Abstract
The outbreak of 2019 novel coronavirus (2019-nCoV) pneumonia was reported in Wuhan, Hubei Province, China in December 2019 and has spread internationally. This article discusses how radiology departments can most effectively respond to this public health emergency.
Keywords: 2019-nCoV, COVID-19, WHO, PHEIC, radiology management
BACKGROUND
On January 31, 2020, the World Health Organization declared a new coronavirus outbreak in Wuhan, China as a “Public Health Emergency of International Concern (PHEIC).” On February 13, 2020, the World Health Organization officially named the 2019-nCoV as Corona Virus Disease-2019 in Geneva, Switzerland. The virus spread rapidly in various cities and provinces in China. On February 13, 2020, the Chinese government officially announced that 59,901 patients were diagnosed with the new coronavirus-infected pneumonia, killing 1368 people, on February 22, 2020, the Chinese government officially announced that 76,003 patients were diagnosed with the new coronavirus-infected pneumonia, killing 2,239 people, and putting hundreds of thousands of people were under quarantine observation (1).
The 2019-nCoV belongs to the same coronavirus group as the severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS) viruses that caused two of the more severe epidemics in recent years. As with SARS and MERS, this new coronavirus, 2019-nCoV, is believed to be of zoonotic origin, but may also be transmitted through the respiratory tract, by direct contact and possibly via patients' excreta which may contain the living virus. Thus, 2019-nCoV has created enormous challenges for medical institutions in China (2). This article discusses how radiology departments can most effectively respond to this public health emergency.
RADIOLOGY DEPARTMENT PROCEDURES
Since the radiology department is often the first stop for patients who present with an acute febrile illness, managing these patients will play a key role in the diagnosis of individual patients and management of an epidemic situation (3). The first concern is how best to protect the staff of the radiology department so they do not become infected with the virus and serve as additional vectors spreading the disease.
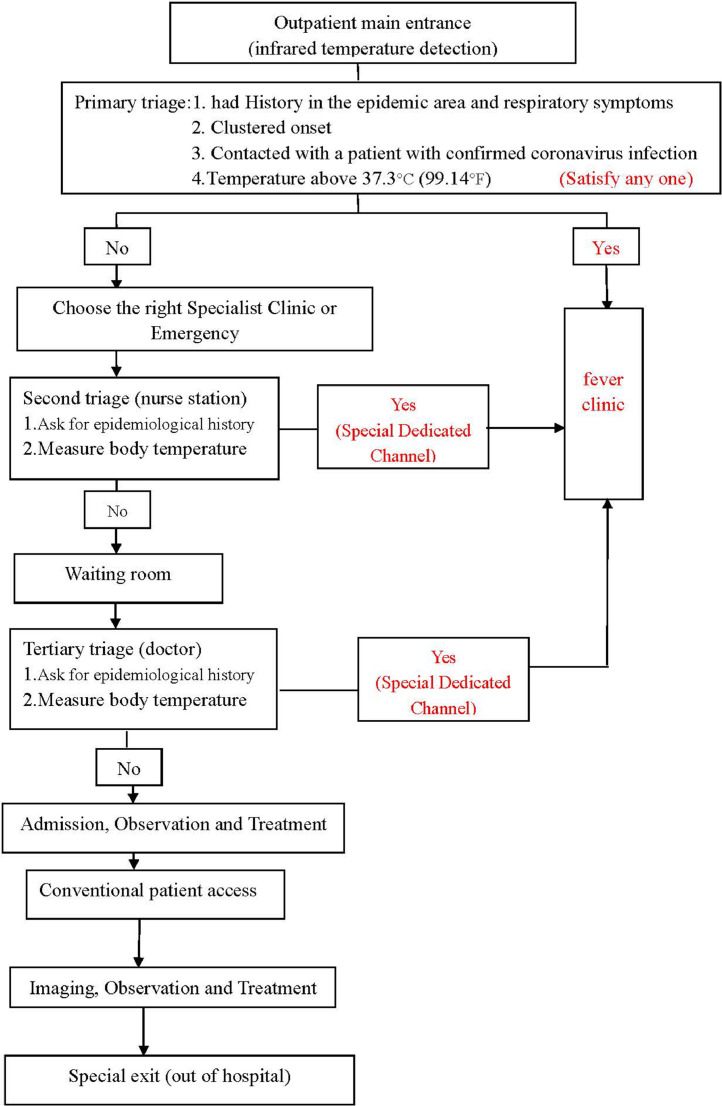
When faced with major public health emergencies from infectious diseases, such as 2019-nCoV, prevention and control should start with the outpatient clinic (Fig 1 ). Patients should undergo infrared temperature detection before entering the health care facility. This type of temperature measurement uses a portable infrared temperature detector to measure the temperature of the patient's head, which is displayed on the device. In the primary triage, patients will be sent to the outpatient fever control area if they have any of the following: (1) coming from the epidemic area and having respiratory symptoms, (2) being part of a cluster of patients with fever and respiratory symptoms, (3) contact with a patient with a confirmed coronavirus infection, or (4) a temperature above 37.3°C (99.14°F).
Figure 1.
Outpatient processing map (for the 2019-nCoV emergency) at the First Affiliated Hospital of Shenzhen University.
Once triaged to the outpatient clinic, further triages are performed by nurses from the outpatient nurses’ station and physicians from the outpatient clinic. After taking the patient's epidemiological history and temperature measurement, potentially infected patients will be sent to the outpatient fever clinic for treatment.
Patients going to fever clinics undergo nucleic acid testing and computed tomography (CT) examinations (4). Currently, the time required for the 2019-nCoV reverse transcription polymerase chain reaction in our institution is 2 hours. Polymerase chain reaction (PCR) is a molecular biology technique used to amplify specific DNA fragments. It can be regarded as a special DNA replication in vitro. In reverse transcription polymerase chain reaction, an RNA strand is reverse transcribed into complementary DNA, which is then used as a template for DNA amplification by PCR. 2019-nCOV (Corona Virus Disease-2019) is a new type of RNA virus. Nucleic acid detection uses RT-RCR to detect the presence of viral nucleic acids in the blood. During this period, a patient will undergo a CT examination and be isolated in an appropriate area of the hospital.
RADIOLOGY CLASSIFICATION AND REGIONAL MANAGEMENT
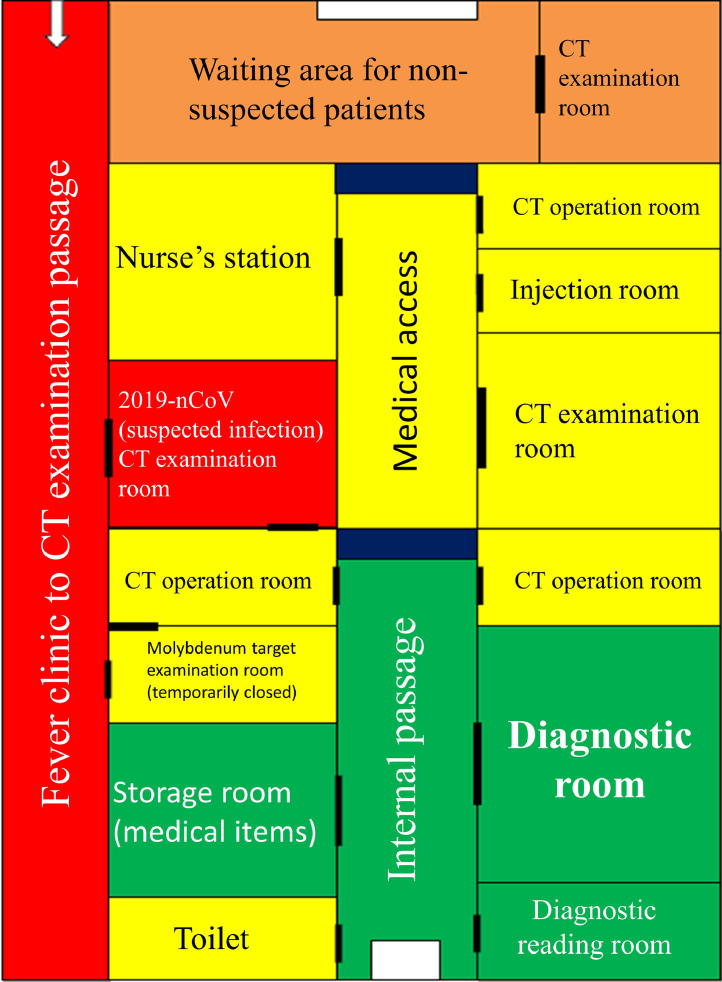
Medical staff are best protected by immediate medical management (Fig 2 ). Due to the shortage of medical supplies, our institution adopted district management and hierarchical protection where the entire department is divided into a contaminated area, a mixed zone, a transition zone and a clean area (5). Hierarchical protection refers to the different levels of protection measures taken in areas with different degrees of infection risk.
Figure 2.
Radiology Department classification and regionalization management map. Red represents contaminated area, orange represents a mixed zone, yellow represents a transition zone, green represents a clean area. (Color version of figure is available online.)
A CT examination room is isolated and used to examine patients suspected of being infected with the 2019-nCoV virus. The passage area from the clinic area where the fever is found to the CT examination room is defined as the contaminated area. Medical personnel performing medical activities in these areas must comply with the secondary protection standards defined by our agency. Medical personnel who have close contact with suspected or confirmed patients must adhere to strict medical protection, which includes: (1) wearing disposable work caps, (2) wearing protective glasses or face masks (antifog type), (3) wearing medical protective masks (N95), (4) wearing protective clothing or isolation clothing, (5) wearing disposable latex gloves (double layered), (6) wearing disposable shoe covers, and (7) strictly implementing good hand hygiene.
Examination rooms and waiting rooms outside the isolation gate are defined as mixed areas, and is where medical staff may contact suspected patients. Medical personnel working in this area should wear (1) disposable work caps, (2) N95 protective masks, (3) isolation gowns, and (4) disposable latex gloves, and strictly perform good hand hygiene. The first-level protection area refers to the area where medical personnel who are engaged in the general diagnosis and treatment activities in ordinary clinics and wards. Medical staff here need to wear disposable work caps, medical surgical masks and work clothes. Patients are forbidden to enter the radiology clean area, which refers to the diagnostic room, which contains the work stations radiologists use for interpretation, and storage room for medical supplies, as contamination of these areas will spread the virus to many parts of the medical center.
DIAGNOSIS AND TREATMENT
All patients must be isolated before receiving the results of the nucleic acid test.
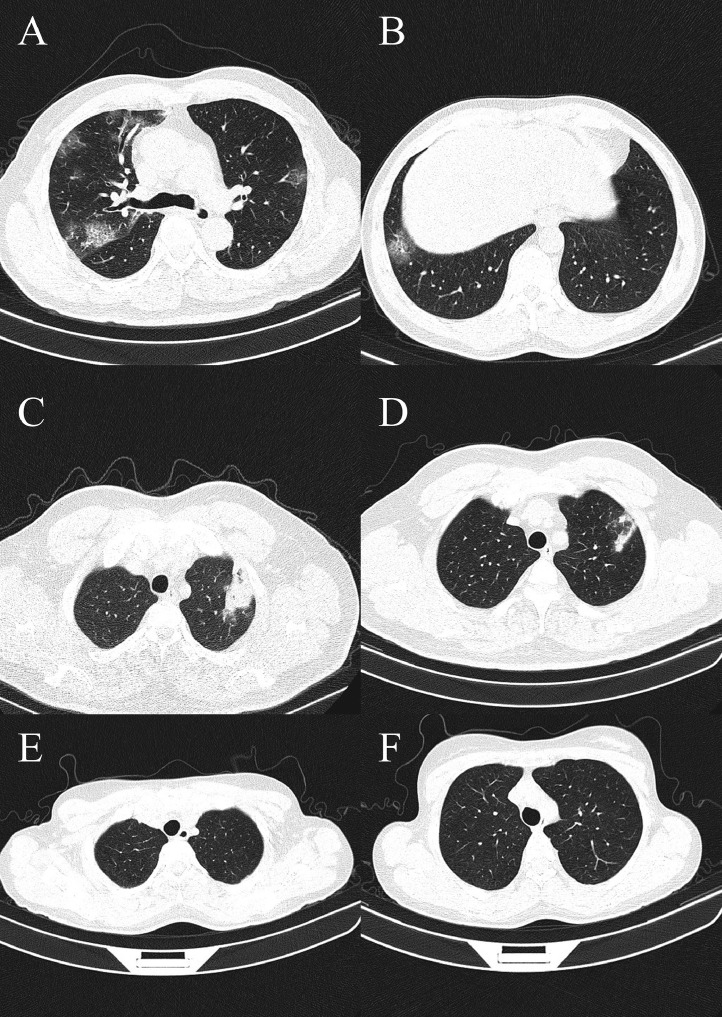
Many patients with positive nucleic acid tests do not have the typical imaging findings of 2019-nCoV pneumonia (Fig 3 ), and patients with negative nucleic acid tests may have typical imaging findings. However, during the isolation period, a second nucleic acid test result may become positive. Therefore, patients with positive nucleic acid tests or typical imaging findings are sent to a designated infectious disease hospital for isolation, observation, and treatment. If the imaging diagnosis is ignored, it may greatly threaten medical personnel and the public.
Figure 3.
All of the previous images were of patients who have a history of living in the epidemic area, and all have been seen for having a fever. (A) and (B) are typical of interstitial changes and ground-glass opacity for pneumonia in patients with positive nucleic acid test results. (C) and (D) show solid lesions on the apex of the lung, which need to be distinguished from tuberculosis; however, these patients had positive nucleic acid test results. (E) and (F) do not show clear lesions, but the nucleic acid test results were positive in these patients.
Early imaging features of the disease in the chest include multiple small patchy opacities and interstitial changes. In the advanced stage, multiple ground glass-like opacities can be seen, often in both lungs. In severe cases, obvious consolidation is present. These findings are not accompanied by pleural effusion. If there are typical imaging features of coronavirus pneumonia, a nucleic acid test is not required to confirm the diagnosis (6).
From January 25, 2020 to February 22, 2020, our institution examined 1467 suspected patients suspected of coronavirus pneumonia; 152 patients had typical imaging findings or positive nucleic acid tests. These patients were sent to a designated infectious disease hospital for centralized isolation and treatment.
DISCUSSION
The epidemic of patients infected with the 2019-nCoV pneumonia poses a huge threat and challenge to the entire Chinese medical system. Many countries have instituted measures to stop the spread of the virus throughout the world. Currently, many hospitals in China have only limited amounts of medical supplies. As one of the first areas in which patients are seen, the radiology department should not delay the use of hierarchical management of the department. Our department is a noncentralized isolation hospital outside of the Hubei region. The patients are diverse, and the medical staff is at risk of infection. Although there may be some deficiencies in the regionalized management of our institution, preliminary prevention and control work can still be promptly instituted. In the face of acute infectious diseases, including SARS, MERS, Zika virus infection, and Ebola virus infection (7), it is very important to maintain strict isolation procedures in the radiology department. This not only protects the medical staff but also improves their clinical work (8).
In conclusion, in an acute infectious disease epidemic, the radiology department plays an essential role in the diagnosis of infected patients. However, management of these potentially infected patients requires protection of both the medical staff and uninfected patients.
References
- 1.Wang W., Tang J., Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan. China J Med Virol. 2020 doi: 10.1002/jmv.25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bassetti M., Vena A., Roberto Giacobbe D. The Novel Chinese Coronavirus (2019-nCoV) infections: challenges for fighting the storm. Eur J Clin Invest. 2020 doi: 10.1111/eci.13209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan China: the mystery and the miracle. J Med Virol. 2020 doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corman V.M., Landt O., Kaiser M. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25(3) doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yoo J.H. The fight against the 2019-nCoV outbreak: an Arduous March has just begun. J Korean Med Sci. 2020;35(4):e56. doi: 10.3346/jkms.2020.35.e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao S., Lin Q., Ran J. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wan Y., Shang J., Graham R. Receptor recognition by novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS. J Virol. 2020 doi: 10.1128/JVI.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]