Abstract
Background
Since the first case of a novel coronavirus (COVID-19) infection pneumonia was detected in Wuhan, China, a series of confirmed cases of the COVID-19 were found in Beijing. We analyzed the data of 262 confirmed cases to determine the clinical and epidemiological characteristics of COVID-19 in Beijing.
Methods
We collected patients who were transferred by Beijing Emergency Medical Service to the designated hospitals. The information on demographic, epidemiological, clinical, laboratory test for the COVID-19 virus, diagnostic classification, cluster case and outcome were obtained. Furthermore we compared the characteristics between severe and common confirmed cases which including mild cases, no-pneumonia cases and asymptomatic cases, and we also compared the features between COVID-19 and 2003 SARS.
Findings
By Feb 10, 2020, 262 patients were transferred from the hospitals across Beijing to the designated hospitals for special treatment of the COVID-19 infected by Beijing emergency medical service. Among of 262 patients, 46 (17.6%) were severe cases, 216 (82.4%) were common cases, which including 192 (73.3%) mild cases, 11(4.2%) non-pneumonia cases and 13 (5.0%) asymptomatic cases respectively. The median age of patients was 47.5 years old and 48.5% were male. 192 (73.3%) patients were residents of Beijing, 50 (26.0%) of which had been to Wuhan, 116 (60.4%) had close contact with confirmed cases, 21 (10.9%) had no contact history. The most common symptoms at the onset of illness were fever (82.1%), cough (45.8%), fatigue (26.3%), dyspnea (6.9%) and headache (6.5%). The median incubation period was 6.7 days, the interval time from between illness onset and seeing a doctor was 4.5 days. As of Feb 10, 17.2% patients have discharged and 81.7% patients remain in hospital in our study, the fatality of COVID-19 infection in Beijing was 0.9%.
Interpretation
On the basis of this study, we provided the ratio of the COVID-19 infection on the severe cases to the mild, asymptomatic and non-pneumonia cases in Beijing. Population was generally susceptible, and with a relatively low fatality rate. The measures to prevent transmission was very successful at early stage, the next steps on the COVID-19 infection should be focused on early isolation of patients and quarantine for close contacts in families and communities in Beijing.
Funding
Beijing Municipal Science and Technology Commission and Ministry of Science and Technology.
Keywords: COVID-19, 2019-nCoV, Characteristics, Beijing
Research in context.
Evidence before this study
We searched PubMed on Feb 10, 2020, using the terms “2019-nCoV” and “characteristics” for articles in English. We found six studies on the characteristics of patients infected with COVID-19. Huang C reported the features of 41 cases in Wuhan in the Lancet on Jan 24, 21,020. Li Q reported the dynamics of 425 cases in Wuhan in the New England Journal Medicine on Jan 29,2020. Chen N reported characteristics of 99 cases in Wuhan in the Lancet on Jan 30, 21,020.Wang D reported characteristics of 138 cases in Wuhan in the JAMA on Feb 7, 2020. Other two studies were case reports. Our search did not reveal any report on the characteristics of patients with COVID-19 infection in other imported city except Wuhan.
Added value of this study
We reported the characteristics of 262 cases infected with COVID-19 from 57 hospitals across Beijing and provided the proportion of the COVID-19 infection on the severe cases to mild, asymptomatic and non-pneumonia cases. We compared the epidemic features between COVID-19 and 2003 SARS for learn lessons and control the outbreak.
Implications of all the available evidence
The COVID-19 infection was generally susceptible, and with a relatively low fatality rate. The measures to prevent transmission was very successful at early stage, the next steps on the COVID-19 infection should be focused on early isolation of patients and quarantine for close contacts in families and communities in Beijing and China.
Alt-text: Unlabelled box
Introduction
As of February 10, 2020, a total of 40,554 cases with laboratory-confirmed COVID-19 infection have been detected in the world reported by the World Health Organization (WHO).1 There have been 42,638 accumulated confirmed cases of COVID-19 infections, of them 1016 patients has died, 3996 have been discharged and 88% remain in hospital in mainland of China,2 and 342 confirmed cases were found in Beijing.3 The infected cases were also reported in Thailand, Japan, South Korea, Singapore, Vietnam, the US, and other 24 countries around the world.4, 5 Given that the current COVID-19 outbreak is moving rapidly, the recently published literatures on the epidemic features of COVID-19 mainly focus on Wuhan, China,6, 7 but the information on the imported city or region is exceedingly rare.
In this study, we provide an analysis of data on the characteristics of patients with confirmed COVID-19 infection throughout Beijing as an imported metropolis, and unravel the proportion on the severe cases to the mild, asymptomatic and non-pneumonia cases. Additionally, Beijing experienced the outbreak of SARS in 2003. For learn lessons and control the outbreak, we compare the epidemic features between COVID-19 and 2003 SARS.
Methods
Study design
This was a retrospective study, we enrolled patients with COVID-19 infection who was transferred from the hospitals of Beijing to the designated hospitals for special treatment infectious diseases by Beijing Emergency Medical Service (EMS) from Jan 20 to Feb 10, 2020. We compared the characteristics between severe and common confirmed cases which including mild cases, no-pneumonia cases and asymptomatic cases. The features were compared between COVID-19 and 2003 SARS. The study was approved by Ethics Committee of Beijing Emergency Medical Center (No.2020-01) and the written informed consent was waived because of the retrospective nature of the study and belongs to emergency medical service.
Definitions
A confirmed case was defined as a suspected case with the laboratory test for the COVID-19 from the respiratory specimens show positive result by the real-time reverse-transcription-polymerase-chain-reaction (RT-PCR) assay, while a suspected case was defined as a case that fulfilled both the following criteria: have fever, radiographic evidence of pneumonia, low or normal white-cell count or low lymphocyte count in clinic; and have a travel to Wuhan or direct contact with patients from Wuhan who have fever or respiratory symptoms within 14 days before illness in the epidemic history according to the new coronavirus pneumonial prevention and control program, and the new coronavirus pneumonial diagnosis and treatment program which were published by the National Health Commission of China.8, 9, 10
A mild case was defined as a confirmed case with fever, respiratory symptoms and radiographic evidence of pneumonia, while a severe case was defined as a mild case with dyspnea or respiratory failure. A non-pneumonia case was defined as a confirmed case with fever and/or respiratory symptoms, but no radiographic evidence of pneumonia, while an asymptomatic case was defined as a confirmed case with normal body temperature or minor discomfort.
Data collection
We modified the medical record form for the COVID-19 infection, which including demographic, epidemiological, clinical, laboratory test for the COVID-19, diagnostic classification, cluster case and outcome etc. Laboratory confirmation of COVID-19 was detected in the first admission hospital and verified by the Beijing Center for Disease Control and Prevention (CDC). Clinical outcomes were followed up to February 10, 2020. If the data missing from the records was needed, we obtained data by direct communication with EMS providers. A double-extraction method in which two independent reviewers extract data and evaluate the eligibility of the original data was applied. All differences were resolved through discussion prior to the final analysis. All data were checked by another two researchers.
Data on the COVID-19 infection in China and Beijing obtained from National Health Commission of the People's Republic of China and Beijing Health Commission respectively between Jan 20 to Feb 10, 2020. The data of SARS in 2003 searched from the office of the Ministry of Health, which started on April 21, 2003, both including accumulative and daily new confirmed cases of the SARS outbreak in China.
Statical analysis
The continuous variables were expressed as mean±SD, and were compared with the Mann-Whitney U test. And the categorical variables were presented as percentage and analyzed by Wilcoxon test between severe and common cases. All statistical analysis were performed with SPSS software version 22.0, and P value less than 0.05 was considered statistically significant.
Results
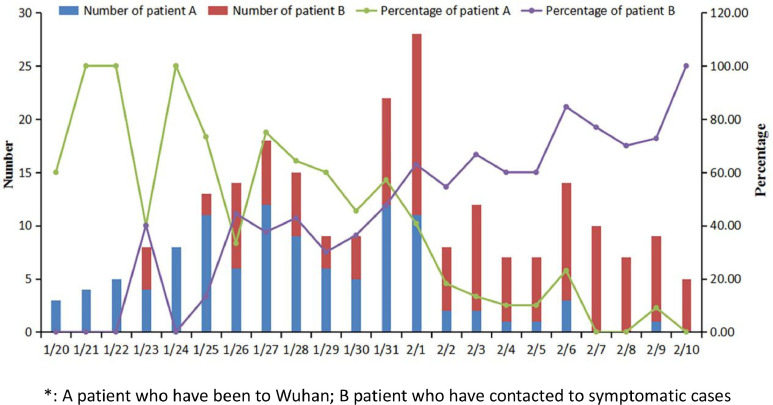
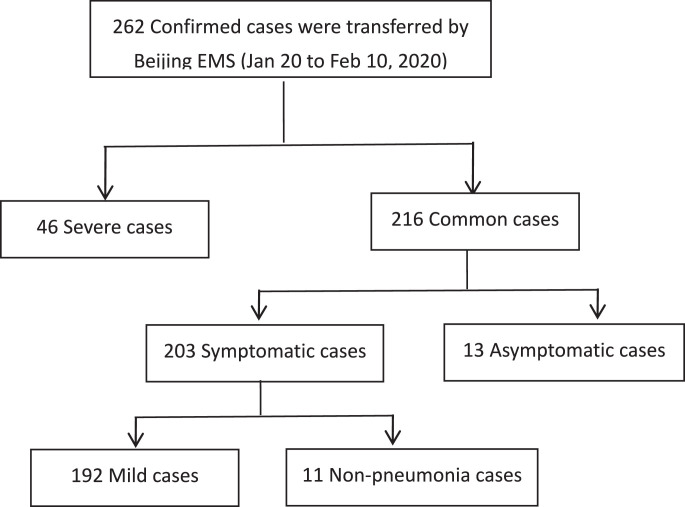
262 patients who were identified as a confirmed COVID-19 infection were included in this study, those patients were transferred from 57 hospitals across Beijing to the designated hospitals by Beijing EMS from January 20 to February 10, 2020. Of the 262 patients, 46 (17.6%) and 216 (82.4%) were categorized into severe and common group respectively. The severe patients required oxygen to support, the average oxygen saturation (SpO2) of the severe patients was 92.6% (68%−100%), the common group included 192 (73.3%) mild cases, 11 (4.2%) non-pneumonia cases and 13 (5.0%) asymptomatic cases. The median age of patients was 47.5 years (rang 6 months to 94 years;95% CI:45.1 to 49.9, Table 1 ); of them, 8 (3.1%) were children younger than 12 years old; 48 (18.3%) were 65 years age of older, 3 infants (two female, 6 months and 9 months respectively; a male 10 months) and a 25-year- old pregnant woman were infected, the gestational age was 33 weeks. 127 (48.5%) patients were males. 53 (20.2%) patients came from Wuhan, Hubei Province of China. 192 (73.3%) patients were residents of Beijing, 50 (26%) of which had been to Wuhan travel or residence, 116 (60.4%) contacted with confirmed cases, 21 (10.9%) had no obviously contact history (Fig. 1 ).
Table 1.
. Characteristics of COVID-19 infection in Beijing.
| Characteristics | All cases (N = 262) | Severe (N = 46) | Common (N = 216) | P value |
|---|---|---|---|---|
| Age, Median (range), years | 47.5(1–94) | 61.4(1–94) | 44.5(1–93) | <0.001 |
| Age groups, n(%) | <0.001 | |||
| <1 | 3(1.1) | 1(2.2) | 2(0.9) | |
| 1–12 | 8(3.1) | 0(0.0) | 8(3.7) | |
| 13–44 | 112(42.7) | 9(19.6) | 103(47.7) | |
| 45–64 | 91(34.7) | 16(34.8) | 75(34.7) | |
| ≥65 | 48(18.3) | 20(43.5) | 28(13.0) | |
| Male, n(%) | 127(48.5) | 26(56.5) | 101(46.8) | 0.230 |
| Resident address, n(%) | 0.239 | |||
| Beijing | 192(73.3) | 39(84.8) | 153(70.8) | |
| Wuhan | 53(20.2) | 5(10.9) | 48(22.2) | |
| Other | 17(6.5) | 2(4.3) | 15(6.9) | |
| Signs and symptoms, n(%) | ||||
| Fever | 215(82.1) | 37(80.4) | 178(82.4) | 0.752 |
| Highest temperature,℃ | 0.688 | |||
| <37.3 | 47(17.9) | 9(19.6) | 38(17.6) | |
| 37.3–38.0 | 110(42) | 16(34.8) | 94(43.5) | |
| 38.1–39.0 | 96(36.6) | 20(43.5) | 76(35.2) | |
| >39.0 | 9(3.4) | 1(2.2) | 8(3.7) | |
| Cough | 120(45.8) | 25(54.3) | 95(44.0) | 0.201 |
| Fatigue | 69(26.3) | 15(32.6) | 54(25.0) | 0.288 |
| Dyspnea | 18(6.9) | 15(32.6) | 3(1.4) | <0.001 |
| Headache | 17(6.5) | 3(6.5) | 14(6.5) | 0.992 |
| Respiratory rate | 124.5 ± 14.8 | 126.1 ± 16.4 | 123.7 ± 14.4 | 0.333 |
| History of contact, n(%) | 241(92.0) | 41(89.1) | 200(92.6) | 0.433 |
| Have been to Wuhan in 14 days | 106(40.5) | 13(28.3) | 93(43.1) | 0.064 |
| Contacted to symptomatic case in 14 days | 129(49.2) | 26(56.5) | 103(47.7) | 0.277 |
| Days from contact to illness onset | 6.7 ± 5.2 | 7.5 ± 7.2 | 6.5 ± 4.6 | 0.373 |
| Days from illness onset to visit hospital | 4.5 ± 3.7 | 5.2 ± 4.6 | 4.4 ± 3.5 | 0.293 |
| Days from visit hospital to defined | 2.1 ± 1.9 | 2.1 ± 1.6 | 2.1 ± 1.9 | 0.863 |
| Cluster case, n(%) | 176(67.2) | 32(69.6) | 144(66.7) | 0.704 |
| Family | 133(50.8) | 24(52.2) | 109(50.5) | 0.833 |
| Other | 43(16.4) | 8(17.4) | 35(16.2) | 0.844 |
| Outcome, n(%) | 0.001 | |||
| Discharge | 45(17.2) | 2(4.3) | 43(19.9) | |
| Hospitalization | 214(81.7) | 41(89.1) | 173(80.1) | |
| Death | 3(0.9*) | 3(6.5) | 0(0.0) | |
The ratio was 3 of 342 confirmed cases which was defined in Beijing by Feb 10, 2020.
Fig. 1.
Change of imported cases.
*A patient who have been to Wuhan; B patient who have contacted to symptomatic cases.
Fig. 2 .
Fig. 2.
. Patients flow and enrollment.
The most common symptoms of illness onset were fever (82.1%), cough (45.8%), and fatigue (26.3%), dyspnea (6.9%) and headache (6.5%), severe cases with dyspnea (32.6%, 15 of 46). The median time from contact symptomatic case to illness onset, which is called the incubation period, was 6.7 days, from illness onset to visit hospital was 4.5 days, from visit hospital to defined confirmed case was 2.1 days. Of the 262 patients, 176 (67.2%) were cluster cases, 133 (50.8%) were family cluster cases, 43 (16.4%) were other cluster cases. The median number of cluster infection was 3 cases, at least 2 cases, at most 5 cases.
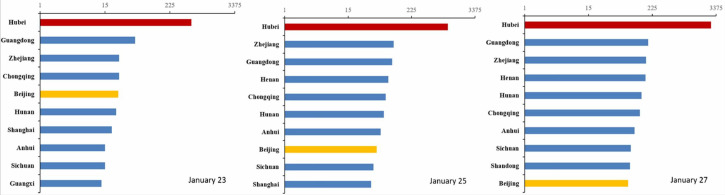
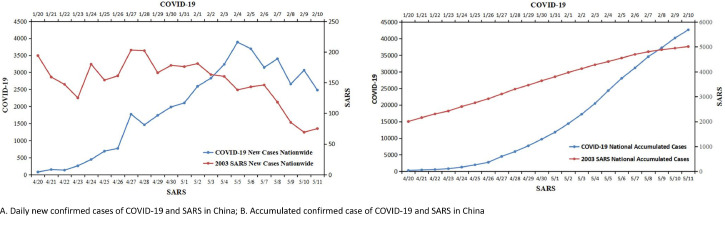
By the end of Feb 10, 2020, 45 (17.2%) of 262 patients were discharged and 214 (81.7%) remained in hospital. Of them, 3 patients died, the first death was a 50-year-old man who had no previous chronic underlying disease, he had been to Wuhan in Jan 8, 2020, came back Beijing in Jan 15, had fever and fatigue in Jan 13, visited hospital in Jan 21, was defined as a confirmed case and transferred to the designated hospital in Jan 22, died in Jan 27, 2020. The second death was a 94-year-old female who was a Beijing resident with pulmonary infection, chronic cardiovascular disease and heart failure, was defined as a confirmed case and transferred to the designated hospital in Feb 6, died in Feb 7, 2020. The third death was a 82-year-old male who was a Beijing resident with pulmonary infection and multiple chronic diseases, was defined as a confirmed case in Feb 2, transferred to the designated hospital in Feb 3, died in Feb 10, 2020. The fatality of COVID-19 infection was significantly lower in Beijing compared with the whole national (0.9% vs 2.4%, P < 0.001), while the rate of discharged in Beijing was significantly higher than the whole national (14% vs 9.4%, P < 0.001). Beijing was the fourth most affected city or province in China for accumulative confirmed cases of the COVID-19 infection at the end of Jan 23, reduced to the 8th in Jan 25, to the 10th in Jan 27, and out of the top ten later.(Fig. 3 ) By contrast, in May 4, 2003, 4280 confirmed SARS cases had been reported, 206 of whom died (4.8%) distributing in 24 provinces in Chinese mainland. The fatality of the COVID-19 infection has no significant with SARS by the same period . From May 1st, the new confirmed case of SARS started to decline, but the COVID-19 confirmed cases was still moving in the mainland of China until Feb 10, 2020. (Fig. 4 )
Fig. 3.
Top 10 provinces in China for accumulative COVID-19 cases. A. Daily new confirmed cases of COVID-19 and SARS in China; B. Accumulated confirmed case of COVID-19 and SARS in China.
Fig. 4.
Comparison of COVID-19 and 2003 SARS in China.
Discussion
China has experienced SARS in 2003 and MERS in 2012 of the coronavirus outbreak.11 As prof. Drazen said, the SARS shows that when confronted by a common enemy, we can forget our differences and work together fruitfully. This was the most important lesson from SARS, let us hope that we can all benefit from it.12 Recently, the COVID-19 infection occurred and spread in the mainland of China, but the proportion of mild and asymptomatic cases versus severe and fatal cases for COVID-19 infection is currently still unknown that hampers realistic assessment of the virus's epidemic potential and complicates the outbreak response,5 furthermore, the recent publications on the epidemiological and clinical characteristics mainly came from Wuhan,6 , 7 , 13 the information about the imported city is exceedingly rare. On the basis of this study, firstly we provided the proportion of severe versus common cases of the COVID-19 infection, which was approximately 1:4, the ratio of severe to mild, non-pneumonia and asymptomatic cases were 18%, 73%, 4% and 5% respectively, the changes and prognosis of those four categories should be future observed in hospitals. 13 asymptomatic cases were the close contacts who were found by medical observation in this study. If not insulated for medical observation, they would not seek health care or visit hospital and cannot be found in the special period, and will spread to the other close contacts.15, 16 Therefore, to identify and control the non-pneumonia and asymptomatic cases are the important measures to prevent transmission on the COVID-19.
The age of patients was from 6 months to 94-year-old, the majority of patients were young adults (77.4%), there was no significant difference between male and female in our study, population was generally susceptible. The patients were mainly residents of Beijing (73.3%), while the other patients mostly came from Wuhan(20.2%). But 89.1% of the residents of Beijing had been travel to Wuhan or contacted with the confirmed case in 14 days especially in the early stage of COVID-19 infection, after Feb. 1, the number of local confirmed cases began to exceed imported cases. In this study, 133 patients from more than 20 families were infected, same as Wuhan, the infection of COVID-19 in Beijing was of clustering onset too.13, 14 Therefore, person-to-person transmission is the main route of transmission.
The most common symptoms of illness onset were fever, cough, fatigue, and headache, severe cases with dyspnea, the results were consistent with the new coronavirus pneumonial diagnosis and treatment program (3rd, in Chinese) published by the National Health Commission of China.9 The median time of incubation period was 6.7 days. The median time from illness onset to visit hospital and from visit hospital to defined confirmed case were 4.5 and 2.1 days respectively. The fatality of patients infected by COVID-19 in Beijing was 0.9%, significantly lower than the whole national average level, and not resembling that in previous studies.6 , 13 The rate of discharged of Beijing was significantly higher than the whole national average level. Among the top 10 provinces and cities with accumulative confirmed cases of COVID-19 cases, the ranking of Beijing has fallen faster than other provinces. Therefore, Beijing was successful in preventing and controlling on the COVID-19 infection, it benefits from the correct leadership and experience of SARS in 2003. From the perspective of death of SARS, as of May 11, 2003, the fatality of the SARS was 5.0%, while the COVID-19 was 2.4% in the whole national, there was no significant with the fatality between SARS and the COVID-19 infection in the early stage, but different in the later, the fatality rate of SARS was up to 10% at last.17
This study has some limitations. First, only the COVID-19 confirmed cases transferred by EMS in Beijing were included, the first admission to the designated hospitals cases were not enrolled, nor other provinces or cities which dominated by imported. It would be better to cover as wide population as possible, to get more accurate results. Second, the observation time of this study is only 22 days, which is a bit short, and indicators such as discharge rate and fatality need further observation. Last, the official data of 2003 SARS is a month later than the outbreak, its epidemic development curve is not precise. However, this study represents characteristics of early stage of COVID-19 in Beijing, which has certain value for future control and research.
In conclusion, the characteristics of patients infected with COVID-19 in Beijing were obviously different from Wuhan with a lower fatality and higher discharge rate, new infected patients has shifted from the imported to local gradually. The next step in preventing and controlling the COVID-19 infection should be focused on the early isolation of patients and quarantine for close contacts in families and communities.
CRediT authorship contribution statement
Sijia Tian: Conceptualization, Formal analysis, Investigation, Methodology, Resources, Supervision, Writing - original draft. Nan Hu: Formal analysis, Investigation, Methodology, Resources, Supervision. Jing Lou: Formal analysis, Investigation, Supervision. Kun Chen: Formal analysis, Supervision. Xuqin Kang: . Zhenjun Xiang: . Hui Chen: Data curation. Dali Wang: Data curation. Ning Liu: Data curation. Dong Liu: Data curation. Gang Chen: Data curation. Yongliang Zhang: Data curation. Dou Li: Data curation. Jianren Li: Data curation. Huixin Lian: . Shengmei Niu: . Luxi Zhang: Data curation. Jinjun Zhang: Conceptualization, Funding acquisition, Investigation, Validation, Visualization, Writing - original draft, Writing - review & editing.
Declaration of Competing Interest
All authors declare no competing interests.
Acknowledgments
We thank all the Beijing EMS staff for their efforts in transferring the confirmed patients. This study was supported by the Beijing Municipal Science and Technology Project (Z191100004419003) and the National Science and Technology Fundamental Resources Investigation Project (2018FY100600).
References
- 1.WHO. World experts and funders set priorities for COVID-19 research. Feb 12, 2020. https://www.who.int/news-room/detail/12-02-2020-world-experts-and-funders-set-priorities-for-covid-19-research(accessed Feb 13, 2020)
- 2.China National Health Commission. February 10, 2020, update on the novel coronavirus pneumonia outbreak). Beijing: national health commission of the People's Republic of China, 2020. http://www.nhc.gov.cn/xcs/yqtb/202002/4a611bc7fa20411f8ba1c8084426c0d4.shtml(accessed Feb 10, 2020)
- 3.Beijing Health Commission . Beijing Health Commission; Beijing: 2020. Update on the novel coronavirus pneumonia outbreak.http://wjw.beijing.gov.cn/xwzx_20031/wnxw/202002/t20200211_1628034.html February 10, 2020. (accessed Feb 5, 2020) [Google Scholar]
- 4.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020 January 24 doi: 10.1016/S0140-6736(20)30185-9. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Munster V.J., Koopmans M., van Doremalen N. A novel coronavirus emerging in China-key questions for impact assessment. N Engl J Med. 2020 Jan 24 doi: 10.1056/NEJMp2000929. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 6.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Jan 24 doi: 10.1016/S0140-6736(20)30183-5. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020 Jan 29 doi: 10.1056/NEJMoa2001316. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.New coronavirus pneumonial prevention and control program (2nd ed.) (in Chinese). 2020 (http://www.nhc.gov.cn/xcs/zhengcwj/202001/c67cfe29ecf1470e8c7fc47d3b751e88.shtml) (accessedFeb 10, 2020).
- 9.New coronavirus pneumonial diagnosis and treatment program (3rd ed.) (in Chinese). 2020http://www.nhc.gov.cn/xcs/zhengcwj/202001/f492c9153ea9437bb587ce2ffcbee1fa.shtml(accessed Feb10, 2020).
- 10.New coronavirus pneumonial diagnosis and treatment program (5th ed.) (in Chinese). 2020http://www.nhc.gov.cn/xcs/zhengcwj/202002/3b09b894ac9b4204a79db5b8912d4440.shtml (accessed Feb10, 2020).
- 11.Chan J.F., Chan K.H., Kao R.Y. Broad-spectrum antivirals for the emerging middle east respiratory syndrome coronavirus. J Infect. 2013;67(6):606–616. doi: 10.1016/j.jinf.2013.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drazen J.M. SARS-looking back over the first 100 days. N Engl J Med. 2003;349(4):319–320. doi: 10.1056/NEJMp038118. [DOI] [PubMed] [Google Scholar]
- 13.Chen N.S., Zhou M., Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30211-7. Jan 24 (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan J.F., Yuan S., Kok K.H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020 doi: 10.1016/S0140-6736(20)30154-9. Jan 24 (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rothe C., Schunk M., Sothmann P. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020 doi: 10.1056/NEJMc2001468. Jan 30(Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30260-9. Jan 31(Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang S., Wu J., Ding C. Epidemiological features of and changes in incidence of infectious diseases in China in the first decade after the SARS outbreak: an observational trend study. Lancet Infect Dis. 2017;17(7):716–725. doi: 10.1016/S1473-3099(17)30227-X. [DOI] [PMC free article] [PubMed] [Google Scholar]