the most common class I and class II haplotypes) has shown promising results in transgenic mice [84]. SCIB2 DNA constructs were found to induce CD4+/CD8+ T cell responses to NY-ESO-1 epitopes with long term survival in 35% of mice. Interestingly, enhanced antitumor responses with 100% long-term survival was observed when SCIB2 was used in combination with checkpoint inhibitors (anti-CTLA-4 and anti-PD-1 antibodies) [84]. Similarly, preclinical study on immunization of lung cancer mouse models with dendritic cell-targeting integration deficient based lentiviral vector), called LV305 demonstrated favorable results [85]. LV305, engineered to deliver NY-ESO-1 gene to human dendritic cells in vivo lead to presentation of NY-ESO-1 antigen peptides to naïve CD8+ T cells via MHC class I. Robust tumor specific cytotoxic T cell response against NY-ESO-1 expressing tumor with significant inhibition of metastatic lung nodule growth was reported in this study [85, 86]. Following the success of preclinical studies, recent phase 1 vaccination trial evaluating LV305 in NY-ESO-1 expressing solid tumors also showed promising results. LV305, was found to selectively induce NY-ESO-1 specific expression in dendritic cells and promoting tumor responses in patients [87]. Similarly, phase 1 study in synovial and myxoid round cell liposarcoma with CMB305 vaccine containing LV305 was shown to prime NY-ESO-1 specific T cell responses leading to enhanced overall survival [88].
Monoclonal antibodies (mAbs) against tumor-associated antigens have also shown promising results. Preclinical studies on combination therapy of NY-ESO-1 specific antibody, 12D7, with chemotherapy has shown to enhance efficacy of chemotherapy via local release of antigens by chemo- or radiotherapy. The released antigen forms an immune complex with mAbs, thus, allowing uptake and presentation of antigen-derived peptides by tumor associated dendritic cells leading to activation of tumor-specific CD8+ T cells [89]. Recently, new approaches, such as use of oncolytic viruses and antibody drug conjugates to target NY-ESO-1 have shown favorable results. For e.g. a study on human melanoma cell lines infected with oncolytic viruses (measles virus, vaccinia virus, vesicular stomatitis virus, herpes simplex type 1 virus, adenovirus or enterovirus) was able to stimulate anti-tumor immune response by inducing the release of NY-ESO-1. The released antigen captured by tumor cells and presented through HLA class 11 pathways leads to cytotoxicity activity and tumor lysis [90]. Furthermore, antibody drug conjugates, such as anti-CD-33 antibody drug conjugate, anti-CD30 antibody drug conjugates and anti-HER2 antibody conjugates have been shown to enhance antibody therapy against cancer cells. However, they have limited effect on intracellular protein. Therefore, novel TCR like antibodies have been developed that allow tumor specific antigens to go through MHC class 1 signaling to present it as tumor specific peptide/MHC complexes on tumor cell surface [91]. A study on NY-ESO-1 specific TCR like antibodies was shown to block recognition of NY-ESO-1/HLA-A2-positive tumour cells by NY-ESO-1peptide-specific CD8 + T cells thus enhancing tumour specific immunological response [92].
Another highly personalized therapeutic model involving NY-ESO-1 includes adoptive transfer of antigen-specific T cells (ACT) [93]. Clinical trials on adoptive transfer of T cells retro-virally transduced to express NY-ESO-1 T-cell repertoire (TCR) have been performed successfully for the treatment of melanoma and synovial sarcoma with response rates as high as 45% and 67% respectively. Furthermore, no on-target toxicities were observed in this trial indicating that ACT with TCRs directed against NY-ESO-1 is effective and safe at mediating tumor regression [94]. In addition to this, a clinical trial on multiple myeloma, utilizing ACT with TCRs directed against NY-ESO-1 showed encouraging results such as effective expansion of engineered T cells in vivo, efficient trafficking of T cells to disease site, long-term persistence/continued expression of TCR (for up to 2 years after infusion) and durable target-specific anti-tumor responses without significant safety concerns indicating clinical feasibility of NY-ESO-1 specific ACT for the management of myeloma [95]. Similarly, a pre-clinical study on glioblastoma, utilizing ACT with TCR directed against NY-ESO-1, in combination with Decitabine (DAC) chemotherapy has shown promising results [96]. Study results evidenced that prior administration of DAC to selectively up regulate NY-ESO-1 followed by ACT immunotherapy resulted in an efficient trafficking of NY-ESO-1-specific T cells towards tumor cells leading to survival advantage in mice [96]. Furthermore, phase I trial on chemo-immunotherapy, has been performed on relapsed/refractory solid tumors including Ewing’s sarcoma, osteosarcoma and rhabdomyosarcoma [97]. Chemo-immunotherapy phase I trial was based on combining DAC with a dendritic cell vaccine (DAC/DC-CT) targeting NY-ESO-1. DAC/DC-CT vaccine was well-tolerated, was able to elicit T cell responses in the majority of patients and achieved progression free survival in patients with minimum disease burden indicating the potential of chemo-immunotherapy in NY-ESO-1 expressing tumors [97].
Another well-known form of ACT, known as Chimeric Antigen Receptors (CARs) are constructed by linking variable regions of tumor-reactive antibody to intracellular signaling chains such as CD3-zeta, including costimulatory domains encoding CD28 or CD137 to fully activate T cells. The functional advantage of CARs is that it provides non-MHC–restricted recognition of cell surface components and can be introduced into T cells with high efficiency using viral vectors [93]. Pre-clinical data for the potential of CARs to be utilized for multiple myeloma has displayed encouraging results [98]. In this study, CARs recognizing the HLA-A*02:01/NY-ESO-1 peptide157-165 with intracellular moiety consisting of CD3z signaling domain (anti-NYESO-1-T1-CD3z) or a combined CD28/CD3z signaling domain (anti-NY-ESO-1-T1-CD28/CD3z) was generated. In cell lines, NY-ESO-1 specific cytolysis, IFNγ release, appearance of early and late effector T memory cells and differentiated effector T cells was observed. Furthermore, to observe the functional activity of anti-NY-ESO-1-T1-CD28/CD3z in vivo, a xenograft multiple myeloma mouse model was established. It was observed that mice were protected against tumor growth with measurable hIgE levels indicating the specificity of anti-NY-ESO-1-T1-CD28/CD3z T cells. In 40% of the blood samples, transduced T cells were present even after 30 days of treatment indicating a rationale for clinical trials against NY-ESO-1 positive myeloma cancer patients [98].
Improving therapeutic responses targeting NY-ESO-1
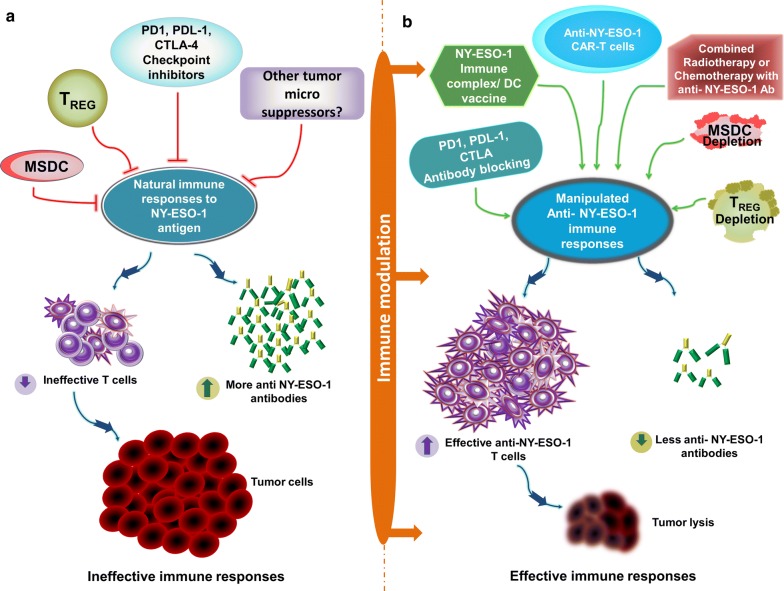
NY-ESO-1 is a highly immunogenic antigen with a potential to induce integrated humoral and cellular responses. As described in Fig. 2a, effective tumor control against NY-ESO-1 expressing tumors is compromised due to strong interplay of the immune checkpoint inhibitory molecules such as programmed death 1 [PD-1], programmed death-ligand 1[PDL-1], cytotoxic T-lymphocyte-associated protein 4 [CTLA-4],immune-suppressive cells such as regulatory T cells (TREG) and myeloid-derived suppressor cells (MDSC). Various strategies to improve and strengthen NY-ESO-1 specific therapeutic responses including (1) vaccination with NY-ESO-1 protein/peptides complexed with dendritic cells can help to stimulate T cells with infiltration of cytotoxic cells; (2) adoptive T cell therapy with anti-NY-ESO-1 chimeric antigen receptor T cells (CAR T) facilitates T-cell expansion with favorable changes within the tumor microenvironment for tumor control; (3) Immune checkpoint inhibitors (anti-PD-1, anti-PDL-1, anti-CTLA-4) block inhibitory signals between T cells and NY-ESO-1 expressing tumor cells thus enhancing cellular responses and facilitating tumor control; (4) Depletion/blocking of immunosuppressive Tregs and MDSCs modulate the tumor microenvironment enhancing NY-ESO-1 specific cytotoxic responses; (5) Combining standard of care therapies, radiotherapy, or chemotherapy, with vaccination/adoptive T cell therapy/immune checkpoint inhibitors can enhance anti-NY-ESO-1 T cells responses leading to effective tumor eradication and a successful clinical response (Fig. 2b).
Fig. 2.
Cancer Immunotherapeutic strategies targeting NY-ESO-1 antigen. a NY-ESO-1 exhibits the capacity to induce a strong natural anti-NY-ESO-1 antibody, CD4 + and CD8 + T cell responses in an integrated manner. Effective tumor control against NY-ESO-1 expressing tumors is compromised due to strong interplay of the immune checkpoint inhibitory molecules such as programmed death 1 [PD-1], programmed death-ligand 1 [PDL-1], cytotoxic T-lymphocyte-associated protein 4 [CTLA-4] and other immune-suppressive tumor microenvironment cells such as regulatory T cells (TREG) and myeloid-derived suppressor cells (MDSC). In the presence of these immune inhibitory and immune suppressive cells, high titers of anti-NY-ESO-1 antibodies are observed while the anti-NY-ESO-1 T cell responses become ineffective. This leads to limited objective clinical responses to control tumors. b To strengthen the induction of effective anti-NY-ESO-1 specific CD4 + and CD8 + T cell immune responses and to reverse immunosuppression, various immune-modulation strategies including anti-PD-1, anti-PDL-1, anti-CTLA-4 blocking antibodies, TREG and MDSC depletion, NY-ESO-1 immune complex/dendritic cells (DC) vaccine, anti-NY-ESO-1 chimeric antigen receptor T cells (CAR T), either alone or in combination with standard of care therapies such as radiotherapy and chemotherapy can be designed for enhanced anti-NY-ESO-1 T cells responses leading to effective tumor eradication and a successful clinical response
Conclusion
Comprehensive and compelling data from preclinical/clinical trials on NY-ESO-1 evidence its dynamic potential as a candidate for immunotherapy for a variety of malignancies. However, further trials and pre-clinical data are in the pipeline that will help to decipher its inherent and powerful immunological prowess to its full potential.
Future perspectives
The future of immunotherapy relies largely on selected tumor antigens such as NY-ESO-1 due to its natural ability to induce both humoral and cellular immune responses. The major aim of researchers now is to counter potential roadblocks in therapeutic pathways encompassing NY-ESO-1. This can potentially be achieved via combination therapy to increase the efficacy of NY-ESO-1 specific immunotherapeutic interventions including (a) vaccines in combination with Tregs depletion and/or blocking of immune checkpoint inhibitors; (b) adoptive T cell therapy with vaccination to boost T cell responses post adoptive transfer; (c) adoptive T cell therapy with immune checkpoint inhibitors/Tregs depletion; (d) antibodies in combination with vaccination/adoptive transfer; (e) NY-ESO-1 vaccine in combination with other cancer testis antigens and f) vaccination/ACT/antibodies in combination with standard of care therapies such as radiation, chemo-radiation and surgery. These strategies will not only enhance the immunogenic potential of NY-ESO-1 but will also be beneficial in overcoming resistance to therapeutic interventions.
Acknowledgements
The publication of this article was funded by the Qatar National Library.
Abbreviations
- NY-ESO-1
New York esophageal squamous cell carcinoma 1
- CTA
Cancer testis antigen
- TAA
Tumor-associated antigens
- TCR
T cell repertoire
- CT6
Cancer testis 6 antigen
- CSC
Cancer stem cells
- MSC
Mesenchymal stem cells
- RT-PCR
Reverse transcriptase PCR
- IHC
Immunohistochemistry
- APC
Antigen presenting cells
- Tregs
Regulatory T cells
- MDSC
Myeloid-derived suppressor cells
- ISCOMATRIX
Saponin based adjuvant
- CHP
Cholesteryl Pullulan
- Poly-ICLC
Polyinosinic-polycytidylic acid-poly-l-lysine carboxymethylcellulose
- MAbs
Monoclonal antibodies
- ACT
Antigen-specific T cells
- DAC
Decitabine
- PD-1
Programmed cell death protein 1
- PD-L1
Programmed death-ligand 1
- CTLA-4
Cytotoxic T-lymphocyte-associated protein 4
- CAR
Chimeric antigen receptor
Authors’ contributions
AR, SD, SK, MM and VP were responsible for conceiving the ideas. AR and SD wrote the manuscript, VP and RP were responsible for making the Figures and the Tables. ALR and SK provided critical input on the manuscript. All authors read and approved the final manuscript.
Funding
Financial support for the preparation of the article was provided by Medical Research Center, Hamad Medical Corporation, Doha, Qatar under the Grant Number 17118/17. The funding source had no involvement in the writing of the report; and in the decision to submit the article for publication.
Availability of data and materials
Not applicable.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Afsheen Raza, Email: ARaza@hamad.qa.
Maysaloun Merhi, Email: MMerhi@hamad.qa.
Varghese Philipose Inchakalody, Email: VInchakalody@hamad.qa.
Roopesh Krishnankutty, Email: RKrishnankutty@hamad.qa.
Allan Relecom, Email: ARelecom@hamad.qa.
Shahab Uddin, Email: SKhan34@hamad.qa.
Said Dermime, Email: SDermime@hamad.qa.
References
- 1.Vergati M, Intrivici C, Huen NY, Schlom J, Tsang KY. Strategies for cancer vaccine development. J Biomed Biotechnol. 2010 doi: 10.1155/2010/596432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ilyas S, Yang JC. Landscape of tumor antigens in T cell immunotherapy. J Immunol. 2015;195(11):5117–5122. doi: 10.4049/jimmunol.1501657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gjerstorff MF, Andersen MH, Ditzel HJ. Oncogenic cancer/testis antigens: prime candidates for immunotherapy. Oncotarget. 2015;6(18):15772–15787. doi: 10.18632/oncotarget.4694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Almeida LG, Sakabe NJ, deOliveira AR, Silva MC, Mundstein AS, Cohen T, et al. CTdatabase: a knowledge-base of high-throughput and curated data on cancer-testis antigens. Nucleic Acids Res. 2009;37(Database issue):D816–D819. doi: 10.1093/nar/gkn673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gnjatic S, Nishikawa H, Jungbluth AA, Gure AO, Ritter G, Jager E, et al. NY-ESO-1: review of an immunogenic tumor antigen. Adv Cancer Res. 2006;95:1–30. doi: 10.1016/S0065-230X(06)95001-5. [DOI] [PubMed] [Google Scholar]
- 6.U.S National Library of Medicine, ClinicalTrials.gov. https://clinicaltrials.gov/.
- 7.Chen YT, Scanlan MJ, Sahin U, Tureci O, Gure AO, Tsang S, et al. A testicular antigen aberrantly expressed in human cancers detected by autologous antibody screening. Proc Natl Acad Sci USA. 1997;94(5):1914–1918. doi: 10.1073/pnas.94.5.1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jager E, Chen YT, Drijfhout JW, Karbach J, Ringhoffer M, Jager D, et al. Simultaneous humoral and cellular immune response against cancer-testis antigen NY-ESO-1: definition of human histocompatibility leukocyte antigen (HLA)-A2-binding peptide epitopes. J Exp Med. 1998;187(2):265–270. doi: 10.1084/jem.187.2.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen Q, Jackson H, Parente P, Luke T, Rizkalla M, Tai TY, et al. Immunodominant CD4 + responses identified in a patient vaccinated with full-length NY-ESO-1 formulated with ISCOMATRIX adjuvant. Proc Natl Acad Sci USA. 2004;101(25):9363–9368. doi: 10.1073/pnas.0403271101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gjerstorff MF, Kock K, Nielsen O, Ditzel HJ. MAGE-A1, GAGE and NY-ESO-1 cancer/testis antigen expression during human gonadal development. Hum Reprod. 2007;22(4):953–960. doi: 10.1093/humrep/del494. [DOI] [PubMed] [Google Scholar]
- 11.Cartron PF, Blanquart C, Hervouet E, Gregoire M, Vallette FM. HDAC1-mSin3a-NCOR1, Dnmt3b-HDAC1-Egr1 and Dnmt1-PCNA-UHRF1-G9a regulate the NY-ESO1 gene expression. Mol Oncol. 2013;7(3):452–463. doi: 10.1016/j.molonc.2012.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barrow C, Browning J, MacGregor D, Davis ID, Sturrock S, Jungbluth AA, et al. Tumor antigen expression in melanoma varies according to antigen and stage. Clin Cancer Res. 2006;12(3 Pt 1):764–771. doi: 10.1158/1078-0432.CCR-05-1544. [DOI] [PubMed] [Google Scholar]
- 13.Nicholaou T, Ebert L, Davis ID, Robson N, Klein O, Maraskovsky E, et al. Directions in the immune targeting of cancer: lessons learned from the cancer-testis Ag NY-ESO-1. Immunol Cell Biol. 2006;84(3):303–317. doi: 10.1111/j.1440-1711.2006.01446.x. [DOI] [PubMed] [Google Scholar]
- 14.Esfandiary A, Ghafouri-Fard S. New York esophageal squamous cell carcinoma-1 and cancer immunotherapy. Immunotherapy. 2015;7(4):411–439. doi: 10.2217/imt.15.3. [DOI] [PubMed] [Google Scholar]
- 15.Sugita Y, Wada H, Fujita S, Nakata T, Sato S, Noguchi Y, et al. NY-ESO-1 expression and immunogenicity in malignant and benign breast tumors. Cancer Res. 2004;64(6):2199–2204. doi: 10.1158/0008-5472.CAN-03-3070. [DOI] [PubMed] [Google Scholar]
- 16.Peng JR, Chen HS, Mou DC, Cao J, Cong X, Qin LL, et al. Expression of cancer/testis (CT) antigens in Chinese hepatocellular carcinoma and its correlation with clinical parameters. Cancer Lett. 2005;219(2):223–232. doi: 10.1016/j.canlet.2004.07.028. [DOI] [PubMed] [Google Scholar]
- 17.Velazquez EF, Jungbluth AA, Yancovitz M, Gnjatic S, Adams S, O’Neill D, et al. Expression of the cancer/testis antigen NY-ESO-1 in primary and metastatic malignant melanoma (MM)–correlation with prognostic factors. Cancer Immun. 2007;7:11. [PMC free article] [PubMed] [Google Scholar]
- 18.Chen YT, Ross DS, Chiu R, Zhou XK, Chen YY, Lee P, et al. Multiple cancer/testis antigens are preferentially expressed in hormone-receptor negative and high-grade breast cancers. PLoS ONE. 2011;6(3):e17876. doi: 10.1371/journal.pone.0017876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baia GS, Caballero OL, Ho JS, Zhao Q, Cohen T, Binder ZA, et al. NY-ESO-1 expression in meningioma suggests a rationale for new immunotherapeutic approaches. Cancer Immunol Res. 2013;1(5):296–302. doi: 10.1158/2326-6066.CIR-13-0029. [DOI] [PubMed] [Google Scholar]
- 20.Balafoutas D, zur Hausen A, Mayer S, Hirschfeld M, Jaeger M, Denschlag D, et al. Cancer testis antigens and NY-BR-1 expression in primary breast cancer: prognostic and therapeutic implications. BMC Cancer. 2013;13:271. doi: 10.1186/1471-2407-13-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aung PP, Liu YC, Ballester LY, Robbins PF, Rosenberg SA, Lee CC. Expression of New York esophageal squamous cell carcinoma-1 in primary and metastatic melanoma. Hum Pathol. 2014;45(2):259–267. doi: 10.1016/j.humpath.2013.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klein O, Davis ID, McArthur GA, Chen L, Haydon A, Parente P, et al. Low-dose cyclophosphamide enhances antigen-specific CD4(+) T cell responses to NY-ESO-1/ISCOMATRIX vaccine in patients with advanced melanoma. Cancer Immunol Immunother. 2015;64(4):507–518. doi: 10.1007/s00262-015-1656-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klar AS, Gopinadh J, Kleber S, Wadle A, Renner C. Treatment with 5-Aza-2′-Deoxycytidine Induces Expression of NY-ESO-1 and Facilitates Cytotoxic T Lymphocyte-Mediated Tumor Cell Killing. PLoS ONE. 2015;10(10):e0139221. doi: 10.1371/journal.pone.0139221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gibbs P, Hutchins AM, Dorian KT, Vaughan HA, Davis ID, Silvapulle M, et al. MAGE-12 and MAGE-6 are frequently expressed in malignant melanoma. Melanoma Res. 2000;10(3):259–264. doi: 10.1097/00008390-200010030-00008. [DOI] [PubMed] [Google Scholar]
- 25.Kubuschok B, Xie X, Jesnowski R, Preuss KD, Romeike BF, Neumann F, et al. Expression of cancer testis antigens in pancreatic carcinoma cell lines, pancreatic adenocarcinoma and chronic pancreatitis. Int J Cancer. 2004;109(4):568–575. doi: 10.1002/ijc.20006. [DOI] [PubMed] [Google Scholar]
- 26.Hudolin T, Kastelan Z, Ilic I, Levarda-Hudolin K, Basic-Jukic N, Rieken M, et al. Immunohistochemical analysis of the expression of MAGE-A and NY-ESO-1 cancer/testis antigens in diffuse large B-cell testicular lymphoma. J Transl Med. 2013;11:123. doi: 10.1186/1479-5876-11-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hayes SJ, Hng KN, Clark P, Thistlethwaite F, Hawkins RE, Ang Y. Immunohistochemical assessment of NY-ESO-1 expression in esophageal adenocarcinoma resection specimens. World J Gastroenterol. 2014;20(14):4011–4016. doi: 10.3748/wjg.v20.i14.4011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Laban S, Atanackovic D, Luetkens T, Knecht R, Busch CJ, Freytag M, et al. Simultaneous cytoplasmic and nuclear protein expression of melanoma antigen-A family and NY-ESO-1 cancer-testis antigens represents an independent marker for poor survival in head and neck cancer. Int J Cancer. 2014;135(5):1142–1152. doi: 10.1002/ijc.28752. [DOI] [PubMed] [Google Scholar]
- 29.Goydos JS, Patel M, Shih W. NY-ESO-1 and CTp11 expression may correlate with stage of progression in melanoma. J Surg Res. 2001;98(2):76–80. doi: 10.1006/jsre.2001.6148. [DOI] [PubMed] [Google Scholar]
- 30.Jungbluth AA, Antonescu CR, Busam KJ, Iversen K, Kolb D, Coplan K, et al. Monophasic and biphasic synovial sarcomas abundantly express cancer/testis antigen NY-ESO-1 but not MAGE-A1 or CT7. Int J Cancer. 2001;94(2):252–256. doi: 10.1002/ijc.1451. [DOI] [PubMed] [Google Scholar]
- 31.Jungbluth AA, Chen YT, Stockert E, Busam KJ, Kolb D, Iversen K, et al. Immunohistochemical analysis of NY-ESO-1 antigen expression in normal and malignant human tissues. Int J Cancer. 2001;92(6):856–860. doi: 10.1002/ijc.1282. [DOI] [PubMed] [Google Scholar]
- 32.Sharma P, Gnjatic S, Jungbluth AA, Williamson B, Herr H, Stockert E, et al. Frequency of NY-ESO-1 and LAGE-1 expression in bladder cancer and evidence of a new NY-ESO-1 T-cell epitope in a patient with bladder cancer. Cancer Immun. 2003;3:19. doi: 10.1186/2051-1426-3-S2-O19. [DOI] [PubMed] [Google Scholar]
- 33.Maio M, Coral S, Sigalotti L, Elisei R, Romei C, Rossi G, et al. Analysis of cancer/testis antigens in sporadic medullary thyroid carcinoma: expression and humoral response to NY-ESO-1. J Clin Endocrinol Metab. 2003;88(2):748–754. doi: 10.1210/jc.2002-020830. [DOI] [PubMed] [Google Scholar]
- 34.Scanlan MJ, Altorki NK, Gure AO, Williamson B, Jungbluth A, Chen YT, et al. Expression of cancer-testis antigens in lung cancer: definition of bromodomain testis-specific gene (BRDT) as a new CT gene, CT9. Cancer Lett. 2000;150(2):155–164. doi: 10.1016/S0304-3835(99)00385-7. [DOI] [PubMed] [Google Scholar]
- 35.Kurashige T, Noguchi Y, Saika T, Ono T, Nagata Y, Jungbluth A, et al. Ny-ESO-1 expression and immunogenicity associated with transitional cell carcinoma: correlation with tumor grade. Cancer Res. 2001;61(12):4671–4674. [PubMed] [Google Scholar]
- 36.Scanlan MJ, Gout I, Gordon CM, Williamson B, Stockert E, Gure AO, et al. Humoral immunity to human breast cancer: antigen definition and quantitative analysis of mRNA expression. Cancer Immun. 2001;1:4. [PubMed] [Google Scholar]
- 37.Oshima Y, Shimada H, Yajima S, Nanami T, Matsushita K, Nomura F, et al. NY-ESO-1 autoantibody as a tumor-specific biomarker for esophageal cancer: screening in 1969 patients with various cancers. J Gastroenterol. 2016;51(1):30–34. doi: 10.1007/s00535-015-1078-8. [DOI] [PubMed] [Google Scholar]
- 38.Jager E, Stockert E, Zidianakis Z, Chen YT, Karbach J, Jager D, et al. Humoral immune responses of cancer patients against “Cancer-Testis” antigen NY-ESO-1: correlation with clinical events. Int J Cancer. 1999;84(5):506–510. doi: 10.1002/(SICI)1097-0215(19991022)84:5<506::AID-IJC10>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 39.Fujiwara S, Wada H, Kawada J, Kawabata R, Takahashi T, Fujita J, et al. NY-ESO-1 antibody as a novel tumour marker of gastric cancer. Br J Cancer. 2013;108(5):1119–1125. doi: 10.1038/bjc.2013.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Long YY, Wang Y, Huang QR, Zheng GS, Jiao SC. Measurement of serum antibodies against NY-ESO-1 by ELISA: a guide for the treatment of specific immunotherapy for patients with advanced colorectal cancer. Exp Ther Med. 2014;8(4):1279–1284. doi: 10.3892/etm.2014.1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Szender JB, Papanicolau-Sengos A, Eng KH, Miliotto AJ, Lugade AA, Gnjatic S, et al. NY-ESO-1 expression predicts an aggressive phenotype of ovarian cancer. Gynecol Oncol. 2017;145(3):420–425. doi: 10.1016/j.ygyno.2017.03.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fossa A, Berner A, Fossa SD, Hernes E, Gaudernack G, Smeland EB. NY-ESO-1 protein expression and humoral immune responses in prostate cancer. Prostate. 2004;59(4):440–447. doi: 10.1002/pros.20025. [DOI] [PubMed] [Google Scholar]
- 43.Nakamura S, Nouso K, Noguchi Y, Higashi T, Ono T, Jungbluth A, et al. Expression and immunogenicity of NY-ESO-1 in hepatocellular carcinoma. J Gastroenterol Hepatol. 2006;21(8):1281–1285. doi: 10.1111/j.1440-1746.2006.04271.x. [DOI] [PubMed] [Google Scholar]
- 44.Luetkens T, Kobold S, Cao Y, Ristic M, Schilling G, Tams S, et al. Functional autoantibodies against SSX-2 and NY-ESO-1 in multiple myeloma patients after allogeneic stem cell transplantation. Cancer Immunol Immunother. 2014;63(11):1151–1162. doi: 10.1007/s00262-014-1588-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lai JP, Robbins PF, Raffeld M, Aung PP, Tsokos M, Rosenberg SA, et al. NY-ESO-1 expression in synovial sarcoma and other mesenchymal tumors: significance for NY-ESO-1-based targeted therapy and differential diagnosis. Mod Pathol. 2012;25(6):854–858. doi: 10.1038/modpathol.2012.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hemminger JA, Ewart Toland A, Scharschmidt TJ, Mayerson JL, Kraybill WG, Guttridge DC, et al. The cancer-testis antigen NY-ESO-1 is highly expressed in myxoid and round cell subset of liposarcomas. Mod Pathol. 2013;26(2):282–288. doi: 10.1038/modpathol.2012.133. [DOI] [PubMed] [Google Scholar]
- 47.Hemminger JA, Iwenofu OH. NY-ESO-1 is a sensitive and specific immunohistochemical marker for myxoid and round cell liposarcomas among related mesenchymal myxoid neoplasms. Mod Pathol. 2013;26(9):1204–1210. doi: 10.1038/modpathol.2013.65. [DOI] [PubMed] [Google Scholar]
- 48.Pollack SM, Jungbluth AA, Hoch BL, Farrar EA, Bleakley M, Schneider DJ, et al. NY-ESO-1 is a ubiquitous immunotherapeutic target antigen for patients with myxoid/round cell liposarcoma. Cancer. 2012;118(18):4564–4570. doi: 10.1002/cncr.27446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Baumgaertner P, Costa Nunes C, Cachot A, Maby-El Hajjami H, Cagnon L, Braun M, et al. Vaccination of stage III/IV melanoma patients with long NY-ESO-1 peptide and CpG-B elicits robust CD8+ and CD4+ T-cell responses with multiple specificities including a novel DR7-restricted epitope. Oncoimmunology. 2016;5(10):e1216290. doi: 10.1080/2162402X.2016.1216290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Singh N, Kulikovskaya I, Barrett DM, Binder-Scholl G, Jakobsen B, Martinez D, et al. T cells targeting NY-ESO-1 demonstrate efficacy against disseminated neuroblastoma. Oncoimmunology. 2016;5(1):e1040216. doi: 10.1080/2162402X.2015.1040216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jager E, Gnjatic S, Nagata Y, Stockert E, Jager D, Karbach J, et al. Induction of primary NY-ESO-1 immunity: CD8+ T lymphocyte and antibody responses in peptide-vaccinated patients with NY-ESO-1 + cancers. Proc Natl Acad Sci USA. 2000;97(22):12198–12203. doi: 10.1073/pnas.220413497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jager E, Jager D, Karbach J, Chen YT, Ritter G, Nagata Y, et al. Identification of NY-ESO-1 epitopes presented by human histocompatibility antigen (HLA)-DRB4*0101-0103 and recognized by CD4(+) T lymphocytes of patients with NY-ESO-1-expressing melanoma. J Exp Med. 2000;191(4):625–630. doi: 10.1084/jem.191.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Komatsu N, Jackson HM, Chan KF, Oveissi S, Cebon J, Itoh K, et al. Fine-mapping naturally occurring NY-ESO-1 antibody epitopes in melanoma patients’ sera using short overlapping peptides and full-length recombinant protein. Mol Immunol. 2013;54(3–4):465–471. doi: 10.1016/j.molimm.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 54.Odunsi K, Jungbluth AA, Stockert E, Qian F, Gnjatic S, Tammela J, et al. NY-ESO-1 and LAGE-1 cancer-testis antigens are potential targets for immunotherapy in epithelial ovarian cancer. Cancer Res. 2003;63(18):6076–6083. [PubMed] [Google Scholar]
- 55.Davis ID, Chen W, Jackson H, Parente P, Shackleton M, Hopkins W, et al. Recombinant NY-ESO-1 protein with ISCOMATRIX adjuvant induces broad integrated antibody and CD4(+) and CD8(+) T cell responses in humans. Proc Natl Acad Sci USA. 2004;101(29):10697–10702. doi: 10.1073/pnas.0403572101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shackleton M, Davis ID, Hopkins W, Jackson H, Dimopoulos N, Tai T, et al. The impact of imiquimod, a Toll-like receptor-7 ligand (TLR7L), on the immunogenicity of melanoma peptide vaccination with adjuvant Flt3 ligand. Cancer Immun. 2004;4:9. [PubMed] [Google Scholar]
- 57.Chen Q, Jackson H, Shackleton M, Parente P, Hopkins W, Sturrock S, et al. Characterization of antigen-specific CD8+ T lymphocyte responses in skin and peripheral blood following intradermal peptide vaccination. Cancer Immun. 2005;5:5. [PubMed] [Google Scholar]
- 58.Nirschl CJ, Anandasabapathy N. Duality at the gate: skin dendritic cells as mediators of vaccine immunity and tolerance. Hum Vaccin Immunother. 2016;12(1):104–116. doi: 10.1080/21645515.2015.1066050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nicholaou T, Chen W, Davis ID, Jackson HM, Dimopoulos N, Barrow C, et al. Immunoediting and persistence of antigen-specific immunity in patients who have previously been vaccinated with NY-ESO-1 protein formulated in ISCOMATRIX. Cancer Immunol Immunother. 2011;60(11):1625–1637. doi: 10.1007/s00262-011-1041-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.von Boehmer L, Mattle M, Bode P, Landshammer A, Schafer C, Nuber N, et al. NY-ESO-1-specific immunological pressure and escape in a patient with metastatic melanoma. Cancer Immun. 2013;13:12. [PMC free article] [PubMed] [Google Scholar]
- 61.Gordeeva O. Cancer-testis antigens: unique cancer stem cell biomarkers and targets for cancer therapy. Semin Cancer Biol. 2018;53:75–89. doi: 10.1016/j.semcancer.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 62.van der Burg SH, Arens R, Ossendorp F, van Hall T, Melief CJ. Vaccines for established cancer: overcoming the challenges posed by immune evasion. Nat Rev Cancer. 2016;16(4):219–233. doi: 10.1038/nrc.2016.16. [DOI] [PubMed] [Google Scholar]
- 63.Buonaguro L, Petrizzo A, Tornesello ML, Buonaguro FM. Translating tumor antigens into cancer vaccines. Clin Vaccine Immunol. 2011;18(1):23–34. doi: 10.1128/CVI.00286-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21(2):137–148. doi: 10.1016/j.immuni.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 65.Klippel ZK, Chou J, Towlerton AM, Voong LN, Robbins P, Bensinger WI, et al. Immune escape from NY-ESO-1-specific T-cell therapy via loss of heterozygosity in the MHC. Gene Ther. 2014;21(3):337–342. doi: 10.1038/gt.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9(3):162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yuan J, Adamow M, Ginsberg BA, Rasalan TS, Ritter E, Gallardo HF, et al. Integrated NY-ESO-1 antibody and CD8 + T-cell responses correlate with clinical benefit in advanced melanoma patients treated with ipilimumab. Proc Natl Acad Sci USA. 2011;108(40):16723–16728. doi: 10.1073/pnas.1110814108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Matsuzaki J, Gnjatic S, Mhawech-Fauceglia P, Beck A, Miller A, Tsuji T, et al. Tumor-infiltrating NY-ESO-1-specific CD8+ T cells are negatively regulated by LAG-3 and PD-1 in human ovarian cancer. Proc Natl Acad Sci U S A. 2010;107(17):7875–7880. doi: 10.1073/pnas.1003345107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Curiel TJ, Coukos G, Zou L, Alvarez X, Cheng P, Mottram P, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med. 2004;10(9):942–949. doi: 10.1038/nm1093. [DOI] [PubMed] [Google Scholar]
- 70.Griffiths RW, Elkord E, Gilham DE, Ramani V, Clarke N, Stern PL, et al. Frequency of regulatory T cells in renal cell carcinoma patients and investigation of correlation with survival. Cancer Immunol Immunother. 2007;56(11):1743–1753. doi: 10.1007/s00262-007-0318-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Weide B, Martens A, Zelba H, Stutz C, Derhovanessian E, Di Giacomo AM, et al. Myeloid-derived suppressor cells predict survival of patients with advanced melanoma: comparison with regulatory T cells and NY-ESO-1- or melan-A-specific T cells. Clin Cancer Res. 2014;20(6):1601–1609. doi: 10.1158/1078-0432.CCR-13-2508. [DOI] [PubMed] [Google Scholar]
- 72.Talmadge JE. Immune cell infiltration of primary and metastatic lesions: mechanisms and clinical impact. Semin Cancer Biol. 2011;21(2):131–138. doi: 10.1016/j.semcancer.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 73.Gooden MJ, de Bock GH, Leffers N, Daemen T, Nijman HW. The prognostic influence of tumour-infiltrating lymphocytes in cancer: a systematic review with meta-analysis. Br J Cancer. 2011;105(1):93–103. doi: 10.1038/bjc.2011.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Thomas NE, Busam KJ, From L, Kricker A, Armstrong BK, Anton-Culver H, et al. Tumor-infiltrating lymphocyte grade in primary melanomas is independently associated with melanoma-specific survival in the population-based genes, environment and melanoma study. J Clin Oncol. 2013;31(33):4252–4259. doi: 10.1200/JCO.2013.51.3002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Onizuka S, Tawara I, Shimizu J, Sakaguchi S, Fujita T, Nakayama E. Tumor rejection by in vivo administration of anti-CD25 (interleukin-2 receptor alpha) monoclonal antibody. Cancer Res. 1999;59(13):3128–3133. [PubMed] [Google Scholar]
- 76.Sutmuller RP, van Duivenvoorde LM, van Elsas A, Schumacher TN, Wildenberg ME, Allison JP, et al. Synergism of cytotoxic T lymphocyte-associated antigen 4 blockade and depletion of CD25(+) regulatory T cells in antitumor therapy reveals alternative pathways for suppression of autoreactive cytotoxic T lymphocyte responses. J Exp Med. 2001;194(6):823–832. doi: 10.1084/jem.194.6.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Moon EK, Ranganathan R, Eruslanov E, Kim S, Newick K, O’Brien S, et al. Blockade of programmed death 1 augments the ability of human T cells engineered to target NY-ESO-1 to control tumor growth after adoptive transfer. Clin Cancer Res. 2016;22(2):436–447. doi: 10.1158/1078-0432.CCR-15-1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fourcade J, Kudela P, Sun Z, Shen H, Land SR, Lenzner D, et al. PD-1 is a regulator of NY-ESO-1-specific CD8 + T cell expansion in melanoma patients. J Immunol. 2009;182(9):5240–5249. doi: 10.4049/jimmunol.0803245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang W, Lau R, Yu D, Zhu W, Korman A, Weber J. PD1 blockade reverses the suppression of melanoma antigen-specific CTL by CD4 + CD25(Hi) regulatory T cells. Int Immunol. 2009;21(9):1065–1077. doi: 10.1093/intimm/dxp072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Curran MA, Montalvo W, Yagita H, Allison JP. PD-1 and CTLA-4 combination blockade expands infiltrating T cells and reduces regulatory T and myeloid cells within B16 melanoma tumors. Proc Natl Acad Sci USA. 2010;107(9):4275–4280. doi: 10.1073/pnas.0915174107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Simpson TR, Li F, Montalvo-Ortiz W, Sepulveda MA, Bergerhoff K, Arce F, et al. Fc-dependent depletion of tumor-infiltrating regulatory T cells co-defines the efficacy of anti-CTLA-4 therapy against melanoma. J Exp Med. 2013;210(9):1695–1710. doi: 10.1084/jem.20130579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cone RE, Li X, Sharafieh R, O’Rourke J, Vella AT. The suppression of delayed-type hypersensitivity by CD8+ regulatory T cells requires interferon-gamma. Immunology. 2007;120(1):112–119. doi: 10.1111/j.1365-2567.2006.02486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Parvanova I, Rettig L, Knuth A, Pascolo S. The form of NY-ESO-1 antigen has an impact on the clinical efficacy of anti-tumor vaccination. Vaccine. 2011;29(22):3832–3836. doi: 10.1016/j.vaccine.2011.03.073. [DOI] [PubMed] [Google Scholar]
- 84.Xue W, Metheringham RL, Brentville VA, Gunn B, Symonds P, Yagita H, et al. SCIB2, an antibody DNA vaccine encoding NY-ESO-1 epitopes, induces potent antitumor immunity which is further enhanced by checkpoint blockade. Oncoimmunology. 2016;5(6):e1169353. doi: 10.1080/2162402X.2016.1169353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Albershardt TC, Campbell DJ, Parsons AJ, Slough MM, Ter Meulen J, Berglund P. LV305, a dendritic cell-targeting integration-deficient ZVex(TM)-based lentiviral vector encoding NY-ESO-1, induces potent anti-tumor immune response. Mol Ther Oncolytics. 2016;3:16010. doi: 10.1038/mto.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tareen SU, Kelley-Clarke B, Nicolai CJ, Cassiano LA, Nelson LT, Slough MM, et al. Design of a novel integration-deficient lentivector technology that incorporates genetic and posttranslational elements to target human dendritic cells. Mol Ther. 2014;22(3):575–587. doi: 10.1038/mt.2013.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Somaiah N, Block MS, Kim JW, Shapiro GI, Do KT, Hwu P, et al. First-in-class, first-in-human study evaluating LV305, a dendritic-cell tropic lentiviral vector, in sarcoma and other solid tumors expressing NY-ESO-1. Clin Cancer Res. 2019;25(19):5808–5817. doi: 10.1158/1078-0432.CCR-19-1025. [DOI] [PubMed] [Google Scholar]
- 88.Pollack SM. The potential of the CMB305 vaccine regimen to target NY-ESO-1 and improve outcomes for synovial sarcoma and myxoid/round cell liposarcoma patients. Expert Rev Vaccines. 2018;17(2):107–114. doi: 10.1080/14760584.2018.1419068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gupta A, Nuber N, Esslinger C, Wittenbrink M, Treder M, Landshammer A, et al. A novel human-derived antibody against NY-ESO-1 improves the efficacy of chemotherapy. Cancer Immun. 2013;13:3. [PMC free article] [PubMed] [Google Scholar]
- 90.Delaunay T, Violland M, Boisgerault N, Dutoit S, Vignard V, Munz C, et al. Oncolytic viruses sensitize human tumor cells for NY-ESO-1 tumor antigen recognition by CD4+ effector T cells. Oncoimmunology. 2018;7(3):e1407897. doi: 10.1080/2162402X.2017.1407897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.He Q, Liu Z, Liu Z, Lai Y, Zhou X, Weng J. TCR-like antibodies in cancer immunotherapy. J Hematol Oncol. 2019;12(1):99. doi: 10.1186/s13045-019-0788-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Held G, Matsuo M, Epel M, Gnjatic S, Ritter G, Lee SY, et al. Dissecting cytotoxic T cell responses towards the NY-ESO-1 protein by peptide/MHC-specific antibody fragments. Eur J Immunol. 2004;34(10):2919–2929. doi: 10.1002/eji.200425297. [DOI] [PubMed] [Google Scholar]
- 93.Rosenberg SA, Restifo NP. Adoptive cell transfer as personalized immunotherapy for human cancer. Science. 2015;348(6230):62–68. doi: 10.1126/science.aaa4967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Robbins PF, Morgan RA, Feldman SA, Yang JC, Sherry RM, Dudley ME, et al. Tumor regression in patients with metastatic synovial cell sarcoma and melanoma using genetically engineered lymphocytes reactive with NY-ESO-1. J Clin Oncol. 2011;29(7):917–924. doi: 10.1200/JCO.2010.32.2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rapoport AP, Stadtmauer EA, Binder-Scholl GK, Goloubeva O, Vogl DT, Lacey SF, et al. NY-ESO-1-specific TCR-engineered T cells mediate sustained antigen-specific antitumor effects in myeloma. Nat Med. 2015;21(8):914–921. doi: 10.1038/nm.3910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Everson RG, Antonios JP, Lisiero DN, Soto H, Scharnweber R, Garrett MC, et al. Efficacy of systemic adoptive transfer immunotherapy targeting NY-ESO-1 for glioblastoma. Neuro Oncol. 2016;18(3):368–378. doi: 10.1093/neuonc/nov153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Krishnadas DK, Shusterman S, Bai F, Diller L, Sullivan JE, Cheerva AC, et al. A phase I trial combining decitabine/dendritic cell vaccine targeting MAGE-A1, MAGE-A3 and NY-ESO-1 for children with relapsed or therapy-refractory neuroblastoma and sarcoma. Cancer Immunol Immunother. 2015;64(10):1251–1260. doi: 10.1007/s00262-015-1731-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Schuberth PC, Jakka G, Jensen SM, Wadle A, Gautschi F, Haley D, et al. Effector memory and central memory NY-ESO-1-specific re-directed T cells for treatment of multiple myeloma. Gene Ther. 2013;20(4):386–395. doi: 10.1038/gt.2012.48. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.