A recent outbreak of Coronavirus 2019 (SARS-CoV-2) has shattered the world and has been declared a pandemic by World Health Organization (WHO) on 11th March 2020 (Fig. 1 ).1., 2. When clinicians worldwide are actively suspecting cases and treating those, who test positive for Coronavirus disease 2019 (COVID-19), at the same time the radiologists are also contributing by interpreting chest computed tomography (CT) scans of COVID-19 patients. We hereby discuss the recently conducted studies analyzing the CT findings of COVID-19 cases.3., 4., 5.
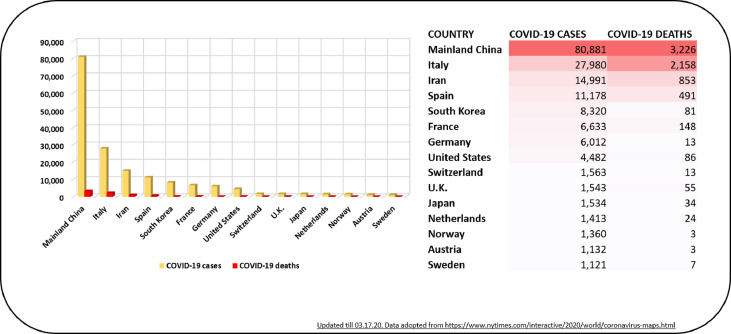
Fig. 1.
Current data on affected patients with COVID-2019 in China and worldwide.
Bernheim et al. outlined the radiological findings in 121 patients in relation to the time between symptom onset and conducting the 1st CT scan on these patients.3 They stratified their patient cohort into 3 groups- [1] Early subgroup, defined as patients who presented between 0 and 2 days (36 patients), [2] Intermediate subgrosup, defined as those who presented between 3 and 5 days (33 patients), [3] Late subgroup, defined as those who presented between 6 and 12 days (25 patients). They reported that 56% of the early subgroup patients (20/36) had normal CT findings. On doing the follow-up CT scans of all the 3 subgroup patients, Bernheim et al. found that, the more the time duration between symptom onset and getting a follow-up CT scan, the more the CT findings were detected. Follow-up CT scans also confirmed an increasing percentage of bilateral lung involvement from 28% in early patients to 88% in late patients.
With regards to the common CT imaging findings, most studies reported ground-glass opacities (GGOs), consolidation, and interlobular thickening as the common abnormalities (Table 1 ). The frequency of lobe involvement was also studied and Bernheim et al. found the right (65%) followed by the left (63%) lower lobe as the most common site of involvement. Similarly, Wu et al. reported the dorsal segment of the right lower lobe (69/80 cases, 86%), a posterior basal segment of the right lower lobe (68/80 cases, 85%), and the lateral segment of the right lower lobe (64/80 cases, 80%) as the top 3 lung segments involved in their study.4 As mentioned above, most studies found bilateral lung disease involvement.
Table 1.
Comparison of various studies conducted recently on radiological findings of COVID-2019 patients.
| Study | PatientNo | Gender | Mean Age | CT Finding | No of lobes/segments involved | MC lung segment/lobe involved |
|---|---|---|---|---|---|---|
| Bernheim et al. (3) | 121 | M- 61 (50.4%) F-60 (49.58%) |
45.3 yrs (18–80 yrs) |
-GGOs plus Consolidation 27 (22%) -GGOs or consolidation 94 (78%) -GGOs without consolidation 41 (34%) -GGOs with consolidation 50 (41%) -Consolidation without GGOs 2 (2%) |
2.11 lobes involved | Right lower lobe 79/121 (65%) |
| Wu et al. (4) | 80 | M-42 (52%) F-38 (48%) |
44 yrs (15–79 yrs) |
-GGOs −73(91%) -Consolidation-50 (63%) -Interlobular septal thickening-47 (59%) |
12 ± 6 lung segments | Dorsal segment of right lower lobe 69/80 (86%) |
| Pan et al. (5) | 63 | M-33 (52.38%) F-30 (47.61%) |
44.9 ± 15.2 yrs | -Patchy/ punctate GGOs 54 (85.7%) -Patchy consolidations 12 (19.0%) -Fibrous stripes 11 (17.5%) -Irregular solid nodules 8 (12.7%) |
3.3 ± 1.8 lobes involved | Not available |
Although, these studies attract significant interest and are very appropriate for the current outbreak, it would certainly benefit from further discussion and refinement. Most of the radiological findings presented in these patients are generic and can be seen in many systemic infectious processes such as pneumonia (viral or bacterial), inflammatory conditions (inflammatory lung diseases, vasculitis) and other cardiac etiologies affecting lung parenchyma such as decompensated congestive heart failure. Even though the authors described cases with confirmed COVID-19, the CT imaging findings could also be due to multiple underlying medical comorbidities, fluid status (volume overload) and other concomitant infections (superadded pneumonia with coronavirus infection).
It would also be interesting to know the difference in the radiological features of patients that required mechanical ventilation (MV) versus patients who did not, since positive pressure ventilation can affect the radiological findings in these patients which none of the studies have reported so far. Knowing the radiological differences in patients that require MV versus in patients that had a more favorable course may have prognostic importance.
Wu et al. also found a significant correlation between the pulmonary inflammation index (PII) and lab results-lymphocyte and monocyte count, serum CRP levels, serum procalcitonin levels, days from illness onset and temperature (P < 0.05). Based on these results, it can be suggested that the patients with the worst blood/laboratory findings are also expected to have worse PII index values.4 , 5 Finally, it is not surprising to find basal lung involvements (right or left), since ill patients would be less ambulatory and hence, likely to develop radiological changes in the dependent areas of the lungs. There are no studies focusing especially on immunocompromised patients, but it is expected that such patients are expected to develop more complications based on the previously established literature.6., 7., 8.
Despite the limitations as discussed above, we believe that similar studies analyzing the COVID-19 CT imaging findings can provide valuable information to the treating physicians and radiologists. However, as of now, it seems that COVID-19 lacks any specific or pathognomonic CT findings limiting its utility for complete reliability and bedside application. Further characterization of radiological features in the right context of patient-specific comorbidities and relation with other medical conditions (superadded pneumonia, underlying heart failure or fluid overload and rheumatological diseases) would definitely add value to the knowledge in this field and educate the treating clinicians, pool of internists, pulmonologists, intensivists and radiologists alike.
Verification
All authors have seen the manuscript and agree to the content and data. All the authors played a significant role in the paper.
Declarations of competing interest
Authors have no conflicts of interest to declare.
References
- 1.Sahu K.K., Mishra A.K., Lal A. Comprehensive update on current outbreak of novel coronavirus infection (2019-nCoV) Ann Transl Med. 2020 doi: 10.21037/atm.2020.02.92. Ahead of Pub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sahu K.K., Mishra A.K., Lal A. Novel coronavirus (2019-nCoV): update on 3rd coronavirus outbreak of 21st century. QJM. 2020 doi: 10.1093/qjmed/hcaa081. pii: hcaa081[Epub ahead of print] PubMed PMID: 32125418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest ct findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 0(0):200463. [DOI] [PMC free article] [PubMed]
- 4.Wu J., Wu X., Zeng W. Chest ct findings in patients with corona virus disease 2019 and its relationship with clinical features. Invest Radiol. 2020 doi: 10.1097/RLI.0000000000000670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan Y., Guan H., Zhou S. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020 doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mishra A.K., Sahu K.K., James A. Disseminated herpes zoster following treatment with benralizumab. Clin Respir J. 2019;13(3):189–191. doi: 10.1111/crj.12998. [DOI] [PubMed] [Google Scholar]
- 7.Sahu K.K., Prakash G., Khadwal A., Varma S.C., Malhotra P. A rare case of hemorrhagic cystitis in allogeneic hematopoietic stem cell transplant patient. Indian J Hematol Blood Transfus. 2016;32(Suppl 1):196–200. doi: 10.1007/s12288-015-0530-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sahu K.K., Mishra A.K., Lal A., Abraham G.M. Mycobacterium Avium complex: a rare cause of pancytopenia in HIV infection. J Microsc Ultrastruct. 2020;8(1):27–30. doi: 10.4103/JMAU.JMAU_18_19. [DOI] [PMC free article] [PubMed] [Google Scholar]