Abstract
Only a month after the outbreak of pneumonia caused by 2019-nCoV, more than forty-thousand people were infected. This put enormous pressure on the Chinese government, medical healthcare provider, and the general public, but also made the international community deeply nervous. On the 25th day after the outbreak, the Chinese government implemented strict traffic restrictions on the area where the 2019-nCoV had originated—Hubei province, whose capital city is Wuhan. Ten days later, the rate of increase of cases in Hubei showed a significant difference (p = 0.0001) compared with the total rate of increase in other provinces of China. These preliminary data suggest the effectiveness of a traffic restriction policy for this pandemic thus far. At the same time, solid financial support and improved research ability, along with network communication technology, also greatly facilitated the application of epidemic prevention measures. These measures were motivated by the need to provide effective treatment of patients, and involved consultation with three major groups in policy formulation—public health experts, the government, and the general public. It was also aided by media and information technology, as well as international cooperation. This experience will provide China and other countries with valuable lessons for quickly coordinating and coping with future public health emergencies.
Keywords: 2019-nCoV, Traffic restriction, Government, Public health emergency
Human history is littered with wars and pandemics, but the death and fear caused by some pandemics cannot be matched by any war. The one with the largest number of deaths in recent human history, the Spanish flu caused by the H1N1 influenza A virus, had infected 500 million people (almost 1/3 of the world population in 1918 [1]) and killed 25 to 50 million people [2,3]. In the 21st century, human epidemics caused by viruses have continuously appeared in the public eye. Among them, the new infectious diseases caused by wild animal coronavirus infections in humans have attracted the most attention, reminding us that people should be fully prepared to respond to a larger pandemic that may occur at any time in the future.
Coronaviruses of wild animal origin have caused 3 serious human infectious diseases in less than 20 years. The first infectious disease was reported in November 2002, in Guangdong Province, China [4]. While the source of the virus was not identified yet, this disease spread quickly, infecting many medical staff. On February 21, 2003, an infected Guangdong doctor travelled to Hong Kong, leading to spread of the virus globally [5]. Not until March 15, after the World Health Organization (WHO) received reports of cases from Guangdong, Hong Kong, and Hanoi, was a global alert on the disease issued, which was officially named “Severe Acute Respiratory Syndrome (SARS)" [6]. The pathogen originated from bats [7] and the intermediate host was the masked palm civet [8]. At the beginning of the epidemic, the international community lacked experience for containment of this type of outbreak, and the disease was not officially diagnosed until 146 days after the first case appeared [9]. From April to May 2003, the Chinese government established a comprehensive prevention network, allocated 2 billion yuan to epidemic prevention, built a “Xiaotangshan” temporary hospital, and actively treated patients. Because of the low coverage by modern communication networks, there was difficulty in communicating information. Nevertheless, the epidemic response was generally satisfactory [10]. Although interpersonal transmission of the first SARS outbreak (November 2002 to July 2003) was successfully stopped thanks to global cooperation [11], the worldwide spread of the SARS coronavirus (SARS-CoV) still caused 8447 cases and 774 deaths in 32 countries [12].
The second infectious disease was Middle East Respiratory Syndrome caused by MERS-CoV in 2012. It occurred in Saudi Arabia and spread to other countries including the United States, England, France, and South Korea. The mortality rate was as high as 34.4%. As of the end of November 2019, a total of 2468 people had been infected worldwide [13]. According to research results, this coronavirus originated from bats and was transmitted to humans through an intermediate host, the camel [14,15].
In 2019, a new type of coronavirus, which is highly homologous to bat coronavirus, hit China again [16,17]. At the end of December, some hospitals in Wuhan reported several cases of unexplained pneumonia in those with a history of South China seafood market exposure [18,19]. In December 31 the pneumonia cases of unknown origin were officially reported; in early January 2020, market store owners were evacuated in succession; and Hubei Province began to investigate the source of the virus. However, after only two weeks, the number of mysterious pneumonia cases nationwide had reached 198 by January 18, then reaching 830 by January 23 [20], and Wuhan immediately began implementing traffic control to prevent the spread of the disease. The “Level 1 Emergency Response to major public health emergencies” was implemented, and comprehensive epidemic prevention began. One week later (January 30), the official reported number of confirmed domestic cases had reached 9,692, which exceeded the total number of previous cases of SARS in the world [21]. On the same day, WHO announced that 2019-nCOV constitutes a Public Health Emergency of International Concern (PHEIC) [22], which noted that this elusive disease is more dangerous than the one in 2003. The Chinese government also made a series of significant responses in a very short period of time, including the establishment of a leading group of experts for epidemic response [23], the construction of a number of temporary hospitals [[24], [25], [26]], the deployment of medical staff [27], and the implementation of a comprehensive national epidemic prevention policy [28]. It remains to be seen whether these measures can quickly control the spread of 2019-nCOV.
The major outbreaks caused by the spread of wild animal viruses across the species barrier have raised important questions for human society. How do we learn from the experience of China and the international community in responding to the outbreak? What preparations can human society make in advance of pandemics, when faced with a potentially more dangerous pandemic in the future? This article presents the actions taken by the government, experts and international parties in response to the two outbreaks caused by SARS-CoV and 2019-nCoV, and analyzes possible preventive measures in future epidemics through a relationship diagram.
1. 2020 in crisis
Although the 2019-nCOV epidemic broke out rapidly in early 2020, the Chinese government and experts have responded much faster than they did to the SARS outbreak – relying on 17 years of technical and economic experience – and various measures were therefore consecutively carried out.
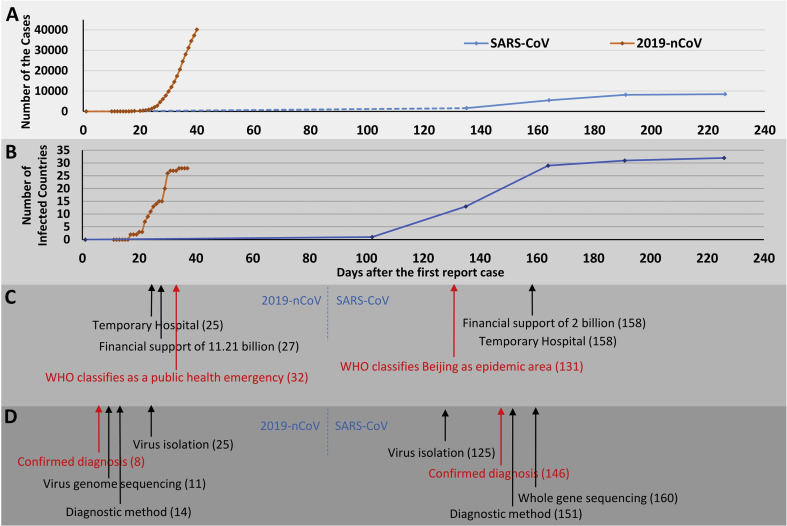
As shown in Fig. 1 A, the challenges brought to us by the two epidemics are quite different. By January 30, 2020, the cumulative number of 2019-nCoV cases in China had exceeded the total number of previous SARS cases worldwide [29], and many new cases appeared in only one month. Currently, there are still more than 3000 new confirmed cases of 2019-nCoV infection daily. As of the date of this publication, the total number of confirmed domestic cases has risen to 78064 [30]. During this period, the diagnosis, isolation, admission and treatment of patients have become the biggest challenges that China and the international community need to face. It is reassuring that the vast majority of cases of 2019-nCOV are still concentrated in China, and the number of transmitting countries and regions is currently 28 (Fig. 1B), slightly lower than the number of countries that reported SARS cases [12,31]. In addition, no deaths have been reported in any country outside of China, except for the death of a pneumonia patient in the Philippines [32] (as of February 9, 2020). Since 2019-nCOV has an incubation period of 5.3–19 days (average of 5.2 days) [33], the effects of international traffic control measures in 2020 need to be further observed.
Fig. 1.
The major progress of research and government measures during the SARS-CoV and 2019-nCoV epidemics. A. The rate of increase in cases during the SARS-CoV and 2019-nCoV outbreaks; B. The increase in number of countries that had cases of infection during the outbreak; C. Government measures; D. Major progress of research. The dotted line in A means that the data are unavailable, the numbers in the brackets in C and D represent the number of days after the first reported case.
Meanwhile, the Chinese government is actively responding to the outbreak (Fig. 1C). On January 24, considering the rapid increase in the number of cases, China began to build several temporary hospitals, including “Huoshenshan” and “Leishenshan”, in many cities of the country. Huoshenshan Hospital was successfully constructed at an astonishing speed, and started to receive patients within ten days [25]. On January 26, the Chinese government invested 11.21 billion RMB; after 11 days [34], the investment increased to 66.74 billion RMB [35] in epidemic prevention and control funds, and has deployed more than 10,000 medical staff nationwide to assist Hubei Province [27]. Back in 2003, China built the Xiaotangshan Temporary Hospital in 6 days [36], with its construction starting as late as 158 days after the first case was reported, indicating that the response to the spread of SARS-CoV was far slower than for 2019-nCoV. Similarly, in the current epidemic, China implemented main domestic response measures before WHO’s announcement of the high risk of a global epidemic; while during SARS, China’s establishment of temporary hospitals and financial support came after WHO’s warning.
The government’s rapid response to the epidemic has benefited in part from the substantial improvement of the national scientific research ability and research equipment, as well as the efficient communication of research results. As shown in Fig. 1D, the disease caused by 2019-nCOV was diagnosed 8 days after the first cases appeared [37], the entire virus gene sequence was obtained on the 11th day, the virus nucleic acid diagnostic technology was established on the 14th day [[38], [39], [40]], the live virus was isolated on the 25th day [41], and the study on the intermediate host was reported on the 39th day [68]. In contrast, the SARS virus was isolated in 125 days [43], the disease was formally diagnosed in 146 days [9], a virus nucleic acid diagnostic method was established in 151 days [44,45], and the full gene sequence of the virus was obtained in 160 days [46]. As noted in Fig. 1C, during the 2019-nCoV epidemic, most of the government’s major epidemic prevention measures were also implemented quickly after the disease was diagnosed.
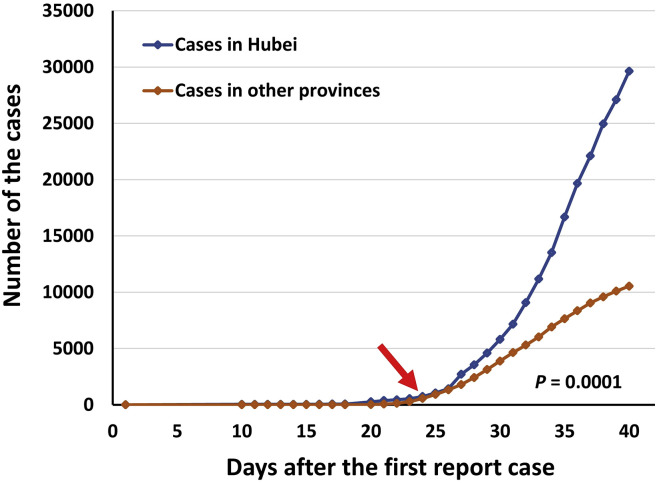
The rapid increase in the number of 2019-nCoV cases in a short period of time has forced society to respond quickly. At present, 2019-nCOV is still spreading rapidly, and the origin of the new virus, transmission modes other than saliva droplets and airborne transmission, the window period, the contagious period after clinical recovery, and patient prognosis are unknown – but the efforts of all parties have begun to bear fruit. In particular, it should be noted that on January 24, 2020, Hubei Province launched the most stringent anti-epidemic traffic control measures in human history, as measured in the number of human individuals affected. Among them, at 9 pm on January 23, Wuhan first launched traffic control [47]. On the second day, other cities in Hubei have also announced measures for epidemic prevention traffic control [48], and rail, high-speed and ordinary road traffic within the jurisdiction of the above-mentioned cities have been suspended to varying degrees, and public transportation such as buses and long-distance passenger transport within the jurisdiction of the city have also been suspended. The control measures appeared to take effect within two days: the case increase rate in other provinces across the country began to be significantly slower than the case increase rate in Hubei Province, as shown in Fig. 2 . Compared with the case number in Hubei Province, the increase in case numbers in other provinces became significantly slower (p = 0.0001).
Fig. 2.
The effect on the increasing rate of cases with strict travel restrictions. Red arrow indicates the date after which Wuhan was under strict travel restriction. It was the first time in human history that the gates of a city with a population of about 9 million were almost totally closed by a virus. The data on day 19 were unavailable. The number of cases in Hubei increased much faster than in other provinces after the travel restrictions were imposed.
This measure established a barrier between the source of infection and healthy uninfected people, in order to block the transmission of the new coronavirus. Although the number of confirmed new cases is still a cause of worry, one can imagine what would have happened if such measures had not been implemented on January 23 or the country had not taken relevant epidemic prevention measures: given the transmission characteristics of 2019-nCOV in China, it is likely that there would have been multiple “Wuhans” by now, and the number of confirmed diagnoses would have been much larger than currently observed. Comparing domestic air passenger traffic data in 2002 and 2018 (the normal passenger traffic in the year before the current outbreak), the national passenger volume in 2018 was 7 times larger than in 2002 [49,50]. One can thus estimate how quickly the new coronavirus would have been transmitted if drastic traffic control measures had not been implemented.
2. Social cooperation during the 2019-nCoV epidemic and lessons for future epidemic prevention
With the increase of the world’s population, improvements and ease of transportation, and the increase of human traffic, the threat of epidemics on human beings is constantly increasing. In addition, despite the unpredictability of each epidemic, the process of battling previous epidemics has brought with it valuable experience for responding to future epidemics. The 2019-nCOV epidemic has challenged the limits of our ability to handle it. As a viral infectious disease that can be transmitted through multiple channels, its onset time also coincided with the Spring Festival (the biggest national holiday in China), when over a billion people begin their annual migration in China. The outbreak also originated in the main traffic hub in China, Wuhan, where both resident and floating populations are dense.
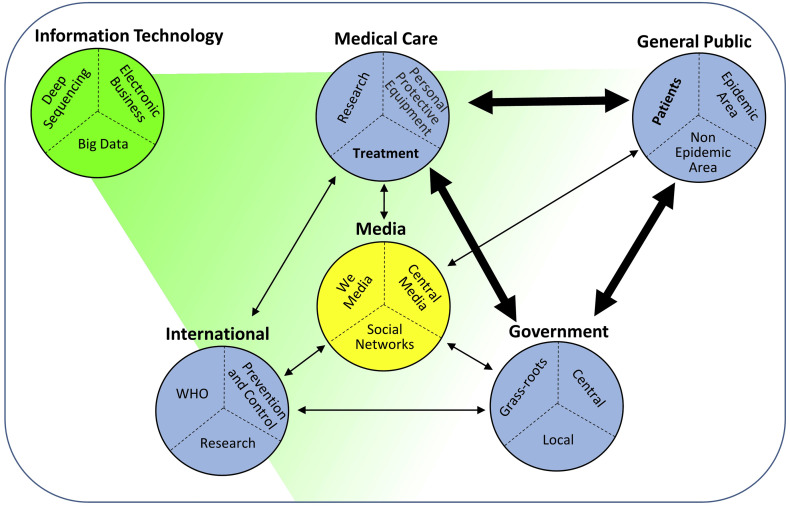
At early stages of the outbreak, Hubei Province had experienced a shortage of personal protection materials, such as masks and hospital supplies. Thus, it began to collect materials from other parts of the country and urgently transferred them to Hubei Province. As of February 6, 2020, there was still shortage of materials in the province [51]; this is a wake-up call for us when dealing with future outbreaks. As shown in Fig. 3 , during a public health emergency, the smooth coordination between the government, medical care and the masses is very important. For example, on February 3, when the number of confirmed cases in Wuhan had reached 6384 [52] and there was a shortage of medical resources, the government promptly claimed stadiums, exhibition halls and other places to establish a number of “square cabin hospitals” for treating non-critical patients. This was done to free up important resources at Huoshenshan Hospital, Leishenshan Hospital and other sites to treat critically ill patients in a more timely manner [53]. The public was promptly guided by governments at all levels in order to maximally prevent the spread of the virus.
Fig. 3.
Interactions in society during the 2019-nCoV pandemic. The arrows represent the interactions between the subjects; the broader arrows indicate the more prominent interactions. Information technology (labelled as green) influences all of the subjects, dramatically improving the process of virus identification, new drug screening, and daily care of the public.
At the same time, cooperation within the medical system enables scientific research results to be used in clinical diagnosis and treatment in a timely manner, and serves as the scientific basis for the government’s response. In addition, prompt communication between international governments served to prevent the spread of the virus worldwide. As of February 9, 2020, 40,171 cases were diagnosed globally, and only 307 cases were found in countries and regions other than China, accounting for 0.76% of the total [54].
Certainly, media and information technology provided important support for societies during the 2019-nCOV epidemic (Fig. 3). At the beginning of 2019, the number of Chinese internet users had reached 829 million, of which 817 million are mobile Internet users, covering almost every corner of the countryside [55]. Back in 2003, there were about 80 million Chinese internet users, mostly concentrated in urban areas [56]; moreover, 63.91% of China’s population was rural [57]. In 2003, television and other media were the main communication channels for epidemic prevention information. In 2019, however, real-time information of the 2019-nCOV epidemic was transmitted in real-time through various channels throughout the country, like WeChat and Weibo like apps. This technology also allows any traveler to check the trend of population flow and exposure to pneumonia patients during their trip at any time. These technologies have greatly facilitated accurate epidemic prevention and control [58].
After the epidemic broke out, the Chinese government adopted a big data platform for epidemic prevention and control —“Close Contact Meter” [59]—on February 8th. By uploading and comparing national health data, it is possible to automatically identify past contacts and potential contacts. The comparison and calculation of the resultant data model provides relative risk coefficients for people, so that the government can carry out precise measures. At the same time, China Unicom formed a joint big data team of more than 100 people, provided the government with 1783 comprehensive epidemic analysis reports and developed 13 data models for epidemic prevention [60]. In addition, e-commerce companies including Alibaba and JD.com donated funds along with a large amount of medical supplies during the epidemic [61], using their industry advantages and logistics to facilitate large-scale material delivery. This level of development in e-commerce can fully overcome logistical obstacles that do not involve direct contact between people, to prevent further viral transmission [62].
Learning from the effective measures used and problems encountered in the prevention and control of this epidemic, the government is likely to set up an emergency decision-making organization when responding to future public health emergencies. Externally, the government needs to guide medical and scientific research and allocate medical care materials, and at the same time, comprehensive epidemic prevention must be implemented rapidly and efficiently. Concurrently, the government also needs to regularly disclose information and ensure international cooperation. For the general population, it is difficult to realize the limitations of government measures and medical care to deal with an emerging infectious disease. However, if the disease spreads too quickly, excessive public support and high expectations may turn into disappointment and propagation of rumors [63]. Patients and uninfected people in both epidemic and non-epidemic areas (Fig. 3) also face different levels of psychological pressure, which also need to be addressed.
Scientific achievements such as development of vaccines, antibodies and antiviral drugs play an important role in fighting epidemics and reducing mortality. Integrating scientific research resources, increasing research investment, strengthening direct cooperation between international and domestic scientists, and accelerating clinical applications of scientific research results enhances the ability to prevent spread of the epidemic or accelerate elimination of the virus.
In summary, in the 2019-nCoV epidemic, the overall response of China and the international community is faster than it was for SARS-CoV. These responses include disease diagnosis, virus isolation, financial support, and temporary hospital construction. To deal with the increasing growth of cases, the Chinese government has adopted comprehensive traffic restrictions in the areas where the epidemic originated. After implementation of the traffic restrictions, the rate of infection in the original outbreak areas and the rest of the country showed a significant difference.
How to fight pandemics will always be a major issue that needs to be addressed worldwide. In 2003, the SARS incident caused global economic losses of US$ 30 billion [64], which exceeded the military expenditures of any one of 221 countries in 2018 [65]. At present we do not have a clear prediction of the funds that would be required to confront a future global pandemic, but it is safe to assume that, in many cases, it would cost much less than the losses caused by the disease [66,67]. Making advance preparations for a pandemic may bring us significant short-term benefits, such as supporting basic health care, encouraging research and development, strengthening interregional cooperation and emergency response systems and biosafety management, and promoting the balanced development of health and security of the world in general.
Declaration of Competing Interest
The authors declare that they have no conflicts of interest.
Acknowledgements
Chungen Pan was supported by a grant from the Panyu Innovation and Entrepreneurship Leading Team Project (2017-R02-4).
References
- 1.Taubenberger J.K., Morens D.M. 1918 Influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12(1):15–22. doi: 10.3201/eid1201.050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taubenberger J.K., Kash J.C., Morens D.M. The 1918 influenza pandemic: 100 years of questions answered and unanswered. Sci Transl Med. 2019;11(502) doi: 10.1126/scitranslmed.aau5485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taubenberger J.K., Reid A.H., Krafft A.E., Bijwaard K.E., Fanning T.G. Initial genetic characterization of the 1918 "Spanish" influenza virus. Science. 1997;275(5307):1793–1796. doi: 10.1126/science.275.5307.1793. [DOI] [PubMed] [Google Scholar]
- 4.Ahmad A., Krumkamp R., Reintjes R. Controlling SARS: a review on China’s response compared with other SARS-affected countries. Trop Med Int Health. 2009;14(Suppl 1):36–45. doi: 10.1111/j.1365-3156.2008.02146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsang K.W., Ho P.L., Ooi G.C., Yee W.K., Wang T., Chan-Yeung M. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348(20):1977–1985. doi: 10.1056/NEJMoa030666. [DOI] [PubMed] [Google Scholar]
- 6.WHO: https://www.who.int/csr/don/2003_03_16/en/.
- 7.Wang L., Shi Z., Zhang S., Daszak P., Eaton B.T. Review of bats and SARS. Emerg Infect Dis. 2006;12(12):1834–1840. doi: 10.3201/eid1212.060401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu B., Zeng L., Yang X., Ge X., Zhang W., Li B. Discovery of a rich gene pool of bat SARS-related coronaviruses provides new insights into the origin of SARS coronavirus. PLoS Pathog. 2017;13(11) doi: 10.1371/journal.ppat.1006698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fouchier R.A., Kuiken T., Schutten M., van Amerongen G., van Doornum G.J., van den Hoogen B.G. Aetiology: Koch’s postulates fulfilled for SARS virus. Nature. 2003;423(6937):240. doi: 10.1038/423240a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pang X., Zhu Z., Xu F., Guo J., Gong X., Liu D. Evaluation of control measures implemented in the severe acute respiratory syndrome outbreak in Beijing, 2003. J Am Med Assoc. 2003;290(24):3215–3221. doi: 10.1001/jama.290.24.3215. [DOI] [PubMed] [Google Scholar]
- 11.Parashar U.D., Anderson L.J. Severe acute respiratory syndrome: review and lessons of the 2003 outbreak. Int J Epidemiol. 2004;33(4):628–634. doi: 10.1093/ije/dyh198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO: https://www.who.int/csr/sars/country/2003_06_30/en/.
- 13.WHO: http://applications.emro.who.int/docs/EMROPub-MERS-SEP-2019-EN.pdf?ua=1&ua=1.
- 14.Memish Z.A., Mishra N., Olival K.J., Fagbo S.F., Kapoor V., Epstein J.H. Middle East respiratory syndrome coronavirus in bats, Saudi Arabia. Emerg Infect Dis. 2013;19(11):1819–1823. doi: 10.3201/eid1911.131172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Omrani A.S., Altawfiq J.A., Memish Z.A. Middle East respiratory syndrome coronavirus (MERS-CoV): animal to human interaction. Pathog Glob Health. 2015;109(8):354–362. doi: 10.1080/20477724.2015.1122852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G. A new coronavirus associated with human respiratory disease in China. Nature. 2020 doi: 10.1038/s41586-020-2008-3. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020 doi: 10.1038/s41586-020-2012-7. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wuhan-MHC: http://wjw.wuhan.gov.cn/front/web/showDetail/2019123108989.
- 19.Kofi Ayittey F., Dzuvor C., Kormla Ayittey M., Bennita Chiwero N., Habib A. Updates on Wuhan 2019 novel coronavirus epidemic. J Med Virol. 2020;92(4):403–407. doi: 10.1002/jmv.25695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.China MHC: http://www.nhc.gov.cn/xcs/yqtb/202001/c5da49c4c5bf4bcfb320ec2036480627.shtml.
- 21.China-MHC: http://www.nhc.gov.cn/xcs/yqtb/202001/a53e6df293cc4ff0b5a16ddf7b6b2b31.shtml.
- 22.WHO: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov).
- 23.SinaNews: http://news.sina.com.cn/o/2020-01-25/doc-iihnzahk6304748.shtml.
- 24.CCTV: http://news.cctv.com/2020/01/25/ARTIj6fo5JL3hCJJuAl3We5C200125.shtml.
- 25.CCTV: http://news.cctv.com/2020/01/27/ARTIMaQ6B6bTGFWXrVvW1Tp6200127.shtml.
- 26.CCTV: http://news.cctv.com/2020/02/02/ARTI4gEc8npt85sZCHx7h7OE200202.shtml. http://news.cctv.com/2020/02/02/ARTI4gEc8npt85sZCHx7h7OE200202.shtml.
- 27.China-MHC: http://www.nhc.gov.cn/xcs/fkdt/202001/50050057b6fe4a2b90763d95c4273ceb.shtml.
- 28.General Office of the State Council,PRC: http://www.gov.cn/xinwen/2020-02/03/content_5474309.htm.
- 29.China-MHC: http://www.nhc.gov.cn/xcs/yqtb/202002/24a796819bf747bd8b945384517e9a51.shtml.
- 30.China-MHC: http://www.nhc.gov.cn/xcs/yqfkdt/202002/741ce06130284a77bfbf699483c0fb60.shtml
- 31.U.S.A-CDC: https://www.cdc.gov/coronavirus/2019-ncov/locations-confirmed-cases.html.
- 32.WHO: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200202-sitrep-13-ncov-v3.pdf?sfvrsn=195f4010_6.
- 33.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001316. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ministry of Finance-PRC: http://www.mof.gov.cn/zhengwuxinxi/caizhengxinwen/202001/t20200126_3464029.htm.
- 35.China-MHC: http://www.nhc.gov.cn/xcs/xwbd/202002/bb65e154ea1e4a23a303355b2e75918e.shtml.
- 36.ChinaDaily: http://www.chinadaily.com.cn/a/202001/30/WS5e32706ba310128217273b2d_2.html.
- 37.China-MHC: http://www.nhc.gov.cn/xcs/xxgzbd/202001/de5f07afe8054af3ab2a25a61d19ac70.shtml.
- 38.Sohu.News: http://www.sohu.com/a/367195671_342073.
- 39.Chu D.K.W., Pan Y., Cheng S.M.S., Hui K.P.Y., Krishnan P., Liu Y. Molecular diagnosis of a novel coronavirus (2019-nCoV) causing an outbreak of pneumonia. Clin Chem. 2020 doi: 10.1093/clinchem/hvaa029. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Corman V.M., Landt O., Kaiser M., Molenkamp R., Meijer A., Chu D.K. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25(3) doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.China-MHC: http://www.nhc.gov.cn/xcs/fkdt/202001/fdae6ee4724542ba82daa1c9ad06ebf7.shtml.
- 43.Guan Y., Zheng B., He Y.Q., Liu X.L., Zhuang Z.X., Cheung C.L. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science. 2003;302(5643):276–278. doi: 10.1126/science.1087139. [DOI] [PubMed] [Google Scholar]
- 44.Poon L.L.M., Chan K.H., Wong O.K., Yam W.C., Yuen K., Guan Y. Early diagnosis of SARS Coronavirus infection by real time RT-PCR. J Clin Virol. 2003;28(3):233–238. doi: 10.1016/j.jcv.2003.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shi Y., Yi Y., Li P., Kuang T., Li L., Dong M. Diagnosis of severe acute respiratory syndrome (SARS) by detection of SARS coronavirus nucleocapsid antibodies in an antigen-capturing enzyme-linked immunosorbent assay. J Clin Microbiol. 2003;41(12):5781–5782. doi: 10.1128/JCM.41.12.5781-5782.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marra M.A., Jones S.J.M., Astell C.R., Holt R.A., Brookswilson A., Butterfield Y.S.N. The genome sequence of the SARS-associated coronavirus. Science. 2003;300(5624):1399–1404. doi: 10.1126/science.1085953. [DOI] [PubMed] [Google Scholar]
- 47.Wuhan-Gov: http://www.wuhan.gov.cn/2019_web/whyw/202001/t20200123_304083.html.
- 48.Hubei-Gov: http://www.hubei.gov.cn/zhuanti/2020/gzxxgzbd/qfqk/202001/t20200124_2014612.shtml.
- 49.CAAC: http://www.caac.gov.cn/XXGK/XXGK/TJSJ/201511/t20151102_8648.html.
- 50.CAAC: http://www.caac.gov.cn/XXGK/XXGK/TJSJ/201905/t20190508_196033.html.
- 51.Hubei-Gov: http://www.hubei.gov.cn/hbfb/bmdt/202002/t20200206_2019987.shtml.
- 52.Hubei-MHC: http://wjw.hubei.gov.cn/fbjd/dtyw/202002/t20200204_2018742.shtml.
- 53.Wuhan-Gov: http://www.wh.gov.cn/2019_web/whyw/202002/t20200206_304478.html.
- 54.WHO: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200209-sitrep-20-ncov.pdf?sfvrsn=6f80d1b9_4.
- 55.ISC-P.R.C: http://www.isc.org.cn/editor/attached/file/20190711/20190711142249_27113.pdf.
- 56.CNNIC: http://www.cnnic.net.cn/hlwfzyj/hlwxzbg/200906/P020120709345366251949.pdf.
- 57.NBS-PRC: http://www.stats.gov.cn/tjsj/ndsj/renkoupucha/2000pucha/html/append21.htm.
- 58.Al-Surimi K., Khalifa M., Bahkali S., El-Metwally A., Househ M. The potential of social media and internet-based data in preventing and fighting infectious diseases: from internet to twitter. Adv Exp Med Biol. 2017;972:131–139. doi: 10.1007/5584_2016_132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.People`s Daily: https://baijiahao.baidu.com/s?id=1657973249061879950&wfr=spider&for=pc.
- 60.SASAC: http://www.sasac.gov.cn/n2588020/n2877938/n2879597/n2879599/c13746709/content.html.
- 61.PeopleCN: http://capital.people.com.cn/n1/2020/0207/c405954-31575857.html.
- 62.CMC-P.R.C: http://images.mofcom.gov.cn/dzsws/201807/20180704151703283.pdf.
- 63.Xie X.F., Zheng R., Xie D.M., Wang H. Analysis on Psychological Panic Phenomenon of SARS. Acta Sci Nat. 2005;41(Suppl 4):628–639. [Google Scholar]
- 64.WHO: https://www.who.int/csr/don/2003_04_11/en/.
- 65.World Bank: https://data.worldbank.org/indicator/MS.MIL.XPND.CD.
- 66.Dixon S., Mcdonald S., Roberts J. The impact of HIV and AIDS on Africa’s economic development. BMJ. 2002;324(7331):232–234. doi: 10.1136/bmj.324.7331.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Keoghbrown M.R., Smith R. The economic impact of SARS: how does the reality match the predictions? Health Pol. 2008;88(1):110–120. doi: 10.1016/j.healthpol.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nature: https://www.nature.com/articles/d41586-020-00364-2