Highlights
-
•
The prevalence of posttraumatic stress symptoms (PTSS) in China hardest-hit areas a month after the COVID-19 outbreak was 7%.
-
•
Hierarchical regression analysis and non-parametric test suggested that women reported significant higher PTSS in the domains of re-experiencing, negative alterations in cognition or mood, and hyper-arousal.
-
•
Participants with better sleep quality or less frequency of early awakenings reported lower PTSS.
Abstract
The outbreak of COVID-19 in China in December 2019 has been identified as a pandemic and a health emergency of global concern. Our objective was to investigate the prevalence and predictors of posttraumatic stress symptoms (PTSS) in China hardest-hit areas during COVID-19 outbreak, especially exploring the gender difference existing in PTSS. One month after the December 2019 COVID-19 outbreak in Wuhan China, we surveyed PTSS and sleep qualities among 285 residents in Wuhan and surrounding cities using the PTSD Checklist for DSM-5 (PCL-5) and 4 items from the Pittsburgh Sleep Quality Index (PSQI). Hierarchical regression analysis and non-parametric test were used to analyze the data. Results indicated that the prevalence of PTSS in China hardest-hit areas a month after the COVID-19 outbreak was 7%. Women reported significant higher PTSS in the domains of re-experiencing, negative alterations in cognition or mood, and hyper-arousal. Participants with better sleep quality or less frequency of early awakenings reported lower PTSS. Professional and effective mental health services should be designed in order to aid the psychological wellbeing of the population in affected areas, especially those living in hardest-hit areas, females and people with poor sleep quality.
1. Introduction
On 30 December 2019, a cluster of pneumonia cases of unknown etiology was reported in Wuhan, Hubei Province, China. On 9 January 2020, China CDC reported a novel coronavirus as the causative agent of this outbreak, which is phylogenetically in the SARS-CoV clade. On 30 January 2020, the World Health Organization (WHO) declared the emergence of the novel coronavirus as a public health emergency of international concern (PHEIC) (Eurosurveillance Editorial, 2020), which is the sixth PHEIC under the International Health Regulations (IHR). On Feb 11, 2020, this novel coronavirus was officially named as Corona Virus Disease 2019 (COVID-19) by WHO. Up to 9 March 2020, 109,577 laboratory-confirmed COVID-19 cases, including 3809 deaths, have been reported worldwide, mainly in Hubei province of China (67,743 cases, 3007 deaths), and 28,673 cases from 104 other countries around the world with accordance to World Health Organization (Novel Coronavirus(2019-nCoV): Situation Report - 49, 2020). As Wuhan city is a major transportation hub with a population of more than 11 million people, the potential impact of global COVID-19 outbreaks is high. Such outbreaks of infectious disease has significant potential for psychological contagion, and typically result in widespread fear, anxiety and a variety of psychological problems, and then incur stigmatization of patients with the disease and their relations, of care workers, even of all residents in hardest-hit areas (Mak et al., 2010; Perrin et al., 2009).
Post-traumatic Stress symptoms (PTSS) follows traumatic occurrences outside the range of common human experience such as violent physical assaults, torture, accidents, rape or natural disasters and is characterized by a typical symptom pattern of intrusions, persistence of trauma, relevant stimuli avoidance, emotional numbing and physiological hyper-arousal (Deja et al., 2006). Several studies have explored the psychological effect during such epidemics, such as Severe Acute Respiratory Syndrome (SARS) and H1N1. One study reported that 3.7% of public cases, including 9.6% of “impacted group” (they or their friends and family had been quarantined, or suspected of being infected), had experienced depression symptoms since the SARS outbreak (Ko et al., 2006). Another study showed 17.3% significant mental symptoms among health care workers during SARS epidemic (Lu et al., 2006). As to research on PTSS, Mak et al. (2010)and Lam et al. (2009) both reported more than 40% of SARS survivors had experienced PTSS at one time during the outbreak. Meanwhile, those respondents who had been isolated, worked in high-risk workplaces such as SARS wards, or had friends or close relatives who contacted SARS were two to three times more likely to develop high levels of PTSS than those who were not exposed to the virus(Wu et al., 2009). In consequence, PTSS should be pay more attention during the outbreak of COVID-19.
As the number of infections increasing, the lack of clear and definite information of virus from the media, the shortage of medical workers and resources, and the lack of masks and protecting supplies in the marketplace resulted in the Chinese people, especially Wuhan residents, suffering intense anxiety due to the uncertainty and insecurity they experienced in the first several weeks. Since the metropolitan-wide quarantine of Wuhan and surrounding cities, which began Jan 23–24, 2020, people bombarded with various discomforting network information, the mental health of public in Wuhan and surrounding cities should not be overlooked either. Although the psychosocial impact will cause a huge impediment to COVID-19 control in these regions, there are barely reports focusing on it so far, except that the local government of Wuhan has implemented policies to address these mental health problems for medical works(Kang et al., 2020).
This study aimed to provide information about the prevalence of PTSS among residents in Wuhan and surrounding cities, and to explore the related factors of the occurrence of PTSS.
2. Methods
2.1. Participants
The psychological impact analysis of COVID-19 Study was conducted in Wuhan and surrounding cities, Hubei Province, which is the hardest-hit area of COVID-19 in China, between January 30 and February 8, 2020. Thirty-nine survey questions were sent to 300 Wuhan and surrounding cities residents who agreed to participate in the study via the Internet. The inclusion criteria were a) age > 18 years, b) no dyslexia, and c) no cognitive impairment. The exclusion criterion was that the answer time for all 39-items questions was more than 30 min or less than 2 min. At recruitment the following parameters were collected: demographic information (gender, age, occupation, education state), birthplace, current and previous location, contact frequency with COVID-19 and infected patients, quarantine status and exercise.
2.2. Measurement of PTSS
PTSS were assessed by the PTSD Checklist for DSM-5 (PCL-5)(Blevins et al., 2015). The PCL-5 is a self-report measure, consisting of 20 items that correspond directly to the DSM-5 PTSD. Each item reflected the severity of a particular symptom, rated on a five-point Likert scale from 0 (not at all) to 4 (extremely) during the previous month. The score of each symptom cluster was calculated as the sum of the corresponding items. PTSS severity (total symptoms) was defined as the sum of the scores of all PCL-5 symptom clusters. The PCL-5 can determine a provisional diagnosis in two ways, a) the presence (endorsed as 2 or greater) of at least one re-experiencing symptom (Criterion B item; questions 1–5), one avoidance symptom (Criterion C item; questions 6–7), two negative alterations in cognition or mood symptoms (Criterion D items; questions 8–14) and two arousal symptoms (Criterion E items; questions 15–20), and b) the sum of total score over cut-point score of 33 point. Based upon current psychometric work, the Chinese version of the original PCL-5 has been validated and is widely used in trauma-related research and practice(Wang et al., 2015).
Wuhan and surrounding cities were the hardest-hit area during the COVID-19 outbreak, causing residents of their being faced with high risks of infection of this fatal pandemic. According to Life Events Checklist for DSM-5 (LEC-5) of PCL-5, this kind of experience was a traumatic event (Weathers et al., 2013). Thus, in present study, Residents of Wuhan and surrounding cities were selected and were instructed to rate how much they were bothered by the outbreak of COVID-19 in the last month upon answering PCL-5.
2.3. Measurement of sleep quality and disturbance
Sleep quality and disturbances were assessed using 4 items of the Pittsburgh Sleep Quality Index (PSQI), a self-report questionnaire containing 9 questions (19 total items) that measure sleep quality and disturbance over the previous 1-month time interval. The 4 items we extracted are a) Subjective sleep quality by asking “how good is your sleep quality?”, b) Unable to fall asleep within 30 min by asking “do you have difficulty in starting sleep?”, c) Easily waking during the night or too early in the morning by asking “do you have easy waking during sleep and early waking in the morning?”, and d) Sleep duration by asking “what is your actual sleep time recently?” within 1-month lasted. Single-item sleep measures have been used in previous studies (Cappelleri et al., 2009; Pien et al., 2008), with evidence that the single-item component of subjective sleep quality correlated most highly with global scores on the full PSQI (Carpenter and Andrykowski, 1998).
2.4. Data analysis
First, we report the prevalence and demographic data of the subjects. Second, t-test and one-way variance analysis (ANOVA) were used to analyze PCL-5 scores among different demographic and exposure groups. Third, the hierarchical regression analysis was applied to identify independent variables associated with PTSS. Last, the gender difference in the PCL-5 scores and the relation between the PTSS and sleep quality were then further explored by means of non-parametric and t-test respectively.
3. Results
3.1. The prevalence and demographic characteristics
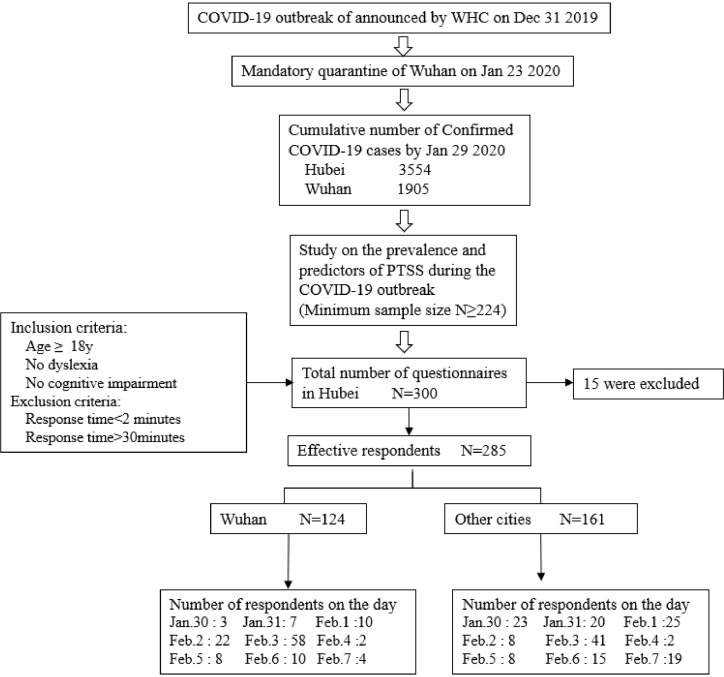
A total of 285 participants were recruited in the study, among which 124(43.5%) were currently in Wuhan, and 188(66%) were previously in Wuhan. Fig. 1 shows each step of the enrolment. The sample size required for an alpha of 0.05 and a power of 80% is 224 cases. Twenty of 285 participants (7%) met the criteria of PTSS symptoms. They treated each item rated as 2 = “Moderately” or higher as a symptom endorsed, and followed the DSM-5 diagnostic rule which requires at least: 1 Criterion B item, 1 Criterion C item, 2 Criterion D items, and 2 Criterion E items.
Fig. 1.
Sampling frame.
The comparison between groups of demographic information, exposure history, and sleep quality in PCL-5 scores is shown in Table 1 . Female respondents had statistically significant higher PCL-5 scores than male respondents (P<0.01). Respondents both currently and previously in Wuhan had statistically significant higher PCL-5 scores than respondents outside the area (P<0.05). Populations more susceptible to infection had statistically significant higher PCL-5 scores(P<0.01). Respondents with poorer subjective sleep quality, more frequent failure of sleep initiation, more frequent early waking during sleep, and less sleep duration had statistically significant higher PCL-5 scores (P<0.001).
Table 1.
Demographic information, exposure history, sleep quality and group differences of PCL-5 scores.
| Respondents | PCL-5 Scores | F/t | p-value | |||
|---|---|---|---|---|---|---|
| N | % | Mean | SD | |||
| Age | ||||||
| ≤35 | 136 | 47.7 | 13.70 | 12.20 | −0.924 | 0.356 |
| >35 | 149 | 52.3 | 14.99 | 11.33 | ||
| Gender | ||||||
| Male | 130 | 45.6 | 12.02 | 10.74 | −3.185 | 0.002 |
| Female | 155 | 54.4 | 16.35 | 12.22 | ||
| Education level | ||||||
| High school or below | 50 | 17.5 | 12.24 | 13.49 | 1.553 | 0.213 |
| University or college | 173 | 60.7 | 15.31 | 12.11 | ||
| Postgraduate or above | 62 | 21.8 | 13.48 | 8.72 | ||
| Currently in Wuhan | ||||||
| No | 161 | 56.5 | 13.03 | 10.95 | −2.210 | 0.028 |
| Yes | 124 | 43.5 | 16.11 | 12.55 | ||
| Previously in Wuhan | ||||||
| No | 97 | 34.0 | 12.37 | 10.67 | −2.077 | 0.039 |
| Yes | 188 | 66.0 | 15.40 | 12.17 | ||
| Classification of susceptible population | ||||||
| General public | 248 | 87.0 | 13.63 | 10.57 | 4.238 | 0.006 |
| Close contact | 21 | 7.4 | 20.71 | 16.06 | ||
| Health care workers | 12 | 4.2 | 14.08 | 11.85 | ||
| Confirmed or suspected cases | 4 | 1.4 | 27.75 | 32.76 | ||
| Subjective sleep quality | ||||||
| Very good | 103 | 36.1 | 9.16 | 8.51 | 36.744 | <0.001 |
| Good | 123 | 43.2 | 13.39 | 9.14 | ||
| Bad | 49 | 17.2 | 23.88 | 11.65 | ||
| Very bad | 10 | 3.5 | 33.60 | 21.27 | ||
| Unable to fall asleep within 30 min | ||||||
| No | 179 | 62.8 | 10.65 | 9.50 | 30.626 | <0.001 |
| <Once a week | 39 | 13.7 | 15.62 | 9.18 | ||
| once or twice a week | 43 | 15.1 | 20.16 | 8.78 | ||
| 24 | 8.4 | 29.75 | 17.49 | |||
| Easily waking during the night or too early in the morning | ||||||
| No | 156 | 54.7 | 11.33 | 9.92 | 15.812 | <0.001 |
| 36 | 12.6 | 12.53 | 9.58 | |||
| once or twice a week | 56 | 19.6 | 17.61 | 10.69 | ||
| 37 | 13.0 | 24.11 | 15.64 | |||
| Sleep duration | ||||||
| 153 | 53.7 | 11.89 | 9.11 | 10.152 | <0.001 | |
| 6–7h | 80 | 28.1 | 14.30 | 12.14 | ||
| 5–6h | 40 | 14.0 | 21.38 | 13.61 | ||
| 12 | 4.2 | 23.17 | 18.81 | |||
| Total | 285 | 100.0 | ||||
3.2. Related factors of the occurrence of PTSS
The results of the hierarchical regression analysis are presented in table 2 . Statistically significant variables in table 1 were used as control variables. Gender and educational levels had significant effects on PCL-5 scores in the model (step 1). As shown in step 2, gender (β = 0.192, p < 0.001) and population susceptibility (β = 0.153, p < 0.01) are positively associated with PCL5-5 scores. As shown in step 3, subjective sleep quality was positively associated with PCL-5 scores (β= 0.312, p < 0.001), unable to fall asleep was positively associated with PCL-5 scores (β = 0.172, p < 0.01). Gender was found to be associated with PCL-5 scores (β= 0.102, p < 0.05).
Table 2.
Regression analyses with PCL-5 score as the dependent variable (n = 285).
| Variables | PCL-5 score | R square | Adjusted R square | R Square Change | F | p-value | |||
|---|---|---|---|---|---|---|---|---|---|
| B | β | t | |||||||
| Step 1 | .051 | .037 | .051 | 3.730 | .006 | ||||
| Age | .041 | .043 | .696 | ||||||
| Female vs. Male | 4.621 | .196 | 3.350*** | ||||||
| High school or below vs. University or college | −4.180 | −0.136 | −2.125* | ||||||
| Postgraduate or above vs. University or college | −1.930 | −0.068 | −1.131 | ||||||
| .089 | .066 | .039 | 3.880 | <0.001 | |||||
| Step 2 | Age | .019 | .020 | .317 | |||||
| Female vs. Male | 4.526 | .192 | 3.326*** | ||||||
| High school or below vs. University or college | −2.901 | −0.094 | −1.406 | ||||||
| Postgraduate or above vs. University or college | −2.247 | −0.079 | −1.329 | ||||||
| Currently in Wuhan Yes vs. No | 1.391 | .059 | .909 | ||||||
| Previously in Wuhan Yes vs. No | 2.036 | .082 | 1.262 | ||||||
| High risk vs. Low risk public | 5.339 | .153 | 2.637** | ||||||
| .303 | .274 | .213 | 10.764 | <0.001 | |||||
| Step 3 | Age | .023 | .024 | .412 | |||||
| Female vs. Male | 2.407 | .102 | 1.958* | ||||||
| High school or below vs. University or college | −1.718 | −0.056 | −0.933 | ||||||
| Postgraduate or above vs. University or college | −1.771 | −0.062 | −1.186 | ||||||
| Currently in Wuhan Yes vs. No | .868 | .037 | .641 | ||||||
| Previously in Wuhan Yes vs. No | 1.380 | .056 | .962 | ||||||
| High risk vs. Low risk public | 1.309 | .038 | .709 | ||||||
| Subjective sleep quality=Bad & Very Bad vs. Good & Very Good | 9.043 | .312 | 4.816*** | ||||||
| Unable to fall asleep within 30 min=Yes vs. No | 4.178 | .172 | 2.750** | ||||||
| Easily waking during the night or too early in the morning | 1.692 | .072 | 1.228 | ||||||
| Sleep duration ≤7 h vs.>7h | 1.575 | .067 | 1.164 | ||||||
Note: B= unstandardized beta; β = standardized regression weight. The education level was transformed into two dummy variables (High school or below vs. University or college, Postgraduate or above vs. University or college) with the University or college as the reference group. Classification of susceptible population was transformed into two groups (Low risk=General public, High risk=Others). Subjective sleep quality was transformed into two groups (Bad & Very Bad vs. Good & Very Good). Unable to fall asleep within 30 min was transformed into two groups (Yes vs. No). Easily waking during the night or too early in the morning was transformed into two groups (Yes vs. No).Sleep duration was transformed into two groups (≤7 h vs.>7 h). *, P<0.05; **, P<0.01; *, P<0.001.
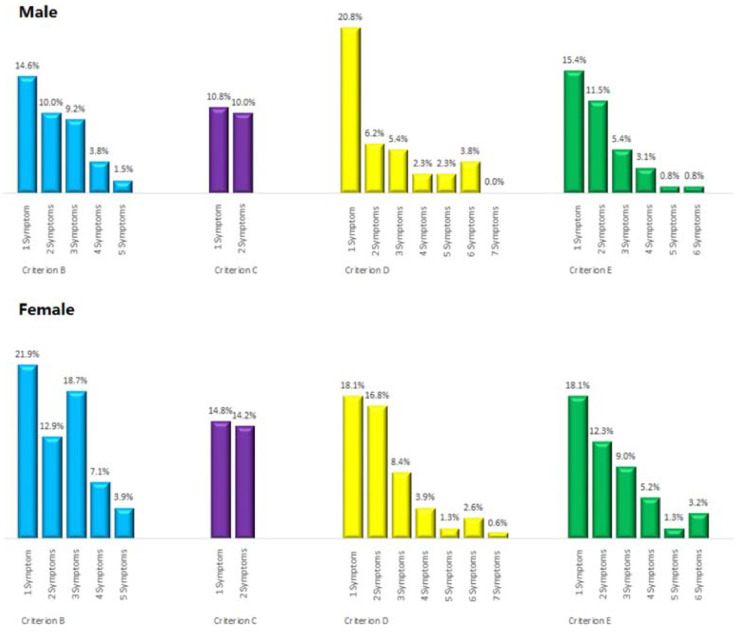
3.3. The gender difference in the PTSS
Symptom prevalence has been shown in Fig. 2 , showing higher symptom prevalence in females. For example, 1 symptom represent only one item that participants rated 2 or higher in the Criterion B, and the prevalence of male in 1 symptom in the Criterion B was 14.6%, while female was 21.9%. As showed in the Fig. 1, females had higher re-experiencing, negative alterations in cognition or mood and hyper-arousal prevalence than males. And both Mann-Whitney U and Wilcoxon W tests demonstrated significant differences of PCL B, D and E scores in male and female respondents.
Fig. 2.
Prevalence differences of PTSS on four Criterion between male and female.
Note: 1 symptom represented only one item of all the items in the Criterion that participants rated 2 or higher and 2 symptoms represented 2 items of all the items in the Criterion that participants rated 2 or higher. For example, in the Criterion B, 14.6% of male rated 2 or higher on one item of all the 5 items of Criterion B. Mann-Whitney U test was used to compare the differences in the prevalence of PTSD symptoms on four Criterion between genders. In the Criterion B, U=−4.209, p-value <0.001. In the Criterion C: U=−1.488, p-value =0.112. In the Criterion D. U=−1.994, p-value <0.05. In the Criterion E: U=−2.273, p-value <0.05. So female show more symptoms than male on B, D, and E Criterion.
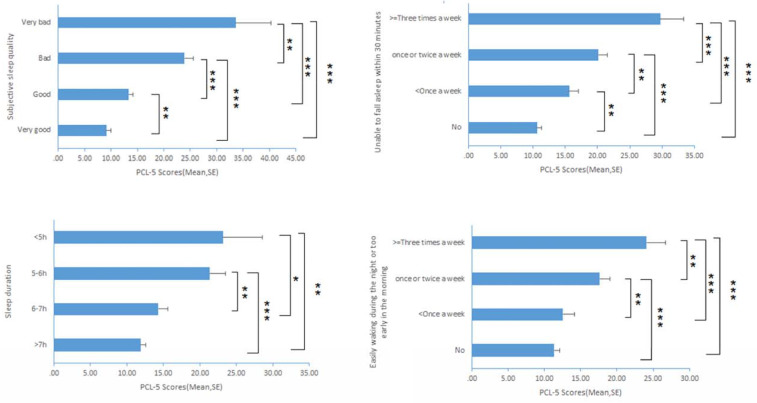
3.4. The group difference of the PTSS in sleep quality and disturbance
Subgroup analysis of PCL-5 scores in sleep quality and disturbance has been shown in Fig. 3 . Pairwise comparison between the 2 significant items in PSQI scores (subjective sleep quality and “unable to fall asleep within 30 min”) was statistically significant. It indicated that the better the subjective sleep qualities, the lower the PCL-5 scores. Similarly, the less the frequency of the reported early awakenings, the lower the PCL-5 scores.
Fig. 3.
Group Differences of PCL-5 scores by Sleep quality
Note: *, p-value < 0.05; **, p-value < 0.01; ***, p-value < 0.001.
4. Discussion
This study firstly found that the prevalence of PTSS a month after the COVID-19 epidemic for hardest-hit areas in China was 7%. Compared with a previous study (Ko et al., 2006), which reported a prevalence of 3.7% of depression symptoms during the post-SARS epidemic for an extrapolated target population in Taiwan. This psychiatrically outbreak seems to have an even greater impact on the public. The reason for this is that most PTSS cases in the current study are actually acute stress disorders instead of chronic psychiatrically problems. It is suggested that most of these acute episodes resembling PTSS may abate in the ensuing period, and only a minority develops chronic disorders (Bryant, 2003). Considering the current epidemic situation that COVID-19 is still dominating headlines throughout the world, the quarantine of Hubei province even China will not be lifted in the near future. Therefore, we have reason to believe that the prevalence of PTSS among the public of the hardest-hit areas will be more severe than the results of this study.
In addition, the study analyzed the difference of PTSS prevalence in gender. To our knowledge, this is the first study to analyze gender-associated PTSS sub-symptom prevalence after public pandemic catastrophes. The study demonstrated higher symptom prevalence in females. In sub-symptom analysis of PCL-5, women suffer more re-experiencing, negative alterations in cognition or mood and hyper-arousal.
In the subgroup of PTSS, it is demonstrated that female respondents have more re-experiencing sub-symptoms than males. This result is consistent with previous studies, among which showed that after traumatic events, acute psychological disorders characterized by intrusive memories are more prevalent in women than men (Kendler et al., 2001; McLean and Anderson, 2009). Some evidence suggests that (fluctuations in) ovarian hormone levels are responsible for altered sensitivity to emotional stimuli during certain phases in the menstrual-cycle in which the intrusive flashbacks were enhanced and this may form the basis of a specific vulnerability to psychological disorders in women (Soni et al., 2013).
Also, we found that female respondents have more negative alterations in cognition or mood sub-symptoms than males. There has been no evidence to suggest the reason for the difference, but animal studies have shown different mood changes in rats of different genders, with female rats showing stronger emotional changes than male rats (Yang et al., 2019).
Moreover, female respondents have higher prevalence of arousal sub-symptom. Some studies have demonstrated that gender differences of fear processing may contribute to higher arousal symptoms and higher PTSS prevalence in women. Experimental studies found that women show more reactivity than men in neural networks associated with fear and arousal responses (Felmingham et al., 2010), and greater differential conditioned skin conductance responses to aversive stimuli (Inslicht et al., 2013). It has been proposed that hyper-activation of neural fear processing networks can explain gender differences in PTSS prevalence (Olff et al., 2007).
The study further demonstrated relationship between self-reported sleep condition and PTSS prevalence, showing participants with worse sleep quality had higher PTSS prevalence. This is in line with previous studies, indicating that poor sleep quality has been linked to both the onset and maintenance of PTSS (Richards et al., 2019). It is reasonable to understand the relationship between sleep quality and PTSS, especially in the worst affected region. This finding provides an effective intervention point for the acute PTSS.
5. Limitation and future directions
Although our study gives a cross-sectional analysis of the prevalence of acute PTSS and sub-symptoms, the time frame is short and future studies are needed for chronic courses and prognosis of PTSS following nation-wide epidemics.
6. Conclusion
2019-Cov pandemics have high prevalence of PTSS in the hardest-hit areas in China of 7%. Most importantly, PTSS sub-symptoms, including re-experiencing, negative alterations in cognition or mood and hyper-arousal, are more common in females than males. Better subjective sleep quality and unfragmented sleep pattern are associated with lower PTSS prevalence. Public attention should be paid with the high prevalence of PTSS and significant gender difference, and certain measures should be prepared to prevent PTSS and other mental problems, especially for women.
Ethics approval and consent to participate
This study was approved by the ethics committees of Naval Medical University.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no conflicts of interest.
Acknowledgments
The authors would like to acknowledge the volunteers who participated in the study.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.112921.
Appendix. Supplementary materials
References
- Blevins C.A., Weathers F.W., Davis M.T., Witte T.K., Domino J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J. Trauma Stress. 2015;28(6):489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Bryant R.A. Early predictors of posttraumatic stress disorder. Biol. Psychiatry. 2003;53(9):789–795. doi: 10.1016/s0006-3223(02)01895-4. [DOI] [PubMed] [Google Scholar]
- Cappelleri J.C., Bushmakin A.G., McDermott A.M., Sadosky A.B., Petrie C.D., Martin S. Psychometric properties of a single-item scale to assess sleep quality among individuals with fibromyalgia. Health Qual. Life Outcomes. 2009;7(54) doi: 10.1186/1477-7525-7-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter J.S., Andrykowski M.A. Psychometric evaluation of the pittsburgh sleep quality index. J. Psychosom. Res. 1998;45(1):5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- Deja M., Denke C., Weber-Carstens S., Schröder J., Pille C.E., Hokema F., ..., Kaisers U. Social support during intensive care unit stay might improve mental impairment and consequently health-related quality of life in survivors of severe acute respiratory distress syndrome. Crit. Care. 2006;10(5):R147. doi: 10.1186/cc5070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eurosurveillance Editorial T. Note from the editors: World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Euro Surveill. 2020 doi: 10.2807/1560-7917.ES.2020.25.5.200131e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felmingham K., Williams L.M., Kemp A.H., Liddell B., Falconer E., Peduto A., Bryant R. Neural responses to masked fear faces: sex differences and trauma exposure in posttraumatic stress disorder. J. Abnorm. Psychol. 2010;119(1):241–247. doi: 10.1037/a0017551. [DOI] [PubMed] [Google Scholar]
- Inslicht S.S., Metzler T.J., Garcia N.M., Pineles S.L., Milad M.R., Orr S.P., ..., Neylan T.C. Sex differences in fear conditioning in posttraumatic stress disorder. J. Psychiatr. Res. 2013;47(1):64–71. doi: 10.1016/j.jpsychires.2012.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Li Y., Hu S., Chen M., Yang C., Yang B.X., ..., Liu Z. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020 doi: 10.1016/s2215-0366(20)30047-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K.S., Thornton L.M., Prescott C.A. Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am. J. Psychiatry. 2001;158(4):587–593. doi: 10.1176/appi.ajp.158.4.587. [DOI] [PubMed] [Google Scholar]
- Ko C.H., Yen C.F., Yen J.Y., Yang M.J. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin. Neurosci. 2006;60(4):397–403. doi: 10.1111/j.1440-1819.2006.01522.x. [DOI] [PubMed] [Google Scholar]
- Lam M.H., Wing Y.K., Yu M.W., Leung C.M., Ma R.C., Kong A.P., ..., Lam S.P. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch. Intern. Med. 2009;169(22):2142–2147. doi: 10.1001/archinternmed.2009.384. [DOI] [PubMed] [Google Scholar]
- Lu Y.C., Shu B.C., Chang Y.Y., Lung F.W. The mental health of hospital workers dealing with severe acute respiratory syndrome. Psychother. Psychosom. 2006;75(6):370–375. doi: 10.1159/000095443. [DOI] [PubMed] [Google Scholar]
- Mak I.W., Chu C.M., Pan P.C., Yiu M.G., Ho S.C., Chan V.L. Risk factors for chronic post-traumatic stress disorder (PTSD) in sars survivors. Gen. Hosp. Psychiatry. 2010;32(6):590–598. doi: 10.1016/j.genhosppsych.2010.07.007. https://www.ncbi.nlm.nih.gov/pubmed/21112450 Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean C.P., Anderson E.R. Brave men and timid women? A review of the gender differences in fear and anxiety. Clin. Psychol. Rev. 2009;29(6):496–505. doi: 10.1016/j.cpr.2009.05.003. [DOI] [PubMed] [Google Scholar]
- Olff M., Langeland W., Draijer N., Gersons B.P. Gender differences in posttraumatic stress disorder. Psychol. Bull. 2007;133(2):183–204. doi: 10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Perrin P.C., McCabe O.L., Everly G.S., Links J.M. Preparing for an influenza pandemic: mental health considerations. Prehosp. Disaster Med. 2009;24(3):223–230. doi: 10.1017/s1049023x00006853. [DOI] [PubMed] [Google Scholar]
- Pien G.W., Sammel M.D., Freeman E.W., Lin H., DeBlasis T.L. Predictors of sleep quality in women in the menopausal transition. Sleep. 2008;31(7):991–999. [PMC free article] [PubMed] [Google Scholar]
- Richards A., Kanady J.C., Neylan T.C. Sleep disturbance in PTSD and other anxiety-related disorders: an updated review of clinical features, physiological characteristics, and psychological and neurobiological mechanisms. Neuropsychopharmacology. 2019;0:1–19. doi: 10.1038/s41386-019-0486-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soni M., Curran V.H., Kamboj S.K. Identification of a narrow post-ovulatory window of vulnerability to distressing involuntary memories in healthy women. Neurobiol. Learn. Mem. 2013;104:32–38. doi: 10.1016/j.nlm.2013.04.003. [DOI] [PubMed] [Google Scholar]
- Wang L., Zhang L., Armour C., Cao C., Qing Y., Zhang J., ..., Fan G. Assessing the underlying dimensionality of DSM-5 ptsd symptoms in chinese adolescents surviving the 2008 wenchuan earthquake. J. Anxiety Disord. 2015;31:90–97. doi: 10.1016/j.janxdis.2015.02.006. [DOI] [PubMed] [Google Scholar]
- Weathers, F.W., Litz, B.T., Keane, T.M., Palmieri, P.A., Marx, B.P., & Schnurr, P.P. (2013). The PTSD checklist for DSM-5 (PCL-5) – LEC-5 and extended criterion a [Measurement instrument]. Available fromhttps://www.ptsd.va.gov/.
- Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., ..., Hoven C.W. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang R., Sun H., Wu Y., Lu G., Wang Y., Li Q., ..., Sun L. Long-Lasting sex-specific effects based on Emotion- and Cognition-Related behavioral assessment of adult rats after post-traumatic stress disorder from different lengths of maternal separation. Front Psychiatry. 2019;10:289. doi: 10.3389/fpsyt.2019.00289. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.